EP1315470B1 - System for mammalian joint resurfacing - Google Patents
System for mammalian joint resurfacing Download PDFInfo
- Publication number
- EP1315470B1 EP1315470B1 EP01964653A EP01964653A EP1315470B1 EP 1315470 B1 EP1315470 B1 EP 1315470B1 EP 01964653 A EP01964653 A EP 01964653A EP 01964653 A EP01964653 A EP 01964653A EP 1315470 B1 EP1315470 B1 EP 1315470B1
- Authority
- EP
- European Patent Office
- Prior art keywords
- implant
- component
- vivo
- diisocyanates
- preformed
- Prior art date
- Legal status (The legal status is an assumption and is not a legal conclusion. Google has not performed a legal analysis and makes no representation as to the accuracy of the status listed.)
- Expired - Lifetime
Links
- 239000012620 biological material Substances 0.000 claims abstract description 65
- 238000011065 in-situ storage Methods 0.000 claims abstract description 45
- 238000000034 method Methods 0.000 claims abstract description 34
- 230000009969 flowable effect Effects 0.000 claims abstract description 28
- 238000012986 modification Methods 0.000 claims abstract description 4
- 230000004048 modification Effects 0.000 claims abstract description 4
- 239000000463 material Substances 0.000 claims description 55
- 239000007943 implant Substances 0.000 claims description 53
- 210000000988 bone and bone Anatomy 0.000 claims description 47
- 229920000642 polymer Polymers 0.000 claims description 26
- 239000004814 polyurethane Substances 0.000 claims description 22
- 229920002635 polyurethane Polymers 0.000 claims description 16
- 239000012948 isocyanate Substances 0.000 claims description 15
- 150000002513 isocyanates Chemical class 0.000 claims description 15
- 239000000853 adhesive Substances 0.000 claims description 10
- 230000001070 adhesive effect Effects 0.000 claims description 10
- 230000008569 process Effects 0.000 claims description 9
- 102000008186 Collagen Human genes 0.000 claims description 5
- 108010035532 Collagen Proteins 0.000 claims description 5
- 229920001436 collagen Polymers 0.000 claims description 5
- 125000001931 aliphatic group Chemical group 0.000 claims description 4
- 125000003118 aryl group Chemical group 0.000 claims description 4
- 238000000465 moulding Methods 0.000 claims description 4
- 210000004872 soft tissue Anatomy 0.000 claims description 4
- 102000004127 Cytokines Human genes 0.000 claims description 3
- 108090000695 Cytokines Proteins 0.000 claims description 3
- 239000013543 active substance Substances 0.000 claims description 3
- 150000001412 amines Chemical class 0.000 claims description 3
- HIFVAOIJYDXIJG-UHFFFAOYSA-N benzylbenzene;isocyanic acid Chemical class N=C=O.N=C=O.C=1C=CC=CC=1CC1=CC=CC=C1 HIFVAOIJYDXIJG-UHFFFAOYSA-N 0.000 claims description 3
- 229910052588 hydroxylapatite Inorganic materials 0.000 claims description 3
- XYJRXVWERLGGKC-UHFFFAOYSA-D pentacalcium;hydroxide;triphosphate Chemical compound [OH-].[Ca+2].[Ca+2].[Ca+2].[Ca+2].[Ca+2].[O-]P([O-])([O-])=O.[O-]P([O-])([O-])=O.[O-]P([O-])([O-])=O XYJRXVWERLGGKC-UHFFFAOYSA-D 0.000 claims description 3
- 125000006850 spacer group Chemical group 0.000 claims description 3
- DVKJHBMWWAPEIU-UHFFFAOYSA-N toluene 2,4-diisocyanate Chemical class CC1=CC=C(N=C=O)C=C1N=C=O DVKJHBMWWAPEIU-UHFFFAOYSA-N 0.000 claims description 3
- MTZUIIAIAKMWLI-UHFFFAOYSA-N 1,2-diisocyanatobenzene Chemical class O=C=NC1=CC=CC=C1N=C=O MTZUIIAIAKMWLI-UHFFFAOYSA-N 0.000 claims description 2
- WWEXBGFSEVKZNE-UHFFFAOYSA-N N=C=O.N=C=O.C1=CC=CC2=CC=CC=C21 Chemical class N=C=O.N=C=O.C1=CC=CC2=CC=CC=C21 WWEXBGFSEVKZNE-UHFFFAOYSA-N 0.000 claims description 2
- OMRDSWJXRLDPBB-UHFFFAOYSA-N N=C=O.N=C=O.C1CCCCC1 Chemical class N=C=O.N=C=O.C1CCCCC1 OMRDSWJXRLDPBB-UHFFFAOYSA-N 0.000 claims description 2
- 239000006096 absorbing agent Substances 0.000 claims description 2
- KIQKWYUGPPFMBV-UHFFFAOYSA-N diisocyanatomethane Chemical class O=C=NCN=C=O KIQKWYUGPPFMBV-UHFFFAOYSA-N 0.000 claims description 2
- RRAMGCGOFNQTLD-UHFFFAOYSA-N hexamethylene diisocyanate Chemical class O=C=NCCCCCCN=C=O RRAMGCGOFNQTLD-UHFFFAOYSA-N 0.000 claims description 2
- 239000001257 hydrogen Substances 0.000 claims description 2
- 229910052739 hydrogen Inorganic materials 0.000 claims description 2
- 125000002887 hydroxy group Chemical group [H]O* 0.000 claims description 2
- NIMLQBUJDJZYEJ-UHFFFAOYSA-N isophorone diisocyanate Chemical class CC1(C)CC(N=C=O)CC(C)(CN=C=O)C1 NIMLQBUJDJZYEJ-UHFFFAOYSA-N 0.000 claims description 2
