EP1868663B1 - Distribution d'agents hautement lipophiles au moyen de dispositifs medicaux - Google Patents
Distribution d'agents hautement lipophiles au moyen de dispositifs medicaux Download PDFInfo
- Publication number
- EP1868663B1 EP1868663B1 EP20060739194 EP06739194A EP1868663B1 EP 1868663 B1 EP1868663 B1 EP 1868663B1 EP 20060739194 EP20060739194 EP 20060739194 EP 06739194 A EP06739194 A EP 06739194A EP 1868663 B1 EP1868663 B1 EP 1868663B1
- Authority
- EP
- European Patent Office
- Prior art keywords
- lipophilic agent
- agent
- beneficial agent
- drug
- lipophilic
- Prior art date
- Legal status (The legal status is an assumption and is not a legal conclusion. Google has not performed a legal analysis and makes no representation as to the accuracy of the status listed.)
- Active
Links
- 0 CC(C(C=C1)OC2C=CC([S+]CC([C@@]3OC(*)(*)OC3)N(C=O)O)=CC2)C=C1OC(F)(F)F Chemical compound CC(C(C=C1)OC2C=CC([S+]CC([C@@]3OC(*)(*)OC3)N(C=O)O)=CC2)C=C1OC(F)(F)F 0.000 description 2
Images
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L31/00—Materials for other surgical articles, e.g. stents, stent-grafts, shunts, surgical drapes, guide wires, materials for adhesion prevention, occluding devices, surgical gloves, tissue fixation devices
- A61L31/08—Materials for coatings
- A61L31/10—Macromolecular materials
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2/00—Filters implantable into blood vessels; Prostheses, i.e. artificial substitutes or replacements for parts of the body; Appliances for connecting them with the body; Devices providing patency to, or preventing collapsing of, tubular structures of the body, e.g. stents
- A61F2/02—Prostheses implantable into the body
- A61F2/04—Hollow or tubular parts of organs, e.g. bladders, tracheae, bronchi or bile ducts
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2/00—Filters implantable into blood vessels; Prostheses, i.e. artificial substitutes or replacements for parts of the body; Appliances for connecting them with the body; Devices providing patency to, or preventing collapsing of, tubular structures of the body, e.g. stents
- A61F2/82—Devices providing patency to, or preventing collapsing of, tubular structures of the body, e.g. stents
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L31/00—Materials for other surgical articles, e.g. stents, stent-grafts, shunts, surgical drapes, guide wires, materials for adhesion prevention, occluding devices, surgical gloves, tissue fixation devices
- A61L31/14—Materials characterised by their function or physical properties, e.g. injectable or lubricating compositions, shape-memory materials, surface modified materials
- A61L31/16—Biologically active materials, e.g. therapeutic substances
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P31/00—Antiinfectives, i.e. antibiotics, antiseptics, chemotherapeutics
- A61P31/04—Antibacterial agents
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P43/00—Drugs for specific purposes, not provided for in groups A61P1/00-A61P41/00
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P9/00—Drugs for disorders of the cardiovascular system
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2/00—Filters implantable into blood vessels; Prostheses, i.e. artificial substitutes or replacements for parts of the body; Appliances for connecting them with the body; Devices providing patency to, or preventing collapsing of, tubular structures of the body, e.g. stents
- A61F2/02—Prostheses implantable into the body
- A61F2/04—Hollow or tubular parts of organs, e.g. bladders, tracheae, bronchi or bile ducts
- A61F2002/044—Oesophagi or esophagi or gullets
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2/00—Filters implantable into blood vessels; Prostheses, i.e. artificial substitutes or replacements for parts of the body; Appliances for connecting them with the body; Devices providing patency to, or preventing collapsing of, tubular structures of the body, e.g. stents
- A61F2/02—Prostheses implantable into the body
- A61F2/04—Hollow or tubular parts of organs, e.g. bladders, tracheae, bronchi or bile ducts
- A61F2002/047—Urethrae
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2250/00—Special features of prostheses classified in groups A61F2/00 - A61F2/26 or A61F2/82 or A61F9/00 or A61F11/00 or subgroups thereof
- A61F2250/0058—Additional features; Implant or prostheses properties not otherwise provided for
- A61F2250/0067—Means for introducing or releasing pharmaceutical products into the body
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L2300/00—Biologically active materials used in bandages, wound dressings, absorbent pads or medical devices
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L2300/00—Biologically active materials used in bandages, wound dressings, absorbent pads or medical devices
- A61L2300/20—Biologically active materials used in bandages, wound dressings, absorbent pads or medical devices containing or releasing organic materials
- A61L2300/216—Biologically active materials used in bandages, wound dressings, absorbent pads or medical devices containing or releasing organic materials with other specific functional groups, e.g. aldehydes, ketones, phenols, quaternary phosphonium groups
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L2300/00—Biologically active materials used in bandages, wound dressings, absorbent pads or medical devices
- A61L2300/20—Biologically active materials used in bandages, wound dressings, absorbent pads or medical devices containing or releasing organic materials
- A61L2300/22—Lipids, fatty acids, e.g. prostaglandins, oils, fats, waxes
- A61L2300/222—Steroids, e.g. corticosteroids
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L2300/00—Biologically active materials used in bandages, wound dressings, absorbent pads or medical devices
- A61L2300/60—Biologically active materials used in bandages, wound dressings, absorbent pads or medical devices characterised by a special physical form
- A61L2300/606—Coatings
Definitions
- the invention relates to apparatuses and systems for remote drug delivery of highly lipophilic agents utilizing medical devices, and more specifically, lipophilic agents having a transfer coefficient of at least approximately 5,000 (ug/mL) -1 .
- cyclosporine (cyclosporin A) has found wide use since its introduction in the fields of organ transplantation and immunomodulation, and has brought about a significant increase in the success rate for transplantation procedures.
- macrocyclic compounds having potent immunomodulatory activity have been discovered.
- Okuhara et al. in European Patent Application No. 184,162, published June 11, 1986 , disclose a number of macrocyclic compounds isolated from the genus Streptomyces , including the immunosuppressant FK-506, a 23-membered macrocyclic lactone, which was isolated from a strain of S . tsukubaensis.
- FR-900520 and FR-900523 which differ from FK - 506 in their alkyl substituent at C-21, have been isolated from S . hygroscopicus yakushimnaensis.
- Another analog, FR-900525, produced by S . tsukubaensis differs from FK-506 in the replacement of a pipecolic acid moiety with a proline group.
- Unsatisfactory side-effects associated with cyclosporine and FK-506 such as nephrotoxicity, have led to a continued search for immunosuppressant compounds having improved efficacy and safety, including an immunosuppressive agent which is effective topically, but ineffective systemically ( U.S. Patent No. 5,457,111 ).
- Rapamycin is a macrocyclic triene antibiotic produced by Streptomyces hygroscopicus , which was found to have antifungal activity, particularly against Candida albicans , both in vitro and in vivo ( C. Vezina et al., J. Antibiot. 1975, 28, 721 ; S. N. Sehgal et al., J. Antibiot. 1975, 28, 727 ; H. A. Baker et al., J. Antibiot. 1978, 31, 539 ; U.S. Patent No. 3,929,992 ; and U.S. Patent No. 3,993,749 ).
- Rapamycin alone ( U.S. Patent No. 4,885,171 ) or in combination with picibanil ( U.S. Patent No. 4,401,653 ) has been shown to have antitumor activity.
- rapamycin was also shown to be effective as an immunosuppressant in the experimental allergic encephalomyelitis model, a model for multiple sclerosis; in the adjuvant arthritis model, a model for rheumatoid arthritis; and was shown to effectively inhibit the formation of IgE-like antibodies ( R. Martel et al., Can. J. Physiol. Pharmacol., 1977, 55, 48 ).
- rapamycin The immunosuppressive effects of rapamycin have also been disclosed in FASEB, 1989, 3, 3411 as has its ability to prolong survival time of organ grafts in histoincompatible rodents ( R. Morris, Med. Sci. Res., 1989,17, 877 ). The ability of rapamycin to inhibit T-cell activation was disclosed by M. Strauch ( FASEB, 1989, 3, 3411 ). These and other biological effects of rapamycin are reviewed in Transplantation Reviews, 1992, 6, 39-87 .
- Rapamycin has been shown to reduce neointimal proliferation in animal models, and to reduce the rate of restenosis in humans. Evidence has been published showing that rapamycin also exhibits an anti-inflammatory effect, a characteristic which supported its selection as an agent for the treatment of rheumatoid arthritis. Because both cell proliferation and inflammation are thought to be causative factors in the formation of restenotic lesions after balloon angioplasty and stent placement, rapamycin and analogs thereof have been proposed for the prevention of restenosis.
- Ester and diester derivatives of rapamycin have been shown to be useful as antifungal agents ( U.S. Patent No. 4,316,885 ) and as water soluble prodrugs of rapamycin ( U.S. Patent No. 4,650,803 ).
- rapamycin Numerous chemical modifications of rapamycin have been attempted. These include the preparation of ester and diester derivatives of rapamycin ( WO 92/05179 ), 27-oximes of rapamycin ( EP0 467606 ); 42-oxo analog of rapamycin ( U.S. Patent No. 5,023,262 ); bicyclic rapamycins ( U.S. Patent No. 5,120,725 ); rapamycin dimers ( U.S. Patent No. 5,120,727 ); silyl ethers of rapamycin ( U.S. Patent No. 5,120,842 ); and arylsulfonates and sulfamates ( U.S. Patent No. 5,177, 203 ).
- Rapamycin was recently synthesized in its naturally occurring enantiomeric form ( K. C. Nicolaou et al., J. Am. Chem. Soc., 1993, 115, 4419-4420 ; S. L. Schreiber, J. Am. Chem. Soc., 1993, 115, 7906-7907 ; S. J. Danishefsky, J. Am. Chem. Soc., 1993, 115, 9345-9346 .
- rapamycin like FK-506, binds to FKBP-12 ( Siekierka, J. J.; Hung, S. H. Y.; Poe, M.; Lin, C. S.; Sigal, N. H. Nature, 1989, 341, 755-757 ; Harding, M. W.; Galat, A.; Uehling, D. E.; Schreiber, S. L. Nature 1989, 341, 758-760 ; Dumont, F. J.; Melino, M. R.; Staruch, M. J.; Koprak, S. L.; Fischer, P. A.; Sigal, N. H. J. Immunol. 1990, 144, 1418-1424 ; Bierer, B.
- PTCA Percutaneous transluminal coronary angioplasty
- stents were introduced to maintain vessel patency after angioplasty. Stenting is involved in 90% of angioplasty performed today.
- rate of restenosis ranged from 30% to 50% of the patients who were treated with balloon angioplasty.
- the recurrence rate after dilatation of in-stent restenosis may be as high as 70% in selected patient subsets, while the angiographic restenosis rate in de novo stent placement is about 20%. Placement of the stent reduced the restenosis rate to 15% to 20%. This percentage likely represents the best results obtainable with purely mechanical stenting.
- the restenotic lesion is caused primarily by neointimal hyperplasia, which is distinctly different from atherosclerotic disease both in time-course and in histopathologic appearance. Restenosis is a healing process of damaged coronary arterial walls, with neointimal tissue impinging significantly on the vessel lumen. Vascular brachytherapy appears to be efficacious against in-stent restenotic lesions. Radiation, however, has limitations of practicality and expense, and lingering questions about safety and durability.
- a medical device having an interventional component including stent devices in blood vessels, urinary tracts or other difficult to access places for the purpose of preventing restenosis, providing vessel or lumen wall support or reinforcement and for other therapeutic or restorative functions has become a common form of long-term treatment.
- interventional components are applied to a location of interest utilizing a vascular catheter, or similar transluminal device, to carry the stent to the location of interest where it is thereafter released to expand or be expanded in situ.
- vascular catheter or similar transluminal device
- Implanted interventional components including stents have also been used to carry medicinal agents, such as thrombolytic agents.
- U.S. Pat. No. 5,163,952 to Froix discloses a thermal memoried expanding plastic stent device that can be formulated to carry a medicinal agent by utilizing the material of the stent itself as an inert polymeric drug carrier. Drug elution rates from a drug-loaded coating containing a hydrophilic (or lipophobic) drug are usually very fast initially when the coated device contacts body fluid or blood.
- an ongoing problem for drug delivery stents is achieving therapeutic drug concentrations at a target site within the body with minimal losses and systemic side effects.
- One technique to reduce the so-called burst effect is to add a membrane containing porosigen over the coating layer containing the biologically active material, as described for example in U.S. Patent Nos. 5,605,696 and 5,447,724 .
- Polymers are also used on stents as drug release coatings, as taught for example in US 6,419,692 .
- U.S. Patent 6,284,305 describes elastomer coated implants in which the elastomer overcoat to control release of biologically active agent from an undercoat applied to a stent.
- U.S. Patent 5,624,411 discloses a porous polymer on a stent to control the administration of a drug.
- WO 0187372 describes a stent coated with a polymer loaded with a combination of drugs, including rapamycin and dexamethasone.
- Pinchuk in U.S. Patent No. 5,092,877 , discloses a stent of a polymeric material that may be employed with a coating associated with the delivery of drugs.
- Other patents which are directed to devices of the class utilizing biodegradable or biosorbable polymers include Tang et al, U.S. Patent No. 4,916,193 and MacGregor, U.S. Patent No. 4,994,071 . Sahatjian in U.S. Patent No.
- 5,304,121 discloses a coating applied to a stent consisting of a hydrogel polymer and a preselected drug; possible drugs include cell growth inhibitors and heparin.
- a further method of making a coated intravascular stent carrying a therapeutic material in which a polymer coating is dissolved in a solvent and the therapeutic material dispersed in the solvent and the solvent thereafter evaporated is described in Berg et al, U.S. Pat. No. 5,464,650 .
- Previous drug eluting stents have been constructed to deliver therapeutic agents predominantly to the tissue immediately adjacent to the site of stent placement.
- the objective has been to control neointimal formation and allow the coronary vascular system to achieve rapid healing. Consequently, the bulk of the drug or drugs delivered is either present in the vascular tissue adjacent to the site of stent implantation, stays on the stent for prolonged periods, or is released into the blood stream.
- agents and devices which offer deep penetration of beneficial agents to tissues not immediately adjacent to the device. For example, delivery of a drug from a stent which not only delivers drug to the adjacent tissue, but also penetrates the myocardium and provides therapeutically useful doses of drug to a wide volume of tissue is particularly attractive.
- the invention relates to a system for delivering a lipophilic agent, comprising: a medical device, a first lipophilic agent, which is capable of penetrating a body lumen, and which is zotarolimus having the structures as follows: and a beneficial agent selected from the group consisting of nifedipine, diltiazem, nicardipine, verapamil, nadolol, metoprolol, propranolol, atenolol, esmolol, nitroglycerin, isosorbide dinitrate, carvedilol, digitalis, levosimendan, batimistat, prinomastat, marimistat, ABT-518, ABT-627 (atrasentan), testosterone, progesterone, indomethacin, phenyl salicylate, ⁇ -estradiol, vindesine, dipyridamole, methotrexate, metrizamide, iopa
- Yet another aspect of the invention relates to a medical device, comprising: a therapeutically effective amount of a first lipophilic agent, which is associated with said medical device and capable of penetrating a body lumen, and which is zotarolimus having the structures as follows: and a beneficial agent selected from the group consisting of nifedipine, diltiazem, nicardipine, verapamil, nadolol, metoprolol, propranolol, atenolol, esmolol, nitroglycerin, isosorbide dinitrate, carvedilol, digitalis, levosimendan, batimistat, prinomastat, marimistat, ABT-518, ABT-627 (atrasentan), testosterone, progesterone, indomethacin, phenyl salicylate, ⁇ -estradiol, vindesine, dipyridamole, methotrexate, metrizamide,
- Still yet another aspect of the invention relates to a stent, comprising: a therapeutically effective amount of a first lipophilic agent, which is associated with said stent and capable of penetrating a body lumen, and which is zotarolimus having the structures as follows: and a beneficial agent selected from the group consisting of nifedipine, diltiazem, nicardipine, verapamil, nadolol, metoprolol, propranolol, atenolol, esmolol, nitroglycerin, isosorbide dinitrate, carvedilol, digitalis, levosimendan, batimistat, prinomastat, marimistat, ABT-518, ABT-627 (atrasentan), testosterone, progesterone, indomethacin, phenyl salicylate, ⁇ -estradiol, vindesine, dipyridamole, methotrexate, metriz
- An object of embodiments of the invention is to provide increased uptake of a drug into the vessel wall with minimal loss of the drug to the more hydrophilic systemic circulation.
- a further object of embodiments of the invention is to provide a drug delivery system that reduces restenosis in percutaneous intervention of coronary arteries.
- Yet another object of embodiments of the invention is to provide a more highly lipophilic compound than rapamycin.
- Still yet other objects of embodiments of the invention are to improve drug transport into tissue cells of the arterial wall and improve tissue retention of the drug.
- Yet another object of embodiments of the invention is to provide a deeper penetration and wider distribution of the drug from the medical device to the adjacent tissue allowing therapeutically effective amounts of the drug to the targeted area in a subject.
- the invention relates to apparatuses, and drug delivery systems for delivering a lipophilic agent to a body lumen.
