EP3533467B1 - Procédés et compositions pour augmenter l'activité iduronate 2-sulfatase dans le système nerveux central - Google Patents
Procédés et compositions pour augmenter l'activité iduronate 2-sulfatase dans le système nerveux central Download PDFInfo
- Publication number
- EP3533467B1 EP3533467B1 EP19150184.0A EP19150184A EP3533467B1 EP 3533467 B1 EP3533467 B1 EP 3533467B1 EP 19150184 A EP19150184 A EP 19150184A EP 3533467 B1 EP3533467 B1 EP 3533467B1
- Authority
- EP
- European Patent Office
- Prior art keywords
- ids
- antibody
- amino acid
- hir
- fusion
- Prior art date
- Legal status (The legal status is an assumption and is not a legal conclusion. Google has not performed a legal analysis and makes no representation as to the accuracy of the status listed.)
- Active
Links
- 102100029199 Iduronate 2-sulfatase Human genes 0.000 title claims description 331
- 101710096421 Iduronate 2-sulfatase Proteins 0.000 title claims description 328
- 230000000694 effects Effects 0.000 title claims description 165
- 239000000203 mixture Substances 0.000 title description 66
- 238000000034 method Methods 0.000 title description 51
- 101000852815 Homo sapiens Insulin receptor Proteins 0.000 claims description 164
- 102000047882 human INSR Human genes 0.000 claims description 164
- 230000004927 fusion Effects 0.000 claims description 157
- 230000008499 blood brain barrier function Effects 0.000 claims description 132
- 210000001218 blood-brain barrier Anatomy 0.000 claims description 132
- 108020001507 fusion proteins Proteins 0.000 claims description 111
- 102000037865 fusion proteins Human genes 0.000 claims description 111
- 125000003275 alpha amino acid group Chemical group 0.000 claims description 90
- 125000002924 primary amino group Chemical group [H]N([H])* 0.000 claims description 45
- 210000004899 c-terminal region Anatomy 0.000 claims description 30
- 108060003951 Immunoglobulin Proteins 0.000 claims description 27
- 102000018358 immunoglobulin Human genes 0.000 claims description 27
- 102000006496 Immunoglobulin Heavy Chains Human genes 0.000 claims description 21
- 108010019476 Immunoglobulin Heavy Chains Proteins 0.000 claims description 21
- 102000013463 Immunoglobulin Light Chains Human genes 0.000 claims description 13
- 108010065825 Immunoglobulin Light Chains Proteins 0.000 claims description 13
- 229920000045 Dermatan sulfate Polymers 0.000 claims description 10
- 229920002971 Heparan sulfate Chemical group 0.000 claims description 10
- 102000005262 Sulfatase Human genes 0.000 claims description 10
- 239000000546 pharmaceutical excipient Substances 0.000 claims description 10
- 108060007951 sulfatase Proteins 0.000 claims description 10
- UGJBHEZMOKVTIM-UHFFFAOYSA-N N-formylglycine Chemical compound OC(=O)CNC=O UGJBHEZMOKVTIM-UHFFFAOYSA-N 0.000 claims description 9
- 235000018417 cysteine Nutrition 0.000 claims description 8
- 239000008194 pharmaceutical composition Substances 0.000 claims description 8
- XUJNEKJLAYXESH-UHFFFAOYSA-N cysteine Natural products SCC(N)C(O)=O XUJNEKJLAYXESH-UHFFFAOYSA-N 0.000 claims description 7
- AVJBPWGFOQAPRH-FWMKGIEWSA-L dermatan sulfate Chemical group CC(=O)N[C@H]1[C@H](O)O[C@H](CO)[C@H](OS([O-])(=O)=O)[C@@H]1O[C@H]1[C@H](O)[C@@H](O)[C@H](O)[C@H](C([O-])=O)O1 AVJBPWGFOQAPRH-FWMKGIEWSA-L 0.000 claims description 7
- 229940051593 dermatan sulfate Drugs 0.000 claims description 7
- 230000007062 hydrolysis Effects 0.000 claims description 7
- 238000006460 hydrolysis reaction Methods 0.000 claims description 7
- HTTJABKRGRZYRN-UHFFFAOYSA-N Heparin Chemical group OC1C(NC(=O)C)C(O)OC(COS(O)(=O)=O)C1OC1C(OS(O)(=O)=O)C(O)C(OC2C(C(OS(O)(=O)=O)C(OC3C(C(O)C(O)C(O3)C(O)=O)OS(O)(=O)=O)C(CO)O2)NS(O)(=O)=O)C(C(O)=O)O1 HTTJABKRGRZYRN-UHFFFAOYSA-N 0.000 claims description 5
- 229920000669 heparin Chemical group 0.000 claims description 5
- 229960002897 heparin Drugs 0.000 claims description 5
- PURMPUDWXOWORS-SKNVOMKLSA-N (2r,3s,4s,5r)-2,3,4-trihydroxy-6-oxo-5-sulfooxyhexanoic acid Chemical group OC(=O)[C@H](O)[C@@H](O)[C@H](O)[C@@H](OS(O)(=O)=O)C=O PURMPUDWXOWORS-SKNVOMKLSA-N 0.000 claims description 3
- 230000004048 modification Effects 0.000 claims description 2
- 238000012986 modification Methods 0.000 claims description 2
- 230000001323 posttranslational effect Effects 0.000 claims 1
- 235000001014 amino acid Nutrition 0.000 description 119
- 229940024606 amino acid Drugs 0.000 description 107
- 108090000623 proteins and genes Proteins 0.000 description 92
- 150000001413 amino acids Chemical class 0.000 description 79
- 235000018102 proteins Nutrition 0.000 description 78
- 102000004169 proteins and genes Human genes 0.000 description 78
- 210000004556 brain Anatomy 0.000 description 77
- 210000004027 cell Anatomy 0.000 description 60
- 125000005647 linker group Chemical group 0.000 description 54
- 102100026031 Beta-glucuronidase Human genes 0.000 description 46
- 101000933465 Homo sapiens Beta-glucuronidase Proteins 0.000 description 46
- 210000003169 central nervous system Anatomy 0.000 description 37
- 229940088598 enzyme Drugs 0.000 description 34
- 102000004190 Enzymes Human genes 0.000 description 33
- 108090000790 Enzymes Proteins 0.000 description 33
- 102000005962 receptors Human genes 0.000 description 33
- 108020003175 receptors Proteins 0.000 description 33
- 230000032258 transport Effects 0.000 description 32
- 125000003178 carboxy group Chemical group [H]OC(*)=O 0.000 description 30
- 108090000765 processed proteins & peptides Proteins 0.000 description 28
- DHMQDGOQFOQNFH-UHFFFAOYSA-N Glycine Chemical compound NCC(O)=O DHMQDGOQFOQNFH-UHFFFAOYSA-N 0.000 description 26
- 208000022018 mucopolysaccharidosis type 2 Diseases 0.000 description 26
- 108010076504 Protein Sorting Signals Proteins 0.000 description 24
- 239000000427 antigen Substances 0.000 description 24
- 108091007433 antigens Proteins 0.000 description 24
- 102000036639 antigens Human genes 0.000 description 24
- 102000003746 Insulin Receptor Human genes 0.000 description 22
- 108010001127 Insulin Receptor Proteins 0.000 description 22
- 239000002609 medium Substances 0.000 description 22
- 238000011282 treatment Methods 0.000 description 22
- NOESYZHRGYRDHS-UHFFFAOYSA-N insulin Substances N1C(=O)C(NC(=O)C(CCC(N)=O)NC(=O)C(CCC(O)=O)NC(=O)C(C(C)C)NC(=O)C(NC(=O)CN)C(C)CC)CSSCC(C(NC(CO)C(=O)NC(CC(C)C)C(=O)NC(CC=2C=CC(O)=CC=2)C(=O)NC(CCC(N)=O)C(=O)NC(CC(C)C)C(=O)NC(CCC(O)=O)C(=O)NC(CC(N)=O)C(=O)NC(CC=2C=CC(O)=CC=2)C(=O)NC(CSSCC(NC(=O)C(C(C)C)NC(=O)C(CC(C)C)NC(=O)C(CC=2C=CC(O)=CC=2)NC(=O)C(CC(C)C)NC(=O)C(C)NC(=O)C(CCC(O)=O)NC(=O)C(C(C)C)NC(=O)C(CC(C)C)NC(=O)C(CC=2NC=NC=2)NC(=O)C(CO)NC(=O)CNC2=O)C(=O)NCC(=O)NC(CCC(O)=O)C(=O)NC(CCCNC(N)=N)C(=O)NCC(=O)NC(CC=3C=CC=CC=3)C(=O)NC(CC=3C=CC=CC=3)C(=O)NC(CC=3C=CC(O)=CC=3)C(=O)NC(C(C)O)C(=O)N3C(CCC3)C(=O)NC(CCCCN)C(=O)NC(C)C(O)=O)C(=O)NC(CC(N)=O)C(O)=O)=O)NC(=O)C(C(C)CC)NC(=O)C(CO)NC(=O)C(C(C)O)NC(=O)C1CSSCC2NC(=O)C(CC(C)C)NC(=O)C(NC(=O)C(CCC(N)=O)NC(=O)C(CC(N)=O)NC(=O)C(NC(=O)C(N)CC=1C=CC=CC=1)C(C)C)CC1=CN=CN1 NOESYZHRGYRDHS-UHFFFAOYSA-N 0.000 description 21
- 230000001404 mediated effect Effects 0.000 description 21
- 238000006467 substitution reaction Methods 0.000 description 21
- 239000002299 complementary DNA Substances 0.000 description 20
- 230000014509 gene expression Effects 0.000 description 20
- 101000840540 Homo sapiens Iduronate 2-sulfatase Proteins 0.000 description 19
- 230000008685 targeting Effects 0.000 description 19
- MTCFGRXMJLQNBG-REOHCLBHSA-N (2S)-2-Amino-3-hydroxypropansäure Chemical compound OC[C@H](N)C(O)=O MTCFGRXMJLQNBG-REOHCLBHSA-N 0.000 description 18
- 108020004414 DNA Proteins 0.000 description 18
- 210000002950 fibroblast Anatomy 0.000 description 18
- 239000003814 drug Substances 0.000 description 17
- 102000057422 human IDS Human genes 0.000 description 16
- 201000002273 mucopolysaccharidosis II Diseases 0.000 description 16
- 238000003752 polymerase chain reaction Methods 0.000 description 16
- 230000037396 body weight Effects 0.000 description 15
- 239000013612 plasmid Substances 0.000 description 15
- 230000009885 systemic effect Effects 0.000 description 15
- 108010078791 Carrier Proteins Proteins 0.000 description 14
- 230000001225 therapeutic effect Effects 0.000 description 14
- 101100437500 Homo sapiens GUSB gene Proteins 0.000 description 13
- 239000000243 solution Substances 0.000 description 13
- 125000003295 alanine group Chemical group N[C@@H](C)C(=O)* 0.000 description 12
- 239000003795 chemical substances by application Substances 0.000 description 12
- 208000037265 diseases, disorders, signs and symptoms Diseases 0.000 description 12
- 229940079593 drug Drugs 0.000 description 12
- 239000012634 fragment Substances 0.000 description 12
- 150000007523 nucleic acids Chemical group 0.000 description 12
- 229920002683 Glycosaminoglycan Polymers 0.000 description 11
- 210000004978 chinese hamster ovary cell Anatomy 0.000 description 11
- 230000002255 enzymatic effect Effects 0.000 description 11
- 239000013613 expression plasmid Substances 0.000 description 11
- 229940125396 insulin Drugs 0.000 description 11
- 230000035772 mutation Effects 0.000 description 11
- 239000002773 nucleotide Substances 0.000 description 11
- 125000003729 nucleotide group Chemical group 0.000 description 11
- 239000013598 vector Substances 0.000 description 11
- 238000002965 ELISA Methods 0.000 description 10
- 239000004471 Glycine Substances 0.000 description 10
- 108090001061 Insulin Proteins 0.000 description 10
- 102000004877 Insulin Human genes 0.000 description 10
- 238000001890 transfection Methods 0.000 description 10
- 108010021625 Immunoglobulin Fragments Proteins 0.000 description 9
- 102000008394 Immunoglobulin Fragments Human genes 0.000 description 9
- 241000699666 Mus <mouse, genus> Species 0.000 description 9
- MTCFGRXMJLQNBG-UHFFFAOYSA-N Serine Natural products OCC(N)C(O)=O MTCFGRXMJLQNBG-UHFFFAOYSA-N 0.000 description 9
- 238000006243 chemical reaction Methods 0.000 description 9
- 150000001875 compounds Chemical class 0.000 description 9
- 238000002641 enzyme replacement therapy Methods 0.000 description 9
- 238000009472 formulation Methods 0.000 description 9
- 238000001990 intravenous administration Methods 0.000 description 9
- 102000039446 nucleic acids Human genes 0.000 description 9
- 108020004707 nucleic acids Proteins 0.000 description 9
- 238000002360 preparation method Methods 0.000 description 9
- 102000004196 processed proteins & peptides Human genes 0.000 description 9
- 238000007910 systemic administration Methods 0.000 description 9
- HSHNITRMYYLLCV-UHFFFAOYSA-N 4-methylumbelliferone Chemical compound C1=C(O)C=CC2=C1OC(=O)C=C2C HSHNITRMYYLLCV-UHFFFAOYSA-N 0.000 description 8
- 238000009825 accumulation Methods 0.000 description 8
- 238000003556 assay Methods 0.000 description 8
- 230000008901 benefit Effects 0.000 description 8
- ZXQYGBMAQZUVMI-GCMPRSNUSA-N gamma-cyhalothrin Chemical compound CC1(C)[C@@H](\C=C(/Cl)C(F)(F)F)[C@H]1C(=O)O[C@H](C#N)C1=CC=CC(OC=2C=CC=CC=2)=C1 ZXQYGBMAQZUVMI-GCMPRSNUSA-N 0.000 description 8
- 230000013595 glycosylation Effects 0.000 description 8
- 238000006206 glycosylation reaction Methods 0.000 description 8
- 229920001184 polypeptide Polymers 0.000 description 8
- 108700026244 Open Reading Frames Proteins 0.000 description 7
- XZKQVQKUZMAADP-IMJSIDKUSA-N Ser-Ser Chemical compound OC[C@H](N)C(=O)N[C@@H](CO)C(O)=O XZKQVQKUZMAADP-IMJSIDKUSA-N 0.000 description 7
- -1 Ser-X Chemical class 0.000 description 7
- 230000001588 bifunctional effect Effects 0.000 description 7
- 239000000872 buffer Substances 0.000 description 7
- 239000003937 drug carrier Substances 0.000 description 7
- 230000006870 function Effects 0.000 description 7
- 229940072221 immunoglobulins Drugs 0.000 description 7
- 238000003780 insertion Methods 0.000 description 7
- 230000037431 insertion Effects 0.000 description 7
- 238000007918 intramuscular administration Methods 0.000 description 7
- 210000005259 peripheral blood Anatomy 0.000 description 7
- 239000011886 peripheral blood Substances 0.000 description 7
- 230000002093 peripheral effect Effects 0.000 description 7
- 238000007920 subcutaneous administration Methods 0.000 description 7
- 108020004705 Codon Proteins 0.000 description 6
- 238000001712 DNA sequencing Methods 0.000 description 6
- FBOZXECLQNJBKD-ZDUSSCGKSA-N L-methotrexate Chemical compound C=1N=C2N=C(N)N=C(N)C2=NC=1CN(C)C1=CC=C(C(=O)N[C@@H](CCC(O)=O)C(O)=O)C=C1 FBOZXECLQNJBKD-ZDUSSCGKSA-N 0.000 description 6
- 208000002678 Mucopolysaccharidoses Diseases 0.000 description 6
- 108010022394 Threonine synthase Proteins 0.000 description 6
- 239000004480 active ingredient Substances 0.000 description 6
- 125000000539 amino acid group Chemical group 0.000 description 6
- 239000002775 capsule Substances 0.000 description 6
- 102000004419 dihydrofolate reductase Human genes 0.000 description 6
- 201000010099 disease Diseases 0.000 description 6
- 208000035475 disorder Diseases 0.000 description 6
- 210000004185 liver Anatomy 0.000 description 6
- 229960000485 methotrexate Drugs 0.000 description 6
- 206010028093 mucopolysaccharidosis Diseases 0.000 description 6
- 229940046166 oligodeoxynucleotide Drugs 0.000 description 6
- 108091033319 polynucleotide Proteins 0.000 description 6
- 239000002157 polynucleotide Substances 0.000 description 6
- 102000040430 polynucleotide Human genes 0.000 description 6
- 150000003839 salts Chemical class 0.000 description 6
- 239000000829 suppository Substances 0.000 description 6
- GOJUJUVQIVIZAV-UHFFFAOYSA-N 2-amino-4,6-dichloropyrimidine-5-carbaldehyde Chemical group NC1=NC(Cl)=C(C=O)C(Cl)=N1 GOJUJUVQIVIZAV-UHFFFAOYSA-N 0.000 description 5
- 102100035028 Alpha-L-iduronidase Human genes 0.000 description 5
- 241000283707 Capra Species 0.000 description 5
- 241000701022 Cytomegalovirus Species 0.000 description 5
- 101001019502 Homo sapiens Alpha-L-iduronidase Proteins 0.000 description 5
- 101000599951 Homo sapiens Insulin-like growth factor I Proteins 0.000 description 5
- 102100037852 Insulin-like growth factor I Human genes 0.000 description 5
- 239000012097 Lipofectamine 2000 Substances 0.000 description 5
- 241000124008 Mammalia Species 0.000 description 5
- 108090000901 Transferrin Proteins 0.000 description 5
- 108010006025 bovine growth hormone Proteins 0.000 description 5
- 239000003636 conditioned culture medium Substances 0.000 description 5
- LOKCTEFSRHRXRJ-UHFFFAOYSA-I dipotassium trisodium dihydrogen phosphate hydrogen phosphate dichloride Chemical compound P(=O)(O)(O)[O-].[K+].P(=O)(O)([O-])[O-].[Na+].[Na+].[Cl-].[K+].[Cl-].[Na+] LOKCTEFSRHRXRJ-UHFFFAOYSA-I 0.000 description 5
- 230000009977 dual effect Effects 0.000 description 5
- 238000004520 electroporation Methods 0.000 description 5
- 238000002474 experimental method Methods 0.000 description 5
- 239000013604 expression vector Substances 0.000 description 5
- 238000007421 fluorometric assay Methods 0.000 description 5
- 238000011534 incubation Methods 0.000 description 5
- 238000007912 intraperitoneal administration Methods 0.000 description 5
- 239000007788 liquid Substances 0.000 description 5
- 230000002132 lysosomal effect Effects 0.000 description 5
- 239000011159 matrix material Substances 0.000 description 5
- 208000025919 mucopolysaccharidosis type 7 Diseases 0.000 description 5
- 239000002953 phosphate buffered saline Substances 0.000 description 5
- 230000004481 post-translational protein modification Effects 0.000 description 5
- 210000002966 serum Anatomy 0.000 description 5
- 239000004017 serum-free culture medium Substances 0.000 description 5
- 238000002415 sodium dodecyl sulfate polyacrylamide gel electrophoresis Methods 0.000 description 5
- 239000000758 substrate Substances 0.000 description 5
- 239000003826 tablet Substances 0.000 description 5
- PSGQCCSGKGJLRL-UHFFFAOYSA-N 4-methyl-2h-chromen-2-one Chemical group C1=CC=CC2=C1OC(=O)C=C2C PSGQCCSGKGJLRL-UHFFFAOYSA-N 0.000 description 4
- 108091003079 Bovine Serum Albumin Proteins 0.000 description 4
- 108010047041 Complementarity Determining Regions Proteins 0.000 description 4
- 241000699802 Cricetulus griseus Species 0.000 description 4
- 101150074155 DHFR gene Proteins 0.000 description 4
- 102100028875 Formylglycine-generating enzyme Human genes 0.000 description 4
- 101710192607 Formylglycine-generating enzyme Proteins 0.000 description 4
- 108010054477 Immunoglobulin Fab Fragments Proteins 0.000 description 4
- 102000001706 Immunoglobulin Fab Fragments Human genes 0.000 description 4
- HNDVDQJCIGZPNO-YFKPBYRVSA-N L-histidine Chemical compound OC(=O)[C@@H](N)CC1=CN=CN1 HNDVDQJCIGZPNO-YFKPBYRVSA-N 0.000 description 4
- 102000016267 Leptin Human genes 0.000 description 4
- 108010092277 Leptin Proteins 0.000 description 4
- 241001465754 Metazoa Species 0.000 description 4
- 108091028043 Nucleic acid sequence Proteins 0.000 description 4
- 229910019142 PO4 Inorganic materials 0.000 description 4
- 239000004365 Protease Substances 0.000 description 4
- 101710192761 Serine-type anaerobic sulfatase-maturating enzyme Proteins 0.000 description 4
- FAPWRFPIFSIZLT-UHFFFAOYSA-M Sodium chloride Chemical compound [Na+].[Cl-] FAPWRFPIFSIZLT-UHFFFAOYSA-M 0.000 description 4
- 239000002253 acid Substances 0.000 description 4
- 238000001042 affinity chromatography Methods 0.000 description 4
- 238000004458 analytical method Methods 0.000 description 4
- 230000015572 biosynthetic process Effects 0.000 description 4
- 238000003776 cleavage reaction Methods 0.000 description 4
- 238000010367 cloning Methods 0.000 description 4
- 239000012091 fetal bovine serum Substances 0.000 description 4
- BRZYSWJRSDMWLG-CAXSIQPQSA-N geneticin Natural products O1C[C@@](O)(C)[C@H](NC)[C@@H](O)[C@H]1O[C@@H]1[C@@H](O)[C@H](O[C@@H]2[C@@H]([C@@H](O)[C@H](O)[C@@H](C(C)O)O2)N)[C@@H](N)C[C@H]1N BRZYSWJRSDMWLG-CAXSIQPQSA-N 0.000 description 4
- HNDVDQJCIGZPNO-UHFFFAOYSA-N histidine Natural products OC(=O)C(N)CC1=CN=CN1 HNDVDQJCIGZPNO-UHFFFAOYSA-N 0.000 description 4
- 239000004615 ingredient Substances 0.000 description 4
- 238000001361 intraarterial administration Methods 0.000 description 4
- 238000000185 intracerebroventricular administration Methods 0.000 description 4
- 229940039781 leptin Drugs 0.000 description 4
- NRYBAZVQPHGZNS-ZSOCWYAHSA-N leptin Chemical compound O=C([C@H](CO)NC(=O)[C@H](CC(C)C)NC(=O)[C@H](CC(O)=O)NC(=O)[C@H](CC(C)C)NC(=O)[C@H](CCC(N)=O)NC(=O)[C@H](CC=1C2=CC=CC=C2NC=1)NC(=O)[C@H](CC(C)C)NC(=O)[C@@H](NC(=O)[C@H](CC(O)=O)NC(=O)[C@H](CCC(N)=O)NC(=O)[C@H](CC(C)C)NC(=O)[C@H](CO)NC(=O)CNC(=O)[C@H](CCC(N)=O)NC(=O)[C@@H](N)CC(C)C)CCSC)N1CCC[C@H]1C(=O)NCC(=O)N[C@@H](CS)C(O)=O NRYBAZVQPHGZNS-ZSOCWYAHSA-N 0.000 description 4
- 229920002521 macromolecule Polymers 0.000 description 4
- HQKMJHAJHXVSDF-UHFFFAOYSA-L magnesium stearate Chemical compound [Mg+2].CCCCCCCCCCCCCCCCCC([O-])=O.CCCCCCCCCCCCCCCCCC([O-])=O HQKMJHAJHXVSDF-UHFFFAOYSA-L 0.000 description 4
- 210000001672 ovary Anatomy 0.000 description 4
- 235000021317 phosphate Nutrition 0.000 description 4
- 229920000642 polymer Polymers 0.000 description 4
- 230000000717 retained effect Effects 0.000 description 4
- 238000010839 reverse transcription Methods 0.000 description 4
- 230000002441 reversible effect Effects 0.000 description 4
- 239000000523 sample Substances 0.000 description 4
- 230000007017 scission Effects 0.000 description 4
- 239000002904 solvent Substances 0.000 description 4
- 239000000725 suspension Substances 0.000 description 4
- 238000001262 western blot Methods 0.000 description 4
- OEANUJAFZLQYOD-CXAZCLJRSA-N (2r,3s,4r,5r,6r)-6-[(2r,3r,4r,5r,6r)-5-acetamido-3-hydroxy-2-(hydroxymethyl)-6-methoxyoxan-4-yl]oxy-4,5-dihydroxy-3-methoxyoxane-2-carboxylic acid Chemical compound CC(=O)N[C@H]1[C@H](OC)O[C@H](CO)[C@H](O)[C@@H]1O[C@H]1[C@H](O)[C@@H](O)[C@H](OC)[C@H](C(O)=O)O1 OEANUJAFZLQYOD-CXAZCLJRSA-N 0.000 description 3
- FBPFZTCFMRRESA-KVTDHHQDSA-N D-Mannitol Chemical compound OC[C@@H](O)[C@@H](O)[C@H](O)[C@H](O)CO FBPFZTCFMRRESA-KVTDHHQDSA-N 0.000 description 3
- 102100028146 F-box/WD repeat-containing protein 2 Human genes 0.000 description 3
- 101001060245 Homo sapiens F-box/WD repeat-containing protein 2 Proteins 0.000 description 3
- 101001076292 Homo sapiens Insulin-like growth factor II Proteins 0.000 description 3
- 108090000723 Insulin-Like Growth Factor I Proteins 0.000 description 3
- 102100025947 Insulin-like growth factor II Human genes 0.000 description 3
- WHUUTDBJXJRKMK-VKHMYHEASA-N L-glutamic acid Chemical compound OC(=O)[C@@H](N)CCC(O)=O WHUUTDBJXJRKMK-VKHMYHEASA-N 0.000 description 3
- ZDXPYRJPNDTMRX-VKHMYHEASA-N L-glutamine Chemical compound OC(=O)[C@@H](N)CCC(N)=O ZDXPYRJPNDTMRX-VKHMYHEASA-N 0.000 description 3
- ROHFNLRQFUQHCH-YFKPBYRVSA-N L-leucine Chemical compound CC(C)C[C@H](N)C(O)=O ROHFNLRQFUQHCH-YFKPBYRVSA-N 0.000 description 3
- 101150027568 LC gene Proteins 0.000 description 3
- 108090001030 Lipoproteins Proteins 0.000 description 3
- 102000004895 Lipoproteins Human genes 0.000 description 3
- 208000015439 Lysosomal storage disease Diseases 0.000 description 3
- 229930195725 Mannitol Natural products 0.000 description 3
- 241001529936 Murinae Species 0.000 description 3
- 241000288906 Primates Species 0.000 description 3
- HEMHJVSKTPXQMS-UHFFFAOYSA-M Sodium hydroxide Chemical compound [OH-].[Na+] HEMHJVSKTPXQMS-UHFFFAOYSA-M 0.000 description 3
- 102000013275 Somatomedins Human genes 0.000 description 3
- 102000004338 Transferrin Human genes 0.000 description 3
- 238000010521 absorption reaction Methods 0.000 description 3
- 238000000246 agarose gel electrophoresis Methods 0.000 description 3
- 230000003321 amplification Effects 0.000 description 3
- 239000003242 anti bacterial agent Substances 0.000 description 3
- 238000013459 approach Methods 0.000 description 3
- 239000007864 aqueous solution Substances 0.000 description 3
- 230000004888 barrier function Effects 0.000 description 3
- 210000004369 blood Anatomy 0.000 description 3
- 239000008280 blood Substances 0.000 description 3
- 208000015114 central nervous system disease Diseases 0.000 description 3
- 230000000295 complement effect Effects 0.000 description 3
- 230000003247 decreasing effect Effects 0.000 description 3
- 230000007812 deficiency Effects 0.000 description 3
- 238000012217 deletion Methods 0.000 description 3
- 230000037430 deletion Effects 0.000 description 3
- 238000012377 drug delivery Methods 0.000 description 3
- 210000002472 endoplasmic reticulum Anatomy 0.000 description 3
- 238000005516 engineering process Methods 0.000 description 3
- 108010072166 idursulfase Proteins 0.000 description 3
- 238000000338 in vitro Methods 0.000 description 3
- 238000002347 injection Methods 0.000 description 3
- 239000007924 injection Substances 0.000 description 3
- 230000003834 intracellular effect Effects 0.000 description 3
- 230000014759 maintenance of location Effects 0.000 description 3
- 239000000594 mannitol Substances 0.000 description 3
- 235000010355 mannitol Nutrition 0.000 description 3
- 238000004519 manufacturing process Methods 0.000 description 3
- 239000000463 material Substances 0.000 description 3
- 238000003199 nucleic acid amplification method Methods 0.000 description 3
- 239000006187 pill Substances 0.000 description 3
- 239000000843 powder Substances 0.000 description 3
- 239000003755 preservative agent Substances 0.000 description 3
- 230000002265 prevention Effects 0.000 description 3
- 239000000047 product Substances 0.000 description 3
- 230000000069 prophylactic effect Effects 0.000 description 3
- 238000000746 purification Methods 0.000 description 3
- 230000009467 reduction Effects 0.000 description 3
- 230000002829 reductive effect Effects 0.000 description 3
- 238000011160 research Methods 0.000 description 3
- 238000002741 site-directed mutagenesis Methods 0.000 description 3
- 239000011780 sodium chloride Substances 0.000 description 3
- 239000000126 substance Substances 0.000 description 3
- 229910021653 sulphate ion Inorganic materials 0.000 description 3
- 208000024891 symptom Diseases 0.000 description 3
- 238000003786 synthesis reaction Methods 0.000 description 3
- 229940124597 therapeutic agent Drugs 0.000 description 3
- 239000012581 transferrin Substances 0.000 description 3
- 239000003981 vehicle Substances 0.000 description 3
- HDTRYLNUVZCQOY-UHFFFAOYSA-N α-D-glucopyranosyl-α-D-glucopyranoside Natural products OC1C(O)C(O)C(CO)OC1OC1C(O)C(O)C(O)C(CO)O1 HDTRYLNUVZCQOY-UHFFFAOYSA-N 0.000 description 2
- QTBSBXVTEAMEQO-UHFFFAOYSA-M Acetate Chemical compound CC([O-])=O QTBSBXVTEAMEQO-UHFFFAOYSA-M 0.000 description 2
- GUBGYTABKSRVRQ-XLOQQCSPSA-N Alpha-Lactose Chemical compound O[C@@H]1[C@@H](O)[C@@H](O)[C@@H](CO)O[C@H]1O[C@@H]1[C@@H](CO)O[C@H](O)[C@H](O)[C@H]1O GUBGYTABKSRVRQ-XLOQQCSPSA-N 0.000 description 2
- 239000004475 Arginine Substances 0.000 description 2
- DCXYFEDJOCDNAF-UHFFFAOYSA-N Asparagine Natural products OC(=O)C(N)CC(N)=O DCXYFEDJOCDNAF-UHFFFAOYSA-N 0.000 description 2
- 108090001008 Avidin Proteins 0.000 description 2
- 241000167854 Bourreria succulenta Species 0.000 description 2
- KRKNYBCHXYNGOX-UHFFFAOYSA-K Citrate Chemical compound [O-]C(=O)CC(O)(CC([O-])=O)C([O-])=O KRKNYBCHXYNGOX-UHFFFAOYSA-K 0.000 description 2
- 229920002261 Corn starch Polymers 0.000 description 2
- FBPFZTCFMRRESA-FSIIMWSLSA-N D-Glucitol Natural products OC[C@H](O)[C@H](O)[C@@H](O)[C@H](O)CO FBPFZTCFMRRESA-FSIIMWSLSA-N 0.000 description 2