- 208000031737 Tissue Adhesions Diseases 0.000 claims 1
- 238000001727 in vivo Methods 0.000 abstract description 21
- 238000002360 preparation method Methods 0.000 abstract description 16
- 239000002131 composite material Substances 0.000 abstract description 10
- 230000007774 longterm Effects 0.000 abstract description 8
- 238000003780 insertion Methods 0.000 abstract description 6
- 230000037431 insertion Effects 0.000 abstract description 6
- 230000000399 orthopedic effect Effects 0.000 abstract description 4
- 239000000203 mixture Substances 0.000 description 43
- 210000001519 tissue Anatomy 0.000 description 27
- 238000001723 curing Methods 0.000 description 24
- 230000000875 corresponding effect Effects 0.000 description 21
- 239000010410 layer Substances 0.000 description 17
- 150000003077 polyols Chemical class 0.000 description 14
- 150000002009 diols Chemical class 0.000 description 13
- 210000003127 knee Anatomy 0.000 description 12
- 229920005862 polyol Polymers 0.000 description 12
- 239000004970 Chain extender Substances 0.000 description 11
- 239000003054 catalyst Substances 0.000 description 11
- -1 polyethylene Polymers 0.000 description 10
- 238000006243 chemical reaction Methods 0.000 description 9
- 239000000835 fiber Substances 0.000 description 9
- 239000012783 reinforcing fiber Substances 0.000 description 9
- 238000012937 correction Methods 0.000 description 8
- 125000005442 diisocyanate group Chemical group 0.000 description 8
- 230000014759 maintenance of location Effects 0.000 description 8
- 229920003224 poly(trimethylene oxide) Polymers 0.000 description 8
- UPMLOUAZCHDJJD-UHFFFAOYSA-N 4,4'-Diphenylmethane Diisocyanate Chemical compound C1=CC(N=C=O)=CC=C1CC1=CC=C(N=C=O)C=C1 UPMLOUAZCHDJJD-UHFFFAOYSA-N 0.000 description 7
- 239000000654 additive Substances 0.000 description 7
- 238000004873 anchoring Methods 0.000 description 7
- PEDCQBHIVMGVHV-UHFFFAOYSA-N Glycerine Chemical compound OCC(O)CO PEDCQBHIVMGVHV-UHFFFAOYSA-N 0.000 description 6
- 230000008901 benefit Effects 0.000 description 6
- WERYXYBDKMZEQL-UHFFFAOYSA-N butane-1,4-diol Chemical compound OCCCCO WERYXYBDKMZEQL-UHFFFAOYSA-N 0.000 description 6
- 210000000845 cartilage Anatomy 0.000 description 6
- 238000002156 mixing Methods 0.000 description 6
- 239000004744 fabric Substances 0.000 description 5
- 210000001624 hip Anatomy 0.000 description 5
- 230000002209 hydrophobic effect Effects 0.000 description 5
- 230000003993 interaction Effects 0.000 description 5
- 229920001228 polyisocyanate Polymers 0.000 description 5
- 239000005056 polyisocyanate Substances 0.000 description 5
- 229920001296 polysiloxane Polymers 0.000 description 5
- 229920000909 polytetrahydrofuran Polymers 0.000 description 5
- 230000000717 retained effect Effects 0.000 description 5
- KAKZBPTYRLMSJV-UHFFFAOYSA-N Butadiene Chemical compound C=CC=C KAKZBPTYRLMSJV-UHFFFAOYSA-N 0.000 description 4
- 229920002121 Hydroxyl-terminated polybutadiene Polymers 0.000 description 4
- RRHGJUQNOFWUDK-UHFFFAOYSA-N Isoprene Chemical compound CC(=C)C=C RRHGJUQNOFWUDK-UHFFFAOYSA-N 0.000 description 4
- PPBRXRYQALVLMV-UHFFFAOYSA-N Styrene Chemical compound C=CC1=CC=CC=C1 PPBRXRYQALVLMV-UHFFFAOYSA-N 0.000 description 4
- 238000005299 abrasion Methods 0.000 description 4
- 230000000996 additive effect Effects 0.000 description 4
- 239000003963 antioxidant agent Substances 0.000 description 4
- 229920001577 copolymer Polymers 0.000 description 4
- 239000004615 ingredient Substances 0.000 description 4
- 239000004745 nonwoven fabric Substances 0.000 description 4
- 238000007493 shaping process Methods 0.000 description 4
- 238000001356 surgical procedure Methods 0.000 description 4
- IMNIMPAHZVJRPE-UHFFFAOYSA-N triethylenediamine Chemical compound C1CN2CCN1CC2 IMNIMPAHZVJRPE-UHFFFAOYSA-N 0.000 description 4
- 239000004593 Epoxy Substances 0.000 description 3
- WSFSSNUMVMOOMR-UHFFFAOYSA-N Formaldehyde Chemical compound O=C WSFSSNUMVMOOMR-UHFFFAOYSA-N 0.000 description 3
- 229920001730 Moisture cure polyurethane Polymers 0.000 description 3
- 229920002396 Polyurea Polymers 0.000 description 3
- ZMANZCXQSJIPKH-UHFFFAOYSA-N Triethylamine Chemical compound CCN(CC)CC ZMANZCXQSJIPKH-UHFFFAOYSA-N 0.000 description 3
- 229920001222 biopolymer Polymers 0.000 description 3
- 239000007795 chemical reaction product Substances 0.000 description 3
- 238000000576 coating method Methods 0.000 description 3