- a system for delivering a lipophilic agent comprising: a medical device, a first lipophilic agent, which is capable of penetrating a body lumen, and which is zotarolimus having the structures as follows: and a beneficial agent selected from the group consisting of nifedipine, diltiazem, nicardipine, verapamil, nadolol, metoprolol, propranolol, atenolol, esmolol, nitroglycerin, isosorbide dinitrate, carvedilol, digitalis, levosimendan, batimistat, prinomastat, marimistat, ABT-518, ABT-627 (atrasentan), testosterone, progesterone, indomethacin, phenyl salicylate, ⁇ -est
- the system of the present invention may be used in a method for improving patency in a subject involving placement of a medical device in a body lumen for treating and/or preventing adjacent diseases or maintaining patency of the body lumen including: providing a medical device in a body lumen, providing a first lipophilic agent capable of penetrating a body lumen, wherein the transfer coefficient of the first lipophilic agent is at least 5,000 ( ⁇ g/mL) -1 , wherein the first lipophilic agent is associated with the medical device, placing the first lipophilic agent/medical device adjacent to a body lumen, and delivering a therapeutically effective amount of the first lipophilic agent to a desired area within a subject.
- Yet another aspect of the invention relates to a medical device, comprising: a therapeutically effective amount of a first lipophilic agent, which is associated with said medical device and capable of penetrating a body lumen, and which is zotarolimus having the structures as follows: and a beneficial agent selected from the group consisting of nifedipine, diltiazem, nicardipine, verapamil, nadolol, metoprolol, propranolol, atenolol, esmolol, nitroglycerin, isosorbide dinitrate, carvedilol, digitalis, levosimendan, batimistat, prinomastat, marimistat, ABT-518, ABT-627 (atrasentan), testosterone, progesterone, indomethacin, phenyl salicylate, ⁇ -estradiol, vindesine, dipyridamole, methotrexate, metrizamide,
- Still yet another aspect of the invention relates to a stent, comprising: a therapeutically effective amount of a first lipophilic agent, which is associated with the stent, and capable of penetrating a body lumen, and which is zotarolimus having the structures as follows: and a beneficial agent selected from the group consisting of nifedipine, diltiazem, nicardipine, verapamil, nadolol, metoprolol, propranolol, atenolol, esmolol, nitroglycerin, isosorbide dinitrate, carvedilol, digitalis, levosimendan, batimistat, prinomastat, marimistat, ABT-518, ABT-627 (atrasentan), testosterone, progesterone, indomethacin, phenyl salicylate, ⁇ -estradiol, vindesine, dipyridamole, methotrexate, metri
- agent as used herein is synonymous with “at least one agent,” “compound,” or “at least one compound,” and means at least one drug or codrug, or a prodrug thereof.
- beneficial agent means agents that exert a therapeutically beneficial effect when delivered from suitable medical devices.
- the beneficial agent can be a polymer, a marker, such as a radiopaque dye or particles, or can be a drag, including pharmaceutical and therapeutic agents, or an agent including inorganic or organic drugs without limitation.
- the agent or drug can be in various forms such as uncharged molecules, components of molecular complexes, pharmacologically-acceptable salts such as hydrochloride, hydrobromide, sulfate, laurate, palmitate, phosphate, nitrate, borate, acetate, maleate, tartrate, oleate, and salicylate.
- pharmacologically-acceptable salts such as hydrochloride, hydrobromide, sulfate, laurate, palmitate, phosphate, nitrate, borate, acetate, maleate, tartrate, oleate, and salicylate.
- An agent or drug that is water insoluble can be used in a form that is a water-soluble derivative thereof to effectively serve as a solute, and on its release from the device, is converted by enzymes, hydrolyzed by body pH, or metabolic processes to a biologically active form.
- the agents or drug formulations can have various known forms such as solutions, dispersions, pastes, particles, granules, emulsions, suspensions and powders.
- the drug or agent may or may not be mixed with polymer or a solvent as desired.
- the drug or agent can include antithrombotics, anticoagulants, antiplatelet agents, thrombolytics, antiproliferatives, anti-inflammatories, agents that inhibit hyperplasia, inhibitors of smooth muscle proliferation, antibiotics, growth factor inhibitors, or cell adhesion inhibitors.
- drugs or agents include but are not limited to antineoplastics, antimitotics, antifibrins, antioxidants, agents that promote endothelial cell recovery, antiallergic substances, radiopaque agents, viral vectors, antisense compounds, oligionucleotides, cell permeation enhancers, cell adhesion promoters, nucleic acids, monoclonal antibodies, hypogylycemic agents, hypolipidemic agents, proteins, agents useful for erythropoiesis stimulation, angiogenesis agents, and combinations thereof.
- antithrombotics examples include sodium heparin, low molecular weight heparins, heparinoids, hirudin, argatroban, forskolin, vapriprost, prostacyclin and prostacylin analogues, dextran, D-phe-pro-arg-chloromethylketone (synthetic antithrombin), dipyridamole, glycoprotein IIb/IIIa - (platelet membrane receptor antagonist antibody), recombinant hirudin, and thrombin inhibitors such as AngiomaxTM, from Biogen, Inc., Cambridge, Mass; and thrombolytic agents, such as urokinase, e.g., AbbokinaseTM from Abbott Laboratories Inc., North Chicago, IL, recombinant urokinase and pro-urokinase from Abbott Laboratories Inc., tissue plasminogen activator (Alte
- cytostatic or antiproliferative agents include rapamycin and its analogs including everolimus, zotarolimus, i.e., 3S,6R,7E,9R,10R,12R,14S,15E,17E,19E,21S, 23S,26R,27R,34aS)-9,10,12,13,14,21,22,23,24,25,26,27,32,33,34,34a-Hexadecahydro-9,27-dihydroxy-3-[(1R)-2-[(1S,3R,4R)-3-methoxy-4-tetrazol-1-yl)cyclohexyl]-1-methylethyl]-10,21-dimethoxy-6,8,12,14,20,26-hexamethyl-23,27-epoxy-3H-pyrido[2,1-c][1,4]oxaazacyclohentriacontine-1,5,11,28,29(4H,
- Mevacor® from Merck & Co., Inc., Whitehouse Station, NJ.
- topoisomerase inhibitors such as etoposide and topotecan, as well as antiestrogens such as tamoxifen may be used.
- anti-inflammatories examples include colchicine and glucocorticoids such as betamethasone, cortisone, dexamethasone, budesonide, prednisolone, methylprednisolone and hydrocortisone.
- Non-steroidal anti-inflammatory agents include flurbiprofen, ibuprofen, ketoprofen, fenoprofen, naproxen, diclofenac, diflunisal, acetominophen, indomethacin, sulindac, etodolac, diclofenac, ketorolac, meclofenamic acid, piroxicam and phenylbutazone.
- antineoplastics examples include alkylating agents including altretamine, bendamucine, carboplatin, carmustine, cisplatin, cyclophosphamide, fotemustine, ifosfamide, lomustine, nimustine, prednimustine, and treosulfin, antimitotics including vincristine, vinblastine, paclitaxel, e.g., TAXOL® by Bristol-Myers Squibb Co., Stamford, Conn., docetaxel, e.g., Taxotere® from Aventis S.A., Frankfort, Germany, antimetabolites including methotrexate, mercaptopurine, pentostatin, trimetrexate, gemcitabine, azathioprine, and fluorouracil, and antibiotics such as doxorubicin hydrochloride, e.g., Adriamycin® from Pharmacia & Upjohn, Peapack, NJ, and
- Additional drugs which may be utilized in this application include inhibitors of tyrosine kinase such as RPR-101511A, PPAR-alpha agonists such as TricorTM (fenofibrate) from Abbott Laboratories Inc., North Chicago, IL, endothelin receptor antagonists including astrasentan (ABT-627) having general formula C 29 H 38 N 2 O 6 .ClH, and the following structural formula from Abbott Laboratories Inc., North Chicago, IL, matrix metalloproteinase inhibitors such as ABT-518 having general formula C 21 H 22 F 3 NO 8 S and having the following structural formula from Abbott Laboratories Inc., North Chicago, IL, antiallergic agents such as permirolast potassium nitroprusside, phosphodiesterase inhibitors, prostaglandin inhibitors, suramin, serotonin blockers, steroids, thioprotease inhibitors, triazolopyrimidine, and nitric oxide.
- tyrosine kinase such as R
- biocompatible and “biocompatibility” when used herein are art-recognized and mean that the referent is neither itself toxic to a host (e.g., an animal or human), nor degrades (if it degrades) at a rate that produces byproducts (e.g., monomeric or oligomeric subunits or other byproducts) at toxic concentrations, causes inflammation or irritation, or induces an immune reaction, in the host. It is not necessary that any subject composition have a purity of 100% to be deemed biocompatible.
- a subject composition may comprise 99%, 98%, 97%, 96%, 95%, 90% 85%, 80%, 75% or even less of biocompatible agents, e.g., including polymers and other materials and excipients described herein, and still be biocompatible.
- biocompatible agents e.g., including polymers and other materials and excipients described herein, and still be biocompatible.
- preventing is art-recognized, and when used in relation to a condition, including a local recurrence (e.g., pain), a disease including cancer, a syndrome complex including heart failure or any other medical condition, is well understood in the art, and includes administration of a composition which reduces the frequency of, or delays the onset of, symptoms of a medical condition in a subject relative to a subject which does not receive the composition.
- a condition including a local recurrence (e.g., pain)
- a disease including cancer
- a syndrome complex including heart failure or any other medical condition
- prevention of cancer includes, for example, reducing the number of detectable cancerous growths in a population of patients receiving a prophylactic treatment relative to an untreated control population, and/or delaying the appearance of detectable cancerous growths in a treated population versus an untreated control population, e.g., by a statistically and/or clinically significant amount.
- Prevention of an infection includes, for example, reducing the number of diagnoses of the infection in a treated population versus an untreated control population, and/or delaying the onset of symptoms of the infection in a treated population versus an untreated control population.
- Prevention of pain includes, for example, reducing the magnitude of, or alternatively delaying, pain sensations experienced by subjects in a treated population versus an untreated control population.
- polymer is intended to include a product of a polymerization reaction inclusive of homopolymers, copolymers, terpolymers, etc., whether natural or synthetic, including random, alternating, block, graft, branched, cross-linked, blends, compositions of blends and variations thereof
- the polymer may be in true solution, saturated, or suspended as particles or supersaturated in the beneficial agent.
- the polymer can be biocompatible, or biodegradable.
- the polymeric material include phosphorylcholine linked macromolecules, including a macromolecule containing pendant phosphorylcholine groups such as poly(MPC.sub.w:LMA.sub.x:HPMA.sub.y:TSMA.sub.z), where MPC is 2-methacryoyloxyethylphosphorylcholine, LMA is lauryl methacrylate, HPMA is hydroxypropyl methacrylate and TSMA is trimethoxysilylpropyl methacrylate, polycaprolactone, poly-D,L-lactic acid, poly-L-lactic acid, poly(lactide-co-glycolide), poly(hydroxybutyrate), poly(hydroxybutyrate-co-valerate), polydioxanone, polyorthoester, polyanhydride, poly(glycolic acid), poly(glycolic acid-co-trimethylene carbonate), polyphosphoester, polyphosphoester urethane, poly(amino acids),
- Non-limiting examples of other suitable polymers include thermoplastic elastomers in general, polyolefin elastomers, EPDM rubbers and polyamide elastomers, and biostable plastic material including acrylic polymers, and its derivatives, nylon, polyesters and expoxies.
- Other polymers include pendant phosphoryl groups as disclosed in U.S. Pat. Nos. 5,705,583 and 6,090,901 to Bowers et al. and U.S. Pat. No. 6,083,257 to Taylor et al. , and U.S. Pat. Nos. 5,705,583 and 6,090,901 teach phosphorylcholine polymers (including PC-1036 and PC-2126).
- pro-drug refers to compounds, which are transformed in vivo to the parent compound of the formula above, for example, by hydrolysis in blood.
- a thorough discussion is provided by T. Higuchi and V. Stella, "Pro-drugs as Novel Delivery systems,” Vol. 14 of the A.C.S. symposium Series , and in Edward B. Roche, ed., "Bioreversible Carriers in Drug Design.” American Pharmaceutical Association and Pergamon Press, 1987 ,
- subject refers to any warm-blooded animal and mammals including, but not limited to, humans, pigs, dogs, monkeys, cows, goats, sheep, horses, rats, mice, and guinea pigs.
- treating includes preventing a disease, disorder or condition from occurring in an animal which may be predisposed to the disease, disorder and/or condition but has not yet been diagnosed as having it; inhibiting the disease, disorder or condition, e.g., impeding its progress; and relieving the disease, disorder, or condition, e.g., causing regression of the disease, disorder and/or condition.
- Treating the disease or condition includes ameliorating at least one symptom of the particular disease or condition, even if the underlying pathophysiology is not affected, such as treating the pain of a subject by administration of an analgesic agent even though such agent does not treat the cause of the pain.
- Solubility is based on a standard measure used in medicinal chemistry.
- the octanol-water partition coefficient (P) is the ratio of distribution of a compound in a mixture of 1-octanol and H 2 O.
- LogP is the base 10 logarithm of the partition coefficient.
- P C ⁇ n - octanol C water
- the shake-flask method was used in both the solubility and partition coefficient studies. Preliminary analyses were conducted to evaluate the optimum conditions for both methods.
- For the partition coefficient methodology drug was dissolved in an organic phase (n-octanol), followed by the addition of buffered water to extract the drug from the organic phase. Ultimately, the drug concentrations in both phases reach an equilibrium determined by the partition coefficient of the drug compound.
- For solubility testing an initial evaluation was conducted to ensure full separation of drug particles from the saturated solution, and to avoid adsorption of drug by the experimental apparatus. The measurements were performed at multiple equilibration times (from 2 hours up to 5 days). Concentrations of all drug compounds were assayed by validated HPLC methods.
- Drug delivery in DES ideally occurs with predominate tissue uptake, however, drug also partitions into the blood. Consequently, high aqueous solubility may have a negative impact on local drug bioavailability. It has been determined by the above tests that lipophilicity and solubility are controlling factors in DES drug delivery.
- DES drugs While most drug-eluting stents have amorphous drugs mixed in a polymer matrix, the bulk DES drug exists in either amorphous or crystalline forms. Therefore, solubility data on DES drugs was investigated for both the amorphous and crystalline forms. It was found that rapamycin can be either amorphous or crystalline, zotarolimus is amorphous, and paclitaxel has two crystal forms. Aqueous solubility of amorphous DES drugs follow the increasing order: paclitaxel, zotarolimus, rapamycin, and dexamethasone (crystalline).
- a transfer coefficient, ⁇ can be defined as P divided by S, where P equals the partition coefficient and S equals theequilibrium aqueous solubility, ( ⁇ g/ml) as shown in Fig 21 .
- the aspects of the invention further include at least one pharmaceutically acceptable carrier or excipient, wherein the medical device is associated with the pharmaceutically acceptable carrier or excipient.
- the pharmaceutically acceptable carrier or excipient is a polymer.
- the delivery mechanism of the first lipophilic agent includes polymer hydration followed by dissolution of the first lipophilic agent, and wherein the first lipophilic agent is thereafter delivered into the body lumen.
- Another delivery mechanism includes the first lipophilic agent/polymer matrix controlling the elution rate of the first lipophilic agent to the body lumen.
- Embodiments of the invention further include at least one of the following: at least one second lipophilic agent, at least one lipophilic prodrug, at least one beneficial agent, at least one lipophilic penetration enhancer, and any combination thereof.
- the enhancer is a pharmaceutical agent.
- a further embodiment of the invention is to provide drug delivery to the myocardial wall to reduce the area or extent of ischemic or infarcted cardiac tissue.
- agents to be used for this purpose include, but are not limited to, calcium channel blockers (nifedipine, diltiazem, nicardipine and verapamil), beta-adrenergic blocking agents (nadolol, metoprolol, propranolol, atenolol and esmolol) and nitrates (nitroglycerin and isosorbide dinitrate).
- Yet another embodiment of the invention is to deliver drug to hypokinetic or akinetic regions of the myocardial wall to improve contractility of the cardiac muscle in the treatment of heart failure.
- Drug examples include, but are not limited to carvedilol, an adrenergic antagonist with nonselective beta- and al-receptor blocking properties, cardiac glycosides such as digitalis, and calcium sensitizers such as levosimendan. Delivery of agents to stabilize vulnerable plaque, such as inhibitors of matrix metalloproteinases (batimistat, prinomastat, marimistat and ABT- . 518) or the macrolide antibiotic azithromycin, may also be delivered. To maintain patency of body lumens including, but not limited to, the urethra, the delivery of chemotherapeutic agents such as alkylating agents and antimetabolites may be utilized.
- chemotherapeutic agents such as alkylating agents and antimetabolites
- the first lipophilic agent and/or second lipophilic agent zotarolimus has the structures as follows.
- the body lumen in the application includes, but is not limited to, a vessel wall, either arterial or venous.
- the body lumen includes, but is not limited to, at least one of a vessel wall, a coronary artery, esophageal lumen, or a urethra.
- the first lipophilic agent/medical device is placed adjacent to a body lumen (coronary arteries) and a therapeutically effective amount of the first lipophilic agent is delivered into said coronary arteries and is diffused into the pericardial sac in a drug delivery system.
- the invention provides for substantially uniform dug delivery of the lipophilic agent to the myocardium and/or is useful for the treatment and/or prevention of vascular diseases in a subject.
- the lipophilic agent is continuously delivered to the epicardium and/or pericardial sac.
- Embodiments of the first lipophilic agent includes agents with partition coefficients greater than 20,000.