- FBPFZTCFMRRESA-JGWLITMVSA-N D-glucitol Chemical compound OC[C@H](O)[C@@H](O)[C@H](O)[C@H](O)CO FBPFZTCFMRRESA-JGWLITMVSA-N 0.000 description 2
- 239000006144 Dulbecco’s modified Eagle's medium Substances 0.000 description 2
- 241000283086 Equidae Species 0.000 description 2
- 108010010803 Gelatin Proteins 0.000 description 2
- 241000282412 Homo Species 0.000 description 2
- CPELXLSAUQHCOX-UHFFFAOYSA-N Hydrogen bromide Chemical class Br CPELXLSAUQHCOX-UHFFFAOYSA-N 0.000 description 2
- 108010067060 Immunoglobulin Variable Region Proteins 0.000 description 2
- 102000017727 Immunoglobulin Variable Region Human genes 0.000 description 2
- 108091092195 Intron Proteins 0.000 description 2
- QNAYBMKLOCPYGJ-REOHCLBHSA-N L-alanine Chemical compound C[C@H](N)C(O)=O QNAYBMKLOCPYGJ-REOHCLBHSA-N 0.000 description 2
- ODKSFYDXXFIFQN-BYPYZUCNSA-P L-argininium(2+) Chemical compound NC(=[NH2+])NCCC[C@H]([NH3+])C(O)=O ODKSFYDXXFIFQN-BYPYZUCNSA-P 0.000 description 2
- DCXYFEDJOCDNAF-REOHCLBHSA-N L-asparagine Chemical compound OC(=O)[C@@H](N)CC(N)=O DCXYFEDJOCDNAF-REOHCLBHSA-N 0.000 description 2
- CKLJMWTZIZZHCS-REOHCLBHSA-N L-aspartic acid Chemical compound OC(=O)[C@@H](N)CC(O)=O CKLJMWTZIZZHCS-REOHCLBHSA-N 0.000 description 2
- AEMOLEFTQBMNLQ-HNFCZKTMSA-N L-idopyranuronic acid Chemical compound OC1O[C@@H](C(O)=O)[C@@H](O)[C@H](O)[C@H]1O AEMOLEFTQBMNLQ-HNFCZKTMSA-N 0.000 description 2
- AGPKZVBTJJNPAG-WHFBIAKZSA-N L-isoleucine Chemical compound CC[C@H](C)[C@H](N)C(O)=O AGPKZVBTJJNPAG-WHFBIAKZSA-N 0.000 description 2
- KDXKERNSBIXSRK-YFKPBYRVSA-N L-lysine Chemical compound NCCCC[C@H](N)C(O)=O KDXKERNSBIXSRK-YFKPBYRVSA-N 0.000 description 2
- FFEARJCKVFRZRR-BYPYZUCNSA-N L-methionine Chemical compound CSCC[C@H](N)C(O)=O FFEARJCKVFRZRR-BYPYZUCNSA-N 0.000 description 2
- LRQKBLKVPFOOQJ-YFKPBYRVSA-N L-norleucine Chemical compound CCCC[C@H]([NH3+])C([O-])=O LRQKBLKVPFOOQJ-YFKPBYRVSA-N 0.000 description 2
- COLNVLDHVKWLRT-QMMMGPOBSA-N L-phenylalanine Chemical compound OC(=O)[C@@H](N)CC1=CC=CC=C1 COLNVLDHVKWLRT-QMMMGPOBSA-N 0.000 description 2
- AYFVYJQAPQTCCC-GBXIJSLDSA-N L-threonine Chemical compound C[C@@H](O)[C@H](N)C(O)=O AYFVYJQAPQTCCC-GBXIJSLDSA-N 0.000 description 2
- QIVBCDIJIAJPQS-VIFPVBQESA-N L-tryptophane Chemical compound C1=CC=C2C(C[C@H](N)C(O)=O)=CNC2=C1 QIVBCDIJIAJPQS-VIFPVBQESA-N 0.000 description 2
- OUYCCCASQSFEME-QMMMGPOBSA-N L-tyrosine Chemical compound OC(=O)[C@@H](N)CC1=CC=C(O)C=C1 OUYCCCASQSFEME-QMMMGPOBSA-N 0.000 description 2
- KZSNJWFQEVHDMF-BYPYZUCNSA-N L-valine Chemical compound CC(C)[C@H](N)C(O)=O KZSNJWFQEVHDMF-BYPYZUCNSA-N 0.000 description 2
- GUBGYTABKSRVRQ-QKKXKWKRSA-N Lactose Natural products OC[C@H]1O[C@@H](O[C@H]2[C@H](O)[C@@H](O)C(O)O[C@@H]2CO)[C@H](O)[C@@H](O)[C@H]1O GUBGYTABKSRVRQ-QKKXKWKRSA-N 0.000 description 2
- ROHFNLRQFUQHCH-UHFFFAOYSA-N Leucine Natural products CC(C)CC(N)C(O)=O ROHFNLRQFUQHCH-UHFFFAOYSA-N 0.000 description 2
- KDXKERNSBIXSRK-UHFFFAOYSA-N Lysine Natural products NCCCCC(N)C(O)=O KDXKERNSBIXSRK-UHFFFAOYSA-N 0.000 description 2
- 239000004472 Lysine Substances 0.000 description 2
- 241000282560 Macaca mulatta Species 0.000 description 2
- 208000036626 Mental retardation Diseases 0.000 description 2
- 206010056893 Mucopolysaccharidosis VII Diseases 0.000 description 2
- 241000699660 Mus musculus Species 0.000 description 2
- 241000699670 Mus sp. Species 0.000 description 2
- 101001055320 Myxine glutinosa Insulin-like growth factor Proteins 0.000 description 2
- 108091007491 NSP3 Papain-like protease domains Proteins 0.000 description 2
- 241001045988 Neogene Species 0.000 description 2
- 108090000526 Papain Proteins 0.000 description 2
- 102000057297 Pepsin A Human genes 0.000 description 2
- 108090000284 Pepsin A Proteins 0.000 description 2
- 108091005804 Peptidases Proteins 0.000 description 2
- 102000003992 Peroxidases Human genes 0.000 description 2
- ISWSIDIOOBJBQZ-UHFFFAOYSA-N Phenol Chemical compound OC1=CC=CC=C1 ISWSIDIOOBJBQZ-UHFFFAOYSA-N 0.000 description 2
- XBDQKXXYIPTUBI-UHFFFAOYSA-N Propionic acid Chemical class CCC(O)=O XBDQKXXYIPTUBI-UHFFFAOYSA-N 0.000 description 2
- 238000012228 RNA interference-mediated gene silencing Methods 0.000 description 2
- 102000007056 Recombinant Fusion Proteins Human genes 0.000 description 2
- 108010008281 Recombinant Fusion Proteins Proteins 0.000 description 2
- 102100037486 Reverse transcriptase/ribonuclease H Human genes 0.000 description 2
- WOUIMBGNEUWXQG-VKHMYHEASA-N Ser-Gly Chemical compound OC[C@H](N)C(=O)NCC(O)=O WOUIMBGNEUWXQG-VKHMYHEASA-N 0.000 description 2
- CDBYLPFSWZWCQE-UHFFFAOYSA-L Sodium Carbonate Chemical compound [Na+].[Na+].[O-]C([O-])=O CDBYLPFSWZWCQE-UHFFFAOYSA-L 0.000 description 2
- UIIMBOGNXHQVGW-UHFFFAOYSA-M Sodium bicarbonate Chemical compound [Na+].OC([O-])=O UIIMBOGNXHQVGW-UHFFFAOYSA-M 0.000 description 2
- 229930006000 Sucrose Natural products 0.000 description 2
- CZMRCDWAGMRECN-UGDNZRGBSA-N Sucrose Chemical compound O[C@H]1[C@H](O)[C@@H](CO)O[C@@]1(CO)O[C@@H]1[C@H](O)[C@@H](O)[C@H](O)[C@@H](CO)O1 CZMRCDWAGMRECN-UGDNZRGBSA-N 0.000 description 2
- QAOWNCQODCNURD-UHFFFAOYSA-L Sulfate Chemical compound [O-]S([O-])(=O)=O QAOWNCQODCNURD-UHFFFAOYSA-L 0.000 description 2
- 239000006180 TBST buffer Substances 0.000 description 2
- AYFVYJQAPQTCCC-UHFFFAOYSA-N Threonine Natural products CC(O)C(N)C(O)=O AYFVYJQAPQTCCC-UHFFFAOYSA-N 0.000 description 2
- 239000004473 Threonine Substances 0.000 description 2
- IQFYYKKMVGJFEH-XLPZGREQSA-N Thymidine Chemical compound O=C1NC(=O)C(C)=CN1[C@@H]1O[C@H](CO)[C@@H](O)C1 IQFYYKKMVGJFEH-XLPZGREQSA-N 0.000 description 2
- HDTRYLNUVZCQOY-WSWWMNSNSA-N Trehalose Natural products O[C@@H]1[C@@H](O)[C@@H](O)[C@@H](CO)O[C@@H]1O[C@@H]1[C@H](O)[C@@H](O)[C@@H](O)[C@@H](CO)O1 HDTRYLNUVZCQOY-WSWWMNSNSA-N 0.000 description 2
- QIVBCDIJIAJPQS-UHFFFAOYSA-N Tryptophan Natural products C1=CC=C2C(CC(N)C(O)=O)=CNC2=C1 QIVBCDIJIAJPQS-UHFFFAOYSA-N 0.000 description 2
- XSQUKJJJFZCRTK-UHFFFAOYSA-N Urea Chemical compound NC(N)=O XSQUKJJJFZCRTK-UHFFFAOYSA-N 0.000 description 2
- KZSNJWFQEVHDMF-UHFFFAOYSA-N Valine Natural products CC(C)C(N)C(O)=O KZSNJWFQEVHDMF-UHFFFAOYSA-N 0.000 description 2
- 108010046516 Wheat Germ Agglutinins Proteins 0.000 description 2
- 150000001242 acetic acid derivatives Chemical class 0.000 description 2
- 239000000654 additive Substances 0.000 description 2
- 235000004279 alanine Nutrition 0.000 description 2
- HDTRYLNUVZCQOY-LIZSDCNHSA-N alpha,alpha-trehalose Chemical compound O[C@@H]1[C@@H](O)[C@H](O)[C@@H](CO)O[C@@H]1O[C@@H]1[C@H](O)[C@@H](O)[C@H](O)[C@@H](CO)O1 HDTRYLNUVZCQOY-LIZSDCNHSA-N 0.000 description 2
- 230000000844 anti-bacterial effect Effects 0.000 description 2
- 230000000692 anti-sense effect Effects 0.000 description 2
- 229940121375 antifungal agent Drugs 0.000 description 2
- 239000003429 antifungal agent Substances 0.000 description 2
- ODKSFYDXXFIFQN-UHFFFAOYSA-N arginine Natural products OC(=O)C(N)CCCNC(N)=N ODKSFYDXXFIFQN-UHFFFAOYSA-N 0.000 description 2
- 235000009697 arginine Nutrition 0.000 description 2
- 235000009582 asparagine Nutrition 0.000 description 2
- 229960001230 asparagine Drugs 0.000 description 2
- 230000009286 beneficial effect Effects 0.000 description 2
- 150000001558 benzoic acid derivatives Chemical class 0.000 description 2
- 239000011230 binding agent Substances 0.000 description 2
- 150000001720 carbohydrates Chemical class 0.000 description 2
- 235000014633 carbohydrates Nutrition 0.000 description 2
- 239000000969 carrier Substances 0.000 description 2
- 210000000170 cell membrane Anatomy 0.000 description 2
- 239000006285 cell suspension Substances 0.000 description 2
- 230000008859 change Effects 0.000 description 2
- 235000019693 cherries Nutrition 0.000 description 2
- OSASVXMJTNOKOY-UHFFFAOYSA-N chlorobutanol Chemical compound CC(C)(O)C(Cl)(Cl)Cl OSASVXMJTNOKOY-UHFFFAOYSA-N 0.000 description 2
- 238000000576 coating method Methods 0.000 description 2
- 238000002648 combination therapy Methods 0.000 description 2
- 239000000470 constituent Substances 0.000 description 2
- 238000010276 construction Methods 0.000 description 2
- 239000008120 corn starch Substances 0.000 description 2
- 229940099112 cornstarch Drugs 0.000 description 2
- 125000000151 cysteine group Chemical group N[C@@H](CS)C(=O)* 0.000 description 2
- 230000007547 defect Effects 0.000 description 2
- 238000013461 design Methods 0.000 description 2
- 239000003599 detergent Substances 0.000 description 2
- 238000009792 diffusion process Methods 0.000 description 2
- 239000000539 dimer Substances 0.000 description 2
- 239000002612 dispersion medium Substances 0.000 description 2
- 230000008029 eradication Effects 0.000 description 2
- 230000005284 excitation Effects 0.000 description 2
- 238000010195 expression analysis Methods 0.000 description 2
- 239000012530 fluid Substances 0.000 description 2
- 235000003599 food sweetener Nutrition 0.000 description 2
- 239000008273 gelatin Substances 0.000 description 2
- 229920000159 gelatin Polymers 0.000 description 2
- 235000019322 gelatine Nutrition 0.000 description 2
- 235000011852 gelatine desserts Nutrition 0.000 description 2
- 230000009368 gene silencing by RNA Effects 0.000 description 2
- ZDXPYRJPNDTMRX-UHFFFAOYSA-N glutamine Natural products OC(=O)C(N)CCC(N)=O ZDXPYRJPNDTMRX-UHFFFAOYSA-N 0.000 description 2
- 235000004554 glutamine Nutrition 0.000 description 2
- YMAWOPBAYDPSLA-UHFFFAOYSA-N glycylglycine Chemical compound [NH3+]CC(=O)NCC([O-])=O YMAWOPBAYDPSLA-UHFFFAOYSA-N 0.000 description 2
- 230000012010 growth Effects 0.000 description 2
- 230000036541 health Effects 0.000 description 2
- 210000002216 heart Anatomy 0.000 description 2
- 150000003840 hydrochlorides Chemical class 0.000 description 2
- FDGQSTZJBFJUBT-UHFFFAOYSA-N hypoxanthine Chemical compound O=C1NC=NC2=C1NC=N2 FDGQSTZJBFJUBT-UHFFFAOYSA-N 0.000 description 2
- 229960002396 idursulfase Drugs 0.000 description 2
- 230000001900 immune effect Effects 0.000 description 2
- 238000003018 immunoassay Methods 0.000 description 2
- 238000010348 incorporation Methods 0.000 description 2
- 239000007972 injectable composition Substances 0.000 description 2
- 229910052500 inorganic mineral Inorganic materials 0.000 description 2
- 238000010253 intravenous injection Methods 0.000 description 2
- AGPKZVBTJJNPAG-UHFFFAOYSA-N isoleucine Natural products CCC(C)C(N)C(O)=O AGPKZVBTJJNPAG-UHFFFAOYSA-N 0.000 description 2
- 229960000310 isoleucine Drugs 0.000 description 2
- 239000007951 isotonicity adjuster Substances 0.000 description 2
- 238000005304 joining Methods 0.000 description 2
- 239000008101 lactose Substances 0.000 description 2
- 150000002605 large molecules Chemical class 0.000 description 2
- 238000012417 linear regression Methods 0.000 description 2
- 150000002632 lipids Chemical class 0.000 description 2
- 235000019359 magnesium stearate Nutrition 0.000 description 2
- 150000002690 malonic acid derivatives Chemical class 0.000 description 2
- 239000012528 membrane Substances 0.000 description 2
- MYWUZJCMWCOHBA-VIFPVBQESA-N methamphetamine Chemical compound CN[C@@H](C)CC1=CC=CC=C1 MYWUZJCMWCOHBA-VIFPVBQESA-N 0.000 description 2
- 229930182817 methionine Natural products 0.000 description 2
- 244000005700 microbiome Species 0.000 description 2
- 239000011707 mineral Substances 0.000 description 2
- 235000010755 mineral Nutrition 0.000 description 2
- 101150091879 neo gene Proteins 0.000 description 2
- 230000004770 neurodegeneration Effects 0.000 description 2
- 239000008203 oral pharmaceutical composition Substances 0.000 description 2
- 150000007524 organic acids Chemical class 0.000 description 2
- 235000005985 organic acids Nutrition 0.000 description 2
- 229940055729 papain Drugs 0.000 description 2
- 235000019834 papain Nutrition 0.000 description 2
- 238000007911 parenteral administration Methods 0.000 description 2
- 230000036961 partial effect Effects 0.000 description 2
- 230000001575 pathological effect Effects 0.000 description 2
- 229940111202 pepsin Drugs 0.000 description 2
- 108040007629 peroxidase activity proteins Proteins 0.000 description 2
- COLNVLDHVKWLRT-UHFFFAOYSA-N phenylalanine Natural products OC(=O)C(N)CC1=CC=CC=C1 COLNVLDHVKWLRT-UHFFFAOYSA-N 0.000 description 2
- NBIIXXVUZAFLBC-UHFFFAOYSA-K phosphate Chemical compound [O-]P([O-])([O-])=O NBIIXXVUZAFLBC-UHFFFAOYSA-K 0.000 description 2
- 239000010452 phosphate Substances 0.000 description 2
- 150000003013 phosphoric acid derivatives Chemical class 0.000 description 2
- 229920003023 plastic Polymers 0.000 description 2
- 239000004033 plastic Substances 0.000 description 2
- 238000007747 plating Methods 0.000 description 2
- 239000000244 polyoxyethylene sorbitan monooleate Substances 0.000 description 2
- 235000010482 polyoxyethylene sorbitan monooleate Nutrition 0.000 description 2
- 229940068968 polysorbate 80 Drugs 0.000 description 2
- 229920000053 polysorbate 80 Polymers 0.000 description 2
- 230000008569 process Effects 0.000 description 2
- 238000011321 prophylaxis Methods 0.000 description 2
- 235000019419 proteases Nutrition 0.000 description 2
- 230000004853 protein function Effects 0.000 description 2
- 230000005180 public health Effects 0.000 description 2
- 230000002685 pulmonary effect Effects 0.000 description 2
- 238000002708 random mutagenesis Methods 0.000 description 2
- 230000001105 regulatory effect Effects 0.000 description 2
- 238000012552 review Methods 0.000 description 2
- CVHZOJJKTDOEJC-UHFFFAOYSA-N saccharin Chemical compound C1=CC=C2C(=O)NS(=O)(=O)C2=C1 CVHZOJJKTDOEJC-UHFFFAOYSA-N 0.000 description 2
- 230000028327 secretion Effects 0.000 description 2
- 229940126586 small molecule drug Drugs 0.000 description 2
- 150000003384 small molecules Chemical class 0.000 description 2
- 229910052938 sodium sulfate Inorganic materials 0.000 description 2
- 239000000600 sorbitol Substances 0.000 description 2
- 210000000278 spinal cord Anatomy 0.000 description 2
- 239000007921 spray Substances 0.000 description 2
- UCSJYZPVAKXKNQ-HZYVHMACSA-N streptomycin Chemical compound CN[C@H]1[C@H](O)[C@@H](O)[C@H](CO)O[C@H]1O[C@@H]1[C@](C=O)(O)[C@H](C)O[C@H]1O[C@@H]1[C@@H](NC(N)=N)[C@H](O)[C@@H](NC(N)=N)[C@H](O)[C@H]1O UCSJYZPVAKXKNQ-HZYVHMACSA-N 0.000 description 2
- 239000005720 sucrose Substances 0.000 description 2
- 235000000346 sugar Nutrition 0.000 description 2
- 150000003467 sulfuric acid derivatives Chemical class 0.000 description 2
- 239000003765 sweetening agent Substances 0.000 description 2
- 239000006188 syrup Substances 0.000 description 2
- 235000020357 syrup Nutrition 0.000 description 2
- 238000002560 therapeutic procedure Methods 0.000 description 2
- 238000011830 transgenic mouse model Methods 0.000 description 2
- OUYCCCASQSFEME-UHFFFAOYSA-N tyrosine Natural products OC(=O)C(N)CC1=CC=C(O)C=C1 OUYCCCASQSFEME-UHFFFAOYSA-N 0.000 description 2
- 239000004474 valine Substances 0.000 description 2
- FDKWRPBBCBCIGA-REOHCLBHSA-N (2r)-2-azaniumyl-3-$l^{1}-selanylpropanoate Chemical compound [Se]C[C@H](N)C(O)=O FDKWRPBBCBCIGA-REOHCLBHSA-N 0.000 description 1
- 108091032973 (ribonucleotides)n+m Proteins 0.000 description 1
- UKAUYVFTDYCKQA-UHFFFAOYSA-N -2-Amino-4-hydroxybutanoic acid Natural products OC(=O)C(N)CCO UKAUYVFTDYCKQA-UHFFFAOYSA-N 0.000 description 1
- VGONTNSXDCQUGY-RRKCRQDMSA-N 2'-deoxyinosine Chemical group C1[C@H](O)[C@@H](CO)O[C@H]1N1C(N=CNC2=O)=C2N=C1 VGONTNSXDCQUGY-RRKCRQDMSA-N 0.000 description 1
- JUAGNSFMKLTCCT-UHFFFAOYSA-N 2-aminoacetic acid;carbonic acid Chemical compound OC(O)=O.NCC(O)=O JUAGNSFMKLTCCT-UHFFFAOYSA-N 0.000 description 1
- 108020005065 3' Flanking Region Proteins 0.000 description 1
- IPWKGIFRRBGCJO-IMJSIDKUSA-N Ala-Ser Chemical compound C[C@H]([NH3+])C(=O)N[C@@H](CO)C([O-])=O IPWKGIFRRBGCJO-IMJSIDKUSA-N 0.000 description 1
- 108010032595 Antibody Binding Sites Proteins 0.000 description 1
- 241000416162 Astragalus gummifer Species 0.000 description 1
- 238000000035 BCA protein assay Methods 0.000 description 1
- DWRXFEITVBNRMK-UHFFFAOYSA-N Beta-D-1-Arabinofuranosylthymine Natural products O=C1NC(=O)C(C)=CN1C1C(O)C(O)C(CO)O1 DWRXFEITVBNRMK-UHFFFAOYSA-N 0.000 description 1
- 125000001433 C-terminal amino-acid group Chemical group 0.000 description 1
- UXVMQQNJUSDDNG-UHFFFAOYSA-L Calcium chloride Chemical compound [Cl-].[Cl-].[Ca+2] UXVMQQNJUSDDNG-UHFFFAOYSA-L 0.000 description 1
- OKTJSMMVPCPJKN-UHFFFAOYSA-N Carbon Chemical compound [C] OKTJSMMVPCPJKN-UHFFFAOYSA-N 0.000 description 1
- 108091026890 Coding region Proteins 0.000 description 1
- 108020004635 Complementary DNA Proteins 0.000 description 1
- FDKWRPBBCBCIGA-UWTATZPHSA-N D-Selenocysteine Natural products [Se]C[C@@H](N)C(O)=O FDKWRPBBCBCIGA-UWTATZPHSA-N 0.000 description 1
- 102000016928 DNA-directed DNA polymerase Human genes 0.000 description 1
- 108010014303 DNA-directed DNA polymerase Proteins 0.000 description 1
- 206010011878 Deafness Diseases 0.000 description 1
- 208000016192 Demyelinating disease Diseases 0.000 description 1
- 206010012305 Demyelination Diseases 0.000 description 1
- 235000019739 Dicalciumphosphate Nutrition 0.000 description 1
- BWGNESOTFCXPMA-UHFFFAOYSA-N Dihydrogen disulfide Chemical compound SS BWGNESOTFCXPMA-UHFFFAOYSA-N 0.000 description 1
- 208000034454 F12-related hereditary angioedema with normal C1Inh Diseases 0.000 description 1
- 206010018341 Gliosis Diseases 0.000 description 1
- WHUUTDBJXJRKMK-UHFFFAOYSA-N Glutamic acid Natural products OC(=O)C(N)CCC(O)=O WHUUTDBJXJRKMK-UHFFFAOYSA-N 0.000 description 1
- BCCRXDTUTZHDEU-VKHMYHEASA-N Gly-Ser Chemical compound NCC(=O)N[C@@H](CO)C(O)=O BCCRXDTUTZHDEU-VKHMYHEASA-N 0.000 description 1
- 102000003886 Glycoproteins Human genes 0.000 description 1
- 108090000288 Glycoproteins Proteins 0.000 description 1
- 241000700721 Hepatitis B virus Species 0.000 description 1
- 101000998953 Homo sapiens Immunoglobulin heavy variable 1-2 Proteins 0.000 description 1
- 101001008255 Homo sapiens Immunoglobulin kappa variable 1D-8 Proteins 0.000 description 1
- 101001047628 Homo sapiens Immunoglobulin kappa variable 2-29 Proteins 0.000 description 1
- 101001008321 Homo sapiens Immunoglobulin kappa variable 2D-26 Proteins 0.000 description 1
- 101001047619 Homo sapiens Immunoglobulin kappa variable 3-20 Proteins 0.000 description 1
- 101001008263 Homo sapiens Immunoglobulin kappa variable 3D-15 Proteins 0.000 description 1
- 101000976075 Homo sapiens Insulin Proteins 0.000 description 1
- UGQMRVRMYYASKQ-UHFFFAOYSA-N Hypoxanthine nucleoside Natural products OC1C(O)C(CO)OC1N1C(NC=NC2=O)=C2N=C1 UGQMRVRMYYASKQ-UHFFFAOYSA-N 0.000 description 1
- 108010003381 Iduronidase Proteins 0.000 description 1
- 102000004627 Iduronidase Human genes 0.000 description 1
- 102000009786 Immunoglobulin Constant Regions Human genes 0.000 description 1
- 108010009817 Immunoglobulin Constant Regions Proteins 0.000 description 1
- 102100036887 Immunoglobulin heavy variable 1-2 Human genes 0.000 description 1
- 102100022949 Immunoglobulin kappa variable 2-29 Human genes 0.000 description 1
- XUJNEKJLAYXESH-REOHCLBHSA-N L-Cysteine Chemical compound SC[C@H](N)C(O)=O XUJNEKJLAYXESH-REOHCLBHSA-N 0.000 description 1
- ONIBWKKTOPOVIA-BYPYZUCNSA-N L-Proline Chemical compound OC(=O)[C@@H]1CCCN1 ONIBWKKTOPOVIA-BYPYZUCNSA-N 0.000 description 1
- DEFJQIDDEAULHB-IMJSIDKUSA-N L-alanyl-L-alanine Chemical compound C[C@H](N)C(=O)N[C@@H](C)C(O)=O DEFJQIDDEAULHB-IMJSIDKUSA-N 0.000 description 1
- UKAUYVFTDYCKQA-VKHMYHEASA-N L-homoserine Chemical compound OC(=O)[C@@H](N)CCO UKAUYVFTDYCKQA-VKHMYHEASA-N 0.000 description 1
- QEFRNWWLZKMPFJ-ZXPFJRLXSA-N L-methionine (R)-S-oxide Chemical compound C[S@@](=O)CC[C@H]([NH3+])C([O-])=O QEFRNWWLZKMPFJ-ZXPFJRLXSA-N 0.000 description 1
- QEFRNWWLZKMPFJ-UHFFFAOYSA-N L-methionine sulphoxide Natural products CS(=O)CCC(N)C(O)=O QEFRNWWLZKMPFJ-UHFFFAOYSA-N 0.000 description 1
- 102000007330 LDL Lipoproteins Human genes 0.000 description 1
- 102000000853 LDL receptors Human genes 0.000 description 1
- 108010001831 LDL receptors Proteins 0.000 description 1
- 235000010643 Leucaena leucocephala Nutrition 0.000 description 1
- 240000007472 Leucaena leucocephala Species 0.000 description 1
- 244000246386 Mentha pulegium Species 0.000 description 1
- 235000016257 Mentha pulegium Nutrition 0.000 description 1
- 235000004357 Mentha x piperita Nutrition 0.000 description 1
- 206010056886 Mucopolysaccharidosis I Diseases 0.000 description 1
- 206010028095 Mucopolysaccharidosis IV Diseases 0.000 description 1
- 208000028781 Mucopolysaccharidosis type 1 Diseases 0.000 description 1
- 101000931108 Mus musculus DNA (cytosine-5)-methyltransferase 1 Proteins 0.000 description 1
- 241000238367 Mya arenaria Species 0.000 description 1
- 229930193140 Neomycin Natural products 0.000 description 1
- 208000012902 Nervous system disease Diseases 0.000 description 1
- 108091005461 Nucleic proteins Proteins 0.000 description 1
- 108091034117 Oligonucleotide Proteins 0.000 description 1
- 241000283973 Oryctolagus cuniculus Species 0.000 description 1
- 102000016979 Other receptors Human genes 0.000 description 1
- 238000012408 PCR amplification Methods 0.000 description 1
- 229930182555 Penicillin Natural products 0.000 description 1
- JGSARLDLIJGVTE-MBNYWOFBSA-N Penicillin G Chemical compound N([C@H]1[C@H]2SC([C@@H](N2C1=O)C(O)=O)(C)C)C(=O)CC1=CC=CC=C1 JGSARLDLIJGVTE-MBNYWOFBSA-N 0.000 description 1
- 206010035226 Plasma cell myeloma Diseases 0.000 description 1
- ONIBWKKTOPOVIA-UHFFFAOYSA-N Proline Natural products OC(=O)C1CCCN1 ONIBWKKTOPOVIA-UHFFFAOYSA-N 0.000 description 1
- 101710118538 Protease Proteins 0.000 description 1
- 108010029485 Protein Isoforms Proteins 0.000 description 1
- 102000001708 Protein Isoforms Human genes 0.000 description 1
- 108020004511 Recombinant DNA Proteins 0.000 description 1
- 108091028664 Ribonucleotide Proteins 0.000 description 1
- SSJMZMUVNKEENT-IMJSIDKUSA-N Ser-Ala Chemical compound OC(=O)[C@H](C)NC(=O)[C@@H](N)CO SSJMZMUVNKEENT-IMJSIDKUSA-N 0.000 description 1
- 229920001800 Shellac Polymers 0.000 description 1
- 201000001828 Sly syndrome Diseases 0.000 description 1
- 239000004280 Sodium formate Substances 0.000 description 1
- 229920002472 Starch Polymers 0.000 description 1
- RYYWUUFWQRZTIU-UHFFFAOYSA-N Thiophosphoric acid Chemical class OP(O)(S)=O RYYWUUFWQRZTIU-UHFFFAOYSA-N 0.000 description 1
- 229920001615 Tragacanth Polymers 0.000 description 1
- 108010033576 Transferrin Receptors Proteins 0.000 description 1
- 102000007238 Transferrin Receptors Human genes 0.000 description 1
- 108700019146 Transgenes Proteins 0.000 description 1
- 229920004890 Triton X-100 Polymers 0.000 description 1
- 239000013504 Triton X-100 Substances 0.000 description 1
- 241000251539 Vertebrata <Metazoa> Species 0.000 description 1
- YVXXRFJXBIWXFT-UHFFFAOYSA-N [1-hydroxy-2-(hydroxymethyl)butan-2-yl]azanium;(4-nitrophenyl) phosphate Chemical compound CCC(N)(CO)CO.CCC(N)(CO)CO.OP(O)(=O)OC1=CC=C([N+]([O-])=O)C=C1 YVXXRFJXBIWXFT-UHFFFAOYSA-N 0.000 description 1
- 239000003070 absorption delaying agent Substances 0.000 description 1
- 230000009471 action Effects 0.000 description 1
- 239000013543 active substance Substances 0.000 description 1
- 230000002411 adverse Effects 0.000 description 1
- 239000000443 aerosol Substances 0.000 description 1
- 239000011543 agarose gel Substances 0.000 description 1
- 230000002776 aggregation Effects 0.000 description 1
- 238000004220 aggregation Methods 0.000 description 1
- 108010056243 alanylalanine Proteins 0.000 description 1
- 229940022705 aldurazyme Drugs 0.000 description 1
- 239000000783 alginic acid Substances 0.000 description 1
- 235000010443 alginic acid Nutrition 0.000 description 1
- 229920000615 alginic acid Polymers 0.000 description 1
- 229960001126 alginic acid Drugs 0.000 description 1
- 150000004781 alginic acids Chemical class 0.000 description 1
- 230000000172 allergic effect Effects 0.000 description 1
- 125000003277 amino group Chemical group 0.000 description 1
- 238000000137 annealing Methods 0.000 description 1
- 230000000845 anti-microbial effect Effects 0.000 description 1
- 229940088710 antibiotic agent Drugs 0.000 description 1
- 230000000890 antigenic effect Effects 0.000 description 1
- 229940125715 antihistaminic agent Drugs 0.000 description 1
- 239000000739 antihistaminic agent Substances 0.000 description 1
- 239000012736 aqueous medium Substances 0.000 description 1
- 229940009098 aspartate Drugs 0.000 description 1
- 235000003704 aspartic acid Nutrition 0.000 description 1
- 208000006673 asthma Diseases 0.000 description 1
- 208000037875 astrocytosis Diseases 0.000 description 1
- 230000007341 astrogliosis Effects 0.000 description 1
- 208000010668 atopic eczema Diseases 0.000 description 1
- IQFYYKKMVGJFEH-UHFFFAOYSA-N beta-L-thymidine Natural products O=C1NC(=O)C(C)=CN1C1OC(CO)C(O)C1 IQFYYKKMVGJFEH-UHFFFAOYSA-N 0.000 description 1
- OQFSQFPPLPISGP-UHFFFAOYSA-N beta-carboxyaspartic acid Natural products OC(=O)C(N)C(C(O)=O)C(O)=O OQFSQFPPLPISGP-UHFFFAOYSA-N 0.000 description 1
- AFYNADDZULBEJA-UHFFFAOYSA-N bicinchoninic acid Chemical compound C1=CC=CC2=NC(C=3C=C(C4=CC=CC=C4N=3)C(=O)O)=CC(C(O)=O)=C21 AFYNADDZULBEJA-UHFFFAOYSA-N 0.000 description 1
- 230000004071 biological effect Effects 0.000 description 1
- 229960000074 biopharmaceutical Drugs 0.000 description 1
- 230000000903 blocking effect Effects 0.000 description 1
- 210000004155 blood-retinal barrier Anatomy 0.000 description 1
- 230000004378 blood-retinal barrier Effects 0.000 description 1
- 210000004781 brain capillary Anatomy 0.000 description 1
- 210000004958 brain cell Anatomy 0.000 description 1