- 239000003431 cross linking reagent Substances 0.000 description 3
- MTHSVFCYNBDYFN-UHFFFAOYSA-N diethylene glycol Chemical compound OCCOCCO MTHSVFCYNBDYFN-UHFFFAOYSA-N 0.000 description 3
- 239000000975 dye Substances 0.000 description 3
- 125000003700 epoxy group Chemical group 0.000 description 3
- 238000011049 filling Methods 0.000 description 3
- 238000009472 formulation Methods 0.000 description 3
- 238000010438 heat treatment Methods 0.000 description 3
- 239000000017 hydrogel Substances 0.000 description 3
- 238000003384 imaging method Methods 0.000 description 3
- 238000002513 implantation Methods 0.000 description 3
- 210000003041 ligament Anatomy 0.000 description 3
- 239000007788 liquid Substances 0.000 description 3
- 238000004519 manufacturing process Methods 0.000 description 3
- 229920000058 polyacrylate Polymers 0.000 description 3
- 229920000647 polyepoxide Polymers 0.000 description 3
- 229920000728 polyester Polymers 0.000 description 3
- 239000000047 product Substances 0.000 description 3
- 238000004513 sizing Methods 0.000 description 3
- 239000007787 solid Substances 0.000 description 3
- 238000003860 storage Methods 0.000 description 3
- 239000000126 substance Substances 0.000 description 3
- PAYRUJLWNCNPSJ-UHFFFAOYSA-N Aniline Chemical compound NC1=CC=CC=C1 PAYRUJLWNCNPSJ-UHFFFAOYSA-N 0.000 description 2
- 229920003171 Poly (ethylene oxide) Polymers 0.000 description 2
- 239000004698 Polyethylene Substances 0.000 description 2
- 239000004743 Polypropylene Substances 0.000 description 2
- ATJFFYVFTNAWJD-UHFFFAOYSA-N Tin Chemical compound [Sn] ATJFFYVFTNAWJD-UHFFFAOYSA-N 0.000 description 2
- RTAQQCXQSZGOHL-UHFFFAOYSA-N Titanium Chemical compound [Ti] RTAQQCXQSZGOHL-UHFFFAOYSA-N 0.000 description 2
- 229910052782 aluminium Inorganic materials 0.000 description 2
- XAGFODPZIPBFFR-UHFFFAOYSA-N aluminium Chemical compound [Al] XAGFODPZIPBFFR-UHFFFAOYSA-N 0.000 description 2
- 230000003078 antioxidant effect Effects 0.000 description 2
- 230000015572 biosynthetic process Effects 0.000 description 2
- 239000013590 bulk material Substances 0.000 description 2
- 239000000919 ceramic Substances 0.000 description 2
- 238000010382 chemical cross-linking Methods 0.000 description 2
- 230000002596 correlated effect Effects 0.000 description 2
- 238000004132 cross linking Methods 0.000 description 2
- 150000004985 diamines Chemical class 0.000 description 2
- 238000005553 drilling Methods 0.000 description 2
- 230000000694 effects Effects 0.000 description 2
- 238000011156 evaluation Methods 0.000 description 2
- 239000002657 fibrous material Substances 0.000 description 2
- 239000003292 glue Substances 0.000 description 2
- 238000007373 indentation Methods 0.000 description 2
- 238000001746 injection moulding Methods 0.000 description 2
- 238000007689 inspection Methods 0.000 description 2
- 229910052751 metal Inorganic materials 0.000 description 2
- 239000002184 metal Substances 0.000 description 2
- 150000002739 metals Chemical class 0.000 description 2
- 201000008482 osteoarthritis Diseases 0.000 description 2
- 229920000515 polycarbonate Polymers 0.000 description 2
- 239000004417 polycarbonate Substances 0.000 description 2
- 229920000573 polyethylene Polymers 0.000 description 2
- 229920001155 polypropylene Polymers 0.000 description 2
- 229920001451 polypropylene glycol Polymers 0.000 description 2
- 238000007788 roughening Methods 0.000 description 2
- 230000000087 stabilizing effect Effects 0.000 description 2
- 230000003068 static effect Effects 0.000 description 2
- 230000001954 sterilising effect Effects 0.000 description 2
- 238000004659 sterilization and disinfection Methods 0.000 description 2
- 239000010936 titanium Substances 0.000 description 2
- 229910052719 titanium Inorganic materials 0.000 description 2
- GETQZCLCWQTVFV-UHFFFAOYSA-N trimethylamine Chemical compound CN(C)C GETQZCLCWQTVFV-UHFFFAOYSA-N 0.000 description 2
- 239000002759 woven fabric Substances 0.000 description 2
- 210000000707 wrist Anatomy 0.000 description 2
- LFSYUSUFCBOHGU-UHFFFAOYSA-N 1-isocyanato-2-[(4-isocyanatophenyl)methyl]benzene Chemical compound C1=CC(N=C=O)=CC=C1CC1=CC=CC=C1N=C=O LFSYUSUFCBOHGU-UHFFFAOYSA-N 0.000 description 1
- VOZKAJLKRJDJLL-UHFFFAOYSA-N 2,4-diaminotoluene Chemical compound CC1=CC=C(N)C=C1N VOZKAJLKRJDJLL-UHFFFAOYSA-N 0.000 description 1