- the first lipophilic agent includes transfer coefficients of at least 10,000 ( ⁇ g/mL) -1 .
- the first lipophilic agent includes transfer coefficient of at least 15,000 ( ⁇ g/mL) -1 .
- Embodiments of the first lipophilic agent include compounds having LogP of at least 4.3, as shown in Fig. 24 .
- the first lipophilic agent includes partition coefficient greater than 20,000 P and the lipophilic agent includes a solubility of less than 30 ug/ml.
- the first lipophilic agent is amorphous.
- Fig. 22 is a rabbit study comparing the drug concentration in rabbit tissue by drug elution from the ZoMaxxTM stent vs. the Cypher ® stent.
- the dosage delivery of the first lipophilic agent into the vascular tissue ranges from 15 ⁇ g/g to 150 ⁇ g/g over a period of up to 5 days. In other embodiments, the dosage delivery of the first lipophilic agent into the vascular tissue ranges from 15 ⁇ g/g to 80 ⁇ g/g over a period from 5 to up to 15 days. At no time points between 0 and 15 days, the comparator Cypher ® stent reaches concentrations of rapamycin higher than 10 ⁇ g/g.
- the dosage delivery of the first lipophilic agent into the vascular tissue ranges from 5 ⁇ g/g to 60 ⁇ g/g over from 15 to up to 28 days. Still in other embodiments, the dosage delivery of the first lipophilic agent is always greater than 5 times the dose delivery of the comparative Cypher ® stent at the 28 day point
- Fig. 23 is a from the same rabbit study comparing the drug levels in rabbit blood for ZoMaxxTM stent vs. Cypher ® stent
- the blood levels of rapamycin eluted from the Cypher ® stents are consistently significantly higher than the blood levels of zotarolimus eluted from the ZoMaxxTM stents.
- Fig. 25 is a graph demonstrating blood, liver, kidney, artery and myocardial concentrations of zotarolimus eluted from ZoMaxxTM stents in a pig model Zotarolimus is delivered in substantial concentrations to the arterial tissue adjacent to the stent placement at all periods out to 28 days. Unexpectedly, zotarolimus also reaches therapeutically significant concentrations in the distal myocardium, the unstent myocardium, and in the subjacent myocardium and in unstented and distal coronary arteries and maintains those concentrations throughout the 28 day course of the experiment.
- the medical device includes, but is not limited to, an endovascular medical device.
- the medical device includes intracoronary medical devices including at least one of stents, drug delivery catheters, grafts, and drug delivery balloons utilized in a subjects' vasculature.
- the stent includes peripheral stents, peripheral coronary stents, degradable coronary stents, nondegradable coronary stents, self-expanding stents, balloon-expanded stents, and esophageal stents.
- the medical device includes at least one of, but is not limited to, arterio-venous grafts, by-pass grafts, penile implants, vascular implants and grafts, intravenous catheters, small diameter grafts, artificial lung catheters, electrophysiology catheters, bone pins, suture anchors, blood pressure and stent graft catheters, breast implants, benign prostatic hyperplasia and prostate cancer implants, bone repair/augmentation devices, breast implants, orthopedic joint implants, dental implants, implanted drug infusion tubes, oncological implants, pain management implants, neurological catheters, central venous access catheters, catheter cuff, vascular access catheters, urological catheters/implants, atherectomy catheters, clot extraction catheters, PTA catheters, PTCA catheters, stylets (vascular and non-vascular), drug infusion catheters, angiographic catheters, hemodialysis catheters, neurovascular balloon catheters, thoracic cavity suction drainage catheters, electrophysiology catheters, stroke therapy
- the medical device includes at least one of, but is not limited to, either arterial or venous, pacemakers, vascular grafts, sphincter devices, urethral devices, bladder devices, renal devices, gastroenteral and anastomotic devices, vertebral disks, hemostatic barriers, clamps, surgical staples/sutures/screws/plates/wires/clips, glucose sensors, blood oxygenator tubing, blood oxygenator membranes, blood bags, birth control/IUDs and associated pregnancy control devices, cartilage repair devices, orthopedic fracture repairs, tissue adhesives, tissue sealants, tissue scaffolds, CSF shunts, dental fracture repair devices, intravitreal drug delivery devices, nerve regeneration conduits, electrostimulation leads, spinal/orthopedic repair devices, wound dressings, embolic protection filters, abdominal aortic aneurysm grafts and devices, neuro aneurysm treatment coils, hemodialysis devices, uterine bleeding patches, anastomotic closures, in vitro
- the first lipophilic agent/medical device is placed adjacent to a body lumen (arteries, veins or grafts) and a therapeutically effective amount of the first lipophilic agent is delivered into said arteries, veins or grafts and is diffused into the pericardial sac in a drug delivery system.
- the invention provides for substantially uniform dug delivery of the lipophilic agent to the myocardium and/or is useful for the treatment and/or prevention of vascular diseases in a subject.
- the medical device is permanently or temporarily implanted into a subject.
- a medical device having an interventional component that is loaded with a beneficial agent that is associated with a hydration inhibitor to control the delivery of the beneficial agent in a patient.
- medical device refers broadly to any device that is deployed in a patient.
- the invention is directed to a medical device having controlled delivery of a beneficial agent for the treatment and prevention of cardio, vascular or other intraluminal diseases.
- the medical device is suitable for intraluminal delivery or implantation.
- such devices can comprise one or more interventional components.
- medical devices include stents, grafts, stent-grafts, valves, filters, coils, staples, sutures, guidewires, catheters, catheter balloons, and the like.
- the interventional component is an interventional component having a first cross-sectional dimension for the purpose of delivery and a second cross-sectional dimension after deployment and can be deployed by known mechanical techniques including balloon expansion deployment techniques, or by electrical or thermal actuation, or self-expansion deployment techniques, as well known in the art.
- a stent, stent-graft or similar interventional component are disclosed in U.S. Patent No. 4,733,665 to Palmaz ; U.S. Patent No. 6,106,548 to Roubin et al. ; U.S. Patent No. 4,580,568 to Gianturco ; U.S. Patent No. 5,755,771 to Penn et al. ; and U.S. Patent No. 6,033,434 to Borghi .
- the interventional component can be any type of implantable or deployable interventional component capable of being loaded with beneficial agent.
- the interventional component can be in an expanded or unexpanded state during the loading of beneficial agent.
- the underlying structure of the interventional component can be virtually any construction and the interventional component can be composed any suitable material including, but not limited to, stainless steel, "MP35N,” “MP20N,” elastinite (Nitinol), tantalum, nickel-titanium alloy, platinum-iridium alloy, chromium-cobalt alloy, gold, magnesium, polymer, ceramic, tissue, or combinations thereof.
- MP35N and “MP20N” are understood to be trade names for alloys of cobalt, nickel, chromium and molybdenum available from Standard Press Steel Co., Jenkintown, PA.
- the interventional component can be made from bioabsorbable or biostable polymers.
- the surface of the interventional component is porous or impervious, or include one or more reservoirs or cavitics formed therein for purpose of retaining beneficial agent therein as is known in the art.
- the interventional component can be fabricated utilizing any number of methods known in the art.
- the interventional component can be fabricated from a hollow or formed tube that is machined using lasers, electric discharge milling, chemical etching or other known techniques.
- the interventional component can be fabricated from a sheet or formed of a wire or filament construction as know in the art.
- the interventional component is loaded with beneficial agent to be delivered therefrom when deployed within the patient
- beneficial agent generally refers to any compound, mixture of compounds, or composition of matter consisting of a compound, which produces a beneficial or useful result in a patient.
- the beneficial agent has a first LogP value.
- P is the calculated partition coefficient of a chemical substance, which is a measure of the way in which a compound will partition itself between the octanol and water phases in the two-phase octanol-water system, and thus an indicator of certain types of biological activity.
- P is the ratio of the concentration (in moles per liter) of the compound in the octanol phase to that in the water phase at infinite dilution.
- the solubility is usually expressed as base 10 logarithm of the partition coefficient, LogP.
- LogP and methods for calculating it are well known to those skilled in the art.
- the LogP value can be calculated by the method described in ( Hansch C. and Leo A.
- LogP is a widely used parameter for correlating biological effects of organic substances. It is a property of the two-phase system in which water and 1-octanol are in equilibrium at a fixed temperature and the substance is distributed between the water-rich and octanol-rich phases. Generally, the greater the LogP value of a compound or agent, the less hydrophilic the compound or agent. It also has been determined that a compound or agent having a greater LogP value (i.e., a "relatively less hydrophilic agent”) will inhibit hydration of the second compound or agent having a lower LogP value (i.e., a "relatively more hydrophilic agent").
- a relatively less hydrophilic agent can be used as a hydration inhibitor for a relatively more hydrophilic beneficial agent, which is to be delivered from an interventional component as a beneficial agent, wherein the hydration inhibitor has a LogP value that is greater than the LogP value of the beneficial agent
- the LogP value of the hydration inhibitor is at least 0.1 units greater than the beneficial agent and at least 0.5 units greater than the beneficial agent.
- the LogP value of the beneficial agent is less than 4.5 units, and more preferably it is less than 3.0 units. See “ CRC Handbook of Chemistry and Physics," 3rd Electronic Edition, 2000 .
- a compound to serve as a hydration inhibitor of the elution of a given beneficial agent according to embodiments of the invention when the beneficial agent's LogP value is less than that of the given hydration inhibitor.
- the beneficial agent's LogP value is less than that of the given hydration inhibitor.
- suitable beneficial agents for delivery of an interventional component are well known.
- various suitable beneficial agents having a LogP value include markers, such as, for example, a radiopaque dyes or particles, drugs, such as, for example, pharmaceutical and therapeutic agents, and inorganic or organic drugs without limitation.
- the agent or drug can be in various forms, components of molecular complexes, pharmacologically-acceptable salts such as hydrochloride, hydrobromide, sulfate, phosphate, nitrate, borate, acetate, maleate, tartrate and salicylate.
- the drug or agent includes antithrombotics, anticoagulants, antiplatelet agents, anti-lipid agents, thrombolytics, antiproliferatives, anti-inflammatories, agents that inhibit hyperplasia, smooth muscle cell inhibitors, antibiotics, growth factor inhibitors, cell adhesion inhibitors, cell adhesion promoters, antimitotics, antifibrins, antioxidants, antineoplastics, agents that promote endothelial cell recovery, antiallergic substances, viral vectors, nucleic acids, monoclonal antibodies, antisense compounds, oligionucleotides, cell permeation enhancers, pro-drugs and combinations thereof.
- beneficial agents include but are not limited to nucleic acids that encode a pharmaceutically useful peptide or an anti-sense oligo-nucleotide used to control a gene of interest in a cell.
- Examples of specific beneficial agents of interest include indomethacin, phenyl salicylate, ⁇ -estradiol, vinblastine, ABT-627 (atrasentan), testosterone, progesterone, paclitaxel, cyclosporin A, vincristine, carvedilol, vindesine, dipyridamole, methotrexate, folic acid, thrombospondin mimetics, estradiol, dexamethasone, metrizamide, iopamidol, iohexol, iopromide, iobitridol, iomeprol, iopentol, ioversol, ioxilan, iodixanol, iotrolan and pro-drugs, analogs, derivatives, or combinations thereof.
- Beneficial agents can have various art known forms including solutions, dispersions, pastes, particles, granules, emulsions, suspensions and powders.
- the beneficial agent typically is associated with the hydration inhibitor as a mixture, although can be associated as a separate application, including an overcoat or layer when a beneficial agent is used as the hydration inhibitor as disclosed further below.
- beneficial agents are well known for their preventive and treatment properties, the substances or agents are provided by way of example and not limitation. Further, other beneficial agents with suitable LogP values that are currently available or can be developed are equally applicable for use with the invention.
- an effective amount of hydration inhibitor is associated with the beneficial agent to be delivered from the interventional component so as to control delivery therefrom.
- the term "hydration inhibitor" as used herein refers to a suitable compound or agent or the like having a LogP value greater than that of the beneficial agent.
- the hydration inhibitor is thus relatively less hydrophilic than the beneficial agent, and controls delivery of the beneficial agent by retarding, inhibiting or otherwise sustaining the rate in which the beneficial agent would be delivered from the interventional component without the hydration inhibitor associated therewith. Delivery of the beneficial agent from the interventional component occurs by any of a variety of know mechanisms, including elution, diffusion, dissolution, permeation or other transport mechanisms in vivo.
- an effective amount of hydration inhibitor refers to an amount sufficient to inhibit hydration of the beneficial agent to be delivered from the interventional component. For example, it is well known to determine hydration as a measure of optical contact angle, wherein a contact angle of about 30° is indicative of a hydrophilic compound and a contact angle of greater than about 50° is indicative of a hydrophobic compound. Optical contact angle and methods for calculating it are well known to those skilled in the art using standard evaluation methods and is disclosed in " McGraw-Hill Encyclopedia of Chemistry," 538 (Sybil P. Parker, 2nd ed. 1993 ) and “ Remington's Pharmaceutical Sciences," 256-7 and 294-5 (Arthur Osol et al. eds., 16th ed. 1980 ). As such, an effective amount of hydration inhibitor is recognized to be a sufficient amount to shift the optical contact angle of the beneficial agent in association with the hydration inhibitor to at least about 50° and to at least about 70°.
- the hydration inhibitor includes beneficial agents (including markers), polymeric materials, additives and combinations thereof.
- beneficial agents including markers
- polymeric materials including markers
- additives and combinations thereof include additives and combinations thereof.
- the LogP value of the second beneficial agent must be greater than the LogP value of the first beneficial agent.
- beneficial agent hydration inhibitors include antioxidants, antithrombotics, anticoagulants, antiplatelet agents, anti-lipid agents, thrombolytics, antiproliferatives, anti-inflammatories, agents that inhibit hyperplasia, smooth muscle cell inhibitors, antibiotics, growth factor inhibitors, cell adhesion inhibitors, cell adhesion promoters, antimitotics, antifibrins, antioxidants, antineoplastics, agents that promote endothelial cell recovery, antiallergic substances, viral vectors, nucleic acids, monoclonal antibodies, antisense compounds, oligionucleotides, cell permeation enhancers, radiopaque agents markers and combinations thereof.
- Non-limiting examples of specific beneficial agent useful as hydration inhibitors include paclitaxel, rapamycin, rapamycin derivatives, pimecrolimus, everolimus, fenofibrate, carvedilol, taxoteres, tacrolimus, butylated hydroxytoluene, butylated hydroxyanisole, vitamin E, danazol, probucol, tocopherols, tocotrienols, zotarolimus, ABT-627 and analogs, derivatives, or combinations thereof.
- ABT-627 and the chemical structure of zotarolimus is A detailed discussion of ABT-627 (atrasentan) is available in PCT/US02/28776, filed September 10, 2002 , and zotarolimus in U.S. Patent Nos. 6,015,815 and 6,329,386 .
- the hydration inhibitor is associated with the beneficial agent as a nurture
- the hydration inhibitor can be associated as an overcoat or encapsulating layer covering at least a portion of the first beneficial agent.
- Polymeric materials suitable as hydration inhibitors are typically a product of a polymerization reaction inclusive of homopolymers, copolymers, terpolymers, etc., whether natural or synthetic, including random, alternating, block, graft, branched, cross-linked, blends, compositions of blends and variations thereof.
- the polymer can be in true solution, saturated, or suspended as particles or supersaturated in the beneficial agent.
- the polymer is biocompatible, and can be biodegradable.
- polymeric materials include phosphorylcholine, polycaprolactone, poly-D,L-lactic acid, poly-L-lactic acid, poly(lactide-co-glycolide), poly(hydroxybutyrate), poly(hydroxybutyrate-co-valerate), polydioxanone, polyorthoester, polyanhydride, poly(glycolic acid), poly(glycolic acid-co-trimethylene carbonate), polyphosphoester, polyhosphoester urethane, poly(amino acids), cyanoacrylates, poly(trimethylene carbonate), poly(iminocarbonate), polyalkylene oxalates, polyphosphazenes, polyiminocarbonates, and aliphatic polycarbonates, fibrin, fibrinogen, cellulose, starch, collagen, Parylene®, Parylast®, polyurethane, polycarbonate urethanes, polyethylene, polyethylene terapthalate, ethylene vinyl acetate, ethylene vinyl alcohol, silicone polys
- the polymeric material has a zwitterionic pendant group.
- the polymer is phosphorylcholine disclosed in U.S. Patent Nos. 5,705,583 and 6,090,901 to Bowers et al. and U.S. Patent No. 6,083,257 to Taylor et al ,.
- the beneficial agent can include a beneficial agent and polymer mixture.
- the first beneficial agent can correspond to a beneficial agent-polymer mixture having a concentration of polymer to effect the delivery rate of the particular beneficial agent in the beneficial agent mixture.
- a beneficial agent-polymer mixture having a higher concentration of polymer would have a slower delivery rate of the beneficial agent within the lumen.
- a beneficial agent-polymer mixture having a lower concentration of polymer would cause a more rapid delivery rate of the beneficial agent.
- the delivery rate is also effected by the difference between the LogP value of the hydration inhibitor and the LogP value of the beneficial agent. For example, generally the greater the difference between the LogP values the greater the retardation of the beneficial agent's delivery rate as compared to the beneficial agent without hydration inhibitor.
- additives suitable as hydration inhibitors include plasticizers, small molecules and oils. Additives are drawn from compounds, polymers, and mixtures without restriction. When used with an interventional device having a polymer coating, an additive is often capable of dispersing through the polymer coating and rendering it effectively more difficult to hydrate as empirically defined as an increase in swelling time in contact with aqueous solution vs. control polymer coating.