- 210000000133 brain stem Anatomy 0.000 description 1
- 244000309464 bull Species 0.000 description 1
- 239000001110 calcium chloride Substances 0.000 description 1
- 235000011148 calcium chloride Nutrition 0.000 description 1
- 229910001628 calcium chloride Inorganic materials 0.000 description 1
- 239000001506 calcium phosphate Substances 0.000 description 1
- 230000004858 capillary barrier Effects 0.000 description 1
- 239000004202 carbamide Substances 0.000 description 1
- 229910052799 carbon Inorganic materials 0.000 description 1
- 230000010261 cell growth Effects 0.000 description 1
- 230000007541 cellular toxicity Effects 0.000 description 1
- 239000001913 cellulose Substances 0.000 description 1
- 229920002678 cellulose Polymers 0.000 description 1
- 238000005119 centrifugation Methods 0.000 description 1
- 238000012512 characterization method Methods 0.000 description 1
- 238000012412 chemical coupling Methods 0.000 description 1
- 239000007958 cherry flavor Substances 0.000 description 1
- 229960004926 chlorobutanol Drugs 0.000 description 1
- 230000019771 cognition Effects 0.000 description 1
- 230000001010 compromised effect Effects 0.000 description 1
- 238000004590 computer program Methods 0.000 description 1
- 230000001143 conditioned effect Effects 0.000 description 1
- 238000007796 conventional method Methods 0.000 description 1
- 238000009295 crossflow filtration Methods 0.000 description 1
- 239000013078 crystal Substances 0.000 description 1
- 150000001945 cysteines Chemical class 0.000 description 1
- 230000034994 death Effects 0.000 description 1
- 230000002950 deficient Effects 0.000 description 1
- 230000001934 delay Effects 0.000 description 1
- 239000005549 deoxyribonucleoside Substances 0.000 description 1
- 239000005547 deoxyribonucleotide Substances 0.000 description 1
- 125000002637 deoxyribonucleotide group Chemical group 0.000 description 1
- 230000001419 dependent effect Effects 0.000 description 1
- 230000006866 deterioration Effects 0.000 description 1
- 238000011161 development Methods 0.000 description 1
- 238000003745 diagnosis Methods 0.000 description 1
- NEFBYIFKOOEVPA-UHFFFAOYSA-K dicalcium phosphate Chemical compound [Ca+2].[Ca+2].[O-]P([O-])([O-])=O NEFBYIFKOOEVPA-UHFFFAOYSA-K 0.000 description 1
- 229940038472 dicalcium phosphate Drugs 0.000 description 1
- 229910000390 dicalcium phosphate Inorganic materials 0.000 description 1
- 235000005911 diet Nutrition 0.000 description 1
- 230000037213 diet Effects 0.000 description 1
- UGMCXQCYOVCMTB-UHFFFAOYSA-K dihydroxy(stearato)aluminium Chemical compound CCCCCCCCCCCCCCCCCC(=O)O[Al](O)O UGMCXQCYOVCMTB-UHFFFAOYSA-K 0.000 description 1
- 238000010790 dilution Methods 0.000 description 1
- 239000012895 dilution Substances 0.000 description 1
- 150000002016 disaccharides Chemical group 0.000 description 1
- 239000006185 dispersion Substances 0.000 description 1
- 238000010494 dissociation reaction Methods 0.000 description 1
- 230000005593 dissociations Effects 0.000 description 1
- 239000002552 dosage form Substances 0.000 description 1
- 238000009510 drug design Methods 0.000 description 1
- 230000005584 early death Effects 0.000 description 1
- 239000012636 effector Substances 0.000 description 1
- 229940012882 elaprase Drugs 0.000 description 1
- 210000001671 embryonic stem cell Anatomy 0.000 description 1
- 239000006274 endogenous ligand Substances 0.000 description 1
- 230000003511 endothelial effect Effects 0.000 description 1
- 239000002702 enteric coating Substances 0.000 description 1
- 238000009505 enteric coating Methods 0.000 description 1
- 238000001952 enzyme assay Methods 0.000 description 1
- BEFDCLMNVWHSGT-UHFFFAOYSA-N ethenylcyclopentane Chemical compound C=CC1CCCC1 BEFDCLMNVWHSGT-UHFFFAOYSA-N 0.000 description 1
- ZMMJGEGLRURXTF-UHFFFAOYSA-N ethidium bromide Chemical compound [Br-].C12=CC(N)=CC=C2C2=CC=C(N)C=C2[N+](CC)=C1C1=CC=CC=C1 ZMMJGEGLRURXTF-UHFFFAOYSA-N 0.000 description 1
- 229960005542 ethidium bromide Drugs 0.000 description 1
- 230000001747 exhibiting effect Effects 0.000 description 1
- 239000000796 flavoring agent Substances 0.000 description 1
- 235000013305 food Nutrition 0.000 description 1
- 235000013355 food flavoring agent Nutrition 0.000 description 1
- 238000004108 freeze drying Methods 0.000 description 1
- 238000010230 functional analysis Methods 0.000 description 1
- 239000007903 gelatin capsule Substances 0.000 description 1
- 229930195712 glutamate Natural products 0.000 description 1
- 235000013922 glutamic acid Nutrition 0.000 description 1
- 239000004220 glutamic acid Substances 0.000 description 1
- 239000001963 growth medium Substances 0.000 description 1
- 230000010370 hearing loss Effects 0.000 description 1
- 231100000888 hearing loss Toxicity 0.000 description 1
- 208000016354 hearing loss disease Diseases 0.000 description 1
- 208000016861 hereditary angioedema type 3 Diseases 0.000 description 1
- 238000013537 high throughput screening Methods 0.000 description 1
- 235000001050 hortel pimenta Nutrition 0.000 description 1
- 210000004408 hybridoma Anatomy 0.000 description 1
- 239000001257 hydrogen Substances 0.000 description 1
- 150000002431 hydrogen Chemical group 0.000 description 1
- 229910052739 hydrogen Inorganic materials 0.000 description 1
- 230000002163 immunogen Effects 0.000 description 1
- 230000006872 improvement Effects 0.000 description 1
- 239000003701 inert diluent Substances 0.000 description 1
- 230000036512 infertility Effects 0.000 description 1
- 238000001802 infusion Methods 0.000 description 1
- 208000015978 inherited metabolic disease Diseases 0.000 description 1
- 230000000977 initiatory effect Effects 0.000 description 1
- 238000007689 inspection Methods 0.000 description 1
- PBGKTOXHQIOBKM-FHFVDXKLSA-N insulin (human) Chemical compound C([C@@H](C(=O)N[C@@H](CC(C)C)C(=O)N[C@H]1CSSC[C@H]2C(=O)N[C@H](C(=O)N[C@@H](CO)C(=O)N[C@H](C(=O)N[C@H](C(N[C@@H](CO)C(=O)N[C@@H](CC(C)C)C(=O)N[C@@H](CC=3C=CC(O)=CC=3)C(=O)N[C@@H](CCC(N)=O)C(=O)N[C@@H](CC(C)C)C(=O)N[C@@H](CCC(O)=O)C(=O)N[C@@H](CC(N)=O)C(=O)N[C@@H](CC=3C=CC(O)=CC=3)C(=O)N[C@@H](CSSC[C@H](NC(=O)[C@H](C(C)C)NC(=O)[C@H](CC(C)C)NC(=O)[C@H](CC=3C=CC(O)=CC=3)NC(=O)[C@H](CC(C)C)NC(=O)[C@H](C)NC(=O)[C@H](CCC(O)=O)NC(=O)[C@H](C(C)C)NC(=O)[C@H](CC(C)C)NC(=O)[C@H](CC=3NC=NC=3)NC(=O)[C@H](CO)NC(=O)CNC1=O)C(=O)NCC(=O)N[C@@H](CCC(O)=O)C(=O)N[C@@H](CCCNC(N)=N)C(=O)NCC(=O)N[C@@H](CC=1C=CC=CC=1)C(=O)N[C@@H](CC=1C=CC=CC=1)C(=O)N[C@@H](CC=1C=CC(O)=CC=1)C(=O)N[C@@H]([C@@H](C)O)C(=O)N1[C@@H](CCC1)C(=O)N[C@@H](CCCCN)C(=O)N[C@@H]([C@@H](C)O)C(O)=O)C(=O)N[C@@H](CC(N)=O)C(O)=O)=O)CSSC[C@@H](C(N2)=O)NC(=O)[C@H](CCC(N)=O)NC(=O)[C@H](CCC(O)=O)NC(=O)[C@H](C(C)C)NC(=O)[C@@H](NC(=O)CN)[C@@H](C)CC)[C@@H](C)CC)[C@@H](C)O)NC(=O)[C@H](CCC(N)=O)NC(=O)[C@H](CC(N)=O)NC(=O)[C@@H](NC(=O)[C@@H](N)CC=1C=CC=CC=1)C(C)C)C1=CN=CN1 PBGKTOXHQIOBKM-FHFVDXKLSA-N 0.000 description 1
- 230000003993 interaction Effects 0.000 description 1
- 238000010255 intramuscular injection Methods 0.000 description 1
- 239000007927 intramuscular injection Substances 0.000 description 1
- 239000007928 intraperitoneal injection Substances 0.000 description 1
- 238000002955 isolation Methods 0.000 description 1
- AEMOLEFTQBMNLQ-CLQWQSTFSA-N l-iduronic acid Chemical compound O[C@H]1O[C@H](C(O)=O)[C@H](O)[C@@H](O)[C@@H]1O AEMOLEFTQBMNLQ-CLQWQSTFSA-N 0.000 description 1
- 102000005861 leptin receptors Human genes 0.000 description 1
- 108010019813 leptin receptors Proteins 0.000 description 1
- XMGQYMWWDOXHJM-UHFFFAOYSA-N limonene Chemical compound CC(=C)C1CCC(C)=CC1 XMGQYMWWDOXHJM-UHFFFAOYSA-N 0.000 description 1
- 239000006193 liquid solution Substances 0.000 description 1
- 239000006194 liquid suspension Substances 0.000 description 1
- 239000000314 lubricant Substances 0.000 description 1
- 239000006166 lysate Substances 0.000 description 1
- 239000012139 lysis buffer Substances 0.000 description 1
- 238000002824 mRNA display Methods 0.000 description 1
- ZLNQQNXFFQJAID-UHFFFAOYSA-L magnesium carbonate Chemical compound [Mg+2].[O-]C([O-])=O ZLNQQNXFFQJAID-UHFFFAOYSA-L 0.000 description 1
- 239000001095 magnesium carbonate Substances 0.000 description 1
- 229910000021 magnesium carbonate Inorganic materials 0.000 description 1
- 239000003550 marker Substances 0.000 description 1
- 230000008384 membrane barrier Effects 0.000 description 1
- 230000015654 memory Effects 0.000 description 1
- OSWPMRLSEDHDFF-UHFFFAOYSA-N methyl salicylate Chemical compound COC(=O)C1=CC=CC=C1O OSWPMRLSEDHDFF-UHFFFAOYSA-N 0.000 description 1
- 125000000325 methylidene group Chemical group [H]C([H])=* 0.000 description 1
- LSDPWZHWYPCBBB-UHFFFAOYSA-O methylsulfide anion Chemical compound [SH2+]C LSDPWZHWYPCBBB-UHFFFAOYSA-O 0.000 description 1
- 238000013508 migration Methods 0.000 description 1
- 230000005012 migration Effects 0.000 description 1
- 230000003278 mimic effect Effects 0.000 description 1
- 108091005601 modified peptides Proteins 0.000 description 1
- 239000000178 monomer Substances 0.000 description 1
- 230000036651 mood Effects 0.000 description 1
- 238000010172 mouse model Methods 0.000 description 1
- 229940126619 mouse monoclonal antibody Drugs 0.000 description 1
- 208000012253 mucopolysaccharidosis IVA Diseases 0.000 description 1
- 238000002703 mutagenesis Methods 0.000 description 1
- 231100000350 mutagenesis Toxicity 0.000 description 1
- 201000000050 myeloid neoplasm Diseases 0.000 description 1
- 229940037525 nasal preparations Drugs 0.000 description 1
- 229960004927 neomycin Drugs 0.000 description 1
- 230000000926 neurological effect Effects 0.000 description 1
- 238000010606 normalization Methods 0.000 description 1
- 235000003715 nutritional status Nutrition 0.000 description 1
- 239000007968 orange flavor Substances 0.000 description 1
- 230000008816 organ damage Effects 0.000 description 1
- 230000008520 organization Effects 0.000 description 1
- 230000007170 pathology Effects 0.000 description 1
- 230000035515 penetration Effects 0.000 description 1
- 229940049954 penicillin Drugs 0.000 description 1
- 239000000816 peptidomimetic Substances 0.000 description 1
- 230000003836 peripheral circulation Effects 0.000 description 1
- 230000002085 persistent effect Effects 0.000 description 1
- 239000008196 pharmacological composition Substances 0.000 description 1
- 229960003742 phenol Drugs 0.000 description 1
- PTMHPRAIXMAOOB-UHFFFAOYSA-N phosphoramidic acid Chemical class NP(O)(O)=O PTMHPRAIXMAOOB-UHFFFAOYSA-N 0.000 description 1
- 230000001766 physiological effect Effects 0.000 description 1
- 229920001515 polyalkylene glycol Polymers 0.000 description 1
- 229920001282 polysaccharide Polymers 0.000 description 1
- 239000005017 polysaccharide Substances 0.000 description 1
- 150000004804 polysaccharides Chemical class 0.000 description 1
- 229920001592 potato starch Polymers 0.000 description 1
- 229940116317 potato starch Drugs 0.000 description 1
- 230000002335 preservative effect Effects 0.000 description 1
- 230000037452 priming Effects 0.000 description 1
- 230000002035 prolonged effect Effects 0.000 description 1
- 235000010232 propyl p-hydroxybenzoate Nutrition 0.000 description 1
- 230000004952 protein activity Effects 0.000 description 1
- 108020001580 protein domains Proteins 0.000 description 1
- 230000020978 protein processing Effects 0.000 description 1
- 239000002510 pyrogen Substances 0.000 description 1
- 238000010188 recombinant method Methods 0.000 description 1
- 210000000664 rectum Anatomy 0.000 description 1
- 230000000241 respiratory effect Effects 0.000 description 1
- 230000004044 response Effects 0.000 description 1
- 230000000979 retarding effect Effects 0.000 description 1
- 210000001525 retina Anatomy 0.000 description 1
- 238000003757 reverse transcription PCR Methods 0.000 description 1
- 239000002342 ribonucleoside Substances 0.000 description 1
- 239000002336 ribonucleotide Substances 0.000 description 1
- 125000002652 ribonucleotide group Chemical group 0.000 description 1
- 229940081974 saccharin Drugs 0.000 description 1
- 235000019204 saccharin Nutrition 0.000 description 1
- 239000000901 saccharin and its Na,K and Ca salt Substances 0.000 description 1
- 238000012216 screening Methods 0.000 description 1
- 238000010845 search algorithm Methods 0.000 description 1
- 230000003248 secreting effect Effects 0.000 description 1
- ZKZBPNGNEQAJSX-UHFFFAOYSA-N selenocysteine Natural products [SeH]CC(N)C(O)=O ZKZBPNGNEQAJSX-UHFFFAOYSA-N 0.000 description 1
- 235000016491 selenocysteine Nutrition 0.000 description 1
- 229940055619 selenocysteine Drugs 0.000 description 1
- 238000000926 separation method Methods 0.000 description 1
- 238000012163 sequencing technique Methods 0.000 description 1
- 239000012679 serum free medium Substances 0.000 description 1
- 239000004208 shellac Substances 0.000 description 1
- ZLGIYFNHBLSMPS-ATJNOEHPSA-N shellac Chemical compound OCCCCCC(O)C(O)CCCCCCCC(O)=O.C1C23[C@H](C(O)=O)CCC2[C@](C)(CO)[C@@H]1C(C(O)=O)=C[C@@H]3O ZLGIYFNHBLSMPS-ATJNOEHPSA-N 0.000 description 1
- 229940113147 shellac Drugs 0.000 description 1
- 235000013874 shellac Nutrition 0.000 description 1
- 239000002356 single layer Substances 0.000 description 1
- 238000003998 size exclusion chromatography high performance liquid chromatography Methods 0.000 description 1
- 235000017557 sodium bicarbonate Nutrition 0.000 description 1
- 229910000030 sodium bicarbonate Inorganic materials 0.000 description 1
- 229910000029 sodium carbonate Inorganic materials 0.000 description 1
- HLBBKKJFGFRGMU-UHFFFAOYSA-M sodium formate Chemical compound [Na+].[O-]C=O HLBBKKJFGFRGMU-UHFFFAOYSA-M 0.000 description 1
- 235000019254 sodium formate Nutrition 0.000 description 1
- 239000007787 solid Substances 0.000 description 1
- 239000007909 solid dosage form Substances 0.000 description 1
- 235000010199 sorbic acid Nutrition 0.000 description 1
- 239000004334 sorbic acid Substances 0.000 description 1
- 229940075582 sorbic acid Drugs 0.000 description 1
- 241000894007 species Species 0.000 description 1
- 239000003381 stabilizer Substances 0.000 description 1
- 230000005477 standard model Effects 0.000 description 1
- 238000010561 standard procedure Methods 0.000 description 1
- 239000008107 starch Substances 0.000 description 1
- 235000019698 starch Nutrition 0.000 description 1
- 230000001954 sterilising effect Effects 0.000 description 1
- 238000004659 sterilization and disinfection Methods 0.000 description 1
- 210000002784 stomach Anatomy 0.000 description 1
- 238000003860 storage Methods 0.000 description 1
- 229960005322 streptomycin Drugs 0.000 description 1
- 238000012916 structural analysis Methods 0.000 description 1
- 150000008163 sugars Chemical class 0.000 description 1
- 239000006228 supernatant Substances 0.000 description 1
- 239000013589 supplement Substances 0.000 description 1
- 238000013268 sustained release Methods 0.000 description 1
- 239000012730 sustained-release form Substances 0.000 description 1
- 238000012360 testing method Methods 0.000 description 1
- RTKIYNMVFMVABJ-UHFFFAOYSA-L thimerosal Chemical compound [Na+].CC[Hg]SC1=CC=CC=C1C([O-])=O RTKIYNMVFMVABJ-UHFFFAOYSA-L 0.000 description 1
- 229940033663 thimerosal Drugs 0.000 description 1
- 125000003396 thiol group Chemical group [H]S* 0.000 description 1
- 229940104230 thymidine Drugs 0.000 description 1
- 210000001578 tight junction Anatomy 0.000 description 1
- 210000001519 tissue Anatomy 0.000 description 1
- 230000005030 transcription termination Effects 0.000 description 1
- 238000010361 transduction Methods 0.000 description 1
- 230000026683 transduction Effects 0.000 description 1
- 238000013519 translation Methods 0.000 description 1
- 150000003626 triacylglycerols Chemical class 0.000 description 1
- 238000011144 upstream manufacturing Methods 0.000 description 1
- 210000003708 urethra Anatomy 0.000 description 1
- 238000001291 vacuum drying Methods 0.000 description 1
- 235000012431 wafers Nutrition 0.000 description 1
- 210000004885 white matter Anatomy 0.000 description 1
- 239000009637 wintergreen oil Substances 0.000 description 1
- DGVVWUTYPXICAM-UHFFFAOYSA-N β‐Mercaptoethanol Chemical compound OCCS DGVVWUTYPXICAM-UHFFFAOYSA-N 0.000 description 1
Images
Classifications
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K16/00—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies
- C07K16/18—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P25/00—Drugs for disorders of the nervous system
- A61P25/28—Drugs for disorders of the nervous system for treating neurodegenerative disorders of the central nervous system, e.g. nootropic agents, cognition enhancers, drugs for treating Alzheimer's disease or other forms of dementia
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K16/00—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies
- C07K16/18—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans
- C07K16/28—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans against receptors, cell surface antigens or cell surface determinants
- C07K16/2869—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans against receptors, cell surface antigens or cell surface determinants against hormone receptors
-
- C—CHEMISTRY; METALLURGY
- C12—BIOCHEMISTRY; BEER; SPIRITS; WINE; VINEGAR; MICROBIOLOGY; ENZYMOLOGY; MUTATION OR GENETIC ENGINEERING
- C12N—MICROORGANISMS OR ENZYMES; COMPOSITIONS THEREOF; PROPAGATING, PRESERVING, OR MAINTAINING MICROORGANISMS; MUTATION OR GENETIC ENGINEERING; CULTURE MEDIA
- C12N9/00—Enzymes; Proenzymes; Compositions thereof; Processes for preparing, activating, inhibiting, separating or purifying enzymes
- C12N9/14—Hydrolases (3)
- C12N9/16—Hydrolases (3) acting on ester bonds (3.1)
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K2039/505—Medicinal preparations containing antigens or antibodies comprising antibodies
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K2317/00—Immunoglobulins specific features
- C07K2317/50—Immunoglobulins specific features characterized by immunoglobulin fragments
- C07K2317/56—Immunoglobulins specific features characterized by immunoglobulin fragments variable (Fv) region, i.e. VH and/or VL
- C07K2317/565—Complementarity determining region [CDR]
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K2317/00—Immunoglobulins specific features
- C07K2317/90—Immunoglobulins specific features characterized by (pharmaco)kinetic aspects or by stability of the immunoglobulin
- C07K2317/92—Affinity (KD), association rate (Ka), dissociation rate (Kd) or EC50 value
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K2319/00—Fusion polypeptide
- C07K2319/30—Non-immunoglobulin-derived peptide or protein having an immunoglobulin constant or Fc region, or a fragment thereof, attached thereto
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K2319/00—Fusion polypeptide
- C07K2319/33—Fusion polypeptide fusions for targeting to specific cell types, e.g. tissue specific targeting, targeting of a bacterial subspecies
-
- C—CHEMISTRY; METALLURGY
- C12—BIOCHEMISTRY; BEER; SPIRITS; WINE; VINEGAR; MICROBIOLOGY; ENZYMOLOGY; MUTATION OR GENETIC ENGINEERING
- C12Y—ENZYMES
- C12Y301/00—Hydrolases acting on ester bonds (3.1)
- C12Y301/06—Sulfuric ester hydrolases (3.1.6)
- C12Y301/06013—Iduronate-2-sulfatase (3.1.6.13)
Definitions
- Type II mucopolysaccharidosis also known as Hunter's syndrome, is an inherited metabolic disease caused by a defect in the enzyme iduronate 2-sulfatase (IDS), which functions to degrade mucopolysaccharides.
- IDS iduronate 2-sulfatase
- An insufficient level of IDS causes a pathological buildup of heparan sulfate and dermatan sulfate in, e.g., the heart, liver, and central nervous system (CNS). Symptoms including neurodegeneration and mental retardation appear during childhood; and early death can occur due to organ damage in the brain.
- treatment includes intravenous enzyme replacement therapy with recombinant IDS.
- systemically administered recombinant IDS does not cross the blood brain barrier (BBB), and therefore has little impact on the effects of the disease in the CNS.
- BBB blood brain barrier
- US 2005/142141 A1 relates to methods of delivery of enzymes to the bran via transport across the BBB utilizing conjugates, of fusion proteins, which are composed of a therapeutic enzyme and a BBB targeting agent such as a monoclonal antibody.
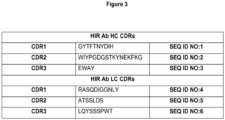
- US 2005/142141 A1 discloses the murine anti-insulin receptor antibody HIRMab clone 81-14. which was humanized.
- US 2005/142141 A1 discloses a humanized HIRMab a-iduronidase (IDUA)fusion protein, wherem IDUA was covalently linked to the carboxyterminus of the heavy chain of the antibody.
- IDUA humanized HIRMab a-iduronidase
- a genetically engineered antibody that targets the human insulin receptor (HIRMab) allows for drug delivery across the human BBB.
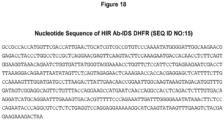
- compositions provided herein comprise fusion antibodies comprising an IDS polypeptide fused to structure (e.g., antibody, immunoglobulin) capable of crossing the blood-brain barrier (BBB).
- the HIR Ab-IDS fusion antibody binds to the extracellular domain of the insulin receptor and is transported across the blood brain barrier (“BBB”) into the CNS, while retaining iduronate 2-sulfatase activity.
- the HIR Ab binds to the endogenous insulin receptor on the BBB, and acts as a molecular Trojan horse to ferry the IDS into the brain.
- a therapeutically effective systemic dose of a HIR Ab-IDS fusion antibody for systemic administration is based, in part, on the specific CNS uptake characteristics of the fusion antibody from peripheral blood as described herein.
- compositions containing an IDS covalently linked to a structure that is capable of crossing the blood brain barrier (BBB), where the structure and the IDS each retains at least about 10, 20, 30, 40, 50, 60, 70, 80, 90, 95, 99, or 100% of its activity, compared to its activity as a separate entity.
- the IDS may retain at least about 10% of its activity compared to its activity as a separate entity.
- the IDS may retain at least 20% of its activity, compared to its activity as a separate entity.
- the IDS may retain at least 30% of its activity, compared to its activity as a separate entity.
- the IDS may retain at least 40% of its activity, compared to its activity as a separate entity.
- the IDS may retain at least 50% of its activity, compared to its activity as a separate entity.
- the IDS may retain at least 60% of its activity, compared to its activity as a separate entity.
- a fusion antibody comprising IDS is post-translationally modified by a sulfatase modifying factor type 1 (SUMF1).
- the post-translational modification comprises a cysteine to formylglycine conversion.
- the fusion antibody comprises a formylglycine residue.
- compositions for use in a method for treating an IDS deficiency in the central nervous system of a subject in need thereof comprising systemically administering to the subject a therapeutically effective dose of a fusion antibody having IDS activity.
- the fusion antibody comprises the amino acid sequence of an immunoglobulin heavy chain, the amino acid sequence of an IDS, and the amino acid sequence of an immunoglobulin light chain; (ii) the fusion antibody binds to an extracellular domain of the human insulin receptor and catalyzes hydrolysis of the 2-sulfate groups of the L-iduronate 2-sulfate units of dermatan sulfate, heparan sulfate or heparin; and (iii) the amino acid sequence of the IDS is covalently linked to the carboxy terminus of the amino acid sequence of the immunoglobulin heavy chain.
- the immunoglobulin heavy chain is an immunoglobulin heavy chain of IgG. In some embodiments, the immunoglobulin heavy chain is an immunoglobulin heavy chain of kappa class.
- the therapeutically effective dose of the fusion antibody comprises at least about 2.5 ⁇ 10 6 units of IDS activity or at least about 50,000 units/Kg of body weight.
- the IDS specific activity of the fusion antibody is at least 30,000 units/mg.
- systemic administration is parenteral, intravenous, subcutaneous, intra-muscular, trans-nasal, intra-arterial, transdermal, or respiratory.
- At least about 25,000, 30,000, 35,000, 40,000, 45,000, 50,000, 60,000, 70,000, 80,000, 90,000, 110,000, 120,000, 130,000, 140,000, 150,000, 160,000, 170,000, 180,000, 190,000, 200,000, 210,000, 220,000, 230,000, 250,000 units of iduronate-2-sulfatase activity is delivered to the brain, normalized per 50 kg body weight. In some embodiments, at least about 25,000 units of iduronate-2-sulfatase activity is delivered to the brain, normalized per 50 kg body weight.
- the fusion antibody is a chimeric antibody.
- the immunoglobulin heavy chain of the fusion antibody comprises a CDR1 corresponding to the amino acid sequence of SEQ ID NO:1, a CDR2 corresponding to the amino acid sequence of SEQ ID NO:2, and a CDR3 corresponding to the amino acid sequence of SEQ ID NO:3; and the immunoglobulin light chain comprises a CDR1 corresponding to the amino acid sequence of SEQ ID NO:4, a CDR2 corresponding to the amino acid sequence of SEQ ID NO:5, and a CDR3 corresponding to the amino acid sequence of SEQ ID NO:6.
- the immunoglobulin heavy chain of the fusion antibody is at least 90% identical to SEQ ID NO:7 and the amino acid sequence of the light chain immunoglobulin is at least 90% identical to SEQ ID NO:8.