- QWGRWMMWNDWRQN-UHFFFAOYSA-N 2-methylpropane-1,3-diol Chemical compound OCC(C)CO QWGRWMMWNDWRQN-UHFFFAOYSA-N 0.000 description 1
- QGMGHALXLXKCBD-UHFFFAOYSA-N 4-amino-n-(2-aminophenyl)benzamide Chemical compound C1=CC(N)=CC=C1C(=O)NC1=CC=CC=C1N QGMGHALXLXKCBD-UHFFFAOYSA-N 0.000 description 1
- NLHHRLWOUZZQLW-UHFFFAOYSA-N Acrylonitrile Chemical compound C=CC#N NLHHRLWOUZZQLW-UHFFFAOYSA-N 0.000 description 1
- 229920000049 Carbon (fiber) Polymers 0.000 description 1
- 241000218645 Cedrus Species 0.000 description 1
- 229920013683 Celanese Polymers 0.000 description 1
- 241000548268 Citrus deliciosa Species 0.000 description 1
- 229910000684 Cobalt-chrome Inorganic materials 0.000 description 1
- 239000004971 Cross linker Substances 0.000 description 1
- 229920004934 Dacron® Polymers 0.000 description 1
- JOYRKODLDBILNP-UHFFFAOYSA-N Ethyl urethane Chemical compound CCOC(N)=O JOYRKODLDBILNP-UHFFFAOYSA-N 0.000 description 1
- IAYPIBMASNFSPL-UHFFFAOYSA-N Ethylene oxide Chemical compound C1CO1 IAYPIBMASNFSPL-UHFFFAOYSA-N 0.000 description 1
- 229920000271 Kevlar® Polymers 0.000 description 1
- 241000124008 Mammalia Species 0.000 description 1
- 206010031264 Osteonecrosis Diseases 0.000 description 1
- 229920002367 Polyisobutene Polymers 0.000 description 1
- GOOHAUXETOMSMM-UHFFFAOYSA-N Propylene oxide Chemical compound CC1CO1 GOOHAUXETOMSMM-UHFFFAOYSA-N 0.000 description 1
- WYURNTSHIVDZCO-UHFFFAOYSA-N Tetrahydrofuran Chemical compound C1CCOC1 WYURNTSHIVDZCO-UHFFFAOYSA-N 0.000 description 1
- 229920004935 Trevira® Polymers 0.000 description 1
- GSEJCLTVZPLZKY-UHFFFAOYSA-N Triethanolamine Chemical compound OCCN(CCO)CCO GSEJCLTVZPLZKY-UHFFFAOYSA-N 0.000 description 1
- ZJCCRDAZUWHFQH-UHFFFAOYSA-N Trimethylolpropane Chemical compound CCC(CO)(CO)CO ZJCCRDAZUWHFQH-UHFFFAOYSA-N 0.000 description 1
- UKLDJPRMSDWDSL-UHFFFAOYSA-L [dibutyl(dodecanoyloxy)stannyl] dodecanoate Chemical compound CCCCCCCCCCCC(=O)O[Sn](CCCC)(CCCC)OC(=O)CCCCCCCCCCC UKLDJPRMSDWDSL-UHFFFAOYSA-L 0.000 description 1
- 238000010521 absorption reaction Methods 0.000 description 1
- 230000001133 acceleration Effects 0.000 description 1
- 210000000588 acetabulum Anatomy 0.000 description 1
- 150000001252 acrylic acid derivatives Chemical class 0.000 description 1
- 239000012790 adhesive layer Substances 0.000 description 1
- 239000002671 adjuvant Substances 0.000 description 1
- 150000001298 alcohols Chemical class 0.000 description 1
- 125000002947 alkylene group Chemical group 0.000 description 1
- 239000000956 alloy Substances 0.000 description 1
- 229910045601 alloy Inorganic materials 0.000 description 1
- 210000003484 anatomy Anatomy 0.000 description 1
- 210000003423 ankle Anatomy 0.000 description 1
- 239000004760 aramid Substances 0.000 description 1
- 229920006231 aramid fiber Polymers 0.000 description 1
- 210000001188 articular cartilage Anatomy 0.000 description 1
- 238000005452 bending Methods 0.000 description 1
- 239000004917 carbon fiber Substances 0.000 description 1
- 208000015100 cartilage disease Diseases 0.000 description 1
- 239000004359 castor oil Substances 0.000 description 1
- 235000019438 castor oil Nutrition 0.000 description 1
- 230000001413 cellular effect Effects 0.000 description 1
- 239000004568 cement Substances 0.000 description 1
- 230000008859 change Effects 0.000 description 1
- 201000005043 chondromalacia Diseases 0.000 description 1
- 239000011248 coating agent Substances 0.000 description 1
- 239000010952 cobalt-chrome Substances 0.000 description 1
- 150000001875 compounds Chemical class 0.000 description 1
- 238000007906 compression Methods 0.000 description 1
- 230000006835 compression Effects 0.000 description 1
- 238000009833 condensation Methods 0.000 description 1
- 230000005494 condensation Effects 0.000 description 1
- 239000007859 condensation product Substances 0.000 description 1
- 230000001276 controlling effect Effects 0.000 description 1
- 238000001816 cooling Methods 0.000 description 1
- 238000005520 cutting process Methods 0.000 description 1
- VEIOBOXBGYWJIT-UHFFFAOYSA-N cyclohexane;methanol Chemical compound OC.OC.C1CCCCC1 VEIOBOXBGYWJIT-UHFFFAOYSA-N 0.000 description 1
- 238000013461 design Methods 0.000 description 1
- 238000011161 development Methods 0.000 description 1
- 230000018109 developmental process Effects 0.000 description 1
- JQZRVMZHTADUSY-UHFFFAOYSA-L di(octanoyloxy)tin Chemical compound [Sn+2].CCCCCCCC([O-])=O.CCCCCCCC([O-])=O JQZRVMZHTADUSY-UHFFFAOYSA-L 0.000 description 1