- additives include nitrophenyl octyl ether, bisethylhexyl sebacate, diisododecylphthalate, N-methylpyrrolidone, linolenic acid, linoleic acid, stearic acid, oleic acid, and combinations thereof.
- the hydration inhibitor can be associated with the beneficial agent in any of a variety of conventional techniques. As embodied herein, and as previously noted, it is to associate the hydration inhibitor with the beneficial agent as a mixture of the compounds. The mixture can be accomplished by a physical combination in a variety of forms, including solution, suspension, solid interspersion, vapor phase deposition or any physical combination.
- An additional aspect of the invention includes the use of a base layer of polymer material to facilitate loading of a beneficial agent on the interventional component. This aspect of the invention is of particular importance if the beneficial agent is difficult or unsuitable for loading alone or in combination with a suitable binder or the like.
- the coating can include any polymeric material in which the therapeutic agent, i.e., the drug, is substantially soluble.
- the purpose of the coating is to serve as a controlled release vehicle for the therapeutic agent or as a reservoir for a therapeutic agent to be delivered at the site of a lesion.
- the coating can be polymeric and can further be hydrophilic, hydrophobic, biodegradable, or non-biodegradable.
- the material for the polymeric coating can be selected from the group consisting of polycarboxylic acids, cellulosic polymers, gelatin, polyvinylpyrrolidone, maleic anhydride polymers, polyamides, polyvinyl alcohols, polyethylene oxides, glycosaminoglycans, polysaccharides, polyesters, polyurethanes, silicones, polyorthoesters, polyanhydrides, polycarbonates, polypropylenes, polylactic acids, polyglycolic acids, polycaprolactones, polyhydroxybutyrate valerates, polyacrylamides, polyethers, and mixtures and copolymers of the foregoing.
- Coatings prepared from polymeric dispersions including polyurethane dispersions (BAYHYDROL, etc.) and acrylic acid latex dispersions can also be used with the therapeutic agents of embodiments of the invention.
- Biodegradable polymers that can be used in this invention include polymers including poly(L-lactic acid), poly(DL-lactic acid), polycaprolactone, poly(hydroxy butyrate), polyglycolide, poly(diaxanone), poly(hydroxy valerate), polyorthoester; copolymers including poly (lactide-co-glycolide), polyhydroxy (butyrate-co-valerate), polyglycolide-co-trimethylene carbonate; polyanhydrides; polyphosphoester; polyphosphoester-urethane; polyamino acids; polycyanoacrylates; biomolecules including fibrin, fibrinogen, cellulose, starch, collagen and hyaluronic acid; and mixtures of the foregoing.
- Biostable materials that are suitable for use in this invention include polymers include polyurethane, silicones, polyesters, polyolefins, polyamides, polycaprolactam, polyimide, polyvinyl chloride, polyvinyl methyl ether, polyvinyl alcohol, acrylic polymers and copolymers, polyacrylonitrile, polystyrene copolymers of vinyl monomers with olefins (including styrene acrylonitrile copolymers, ethylene methyl methacrylate copolymers, ethylene vinyl acetate), polyethers, rayons, cellulosics (including cellulose acetate, cellulose nitrate, cellulose propionate, etc.), parylene and derivatives thereof; and mixtures and copolymers of the foregoing.
- polymers include polyurethane, silicones, polyesters, polyolefins, polyamides, polycaprolactam, polyimide, polyvinyl chloride, polyvinyl methyl
- a medical devices to which coatings are applied according to the invention can be pretreated to prepare the surfaces for application of coatings.
- stainless steel stents may be electropolished prior to coating (e.g., undercoat) application.
- Useful medical devices can be formed from NITINOL alloy, TRIPLEX (stainless steel/tantalum/stainless steel layer) or cobalt chromium alloy.
- the coatings optionally include a polymeric material, e.g., phosphorylcholine, polycaprolactone, poly-D,L-lactic acid, poly-L-lactic acid, poly(lactide-co-glycolide), poly(hydroxybutyrate), poly(hydroxybutyrate-co-valerate), polydioxanone, polyorthoester, polyanhydride, poly(glycolic acid), poly(glycolic acid-co-trimethylene carbonate), polyphosphoester, polyphosphoester urethane, poly(amino acids), cyanoacrylates, poly(trimethylene carbonate), poly(iminocarbonate), polyalkylene oxalates, polyphosphazenes, polyiminocarbonates, and aliphatic polycarbonates, fibrin, fibrinogen, cellulose, starch, collagen, Parylene® brand poly-para-xylylene (available from SCSCookson Industries, Indianapolis, Indiana), Paryl ASTTM brand biocompatible dielectric polymer
- Patent Nos. 5,355,832 and 5,447,799 commercially available from AST Products of Billerica, MA); polyurethane, polycarbonate urethanes, polyethylene, polyethylene terephthalate, ethylene vinyl acetate, ethylene vinyl alcohol, silicone polysiloxanes, substituted polysiloxanes, polyethylene oxide, polybutylene terephthalate-co-PEG, PCL-co-PEG (i.e., polycaprolactone co-polyethylene glycol), PLA-co-PEG (i.e., polylactic acid-co-polyethylene glycol), polyacrylates, polyvinyl pyrrolidone, polyacrylamide, thermoplastic elastomers, polyolefin elastomers, EPDM rubbers, polyamide elastomers, biostable plastic, acrylic polymers, nylon, polyesters, epoxies and derivatives or blends thereof (e.g., PLLA-phosphorylcholine).
- a porous or biodegradable membrane or layer made of biocompatible materials may be coated over the beneficial agent for sustained release thereof, if desired.
- a suitable base coating capable of retaining beneficial agent therein can be applied uniformly over the surface of the prosthesis, and then selected portions of the base coating can be loaded with the beneficial agent in accordance with embodiments of the invention.
- a greater amount of beneficial agent can be loaded over a unit surface area intended to have a greater local areal density and a lower amount of beneficial agent can be loaded over a unit surface area intended to have a lower local areal density.
- the beneficial agent may be applied directly to the surface of the prosthesis.
- a binder or similar component may be used to ensure sufficient adhesion.
- this coating technique may include admixing the beneficial agent with a suitable binder or polymer to form a coating mixture, which is then coated onto the surface of the prosthesis.
- the coating mixture would be prepared in higher or lower concentrations of beneficial agent as desired, and then applied to selected portions of the prosthesis appropriately.
- the beneficial agent may be applied to the interventional component in a polymer, include drug/polymer mixture.
- the amount of polymer in the mixture is small compared to the amount of drug.
- the polymer can be about 10% of the amount of drug.
- the polymer facilitates processing or loading or enhances retention of the drug on the interventional device, but is in an amount that is not effective to substantially inhibit the hydration of the drug.
- the presence of the hydration inhibitor of suitable LogP as set forth above has the greater influence on delivery of the drug in this circumstance.
- the first and second beneficial agents may correspond to drug-polymer mixtures having different concentrations of polymer to effect different release rates of the particular drug in each beneficial agent.
- the drug-polymer mixture having a higher concentration of polymer would have a slower release of the drug within the lumen.
- the drug-polymer mixture having a lower concentration of polymer would cause a more rapid release of the drug.
- beneficial agents can be released at rates appropriate for their activities and the prosthesis of the invention has multiple beneficial agents that elute off the prosthesis at desired rates.
- a cationic phosphorylcholine which has a higher affinity for anionic therapeutic agents can be blended and dispersed as a first beneficial agent and lipophilic phosphorylcholine can be blended with lipophilic drugs as the second beneficial agent to effect different release rates respectively.
- the beneficial agent(s) and hydration inhibitors can be applied to the medical device in one or more coating layers.
- alternating layers may be used to control delivery of multiple beneficial agents.
- Beneficial agents can be applied to the medical device alone or in combination with a suitable hydration inhibitor.
- Coatings that are suitable for use in this invention include, but are not limited to, any biocompatible polymeric material having suitable mechanical properties and in which the beneficial agent(s) is substantially soluble.
- Conventional coating techniques also may be utilized to coat the beneficial agent onto the surface of the prosthesis such as spraying, dipping or sputtering and still provide the desired effect if performed appropriately. With such techniques, it may be desirable or necessary to use known masking or extraction techniques to control the location and amount in which beneficial agent is loaded.
- the beneficial agent may be loaded directly onto a component (e.g., by pipetting) or alternatively, the beneficial agent is loaded onto a base material layer that is applied a surface of the component (e.g., dip loading).
- a base coating such as a binder or suitable polymer, is applied to a selected surface of the interventional component.
- a pattern may be formed on a component surface.
- Beneficial agent is then applied directly to the pattern of the base material.
- beneficial agent can be delivered at rates appropriate for the intended use or application.
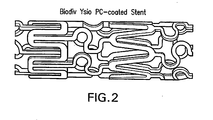
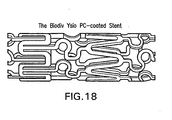
- the interventional device is stent 5, having stent struts 10.
- the interventional device in the form of a stent 5 has a base phosphorylchoine coating in which the beneficial drug is loaded.
- Figure 3A shows a cross-sectional view of a vessel segment in which was placed a stent 5 coated with a PC polymer only
- Figure 3B shows a cross-sectional view of a vessel segment in which was placed a stent 5 coated with a polymer plus drug.
- a cross-sectional view of a stent strut 10 of the stent 5 of Figure 1 is shown in Figures 4-7 .
- the stent strut 10 is loaded with a layer of beneficial agent 11 associated with a hydration inhibitor 12 as a mixture.
- the mixture is loaded on the stent strut 10 thicker on one side for increased dosage when desired.
- the beneficial agent 11 and hydration inhibitor 12 can be loaded evenly throughout or selectively at desired locations on the surface of the interventional component.
- the stent strut 10 is loaded with a layer of beneficial agent 11, which is covered by a layer of a second beneficial agent acting as a hydration inhibitor 22.
- the stent strut 10 has a base layer of a polymer material 31, preferably phosphorlycholine, wherein the polymer material is loaded with a beneficial agent 32 associated with a hydration inhibitor 12 as a mixture.
- Figure 7 depicts yet another embodiment of the invention wherein a stent strut 10 has a base layer of polymer material 31 loaded with a beneficial agent 32, and a coating of a second beneficial agent acts as a hydration inhibitor 22 to control delivery of the first beneficial agent.
- a stent strut 10 has layers 11A, 11B and 11C of a first beneficial agent alternating with layers 12A and 12B of a second beneficial agent/hydration inhibitor.
- first beneficial agent e.g., estradiol
- second beneficial agent/hydration inhibitor e.g., zotarolimus
- the LogP value of the second beneficial agent/hydration inhibitor is greater than the LogP value of the first beneficial agent, in accordance with principles of the invention.
- second beneficial agent/hydration inhibitor in layer 12A controls elution of first beneficial agent in layer 11A.
- Layers 12A and 12B enable midterm and late term delivery of first beneficial agent along with second beneficial agent/hydration inhibitor.
- layers 11A, 11B, 11C, 12A and 12B may optionally contain a polymer carrier or binder or other additive to facilitate processing or retention of the beneficial agent on the interventional device.
- layers 11A, 11B and 11C need not include the same beneficial agent.
- Each can include a different beneficial agent or two can include the same beneficial agent with the third including another beneficial agent.
- layers 12A and 12B need not contain the same beneficial agent.
- the hydration inhibitor has a LogP value of greater than 4.5 units and the beneficial agent has a LogP value less than 3 units. In this manner, the hydration inhibitor acts as a water barrier for the less hydrophobic beneficial agent, thereby reducing the release rate of the beneficial agent.
- the less hydrophobic beneficial agent can be ABT 620 ⁇ 1-Methyl-N-(3,4,5-trimethoxyphenyl)-1H-indole-5-sulfonamide ⁇ , ABT 627, ABT 518 ⁇ [S - (R*,R*)]-N-[1-(2,2-dimethyl-1,3-dioxol-4-yl)-2-[[4-[4-(trifluoro-methoxy)-phenoxy]phenyl]sulfonyl]ethyl]-N-hydroxyformamide ⁇ , dexamethasone and the like and the hydration inhibitor can be Fenofibrate, TricorTM or 3S,6R,7E,9R,10R,12R,14S,15E,17E,19E,21S,23S,26R,27R,34aS)-9,10,12,13,14,21,22,23,24, 25,26,27,32,
- the intervention component can include at least one reservoir or cavity therein.
- one or more of the reservoirs or cavities is loaded with a more hydrophilic first beneficial agent and then a second more hydrophobic beneficial agent can be loaded onto the first beneficial agent within the cavity or reservoir in a manner as described above
- the interventional device can include a third beneficial agent.
- the third beneficial agent can be any of the beneficial agents disclosed above.
- the third beneficial agent covers the second beneficial agent, the third beneficial agent having a LogP value less than the second LogP for rapid release of the third beneficial agent.
- the third beneficial agent can be the same as the first, so the beneficial agent is released rapidly upon implantation followed by a controlled release of the beneficial agent.
- the invention also provides a method for manufacturing a medical device for controlled delivery of beneficial agent.
- This method comprises the steps of providing an interventional component to be deployed in a patient; loading a beneficial agent on the interventional component for delivery therefrom, the beneficial agent having a first LogP value; and associating an effective amount of a hydration inhibitor with the beneficial agent to control delivery of the beneficial agent from the interventional component, the hydration inhibitor having a second LogP value, the second LogP value being greater than the first LogP value.
- the interventional component can be constructed to include pores or reservoirs which are impregnated or filled with beneficial agent, alone or in combination with a hydration inhibitor.
- the pores can be sized or spaced apart to correspond to or limit the amount of beneficial agent contained therein in accordance with the desired local areal density pattern along the length of the interventional device, wherein larger pores or more dense spacing would be provided in such portions intended to have a greater local areal density.
- the beneficial agent can be loaded directly onto the interventional component or alternatively, the beneficial agent is loaded onto a base material layer that is applied to at least a portion of the interventional component.
- a base coating including a binder or suitable polymer, is applied to a selected surface of the interventional component such that a desired pattern is formed on the interventional component surface.
- Beneficial agent and hydration inhibitor is then applied directly to the pattern of the base material.
- controlled areal density is understood to mean a known or predetermined amount of beneficial agent or mixture of beneficial agent and hydration inhibitor, either by weight or volume, over a unit surface area of the interventional component.
- the desired pattern corresponds to the desired controlled local areal density.
- a greater amount of base material layer is applied to portions of the interventional device intended to have a greater local areal density of beneficial agent, and a lesser amount of base material is applied to portions of the interventional device intended to have a lower local areal density of beneficial agent.
- the beneficial agent can be applied directly to the surface of the interventional component.
- Conventional coating techniques also can be utilized to coat the beneficial agent onto the surface of the interventional component such as spraying, dipping or sputtering and still provide the desired effect if performed appropriately. With such techniques, it can be desirable or necessary to use known masking or extraction techniques to control the location and amount in which beneficial agent is loaded. See U.S. Patent Application No. 09/950,307, filed September 10, 2001 ; U.S. Patent Nos. 6,329,386 and 6,015,815 ; and U.S. Patent Provisional Application entitled, "Medical Device Having a Hydration Inhibitor," filed on March 10, 2003.
- the beneficial agent(s) described herein can be applied to an intervention component that has been coated with a polymeric compound.
- Incorporation of the compound or drug into the polymeric coating of the interventional component can be carried out by dipping the polymer-coated interventional component into a solution containing the compound or drug for a sufficient period of time (such as, for example, five minutes) and then drying the coated interventional component, preferably by means of air drying for a sufficient period of time (such as, for example, 30 minutes).
- the polymer-coated interventional component containing the compound or drug can then be delivered to the coronary vessel by deployment from a balloon catheter, for example.
- the beneficial agent and hydration inhibitor is "printed" onto the surface of the interventional component by a fluid-dispenser having a dispensing element capable of dispensing beneficial agent in discrete droplets, wherein each droplet has a controlled trajectory.
- the beneficial agent or mixture is selectively dispensed from the dispensing element to a predetermined portion of the interventional component in a raster format along a dispensing path.
- fluid-jetting technology can be used to deposit materials, such as beneficial agents and hydration inhibitors, in controlled volumes onto a substrate at a controlled location. See U.S. Provisional Patent Application Nos. 60/424,575 ; 60/424,577 ; 60/424,607 ; 60/424,574 ; and 60/424,576 , all filed November 7, 2002.
- the first beneficial agent loaded onto the interventional component has a first local areal density and the second beneficial agent loaded onto the interventional component has a second local areal density.
- area density refers to the amount of beneficial agent per unit surface area of a selected portion of the interventional component.
- Local areal density refers to the dosage of beneficial agent per local surface area of the interventional component.
- the local areal density of the first beneficial agent and the local areal density of the second beneficial agent can be uniform across each respective portion to define stepped changes in local area density or can be varied across a selected portion of the interventional component to define gradients of local area density. Accordingly, a medical device is provided having an interventional component that is at least partially loaded with beneficial agent having a local areal density that is varied along a selected portion of the body of the interventional component.
- the local areal density can be varied by varying the relative rate in which beneficial agent is loaded to a selected location along the interventional component.
- the frequency in which the droplets of beneficial agent are applied along a unit length of the dispensing path to the interventional component is varied.
- the relative rate of loading beneficial agent can be varied by varying the relative movement between the dispensing element and the interventional component.