- the immunoglobulin heavy chain of the fusion antibody comprises SEQ ID NO:7 and the amino acid sequence of the light chain immunoglobulin comprises SEQ ID NO:8
- the IDS comprises an amino acid sequence at least 90% (e.g., 95%, or 100%) identical to SEQ ID NO:9.
- the amino acid sequence of the immunoglobulin heavy chain of the fusion antibody at least 90% identical to SEQ ID NO:7; the amino acid sequence of the light chain immunoglobulin is at least 90% identical to SEQ ID NO:8; and the amino acid sequence of the IDS is at least 95% identical to SEQ ID NO:9 or comprises SEQ ID NO:9.
- the amino acid sequence of the immunoglobulin heavy chain of the fusion antibody comprises SEQ ID NO:8
- the amino acid sequence of the immunoglobulin light chain comprises SEQ ID NO:8
- the amino acid sequence of the IDS comprises SEQ ID NO:9.
- compositions comprising a therapeutically effective amount of a fusion antibody and a pharmaceutically acceptable excipient.
- isolated polynucleotides encoding a fusion antibody.
- the isolated polynucleotide comprises the nucleic acid sequence of SEQ ID NO:14.
- vectors comprising the isolated polynucleotides encoding a fusion antibody.
- the vectors comprise the nucleic acid sequence of SEQ ID NO:14.
- host cells comprising the vectors comprising the isolated polynucleotides encoding a fusion antibody.
- the host cell is a Chinese Hamster Ovary (CHO).
- a method for treating an IDS deficiency in the central nervous system of a subject in need thereof comprising systemically administering to the subject a therapeutically effective dose of a fusion antibody having IDS activity, wherein: (i) the fusion antibody comprises: (a) a fusion protein at least 95% identical to SEQ ID NO:10, and (b) an immunoglobulin light chain; and (ii) the fusion antibody binds to an extracellular domain of the human insulin receptor and catalyzes hydrolysis of linkages in dermatan or heparan sulfate.
- a method for treating an IDS deficiency in the central nervous system of a subject in need thereof comprising systemically administering to the subject a therapeutically effective dose of a fusion antibody having IDS activity, wherein: (i) the fusion antibody comprises a fusion protein containing the amino acid sequence of an immunoglobulin heavy chain and an IDS or comprises a fusion protein containing the amino acid sequence of an immunoglobulin light chain and an IDS; the fusion antibody binds to the extracellular domain of the human insulin receptor; and the fusion antibody catalyzes hydrolysis of linkages in dermatan or heparan sulfate; and (ii) the amino acid sequence of the IDS is covalently linked to the carboxy terminus of the amino acid sequence of the immunoglobulin heavy chain or the immunoglobulin light chain.
- the blood brain barrier is a severe impediment to the delivery of systemically administered IDS (e.g., recombinant IDS) to the central nervous system.
- IDS systemically administered IDS
- the present disclosure provides methods and compositions for delivering therapeutically significant levels of IDS activity across the BBB to the CNS.
- the IDS is modified to allow it to cross the BBB.
- the amount and rate of uptake of systemically administered modified IDS into the CNS is provided.
- the IDS retains a certain activity after being modified or after crossing the BBB.
- the present disclosure provides, inter alia : (1) IDS fusion antibodies comprising an IDS fused, with or without intervening sequence, to an immunoglobulin (heavy chain or light chain) capable of crossing the BBB, and related methods and compositions. (2) human insulin receptor (HIR) antibody (Ab)-IDS fusion antibodies comprising an IDS fused, with or without intervening sequence, to an immunoglobulin (heavy chain or light chain) directed against the extracellular domain of a human insulin receptor, and related methods and compositiosn; (3) methods of treating an IDS deficiency; and (4) methods of establishing therapeutically effective systemic doses of the fusion antibodies based on a characterization of their uptake in the CNS and their specific activity.
- the invention provides compositions and methods for treating a nIDS deficiency in the central nervous system by systemically administering to a subject in need thereof a therapeutically effective dose of a bifunctional IDS fusion antibody (e.g., HIR Ab-IDS) having IDS activity and selectively binding to the receptor-mediated BBB transport system (e.g., the extracellular domain of a human insulin receptor).
- a bifunctional IDS fusion antibody e.g., HIR Ab-IDS
- BBB transport system e.g., the extracellular domain of a human insulin receptor
- Treatment includes achieving a therapeutic benefit and/or a prophylactic benefit.
- therapeutic benefit is meant eradication or amelioration of the underlying disorder or condition being treated.
- therapeutic benefit includes partial or complete halting of the progression of the disorder, or partial or complete reversal of the disorder.
- a therapeutic benefit is achieved with the eradication or amelioration of one or more of the physiological or psychological symptoms associated with the underlying condition such that an improvement is observed in the patient, notwithstanding the fact that the patient may still be affected by the condition.
- a prophylactic benefit of treatment includes prevention of a condition, retarding the progress of a condition (e.g., slowing the progression of a lysosomal storage disorder), or decreasing the likelihood of occurrence of a condition.
- “treating” or “treatment” includes prophylaxis.
- an effective amount can be an amount, which when administered systemically, is sufficient to effect beneficial or desired results in the CNS, such as beneficial or desired clinical results, or enhanced cognition, memory, mood, or other desired CNS results.
- An effective amount is also an amount that produces a prophylactic effect, e.g., an amount that delays, reduces, or eliminates the appearance of a pathological or undesired condition. Such conditions include, but are not limited to, mental retardation, hearing loss, and neurodegeneration.
- An effective amount can be administered in one or more administrations.
- an “effective amount” of a composition of the invention is an amount that is sufficient to palliate, ameliorate, stabilize, reverse or slow the progression of a disorder, e.g., a neurological disorder.
- An “effective amount” may be of any of the compositions of the invention used alone or in conjunction with one or more agents used to treat a disease or disorder.
- An “effective amount” of a therapeutic agent within the meaning of the present invention is determined by a patient's attending physician or veterinarian. Such amounts are readily ascertained by one of ordinary skill in the art and will a therapeutic effect when administered in accordance with the present invention.
- Factors which influence what a therapeutically effective amount will be include, the IDS specific activity of the IDS fusion antibody (e.g., HIR Ab-IDS ) administered, its absorption profile (e.g., its rate of uptake into the brain), time elapsed since the initiation of the disorder, and the age, physical condition, existence of other disease states, and nutritional status of the individual being treated. Additionally, other medication the patient may be receiving will affect the determination of the therapeutically effective amount of the therapeutic agent to administer.
- the IDS specific activity of the IDS fusion antibody e.g., HIR Ab-IDS
- its absorption profile e.g., its rate of uptake into the brain
- time elapsed since the initiation of the disorder e.g., its rate of uptake into the brain
- time elapsed since the initiation of the disorder e.g., its rate of uptake into the brain
- time elapsed since the initiation of the disorder e.g., its rate of uptake into the brain
- a “subject” or an “individual,” as used herein, is an animal, for example, a mammal. In some embodiments a “subject” or an “individual” is a human. In some embodiments, the subject suffers from Mucopolysaccharidosis Type II ("Hunter's Syndrome").
- a pharmacological composition comprising an IDS fusion antibody (e.g., HIR Ab-IDS ) fusion antibody is "administered peripherally" or “peripherally administered.”
- IDS fusion antibody e.g., HIR Ab-IDS
- these terms refer to any form of administration of an agent, e.g., a therapeutic agent, to an individual that is not direct administration to the CNS, i.e., that brings the agent in contact with the non-brain side of the blood-brain barrier.
- Peripheral administration includes intravenous, intra-arterial, subcutaneous, intramuscular, intraperitoneal, transdermal, by inhalation, transbuccal, intranasal, rectal, oral, parenteral, sublingual, or trans-nasal.
- a “pharmaceutically acceptable carrier” or “pharmaceutically acceptable excipient” herein refers to any carrier that does not itself induce the production of antibodies harmful to the individual receiving the composition. Such carriers are well known to those of ordinary skill in the art. A thorough discussion of pharmaceutically acceptable carriers/excipients can be found in Remington's Pharmaceutical Sciences, Gennaro, AR, ed., 20th edition, 2000: Williams and Wilkins PA, USA ..
- Exemplary pharmaceutically acceptable carriers can include salts, for example, mineral acid salts such as hydrochlorides, hydrobromides, phosphates, sulfates, and the like; and the salts of organic acids such as acetates, propionates, malonates, benzoates, and the like.
- compositions of the invention may be provided in liquid form, and formulated in saline based aqueous solution of varying pH (5-8), with or without detergents such polysorbate-80 at 0.01-1%, or carbohydrate additives, such mannitol, sorbitol, or trehalose.
- detergents such as polysorbate-80 at 0.01-1%
- carbohydrate additives such mannitol, sorbitol, or trehalose.
- Commonly used buffers include histidine, acetate, phosphate, or citrate.
- a “recombinant host cell” or “host cell” refers to a cell that includes an exogenous polynucleotide, regardless of the method used for insertion, for example, direct uptake, transduction, f-mating, or other methods known in the art to create recombinant host cells.
- the exogenous polynucleotide may be maintained as a nonintegrated vector, for example, a plasmid, or alternatively, may be integrated into the host genome.
- polypeptide peptide
- protein protein
- polypeptide polymer of amino acid residues. That is, a description directed to a polypeptide applies equally to a description of a peptide and a description of a protein, and vice versa.
- the terms apply to naturally occurring amino acid polymers as well as amino acid polymers in which one or more amino acid residues is a non-naturally occurring amino acid, e.g., an amino acid analog.
- the terms encompass amino acid chains of any length, including full length proteins (i.e., antigens), wherein the amino acid residues are linked by covalent peptide bonds.
- amino acid refers to naturally occurring and non-naturally occurring amino acids, as well as amino acid analogs and amino acid mimetics that function in a manner similar to the naturally occurring amino acids.
- Naturally encoded amino acids are the 20 common amino acids (alanine, arginine, asparagine, aspartic acid, cysteine, glutamine, glutamic acid, glycine, histidine, isoleucine, leucine, lysine, methionine, phenylalanine, proline, serine, threonine, tryptophan, tyrosine, and valine) and pyrolysine and selenocysteine.
- Amino acid analogs refers to compounds that have the same basic chemical structure as a naturally occurring amino acid, i.e., an ⁇ carbon that is bound to a hydrogen, a carboxyl group, an amino group, and an R group, such as, homoserine, norleucine, methionine sulfoxide, methionine methyl sulfonium.
- Such analogs have modified R groups (such as, norleucine) or modified peptide backbones, but retain the same basic chemical structure as a naturally occurring amino acid.
- Amino acids may be referred to herein by either their commonly known three letter symbols or by the oneletter symbols recommended by the IUPAC-IUB Biochemical Nomenclature Commission. Nucleotides, likewise, may be referred to by their commonly accepted single-letter codes.
- nucleic acid refers to deoxyribonucleotides, deoxyribonucleosides, ribonucleosides, or ribonucleotides and polymers thereof in either single- or double-stranded form. Unless specifically limited, the term encompasses nucleic acids containing known analogues of natural nucleotides which have similar binding properties as the reference nucleic acid and are metabolized in a manner similar to naturally occurring nucleotides. Unless specifically limited otherwise, the term also refers to oligonucleotide analogs including PNA (peptidonucleic acid), analogs of DNA used in antisense technology (phosphorothioates, phosphoroamidates, and the like).
- PNA peptidonucleic acid
- analogs of DNA used in antisense technology phosphorothioates, phosphoroamidates, and the like.
- nucleic acid sequence also implicitly encompasses conservatively modified variants thereof (including but not limited to, degenerate codon substitutions) and complementary sequences as well as the sequence explicitly indicated.
- degenerate codon substitutions may be achieved by generating sequences in which the third position of one or more selected (or all) codons is substituted with mixed-base and/or deoxyinosine residues ( Batzer et al., Nucleic Acid Res. 19:5081 (1991 ); Ohtsuka et al., J. Biol. Chem. 260:2605-2608 (1985 ); and Cassol et al. (1992); Rossolini et al., Mol. Cell. Probes 8:91-98 (1994 )).
- isolated and purified refer to a material that is substantially or essentially removed from or concentrated in its natural environment.
- an isolated nucleic acid may be one that is separated from the nucleic acids that normally flank it or other nucleic acids or components (proteins, lipids, etc%) in a sample.
- a polypeptide is purified if it is substantially removed from or concentrated in its natural environment. Methods for purification and isolation of nucleic acids and proteins are well known in the art.
- the invention provides compositions and methods that utilize an IDS fusion antibody (e.g., HIR Ab-IDS ) capable of crossing the blood brain barrier (BBB).
- IDS fusion antibody e.g., HIR Ab-IDS
- BBB blood brain barrier
- the compositions and methods are useful in transporting IDS from the peripheral blood and across the blood brain barrier into the CNS.
- the "blood-brain barrier” refers to the barrier between the peripheral circulation and the brain and spinal cord which is formed by tight junctions within the brain capillary endothelial plasma membranes and creates an extremely tight barrier that restricts the transport of molecules into the brain; the BBB is so tight that it is capable of restricting even molecules as small as urea, molecular weight of 60 Da.
- the blood-brain barrier within the brain, the bloodspinal cord barrier within the spinal cord, and the blood-retinal barrier within the retina, are contiguous capillary barriers within the central nervous system (CNS), and are collectively referred to as the blood-brain barrier or BBB.
- CNS central nervous system
- the BBB limits the development of new neurotherapeutics, diagnostics, and research tools for the brain and CNS.
- Most large molecule therapeutics such as recombinant proteins, antisense drugs, gene medicines, purified antibodies, or RNA interference (RNAi)-based drugs, do not cross the BBB in pharmacologically significant amounts.
- RNAi RNA interference
- small molecule drugs can cross the BBB, in fact, ⁇ 2% of all small molecule drugs are active in the brain owing to the lack transport across the BBB.
- a molecule must be lipid soluble and have a molecular weight less than 400 Daltons (Da) in order to cross the BBB in pharmacologically significant amounts, and the vast majority of small molecules do not have these dual molecular characteristics.
- ICV intracerebro-ventricular
- IC intracerebral
- CED convection enhanced diffusion
- the methods described herein offer an alternative to these highly invasive and generally unsatisfactory methods for bypassing the BBB, allowing a functional IDS to cross the BBB from the peripheral blood into the CNS following systemic administration of an the IDS fusion antibody (e.g., HIR Ab-IDS ) fusion antibody composition described herein.
- the methods described herein exploit the expression of insulin receptors (e.g., human insulin receptors) or other receptor on the BBB to shuttle a desired bifunctional IDS fusion antibody (e.g., HIR Ab-IDS ) from peripheral blood into the CNS.
- the BBB has been shown to have specific receptors that allow the transport from the blood to the brain of several macromolecules; these transporters are suitable as transporters for compositions of the invention.
- Endogenous BBB receptor-mediated transport systems useful in the invention include those that transport insulin, transferrin, insulin-like growth factors 1 and 2 (IGF1 and IGF2), leptin, and lipoproteins.
- the invention utilizes a structure (e.g., immunoglobulin, antibody) that is capable of crossing the BBB via the endogenous insulin BBB receptor-mediated transport system, e.g., the human endogenous insulin BBB receptor-mediated transport system.
- the structure e.g., immunoglobulin, antibody
- the BBB has been shown to have specific receptors, including insulin receptors, that allow the transport from the blood to the brain of several macromolecules.
- insulin receptors are suitable as transporters for the IDS fusion antibodies described herein (e.g., HIR Ab-IDS ).
- HIR-IDS fusion antibodies described herein bind to the extracellular domain (ECD) of the human insulin receptor.
- Insulin receptors and their extracellular, insulin binding domain have been extensively characterized in the art both structurally and functionally. See, e.g., Yip et al (2003), J Biol. Chem, 278(30):27329-27332 ; and Whittaker et al. (2005), J Biol Chem, 280(22):20932-20936 .
- the amino acid and nucleotide sequences of the human insulin receptor can be found under GenBank accession No. NM_000208.
- MTH molecular Trojan horses
- a MTH is an exogenous peptide or peptidomimetic moiety (e.g., a MAb ) capable of binding to an endogenous BBB receptor mediated transport system that traverses the BBB on the endogenous BBB receptor-mediated transport system.
- the MTH can be an antibody to a receptor of the transport system, e.g., the insulin receptor.
- the antibody is a monoclonal antibody (MAb).
- the MAb is a chimeric MAb.
- the method comprises a method of transporting IDS across the BBB, by using a fusion antibody comprising IDS fused to an antibody capable of binding to a BBB receptor-mediated transport system.
- the method comprises a method of transporting IDS across the BBB, by using a fusion antibody comprising IDS fused to an antibody capable of selectively binding to the a BBB receptor-mediated transport system (e.g., a receptor for one or more of the following: insulin, transferrin, insulin-like growth factors 1 and 2 (IGF1 and IGF2), leptin, and/or lipoproteins).
- a BBB receptor-mediated transport system e.g., a receptor for one or more of the following: insulin, transferrin, insulin-like growth factors 1 and 2 (IGF1 and IGF2), leptin, and/or lipoproteins.
- the method comprises a method of transporting IDS across the BBB, by using a fusion antibody comprising IDS fused to an antibody capable of selectively binding to the ECD of the insulin receptor.
- Insulin receptors expressed on the BBB can thereby serve as a vector for transport of the IDS across the BBB.
- Certain ECD-specific antibodies may mimic the endogenous ligand and thereby traverse a plasma membrane barrier via transport on the specific receptor system.
- Such insulin receptor antibodies act as molecular "Trojan horses," or "TH" as depicted schematically in Fig. 7 .
- IDS normally does not cross the blood-brain barrier (BBB).
- BBB blood-brain barrier
- the enzyme is able to cross the BBB, and the brain cell membrane, by trafficking on the IR, which is expressed at both membranes in the brain.
- an HIR Ab-IDS fusion antibody binds an exofacial epitope on the human BBB HIR and this binding enables the fusion antibody to traverse the BBB via a transport reaction that is mediated by the human BBB insulin receptor.
- antibody describes an immunoglobulin whether natural or partly or wholly synthetically produced.
- the term also covers any polypeptide or protein having a binding domain which is, or is homologous to, an antigen-binding domain.
- CDR grafted antibodies are also contemplated by this term.
- “Native antibodies” and “native immunoglobulins” are usually heterotetrameric glycoproteins of about 150,000 daltons, composed of two identical light (L) chains and two identical heavy (H) chains. Each light chain is typically linked to a heavy chain by one covalent disulfide bond, while the number of disulfide linkages varies among the heavy chains of different immunoglobulin isotypes. Each heavy and light chain also has regularly spaced intrachain disulfide bridges. Each heavy chain has at one end a variable domain ("VH”) followed by a number of constant domains ("CH").
- VH variable domain
- CH constant domains
- Each light chain has a variable domain at one end (“VL”) and a constant domain (“CL”) at its other end; the constant domain of the light chain is aligned with the first constant domain of the heavy chain, and the light-chain variable domain is aligned with the variable domain of the heavy chain. Particular amino acid residues are believed to form an interface between the light- and heavy-chain variable domains.
- variable domain refers to protein domains that differ extensively in sequence among family members (i.e., among different isoforms, or in different species).
- variable domain refers to the variable domains of antibodies that are used in the binding and specificity of each particular antibody for its particular antigen.
- variability is not evenly distributed throughout the variable domains of antibodies. It is concentrated in three segments called hypervariable regions both in the light chain and the heavy chain variable domains. The more highly conserved portions of variable domains are called the "framework region" or "FR".
- variable domains of unmodified heavy and light chains each comprise four FRs (FR1, FR2, FR3 and FR4, respectively), largely adopting a ⁇ -sheet configuration, connected by three hypervariable regions, which form loops connecting, and in some cases forming part of, the ⁇ -sheet structure.
- the hypervariable regions in each chain are held together in close proximity by the FRs and, with the hypervariable regions from the other chain, contribute to the formation of the antigen-binding site of antibodies (see Kabat et al., Sequences of Proteins of Immunological Interest, 5th Ed. Public Health Service, National Institutes of Health, Bethesda, Md. (1991), pages 647-669 ).
- the constant domains are not involved directly in binding an antibody to an antigen, but exhibit various effector functions, such as participation of the antibody in antibody-dependent cellular toxicity.
- hypervariable region when used herein refers to the amino acid residues of an antibody which are responsible for antigen-binding.
- the hypervariable region comprises amino acid residues from three “complementarity determining regions” or “CDRs”, which directly bind, in a complementary manner, to an antigen and are known as CDR1, CDR2, and CDR3 respectively.
- the CDRs typically correspond to approximately residues 24-34 (CDRL1), 50-56 (CDRL2) and 89-97 (CDRL3), and in the heavy chain variable domain the CDRs typically correspond to approximately residues 31-35 (CDRH1), 50-65 (CDRH2) and 95-102 (CDRH3); Kabat et al., Sequences of Proteins of Immunological Interest, 5th Ed. Public Health Service, National Institutes of Health, Bethesda, Md.
- residues from a "hypervariable loop” i.e., residues 26-32 (L1), 50-52 (L2) and 91-96 (L3) in the light chain variable domain and 26-32 (H1), 53-55 (H2) and 96-101 (H3) in the heavy chain variable domain; Chothia and Lesk, J. Mol. Biol. 196:901 917 (1987 )).
- variable framework region refers to framework residues that form a part of the antigen binding pocket or groove and/or that may contact antigen.
- the framework residues form a loop that is a part of the antigen binding pocket or groove.
- the amino acids residues in the loop may or may not contact the antigen.
- the loop amino acids of a VFR are determined by inspection of the three-dimensional structure of an antibody, antibody heavy chain, or antibody light chain. The three-dimensional structure can be analyzed for solvent accessible amino acid positions as such positions are likely to form a loop and/or provide antigen contact in an antibody variable domain. Some of the solvent accessible positions can tolerate amino acid sequence diversity and others (e.g. structural positions) can be less diversified.
- the three dimensional structure of the antibody variable domain can be derived from a crystal structure or protein modeling.
- the VFR comprises, consist essentially of, or consists of amino acid positions corresponding to amino acid positions 71 to 78 of the heavy chain variable domain, the positions defined according to Kabat et al ., 1991.
- VFR forms a portion of Framework Region 3 located between CDRH2 and CDRH3. The VFR can form a loop that is well positioned to make contact with a target antigen or form a part of the antigen binding pocket.
- immunoglobulins can be assigned to different classes. There are five major classes of immunoglobulins: IgA, IgD, IgE, IgG, and IgM, and several of these can be further divided into subclasses (isotypes), e.g., IgG1, IgG2, IgG3, IgG4, IgA, and IgA2.
- the heavy-chain constant domains (Fc) that correspond to the different classes of immunoglobulins are called ⁇ , ⁇ , ⁇ , ⁇ , and ⁇ , respectively.
- the subunit structures and three-dimensional configurations of different classes of immunoglobulins are well known.
- the "light chains” of antibodies (immunoglobulins) from any vertebrate species can be assigned to one of two clearly distinct types, called kappa or (" ⁇ ") and lambda or (" ⁇ "), based on the amino acid sequences of their constant domains.
- the terms “selectively bind,” “selectively binding,” “specifically binds,” or “specifically binding” refer to binding to the antibody or fusion antibody to its target antigen for which the dissociation constant (Kd) is about 10 -6 M or lower, i.e., 10 -7 , 10 -8 , 10 -9 , 10 -10 , 10 -11 , or 10 -12 M.
- antibody as used herein will also be understood to mean one or more fragments of an antibody that retain the ability to specifically bind to an antigen, (see generally, Holliger et al., Nature Biotech. 23 (9) 1126-1129 (2005 )).
- Non-limiting examples of such antibodies include (i) a Fab fragment, a monovalent fragment consisting of the VL, VH, CL and CH1 domains; (ii) a F(ab')2 fragment, a bivalent fragment comprising two Fab fragments linked by a disulfide bridge at the hinge region; (iii) a Fd fragment consisting of the VH and CH1 domains; (iv) a Fv fragment consisting of the VL and VH domains of a single arm of an antibody, (v) a dAb fragment ( Ward et al., (1989) Nature 341:544 546 ), which consists of a VH domain; and (vi) an isolated complementarity determining region (CDR).
- CDR
- the two domains of the Fv fragment, VL and VH are coded for by separate genes, they can be joined, using recombinant methods, by a synthetic linker that enables them to be made as a single protein chain in which the VL and VH regions pair to form monovalent molecules (known as single chain Fv (scFv); see e.g., Bird et al. (1988) Science 242:423 426 ; and Huston et al. (1988) Proc. Natl. Acad. Sci. USA 85:5879 5883 ; and Osbourn et al. (1998) Nat. Biotechnol. 16:778 ).
- single chain Fv single chain Fv
- Such single chain antibodies are also intended to be encompassed within the term antibody.
- VH and VL sequences of specific scFv can be linked to human immunoglobulin constant region cDNA or genomic sequences, in order to generate expression vectors encoding complete IgG molecules or other isotypes.
- VH and VL can also be used in the generation of Fab, Fv or other fragments of immunoglobulins using either protein chemistry or recombinant DNA technology.
- Other forms of single chain antibodies, such as diabodies are also encompassed.
- F(ab')2" and “Fab'” moieties can be produced by treating immunoglobulin (monoclonal antibody) with a protease such as pepsin and papain, and includes an antibody fragment generated by digesting immunoglobulin near the disulfide bonds existing between the hinge regions in each of the two H chains.
- immunoglobulin monoclonal antibody
- protease such as pepsin and papain
- papain cleaves IgG upstream of the disulfide bonds existing between the hinge regions in each of the two H chains to generate two homologous antibody fragments in which an L chain composed of VL (L chain variable region) and CL (L chain constant region), and an H chain fragment composed of VH (H chain variable region) and CHy1 ( ⁇ 1 region in the constant region of H chain) are connected at their C terminal regions through a disulfide bond.
- Each of these two homologous antibody fragments is called Fab'.
- Pepsin also cleaves IgG downstream of the disulfide bonds existing between the hinge regions in each of the two H chains to generate an antibody fragment slightly larger than the fragment in which the two above-mentioned Fab' are connected at the hinge region. This antibody fragment is called F(ab')2.
- the Fab fragment also contains the constant domain of the light chain and the first constant domain (CH1) of the heavy chain.
- Fab' fragments differ from Fab fragments by the addition of a few residues at the carboxyl terminus of the heavy chain CH1 domain including one or more cysteine(s) from the antibody hinge region.
- Fab'-SH is the designation herein for Fab' in which the cysteine residue(s) of the constant domains bear a free thiol group.
- F(ab')2 antibody fragments originally were produced as pairs of Fab' fragments which have hinge cysteines between them. Other chemical couplings of antibody fragments are also known.
- Fv is the minimum antibody fragment which contains a complete antigen-recognition and antigen-binding site. This region consists of a dimer of one heavy chain and one light chain variable domain in tight, noncovalent association. It is in this configuration that the three hypervariable regions of each variable domain interact to define an antigen-binding site on the surface of the VH-VL dimer. Collectively, the six hypervariable regions confer antigen-binding specificity to the antibody. However, even a single variable domain (or half of an Fv comprising only three hypervariable regions specific for an antigen) has the ability to recognize and bind antigen, although at a lower affinity than the entire binding site.
- Single-chain Fv or “sFv” antibody fragments comprise a VH, a VL, or both a VH and VL domain of an antibody, wherein both domains are present in a single polypeptide chain.
- the Fv polypeptide further comprises a polypeptide linker between the VH and VL domains which enables the sFv to form the desired structure for antigen binding.
- a "chimeric" antibody includes an antibody derived from a combination of different mammals.
- the mammal may be, for example, a rabbit, a mouse, a rat, a goat, or a human.
- the combination of different mammals includes combinations of fragments from human and mouse sources.
- an antibody of the present invention is a monoclonal antibody (MAb), typically a chimeric human-mouse antibody derived by humanization of a mouse monoclonal antibody.
- MAb monoclonal antibody
- Such antibodies are obtained from, e.g., transgenic mice that have been "engineered” to produce specific human antibodies in response to antigenic challenge.
- elements of the human heavy and light chain locus are introduced into strains of mice derived from embryonic stem cell lines that contain targeted disruptions of the endogenous heavy chain and light chain loci.
- the transgenic mice can synthesize human antibodies specific for human antigens, and the mice can be used to produce human antibody-secreting hybridomas.
- a chimeric antibody e.g., HIR Ab, other antibodies capable of crossing the BBB
- contains enough human sequence that it is not significantly immunogenic when administered to humans, e.g., about 80% human and about 20% mouse, or about 85% human and about 15% mouse, or about 90% human and about 10% mouse, or about 95% human and 5% mouse, or greater than about 95% human and less than about 5% mouse.
- a more highly humanized form of the antibody( e.g., HIR Ab, other antibodies capable of crossing the BBB) can also be engineered, and the humanized antibody (e.g. HIR Ab) has activity comparable to the murine HIR Ab and can be used in embodiments of the invention. See, e.g., U.S.
- Humanized antibodies to the human BBB insulin receptor with sufficient human sequences for use in the invention are described in, e.g., Boado et al. (2007), Biotechnol Bioeng, 96(2):381-391 .
- the HIR antibodies or HIR-IDS fusion antibodies derived therefrom contain an immunoglobulin heavy chain comprising CDRs corresponding to the sequence of at least one of the HC CDRs listed in Fig. 3 (SEQ ID NOs 1-3) or a variant thereof.
- a HC CDR1 corresponding to the amino acid sequence of SEQ ID NO:1 with up to 1, 2, 3, 4, 5, or 6 single amino acid mutations
- a HC CDR2 corresponding to the amino acid sequence of SEQ ID NO:2 with up to 1, 2, 3, 4, 5, 6, 7, 8, 9, or 10 single amino acid mutations
- a HC CDR3 corresponding to the amino acid sequence of SEQ ID NO:3 with up to 1, or 2 single amino acid mutations, where the single amino acid mutations are substitutions, deletions, or insertions.
- the HIR Abs or HIR Ab-IDS fusion Abs contain an immunoglobulin HC the amino acid sequence of which is at least 50% identical (i.e., at least, 55, 60, 65, 70, 75, 80, 85, 90, 95, or any other percent up to 100% identical) to SEQ ID NO:7 (shown in Fig. 1 ).
- the HIR Abs or HIR Ab-IDS fusion Abs include an immunoglobulin light chain comprising CDRs corresponding to the sequence of at least one of the LC CDRs listed in Fig. 3 (SEQ ID NOs: 4-6) or a variant thereof.
- a LC CDR1 corresponding to the amino acid sequence of SEQ ID NO:4 with up to 1, 2, 3, 4, or 5 single amino acid mutations
- a LC CDR2 corresponding to the amino acid sequence of SEQ ID NO:5 with up to 1, 2, 3, or 4 single amino acid mutations
- a LC CDR3 corresponding to the amino acid sequence of SEQ ID NO:6 with up to 1, 2, 3, 4, or 5 single amino acid mutations.
- the HIR Abs or HIR Ab-IDS fusion Abs contain an immunoglobulin LC the amino acid sequence of which is at least 50% identical (i.e., at least, 55, 60, 65, 70, 75, 80, 85, 90, 95, or any other percent up to 100% identical) to SEQ ID NO:8 (shown in Fig. 2 ).
- the HIR Abs or HIR Ab-IDS fusion Abs contain both a heavy chain and a light chain corresponding to any of the above-mentioned HIR heavy chains and HIR light chains.