- 238000003745 diagnosis Methods 0.000 description 1
- 239000012975 dibutyltin dilaurate Substances 0.000 description 1
- 238000006073 displacement reaction Methods 0.000 description 1
- 238000004090 dissolution Methods 0.000 description 1
- 238000001035 drying Methods 0.000 description 1
- 229920001971 elastomer Polymers 0.000 description 1
- 210000001513 elbow Anatomy 0.000 description 1
- 238000005530 etching Methods 0.000 description 1
- HGVSZIWPYBQNOR-UHFFFAOYSA-N ethane-1,2-diol;propane-1,3-diol Chemical compound OCCO.OCCCO HGVSZIWPYBQNOR-UHFFFAOYSA-N 0.000 description 1
- 150000002170 ethers Chemical class 0.000 description 1
- 239000011152 fibreglass Substances 0.000 description 1
- 210000000968 fibrocartilage Anatomy 0.000 description 1
- 239000000945 filler Substances 0.000 description 1
- 210000003811 finger Anatomy 0.000 description 1
- 238000007667 floating Methods 0.000 description 1
- 210000002683 foot Anatomy 0.000 description 1
- 239000000499 gel Substances 0.000 description 1
- 239000003365 glass fiber Substances 0.000 description 1
- ZEMPKEQAKRGZGQ-XOQCFJPHSA-N glycerol triricinoleate Natural products CCCCCC[C@@H](O)CC=CCCCCCCCC(=O)OC[C@@H](COC(=O)CCCCCCCC=CC[C@@H](O)CCCCCC)OC(=O)CCCCCCCC=CC[C@H](O)CCCCCC ZEMPKEQAKRGZGQ-XOQCFJPHSA-N 0.000 description 1
- 238000009499 grossing Methods 0.000 description 1
- 239000011440 grout Substances 0.000 description 1
- 239000003324 growth hormone secretagogue Substances 0.000 description 1
- 238000010348 incorporation Methods 0.000 description 1
- 230000006698 induction Effects 0.000 description 1
- 230000036512 infertility Effects 0.000 description 1
- 238000002347 injection Methods 0.000 description 1
- 239000007924 injection Substances 0.000 description 1
- 239000012784 inorganic fiber Substances 0.000 description 1
- 239000004761 kevlar Substances 0.000 description 1
- 210000000629 knee joint Anatomy 0.000 description 1
- 230000005499 meniscus Effects 0.000 description 1
- 239000007769 metal material Substances 0.000 description 1
- CRVGTESFCCXCTH-UHFFFAOYSA-N methyl diethanolamine Chemical compound OCCN(C)CCO CRVGTESFCCXCTH-UHFFFAOYSA-N 0.000 description 1
- 230000003278 mimic effect Effects 0.000 description 1
- 238000013008 moisture curing Methods 0.000 description 1
- 239000012778 molding material Substances 0.000 description 1
- 210000003205 muscle Anatomy 0.000 description 1
- SYSQUGFVNFXIIT-UHFFFAOYSA-N n-[4-(1,3-benzoxazol-2-yl)phenyl]-4-nitrobenzenesulfonamide Chemical class C1=CC([N+](=O)[O-])=CC=C1S(=O)(=O)NC1=CC=C(C=2OC3=CC=CC=C3N=2)C=C1 SYSQUGFVNFXIIT-UHFFFAOYSA-N 0.000 description 1
- 210000005036 nerve Anatomy 0.000 description 1
- 230000036961 partial effect Effects 0.000 description 1
- 210000004417 patella Anatomy 0.000 description 1
- 230000036314 physical performance Effects 0.000 description 1
- 230000004962 physiological condition Effects 0.000 description 1
- 239000004014 plasticizer Substances 0.000 description 1
- 229920000233 poly(alkylene oxides) Polymers 0.000 description 1
- 229920001610 polycaprolactone Polymers 0.000 description 1
- 239000004632 polycaprolactone Substances 0.000 description 1
- 229920000570 polyether Polymers 0.000 description 1
- 229920001195 polyisoprene Polymers 0.000 description 1
- 239000011148 porous material Substances 0.000 description 1
- 238000004080 punching Methods 0.000 description 1
- 239000000376 reactant Substances 0.000 description 1
- 229920013730 reactive polymer Polymers 0.000 description 1
- 238000002694 regional anesthesia Methods 0.000 description 1
- 230000002787 reinforcement Effects 0.000 description 1
- 239000012779 reinforcing material Substances 0.000 description 1
- 230000008439 repair process Effects 0.000 description 1
- 230000000452 restraining effect Effects 0.000 description 1
- 230000002441 reversible effect Effects 0.000 description 1
- 238000005096 rolling process Methods 0.000 description 1
- 238000005204 segregation Methods 0.000 description 1
- 210000002832 shoulder Anatomy 0.000 description 1
- 238000007711 solidification Methods 0.000 description 1
- 230000008023 solidification Effects 0.000 description 1
- 238000001228 spectrum Methods 0.000 description 1
- 230000006641 stabilisation Effects 0.000 description 1
- 238000011105 stabilization Methods 0.000 description 1
- 239000003381 stabilizer Substances 0.000 description 1
- 239000010935 stainless steel Substances 0.000 description 1