- Another alternative for varying the relative rate of loading beneficial agent is to vary the amount of beneficial agent per droplet dispensed from the dispensing element.
- Other alternatives for varying the local areal density of beneficial agent loaded onto the interventional component include mixing the beneficial agent with a binder and varying the ratio of beneficial agent to binder.
- the amount of the mixture of beneficial agent and binder that is applied to the interventional component can be varied to achieve a varied local areal density of beneficial agent.
- other methods of varying the local areal density of beneficial agent known in the art can be used.
- the first surface of the interventional component is defined by a plurality of interconnecting structural members.
- the first surface can include a first selected set of structural members, e.g ., a connector member
- the second surface can include a second selected set of the structural members, e.g ., a ring-shaped element extending around the circumference of the interventional component.
- Another feature of the invention includes applying a layer of base material on a selected portion of the interventional component described above.
- the beneficial agent or mixture with hydration inhibitor is loaded onto the base material layer according to the methods described above.
- the base material layer can define a pattern for loading the beneficial agent onto the interventional component.
- coated stainless steel coupons were prepared. These coupons were 316L electropolished stainless steel discs (10 mm diameter). This size was chosen because the surface area of one side of the coupon is similar to the surface area of a 15-mm open cell BiodivYsio stent.
- the coupon was prepared by scratching a mark on one side of the coupon, to indicate the side of the coupon that will not be coated, and then cleaned. The cleaning was a two-step process in which the coupons are sonicated for 3 minutes in dichloromethylene and 3 minutes in ethanol. The coupons were allowed to dry at room temperature.
- FIG. 9A-B is a top and side view of a coated stainless steel coupon 30, having a PC-coating 20 on a electropolished stainless steel disc.
- beneficial agents were loaded onto coupons and elution profiles examined.
- the procedure is as follows. Twelve PC-coated coupons were loaded with each drug. The solutions of the drugs were usually 5.0 mg/mL in 100% ethanol and were filtered with a 0.45 ⁇ m filter prior to use.
- the coupons were weighed before loading with the drug solution.
- 100 ⁇ g of drug 20 ⁇ L of solution was placed (e.g., pipetted) on the center of the PC coated side of the coupon.
- the coupon was placed in a vial for 30 minutes with the lid closed to allow the drug to penetrate the coating.
- the lid was removed and the coupon was allowed to dry for an additional 90 minutes.
- the coupon was weighed, and after 15 minutes the coupon was weighed a third time. When two weightings of the coupon were the same, the coupon was considered dry.
- the loaded, dry coupons were stored in a refrigerator protected from light.
- the coupons were removed from the elution media and immersed in 5 mL of 50% ethanol, 50% water solution and sonicated for 1 hour.
- the concentration of the drug in these vials indicated the amount of the drug remaining in the coupons at the end of the elution experiments.
- the coupons were individually placed, coating side up, in small metal cups to hold the coupon and to allow movement to a new vial at each time point.
- the coupons were usually placed in a vial containing 10 mL of pH 7.4 phosphate buffered saline.
- the vials were stored in an orbital shaker, with horizontal shaking of 100 rpm, at 37 °C for at least 30 minutes before insertion of a coupon to allow the solution to equilibrate at the desired temperature. At least nine different time points were observed as shown in Table 2. After the desired time had lapsed, the coupon holder was lifted and allowed to drain.
- Figures 10 , 11 , 12 , 13 and 14 illustrate the effect of a hydration inhibitor according to the invention on the elution of a relatively more hydrophilic beneficial agent.
- the drugs were applied to coupons; in Figure 14 , stents were coated.
- the six-hour elution profile shown is where the beneficial agent is fenofibrate and the hydration inhibitor is zotarolimus. Elution was carried out as described above.
- Curve A is the elution profile of zotarolimus alone.
- Curves B and C are the profiles for fenofibrate, in combination with zotarolimus and alone, respectively.
- Curve B shows that only about 7% of the fenofibrate was released from the coupon after 6 hours. As can be seen by comparing Curves B and C, the release of fenofibrate was significantly reduced by the presence of zotarolimus.
- Figure 11 illustrates the six-hour elution profile of beneficial agent ABT-627 (atrasentan) in the presence of hydration inhibitor zotarolimus.
- Curves A and C are the elution profiles of ABT-627, in the presence of zotarolimus and alone, respectively.
- Curve B shows the elution of zotarolimus under the same conditions. Comparing Curves A and C, it is seen that the elution rate of relatively more hydrophilic ABT-627 is reduced in the presence of relatively less hydrophilic zotarolimus. After six hours, much less than 10% of ABT-627 was released in the presence of zotarolimus (Curve C), compared to 50% in the absence of zotarolimus (Curve A).
- Figure 12 illustrates the six-hour elution profile of beneficial agent dipyridamole in the presence of hydration inhibitor zotarolimus.
- Curves A and B are the elution profiles of dipyridamole, in the presence of zotarolimus and alone, respectively.
- Curve C shows the elution profile of ABT 578 under the same conditions.
- the amount of dipyridamole released from the coupons coated with zotarolimus and dipyridamole is only about 52% after six hours, compared to nearly 90% in the absence of zotarolimus.
- Figure 13 illustrates the six-hour elution profiles of beneficial agent dexamethasone in the presence of hydration inhibitor zotarolimus.
- Curves A and B are the elution profiles of dexamethasone, alone and in the presence of zotarolimus, respectively.
- Curves C and D are the elution profiles for zotarolimus, alone and in the presence of dexamethasone, respectively, under the same conditions.
- the amount of dexamethasone remaining on the coupon containing dexamethasone and zotarolimus was nearly 70% compared to only 25% on the coupon on which no zotarolimus was present.
- Figure 14 illustrates the six-hour elution profile of beneficial agent dexamethasone in the presence of hydration inhibitor zotarolimus on a PC-coated stent. Loading was accomplished by dip loading, that I,s a stent was dipped into a solution containing either one or both drugs and then permitted to dry.
- Curves A and B are the elution profiles for dexamethasone in the presence of zotarolimus and alone, respectively.
- Curves C and D are the elution profiles for zotarolimus in the presence of dexamethasone and alone, respectively.
- coated stents were prepared. These were 3.0 mm X 15 mm 316L electropolished stainless steel stents. Each stent was spray coated using a filtered 20-mg/mL solution of phosphoryl choline polymer PC1036 (product of Biocompatibles Ltd., Farnham, Surrey, UK) in ethanoL The stents were initially air dried and then cured at 70°C for 16 hours. They were then sent for gamma irradiation at ⁇ 25KGy.
- PC1036 product of Biocompatibles Ltd., Farnham, Surrey, UK
- beneficial agents were loaded onto stents and elution profiles examined.
- the procedure was as follows. Multiple PC-coated stents were loaded with each drug combination solution.
- the solutions of the drugs were usually in the range of 2-20 mg/mL of zotarolimus and 10.0 mg/mL dexamethasone in 100% ethanol, with ⁇ 10% PC1036 added to the solution to enhance film formation.
- the stents were weighed before loading with the drug solution. To load approximately 10 ⁇ g/mL of each drug, a solution with equal amounts of zotarolimus and dexamethasone was sprayed onto the stent in a controlled fashion. The stent was allowed to dry before the stents were re-weighted to determine total drug load. The loaded, dry stents were stored in a refrigerator and were protected from light
- stents were used to evaluate the total amount of drug loaded by the above procedure.
- the stents were immersed in 6 mL of 50% ethanol, 50% water solution and sonicated for 20 minutes.
- the concentration of the drug in the extraction solution was analyzed by HPLC.
- the stents were removed from the dissolution media and immersed in 5 mL of 50% ethanol, 50% water solution and sonicated for 20 minutes.
- the concentration of the drug in these vials indicated the amount of the drug remaining on the stents at the end of the accelerated elution experiments. In this way, drug extraction was measured.
- HPLC method was developed for the determination of the amount of zotarolimus and dexamethasone eluted from phosphorylcholine (PC) coated metal stents (described above) in dissolution studies using an aqueous solution of polyethylene glycol 660 buffered at pH 4 as the dissolution medium. The method is used to determine the amount of drug that has eluted from the stent into the dissolution medium at 37°C at selected time points, typically in a 24-hour period. This rapid, in vitro elution test is intended for use as a quality check on the manufacturing process and a fast reliable research tool for understanding the factors controlling elution of drugs from stents.
- PC phosphorylcholine
- Figure 15 illustrates the effect of a hydration inhibitor according to the invention on the elution of a relatively more hydrophilic beneficial agent from, for example, a stent
- Figure 15 illustrates accelerated elution profiles (generated for example, by the technique described above) of beneficial agent dexamethasone in the presence of hydration inhibitor zotarolimus at different ratios.
- Curves A and B are the accelerated elution profiles of dexamethasone. As can be seen from the table in the plot, the amount of dexamethasone is higher than zotarolimus.
- Curves C and D show the accelerated elution profiles for dexamethasone. In these curves, the ratio of zotarolimus-to-dexamethasone increases to 1:1 and 2:1.
- dexamethasone elution becomes increasingly slow with increasing zotarolimus concentration.
- the amount of dexamethasone remaining on a zotarolimus /dexamethasone coated stent increases as the ratio of zotarolimus-to-dexamethasone increases.
- zotarolimus acts as an elution inhibitor for the more hydrophilic dexamethasone, further supporting the conclusion that relatively less hydrophilic beneficial agents can act as hydration inhibitors of relatively more hydrophilic agents.
- beneficial agents were loaded onto stents and the stability of the two drugs was examined.
- the procedure was as follows. Multiple PC-coated stents were loaded with each drug combination from solution.
- the solutions of the drugs were usually in the range of 2 - 20 mg/mL of zotarolimus and 10.0 mg/mL dexamethasone in 100% ethanol, with ⁇ 10% PC1036 added to the solution to enhance film formation.
- the stents were weighed before loading with the drug solution. To load approximately 10 ⁇ g/mL of each drug, a solution with equal amounts of zotarolimus and dexamethasone was sprayed onto the stent in a controlled fashion. The stent was allowed to dry before the stents were re-weighed to determine total drug load. The loaded, dry stents were stored in a refrigerator and were protected from light.
- stents were crimped onto catheter balloons and packaged into medical product Tyvek pouches for ETO (ethylene oxide) sterilization.
- ETO ethylene oxide
- the ETO sterilization process is standard in the medical device industry to ensure product safety.
- the ETO process was performed in a high humidity, elevated temperature environment to ensure microbe and spore kill.
- stents were used to evaluate the purity and stability of the drug loaded by the above procedure.
- the stents were immersed in 6 mL of 50% ethanol, 50% water solution and sonicated for 20 minutes.
- the concentration and the presence of degradant-related impurities of the drug in the extraction solution were analyzed by HPLC.
- Figure 16 shows the overlay of a chromatogram of a stent loaded with only dexamethasone and a chromatogram of a stent loaded with both dexamethasone and zotarolimus at a 1-to-1 ratio.
- dexamethasone in the dexamethasone-only coating degraded in the ETO sterilization environment with the production of at least three impurity peaks at 8.3, 11.3, and 21.8 minutes.
- dexamethasone that was loaded in combination with zotarolimus in this same high humidity environment did not degrade.
- the impurity peaks seen in the dexamethasone-only coated stents were not present, nor were any impurity peaks evident in the chromatogram.
- the compounds of this invention may be prepared by a variety of synthetic routes. A representative procedure is shown in Scheme 1.
- Example 1A A solution of Example 1A in isopropyl acetate (0.3 mL) was treated sequentially with diisopropylethylamine (87 L, 0.5 mmol) and 1H-tetrazole (35 mg, 0.5 mmol), and thereafter stirred for 18 hours. This mixture was partitioned between water (10 mL) and ether (10 mL). The organics were washed with brine (10 mL) and dried (Na 2 SO 4 ).
- Example 1B Collection of the slower moving band from the chromatography column using the hexane:acetone (1:1) mobile phase in Example 1B provided the designated compound. MS (ESI) m/e 966 (M) - .
- the immunosuppressant activity of the compounds of the present invention was compared to rapamycin and two rapamycin analogs: 40-epi-N-[2'-pyridone]-rapamycin and 40-epi-N-[4'-pyridone]-rapamycin.
- the activity was determined using the human mixed lymphocyte reaction (MLR) assay described by Kino, T. et al. in Transplantation Proceedings, XIX(5):36-39, Suppl. 6 (1987 ).
- MLR human mixed lymphocyte reaction
- the results of the assay demonstrate that the compounds of the invention are effective immunomodulators at nanomolar concentrations, as shown in Table 1.
- AUC Area under the curve
- Example 2 Example 2 and the internal standard were determined using the Sciex MacQuanTM software.
- Calibration curves were derived from peak area ratio (parent drug/internal standard) of the spiked blood standards using least squares linear regression of the ratio versus the theoretical concentration. The methods were linear for both compounds over the range of the standard curve (correlation > 0.99) with an estimated quantitation limit of 0.1 ng/mL.
- the maximum blood concentration (C MAX ) and the time to reach the maximum blood concentration (T MAX ) were read directly from the observed blood concentration-time data.
- the blood concentration data were submitted to multi-exponential curve fitting using CSTRIP to obtain estimates of pharmacokinetic parameters.
- the estimated parameters were further defined using NONLIN84.
- the area under the blood concentration-time curve from 0 to t hours (last measurable blood concentration time point) after dosing (AUC 0-t ) was calculated using the linear trapeziodal rule for the blood-time profiles.
- Example 1 and Example 2 had a surprisingly substantially shorter terminal elimination half life (t 1/2 ) when compared to rapamycin.
- t 1/2 terminal elimination half life
- Table 2 Compound AUC ng ⁇ hr/mL t 1/2 (hours) Rapamycin 6.87 16.7 2-pyridone 2.55 2.8 4-pyridone 5.59 13.3
Landscapes
- Health & Medical Sciences (AREA)
- Life Sciences & Earth Sciences (AREA)
- Veterinary Medicine (AREA)
- Public Health (AREA)
- General Health & Medical Sciences (AREA)
- Animal Behavior & Ethology (AREA)
- Engineering & Computer Science (AREA)
- Heart & Thoracic Surgery (AREA)
- Vascular Medicine (AREA)
- Biomedical Technology (AREA)
- Medicinal Chemistry (AREA)
- Chemical & Material Sciences (AREA)
- Cardiology (AREA)
- Surgery (AREA)
- Epidemiology (AREA)
- General Chemical & Material Sciences (AREA)
- Chemical Kinetics & Catalysis (AREA)
- Organic Chemistry (AREA)
- Nuclear Medicine, Radiotherapy & Molecular Imaging (AREA)
- Pharmacology & Pharmacy (AREA)
- Transplantation (AREA)
- Oral & Maxillofacial Surgery (AREA)
- Molecular Biology (AREA)
- Bioinformatics & Cheminformatics (AREA)
- Gastroenterology & Hepatology (AREA)
- Pulmonology (AREA)
- Oncology (AREA)
- Communicable Diseases (AREA)
- Materials For Medical Uses (AREA)
- Pharmaceuticals Containing Other Organic And Inorganic Compounds (AREA)
- Infusion, Injection, And Reservoir Apparatuses (AREA)
- Medicines That Contain Protein Lipid Enzymes And Other Medicines (AREA)
Claims (15)
- Système pour délivrer un agent lipophile, comprenant :un dispositif médical ;un premier agent lipophile, qui est capable de pénétrer dans une lumière corporelle, et qui est le zotarolimus ayant les structures suivantes :
- Système suivant la revendication 1, comprenant en outre au moins un support ou excipient pharmaceutiquement acceptable, dans lequel ledit dispositif médical est associé audit support ou excipient pharmaceutiquement acceptable.
- Système suivant la revendication 2, dans lequel ledit support ou excipient pharmaceutiquement acceptable est un polymère.
- Système suivant la revendication 3, dans lequel ledit polymère est une macromolécule contenant des groupes phosphorylcholine appendus.
- Système suivant la revendication 1, dans lequel ledit premier agent lipophile/dispositif médical est placé en position adjacente à ladite lumière corporelle comprenant des artères coronaires, où une quantité thérapeutiquement efficace dudit premier agent lipophile est délivrée dans lesdites artères coronaires et diffusée dans le sac péricardique dans ledit système d'administration de médicament.
- Système suivant la revendication 3, dans lequel ledit mécanisme d'administration dudit premier agent lipophile comprend une matrice d'agent lipophile/polymère qui commande la vitesse d'élution dudit premier agent lipophile à ladite lumière corporelle.
- Système suivant la revendication 1, ledit système comprenant un premier agent lipophile ayant des coefficients de transfert d'au moins 10 000 (µg/ml)-1.
- Système suivant la revendication 1, ledit système comprenant un premier agent lipophile ayant des coefficients de transfert d'au moins 15 000 (µg/ml)-1.
- Système suivant la revendication 1, dans lequel l'administration posologique dudit premier agent lipophile dans ladite lumière corporelle va de 15 µg/g à 150 µg/g pendant une période allant jusqu'à 5 jours.
- Système suivant la revendication 1, dans lequel l'administration posologique dudit premier agent lipophile dans ladite lumière corporelle va de 5 µg/g à 80 µg/g pendant une période de 5 jours à 15 jours.
- Système suivant la revendication 1, dans lequel l'administration posologique dudit premier agent lipophile dans ladite lumière corporelle va de 5 µg/g à 60 µg/g pendant une période de 15 jours à 28 jours.