- HIR antibodies used in the invention may be glycosylated or non-glycosylated. If the antibody is glycosylated, any pattern of glycosylation that does not significantly affect the function of the antibody may be used. Glycosylation can occur in the pattern typical of the cell in which the antibody is made, and may vary from cell type to cell type. For example, the glycosylation pattern of a monoclonal antibody produced by a mouse myeloma cell can be different than the glycosylation pattern of a monoclonal antibody produced by a transfected Chinese hamster ovary (CHO) cell. In some embodiments, the antibody is glycosylated in the pattern produced by a transfected Chinese hamster ovary (CHO) cell..
- sequence variants of candidate antibodies e.g., HIR Ab, other antibodies capable of crossing the BBB
- candidate antibodies e.g., HIR Ab, other antibodies capable of crossing the BBB
- a target antigen such as the ECD of the human insulin receptor or an isolated epitope thereof.
- Fukuda et al. (2006) "In vitro evolution of single-chain antibodies using mRNA display," Nuc. Acid Res., 34(19 ) (published online) for an example of ⁇ ltra high throughput screening of antibody sequence variants. See also, Chen et al.
- An insulin receptor ECD can be purified as described in, e.g., Coloma et al. (2000) Pharm Res, 17:266-274 , and used to screen for HIR Abs and HIR Ab sequence variants of known HIR Abs.
- a genetically engineered HIR Ab with the desired level of human sequences, is fused to an IDS, to produce a recombinant fusion antibody that is a bi-functional molecule.
- the HIR Ab-IDS fusion antibody (i) binds to an extracellular domain of the human insulin receptor; (ii) catalyzes hydrolysis of linkages in dermatan and/or heparan sulfate; and (iii) is able to cross the BBB, via transport on the BBB HIR, and retain IDS activity once inside the brain, following peripheral administration.
- IDS Iduronate 2-sulfatase
- IDS e.g., Elaprase ®
- recombinant IDS fails to rescue a deficiency of IDS in the CNS of patients suffering from Hunter's syndrome. IDS does not cross the BBB, and the lack of transport of the enzyme across the BBB prevents it from having a significant therapeutic effect in the CNS following peripheral administration.
- the IDS when the IDS is fused to an antibody capable of crossing the BBB (e.g., HIR Ab), the IDS is able to enter the CNS from blood following a non-invasive peripheral route of administration such as intravenous, intra-arterial, intramuscular, subcutaneous, intraperitoneal, or even oral administration, or other route described herein.
- Administration of a IDS fusion antibody e.g., HIR Ab-IDS
- a systemic dose of a IDS fusion antibody e.g., HIR Ab-IDS
- a systemic dose of a IDS fusion antibody e.g., HIR Ab-IDS
- an IDS fusion antibody e.g., HIR Ab-IDS
- Dermatan sulfate, heparan sulfate and heparin are variably sulfated glycosaminoglycans, which are long, unbranched polysaccharides made up of a repeating disaccharide unit.
- L-iduronate or L-iduronic acid
- dermatan sulfate and heparin is also present in heparan sulfate.
- IDS e.g., the human IDS sequence listed under GenBank Accession No. NP_000193
- NP_000193 refers to any naturally occurring or artificial enzyme that can catalyze the hydrolysis or removal of 2-sulfate groups of the L-iduronate 2-sulfate units of dermatan sulfate, heparan sulfate and heparin.
- IDS is a member of a family of sulfatases that requires a specific post-translational modification for expression of IDS enzyme activity.
- the activity of the IDS enzyme is activated following the conversion of Cys-59 to a formylglycine residue by a sulfatase modifying factor type 1 (SUMF1), which is also called the formylglycine generating enzyme (FGE).
- SUMF1 sulfatase modifying factor type 1
- FGE formylglycine generating enzyme
- the fusion antibody comprising IDS is post-translationally modified by a sulfatase modifying factor type 1 (SLTMF1).
- the post-translational modification comprises a cysteine to formylglycine conversion.
- the fusion antibody comprises an IDS that comprises a formylglycine residue.
- the subject composition comprises an IDS has an amino acid sequence that is at least 50% identical (i.e., at least, 55, 60, 65, 70, 75, 80, 85, 90, 95, or any other percent up to 100% identical) to the amino acid sequence of human IDS, a 550 amino acid protein listed under GenBank Accession No. NP_000193, or a 525 amino acid subsequence thereof, which lacks a 25 amino acid signal peptide, and corresponds to SEQ ID NO:9 ( Fig. 4 ).
- the structure-function relationship of human IDS is well established, as described in, e.g., Sukegawa-Hayasaka et al.
- residues that are critical to the function of IDS include, e.g., Arg 48, Ala 85, Pro 86, Ser 333, Trp 337, Ser 349, Arg 468, and Gln 531.
- IDS has an amino acid sequence at least 50% identical (i.e., at least, 55, 60, 65, 70, 75, 80, 85, 90, 95, or any other percent up to 100% identical) to SEQ ID NO:9 (shown in Fig. 4 ).
- Sequence variants of a canonical IDS sequence such as SEQ ID NO:9 can be generated, e.g., by random mutagenesis of the entire sequence or specific subsequences corresponding to particular domains.
- site directed mutagenesis can be performed reiteratively while avoiding mutations to residues known to be critical to IDS function such as those given above.
- mutation tolerance prediction programs can be used to greatly reduce the number of non-functional sequence variants that would be generated by strictly random mutagenesis.
- Various programs) for predicting the effects of amino acid substitutions in a protein sequence on protein function are described in, e.g., Henikoff et al. (2006), "Predicting the Effects of Amino Acid Substitutions on Protein Function," Annu. Rev. Genomics Hum. Genet., 7:61-80 .
- IDS sequence variants can be screened for of IDS activity/retention of IDS activity by, e.g., 4-methylumbelliferyl -L-iduronide-2-sulphate (4-MUS) flurometric IDS assays known in the art. See, e.g., Voznyi et al. (2001), J. Inherit. Metab. Dis.24: 675-680 .
- One unit of IDS activity is defined as the hydrolysis of 1 nmole substrate/hour. Accordingly, one of ordinary skill in the art will appreciate that a very large number of operable IDS sequence variants can be obtained by generating and screening extremely diverse "libraries" of IDS sequence variants by methods that are routine in the art, as described above.
- Percent sequence identity is determined by conventional methods. See, for example, Altschul et al., Bull. Math. Bio. 48:603 (1986 ), and Henikoff and Henikoff, Proc. Natl. Acad. Sci. USA 89:10915 (1992 ). Briefly, two amino acid sequences are aligned to optimize the alignment scores using a gap opening penalty of 10, a gap extension penalty of 1, and the "BLOSUM62" scoring matrix of Henikoff and Henikoff (ibid.). The percent identity is then calculated as: ([Total number of identical matches]/[length of the longer sequence plus the number of gaps introduced into the longer sequence in order to align the two sequences])(100).
- the "FASTA" similarity search algorithm of Pearson and Lipman is a suitable protein alignment method for examining the level of identity shared by an amino acid sequence disclosed herein and the amino acid sequence of another peptide.
- the FASTA algorithm is described by Pearson and Lipman, Proc. Nat'l Acad. Sci. USA 85:2444 (1988 ), and by Pearson, Meth. Enzymol. 183:63 (1990 ).
- the ten regions with the highest density of identities are then rescored by comparing the similarity of all paired amino acids using an amino acid substitution matrix, and the ends of the regions are "trimmed" to include only those residues that contribute to the highest score.
- the trimmed initial regions are examined to determine whether the regions can be joined to form an approximate alignment with gaps.
- the highest scoring regions of the two amino acid sequences are aligned using a modification of the Needleman-Wunsch-Sellers algorithm ( Needleman and Wunsch, J. Mol. Biol. 48:444 (1970 ); Sellers, SIAM J. Appl. Math. 26:787 (1974 )), which allows for amino acid insertions and deletions.
- the present invention also includes proteins having a conservative amino acid change, compared with an amino acid sequence disclosed herein.
- a "conservative amino acid substitution” is illustrated by a substitution among amino acids within each of the following groups: (1) glycine, alanine, valine, leucine, and isoleucine, (2) phenylalanine, tyrosine, and tryptophan, (3) serine and threonine, (4) aspartate and glutamate, (5) glutamine and asparagine, and (6) lysine, arginine and histidine.
- the BLOSUM62 table is an amino acid substitution matrix derived from about 2,000 local multiple alignments of protein sequence segments, representing highly conserved regions of more than 500 groups of related proteins ( Henikoff and Henikoff, Proc. Nat'l Acad. Sci. USA 89:10915 (1992 )). Accordingly, the BLOSUM62 substitution frequencies can be used to define conservative amino acid substitutions that may be introduced into the amino acid sequences of the present invention. Although it is possible to design amino acid substitutions based solely upon chemical properties (as discussed above), the language "conservative amino acid substitution” preferably refers to a substitution represented by a BLOSUM62 value of greater than -1.
- an amino acid substitution is conservative if the substitution is characterized by a BLOSUM62 value of 0, 1, 2, or 3.
- preferred conservative amino acid substitutions are characterized by a BLOSUM62 value of at least 1 (e.g., 1, 2 or 3), while more preferred conservative amino acid substitutions are characterized by a BLOSUM62 value of at least 2 (e.g., 2 or 3).
- amino acid sequences may include additional residues, such as additional Nor C-terminal amino acids, and yet still be essentially as set forth in one of the sequences disclosed herein, so long as the sequence retains sufficient biological protein activity to be functional in the compositions and methods of the invention.
- compositions of the invention are useful for multiple reasons including being useful for: transporting IDS across the BBB, delivering a therapeutic effective dose of IDS, and/or retaining activity of the IDS once transported across the BBB, or once fused to a targeting antibody.
- Compositions of the invention are also useful in that the IDS and/or the structure it is bound to (e.g., immunogloblulin, antibody) within the fusion antibody each retains a certain amount of its activity compared to its activity as a separate entity.
- the invention provides compositions containing an IDS covalently linked to a structure (e.g., immunoglobulin, antibody) that is capable of crossing the blood brain barrier (BBB), where the IDS retains at least about 10, 20, 30, 40, 50, 60, 70, 80, 90, 95, 99, or 100% of its activity, compared to its activity as a separate entity.
- the invention provides compositions containing an IDS covalently linked to a structure (e.g., immunoglobulin, antibody) that is capable of crossing the blood brain barrier (BBB), where the structure retains at least about 10, 20, 30, 40, 50, 60, 70, 80, 90, 95, 99, or 100% of its activity, compared to its activity as a separate entity.
- the invention provides compositions containing an IDS covalently linked to a structure (e.g., immunoglobulin, antibody) that is capable of crossing the blood brain barrier (BBB), where the structure and the IDS each retains at least about 10, 20, 30, 40, 50, 60, 70, 80, 90, 95, 99, or 100% of its activity, compared to its activity as a separate entity.
- a structure e.g., immunoglobulin, antibody
- BBB blood brain barrier
- the IDS retains at least about 10% of its activity compared to its activity as a separate entity.
- the IDS retains at least 20% of its activity, compared to its activity as a separate entity.
- the IDS retains at least 30% of its activity, compared to its activity as a separate entity.
- the IDS retains at least 40% of its activity, compared to its activity as a separate entity. In some embodiments, the IDS retains at least 50% of its activity, compared to its activity as a separate entity. In some embodiments, the IDS retains at least 60% of its activity, compared to its activity as a separate entity.
- the invention also provides compositions containing an IDS that is covalently linked to a chimeric MAb to the human BBB insulin receptor.
- the invention also provides pharmaceutical compositions that contain one or more compositions of the invention and a pharmaceutically acceptable excipient.
- the subject composition comprises a IDS fusion antibody where at least about 0.3% (i.e., about 0.32%), 0.4%, 0.48%, 0.6%, 0.74%, 0.8%, 0.9%, 1.05, 1.1, 1.2, 1.3%, 1.5%, 2%, 2.5%, 5%, or any % from about 0.3% to about 12%) of the systemically administered IDS fusion antibody is capable of being delivered to the brain as a result of its uptake from peripheral blood across the BBB.
- the composition comprises an IDS fusion antibody wherein at least 0.5%, (i.e., about 0.32%, 0.4%, 0.48%, 0.6%, 0.74%, 0.8%, 0.9%, 1.05, 1.1, 1.2, 1.3%, 1.5%, 2%, 2.5%, 5%, or any % from about 0.3% to about 12%) of the systemically administered dose of the IDS fusion antibody is delivered to the brain within two hours or less, i.e., 1.8, 1.7, 1.5, 1.4, 1.3, 1.2, 1.1, 0.9, 0.8, 0.6, 0.5 or any other period from about 0.5 to about two hours after systemic administration.
- the present IDS fusion antibodies can cross the BBB, and thereby provide at least 0.125 units of IDS activity/mg protein in the subject's brain, e.g., 0.14, 0.15, 0.16, 0.17, 0.18, 0.19, 0.2, 0.21, 0.22, 0.23, 0.24, 0.25, 0.3, 0.4, 0.5, 0.75, 1.0, 1.5, 2, or any other value from 0.125 to 2.5 of units of IDS activity/mg protein in the subject's brain.
- the total number of units of IDS activity delivered to a subject's brain is at least, 12,500 units, e.g., at least 25,000, 30,000, 35,000, 40,000, 45,000, 50,000, 60,000, 70,000, 80,000, 90,000, 110,000, 120,000, 130,000, 140,000, 150,000, 160,000, 170,000, 180,000, 190,000, 200,000, 210,000, 220,000, 230,000, 250,000 or any other total number of IDS units from about 12,500 to 250,000 units of IDS activity.
- the total number of units of IDS activity delivered to a subject's brain is at least, 10,000 units, e.g., at least 10,000, 12,500, 25,000, 30,000, 35,000, 40,000, 45,000, 50,000, 60,000, 70,000, 80,000, 90,000, 110,000, 120,000, 130,000, 140,000, 150,000, 160,000, 170,000, 180,000, 190,000, 200,000, 210,000, 220,000, 230,000, 250,000, 300,000, 5000,000 any other total number of IDS units from about 10,000 to 500,000 units of IDS activity.
- at least about 25,000 units of iduronate-2-sulfatase activity is delivered to the brain, normalized per 50 kg body weight.
- At least about 10,000, 15,000, 25,000, 30,000, 35,000, 40,000, 45,000, 50,000, 60,000, 70,000, 80,000, 90,000, 110,000, 120,000, 130,000, 140,000, 150,000, 160,000, 170,000, 180,000, 190,000, 200,000, 210,000, 220,000, 230,000, 250,000 units of iduronate-2-sulfatase activity is delivered to the brain, normalized per 50 kg body weight. In some embodiments, at least about 25,000 000 units of iduronate-2-sulfatase activity is delivered to the brain, normalized per 50 kg body weight.
- a therapeutically effective systemic dose comprises at least 5 x 10 5 , 1 x 10 6 , 2 x 10 6 , 3 ⁇ 10 6 , 4, 10 6 5 ⁇ 10 6 , 6 ⁇ 10 6 , 7 ⁇ 10 6 , 8 ⁇ 10 6 , 9 ⁇ 10 6 , 1 ⁇ 10 7 , 1.1 ⁇ 10 7 , 1.2 ⁇ 10 7 , 1.5 ⁇ 10 7 , 1.6 ⁇ 10 7 , 1.7 ⁇ 10 7 , 1.8 ⁇ 10 7 , 1.9 ⁇ 10 7 , 2 ⁇ 10 7 , 2.1 ⁇ 10 7 , 3 ⁇ 10 7 , or any other systemic dose from about 5 ⁇ 10 5 to 3 ⁇ 10 7 units of IDS activity.
- a therapeutically effective systemic dose is at least about 20,000 units, or at least about 10,000 units of IDS activity/kg body weight, at least about 10,000, 15,000, 20,000, 22,000, 24,000, 25,000, 30,000, 40,000, 50,000, 60,000, 70,000, 80,000, 90,000, 100,000, 125,000, 150,000, 200,000, or 500,000 units/kg body weight.
- the mass amount of a therapeutically effective systemic dose of an IDS fusion antibody (e.g., HIR Ab-IDS ) will depend, in part, on its IDS specific activity.
- the IDS specific activity of the IDS fusion antibody is at least 10,000 U/mg of protein, at least about 11,000, 12,000, 13,000, 14,000, 20,000, 21,000, 22,000, 23,000, 24,000, 25,000, 26,000, 27,000, 28,000, 30,000, 32,000, 34,000, 35,000, 36,000, 37,000, 40,000, 45,000, 50,000, or any other specific activity value from about 10,000 units/mg to about 50,000 units/mg.
- the structure that is capable of crossing the BBB utilizes an endogenous BBB receptor mediated transport system, such as a system that utilizes the insulin receptor, transferrin receptor, leptin receptor, LDL receptor, or IGF receptor.
- the endogenous BBB receptor mediated transport system is the insulin BBB receptor mediated transport system.
- the structure that is capable of crossing the BBB is an antibody, e.g., a monoclonal antibody (MAb) such as a chimeric MAb.
- the antibody can be a chimeric antibody with sufficient human sequence that it is suitable for administration to a human.
- the structure capable of crossing the blood brain barrier crosses the BBB on an endogenous BBB receptor-mediated transporter, such as a transporter selected from the group consisting of the insulin transporter, the transferrin transporter, the leptin transporter, the LDL transporter, and the IGF receptor.
- the endogenous BBB receptor-mediated transporter is selected from the group consisting of the insulin transporter and the transferrin transporter.
- the endogenous BBB receptor-mediated transporter is the insulin transporter, e.g., the human insulin transporter.
- the structure capable of crossing the BBB can be an antibody, e.g., a MAb such as a chimeric MAb.
- the antibody can be an antibody to an endogenous BBB receptor-mediated transporter, as described herein.
- the antibody can be glycosylated or nonglycosylated; in some embodiments, the antibody is glycosylated, e.g., in a glycosylation pattern produced by its synthesis in a CHO cell.
- the covalent linkage between the antibody and the IDS may be a linkage between any suitable portion of the antibody and the IDS, as long as it allows the IDS fusion antibody to cross the blood brain barrier and/or the IDS to retain a therapeutically useful portion of its activity within the CNS.
- the covalent link is between one or more light chains of the antibody and the IDS.
- the IDS can be covalently linked by its carboxy or amino terminus to the carboxy or amino terminus of the light chain (LC) or heavy chain (HC) of the antibody.
- Any suitable linkage may be used, e.g., carboxy terminus of light chain to amino terminus of peptide, carboxy terminus of heavy chain to amino terminus of peptide, amino terminus of light chain to amino terminus of peptide, amino terminus of heavy chain to amino terminus of peptide, carboxy terminus of light chain to carboxy terminus of peptide, carboxy terminus of heavy chain to carboxy terminus of peptide, amino terminus of light chain to carboxy terminus of peptide, or amino terminus of heavy chain to carboxy terminus of peptide.
- the linkage is from the carboxy terminus of the HC to the amino terminus of the peptide. It will be appreciated that a linkage between terminal amino acids is not required, and any linkage which meets the requirements of the invention may be used; such linkages between non-terminal amino acids of peptides are readily accomplished by those of skill in the art.
- more than one molecule of the IDS is attached to the structure that crosses the BBB.
- 2, 3, 4, 5, 6, 7, 8, 9, 10, or more than 10 IDS molecules (or fraction thereof) may be attached to the structure that is capable of crossing the blood brain barrier.
- the bifunctional IDS fusion antibody (e.g., HIR Ab-IDS ) described herein, may retain a high proportion of the activity of their separate constituent proteins, e.g., binding of the HIR Ab to the IR ECD, and the enzymatic activity of IDS.
- Construction of cDNAs and expression vectors encoding any of the proteins described herein, as well as their expression and purification are well within those of ordinary skill in the art, and are described in detail herein in, e.g., Examples 1-3, and, in Boado et al (2007), Biotechnol Bioeng 96:381-391 , U.S. Patent Application Serial No. 11/061,956 , and U.S. Patent Application Serial No. 11/245,710 .
- bifunctional IDS fusion antibodies e.g., HIR Ab-IDS containing a targeting antibody (e.g., HIR Ab), as described herein, capable of crossing the BBB fused to IDS, where the targeting antibody (e.g., HIR Ab) capable of crossing the blood brain barrier and the IDS each retain an average of at least about 10, 20, 30, 40, 50, 60, 70, 80, 90, 95,99, or 100% of their activities, compared to their activities as separate entities.
- the invention provides a HIR Ab-IDS fusion antibody where the HIR Ab and IDS each retain an average of at least about 50% of their activities, compared to their activities as separate entities.
- the invention provides a HIR Ab-IDS fusion antibody where the HIR Ab and IDS each retain an average of at least about 60% of their activities, compared to their activities as separate entities. In some embodiments, the invention provides a HIR Ab-IDS fusion antibody where the HIR Ab and IDS each retain an average of at least about 70% of their activities, compared to their activities as separate entities. In some embodiments, the invention provides a HIR Ab-IDS fusion antibody where the HIR Ab and IDS each retain an average of at least about 80% of their activities, compared to their activities as separate entities.
- the invention provides a fusion HIR Ab-IDS fusion antibody where the HIR Ab and IDS each retain an average of at least about 90% of their activities, compared to their activities as separate entities.
- the HIR Ab retains at least about 10, 20, 30, 40, 50, 60, 70, 80, 90, 95, 99, or 100% of its activity, compared to its activity as a separate entity
- the IDS retains at least about 10, 20, 30, 40, 50, 60, 70, 80, 90, 95, 99, or 100% of its activity, compared to its activity as a separate entity.
- compositions containing a bifunctional IDS fusion antibody capable of crossing the BBB, where the constituent antibody (e.g., HIR Ab) and IDS each retain, as part of the fusion antibody, an average of at least about 10, 20, 30, 40, 50, 60, 70, 80, 90, 95, 99, or 100% of their activities, e.g., HIR binding and IDS activity, respectively, compared to their activities as separate proteins.
- a bifunctional IDS fusion antibody e.g., HIR Ab-IDS
- HIR Ab a bifunctional IDS fusion antibody capable of crossing the BBB
- the constituent antibody e.g., HIR Ab
- IDS each retain, as part of the fusion antibody, an average of at least about 10, 20, 30, 40, 50, 60, 70, 80, 90, 95, 99, or 100% of their activities, e.g., HIR binding and IDS activity, respectively, compared to their activities as separate proteins.
- An HIR Ab IDS fusion antibody refers to a fusion protein comprising any
- the IDS fusion antibodies (e.g., HIR Ab-IDS ) described herein, comprise a covalent linkage between the carboxy terminus of the antibody (e.g., HIR Ab) and the amino terminus of the IDS (or, between the amino terminus of the antibody and the carboxy terminus of the IDS), wherein the IDS fusion antibody (e.g., HIR Ab-IDS) binds to the receptor-mediated BBB transport system (e.g., to the ECD of the IR ) and crosses the blood brain barrier.
- the IDS retains a therapeutically useful portion of its activity.
- the covalent linkage between the antibody and the IDS may be to the carboxy or amino terminal of the targeting antibody (e.g., HIR antibody) and the amino or carboxy terminal of the IDS and linkage allows the HIR Ab-IDS fusion antibody to bind to the ECD of the IR and cross the blood brain barrier, and allows the IDS to retain a therapeutically useful portion of its activity.
- the covalent link is between an HC of the antibody and the IDS or a LC of the antibody and the IDS.
- any suitable linkage may be used, e.g., carboxy terminus of light chain to amino terminus of IDS, carboxy terminus of heavy chain to amino terminus of IDS, amino terminus of light chain to amino terminus of IDS, amino terminus of heavy chain to amino terminus of IDS, carboxy terminus of light chain to carboxy terminus of IDS, carboxy terminus of heavy chain to carboxy terminus of IDS, amino terminus of light chain to carboxy terminus of IDS, or amino terminus of heavy chain to carboxy terminus of IDS.
- the linkage is from the carboxy terminus of the HC to the amino terminus of the IDS.
- the IDS may be fused, or covalently linked, to the targeting antibody (e.g., MAb, HIR-MAb) through a linker.
- a linkage between terminal amino acids can be accomplished by an intervening peptide linker sequence that forms part of the fused amino acid sequence.
- the peptide sequence linker may be 0, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, or more than 10 amino acids in length. In some embodiments, including some preferred embodiments, the peptide linker is less than 20, 15, 14, 13, 12, 11, 10, 9, 8, 7, 6, 5, 4, 3, 2, or 1 amino acids in length. In some embodiments, including some preferred embodiments, the peptide linker is at least 0, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10 amino acids in length.
- the IDS is directly linked to the targeting antibody, and is therefore 0 amino acids in length. In some embodiments, there is no linker linking the IDS to the targeting antibody. In some embodiments, the amino terminus of the IDS is fused directly to the carboxyl terminal of the targeting antibody (e.g., HIR MAb), and therefore there is no linker linking the IDS to the targeting antibody (e.g., HIR MAb),. In some embodiments, the carboxy terminus of the IDS is fused directly to the amino terminus of the targeting antibody (e.g., HIR MAb), and therefore there is no linker linking the IDS to the targeting antibody (e.g., HIR MAb).
- the amino terminus of the IDS is fused directly to the carboxyl terminal of the targeting antibody (e.g., HIR MAb), and therefore there is no linker linking the IDS to the targeting antibody (e.g., HIR MAb).
- the amino terminus of the IDS is fused directly to the carboxyl terminus of the HC of the to the targeting antibody (e.g., HIR MAb). In some embodiments, the amino terminus of the IDS is fused to the carboxyl terminal of the targeting antibody (e.g., HIR MAb) through a linker (e.g., any linker described herein). In some embodiments, the carboxy terminus of the IDS is fused to the amino terminus of the targeting antibody (e.g., HIR MAb) through a linker (e.g., any linker described herein). In some embodiments, the amino terminus of the IDS is fused to the carboxyl terminus of the HC of the HIR through a linker (e.g., any linker described herein).
- the linker comprises glycine, serine, and/or alanine residues in any combination or order.
- the combined percentage of glycine, serine, and alanine residues in the linker is at least 5%, 10%, 15%, 20%, 25%, 30%, 40%, 50%, 60%, 70%, 75%, 80%, 90%, or 95% of the total number of residues in the linker.
- the combined percentage of glycine, serine, and alanine residues in the linker is at least 50%, 60%, 70%, 75%, 80%, 90%, or 95% of the total number of residues in the linker.
- any number of combinations of amino acids can be used for the linker.
- a two amino acid linker is used.
- the linker has the sequence Ser-Ser.
- a two amino acid linker comprises glycine, serine, and/or alanine residues in any combination or order (e.g., Gly-Gly, Ser-Gly, Gly-Ser, Ser-Ser, Ala-Ala, Ser-Ala, or Ala-Ser linker).
- a two amino acid linker consists of one glycine, serine, and/or alanine residue along with another amino acid (e.g., Ser-X, where X is any known amino acid).
- the two-amino acid linker consists of any two amino acids (e.g., X-X), exept gly, ser, or ala..
- a linker for use in the present disclosure is greater than two amino acids in length.
- Such linker may also comprise glycine, serine, and/or alanine residues in any combination or order, as described further herein..
- the linker consists of one glycine, serine, and/or alanine residue along with other amino acids (e.g., Ser-nX, where X is any known amino acid, and n is the number of amino acids).
- the linker consists of any two amino acids (e.g., X-X).
- said any two amino acids are Gly, Ser, or Ala, in any combination or order, and within a variable number of amino acids intervening between them.
- the linker consists of at least one Gly. In an example of an embodiment, the linker consists of at least one Ser. In an example of an embodiment, the linker consists of at least one Ala. In some embodiments, the linker consists of at least 1, 2, 3, 4, 5, 6, 7, 8, 9, or 10 Gly, Ser, and/or Ala residues. In preferred embodiments, the linker comprises Gly and Ser in repeating sequences, in any combination or number, such as (Gly 4 Ser) 3 , or other variations.
- a linker for use in the present invention may be designed by using any method known in the art. For example, there are multiple publicly-available programs for determining optimal amino acid linkers in the engineering of fusion proteins. Publicly-available computer programs (such as the LINKER program) that automatically generate the amino acid sequence of optimal linkers based on the user's input of the sequence of the protein and the desired length of the linker may be used for the present methods and compositions. Often, such programs may use observed trends of naturally-occurring linkers joining protein subdomains to predict optimal protein linkers for use in protein engineering. In some cases, such programs use other methods of predicting optimal linkers.
- Publicly-available computer programs such as the LINKER program
- Such programs may use observed trends of naturally-occurring linkers joining protein subdomains to predict optimal protein linkers for use in protein engineering. In some cases, such programs use other methods of predicting optimal linkers.
- the peptide linker sequence may include a protease cleavage site, however this is not a requirement for activity of the IDS; indeed, an advantage of these embodiments of the present invention is that the bifunctional IDS fusion antibody (e.g., HIR Ab-IDS ) described herein, without cleavage, is partially or fully active both for transport and for activity once across the BBB.
- Fig. 5 shows an exemplary embodiment of the amino acid sequence of a HIR Ab-IDS fusion antibody (SEQ ID NO:10) in which the HC is fused through its carboxy terminus via a two amino acid "ser-ser" linker to the amino terminus of the IDS.
- the fused IDS sequence is devoid of its 25 amino acid signal peptide, as shown in Fig. 4 .
- an IDS fusion antibody (e.g., HIR Ab-IDS ) described herein comprises both a HC and a LC.
- an IDS fusion antibody (e.g., HIR Ab-IDS ) described herein is a monovalent antibody.
- the IDS fusion antibody (e.g., HIR Ab-IDS ) described herein is a divalent antibody, as described herein in the Example section.
- the targeting antibody used as part of the IDS fusion antibody can be glycosylated or nonglycosylated; in some embodiments, the antibody is glycosylated, e.g., in a glycosylation pattern produced by its synthesis in a CHO cell.
- activity includes physiological activity (e.g., ability to cross the BBB and/or therapeutic activity), binding affinity (including binding affinity of the targeting antibody (e.g., HIR MAb) for the receptor-mediated BBB transport system), or the enzymatic activity of IDS.
- physiological activity e.g., ability to cross the BBB and/or therapeutic activity
- binding affinity including binding affinity of the targeting antibody (e.g., HIR MAb) for the receptor-mediated BBB transport system
- the enzymatic activity of IDS includes physiological activity (e.g., ability to cross the BBB and/or therapeutic activity), binding affinity (including binding affinity of the targeting antibody (e.g., HIR MAb) for the receptor-mediated BBB transport system), or the enzymatic activity of IDS.
- Transport of the IDS fusion antibody (e.g., HIR Ab-IDS ) across the BBB may be compared to transport across the BBB of the targeting antibody (e.g., HIR Ab) alone by standard methods.
- the targeting antibody e.g., HIR Ab
- pharmacokinetics and brain uptake of the HIR Ab-IDS fusion antibody by a model animal, e.g., a mammal such as a primate may be used.
- standard models for determining IDS activity may also be used to compare the function of the IDS alone and as part of a HIR Ab-IDS fusion antibody. See, e.g., Example 3, which demonstrates the enzymatic activity of IDS versus HIR Ab-IDS fusion antibody.
- Binding affinity for the IR ECD can be compared for the HIR Ab-IDS fusion antibody versus the HIR Ab alone. See, e.g., Example 3 herein.
- compositions that contain one or more IDS fusion antibodies (e.g., HIR Ab-IDS ) described herein and a pharmaceutically acceptable excipient.
- IDS fusion antibodies e.g., HIR Ab-IDS
- Pharmaceutical compositions of the invention include compositions suitable for administration via any peripheral route, including intravenous, subcutaneous, intramuscular, intraperitoneal injection; oral, rectal, transbuccal, pulmonary, transdermal, intranasal, or any other suitable route of peripheral administration.
- compositions of the invention are particular suited for injection, e.g., as a pharmaceutical composition for intravenous, subcutaneous, intramuscular, or intraperitoneal administration.