- 229910001220 stainless steel Inorganic materials 0.000 description 1
- 238000007655 standard test method Methods 0.000 description 1
- 210000005065 subchondral bone plate Anatomy 0.000 description 1
- 238000004381 surface treatment Methods 0.000 description 1
- 229910052715 tantalum Inorganic materials 0.000 description 1
- GUVRBAGPIYLISA-UHFFFAOYSA-N tantalum atom Chemical compound [Ta] GUVRBAGPIYLISA-UHFFFAOYSA-N 0.000 description 1
- 238000010998 test method Methods 0.000 description 1
- 230000003685 thermal hair damage Effects 0.000 description 1
- 229920001169 thermoplastic Polymers 0.000 description 1
- 239000004416 thermosoftening plastic Substances 0.000 description 1
- 210000002303 tibia Anatomy 0.000 description 1
- 239000012974 tin catalyst Substances 0.000 description 1
- 239000003106 tissue adhesive Substances 0.000 description 1
- 230000017423 tissue regeneration Effects 0.000 description 1
- 210000003371 toe Anatomy 0.000 description 1
- 229940086542 triethylamine Drugs 0.000 description 1
- 239000013638 trimer Substances 0.000 description 1
- 150000004072 triols Chemical class 0.000 description 1
- 229960004418 trolamine Drugs 0.000 description 1
- 210000000689 upper leg Anatomy 0.000 description 1
Images
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods
- A61B17/56—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor
- A61B17/562—Implants for placement in joint gaps without restricting joint motion, e.g. to reduce arthritic pain
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2/00—Filters implantable into blood vessels; Prostheses, i.e. artificial substitutes or replacements for parts of the body; Appliances for connecting them with the body; Devices providing patency to, or preventing collapsing of, tubular structures of the body, e.g. stents
- A61F2/02—Prostheses implantable into the body
- A61F2/30—Joints
- A61F2/30721—Accessories
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2/00—Filters implantable into blood vessels; Prostheses, i.e. artificial substitutes or replacements for parts of the body; Appliances for connecting them with the body; Devices providing patency to, or preventing collapsing of, tubular structures of the body, e.g. stents
- A61F2/02—Prostheses implantable into the body
- A61F2/30—Joints
- A61F2/32—Joints for the hip
- A61F2/34—Acetabular cups
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2/00—Filters implantable into blood vessels; Prostheses, i.e. artificial substitutes or replacements for parts of the body; Appliances for connecting them with the body; Devices providing patency to, or preventing collapsing of, tubular structures of the body, e.g. stents
- A61F2/02—Prostheses implantable into the body
- A61F2/30—Joints
- A61F2/38—Joints for elbows or knees
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2/00—Filters implantable into blood vessels; Prostheses, i.e. artificial substitutes or replacements for parts of the body; Appliances for connecting them with the body; Devices providing patency to, or preventing collapsing of, tubular structures of the body, e.g. stents
- A61F2/02—Prostheses implantable into the body
- A61F2/30—Joints
- A61F2/38—Joints for elbows or knees
- A61F2/3872—Meniscus for implantation between the natural bone surfaces
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2/00—Filters implantable into blood vessels; Prostheses, i.e. artificial substitutes or replacements for parts of the body; Appliances for connecting them with the body; Devices providing patency to, or preventing collapsing of, tubular structures of the body, e.g. stents
- A61F2/02—Prostheses implantable into the body
- A61F2/30—Joints
- A61F2/38—Joints for elbows or knees
- A61F2/3877—Patellae or trochleae
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2/00—Filters implantable into blood vessels; Prostheses, i.e. artificial substitutes or replacements for parts of the body; Appliances for connecting them with the body; Devices providing patency to, or preventing collapsing of, tubular structures of the body, e.g. stents
- A61F2/02—Prostheses implantable into the body
- A61F2/30—Joints
- A61F2/38—Joints for elbows or knees
- A61F2/389—Tibial components
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L27/00—Materials for grafts or prostheses or for coating grafts or prostheses
- A61L27/14—Macromolecular materials