- Système suivant la revendication 1, dans lequel ledit premier agent lipophile atteint des concentrations thérapeutiquement significatives dans des zones ciblées chez ledit sujet, comprenant au moins une des zones consistant en le myocarde distal, le myocarde sans extension, dans ledit myocarde sous-jacent, dans des artères coronaires sans extension et distales, et maintient ces concentrations pendant une période de 28 jours.
- Dispositif médical, comprenant :une quantité thérapeutiquement efficace d'un premier agent lipophile, qui est associé audit dispositif médical et qui est capable de pénétrer dans une lumière corporelle, et qui est le zotarolimus ayant les structures suivantes :
- Extenseur, comprenant :une quantité thérapeutiquement efficace d'un premier agent lipophile, qui est associé audit extenseur et qui est capable de pénétrer dans une lumière corporelle, et qui est le zotarolimus ayant les structures suivantes :
Priority Applications (1)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| EP20100183267 EP2327429B1 (fr) | 2005-03-23 | 2006-03-22 | Administration d'agents lipophiles par dispositifs médicaux |
Applications Claiming Priority (2)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US66432805P | 2005-03-23 | 2005-03-23 | |
| PCT/US2006/010307 WO2006102359A2 (fr) | 2005-03-23 | 2006-03-22 | Distribution d'agents hautement lipophiles au moyen de dispositifs medicaux |
Related Child Applications (2)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP20100183267 Division EP2327429B1 (fr) | 2005-03-23 | 2006-03-22 | Administration d'agents lipophiles par dispositifs médicaux |
| EP10183267.3 Division-Into | 2010-09-30 |
Publications (2)
| Publication Number | Publication Date |
|---|---|
| EP1868663A2 EP1868663A2 (fr) | 2007-12-26 |
| EP1868663B1 true EP1868663B1 (fr) | 2011-11-16 |
Family
ID=36940009
Family Applications (2)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP20060739194 Active EP1868663B1 (fr) | 2005-03-23 | 2006-03-22 | Distribution d'agents hautement lipophiles au moyen de dispositifs medicaux |
| EP20100183267 Active EP2327429B1 (fr) | 2005-03-23 | 2006-03-22 | Administration d'agents lipophiles par dispositifs médicaux |
Family Applications After (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP20100183267 Active EP2327429B1 (fr) | 2005-03-23 | 2006-03-22 | Administration d'agents lipophiles par dispositifs médicaux |
Country Status (6)
| Country | Link |
|---|---|
| US (2) | US20090216317A1 (fr) |
| EP (2) | EP1868663B1 (fr) |
| JP (1) | JP5271697B2 (fr) |
| AT (1) | ATE533520T1 (fr) |
| TW (1) | TWI455708B (fr) |
| WO (1) | WO2006102359A2 (fr) |
Families Citing this family (189)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US6302875B1 (en) | 1996-10-11 | 2001-10-16 | Transvascular, Inc. | Catheters and related devices for forming passageways between blood vessels or other anatomical structures |
| US20060198867A1 (en) * | 1997-09-25 | 2006-09-07 | Abbott Laboratories, Inc. | Compositions and methods of administering rapamycin analogs using medical devices for long-term efficacy |
| US8257725B2 (en) * | 1997-09-26 | 2012-09-04 | Abbott Laboratories | Delivery of highly lipophilic agents via medical devices |
| US8257724B2 (en) * | 1998-09-24 | 2012-09-04 | Abbott Laboratories | Delivery of highly lipophilic agents via medical devices |
| US20060240070A1 (en) * | 1998-09-24 | 2006-10-26 | Cromack Keith R | Delivery of highly lipophilic agents via medical devices |
| US20080213331A1 (en) | 2002-04-08 | 2008-09-04 | Ardian, Inc. | Methods and devices for renal nerve blocking |
| US8347891B2 (en) | 2002-04-08 | 2013-01-08 | Medtronic Ardian Luxembourg S.A.R.L. | Methods and apparatus for performing a non-continuous circumferential treatment of a body lumen |
| US20070129761A1 (en) | 2002-04-08 | 2007-06-07 | Ardian, Inc. | Methods for treating heart arrhythmia |
| US7617005B2 (en) | 2002-04-08 | 2009-11-10 | Ardian, Inc. | Methods and apparatus for thermally-induced renal neuromodulation |
| US8150519B2 (en) | 2002-04-08 | 2012-04-03 | Ardian, Inc. | Methods and apparatus for bilateral renal neuromodulation |
| US20070135875A1 (en) | 2002-04-08 | 2007-06-14 | Ardian, Inc. | Methods and apparatus for thermally-induced renal neuromodulation |
| US9636174B2 (en) | 2002-04-08 | 2017-05-02 | Medtronic Ardian Luxembourg S.A.R.L. | Methods for therapeutic renal neuromodulation |
| US7756583B2 (en) | 2002-04-08 | 2010-07-13 | Ardian, Inc. | Methods and apparatus for intravascularly-induced neuromodulation |
| US20040054413A1 (en) * | 2002-09-16 | 2004-03-18 | Howmedica Osteonics Corp. | Radiovisible hydrogel intervertebral disc nucleus |
| US7920906B2 (en) | 2005-03-10 | 2011-04-05 | Dexcom, Inc. | System and methods for processing analyte sensor data for sensor calibration |
| EP1667595B1 (fr) | 2003-09-12 | 2014-01-01 | Vessix Vascular, Inc. | Systeme de remodelage excentrique et/ou ablation d'une matiere atherosclereuse |
| US9247900B2 (en) | 2004-07-13 | 2016-02-02 | Dexcom, Inc. | Analyte sensor |
| US20070045902A1 (en) | 2004-07-13 | 2007-03-01 | Brauker James H | Analyte sensor |
| US7713574B2 (en) | 2004-07-13 | 2010-05-11 | Dexcom, Inc. | Transcutaneous analyte sensor |
| US8920414B2 (en) | 2004-09-10 | 2014-12-30 | Vessix Vascular, Inc. | Tuned RF energy and electrical tissue characterization for selective treatment of target tissues |
| US8396548B2 (en) | 2008-11-14 | 2013-03-12 | Vessix Vascular, Inc. | Selective drug delivery in a lumen |
| US9713730B2 (en) | 2004-09-10 | 2017-07-25 | Boston Scientific Scimed, Inc. | Apparatus and method for treatment of in-stent restenosis |
| JP5219518B2 (ja) | 2004-12-09 | 2013-06-26 | ザ ファウンドリー, エルエルシー | 大動脈弁修復 |
| ES2691646T3 (es) | 2005-07-15 | 2018-11-28 | Micell Technologies, Inc. | Revestimientos poliméricos que contienen polvo de fármaco de morfología controlada |
| US20090062909A1 (en) | 2005-07-15 | 2009-03-05 | Micell Technologies, Inc. | Stent with polymer coating containing amorphous rapamycin |
| ES2540059T3 (es) | 2006-04-26 | 2015-07-08 | Micell Technologies, Inc. | Recubrimientos que contienen múltiples fármacos |
| US8019435B2 (en) | 2006-05-02 | 2011-09-13 | Boston Scientific Scimed, Inc. | Control of arterial smooth muscle tone |
| AU2007310991B2 (en) | 2006-10-18 | 2013-06-20 | Boston Scientific Scimed, Inc. | System for inducing desirable temperature effects on body tissue |
| CA2666660C (fr) | 2006-10-18 | 2015-06-02 | Minnow Medical, Inc. | Induction d'effets souhaitables de temperature sur un tissu humain |
| WO2008052000A2 (fr) | 2006-10-23 | 2008-05-02 | Micell Technologies, Inc. | Support pour charger électriquement un substrat au cours de l'enduction |
| WO2008063581A2 (fr) * | 2006-11-20 | 2008-05-29 | Lutonix, Inc. | Traitement de l'asthme et de la bronchopneumopathie chronique obstructive à l'aide de médicaments antiprolifératifs et anti-inflammatoires |
| US11426494B2 (en) | 2007-01-08 | 2022-08-30 | MT Acquisition Holdings LLC | Stents having biodegradable layers |
| US9737642B2 (en) | 2007-01-08 | 2017-08-22 | Micell Technologies, Inc. | Stents having biodegradable layers |
| KR101144984B1 (ko) | 2007-01-21 | 2012-05-21 | 헤모텍 아게 | 체강의 협착 치료 및 급성 재협착 예방을 위한 의료 제품 |
| US9433516B2 (en) | 2007-04-17 | 2016-09-06 | Micell Technologies, Inc. | Stents having controlled elution |
| WO2008148013A1 (fr) | 2007-05-25 | 2008-12-04 | Micell Technologies, Inc. | Films de polymères pour le revêtement des dispositifs médicaux |
| DE102007025921A1 (de) * | 2007-06-02 | 2008-12-04 | Biotronik Vi Patent Ag | Medizinisches Implantat, insbesondere Stent |
| US9192697B2 (en) | 2007-07-03 | 2015-11-24 | Hemoteq Ag | Balloon catheter for treating stenosis of body passages and for preventing threatening restenosis |
| WO2009051780A1 (fr) * | 2007-10-19 | 2009-04-23 | Micell Technologies, Inc. | Endoprothèses vasculaires revêtues de médicament |
| WO2009112741A2 (fr) * | 2008-02-21 | 2009-09-17 | Hexacath | Dispositif medical implantable avec une couche de protection/retention d'un agent actif ou medicament, notamment hydrosoluble |
| FR2927815B1 (fr) * | 2008-02-21 | 2011-01-14 | Hexacath | Dispositif medical comprenant un agent precurseur de no, tel que la l-arginine ou l-lysine, et une couche de protection et/ou de retention de celui-ci |
| FR2927813B1 (fr) * | 2008-02-21 | 2017-07-21 | Hexacath | Dispositif medical implantable sur une couche de protection/retention d'un agent actif ou medicament, notamment hydrosoluble |
| EA020655B1 (ru) | 2008-04-17 | 2014-12-30 | Миселл Текнолоджиз, Инк. | Стенты, имеющие биорассасывающиеся слои |
| US9510856B2 (en) | 2008-07-17 | 2016-12-06 | Micell Technologies, Inc. | Drug delivery medical device |
| CN102159257B (zh) | 2008-07-17 | 2015-11-25 | 米歇尔技术公司 | 药物递送医疗设备 |
| US8257722B2 (en) | 2008-09-15 | 2012-09-04 | Cv Ingenuity Corp. | Local delivery of water-soluble or water-insoluble therapeutic agents to the surface of body lumens |
| US8128951B2 (en) | 2008-09-15 | 2012-03-06 | Cv Ingenuity Corp. | Local delivery of water-soluble or water-insoluble therapeutic agents to the surface of body lumens |
| US8114429B2 (en) | 2008-09-15 | 2012-02-14 | Cv Ingenuity Corp. | Local delivery of water-soluble or water-insoluble therapeutic agents to the surface of body lumens |
| US9198968B2 (en) | 2008-09-15 | 2015-12-01 | The Spectranetics Corporation | Local delivery of water-soluble or water-insoluble therapeutic agents to the surface of body lumens |
| KR101138294B1 (ko) * | 2008-09-24 | 2012-04-25 | 김형일 | 혈관벽 임시 골격용 생분해성 블랜드 |
| AU2009295960A1 (en) | 2008-09-29 | 2010-04-01 | Cardiaq Valve Technologies, Inc. | Heart valve |
| EP2341871B1 (fr) | 2008-10-01 | 2017-03-22 | Edwards Lifesciences CardiAQ LLC | Système de mise en place pour implant vasculaire |
| WO2010056745A1 (fr) | 2008-11-17 | 2010-05-20 | Minnow Medical, Inc. | Accumulation sélective d’énergie avec ou sans connaissance de la topographie tissulaire |
| US8834913B2 (en) | 2008-12-26 | 2014-09-16 | Battelle Memorial Institute | Medical implants and methods of making medical implants |
| WO2010120552A2 (fr) | 2009-04-01 | 2010-10-21 | Micell Technologies, Inc. | Endoprothèses enduites |
| EP2419050B2 (fr) | 2009-04-15 | 2023-10-18 | Edwards Lifesciences CardiAQ LLC | Implant vasculaire et système d'introduction |
| EP2451496B1 (fr) | 2009-07-10 | 2015-07-22 | Boston Scientific Scimed, Inc. | Utilisation de nanocristaux pour un ballonnet de distribution de médicament |
| EP2962707B1 (fr) | 2009-07-17 | 2019-07-24 | Boston Scientific Scimed, Inc. | Ballons d'administration de médicament avec une taille et une densité des cristaux améliorées |
| US11369498B2 (en) | 2010-02-02 | 2022-06-28 | MT Acquisition Holdings LLC | Stent and stent delivery system with improved deliverability |
| WO2011119536A1 (fr) | 2010-03-22 | 2011-09-29 | Abbott Cardiovascular Systems Inc. | Système de pose d'endoprothèse pourvu d'une matrice fibreuse ayant une capacité de rétention améliorée de l'endoprothèse |
| US8795762B2 (en) | 2010-03-26 | 2014-08-05 | Battelle Memorial Institute | System and method for enhanced electrostatic deposition and surface coatings |
| AU2011238925B2 (en) | 2010-04-09 | 2016-06-16 | Vessix Vascular, Inc. | Power generating and control apparatus for the treatment of tissue |
| US9192790B2 (en) | 2010-04-14 | 2015-11-24 | Boston Scientific Scimed, Inc. | Focused ultrasonic renal denervation |
| US10232092B2 (en) | 2010-04-22 | 2019-03-19 | Micell Technologies, Inc. | Stents and other devices having extracellular matrix coating |
| US8579964B2 (en) | 2010-05-05 | 2013-11-12 | Neovasc Inc. | Transcatheter mitral valve prosthesis |
| US8473067B2 (en) | 2010-06-11 | 2013-06-25 | Boston Scientific Scimed, Inc. | Renal denervation and stimulation employing wireless vascular energy transfer arrangement |
| EP2593039B1 (fr) | 2010-07-16 | 2022-11-30 | Micell Technologies, Inc. | Dispositif médical d'administration de médicament |
| US9408661B2 (en) | 2010-07-30 | 2016-08-09 | Patrick A. Haverkost | RF electrodes on multiple flexible wires for renal nerve ablation |
| US9358365B2 (en) | 2010-07-30 | 2016-06-07 | Boston Scientific Scimed, Inc. | Precision electrode movement control for renal nerve ablation |
| US9155589B2 (en) | 2010-07-30 | 2015-10-13 | Boston Scientific Scimed, Inc. | Sequential activation RF electrode set for renal nerve ablation |
| US9463062B2 (en) | 2010-07-30 | 2016-10-11 | Boston Scientific Scimed, Inc. | Cooled conductive balloon RF catheter for renal nerve ablation |
| US9084609B2 (en) | 2010-07-30 | 2015-07-21 | Boston Scientific Scime, Inc. | Spiral balloon catheter for renal nerve ablation |
| WO2012031236A1 (fr) | 2010-09-02 | 2012-03-08 | Boston Scientific Scimed, Inc. | Procédé d'enrobage de ballonnets d'administration de médicaments utilisant une mémoire d'enveloppe induite par la chaleur |
| US8974451B2 (en) | 2010-10-25 | 2015-03-10 | Boston Scientific Scimed, Inc. | Renal nerve ablation using conductive fluid jet and RF energy |
| US9220558B2 (en) | 2010-10-27 | 2015-12-29 | Boston Scientific Scimed, Inc. | RF renal denervation catheter with multiple independent electrodes |
| US9028485B2 (en) | 2010-11-15 | 2015-05-12 | Boston Scientific Scimed, Inc. | Self-expanding cooling electrode for renal nerve ablation |
| US9089350B2 (en) | 2010-11-16 | 2015-07-28 | Boston Scientific Scimed, Inc. | Renal denervation catheter with RF electrode and integral contrast dye injection arrangement |
| US9668811B2 (en) | 2010-11-16 | 2017-06-06 | Boston Scientific Scimed, Inc. | Minimally invasive access for renal nerve ablation |
| US9326751B2 (en) | 2010-11-17 | 2016-05-03 | Boston Scientific Scimed, Inc. | Catheter guidance of external energy for renal denervation |
| US9060761B2 (en) | 2010-11-18 | 2015-06-23 | Boston Scientific Scime, Inc. | Catheter-focused magnetic field induced renal nerve ablation |
| US9023034B2 (en) | 2010-11-22 | 2015-05-05 | Boston Scientific Scimed, Inc. | Renal ablation electrode with force-activatable conduction apparatus |
| US9192435B2 (en) | 2010-11-22 | 2015-11-24 | Boston Scientific Scimed, Inc. | Renal denervation catheter with cooled RF electrode |
| US20120157993A1 (en) | 2010-12-15 | 2012-06-21 | Jenson Mark L | Bipolar Off-Wall Electrode Device for Renal Nerve Ablation |
| CA2822381C (fr) | 2010-12-23 | 2019-04-02 | Foundry Newco Xii, Inc. | Systeme de reparation et remplacement de valvule mitrale |
| WO2012100095A1 (fr) | 2011-01-19 | 2012-07-26 | Boston Scientific Scimed, Inc. | Cathéter à grande électrode compatible avec un guide pour ablation de nerf rénal à lésion artérielle réduite |
| WO2012116182A1 (fr) * | 2011-02-23 | 2012-08-30 | Ams Research Corporation | Système et procédé d'implant pelvien et d'agent thérapeutique |
| JP5759615B2 (ja) | 2011-04-08 | 2015-08-05 | コヴィディエン リミテッド パートナーシップ | 腎交感神経の除神経およびイオン導入薬物送達のためのイオン導入カテーテルシステムならびに方法 |
| TW201242570A (en) | 2011-04-25 | 2012-11-01 | Medtronic Ardian Luxembourg | Apparatus and methods related to constrained deployment of cryogenic balloons for limited cryogenic ablation of vessel walls |
| US9308087B2 (en) | 2011-04-28 | 2016-04-12 | Neovasc Tiara Inc. | Sequentially deployed transcatheter mitral valve prosthesis |