- Aqueous compositions of the present invention comprise an effective amount of a composition of the present invention, which may be dissolved or dispersed in a pharmaceutically acceptable carrier or aqueous medium.
- pharmaceutically or pharmacologically acceptable refer to molecular entities and compositions that do not produce an adverse, allergic or other untoward reaction when administered to an animal, e.g., a human, as appropriate.
- pharmaceutically acceptable carrier includes any and all solvents, dispersion media, coatings, antibacterial and antifungal agents, isotonic and absorption delaying agents and the like.
- the use of such media and agents for pharmaceutically active substances is well known in the art. Except insofar as any conventional media or agent is incompatible with the active ingredient, its use in the therapeutic compositions is contemplated. Supplementary active ingredients can also be incorporated into the compositions.
- Exemplary pharmaceutically acceptable carriers for injectable compositions can include salts, for example, mineral acid salts such as hydrochlorides, hydrobromides, phosphates, sulfates, and the like; and the salts of organic acids such as acetates, propionates, malonates, benzoates, and the like.
- compositions of the invention may be provided in liquid form, and formulated in saline based aqueous solution of varying pH (5-8), with or without detergents such polysorbate-80 at 0.01-1%, or carbohydrate additives, such mannitol, sorbitol, or trehalose.
- Commonly used buffers include histidine, acetate, phosphate, or citrate.
- these preparations can contain a preservative to prevent the growth of microorganisms.
- the prevention of the action of microorganisms can be brought about by various antibacterial and antifungal agents, for example, parabens, chlorobutanol; phenol, sorbic acid, thimerosal, and the like.
- isotonic agents for example, sugars or sodium chloride.
- Prolonged absorption of the injectable compositions can be brought about by the use in the compositions of agents delaying absorption, for example, aluminum monostearate, and gelatin.
- compositions For human administration, preparations meet sterility, pyrogenicity, general safety, and purity standards as required by FDA and other regulatory agency standards.
- the active compounds will generally be formulated for parenteral administration, e.g., formulated for injection via the intravenous, intramuscular, subcutaneous, intralesional, or intraperitoneal routes.
- parenteral administration e.g., formulated for injection via the intravenous, intramuscular, subcutaneous, intralesional, or intraperitoneal routes.
- the preparation of an aqueous composition that contains an active component or ingredient will be known to those of skill in the art in light of the present disclosure.
- such compositions can be prepared as injectables, either as liquid solutions or suspensions; solid forms suitable for use in preparing solutions or suspensions upon the addition of a liquid prior to injection can also be prepared; and the preparations can also be emulsified.
- Sterile injectable solutions are prepared by incorporating the active compounds in the required amount in the appropriate solvent with various of the other ingredients enumerated above, as required, followed by filtered sterilization.
- dispersions are prepared by incorporating the various sterilized active ingredients into a sterile vehicle which contains the basic dispersion medium and the required other ingredients from those enumerated above.
- methods of preparation include vacuum-drying and freeze-drying techniques which yield a powder of the active ingredient plus any additional desired ingredient from a previously sterile-filtered solution thereof.
- solutions Upon formulation, solutions will be systemically administered in a manner compatible with the dosage formulation and in such amount as is therapeutically effective based on the criteria described herein.
- the formulations are easily administered in a variety of dosage forms, such as the type of injectable solutions described above, but drug release capsules and the like can also be employed
- the appropriate quantity of a pharmaceutical composition to be administered, the number of treatments, and unit dose will vary according to the CNS uptake characteristics of the IDS fusion antibody (e.g., HIR Ab-IDS ) as described herein, and according to the subject to be treated, the state of the subject and the effect desired. The person responsible for administration will, in any event, determine the appropriate dose for the individual subject.
- the IDS fusion antibody e.g., HIR Ab-IDS
- intradermal administration See U.S. Pat. Nos. 5,997,501 ; 5,848,991 ; and 5,527,288
- pulmonary administration See U.S. Pat. Nos. 6,361,760 ; 6,060,069 ; and 6,041,775
- buccal administration See U.S. Pat. Nos. 6,375,975 ; and 6,284,262
- transdermal administration See U.S. Pat. Nos. 6,348,210 ; and 6,322,808
- transmucosal administration See U.S. Pat.
- nasal solutions are usually aqueous solutions designed to be administered to the nasal passages in drops or sprays.
- Nasal solutions are prepared so that they are similar in many respects to nasal secretions.
- the aqueous nasal solutions usually are isotonic and slightly buffered to maintain a pH of 5.5 to 6.5.
- antimicrobial preservatives similar to those used in ophthalmic preparations and appropriate drug stabilizers, if required, may be included in the formulation.
- Various commercial nasal preparations are known and include, for example, antibiotics and antihistamines and are used for asthma prophylaxis.
- Additional formulations which are suitable for other modes of administration, include suppositories and pessaries.
- a rectal pessary or suppository may also be used.
- Suppositories are solid dosage forms of various weights and shapes, usually medicated, for insertion into the rectum or the urethra. After insertion, suppositories soften, melt or dissolve in the cavity fluids.
- traditional binders and carriers generally include, for example, polyalkylene glycols or triglycerides; such suppositories may be formed from mixtures containing the active ingredient in any suitable range, e.g., in the range of 0.5% to 10%, preferably 1%-2%.
- Oral formulations include such normally employed excipients as, for example, pharmaceutical grades of mannitol, lactose, starch, magnesium stearate, sodium saccharine, cellulose, magnesium carbonate and the like. These compositions take the form of solutions, suspensions, tablets, pills, capsules, sustained release formulations, or powders.
- oral pharmaceutical compositions will comprise an inert diluent or assimilable edible carrier, or they may be enclosed in a hard or soft shell gelatin capsule, or they may be compressed into tablets, or they may be incorporated directly with the food of the diet.
- the active compounds may be incorporated with excipients and used in the form of ingestible tablets, buccal tables, troches, capsules, elixirs, suspensions, syrups, wafers, and the like.
- Such compositions and preparations can contain at least 0.1% of active compound.
- the percentage of the compositions and preparations may, of course, be varied, and may conveniently be between about 2 to about 75% of the weight of the unit, or between about 25-60%.
- the amount of active compounds in such therapeutically useful compositions is such that a suitable dosage will be obtained.
- the tablets, troches, pills, capsules and the like may also contain the following: a binder, such as gum tragacanth, acacia, cornstarch, or gelatin; excipients, such as dicalcium phosphate; a disintegrating agent, such as corn starch, potato starch, alginic acid and the like; a lubricant, such as magnesium stearate; and a sweetening agent, such as sucrose, lactose or saccharin may be added or a flavoring agent, such as peppermint, oil of wintergreen, or cherry flavoring.
- a binder such as gum tragacanth, acacia, cornstarch, or gelatin
- excipients such as dicalcium phosphate
- a disintegrating agent such as corn starch, potato starch, alginic acid and the like
- a lubricant such as magnesium stearate
- a sweetening agent such as sucrose, lactose or saccharin may be added or
- tablets, pills, or capsules may be coated with shellac, sugar or both.
- a syrup of elixir may contain the active compounds sucrose as a sweetening agent, methylene and propyl parabens as preservatives, a dye and flavoring, such as cherry or orange flavor.
- an oral pharmaceutical composition may be enterically coated to protect the active ingredients from the environment of the stomach; enteric coating methods and formulations are well-known in the art.
- Described herein are methods for delivering an effective dose of IDS to the CNS across the BBB by systemically administering a therapeutically effective amount of a HIR Ab-IDS fusion antibody, as described herein.
- Suitable systemic doses for delivery of a IDS fusion antibody e.g., HIR MAb
- a IDS fusion antibody e.g., HIR MAb
- Systemic administration of of a IDS fusion antibody (e.g., HIR MAb) to a subject suffering from an IDS deficiency is an effective approach to the non-invasive delivery of IDS to the CNS.
- the amount of a IDS fusion antibody (e.g., HIR MAb) fusion antibody that is a therapeutically effective systemic dose depends, in part, on the CNS uptake characteristics of the of a IDS fusion antibody (e.g., HIR MAb) to be administered, as described herein., e.g., the percentage of the systemically administered dose to be taken up in the
- 0.3% i.e., about 0.32%
- 0.4%, 0.48%, 0.6%, 0.74%, 0.8%, 0.9%, 1.05, 1.1, 1.2, 1.3%, 1.5%, 2%, 2.5%, 5%, or any % from about 0.3% to about 12%) of the systemically administered of the IDS fusion antibody (e.g., HIR MAb) is delivered to the brain as a result of its uptake from peripheral blood across the BBB.
- At least 0.5%, (i.e., about 0.32%, 0.4%, 0.48%, 0.6%, 0.74%, 0.8%, 0.9%, 1.05, 1.1, 1.2, 1.3%, 1.5%, 2%, 2.5%, 5%, or any % from about 0.3% to about 12%) of the systemically administered dose of a IDS fusion antibody (e.g., HIR MAb) is delivered to the brain within two hours or less, i.e., 1.8, 1.7, 1.5, 1.4, 1.3, 1.2, 1.1, 0.9, 0.8, 0.6, 0.5 or any other period from about 0.5 to about two hours after systemic administration.
- a IDS fusion antibody e.g., HIR MAb
- the invention provides methods of administering a therapeutically effective amount of a IDS fusion antibody (e.g., HIR MAb) systemically, such that the amount of the IDS fusion antibody (e.g., HIR MAb) to cross the BBB provides at least 0.125 units of IDS activity/mg protein in the subject's brain, e.g., 0.14, 0.15, 0.16, 0.17, 0.18, 0.19, 0.2, 0.21, 0.22, 0.23, 0.24, 0.25, 0.3, 0.4, 0.5, 0.75, 1.0, 1.5, 2, or any other value from 0.125 to 2.5 of units of IDS activity/mg protein in the subject's brain.
- a IDS fusion antibody e.g., HIR MAb
- the total number of units of IDS activity delivered to a subject's brain is at least, 12,500 units, e.g., at least 12,500, 25,000, 30,000, 35,000, 40,000, 45,000, 50,000, 60,000, 70,000, 80,000, 90,000, 110,000, 120,000, 130,000, 140,000, 150,000, 160,000, 170,000, 180,000, 190,000, 200,000, 210,000, 220,000, 230,000, 250,000 or any other total number of IDS units from about 12,500 to 250,000 units of IDS activity.
- a therapeutically effective systemic dose comprises at least 5 x 10 5 , 1 x 10 6 , 2 x 10 6 , 3 ⁇ 10 6 , 4, 10 6 , 5 ⁇ 10 6 , 6 ⁇ 10 6 , 7 ⁇ 10 6 , 8 ⁇ 10 6 , 9 ⁇ 10 6 , 1 ⁇ 10 7 , 1.1 ⁇ 10 7 , 1.2 ⁇ 10 7 , 1.5 ⁇ 10 7 , 1.6 ⁇ 10 7 , 1.7 x 10 7 , 1.8 ⁇ 10 7 , 1.9 ⁇ 10 7 , 2 ⁇ 10 7 , 2.1 ⁇ 10 7 , 3 ⁇ 10 7 , or any other systemic dose from about 5 ⁇ 10 5 to 3 ⁇ 10 7 units of IDS activity.
- a therapeutically effective systemic dose is at least about 20,000 units of IDS activity/kg body weight, at least about 22,000, 24,000, 25,000, 30,000, 40,000, 50,000, 60,000, 70,000, 80,000, 90,000, 100,000, 125,000, 150,000, 200,000 or any other number of IDS units from about 20,000 to 200,000 units of IDS activity/kg of body weight.
- At least about 10,000, 15,000, 25,000, 30,000, 35,000, 40,000, 45,000, 50,000, 60,000, 70,000, 80,000, 90,000, 110,000, 120,000, 130,000, 140,000, 150,000, 160,000, 170,000, 180,000, 190,000, 200,000, 210,000, 220,000, 230,000, 250,000 units of iduronate-2-sulfatase activity is delivered to the brain, normalized per 50 kg body weight. In some embodiments, at least about 25,000 000 units of iduronate-2-sulfatase activity is delivered to the brain, normalized per 50 kg body weight.
- the mass amount of a therapeutically effective systemic dose of a IDS fusion antibody will depend, in part, on its IDS specific activity.
- the IDS specific activity of a IDS fusion antibody is at least 10,000 U/mg of protein, at least about 11,000, 12,000, 13,000, 14,000, 20,000, 21,000, 22,000, 23,000, 24,000, 25,000, 26,000, 27,000, 28,000, 30,000, 32,000, 34,000, 35,000, 36,000, 37,000, 40,000, 45,000, 50,000, or any other specific activity value from about 10,000 units/mg to about 50,000 units/mg.
- a systemic dose of a IDS fusion antibody can be at least 2 mg, e.g., 5, 10, 15, 20, 25, 30, 35, 40, 45, 50, 55, 60, 65, 70, 75, 100, or any other value from about 2 mg to about 100 mg of a IDS fusion antibody (e.g., HIR MAb).
- systemic administration includes any method of administration that is not direct administration into the CNS, i.e., that does not involve physical penetration or disruption of the BBB.
- Systemic administration includes, but is not limited to, intravenous , intra-arterial intramuscular, subcutaneous, intraperitoneal, intranasal, transbuccal, transdermal, rectal, transalveolar (inhalation), or oral administration. Any suitable IDS fusion antibody (e.g., HIR MAb), as described herein, may be used.
- An IDS deficiency as referred to herein includes, one or more conditions known as Hunter's syndrome, Hunter's disease, and mucopolysaccharidosis type II.
- the IDS deficiency is characterized by the buildup of heparan sulfate and dermatan sulfate that occurs in the body (the heart, liver, brain etc.).
- compositions of the invention may be administered as part of a combination therapy.
- the combination therapy involves the administration of a composition of the invention in combination with another therapy for treatment or relief of symptoms typically found in a patient suffering from an IDS deficiency.
- any combination of the composition of the invention and the additional method or composition may be used.
- the two may be administered simultaneously, consecutively, in overlapping durations, in similar, the same, or different frequencies, etc.
- a composition will be used that contains a composition of the invention in combination with one or more other CNS disorder treatment agents.
- the composition e.g., an HIR Ab-IDS fusion antibody is co-administered to the patient with another medication, either within the same formulation or as a separate composition.
- the HIR Ab-IDS fusion antibody may be formulated with another fusion protein that is also designed to deliver across the human blood-brain barrier a recombinant protein other than IDS.
- the fusion HIR Ab-IDS fusion antibody may be formulated in combination with other large or small molecules. Table 1.
- GUSB enzyme activity in COS cells following transfection Experiment Treatment Medium GUSB activity (nmol/hour/mL)
- IDS FWD phosphate-CCTCCGAAACGCAGGCCAACTCG (SEQ ID NO. 11)
- IDS REV phosphate-TCAAGGCATCAACAACTGGAAAAGATC (SEQ ID NO. 12)
- IDS FWD2 phosphate-CCACAGATGCTCTGAACGTTCTTC (SEQ ID NO. 19)
- MPS-VII The lysosomal enzyme mutated in MPS-VII, also called Sly syndrome, is -glucuronidase (GUSB).
- GUSB -glucuronidase
- MPS-VII results in accumulation of glycosoaminoglycans in the brain.
- Enzyme replacement therapy (ERT) of MPS-VII would not likely be effective for treatment of the brain because the GUSB enzyme does not cross the BBB.
- ERT enzyme replacement therapy
- RT reverse transcription
- ODNs custom oligodexoynucleotides
- This substrate is hydolyzed to 4-methylumbelliferone (4-MU) by GUSB, and the 4-MU is detected fluorometrically with a fluorometer using an emission wavelength of 450 nm and an excitation wavelength of 365 nm.
- a new pCD-HC-GUSB plasmid expression plasmid was engineered, which expresses the fusion protein wherein the carboxyl terminus of the heavy chain (HC) of the HIR Ab is fused to the amino terminus of human GUSB, minus the 22 amino acid GUSB signal peptide, and minus the 18 amino acid carboxyl terminal GUSB propeptide.
- the GUSB cDNA was cloned by PCR using the pCD-GUSB as template.
- the forward PCR primer introduces "CA” nucleotides to maintain the open reading frame and to introduce a Ser-Ser linker between the carboxyl terminus of the CH3 region of the HIR Ab HC and the amino terminus of the GUSB minus the 22 amino acid signal peptide of the enzyme.
- the GUSB reverse PCR primer introduces a stop codon, "TGA,” immediately after the terminal Thr of the mature human GUSB protein.
- DNA sequencing of the expression cassette of the pCD-HC-GUSB encompassed 4,321 nucleotides (nt), including a 714 nt cytomegalovirus (CMV) promoter, a 9 nt Kozak site (GCCGCCACC), a 3,228 nt HC-GUSB fusion protein open reading frame, and a 370 nt bovine growth hormone (BGH) transcription termination sequence.
- nt 4,321 nucleotides
- CMV cytomegalovirus
- GCCGCCACC 9 nt Kozak site
- BGH bovine growth hormone
- the plasmid encoded for a 1,075 amino acid protein comprised of a 19 amino acid IgG signal peptide, the 443 amino acid HIRMAb HC, a 2 amino acid linker (Ser-Ser), and the 611 amino acid human GUSB minus the enzyme signal peptide and carboxyl terminal propeptide.
- the GUSB sequence was 100% identical to Leu 23 -Thf 633 of human GUSB (NP_000172).
- the predicted molecular weight of the heavy chain fusion protein, minus glycosylation, is 119,306 Da, with a predicted isoelectric point (pI) of 7.83.
- COS cells were plated in 6-well cluster dishes, and were dual transfected with pCD-LC and pCD-HC-GUSB, where pCD-LC is the expression plasmid encoding the light chain (LC) of the chimeric HIR Ab. Transfection was performed using Lipofectamine 2000, with a ratio of 1:2.5, ug DNA:uL Lipofectamine 2000, and conditioned serum free medium was collected at 3 and 7 days. However, there was no specific increase in GUSB enzyme activity following dual transfection of COS cells with the pCD-HC-GUSB and pCD-LC expression plasmids (Table 1, Experiment B).
- the low GUSB activity in the medium could be attributed to the low secretion of the HIRMAb-GUSB fusion protein, as the medium IgG was only 23 ⁇ 2 ng/mL, as determined by a human IgG-specific ELISA. Therefore, COS cell transfection was scaled up to 10xT500 plates, and the HIRMAb-GUSB fusion protein was purified by protein A affinity chromatography. IgG Western blotting demonstrated the expected increase in size of the fusion protein heavy chain. However, the GUSB enzyme activity of the HIRMAb-GUSB fusion protein was low at 6.1 ⁇ 0.1 nmol/hr/ug protein.
- CHO cells permanently transfected with the HIR ECD were grown in serum free media (SFM), and the HIR ECD was purified with a wheat germ agglutinin affinity column.
- SFM serum free media
- the HIR ECD was plated on 96-well dishes and the binding of the HIR Ab, and the HIR Ab-GUSB fusion protein to the HIR ECD was detected with a biotinylated goat anti-human IgG (H+L) secondary antibody, followed by avidin and biotinylated peroxidase.
- the concentration of protein that gave 50% maximal binding, ED 50 was determined with a non-linear regression analysis.
- the HIR receptor assay showed there was no decrease in affinity for the HIR following fusion of the 611 amino acid GUSB to the carboxyl terminus of the HIRMAb heavy chain.
- the ED50 of the HIR Ab binding to the HIR ECD was 0.77 ⁇ 0.10 nM and the ED50 of binding of the HIR Ab-GUSB fusion protein was 0.81 ⁇ 0.04 nM.
- the pCD-GUSB-HC plasmid expresses the fusion protein wherein the amino terminus of the heavy chain (HC) of the HIRMAb, minus its 19 amino acid signal peptide, is fused to the carboxyl terminus of human GUSB, including the 22 amino acid GUSB signal peptide, but minus the 18 amino acid carboxyl terminal GUSB propeptide.
- the pCD-GUSB vector was used as template for PCR amplification of the GUSB cDNA expressing a GUSB protein that contained the 22 amino acid GUSB signal peptide, but lacking the 18 amino acid propeptide at the GUSB carboxyl terminus.
- the GUSB 18 amino acid carboxyl terminal propeptide in pCD-GUSB was deleted by site-directed mutagenesis (SDM). The latter created an AfeI site on the 3'-flanking region of the Thr 633 residue of GUSB, and it was designated pCD-GUSB-AfeI.
- SDM site-directed mutagenesis
- the carboxyl terminal propeptide was then deleted with AfeI and HindIII (located on the 3'-non coding region of GUSB).
- the PCR generated HIRMAb HC cDNA was inserted at the AfeI-HindIII sites of pCD-GUSB-AfeI to form the pCD-GUSB-HC.
- a Ser-Ser linker between the carboxyl terminus of GUSB and amino terminus of the HIRMAb HC was introduced within the AfeI site by the PCR primer used for the cloning of the HIRMAb HC cDNA.
- DNA sequencing of the pCD-GUSB-HC expression cassette showed the plasmid expressed 1,078 amino acid protein, comprised of a 22 amino acid GUSB signal peptide, the 611 amino acid GUSB, a 2 amino acid linker (Ser-Ser), and the 443 amino acid HIRMAb HC.
- the GUSB sequence was 100% identical to Met 1 -Thr 633 of human GUSB (NP_000172).
- SDSPAGE demonstrated the expected increase in size of the fusion protein heavy chain.
- the GUSB enzyme activity of the purified GUSB-HIRMAb fusion protein was high at 226 ⁇ 8 nmol/hr/ug protein, which is 37-fold higher than the specific GUSB enzyme activity of the HIRMAb-GUSB fusion protein.
- the HIR receptor assay showed there was a marked decrease in affinity for the HIR following fusion of the GUSB to the amino terminus of the HIRMAb heavy chain, which resulted in a 95% reduction in receptor binding affinity.
- the ED50 of the HIR Ab binding to the HIR ECD was 0.25 ⁇ 0.03 nM and the ED50 of binding of the HIR Ab-GUSB fusion protein was 4.8 ⁇ 0.4 nM.
- fusion of the GUSB to the amino terminus of the HIR Ab HC resulted in retention of GUSB enzyme activity of the fusion protein, but caused a 95% reduction in binding of the GUSB-HIR Ab fusion protein to the HIR.
- fusion of the GUSB to the carboxyl terminus of the HIR Ab HC resulted in no loss in affinity of binding of the HIR Ab-GUSB fusion protein to the HIR.
- the GUSB enzyme activity of this fusion protein was decreased by >95%.
- MPS-II The lysosomal enzyme mutated in MPS-II, also called Hunter's syndrome, is iduronate 2-sulfatase (IDS).
- IDDS iduronate 2-sulfatase
- MPS-II results in accumulation of glycosoaminoglycans in the brain.
- Enzyme replacement therapy of MPS-II would likely not be effective for treatment of the brain because the IDS enzyme does not cross the BBB.
- IDS was fused to the HIR Ab in order to develop a bifunctional molecule capable of both crossing the BBB and exhibiting enzymatic activity.
- IDS is a member of a family of sulfatases, wherein the activity of the enzyme is activated following the conversion of Cys-59 to a formylglycine residue by a sulfatase modifying factor in the endoplasmic reticulum [ Zito et al, Sulphatase activities are regulated by the interaction of sulphatase-modifying factor 1 with SLTMF2.
- the enzyme Without this conversion of the internal cysteine into a formylglycine residue, the enzyme has no activity. If the IDS was fused to the carboxyl terminus of the HC of the HIR Ab, e.g. in an effort to retain high affinity binding of the fusion protein to the HIR, then the IgG heavy chain would fold into the 3-dimensional structure following translation within the host cell, followed by folding of the IDS part of the fusion protein.
- the human IDS cDNA encoding Ser 26 -Pro 550 , minus the 25 amino acid signal peptide (Genbank NP_000193) was produced by reverse transcription and PCR, starting with human liver polyA+ RNA (Clontech). Human liver cDNA was prepared using the SuperScript first-strand synthesis kit (Invitrogen, San Diego, CA) and oligodeoxythymidine priming.
- the IDS cDNA was cloned using 2 ⁇ l liver cDNA reverse transcription reaction, 0.2 ⁇ M IDS forward and reverse ODN primers (Table 2), 0.2 mM deoxynucleotidetriphosphates and 2.5 U PfuUltra DNA polymerase (Stratagene, San Diego, CA) in a 50 ⁇ l Pfu buffer (Stratagene).
- the amplification was performed in a Mastercycler temperature cycler (Eppendorf, Hamburg, Germany) with an initial denaturing step of 95°C for 2 min followed by 30 cycles of denaturing at 95°C for 30 sec, annealing at 55°C for 30 sec and amplification at 72°C for 1 min.
- PCR products were resolved in 1% agarose gel electrophoresis, and the expected major single band of ⁇ 1.6 kb corresponding to the human IDS cDNA was isolated ( Fig. 8A ).
- the cloned human IDS was inserted into the pCD-HIRMAb HC eukaryotic expression plasmid at the HpaI site, and this expression plasmid was designated pCD-HIRMAb-IDS, as outlined in Fig. 8B ; the pCD-HIRMAb-HC expression plasmid encodes the heavy chain (HC) of the chimeric HIRMAb.
- the entire expression cassette of the plasmid was confirmed by bi-directional DNA sequencing.
- the IDS forward PCR primer (SEQ ID NO:11) was a 23-mer coding for the 7 amino acids at the beginning of the mature IDS protein. This primer introduces "CC" nucleotides to maintain the open reading frame and to introduce a Ser-Ser linker between the carboxyl terminus of the CH3 region of the HIRMAb HC and the amino terminus of the IDS minus the 25 amino acid signal peptide of the enzyme.
- the IDS reverse PCR primer (SEQ ID NO:12) was a 27-mer complementary to the end of the IDS cDNA including the stop codon, "TGA,” immediately after the terminal Pro of the mature human IDS protein. The fusion of the IDS monomer to the carboxyl terminus of each HC is depicted in Fig. 6 . The entire expression cassette of the plasmid was confirmed by sequencing both strands.
- DNA sequencing of the expression cassette of the pCD-HIRMAb-IDS plasmid encompassed 4,063 nucleotides (nt), including a 714 nt cytomegalovirus promoter, a 9 nt full Kozak site (GCCGCCACC), a 2,970 nt HIRMAb HC-IDS fusion protein open reading frame, and a 370 nt bovine growth hormone polyA sequence.
- nt 4,063 nucleotides
- the plasmid encoded for a 989 amino acid protein (SEQ ID NO:10), comprised of a 19 amino acid IgG signal peptide, the 443 amino acid HIRMAb HC, a 2 amino acid linker (Ser-Ser), and the 525 amino acid human IDS minus the enzyme signal peptide.
- the predicted molecular weight of the heavy chain fusion protein, minus glycosylation, is 108,029 Da, with a predicted isoelectric point (pI) of 6.03..
- COS cells were plated in 6-well cluster dishes, and were dually transfected with the pCD-HC-IDS, and pCD-LC, where pCD-LC is the expression plasmid encoding the light chain (LC) of the chimeric HIRMAb, which is also used by the HIR Ab-IDS fusion protein. Expression of the fusion protein was screened with an ELISA specific for human IgG. For production of larger amounts of fusion protein, COS cells were transfected in 10 x T500 flasks. The 3 day and 7 day medium was pooled, and the 2 L of serum free conditioned medium was concentrated to 400 mL with tangential flow filtration (Millipore) followed by purification with protein A affinity chromatography.
- LC light chain
- the purity of protein A purified fusion protein produced by COS cells was evaluated with 12% sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDSPAGE) with 5% ⁇ -mercaptoethanol, and shown to have a homogeneity comparable to the purified HIR Ab ( Figure 9 ). Immunoreactivity was tested with a goat antibody to human IDS, or a primary goat antiserum against human IgG heavy and light chains.
- SDSPAGE sodium dodecyl sulfate polyacrylamide gel electrophoresis
- the anti-human IgG antibody reacts with a 135 kDa HC for the fusion protein, and a 50 kDa HC for the chimeric HIR Ab, and the difference in size, 85 kDa, is due to the fusion of IDS ( Fig. 10A ).
- the anti-human IgG antibody reacts equally with the light chain of either the HIR Ab-IDS fusion protein or the HIR Ab, since both proteins are comprised of the same light chain.
- the anti-IDS antibody reacts with the 135 kDa HC of the fusion protein, but not with the HC of the chimeric HIR Ab ( Fig. 10B ).
- the affinity of the fusion protein for the HIR extracellular domain (ECD) was determined with an ELISA.
- CHO cells permanently transfected with the HIR ECD were grown in serum free media (SFM), and the HIR ECD was purified with a wheat germ agglutinin affinity column, as previously described in Coloma et al. (2000) Pharm Res, 17:266-274 .
- the HIR ECD was plated on Nunc-Maxisorb 96 well dishes and the binding of the HIR Ab, or the HIR Ab-IDS fusion protein, to the HIR ECD was detected with a biotinylated goat anti-human IgG (H+L) secondary antibody, followed by avidin and biotinylated peroxidase (Vector Labs, Burlingame, CA).
- the concentration of either HIR Ab or HIR Ab-IDS fusion protein that gave 50% maximal binding was determined with a non-linear regression analysis. As shown in Fig. 11 there was comparable binding of either the chimeric HIR Ab or the HIR Ab-IDS fusion protein for the HIR ECD with ED50 of 0.32 ⁇ 0.05 nM and 0.40 ⁇ 0.05 nM, respectively.
- the IDS enzyme activity was determined with a fluorometric assay using 4-methylumbelliferyl a-L-iduronide-2-sulphate (4-MUS), which was purchased from Moscerdam Substrates (Rotterdam, The Netherlands).
- This substrate is hydrolyzed by IDS to 4-methylumbelliferyl a-L-iduronide (MUBI), and the MUBI is hydrolyzed by iduronidase (IDUA, Aldurazyme, Genzyme, Boston, MA) to 4-methylumbelliferone (4-MU), which is detected fluorometrically with a Farrand filter fluorometer using an emission wavelength of 450 nm and an excitation wavelength of 365 nm.
- 4-MUS 4-methylumbelliferyl a-L-iduronide-2-sulphate
- a standard curve was constructed with known amounts of 4-MU (Sigma-Aldrich, St. Louis, MO).
- One unit 1 nmol/hr.
- the 2-step enzymatic fluorometric assay is outlined in Fig. 12A .
- the fluorometric units were proportional to the mass of purified HIRMAb-IDS fusion protein and the enzymatic activity of the fusion protein was 51 ⁇ 7 nmol/hr/ug protein ( Fig. 12B ), which is comparable to the IDS enzyme activity reported for human recombinant Idursulfase ( G. Zareba, Idursulfase in Hunter syndrome treatment. Drugs Today (Barc) 43 (2007) 759-767 ).
- Example 5 HIR Ab-IDS fusion protein uptake and biological activity in MPS Type II fibroblasts
- Type II MPS Hunter fibroblasts (GM000298) and healthy human fibroblasts (GM000497) were obtained from the Coriell Institute for Medical Research (Camden, NJ), and grown in 6-well cluster dishes to confluency. The medium was aspirated, wells washed with phosphate buffered saline (PBS), and incubated with 1 mL of Dulbecco's modified Eagle medium without serum, along with a range of concentrations of the HIRMAb-IDS fusion protein, for 2 hr at 37C.
- PBS phosphate buffered saline
- the HIRMAb-IDS fusion protein was taken up by MPS Type II fibroblasts ( Fig. 13 ).
- the basal IDS activity in these cells without treatment is very low, ⁇ 10 nmol/hr/mg p .