- A61L27/18—Macromolecular materials obtained otherwise than by reactions only involving carbon-to-carbon unsaturated bonds
-
- C—CHEMISTRY; METALLURGY
- C08—ORGANIC MACROMOLECULAR COMPOUNDS; THEIR PREPARATION OR CHEMICAL WORKING-UP; COMPOSITIONS BASED THEREON
- C08G—MACROMOLECULAR COMPOUNDS OBTAINED OTHERWISE THAN BY REACTIONS ONLY INVOLVING UNSATURATED CARBON-TO-CARBON BONDS
- C08G18/00—Polymeric products of isocyanates or isothiocyanates
- C08G18/06—Polymeric products of isocyanates or isothiocyanates with compounds having active hydrogen
- C08G18/08—Processes
- C08G18/10—Prepolymer processes involving reaction of isocyanates or isothiocyanates with compounds having active hydrogen in a first reaction step
-
- C—CHEMISTRY; METALLURGY
- C08—ORGANIC MACROMOLECULAR COMPOUNDS; THEIR PREPARATION OR CHEMICAL WORKING-UP; COMPOSITIONS BASED THEREON
- C08G—MACROMOLECULAR COMPOUNDS OBTAINED OTHERWISE THAN BY REACTIONS ONLY INVOLVING UNSATURATED CARBON-TO-CARBON BONDS
- C08G18/00—Polymeric products of isocyanates or isothiocyanates
- C08G18/06—Polymeric products of isocyanates or isothiocyanates with compounds having active hydrogen
- C08G18/28—Polymeric products of isocyanates or isothiocyanates with compounds having active hydrogen characterised by the compounds used containing active hydrogen
- C08G18/40—High-molecular-weight compounds
- C08G18/48—Polyethers
- C08G18/4854—Polyethers containing oxyalkylene groups having four carbon atoms in the alkylene group
-
- C—CHEMISTRY; METALLURGY
- C08—ORGANIC MACROMOLECULAR COMPOUNDS; THEIR PREPARATION OR CHEMICAL WORKING-UP; COMPOSITIONS BASED THEREON
- C08G—MACROMOLECULAR COMPOUNDS OBTAINED OTHERWISE THAN BY REACTIONS ONLY INVOLVING UNSATURATED CARBON-TO-CARBON BONDS
- C08G18/00—Polymeric products of isocyanates or isothiocyanates
- C08G18/06—Polymeric products of isocyanates or isothiocyanates with compounds having active hydrogen
- C08G18/28—Polymeric products of isocyanates or isothiocyanates with compounds having active hydrogen characterised by the compounds used containing active hydrogen
- C08G18/40—High-molecular-weight compounds
- C08G18/61—Polysiloxanes
-
- C—CHEMISTRY; METALLURGY
- C08—ORGANIC MACROMOLECULAR COMPOUNDS; THEIR PREPARATION OR CHEMICAL WORKING-UP; COMPOSITIONS BASED THEREON
- C08G—MACROMOLECULAR COMPOUNDS OBTAINED OTHERWISE THAN BY REACTIONS ONLY INVOLVING UNSATURATED CARBON-TO-CARBON BONDS
- C08G18/00—Polymeric products of isocyanates or isothiocyanates
- C08G18/06—Polymeric products of isocyanates or isothiocyanates with compounds having active hydrogen
- C08G18/28—Polymeric products of isocyanates or isothiocyanates with compounds having active hydrogen characterised by the compounds used containing active hydrogen
- C08G18/67—Unsaturated compounds having active hydrogen
- C08G18/69—Polymers of conjugated dienes
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2/00—Filters implantable into blood vessels; Prostheses, i.e. artificial substitutes or replacements for parts of the body; Appliances for connecting them with the body; Devices providing patency to, or preventing collapsing of, tubular structures of the body, e.g. stents
- A61F2/02—Prostheses implantable into the body
- A61F2/30—Joints
- A61F2002/30001—Additional features of subject-matter classified in A61F2/28, A61F2/30 and subgroups thereof
- A61F2002/30316—The prosthesis having different structural features at different locations within the same prosthesis; Connections between prosthetic parts; Special structural features of bone or joint prostheses not otherwise provided for
- A61F2002/30535—Special structural features of bone or joint prostheses not otherwise provided for
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61F—FILTERS IMPLANTABLE INTO BLOOD VESSELS; PROSTHESES; DEVICES PROVIDING PATENCY TO, OR PREVENTING COLLAPSING OF, TUBULAR STRUCTURES OF THE BODY, e.g. STENTS; ORTHOPAEDIC, NURSING OR CONTRACEPTIVE DEVICES; FOMENTATION; TREATMENT OR PROTECTION OF EYES OR EARS; BANDAGES, DRESSINGS OR ABSORBENT PADS; FIRST-AID KITS
- A61F2250/00—Special features of prostheses classified in groups A61F2/00 - A61F2/26 or A61F2/82 or A61F9/00 or A61F11/00 or subgroups thereof
- A61F2250/0058—Additional features; Implant or prostheses properties not otherwise provided for
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L2430/00—Materials or treatment for tissue regeneration
- A61L2430/24—Materials or treatment for tissue regeneration for joint reconstruction