| US9554897B2 (en) | 2011-04-28 | 2017-01-31 | Neovasc Tiara Inc. | Methods and apparatus for engaging a valve prosthesis with tissue |
| US10464100B2 (en) | 2011-05-31 | 2019-11-05 | Micell Technologies, Inc. | System and process for formation of a time-released, drug-eluting transferable coating |
| WO2012177942A2 (fr) | 2011-06-21 | 2012-12-27 | Hanson Gifford, Iii | Dispositifs de valvule cardiaque prosthétiques et systèmes et procédés associés |
| US10117972B2 (en) | 2011-07-15 | 2018-11-06 | Micell Technologies, Inc. | Drug delivery medical device |
| US9579030B2 (en) | 2011-07-20 | 2017-02-28 | Boston Scientific Scimed, Inc. | Percutaneous devices and methods to visualize, target and ablate nerves |
| EP2734264B1 (fr) | 2011-07-22 | 2018-11-21 | Boston Scientific Scimed, Inc. | Système de neuromodulation avec un élément de neuromodulation positionnable dans un guide hélicoïdal |
| WO2013022458A1 (fr) | 2011-08-05 | 2013-02-14 | Boston Scientific Scimed, Inc. | Procédés de conversion d'une substance médicamenteuse amorphe en une forme cristalline |
| US9056152B2 (en) | 2011-08-25 | 2015-06-16 | Boston Scientific Scimed, Inc. | Medical device with crystalline drug coating |
| WO2013055826A1 (fr) | 2011-10-10 | 2013-04-18 | Boston Scientific Scimed, Inc. | Dispositifs médicaux comprenant des électrodes d'ablation |
| EP2765940B1 (fr) | 2011-10-11 | 2015-08-26 | Boston Scientific Scimed, Inc. | Dispositif d'électrode hors paroi pour une modulation nerveuse |
| US9420955B2 (en) | 2011-10-11 | 2016-08-23 | Boston Scientific Scimed, Inc. | Intravascular temperature monitoring system and method |
| US9364284B2 (en) | 2011-10-12 | 2016-06-14 | Boston Scientific Scimed, Inc. | Method of making an off-wall spacer cage |
| EP2768563B1 (fr) | 2011-10-18 | 2016-11-09 | Boston Scientific Scimed, Inc. | Dispositifs médicaux pouvant être déviés |
| US10188772B2 (en) | 2011-10-18 | 2019-01-29 | Micell Technologies, Inc. | Drug delivery medical device |
| US9079000B2 (en) | 2011-10-18 | 2015-07-14 | Boston Scientific Scimed, Inc. | Integrated crossing balloon catheter |
| US11202704B2 (en) | 2011-10-19 | 2021-12-21 | Twelve, Inc. | Prosthetic heart valve devices, prosthetic mitral valves and associated systems and methods |
| US9039757B2 (en) | 2011-10-19 | 2015-05-26 | Twelve, Inc. | Prosthetic heart valve devices, prosthetic mitral valves and associated systems and methods |
| US9655722B2 (en) | 2011-10-19 | 2017-05-23 | Twelve, Inc. | Prosthetic heart valve devices, prosthetic mitral valves and associated systems and methods |
| CN111000663B (zh) | 2011-10-19 | 2022-04-15 | 托尔福公司 | 人工心脏瓣膜装置、人工二尖瓣和相关系统及方法 |
| US9763780B2 (en) | 2011-10-19 | 2017-09-19 | Twelve, Inc. | Devices, systems and methods for heart valve replacement |
| CA2848334C (fr) | 2011-10-19 | 2020-10-20 | Twelve, Inc. | Dispositifs, systemes et procedes de remplacement de valvule cardiaque |
| EP3366250A1 (fr) | 2011-11-08 | 2018-08-29 | Boston Scientific Scimed, Inc. | Ablation ostiale du nerf rénal |
| JP5921153B2 (ja) * | 2011-11-09 | 2016-05-24 | キヤノン株式会社 | 放射線発生管および放射線発生装置 |
| WO2013074813A1 (fr) | 2011-11-15 | 2013-05-23 | Boston Scientific Scimed, Inc. | Dispositif et procédés pour surveiller la modulation nerveuse rénale |
| US9119632B2 (en) | 2011-11-21 | 2015-09-01 | Boston Scientific Scimed, Inc. | Deflectable renal nerve ablation catheter |
| US8546412B2 (en) * | 2011-12-21 | 2013-10-01 | Abbott Cardiovascular Systems, Inc. | Methods of treating heart failure |
| US9265969B2 (en) | 2011-12-21 | 2016-02-23 | Cardiac Pacemakers, Inc. | Methods for modulating cell function |
| US9037259B2 (en) | 2011-12-23 | 2015-05-19 | Vessix Vascular, Inc. | Methods and apparatuses for remodeling tissue of or adjacent to a body passage |
| WO2013101452A1 (fr) | 2011-12-28 | 2013-07-04 | Boston Scientific Scimed, Inc. | Dispositif et procédés pour la modulation nerveuse à l'aide d'un nouveau cathéter d'ablation doté d'éléments ablatifs polymères |
| US9050106B2 (en) | 2011-12-29 | 2015-06-09 | Boston Scientific Scimed, Inc. | Off-wall electrode device and methods for nerve modulation |
| US9579198B2 (en) | 2012-03-01 | 2017-02-28 | Twelve, Inc. | Hydraulic delivery systems for prosthetic heart valve devices and associated methods |
| WO2013169927A1 (fr) | 2012-05-08 | 2013-11-14 | Boston Scientific Scimed, Inc. | Dispositifs de modulation du nerf rénal |
| US9345573B2 (en) | 2012-05-30 | 2016-05-24 | Neovasc Tiara Inc. | Methods and apparatus for loading a prosthesis onto a delivery system |
| US9956385B2 (en) | 2012-06-28 | 2018-05-01 | The Spectranetics Corporation | Post-processing of a medical device to control morphology and mechanical properties |
| US10321946B2 (en) | 2012-08-24 | 2019-06-18 | Boston Scientific Scimed, Inc. | Renal nerve modulation devices with weeping RF ablation balloons |
| WO2014039964A2 (fr) | 2012-09-10 | 2014-03-13 | The Regents Of The University Of California | Composés et méthodes de modulation de blessures vasculaires |
| US9173696B2 (en) | 2012-09-17 | 2015-11-03 | Boston Scientific Scimed, Inc. | Self-positioning electrode system and method for renal nerve modulation |
| WO2014047411A1 (fr) | 2012-09-21 | 2014-03-27 | Boston Scientific Scimed, Inc. | Système de modulation des nerfs et blocage des nerfs par gradient thermique inoffensif |
| US10549127B2 (en) | 2012-09-21 | 2020-02-04 | Boston Scientific Scimed, Inc. | Self-cooling ultrasound ablation catheter |
| JP6074051B2 (ja) | 2012-10-10 | 2017-02-01 | ボストン サイエンティフィック サイムド,インコーポレイテッドBoston Scientific Scimed,Inc. | 血管内神経変調システム及び医療用デバイス |
| US10583002B2 (en) | 2013-03-11 | 2020-03-10 | Neovasc Tiara Inc. | Prosthetic valve with anti-pivoting mechanism |
| WO2014143571A1 (fr) | 2013-03-11 | 2014-09-18 | Boston Scientific Scimed, Inc. | Dispositifs médicaux pour moduler des nerfs |
| US9956033B2 (en) | 2013-03-11 | 2018-05-01 | Boston Scientific Scimed, Inc. | Medical devices for modulating nerves |
| US11039943B2 (en) | 2013-03-12 | 2021-06-22 | Micell Technologies, Inc. | Bioabsorbable biomedical implants |
| US9808311B2 (en) | 2013-03-13 | 2017-11-07 | Boston Scientific Scimed, Inc. | Deflectable medical devices |
| US9681951B2 (en) | 2013-03-14 | 2017-06-20 | Edwards Lifesciences Cardiaq Llc | Prosthesis with outer skirt and anchors |
| EP2967734B1 (fr) | 2013-03-15 | 2019-05-15 | Boston Scientific Scimed, Inc. | Procédés et appareils pour remodéliser un tissu de ou adjacent à un passage corporel |
| US10265122B2 (en) | 2013-03-15 | 2019-04-23 | Boston Scientific Scimed, Inc. | Nerve ablation devices and related methods of use |
| EP2967725B1 (fr) | 2013-03-15 | 2019-12-11 | Boston Scientific Scimed, Inc. | Unité de commande de détection de fuite électrique entre des plots d'électrodes et système comprenant une telle unité de commande |
| US9572665B2 (en) | 2013-04-04 | 2017-02-21 | Neovasc Tiara Inc. | Methods and apparatus for delivering a prosthetic valve to a beating heart |
| KR102079613B1 (ko) | 2013-05-15 | 2020-02-20 | 미셀 테크놀로지즈, 인코포레이티드 | 생흡수성 생체의학적 임플란트 |
| CN105246431B (zh) | 2013-05-20 | 2018-04-06 | 托尔福公司 | 可植入心脏瓣膜装置、二尖瓣修复装置以及相关系统和方法 |
| CN105473091B (zh) | 2013-06-21 | 2020-01-21 | 波士顿科学国际有限公司 | 具有可一起移动的电极支撑件的肾脏去神经球囊导管 |
| EP3010436A1 (fr) | 2013-06-21 | 2016-04-27 | Boston Scientific Scimed, Inc. | Dispositifs médicaux pour une ablation de nerf rénal ayant des tiges rotatives |
| US9707036B2 (en) | 2013-06-25 | 2017-07-18 | Boston Scientific Scimed, Inc. | Devices and methods for nerve modulation using localized indifferent electrodes |
| WO2015002787A1 (fr) | 2013-07-01 | 2015-01-08 | Boston Scientific Scimed, Inc. | Dispositifs médicaux pour une ablation de nerf rénal |
| EP3019106A1 (fr) | 2013-07-11 | 2016-05-18 | Boston Scientific Scimed, Inc. | Dispositif médical équipé d'ensembles électrodes extensibles |
| EP3019105B1 (fr) | 2013-07-11 | 2017-09-13 | Boston Scientific Scimed, Inc. | Dispositifs de modulation nerveuse |
| US9925001B2 (en) | 2013-07-19 | 2018-03-27 | Boston Scientific Scimed, Inc. | Spiral bipolar electrode renal denervation balloon |
| JP2016527959A (ja) | 2013-07-22 | 2016-09-15 | ボストン サイエンティフィック サイムド,インコーポレイテッドBoston Scientific Scimed,Inc. | 腎神経アブレーション用医療器具 |
| WO2015013301A1 (fr) | 2013-07-22 | 2015-01-29 | Boston Scientific Scimed, Inc. | Cathéter d'ablation de nerf rénal ayant un ballonnet de torsion |
| CN105473093B (zh) | 2013-08-22 | 2019-02-05 | 波士顿科学国际有限公司 | 具有至肾神经调制球囊的改善的粘附力的柔性电路 |
| CN105555218B (zh) | 2013-09-04 | 2019-01-15 | 波士顿科学国际有限公司 | 具有冲洗和冷却能力的射频(rf)球囊导管 |
| WO2015038947A1 (fr) | 2013-09-13 | 2015-03-19 | Boston Scientific Scimed, Inc. | Ballonnet d'ablation à couche de revêtement déposée en phase vapeur |
| EP3057488B1 (fr) | 2013-10-14 | 2018-05-16 | Boston Scientific Scimed, Inc. | Cathéter de cartographie cardiaque à haute résolution comportant un ensemble d'électrodes |
| US11246654B2 (en) | 2013-10-14 | 2022-02-15 | Boston Scientific Scimed, Inc. | Flexible renal nerve ablation devices and related methods of use and manufacture |
| US9770606B2 (en) | 2013-10-15 | 2017-09-26 | Boston Scientific Scimed, Inc. | Ultrasound ablation catheter with cooling infusion and centering basket |
| WO2015057584A1 (fr) | 2013-10-15 | 2015-04-23 | Boston Scientific Scimed, Inc. | Ballonnet de dispositif médical |
| JP6259099B2 (ja) | 2013-10-18 | 2018-01-10 | ボストン サイエンティフィック サイムド,インコーポレイテッドBoston Scientific Scimed,Inc. | 可撓性を備える導電性ワイヤを備えるバルーン・カテーテル、並びに関連する使用および製造方法 |
| JP2016534842A (ja) | 2013-10-25 | 2016-11-10 | ボストン サイエンティフィック サイムド,インコーポレイテッドBoston Scientific Scimed,Inc. | 除神経フレックス回路における埋め込み熱電対 |
| CN105899157B (zh) | 2014-01-06 | 2019-08-09 | 波士顿科学国际有限公司 | 抗撕裂柔性电路组件 |
| US10525171B2 (en) | 2014-01-24 | 2020-01-07 | The Spectranetics Corporation | Coatings for medical devices |
| JP6325121B2 (ja) | 2014-02-04 | 2018-05-16 | ボストン サイエンティフィック サイムド,インコーポレイテッドBoston Scientific Scimed,Inc. | 双極電極上の温度センサの代替配置 |
| US11000679B2 (en) | 2014-02-04 | 2021-05-11 | Boston Scientific Scimed, Inc. | Balloon protection and rewrapping devices and related methods of use |
| US10709490B2 (en) | 2014-05-07 | 2020-07-14 | Medtronic Ardian Luxembourg S.A.R.L. | Catheter assemblies comprising a direct heating element for renal neuromodulation and associated systems and methods |
| JP2016005533A (ja) * | 2014-05-30 | 2016-01-14 | 株式会社日本ステントテクノロジー | ステント |
| US9700664B2 (en) | 2015-04-01 | 2017-07-11 | Elwha Llc | Implantable heart treatment systems, devices, and methods |
| US9675812B2 (en) | 2015-04-01 | 2017-06-13 | Elwha Llc | Implantable heart treatment systems, devices, and methods |
| US9682245B2 (en) | 2015-04-01 | 2017-06-20 | Elwha Llc | Implantable heart treatment systems, devices, and methods |
| WO2017035002A1 (fr) | 2015-08-21 | 2017-03-02 | Twelve Inc. | Dispositifs de valves cardiaques implantables, dispositifs de réparation de valves mitrales et systèmes et procédés associés |
| CN109069272A (zh) | 2016-04-29 | 2018-12-21 | 美敦力瓦斯科尔勒公司 | 具有带系绳的锚定件的假体心脏瓣膜设备以及相关联的系统和方法 |
| IL265511B (en) * | 2016-12-22 | 2022-07-01 | Sino Medical Sciences Tech Inc | A stent containing a drug for elution and a method for using it to enable restoration of endothelial cell layer function |
| US10575950B2 (en) | 2017-04-18 | 2020-03-03 | Twelve, Inc. | Hydraulic systems for delivering prosthetic heart valve devices and associated methods |
| US10702378B2 (en) | 2017-04-18 | 2020-07-07 | Twelve, Inc. | Prosthetic heart valve device and associated systems and methods |
| US10433961B2 (en) | 2017-04-18 | 2019-10-08 | Twelve, Inc. | Delivery systems with tethers for prosthetic heart valve devices and associated methods |
| US10792151B2 (en) | 2017-05-11 | 2020-10-06 | Twelve, Inc. | Delivery systems for delivering prosthetic heart valve devices and associated methods |
| US10646338B2 (en) | 2017-06-02 | 2020-05-12 | Twelve, Inc. | Delivery systems with telescoping capsules for deploying prosthetic heart valve devices and associated methods |
| US10709591B2 (en) | 2017-06-06 | 2020-07-14 | Twelve, Inc. | Crimping device and method for loading stents and prosthetic heart valves |
| US10729541B2 (en) | 2017-07-06 | 2020-08-04 | Twelve, Inc. | Prosthetic heart valve devices and associated systems and methods |
| US10786352B2 (en) | 2017-07-06 | 2020-09-29 | Twelve, Inc. | Prosthetic heart valve devices and associated systems and methods |
| EP3459469A1 (fr) | 2017-09-23 | 2019-03-27 | Universität Zürich | Dispositif occlusif médical |
| CN111565674A (zh) * | 2017-10-11 | 2020-08-21 | 艾奎登医疗公司 | 主动脉夹层的治疗系统和方法 |
| US11260216B2 (en) | 2017-12-01 | 2022-03-01 | Cardiac Pacemakers, Inc. | Methods and systems for detecting atrial contraction timing fiducials during ventricular filling from a ventricularly implanted leadless cardiac pacemaker |
| US11071870B2 (en) | 2017-12-01 | 2021-07-27 | Cardiac Pacemakers, Inc. | Methods and systems for detecting atrial contraction timing fiducials and determining a cardiac interval from a ventricularly implanted leadless cardiac pacemaker |
| CN111417432B (zh) | 2017-12-01 | 2024-04-30 | 心脏起搏器股份公司 | 具有复归行为的无引线心脏起搏器 |
| US11116561B2 (en) | 2018-01-24 | 2021-09-14 | Medtronic Ardian Luxembourg S.A.R.L. | Devices, agents, and associated methods for selective modulation of renal nerves |
| KR102322711B1 (ko) * | 2019-08-20 | 2021-11-04 | 주식회사 포스코 | 수용성 고분자 담지체를 포함하는 혈관 문합 장치 |
| WO2021059273A2 (fr) | 2019-09-26 | 2021-04-01 | Universitat Zurich | Dispositifs de fermeture de l'auricule gauche |
| CN112370634B (zh) * | 2020-11-03 | 2023-04-25 | 山东华安生物科技有限公司 | 一种复合管及其制备方法和应用 |
| WO2022271595A1 (fr) | 2021-06-23 | 2022-12-29 | International Imaging Materials, Inc. | Élément d'imagerie thermographique |
Family Cites Families (67)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| ZA737247B (en) * | 1972-09-29 | 1975-04-30 | Ayerst Mckenna & Harrison | Rapamycin and process of preparation |
| US3993749A (en) | 1974-04-12 | 1976-11-23 | Ayerst Mckenna And Harrison Ltd. | Rapamycin and process of preparation |
| US4885171A (en) * | 1978-11-03 | 1989-12-05 | American Home Products Corporation | Use of rapamycin in treatment of certain tumors |
| US4316885A (en) * | 1980-08-25 | 1982-02-23 | Ayerst, Mckenna And Harrison, Inc. | Acyl derivatives of rapamycin |
| US4401653A (en) | 1981-03-09 | 1983-08-30 | Ayerst, Mckenna & Harrison Inc. | Combination of rapamycin and picibanil for the treatment of tumors |
| US4894366A (en) | 1984-12-03 | 1990-01-16 | Fujisawa Pharmaceutical Company, Ltd. | Tricyclo compounds, a process for their production and a pharmaceutical composition containing the same |
| EP0163829B1 (fr) * | 1984-03-21 | 1989-08-23 | Nippon Telegraph And Telephone Corporation | Dispositif pour le traitement des signaux de parole |
| US4580568A (en) | 1984-10-01 | 1986-04-08 | Cook, Incorporated | Percutaneous endovascular stent and method for insertion thereof |
| US4733665C2 (en) | 1985-11-07 | 2002-01-29 | Expandable Grafts Partnership | Expandable intraluminal graft and method and apparatus for implanting an expandable intraluminal graft |
| US4650803A (en) | 1985-12-06 | 1987-03-17 | University Of Kansas | Prodrugs of rapamycin |
| US5527337A (en) * | 1987-06-25 | 1996-06-18 | Duke University | Bioabsorbable stent and method of making the same |