- the intracellular IDS enzyme activity increases in proportion to the concentration of medium HIRMAb-IDS ( Fig. 13 ).
- the normal IDS enzymatic activity in healthy human fibroblasts is shown by the horizontal bar in Fig. 13 .
- HIRMAb-IDS fusion protein on cell glycosoaminoglycan (GAG) accumulation was assessed with a 35 S incorporation assay.
- Type II MPS or healthy human fibroblasts were plated in 6-well cluster dishes at 250,000 cells/well and grown for 4 days in DMEM with 10% fetal bovine serum.
- the medium was discarded, the wells were washed with PBS, and 1 mL/well of low sulfate F12 medium with 10% dialyzed fetal bovine serum was added, along with 5 mM CaCl2, the HIRMAb-IDS fusion protein (0.3 ug/mL), and 10 uCi/mL of 35 S-sodium sulfate (Perkin Elmer, Boston, MA).
- the medium was aspirated, the wells were washed with cold PBS (1 mL, 5 washes), and the cells were lysed with 0.4 mL/well of 1 N NaOH.
- the lysate was heated 60°C 60 min to solubilize protein, an aliquot was removed for BCA protein assay, and the sample was counted for radioactivity with a Perkin Elmer Tri-Carb 2100 liquid scintillation counter. The data were expressed as 35 S counts per minute (CPM) per ug protein.
- Treatment with the HIRMAb-IDS fusion protein reduces GAG accumulation in Hunter fibroblasts by 84% as compared to healthy fibroblasts (p ⁇ 0.0005) ( Fig.14 ).
- the prevention of GAG accumulation in Hunter fibroblasts indicates the HIR Ab-IDS fusion antibody was directed to the lysosomal compartment of the cell, where GAG accumulates.
- the HIRAb-IDS fusion protein is a hetero-tetrameric protein comprised of 2 heavy chains (HC) and 2 light chains (LC) ( Figure 6 ), wherein the separate HC and LC proteins are produced from separate HC and LC genes. Therefore, in order to insure high production of the entire fusion protein by a permanently transfected host cell, it is necessary to achieve equally high expression of both the HC and the LC within the host cell. In addition, the host cell must be permanently transfected with a marker gene that allows for selective amplification of the host genome around the site of insertion of the transgene.
- a drug such as methotrexate (MTX)
- MTX methotrexate
- DHFR dihydrofolate reductase
- the expression cassettes encoding these 3 genes were all placed on a single strand of DNA, called a tandem vector, which is outlined in Figure 15 .
- the HC fusion gene and the LC gene are 5'-flanked by a cytomegalovirus (CMV)-derived promoter and 5'-flanked by the polyA+ sequence from the bovine growth hormone (BGH) gene.
- CMV cytomegalovirus
- BGH bovine growth hormone
- the DHFR gene was 5'-flanked by the SV40 promoter and 3'-flanked by the polyA sequence from the hepatitis B virus (HBV) genome.
- the TV-HIRMAb-IDS also included the expression cassette encoding neo, the neomycin resistance gene, to enable selection with G418 ( Figure 15 )
- the engineering of the TV was validated by (a) agarose gel electrophoresis, (b) IgG expression in COS cells, and (c) by bi-directional DNA sequencing.
- nucleotide (nt) sequence encoding the open reading frame of the LC, the HC fusion protein, and the DHFR is given in SEQ ID NO:13, SEQ ID NO:14, and SEQ ID NO:15, respectively ( Figures 16 , 17 , 18 respectively).
- amino acid (AA) sequences encoded by the HC fusion gene, the LC gene, and the DHFR gene on the tandem vector are given in SEQ ID NO:10, SEQ ID NO:16, and SEQ ID NO:17, respectively ( Figures 5 , 19 , and 20 , respectively).
- CHO cells Chinese hamster ovary (CHO) cells were grown in serum free HyQ SFM4CHO utility medium (HyClone), containing 1 ⁇ HT supplement (hypoxanthine and thymidine).
- CHO cells (5 ⁇ 10 6 viable cells) were electroporated with 5 ⁇ g PvuI-linearized TV-HIRMAb-IDS plasmid DNA. The cell-DNA suspension was then incubated for 10 min on ice. Cells were electroporated with BioRad pre-set protocol for CHO cells, i.e. square wave with pulse of 15 msec and 160 volts. After electroporation, cells were incubated for 10 min on ice. The cell suspension was transferred to 50 ml culture medium and plated at 125 ⁇ l per well in 4 ⁇ 96-well plates (10,000 cells per well). A total of 10 electroporations and 4,000 wells were performed per study.
- the CHO cells were placed in the incubator at 37 C and 8% CO2. Owing to the presence of the neo gene in the TV, transfected cell lines were initially selected with G418.
- the TV-HIRMAb-IDS also contains the gene for DHFR ( Figure 15 ), so the transfected cells were also selected with 20 nM methotrexate (MTX) and HT deficient medium.
- MTX methotrexate
- HT deficient medium Once visible colonies were detected at about 21 days after EP, the conditioned medium was sampled for human IgG by ELISA. Wells with high human IgG signals in the ELISA were transferred from the 96-well plate to a 24-well plate with 1mL of HyQ SFM4CHO-Utility.
- the 24-well plates were returned to the incubator at 37 C and 8% CO2.
- the following week IgG ELISA was performed on the clones in the 24-well plates. This was repeated through the 6-well plates to T75 flasks and finally to 60 mL and 125 mL square plastic bottles on an orbital shaker. At this stage, the final MTX concentration was 80 nM, and the medium IgG concentration, which was a measure of HIRMAb-IDS fusion protein in the medium is >10 mg/L at a cell density of 10 6 /mL.
- Clones selected for dilutional cloning were removed from the orbital shaker in the incubator and transferred to the sterile hood.
- the cells were diluted to 500 mL in F-12K medium with 5% dialyzed fetal bovine serum (d-FBS) and Penicillin/Streptomycin, and the final dilution is 8 cells per mL, so that 4,000 wells in 40 ⁇ 96-well plates can be plated at a cell density of 1 cell per well (CPW).
- d-FBS dialyzed fetal bovine serum
- Penicillin/Streptomycin Penicillin/Streptomycin
- the plates were returned to the incubator at 37 C and 8% CO2. The cells diluted to 1 cell/well cannot survive without serum.
- DC plates were removed from the incubator and transferred to the sterile hood where 125 ⁇ l of F-12K medium with 5% dialyzed fetal bovine serum (d-FBS) was added to each well.
- This selection media now contained 5% d-FBS, 30 nM MTX and 0.25 mg/mL Geneticin.
- aliquots from each of the 4,000 wells were removed for human IgG ELISA, using robotics equipment.
- DC plates were removed from the incubator and transferred to the sterile hood, where 100 ⁇ l of media was removed per well of the 96-well plate and transferred into a new, sterile sample 96-well plate using an 8-channel pipettor or the precision pipettor system.
- the highest producing 24-well plates from the 1 CPW DC were transferred to the sterile hood and gradually subcloned through 6-well dishes, T75 flasks, and 125 mL square plastic bottles on an orbital shaker. During this process the serum was reduced to zero, at the final stage of centrifugation of the cells and resuspension in SFM.
- the HIR Ab-IDS fusion protein was secreted to the medium by the stably transfected CHO cells in high amounts at medium concentrations of 10-20 mg/L at a cell density of 1-2 million cells/mL.
- the CHO-derived HIRMAb was purified by protein A affinity chromatography, and the patterns of migration of the fusion protein on SDS-PAGE and on IgG or IDS Western blotting was identical to that shown in Figures 9 and 10 for the HIR Ab-IDS fusion protein produced by transiently transfected COS cells.
- the CHO-derived fusion protein migrated as a single peak, without aggregation, on size exclusion HPLC.
- the CHO-derived fusion protein retained high affinity binding to the HIR.
- the CHO-derived fusion protein was shown to have a high affinity for binding to the HIR, with an EC50 of 0.36 ⁇ 0.04 nM, which was not significantly different from the EC50, 0.41 ⁇ 0.09 nM, for the HIR Ab without the fused IDS.
- the CHO-derived HIR Ab-IDS fusion protein retained high IDS enzyme activity despite fusion of the IDS to the HIR Ab.
- the IDS enzyme specific activity of the CHO-derived HIR Ab-IDS fusion protein is 115 ⁇ 7 nmol/ug protein/hour, which is even higher than the IDS specific activity of the COS-derived fusion protein ( Figure 12B ).
- the high IDS enzyme activity of the CHO-derived HIR Ab-IDS fusion protein is surprising, because IDS is a member of a family of sulfatases that requires a specific post-translational modification for expression of IDS enzyme activity.
- the activity of the IDS enzyme is activated following the conversion of Cys-59 to a formylglycine residue by a sulfatase modifying factor type 1 (SLTMF1), which is also called the formylglycine generating enzyme (FGE).
- STMF1 sulfatase modifying factor type 1
- FGE formylglycine generating enzyme
- the first 8 amino acids of IDS following the 25 amino acid signal peptide constitute a propeptide ( Flomen et al, Determination of the organization of coding sequences within the iduronate sulphate sulphatase (IDS) gene, Hum. Mol. Genet. 2, 5-10,1993 ), which may be subject to cleavage by endoproteases. Such cleavage could result in the separation of the IDS from the HIR Ab, in which case the IDS could not be carried across the BBB by the HIR Ab Trojan horse. In this event, the IDS cDNA would be re-amplified by PCR using the new forward ODN listed in Table 2 (SEQ ID NO:19).
- IDS FWD2 ODN PCR with the IDS FWD2 ODN and IDS REV ODN listed in Table 2 will amplify an IDS cDNA that encodes for the IDS enzyme minus the 25 amino acid signal peptide, from Met-1 to Gly-25, and minus the 8 amino acid propeptide, from Ser-26 to Thr-33, and beginning with Thr-34 and ending in Pro-550 of the human IDS sequence (NP_000193).
- the IDS FWD2 ODN has 'CC' on the 5'-end to maintain the open reading frame with the carboxyl terminus of the CH3 region of the HC of the HIR Ab, and the Ser-Ser linker placed between the carboxyl terminus of the HIR Ab HC and the amino terminus of the IDS.
- the mature human IDS is fused to the carboxyl terminus of the HC of the HIR Ab with a 2-amino acid linker, Ser-Ser (underlined in Figure 5 ). Any number of variations of linkers are used as substitutions for the Ser-Ser linker.
- the 2-amino acid linker may be retained, but the amino acid sequence is changed to alternative amino acids, such as Gly-Gly, or Ser-Gly, or Ala-Ser, or any number of combinations of the 20 natural amino acids. Or, the linker is reduced to a single amino acid, or zero amino acids. In the case of a zero amino acid linker, the amino terminus of the IDS is fused directly to the carboxyl terminus of the HC of the HIR Ab.
- the length of the linker is expanded to 3,4,5,6,7,8,9,10,11,12,13,14,15 amino acids.
- linkers are well known in the art, as there are multiple publicly available programs for determining optimal amino acid linkers in the engineering of fusion proteins.
- a frequently used linker includes various combinations of Gly and Ser in repeating sequences, such as (Gly 4 Ser) 3 , or other variations.
- Example 10 Receptor-mediated delivery of IDS to the human brain
- Mucopolysaccharidosis Type II (MPS-II), or Hunter's syndrome, is a lysosomal storage disorder caused by defects in the gene encoding the lysosomal enzyme, iduronate-2-sulfatase (IDS).
- MPS-II is treated with recombinant human IDS in enzyme replacement therapy (ERT) [ Muenzer, et al, A phase II/III clinical study of enzyme replacement therapy with idurosulfase in mucopolysaccharidosis II (Hunter syndrome). Genet. Med. 8 (2006) 465-473 ].
- IDS is made to cross the human BBB following the re-engineering of the enzyme as a fusion protein with a BBB molecular Trojan horse such as the HIR Ab ( Figure 6 ).
- the brain uptake of the HIR Ab in the Rhesus monkey is about 1% of injected dose (ID) per 100 gram brain [ Boado et al. (2007), Biotechnol Bioeng, 96(2):381-391 .].
- ID injected dose
- the size of the Rhesus monkey brain is approximately 100 grams; therefore, about 1% of the injected dose is distributed to the primate brain.
- the uptake of the fusion protein by brain is expected to be reduced, as compared to the primate, in proportion to body weight. Therefore, the expected brain uptake of the fusion protein in the human brain is about 1% of the injected dose per human brain, or about 1% of the ID per 1000 g human brain.
- One gram of brain contains about 100 mg brain protein.
- the brain uptake of the fusion protein is about 10 -2 /human brain, or about 10 -5 /gram brain, or about 10 -7 /mg brain protein. Therefore, the brain concentration of the HIR Ab-IDS fusion protein is about [(10 -7 /mg protein) ⁇ (5 ⁇ 10 7 ng of fusion protein injected)] or about 5 ng fusion protein per mg brain protein.
- the IDS activity delivered to the human brain is expected to be about 60,000 units.
- the normal IDS enzyme activity in brain is about 2.5 units/mg protein ( Tomatsu et al, Murine model of MPS IVA with missense mutation at the active site cysteine conserved among sulfatase proteins. Molec. Genet. Metab. 91, 251-258, 2007 ).
- the administration of the HIR Ab-IDS fusion protein is expected to produce a 20% replacement of the normal brain IDS enzyme activity.
- Therapeutic effects in lysosomal storage disorders are achieved with the replacement of ⁇ 5% of normal tissue enzyme activity [ Muenzer and Fisher, Advances in the treatment of mucopolysaccharidosis type I. N Engl J Med 350 (2004) 1932-1934 ]. Higher degrees of replacement of IDS enzyme activity in the human brain would be possible by increasing the dosage of the HIR Ab-IDS fusion protein
Landscapes
- Health & Medical Sciences (AREA)
- Chemical & Material Sciences (AREA)
- Organic Chemistry (AREA)
- Life Sciences & Earth Sciences (AREA)
- Immunology (AREA)
- Genetics & Genomics (AREA)
- Engineering & Computer Science (AREA)
- Medicinal Chemistry (AREA)
- General Health & Medical Sciences (AREA)
- Biochemistry (AREA)
- Molecular Biology (AREA)
- Biomedical Technology (AREA)
- Bioinformatics & Cheminformatics (AREA)
- Biophysics (AREA)
- Proteomics, Peptides & Aminoacids (AREA)
- Zoology (AREA)
- Wood Science & Technology (AREA)
- Neurology (AREA)
- Biotechnology (AREA)
- Microbiology (AREA)
- General Engineering & Computer Science (AREA)
- Endocrinology (AREA)
- Neurosurgery (AREA)
- Chemical Kinetics & Catalysis (AREA)
- Psychiatry (AREA)
- Public Health (AREA)
- Animal Behavior & Ethology (AREA)
- Pharmacology & Pharmacy (AREA)
- Nuclear Medicine, Radiotherapy & Molecular Imaging (AREA)
- General Chemical & Material Sciences (AREA)
- Veterinary Medicine (AREA)
- Hospice & Palliative Care (AREA)
- Peptides Or Proteins (AREA)
- Enzymes And Modification Thereof (AREA)
- Medicinal Preparation (AREA)
- Medicines Containing Antibodies Or Antigens For Use As Internal Diagnostic Agents (AREA)
- Micro-Organisms Or Cultivation Processes Thereof (AREA)
- Medicines That Contain Protein Lipid Enzymes And Other Medicines (AREA)
Claims (6)
- Anticorps de fusion comprenant :(a) une immunoglobuline qui traverse une barrière hémato-encéphalique (BBB) en se liant à un domaine extracellulaire d'un récepteur d'insuline humaine, l'immunoglobuline comprenant une chaîne lourde d'immunoglobuline et une chaîne légère d'immunoglobuline ; et(b) une iduronate-2-sulfatase, dans lequel la terminaison amino de l'iduronate-2-sulfatase est liée de manière covalente à la terminaison carboxy de la séquence d'acides aminés de la chaîne lourde d'immunoglobuline, en formant ainsi une protéine de fusion ;(c) un lieur entre la terminaison amino de l'iduronate-2-sulfatase et la terminaison carboxy de la séquence d'acides aminés de la chaîne lourde d'immunoglobuline ;dans lequel l'anticorps de fusion traverse la barrière hémato-encéphalique (BBB) et catalyse l'hydrolyse de groupes 2-sulfate des unités 2-sulfate de L-iduronate du sulfate de dermatane, du sulfate d'héparane ou de l'héparine,dans lequel l'anticorps de fusion comprend une modification post-traductionnelle de la cystéine en formylglycine à la position correspondant à Cys-59 de l'enzyme iduronate-2-sulfatase,dans lequel la chaîne lourde d'immunoglobuline comprend une CDR1 comprenant la séquence d'acides aminés de SEQ ID NO : 1, une CDR2 comprenant la séquence d'acides aminés de SEQ ID NO : 2, et une CDR3 comprenant la séquence d'acides aminés de SEQ ID NO : 3, et dans lequel la chaîne légère d'immunoglobuline comprend une CDR1 comprenant la séquence d'acides aminés de SEQ ID NO : 4, une CDR2 comprenant la séquence d'acides aminés de SEQ ID NO : 5, et une CDR3 comprenant la séquence d'acides aminés de SEQ ID NO : 6.
- Anticorps de fusion selon la revendication 1, dans lequel l'anticorps de fusion est modifié de manière post-traductionnelle par un facteur de modification de sulfatase de type 1 (SUMF1).
- Anticorps de fusion selon la revendication 1, dans lequel l'activité spécifique de l'iduronate-2-sulfatase de l'anticorps de fusion est d'au moins 10 000 unités/mg.
- Anticorps de fusion selon la revendication 1, dans lequel la chaîne lourde d'immunoglobuline est une chaîne lourde d'immunoglobuline d'IgG.
- Anticorps de fusion selon la revendication 1, dans lequel la chaîne légère d'immunoglobuline est une chaîne légère d'immunoglobuline de classe kappa.
- Composition pharmaceutique comprenant une quantité thérapeutiquement efficace d'un anticorps de fusion selon la revendication 1, et un excipient pharmaceutiquement acceptable.
Priority Applications (1)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| EP23183395.5A EP4273164A3 (fr) | 2009-10-09 | 2010-10-08 | Procédés et compositions pour augmenter l'activité iduronate 2-sulfatase dans le système nerveux central |
Applications Claiming Priority (4)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US25037809P | 2009-10-09 | 2009-10-09 | |
| US25604909P | 2009-10-29 | 2009-10-29 | |
| EP10822810.7A EP2485761B1 (fr) | 2009-10-09 | 2010-10-08 | Procédés et compositions destinés à augmenter l'activité iduronate 2-sulfatase dans le snc |
| PCT/US2010/052113 WO2011044542A1 (fr) | 2009-10-09 | 2010-10-08 | Procédés et compositions destinés à augmenter l'activité iduronate 2-sulfatase dans le snc |
Related Parent Applications (2)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP10822810.7A Division EP2485761B1 (fr) | 2009-10-09 | 2010-10-08 | Procédés et compositions destinés à augmenter l'activité iduronate 2-sulfatase dans le snc |
| EP10822810.7A Division-Into EP2485761B1 (fr) | 2009-10-09 | 2010-10-08 | Procédés et compositions destinés à augmenter l'activité iduronate 2-sulfatase dans le snc |
Related Child Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP23183395.5A Division EP4273164A3 (fr) | 2009-10-09 | 2010-10-08 | Procédés et compositions pour augmenter l'activité iduronate 2-sulfatase dans le système nerveux central |
Publications (3)
| Publication Number | Publication Date |
|---|---|
| EP3533467A2 EP3533467A2 (fr) | 2019-09-04 |
| EP3533467A3 EP3533467A3 (fr) | 2020-01-15 |
| EP3533467B1 true EP3533467B1 (fr) | 2023-07-26 |
Family
ID=43857180
Family Applications (3)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP19150184.0A Active EP3533467B1 (fr) | 2009-10-09 | 2010-10-08 | Procédés et compositions pour augmenter l'activité iduronate 2-sulfatase dans le système nerveux central |
| EP10822810.7A Active EP2485761B1 (fr) | 2009-10-09 | 2010-10-08 | Procédés et compositions destinés à augmenter l'activité iduronate 2-sulfatase dans le snc |
| EP23183395.5A Pending EP4273164A3 (fr) | 2009-10-09 | 2010-10-08 | Procédés et compositions pour augmenter l'activité iduronate 2-sulfatase dans le système nerveux central |
Family Applications After (2)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP10822810.7A Active EP2485761B1 (fr) | 2009-10-09 | 2010-10-08 | Procédés et compositions destinés à augmenter l'activité iduronate 2-sulfatase dans le snc |
| EP23183395.5A Pending EP4273164A3 (fr) | 2009-10-09 | 2010-10-08 | Procédés et compositions pour augmenter l'activité iduronate 2-sulfatase dans le système nerveux central |
Country Status (11)
| Country | Link |
|---|---|
| US (4) | US8834874B2 (fr) |
| EP (3) | EP3533467B1 (fr) |
| JP (5) | JP2013507131A (fr) |
| DK (1) | DK2485761T3 (fr) |
| ES (1) | ES2725200T3 (fr) |
| HR (1) | HRP20190690T1 (fr) |
| HU (1) | HUE044865T2 (fr) |
| PL (1) | PL2485761T3 (fr) |
| PT (1) | PT2485761T (fr) |
| SI (1) | SI2485761T1 (fr) |
| WO (1) | WO2011044542A1 (fr) |
Families Citing this family (47)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| EP1463512B1 (fr) | 2002-01-11 | 2014-05-28 | biOasis Technologies Inc. | Utilisation de p97 en tant que systeme d'administration d'enzymes en vue d'administrer des enzymes lysosomales therapeutiques |
| US8741260B2 (en) * | 2005-10-07 | 2014-06-03 | Armagen Technologies, Inc. | Fusion proteins for delivery of GDNF to the CNS |
| US8497246B2 (en) * | 2006-08-18 | 2013-07-30 | Armagen Technologies, Inc. | Methods for diagnosing and treating CNS disorders by trans-blood-brain barrier delivery of protein compositions |
| EP2997976A1 (fr) | 2007-07-27 | 2016-03-23 | Armagen Technologies, Inc. | Procédés et compositions pour augmenter l'activité alpha-l-iduronidase dans le système nerveux central |
| WO2010108048A2 (fr) * | 2009-03-18 | 2010-09-23 | Armagen Technologies, Inc. | Compositions et procédés pour le transport de protéines de fusion igg-récepteur leurre à travers la barrière hémato-encéphalique |
| PT2485761T (pt) * | 2009-10-09 | 2019-05-30 | Armagen Inc | Métodos e composições para aumentar a atividade da iduronato 2-sulfatase no snc |
| US20160145589A1 (en) | 2011-06-24 | 2016-05-26 | Green Cross Corporation | Composition and formulation comprising recombinant human iduronate-2-sulfatase and preparation method thereof |
| CA2840221A1 (fr) | 2011-07-05 | 2013-01-10 | Bioasis Technologies Inc. | Conjugues p97-anticorps et procedes d'utilisation |
| US8486399B2 (en) | 2011-12-02 | 2013-07-16 | Armagen Technologies, Inc. | Methods and compositions for increasing arylsulfatase A activity in the CNS |
| EP2802603A4 (fr) | 2012-01-09 | 2015-11-04 | Scripps Research Inst | Régions déterminant la complémentarité ultralongues et utilisations associées |
| JP2015509091A (ja) | 2012-01-09 | 2015-03-26 | ザ スクリプス リサーチ インスティテュート | ヒト化抗体 |
| US9603908B2 (en) | 2012-03-30 | 2017-03-28 | Shire Human Genetic Therapies, Inc. | Subcutaneous administration of iduronate-2-sulfatase |
| US20140004097A1 (en) * | 2012-06-29 | 2014-01-02 | Shire Human Genetic Therapies, Inc. | Method of producing recombinant iduronate-2-sulfatase |
| US9150841B2 (en) * | 2012-06-29 | 2015-10-06 | Shire Human Genetic Therapies, Inc. | Cells for producing recombinant iduronate-2-sulfatase |
| KR101380740B1 (ko) * | 2012-06-29 | 2014-04-11 | 쉐어 휴먼 제네텍 세러피스, 인코포레이티드 | 이듀로네이트-2-설파타제의 정제 |
| CA2880162C (fr) * | 2012-07-31 | 2023-04-04 | Bioasis Technologies, Inc. | Proteines de maladie de stockage lysosomal dephosphorylees et leurs procedes d'utilisation |
| US20150290341A1 (en) * | 2012-11-30 | 2015-10-15 | Anglachem Inc. | Targeted iduronate-2-sulfatase compounds |
| EP2943512A4 (fr) * | 2013-01-11 | 2016-06-01 | California Inst Biomedical Res | Anticorps bovins de fusion |
| CN110478481A (zh) | 2013-03-13 | 2019-11-22 | 比奥阿赛斯技术有限公司 | p97片段及其应用 |
| JP6687520B2 (ja) | 2013-07-18 | 2020-04-22 | トーラス バイオサイエンシズ リミテッド ライアビリティ カンパニー | 極めて長い相補性決定領域を有するヒト化抗体 |
| WO2015012944A1 (fr) * | 2013-07-22 | 2015-01-29 | Armagen Technologies, Inc | Procédés et compositions pour augmenter l'activité enzymatique dans le snc |
| US20150093399A1 (en) | 2013-08-28 | 2015-04-02 | Bioasis Technologies, Inc. | Cns-targeted conjugates having modified fc regions and methods of use thereof |
| WO2015098989A1 (fr) | 2013-12-25 | 2015-07-02 | Jcrファーマ株式会社 | Nouvel anticorps anti-récepteur de transferrine qui traverse la barrière hémato-encéphalique |
| US20160347821A1 (en) | 2014-02-03 | 2016-12-01 | Bioasis Technologies, Inc. | P97 fusion proteins |
| JP6605482B2 (ja) | 2014-02-19 | 2019-11-13 | バイオアシス テクノロジーズ インコーポレイテッド | P97−ids融合タンパク質 |
| JP6541236B2 (ja) * | 2014-03-06 | 2019-07-10 | ナショナル リサーチ カウンシル オブ カナダ | インスリン様成長因子1受容体特異的抗体及びそれらの使用 |
| EP3114142B1 (fr) * | 2014-03-06 | 2019-06-05 | National Research Council of Canada | Anticorps analogues à l'insuline spécifiques du récepteur du facteur de croissance 1 et leurs utilisations |
| KR102355310B1 (ko) | 2014-03-06 | 2022-01-24 | 내셔날 리서치 카운실 오브 캐나다 | 인슐린-유사 성장 인자 1 수용체-특이적 항체 및 그의 용도 |
| DE102014205817A1 (de) * | 2014-03-28 | 2015-10-01 | Aktiebolaget Skf | Wälzlagerkäfig und Verfahren zur Montage eines Wälzlagerkäfigs |
| US10538589B2 (en) | 2015-01-14 | 2020-01-21 | Armagen Inc. | Methods and compositions for increasing N-acetylglucosaminidase (NAGLU) activity in the CNS using a fusion antibody comprising an anti-human insulin receptor antibody and NAGLU |
| EP3101125A1 (fr) * | 2015-06-05 | 2016-12-07 | Laboratorios Del Dr. Esteve, S.A. | Vecteurs viraux recombinés adéno-associés pour le traitement de la mucopolysaccharidose |
| EP3307326B9 (fr) | 2015-06-15 | 2021-02-24 | Angiochem Inc. | Procédés de traitement d'une carcinomatose leptoméningée |
| US11130815B2 (en) | 2015-06-24 | 2021-09-28 | Jcr Pharmaceuticals Co., Ltd. | Fusion proteins containing a BDNF and an anti-human transferrin receptor antibody |
| CN114409783A (zh) * | 2015-06-24 | 2022-04-29 | Jcr制药股份有限公司 | 通过血脑屏障的抗人转铁蛋白受体抗体 |
| WO2017048495A1 (fr) | 2015-09-14 | 2017-03-23 | Children's Hospital Medical Center | Méthodes et compositions pour le traitement de la maladie de gaucher par l'intermédiaire de la modulation du récepteur c5a |
| RU2673038C2 (ru) * | 2016-01-18 | 2018-11-21 | ООО "Международный Биотехнологический Центр "Генериум" | Лекарственное средство на основе бифункционального антитела для лечения мукополисахаридоза II типа |
| KR102318480B1 (ko) * | 2016-08-25 | 2021-10-28 | 제이씨알 파마 가부시키가이샤 | 항체 융합 단백질의 제조 방법 |
| US10759864B2 (en) | 2016-12-26 | 2020-09-01 | Jcr Pharmaceuticals Co., Ltd. | Anti-human transferrin receptor antibody capable of penetrating blood-brain barrier |
| BR112020005271A2 (pt) | 2017-10-02 | 2020-09-15 | Denali Therapeutics Inc. | proteína, polipeptídeo, polinucleotídeo, vetor, célula hospedeira, método para produção de um polipeptídeo, métodos de tratamento de um distúrbio, de diminuição do acúmulo, de monitoramento, de transporte de um agente e de tratamento de um lsd e composição farmacêutica |
| WO2019143761A1 (fr) * | 2018-01-17 | 2019-07-25 | Children's Hospital Medical Center | Compositions et méthodes pour le traitement du syndrome de hunter |
| CA3098162A1 (fr) * | 2018-04-24 | 2019-10-31 | National Research Council Of Canada | Composes therapeutiques franchissant la barriere hemato-encephalique et leurs utilisations |
| KR20200047937A (ko) * | 2018-10-26 | 2020-05-08 | 재단법인 목암생명과학연구소 | Ids를 포함하는 융합 단백질 및 이의 용도 |
| JP7458404B2 (ja) | 2018-12-20 | 2024-03-29 | アーマジェン・インコーポレイテッド | イズロン酸-2-スルファターゼ免疫グロブリン融合タンパク質の精製 |
| EP3947661A1 (fr) * | 2019-04-03 | 2022-02-09 | Denali Therapeutics Inc. | Formulations de molécules protéiques comprenant de l'iduronate 2-sulfatase |
| CA3128035A1 (fr) | 2020-08-13 | 2022-02-13 | Bioasis Technologies, Inc. | Polytherapies pour l'administration dans l'ensemble de la barriere hemato-encephalique |
| US20240066149A1 (en) | 2021-01-12 | 2024-02-29 | Jcr Pharmaceuticals Co., Ltd. | Nucleic Acid Molecule Containing Incorporated Gene Encoding Fused Protein of Ligand and Protein Having Physiological Activity |
| AU2022329856A1 (en) | 2021-08-18 | 2024-03-28 | Joint-Stock Company "Generium" | Targeted delivery of therapeutic enzymes |
Family Cites Families (133)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US5618920A (en) * | 1985-11-01 | 1997-04-08 | Xoma Corporation | Modular assembly of antibody genes, antibodies prepared thereby and use |
| US4801575A (en) * | 1986-07-30 | 1989-01-31 | The Regents Of The University Of California | Chimeric peptides for neuropeptide delivery through the blood-brain barrier |
| US4902505A (en) * | 1986-07-30 | 1990-02-20 | Alkermes | Chimeric peptides for neuropeptide delivery through the blood-brain barrier |
| US4946778A (en) * | 1987-09-21 | 1990-08-07 | Genex Corporation | Single polypeptide chain binding molecules |
| US5530101A (en) * | 1988-12-28 | 1996-06-25 | Protein Design Labs, Inc. | Humanized immunoglobulins |
| US5180820A (en) * | 1989-08-30 | 1993-01-19 | Barde Yves Alain | Brain-derived neurotrophic factor |
| US5229500A (en) * | 1989-08-30 | 1993-07-20 | Regeneron Pharmaceuticals, Inc. | Brain derived neurotrophic factor |
| US6541610B1 (en) | 1989-09-05 | 2003-04-01 | Immunex Corporation | Fusion proteins comprising tumor necrosis factor receptor |
| NZ235148A (en) | 1989-09-05 | 1991-12-23 | Immunex Corp | Tumour necrosis factor receptor protein and dna sequences |
| US5182107A (en) * | 1989-09-07 | 1993-01-26 | Alkermes, Inc. | Transferrin receptor specific antibody-neuropharmaceutical or diagnostic agent conjugates |
| US6329508B1 (en) * | 1989-09-07 | 2001-12-11 | Alkermes, Inc. | Transferrin receptor reactive chimeric antibodies |
| US5154924A (en) * | 1989-09-07 | 1992-10-13 | Alkermes, Inc. | Transferrin receptor specific antibody-neuropharmaceutical agent conjugates |
| US5977307A (en) * | 1989-09-07 | 1999-11-02 | Alkermes, Inc. | Transferrin receptor specific ligand-neuropharmaceutical agent fusion proteins |
| US5672683A (en) * | 1989-09-07 | 1997-09-30 | Alkermes, Inc. | Transferrin neuropharmaceutical agent fusion protein |
| US5527527A (en) * | 1989-09-07 | 1996-06-18 | Alkermes, Inc. | Transferrin receptor specific antibody-neuropharmaceutical agent conjugates |
| EP0417563B1 (fr) * | 1989-09-12 | 2000-07-05 | F. Hoffmann-La Roche Ag | Protéines qui lient le TNF |
| US5527288A (en) | 1990-12-13 | 1996-06-18 | Elan Medical Technologies Limited | Intradermal drug delivery device and method for intradermal delivery of drugs |
| TW279133B (fr) | 1990-12-13 | 1996-06-21 | Elan Med Tech | |
| US6060069A (en) | 1991-05-20 | 2000-05-09 | Dura Pharmaceuticals, Inc. | Pulmonary delivery of pharmaceuticals |
| US6287792B1 (en) * | 1991-06-17 | 2001-09-11 | The Regents Of The University Of California | Drug delivery of antisense oligonucleotides and peptides to tissues in vivo and to cells using avidin-biotin technology |
| EP0528767B1 (fr) * | 1991-08-21 | 2000-01-12 | Novartis AG | Dérivés d'anticorps |
| SG48145A1 (en) * | 1991-09-20 | 1998-04-17 | Synergen Inc | Glial derived neurotphic factor |
| JPH06228199A (ja) | 1992-11-27 | 1994-08-16 | Takeda Chem Ind Ltd | 血液脳関門通過可能なペプチド結合体 |
| CA2115900A1 (fr) | 1993-02-22 | 1994-08-23 | Gerald W. Becker | Cribles pharmaceutiques et anticorps |
| US6195608B1 (en) | 1993-05-28 | 2001-02-27 | Lucent Technologies Inc. | Acoustic highway monitor |
| US5997501A (en) | 1993-11-18 | 1999-12-07 | Elan Corporation, Plc | Intradermal drug delivery device |
| ATE208633T1 (de) * | 1994-09-16 | 2001-11-15 | Merck Patent Gmbh | Immunokonjugate |
| US5656284A (en) | 1995-04-24 | 1997-08-12 | Balkin; Michael S. | Oral transmucosal delivery tablet and method of making it |
| AU6163196A (en) * | 1995-06-07 | 1996-12-30 | Smithkline Beecham Corporation | Method for obtaining receptor agonist antibodies |
| KR100523754B1 (ko) | 1995-09-19 | 2007-06-04 | 아스텔라스세이야쿠 가부시키가이샤 | 에어졸조성물 |
| US6015662A (en) * | 1996-01-23 | 2000-01-18 | Abbott Laboratories | Reagents for use as calibrators and controls |
| US5837231A (en) * | 1996-06-27 | 1998-11-17 | Regents Of The University Of Minnesota | GM-CSF administration for the treatment and prevention of recurrence of brain tumors |
| WO1998002421A1 (fr) | 1996-07-16 | 1998-01-22 | De Staat Der Nederlanden, Vertegenwoordigd Door De Minister Van Welzijn, Volksgezondheid En Cultuur | Esters dibenzodihydropyridinecarboxyliques et leur utilisation dans le cadre d'analyses de chimiluminescence |
| US8173127B2 (en) | 1997-04-09 | 2012-05-08 | Intellect Neurosciences, Inc. | Specific antibodies to amyloid beta peptide, pharmaceutical compositions and methods of use thereof |
| WO1999000150A2 (fr) | 1997-06-27 | 1999-01-07 | Regents Of The University Of California | Ciblage d'un medicament radiopharmaceutique peptidique utilisant in vivo la barriere hemato-encephalique d'un primate et un anticorps monoclonal dirige contre le recepteur humain de l'insuline |
| WO1999000951A1 (fr) | 1997-06-30 | 1999-01-07 | Motorola Inc. | Interconnexion de reseaux a commutation de circuits et de paquets |
| US6165476A (en) | 1997-07-10 | 2000-12-26 | Beth Israel Deaconess Medical Center | Fusion proteins with an immunoglobulin hinge region linker |
| US6482923B1 (en) | 1997-09-17 | 2002-11-19 | Human Genome Sciences, Inc. | Interleukin 17-like receptor protein |
| US6016800A (en) | 1997-10-24 | 2000-01-25 | Century; Theodore J. | Intrapulmonary aerosolizer |
| US6165783A (en) * | 1997-10-24 | 2000-12-26 | Neuro Spheres Holdings Ltd. | Erythropoietin-mediated neurogenesis |
| US6743427B1 (en) * | 1997-12-02 | 2004-06-01 | Neuralab Limited | Prevention and treatment of amyloidogenic disease |
| CN1206004C (zh) | 1997-12-11 | 2005-06-15 | 阿尔扎有限公司 | 增强透皮物剂流量的装置 |
| EP2261229A3 (fr) | 1998-04-20 | 2011-03-23 | GlycArt Biotechnology AG | Modification par glycosylation d'anticorps aux fins d'amélioration de la cytotoxicité cellulaire dépendant des anticorps |
| WO1999066951A2 (fr) | 1998-06-22 | 1999-12-29 | Immunomedics, Inc. | Utilisation d'anticorps bi-specifiques pour diagnostic et therapie de pre-ciblage |
| US6348210B1 (en) | 1998-11-13 | 2002-02-19 | Alza Corporation | Methods for transdermal drug administration |
| US6375975B1 (en) * | 1998-12-21 | 2002-04-23 | Generex Pharmaceuticals Incorporated | Pharmaceutical compositions for buccal and pulmonary application |
| EP2016953A3 (fr) | 1998-12-22 | 2009-04-15 | Genentech, Inc. | Antagonistes de facteur de croissance cellulaire endothéliale vasculaire et utilisations associées |
| US6284262B1 (en) | 1999-01-26 | 2001-09-04 | Virgil A. Place | Compact dosage unit for buccal administration of a pharmacologically active agent |
| US7214658B2 (en) * | 2004-07-06 | 2007-05-08 | Tact Ip, Llc | Method of delivering a TNF antagonist to the brain of a human by perispinal administration without direct intrathecal injection |
| IL145034A0 (en) | 1999-03-05 | 2002-06-30 | Epigenesis Pharmaceuticals Inc | Method for validating/invalidating target(s) and pathways |
| US7309687B1 (en) * | 1999-04-13 | 2007-12-18 | The Kenneth S. Warren Institute, Inc. | Methods for treatment and prevention of neuromuscular and muscular conditions by peripherally administered erythropoietin |
| DE60040024D1 (de) * | 1999-06-16 | 2008-10-02 | Boston Biomedical Res Inst | Immunologische kontrolle des beta-amyloid gehaltes in vivo |
| CZ299516B6 (cs) * | 1999-07-02 | 2008-08-20 | F. Hoffmann-La Roche Ag | Konjugát erythropoetinového glykoproteinu, zpusobjeho výroby a použití a farmaceutická kompozice sjeho obsahem |
| US20020052311A1 (en) * | 1999-09-03 | 2002-05-02 | Beka Solomon | Methods and compostions for the treatment and/or diagnosis of neurological diseases and disorders |
| JP3589912B2 (ja) * | 1999-09-03 | 2004-11-17 | 泰久 福井 | ホスファチジルイノシトール−3,4−二リン酸を認識するモノクローナル抗体 |
| US6195605B1 (en) | 1999-09-29 | 2001-02-27 | Bmi Technologies Inc. | Impact monitor |
| US6585971B1 (en) * | 1999-11-12 | 2003-07-01 | Harbor-Ucla Research And Education Institute | Recombinant α-L-iduronidase, methods for producing and purifying the same and methods for treating disease caused by deficiencies thereof |
| WO2001045730A2 (fr) | 1999-12-20 | 2001-06-28 | Immunex Corporation | Recepteur tweak |
| US6248262B1 (en) * | 2000-02-03 | 2001-06-19 | General Electric Company | Carbon-reinforced thermoplastic resin composition and articles made from same |
| JP2003531582A (ja) * | 2000-02-29 | 2003-10-28 | レキシコン・ジェネティクス・インコーポレーテッド | ヒトトランスポータータンパクおよびそれをコードするポリヌクレオチド |
| US6372250B1 (en) * | 2000-04-25 | 2002-04-16 | The Regents Of The University Of California | Non-invasive gene targeting to the brain |
| US6696274B2 (en) * | 2000-05-03 | 2004-02-24 | Supratek Pharma, Inc. | Ligand for enhancing oral and CNS delivery of biological agents |
| US7078376B1 (en) * | 2000-08-11 | 2006-07-18 | Baxter Healthcare S.A. | Therapeutic methods for treating subjects with a recombinant erythropoietin having high activity and reduced side effects |
| WO2002055736A2 (fr) * | 2000-12-04 | 2002-07-18 | Univ California | Imagerie antisens de l'expression d'un gene du cerveau in vivo |
| ATE361089T1 (de) * | 2001-02-02 | 2007-05-15 | Ortho Mcneil Pharm Inc | Behandlung von neurologischen funktionsstörungen mit fructopyranosesulfamaten und erythropoetin |
| RU2003125637A (ru) * | 2001-02-06 | 2005-03-10 | Мерк Патент ГмбХ (DE) | Модифицированный нейтрофический фактор выделенный из мозга человека (bdnf) с уменьшенной иммуногенностью |
| US8163289B2 (en) | 2001-03-09 | 2012-04-24 | Iterative Therapeutics, Inc. | Methods and compositions involving polymeric immunoglobulin fusion proteins |
| CA2450073C (fr) * | 2001-07-25 | 2017-08-29 | Biomarin Pharmaceutical Inc. | Compositions et procedes de modulation du transport a travers la barriere hematho-encephalique |
| EP1944040B1 (fr) * | 2001-08-17 | 2012-08-01 | Washington University | Procédé d'analyse pour la maladie d'Alzheimer |
| US7125843B2 (en) | 2001-10-19 | 2006-10-24 | Neose Technologies, Inc. | Glycoconjugates including more than one peptide |
| US7053202B2 (en) * | 2001-10-19 | 2006-05-30 | Millennium Pharmaceuticals, Inc. | Immunoglobulin DNA cassette molecules, monobody constructs, methods of production, and methods of use therefor |
| AU2003244817B2 (en) | 2002-06-28 | 2010-08-26 | Domantis Limited | Antigen-binding immunoglobulin single variable domains and dual-specific constructs |
| US20040102369A1 (en) * | 2002-11-27 | 2004-05-27 | The Regents Of The University Of California | Transport of basic fibroblast growth factor across the blood brain barrier |
| US7388079B2 (en) | 2002-11-27 | 2008-06-17 | The Regents Of The University Of California | Delivery of pharmaceutical agents via the human insulin receptor |
| US20050142141A1 (en) * | 2002-11-27 | 2005-06-30 | Pardridge William M. | Delivery of enzymes to the brain |
| CN101444621B (zh) | 2003-02-11 | 2013-11-20 | 夏尔人类遗传性治疗公司 | 使用甲酰-甘氨酸生成酶(fge)对多种硫酸酯酶缺乏症和其它病症进行诊断和治疗 |
| WO2004108071A2 (fr) | 2003-06-05 | 2004-12-16 | Salk Institute For Biological Studies | Compositions et methodes destinees a cibler un polypeptide sur le systeme nerveux central |
| US20050026823A1 (en) | 2003-06-20 | 2005-02-03 | Biomarin Pharmaceutical Inc. | Use of the chaperone receptor-associated protein (RAP) for the delivery of therapeutic compounds to the brain and other tissues |
| NZ544924A (en) | 2003-06-27 | 2009-03-31 | Biogen Idec Inc | Modified binding molecules comprising connecting peptides |
| US7112299B2 (en) | 2003-07-09 | 2006-09-26 | Michael Merrick | Systems and methods for fabricating composite fiberglass laminate articles |
| US7294704B2 (en) * | 2003-08-15 | 2007-11-13 | Diadexus, Inc. | Pro108 antibody compositions and methods of use and use of Pro108 to assess cancer risk |
| EP1548031A1 (fr) * | 2003-12-22 | 2005-06-29 | Dubai Genetics FZ-LLC | Erythropoietin identique à la nature |
| NZ576986A (en) * | 2004-01-30 | 2010-12-24 | Shire Pharmaceuticals Ireland Ltd | Production and purification of recombinant arylsulfatase A |
| US7939490B2 (en) * | 2004-12-13 | 2011-05-10 | University Of Maryland, Baltimore | TWEAK as a therapeutic target for treating central nervous system diseases associated with cerebral edema and cell death |
| WO2006074399A2 (fr) | 2005-01-05 | 2006-07-13 | Biogen Idec Ma Inc. | Molecules de liaison multispecifiques comprenant des peptides de connexion |
| US7906625B2 (en) * | 2005-01-24 | 2011-03-15 | Amgen Inc. | Humanized anti-amyloid antibody |
| US7341720B2 (en) | 2005-04-06 | 2008-03-11 | Genzyme Corporation | Targeting of glycoprotein therapeutics |
| WO2006118308A1 (fr) | 2005-05-02 | 2006-11-09 | Toray Industries, Inc. | Composition et procede permettant de diagnostiquer un cancer esophagien et une metastase d’un cancer esophagien |
| NZ564843A (en) | 2005-08-03 | 2012-05-25 | Immunogen Inc | Immunoconjugate formulations comprising an immunoconjugate and an excipient in a buffered aqueous solution |
| WO2007022416A2 (fr) | 2005-08-18 | 2007-02-22 | Ramot At Tel Aviv University Ltd. | Anticorps monocatenaires diriges contre le peptide $g(b)-amyloide |
| US20090047338A1 (en) | 2005-10-05 | 2009-02-19 | Immune Disease Institute, Inc. | Method to Treat Flavivirus Infection with siRNA |
| US8124095B2 (en) * | 2005-10-07 | 2012-02-28 | Armagen Technologies, Inc. | Fusion proteins for delivery of erythropoietin to the CNS |
| US8053569B2 (en) * | 2005-10-07 | 2011-11-08 | Armagen Technologies, Inc. | Nucleic acids encoding and methods of producing fusion proteins |
| US8741260B2 (en) | 2005-10-07 | 2014-06-03 | Armagen Technologies, Inc. | Fusion proteins for delivery of GDNF to the CNS |
| DE602006021335D1 (de) | 2005-10-21 | 2011-05-26 | Hoffmann La Roche | Methode zur rekombinanten expression eines polyeptids |
| WO2007091250A2 (fr) | 2006-02-06 | 2007-08-16 | The Medical Research And Infrastructure Fund Of The Tel-Aviv Sourasky Medical Center | Enzymotherapie de remplacement pour le traitement des maladies lysosomiales |
| US7981417B2 (en) | 2006-06-07 | 2011-07-19 | Wisconsin Alumni Research Foundation | Blood-brain barrier targeting anti-bodies |
| EP2029621A2 (fr) | 2006-06-07 | 2009-03-04 | Wisconsin Alumni Research Foundation | Anticorps ciblant la barrière hémato-encéphalique |
| GB0614780D0 (en) | 2006-07-25 | 2006-09-06 | Ucb Sa | Biological products |
| US8497246B2 (en) * | 2006-08-18 | 2013-07-30 | Armagen Technologies, Inc. | Methods for diagnosing and treating CNS disorders by trans-blood-brain barrier delivery of protein compositions |
| US9388425B2 (en) | 2006-10-20 | 2016-07-12 | Trustees Of Boston University | Tunable genetic switch for regulating gene expression |
| WO2008065372A2 (fr) * | 2006-11-28 | 2008-06-05 | Nautilus Biotech, S.A. | Polypeptides d'érythropoïétine modifiés et utilisation de ceux-ci dans des traitements |
| AU2008261212A1 (en) * | 2007-06-15 | 2008-12-18 | University Of Zurich | Treatment for Alzheimer' s disease |
| EP2997976A1 (fr) * | 2007-07-27 | 2016-03-23 | Armagen Technologies, Inc. | Procédés et compositions pour augmenter l'activité alpha-l-iduronidase dans le système nerveux central |
| WO2009070597A2 (fr) | 2007-11-26 | 2009-06-04 | Armagen Technologies, Inc. | Protéines de fusion assurant le transport du gdnf jusqu'au système nerveux central |
| MX2011000071A (es) | 2008-07-02 | 2011-05-03 | Emergent Product Dev Seattle | Inmunoterapeuticos de interleucina-6 (il6). |
| US20100077498A1 (en) * | 2008-09-11 | 2010-03-25 | Pardridge William M | Compositions and methods for blood-brain barrier delivery in the mouse |
| US20100098693A1 (en) * | 2008-10-07 | 2010-04-22 | Pardridge William M | Compositions and methods for blood-brain barrier delivery of organophosphatases |
| MX2011006685A (es) | 2008-12-17 | 2011-09-27 | Angiochem Inc | Inhibidores de metaloproteinas de matriz de membrana tipo-1 y sus usos. |
| WO2010108048A2 (fr) | 2009-03-18 | 2010-09-23 | Armagen Technologies, Inc. | Compositions et procédés pour le transport de protéines de fusion igg-récepteur leurre à travers la barrière hémato-encéphalique |
| BRPI1010024A2 (pt) | 2009-06-05 | 2019-09-24 | Link Medicine Corp | derivados de aminopirrolidinona e uso dos mesmos |
| EP2446036B1 (fr) | 2009-06-24 | 2017-03-01 | CuRNA, Inc. | Traitement de maladies associées au récepteur de facteur nécrosant des tumeurs 2 (tnfr2) par inhibition de la transcription antisens naturelle de tnfr2 |
| PT2485761T (pt) | 2009-10-09 | 2019-05-30 | Armagen Inc | Métodos e composições para aumentar a atividade da iduronato 2-sulfatase no snc |
| EP2585105B1 (fr) | 2010-06-25 | 2017-08-09 | Shire Human Genetic Therapies, Inc. | Traitement du syndrome de sanfilippo de type b |
| PT2585104T (pt) | 2010-06-25 | 2019-10-30 | Shire Human Genetic Therapies | Métodos e composições de arilsulfatase a para a administração no snc |
| KR20140005842A (ko) | 2010-06-25 | 2014-01-15 | 샤이어 휴먼 지네틱 테라피즈 인크. | 헤파란 n-설파타제의 cns 전달을 위한 방법들 및 조성물들 |
| ES2631356T3 (es) | 2010-11-30 | 2017-08-30 | F. Hoffmann-La Roche Ag | Anticuerpos anti-receptor de transferrina de baja afinidad y su uso para transferir scFv terapéuticos a través de la barrera hematoencefálica |
| WO2012085622A1 (fr) | 2010-12-22 | 2012-06-28 | Fondazione Telethon | Stratégies thérapeutiques pour traiter une pathologie du snc dans des mucopolysaccharidoses |
| US8580922B2 (en) | 2011-03-04 | 2013-11-12 | Shire Human Genetic Therapies, Inc. | Peptide linkers for polypeptide compositions and methods for using same |
| US20130039888A1 (en) | 2011-06-08 | 2013-02-14 | Nationwide Children's Hospital Inc. | Products and methods for delivery of polynucleotides by adeno-associated virus for lysosomal storage disorders |
| JP6061922B2 (ja) | 2011-06-22 | 2017-01-18 | ザ ジェネラル ホスピタル コーポレイション | プロテイノパチーの処置方法 |
| US8859256B2 (en) | 2011-10-05 | 2014-10-14 | Genelux Corporation | Method for detecting replication or colonization of a biological therapeutic |
| US9579366B2 (en) | 2011-10-12 | 2017-02-28 | Alexion Pharmaceuticals, Inc. | Recombinant human NaGlu protein and uses thereof |
| US8486399B2 (en) * | 2011-12-02 | 2013-07-16 | Armagen Technologies, Inc. | Methods and compositions for increasing arylsulfatase A activity in the CNS |
| US20130323221A1 (en) | 2012-05-30 | 2013-12-05 | Biostrategies LC | Plant lectins as carriers of associated drug substances into animal and human cells |
| CN104684928A (zh) | 2012-08-02 | 2015-06-03 | Jn生物科学有限责任公司 | 通过半胱氨酸突变和μ尾端多聚化的抗体或融合蛋白 |
| US10400226B2 (en) | 2012-10-19 | 2019-09-03 | Tokushima University | High functional enzyme having modified substrate specificity of human β-hexosaminidase B and exhibiting protease resistance |
| JP6083219B2 (ja) | 2012-12-06 | 2017-02-22 | 富士通セミコンダクター株式会社 | プラズマフラッドガン及びイオン注入装置 |
| US20140354655A1 (en) | 2013-06-04 | 2014-12-04 | Qualcomm Mems Technologies, Inc. | Reducing floating node leakage current with a feedback transistor |
| US10906981B2 (en) | 2013-07-19 | 2021-02-02 | The Regents Of The University Of California | Compositions and methods related to structures that cross the blood brain barrier |
| WO2015012944A1 (fr) | 2013-07-22 | 2015-01-29 | Armagen Technologies, Inc | Procédés et compositions pour augmenter l'activité enzymatique dans le snc |
| WO2015150922A2 (fr) | 2014-03-17 | 2015-10-08 | The Hospital For Sick Children | Variants de protéine β-hexosaminidase et procédés associés permettant de traiter des gangliosidoses de gm2 |
| US10538589B2 (en) | 2015-01-14 | 2020-01-21 | Armagen Inc. | Methods and compositions for increasing N-acetylglucosaminidase (NAGLU) activity in the CNS using a fusion antibody comprising an anti-human insulin receptor antibody and NAGLU |
-
2010
- 2010-10-08 PT PT10822810T patent/PT2485761T/pt unknown
- 2010-10-08 US US12/901,481 patent/US8834874B2/en active Active
- 2010-10-08 SI SI201031879T patent/SI2485761T1/sl unknown
- 2010-10-08 EP EP19150184.0A patent/EP3533467B1/fr active Active
- 2010-10-08 ES ES10822810T patent/ES2725200T3/es active Active
- 2010-10-08 EP EP10822810.7A patent/EP2485761B1/fr active Active
- 2010-10-08 JP JP2012533375A patent/JP2013507131A/ja not_active Withdrawn
- 2010-10-08 EP EP23183395.5A patent/EP4273164A3/fr active Pending
- 2010-10-08 WO PCT/US2010/052113 patent/WO2011044542A1/fr active Application Filing
- 2010-10-08 DK DK10822810.7T patent/DK2485761T3/da active
- 2010-10-08 HU HUE10822810 patent/HUE044865T2/hu unknown
- 2010-10-08 PL PL10822810T patent/PL2485761T3/pl unknown
-
2014
- 2014-06-16 US US14/305,402 patent/US10011651B2/en active Active
-
2016
- 2016-01-28 JP JP2016014716A patent/JP2016155805A/ja active Pending
-
2018
- 2018-05-08 JP JP2018089998A patent/JP2018154629A/ja active Pending
- 2018-05-17 US US15/982,990 patent/US11028156B2/en active Active
-
2019
- 2019-04-12 HR HRP20190690TT patent/HRP20190690T1/hr unknown
-
2020
- 2020-10-01 JP JP2020167101A patent/JP2021008488A/ja active Pending
-
2021
- 2021-04-30 US US17/246,288 patent/US20210253681A1/en active Pending
-
2022
- 2022-12-22 JP JP2022205808A patent/JP2023033321A/ja active Pending
Also Published As
| Publication number | Publication date |
|---|---|
| SI2485761T1 (sl) | 2019-05-31 |
| WO2011044542A1 (fr) | 2011-04-14 |
| US11028156B2 (en) | 2021-06-08 |
| EP2485761A1 (fr) | 2012-08-15 |
| JP2018154629A (ja) | 2018-10-04 |
| EP4273164A3 (fr) | 2024-01-24 |
| US20190185551A2 (en) | 2019-06-20 |
| EP3533467A2 (fr) | 2019-09-04 |
| DK2485761T3 (da) | 2019-05-06 |
| EP2485761B1 (fr) | 2019-02-27 |
| US20180251535A1 (en) | 2018-09-06 |
| HUE044865T2 (hu) | 2019-11-28 |
| US8834874B2 (en) | 2014-09-16 |
| HRP20190690T1 (hr) | 2019-06-28 |
| JP2013507131A (ja) | 2013-03-04 |
| US20110110935A1 (en) | 2011-05-12 |
| PT2485761T (pt) | 2019-05-30 |
| EP2485761A4 (fr) | 2013-04-03 |
| JP2016155805A (ja) | 2016-09-01 |
| EP3533467A3 (fr) | 2020-01-15 |
| JP2023033321A (ja) | 2023-03-10 |
| US10011651B2 (en) | 2018-07-03 |
| US20150004160A1 (en) | 2015-01-01 |
| US20210253681A1 (en) | 2021-08-19 |
| PL2485761T3 (pl) | 2019-10-31 |
| EP4273164A2 (fr) | 2023-11-08 |
| ES2725200T3 (es) | 2019-09-20 |
| JP2021008488A (ja) | 2021-01-28 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| US20210253681A1 (en) | Methods and compositions for increasing iduronate 2-sulfatase activity in the cns | |
| US9975955B2 (en) | Methods and compositions for increasing arylsulfatase A activity in the CNS | |
| US20220348672A1 (en) | Methods and compositions for increasing enzyme activity in the cns | |
| US20220127369A1 (en) | Methods and compositions for increasing n-acetylglucosaminidase activity in the cns |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| PUAI | Public reference made under article 153(3) epc to a published international application that has entered the european phase |
Free format text: ORIGINAL CODE: 0009012 |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: THE APPLICATION HAS BEEN PUBLISHED |
|
| AC | Divisional application: reference to earlier application |
Ref document number: 2485761 Country of ref document: EP Kind code of ref document: P |
|
| AK | Designated contracting states |
Kind code of ref document: A2 Designated state(s): AL AT BE BG CH CY CZ DE DK EE ES FI FR GB GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO RS SE SI SK SM TR |
|
| PUAL | Search report despatched |
Free format text: ORIGINAL CODE: 0009013 |
|
| AK | Designated contracting states |
Kind code of ref document: A3 Designated state(s): AL AT BE BG CH CY CZ DE DK EE ES FI FR GB GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO RS SE SI SK SM TR |
|
| RIC1 | Information provided on ipc code assigned before grant |
Ipc: C07K 16/28 20060101AFI20191209BHEP Ipc: A61P 25/28 20060101ALI20191209BHEP Ipc: A61K 39/00 20060101ALN20191209BHEP Ipc: A61K 39/395 20060101ALI20191209BHEP |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: REQUEST FOR EXAMINATION WAS MADE |
|
| REG | Reference to a national code |
Ref country code: HK Ref legal event code: DE Ref document number: 40013772 Country of ref document: HK |
|
| 17P | Request for examination filed |
Effective date: 20200714 |
|
| RBV | Designated contracting states (corrected) |
Designated state(s): AL AT BE BG CH CY CZ DE DK EE ES FI FR GB GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO RS SE SI SK SM TR |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: EXAMINATION IS IN PROGRESS |
|
| 17Q | First examination report despatched |
Effective date: 20201015 |
|
| REG | Reference to a national code |
Ref country code: DE Ref legal event code: R079 Ref document number: 602010068939 Country of ref document: DE Free format text: PREVIOUS MAIN CLASS: A61K0039395000 Ipc: C07K0016280000 Ref country code: DE Ref legal event code: R079 Free format text: PREVIOUS MAIN CLASS: A61K0039395000 |
|
| GRAP | Despatch of communication of intention to grant a patent |
Free format text: ORIGINAL CODE: EPIDOSNIGR1 |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: GRANT OF PATENT IS INTENDED |
|
| RIC1 | Information provided on ipc code assigned before grant |
Ipc: A61K 39/00 20060101ALN20230118BHEP Ipc: C07K 16/18 20060101ALI20230118BHEP Ipc: A61P 25/28 20060101ALI20230118BHEP Ipc: A61K 39/395 20060101ALI20230118BHEP Ipc: C07K 16/28 20060101AFI20230118BHEP |
|
| INTG | Intention to grant announced |
Effective date: 20230207 |
|
| RIC1 | Information provided on ipc code assigned before grant |
Ipc: A61K 39/00 20060101ALN20230130BHEP Ipc: C07K 16/18 20060101ALI20230130BHEP Ipc: A61P 25/28 20060101ALI20230130BHEP Ipc: A61K 39/395 20060101ALI20230130BHEP Ipc: C07K 16/28 20060101AFI20230130BHEP |
|
| GRAS | Grant fee paid |
Free format text: ORIGINAL CODE: EPIDOSNIGR3 |
|
| GRAA | (expected) grant |
Free format text: ORIGINAL CODE: 0009210 |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: THE PATENT HAS BEEN GRANTED |
|
| AC | Divisional application: reference to earlier application |
Ref document number: 2485761 Country of ref document: EP Kind code of ref document: P |
|
| AK | Designated contracting states |
Kind code of ref document: B1 Designated state(s): AL AT BE BG CH CY CZ DE DK EE ES FI FR GB GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO RS SE SI SK SM TR |
|
| REG | Reference to a national code |
Ref country code: CH Ref legal event code: EP |
|
| REG | Reference to a national code |
Ref country code: IE Ref legal event code: FG4D |
|
| REG | Reference to a national code |
Ref country code: DE Ref legal event code: R096 Ref document number: 602010068939 Country of ref document: DE |
|
| P01 | Opt-out of the competence of the unified patent court (upc) registered |
Effective date: 20230914 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: GB Payment date: 20230829 Year of fee payment: 14 |
|
| REG | Reference to a national code |
Ref country code: LT Ref legal event code: MG9D |
|
| REG | Reference to a national code |
Ref country code: NL Ref legal event code: MP Effective date: 20230726 |
|
| REG | Reference to a national code |
Ref country code: AT Ref legal event code: MK05 Ref document number: 1591869 Country of ref document: AT Kind code of ref document: T Effective date: 20230726 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: NL Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: GR Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20231027 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: IS Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20231126 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: SE Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 Ref country code: RS Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 Ref country code: PT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20231127 Ref country code: NO Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20231026 Ref country code: LV Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 Ref country code: LT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 Ref country code: IS Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20231126 Ref country code: HR Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 Ref country code: GR Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20231027 Ref country code: FI Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 Ref country code: AT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: PL Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: ES Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: SM Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 Ref country code: RO Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 Ref country code: ES Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 Ref country code: EE Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 Ref country code: DK Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 Ref country code: CZ Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 Ref country code: SK Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20230726 |