| US4916193A (en) * | 1987-12-17 | 1990-04-10 | Allied-Signal Inc. | Medical devices fabricated totally or in part from copolymers of recurring units derived from cyclic carbonates and lactides |
| US5092877A (en) * | 1988-09-01 | 1992-03-03 | Corvita Corporation | Radially expandable endoprosthesis |
| US4994071A (en) * | 1989-05-22 | 1991-02-19 | Cordis Corporation | Bifurcating stent apparatus and method |
| US5304121A (en) | 1990-12-28 | 1994-04-19 | Boston Scientific Corporation | Drug delivery system making use of a hydrogel polymer coating |
| WO1991017724A1 (fr) | 1990-05-17 | 1991-11-28 | Harbor Medical Devices, Inc. | Polymere utilise dans un dispositif medical |
| JPH04230389A (ja) | 1990-07-16 | 1992-08-19 | American Home Prod Corp | ラパマイシン誘導体 |
| US5023262A (en) | 1990-08-14 | 1991-06-11 | American Home Products Corporation | Hydrogenated rapamycin derivatives |
| US5163952A (en) | 1990-09-14 | 1992-11-17 | Michael Froix | Expandable polymeric stent with memory and delivery apparatus and method |
| PT98990A (pt) | 1990-09-19 | 1992-08-31 | American Home Prod | Processo para a preparacao de esteres de acidos carboxilicos de rapamicina |
| US5120842A (en) * | 1991-04-01 | 1992-06-09 | American Home Products Corporation | Silyl ethers of rapamycin |
| US5120725A (en) * | 1991-05-29 | 1992-06-09 | American Home Products Corporation | Bicyclic rapamycins |
| US5120727A (en) | 1991-05-29 | 1992-06-09 | American Home Products Corporation | Rapamycin dimers |
| US6090901A (en) | 1991-07-05 | 2000-07-18 | Biocompatibles Limited | Polymeric surface coatings |
| US5705583A (en) | 1991-07-05 | 1998-01-06 | Biocompatibles Limited | Polymeric surface coatings |
| US5457111A (en) | 1991-09-05 | 1995-10-10 | Abbott Laboratories | Macrocyclic immunomodulators |
| US5516781A (en) * | 1992-01-09 | 1996-05-14 | American Home Products Corporation | Method of treating restenosis with rapamycin |
| US5177203A (en) * | 1992-03-05 | 1993-01-05 | American Home Products Corporation | Rapamycin 42-sulfonates and 42-(N-carboalkoxy) sulfamates useful as immunosuppressive agents |
| US5355832A (en) | 1992-12-15 | 1994-10-18 | Advanced Surface Technology, Inc. | Polymerization reactor |
| US5464650A (en) | 1993-04-26 | 1995-11-07 | Medtronic, Inc. | Intravascular stent and method |
| US5994341A (en) * | 1993-07-19 | 1999-11-30 | Angiogenesis Technologies, Inc. | Anti-angiogenic Compositions and methods for the treatment of arthritis |
| CA2134997C (fr) | 1994-11-03 | 2009-06-02 | Ian M. Penn | Stent |
| FR2730231B1 (fr) * | 1995-02-02 | 1997-04-04 | Fournier Sca Lab | Association de fenofibrate et de vitamine e, utilisation en therapeutique |
| US5605696A (en) | 1995-03-30 | 1997-02-25 | Advanced Cardiovascular Systems, Inc. | Drug loaded polymeric material and method of manufacture |
| US6099562A (en) * | 1996-06-13 | 2000-08-08 | Schneider (Usa) Inc. | Drug coating with topcoat |
| US5837313A (en) | 1995-04-19 | 1998-11-17 | Schneider (Usa) Inc | Drug release stent coating process |
| AU5675196A (en) * | 1995-06-08 | 1997-01-09 | Bard Galway Limited | Endovascular stent |
| BE1009856A5 (fr) * | 1995-07-14 | 1997-10-07 | Sandoz Sa | Composition pharmaceutique sous la forme d'une dispersion solide comprenant un macrolide et un vehicule. |
| GB9522332D0 (en) | 1995-11-01 | 1996-01-03 | Biocompatibles Ltd | Braided stent |
| US5722984A (en) * | 1996-01-16 | 1998-03-03 | Iso Stent, Inc. | Antithrombogenic radioactive coating for an intravascular stent |
| US5827321A (en) * | 1997-02-07 | 1998-10-27 | Cornerstone Devices, Inc. | Non-Foreshortening intraluminal prosthesis |
| US6273913B1 (en) * | 1997-04-18 | 2001-08-14 | Cordis Corporation | Modified stent useful for delivery of drugs along stent strut |
| US6233550B1 (en) * | 1997-08-29 | 2001-05-15 | The Regents Of The University Of California | Method and apparatus for hybrid coding of speech at 4kbps |
| US6015815A (en) | 1997-09-26 | 2000-01-18 | Abbott Laboratories | Tetrazole-containing rapamycin analogs with shortened half-lives |
| US6890546B2 (en) * | 1998-09-24 | 2005-05-10 | Abbott Laboratories | Medical devices containing rapamycin analogs |
| US20030129215A1 (en) * | 1998-09-24 | 2003-07-10 | T-Ram, Inc. | Medical devices containing rapamycin analogs |
| US8257725B2 (en) * | 1997-09-26 | 2012-09-04 | Abbott Laboratories | Delivery of highly lipophilic agents via medical devices |
| US20010029351A1 (en) * | 1998-04-16 | 2001-10-11 | Robert Falotico | Drug combinations and delivery devices for the prevention and treatment of vascular disease |
| US8029561B1 (en) * | 2000-05-12 | 2011-10-04 | Cordis Corporation | Drug combination useful for prevention of restenosis |
| US6153252A (en) * | 1998-06-30 | 2000-11-28 | Ethicon, Inc. | Process for coating stents |
| AU771367B2 (en) * | 1998-08-20 | 2004-03-18 | Cook Medical Technologies Llc | Coated implantable medical device |
| US20060240070A1 (en) * | 1998-09-24 | 2006-10-26 | Cromack Keith R | Delivery of highly lipophilic agents via medical devices |
| US8257724B2 (en) * | 1998-09-24 | 2012-09-04 | Abbott Laboratories | Delivery of highly lipophilic agents via medical devices |
| US6419692B1 (en) * | 1999-02-03 | 2002-07-16 | Scimed Life Systems, Inc. | Surface protection method for stents and balloon catheters for drug delivery |
| US6610317B2 (en) * | 1999-05-27 | 2003-08-26 | Acusphere, Inc. | Porous paclitaxel matrices and methods of manufacture thereof |
| US6510407B1 (en) * | 1999-10-19 | 2003-01-21 | Atmel Corporation | Method and apparatus for variable rate coding of speech |
| GB0100760D0 (en) * | 2001-01-11 | 2001-02-21 | Biocompatibles Ltd | Drug delivery from stents |
| WO2002085253A1 (fr) * | 2001-04-20 | 2002-10-31 | The Board Of Trustees Of The Leland Stanford Junior University | Plate-forme d'administration de medicaments et procedes d'inhibition de la formation de la neointima |
| WO2003057218A1 (fr) * | 2002-01-10 | 2003-07-17 | Novartis Ag | Systemes de liberation de medicament pour la prevention et le traitement de maladies vasculaires, comprenant de la rapamycine et des derives de celle-ci |
| US20030181973A1 (en) * | 2002-03-20 | 2003-09-25 | Harvinder Sahota | Reduced restenosis drug containing stents |
| PA8577501A1 (es) * | 2002-07-25 | 2004-02-07 | Warner Lambert Co | Inhibidores de quinasas |
| EP3175870A1 (fr) * | 2002-09-06 | 2017-06-07 | Abbott Laboratories | Dispositif médical doté d'un inhibiteur de l'hydratation |
| EP1596895B1 (fr) * | 2003-02-18 | 2009-02-04 | Medtronic, Inc. | Derivation interne pour hydrocephalie resistant a l'occlusion |
| US20050033417A1 (en) * | 2003-07-31 | 2005-02-10 | John Borges | Coating for controlled release of a therapeutic agent |
| US20050288481A1 (en) * | 2004-04-30 | 2005-12-29 | Desnoyer Jessica R | Design of poly(ester amides) for the control of agent-release from polymeric compositions |
| US7820732B2 (en) * | 2004-04-30 | 2010-10-26 | Advanced Cardiovascular Systems, Inc. | Methods for modulating thermal and mechanical properties of coatings on implantable devices |
| US7906134B2 (en) * | 2005-12-21 | 2011-03-15 | Abbott Laboratories | Room temperature-curable polymers |
-
2006
- 2006-03-22 EP EP20060739194 patent/EP1868663B1/fr active Active
- 2006-03-22 AT AT06739194T patent/ATE533520T1/de active
- 2006-03-22 EP EP20100183267 patent/EP2327429B1/fr active Active
- 2006-03-22 JP JP2008503102A patent/JP5271697B2/ja active Active
- 2006-03-22 US US11/886,815 patent/US20090216317A1/en not_active Abandoned
- 2006-03-22 WO PCT/US2006/010307 patent/WO2006102359A2/fr active Application Filing
- 2006-03-23 TW TW95110143A patent/TWI455708B/zh not_active IP Right Cessation
-
2014
- 2014-12-31 US US14/588,053 patent/US20150112425A1/en not_active Abandoned
Also Published As
| Publication number | Publication date |
|---|---|
| ATE533520T1 (de) | 2011-12-15 |
| US20150112425A1 (en) | 2015-04-23 |
| EP1868663A2 (fr) | 2007-12-26 |
| WO2006102359A3 (fr) | 2007-05-10 |
| TWI455708B (zh) | 2014-10-11 |
| US20090216317A1 (en) | 2009-08-27 |
| EP2327429A1 (fr) | 2011-06-01 |
| TW200722064A (en) | 2007-06-16 |
| WO2006102359A2 (fr) | 2006-09-28 |
| EP2327429B1 (fr) | 2014-09-17 |
| JP2008534058A (ja) | 2008-08-28 |
| JP5271697B2 (ja) | 2013-08-21 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| EP1868663B1 (fr) | Distribution d'agents hautement lipophiles au moyen de dispositifs medicaux | |
| US8257724B2 (en) | Delivery of highly lipophilic agents via medical devices | |
| US8257725B2 (en) | Delivery of highly lipophilic agents via medical devices | |
| US20060240070A1 (en) | Delivery of highly lipophilic agents via medical devices | |
| AU2003218077B2 (en) | Medical device having hydration inhibitor | |
| US7445792B2 (en) | Medical device having a hydration inhibitor | |
| US8318190B2 (en) | Method of treating disorders using compositions comprising zotarolimus and paclitaxel | |
| TWI435724B (zh) | 組合物、系統、套組及使用醫藥裝置施加雷帕黴素(rapamycin)類似物及紫杉醇之方法 | |
| US20090162413A1 (en) | Compositions and methods of administering rapamycin analogs with paclitaxel using medical devices | |
| US20090060970A1 (en) | Compositions and methods of administering paclitaxel with other drugs using medical devices | |
| WO2008063319A2 (fr) | Procédés d'administration d'analogues à la rapamycine avec des anti-inflammatoires au moyen de dispositifs médicaux |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| PUAI | Public reference made under article 153(3) epc to a published international application that has entered the european phase |
Free format text: ORIGINAL CODE: 0009012 |
|
| 17P | Request for examination filed |
Effective date: 20071012 |
|
| AK | Designated contracting states |
Kind code of ref document: A2 Designated state(s): AT BE BG CH CY CZ DE DK EE ES FI FR GB GR HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI SK TR |
|
| DAX | Request for extension of the european patent (deleted) | ||
| 17Q | First examination report despatched |
Effective date: 20080605 |
|
| GRAP | Despatch of communication of intention to grant a patent |
Free format text: ORIGINAL CODE: EPIDOSNIGR1 |
|
| GRAS | Grant fee paid |
Free format text: ORIGINAL CODE: EPIDOSNIGR3 |
|
| GRAA | (expected) grant |
Free format text: ORIGINAL CODE: 0009210 |
|
| AK | Designated contracting states |
Kind code of ref document: B1 Designated state(s): AT BE BG CH CY CZ DE DK EE ES FI FR GB GR HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI SK TR |
|
| REG | Reference to a national code |
Ref country code: GB Ref legal event code: FG4D |
|
| REG | Reference to a national code |
Ref country code: CH Ref legal event code: EP |
|
| REG | Reference to a national code |
Ref country code: IE Ref legal event code: FG4D |
|
| REG | Reference to a national code |
Ref country code: DE Ref legal event code: R096 Ref document number: 602006025851 Country of ref document: DE Effective date: 20120126 |
|
| REG | Reference to a national code |
Ref country code: NL Ref legal event code: VDEP Effective date: 20111116 |
|
| LTIE | Lt: invalidation of european patent or patent extension |
Effective date: 20111116 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: LT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: IS Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20120316 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: SE Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: PL Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: GR Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20120217 Ref country code: NL Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: BE Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: SI Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: LV Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: PT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20120316 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: CY Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: EE Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: SK Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: CZ Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: DK Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: BG Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20120216 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: RO Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: IT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 |
|
| REG | Reference to a national code |
Ref country code: AT Ref legal event code: MK05 Ref document number: 533520 Country of ref document: AT Kind code of ref document: T Effective date: 20111116 |
|
| PLBE | No opposition filed within time limit |
Free format text: ORIGINAL CODE: 0009261 |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: NO OPPOSITION FILED WITHIN TIME LIMIT |
|
| 26N | No opposition filed |
Effective date: 20120817 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: MC Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20120331 |
|
| REG | Reference to a national code |
Ref country code: CH Ref legal event code: PL |
|
| REG | Reference to a national code |
Ref country code: DE Ref legal event code: R097 Ref document number: 602006025851 Country of ref document: DE Effective date: 20120817 |
|
| REG | Reference to a national code |
Ref country code: IE Ref legal event code: MM4A |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: IE Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20120322 Ref country code: LI Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20120331 Ref country code: AT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 Ref country code: CH Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20120331 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: ES Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20120227 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: FI Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: TR Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20111116 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: LU Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20120322 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: HU Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20060322 |
|
| REG | Reference to a national code |
Ref country code: FR Ref legal event code: PLFP Year of fee payment: 11 |
|
| REG | Reference to a national code |
Ref country code: FR Ref legal event code: PLFP Year of fee payment: 12 |
|
| REG | Reference to a national code |
Ref country code: FR Ref legal event code: PLFP Year of fee payment: 13 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: GB Payment date: 20180223 Year of fee payment: 13 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: FR Payment date: 20180223 Year of fee payment: 13 |
|
| GBPC | Gb: european patent ceased through non-payment of renewal fee |
Effective date: 20190322 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: GB Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20190322 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: FR Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20190331 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: DE Payment date: 20230210 Year of fee payment: 18 |
|
| P01 | Opt-out of the competence of the unified patent court (upc) registered |
Effective date: 20230530 |