Definitions
- this disclosure relates to biomaterials formed ex vivo for implantation and use within the body.
- the disclosure relates to in situ curable biomaterials.
- this invention further relates to systems in the field of orthopedic implants and prostheses, and more particularly, for implantable materials for use in orthopedic joints.
- Certain of these applications describe, inter alia , the formation of a prosthetic nucleus within an intervertebral disc by a method that includes, for instance, the steps of inserting a collapsed mold apparatus (which in a preferred embodiment is described as a "balloon") through a cannula that is itself positioned through an opening within the annulus, and filling the balloon with a flowable biomaterial that is adapted to finally cure in situ and provide a permanent disc replacement.
- a collapsed mold apparatus which in a preferred embodiment is described as a "balloon”
- Applicant's PCT Application No. PCT/US97/00457 includes the optional use of a mold, such as a balloon, and describes the manner in which "[t]he mold created within the joint is preferably of sufficient shape and dimensions to allow the resulting cured biomaterial to replace or mimic the structure and function of the removed fibrocartilage.
- the mold can be formed of synthetic and/or natural materials, including those that are provided exogenously and those provided by the remaining natural tissues. The mold can either be removed from the site, upon curing of the biomaterial, or is sufficiently biocompatible to allow it to remain in position.”
- a mold may include or rely upon natural tissues (such as the annular shell of an intervertebral disc) for at least a portion of its structure, conformation or function.
- the mold is responsible, at least in part, for determining the position and final dimensions of the cured prosthetic implant.
- the mold material can itself become integral to the body of the cured biomaterial.”
- US Patent No. 6,206,927 describes a self-centering meniscal prosthesis device suitable for minimally invasive, surgical implantation into the cavity between a femoral condyle and the corresponding tibial plateau is composed of a hard, high modulus material shaped such that the contour of the device and the natural articulation of the knee exerts a restoring force on the free-floating device.
- Sulzer has introduced a unicompartmental interpositional spacer to treat osteoarthritis in the knee.
- the device is described as a metallic kidney-shaped insert which fills in for the damaged cartilage between the femur and the tibia.
- Such a metallic device as described in either the Fell patent and/or Sulzer's product literature, is described as appropriate for use in younger patients with moderate to severe chondromalacia, particularly since the product provides a hard, self-centering meniscal device that is "devoid of physical means that fix its location".
- the device of Fell et al. tends to require a significant amount of intact cartilage and meniscus.
- Applicant's own products to date, including those improved embodiments described herein have been largely geared toward more elderly patients, where such healthy cartilage is lacking.
- Applicant's devices tend to provide angular correction and improved anchoring of the implant at the joint surface.
- the present invention provides a system for the creation or modification of the wear surface of orthopedic joints in the spine .
- the method relies, at least in part, upon the manner in which the various stages of curing a curable biomaterial, and in turn, the various stages of forming a component from the cured or curing biomaterial, can be correlated and optimized in a desired manner.
- such a method provides the ability to both generally and specifically form the component for use in situ .
- the present invention includes a variety of embodiments, each of which preferably includes one or more components that are formed ex vivo , and that are adapted to be inserted and finally formed or assembled in situ in order to provide a final prosthesis and articulating joint surface.
- the various embodiments include, for instance,
- the present invention provides an optimal combination of benefits, as compared to methods previously described.
- benefits include those that arise in the course of preparation and storage (e.g., sterility, storage stability), those that arise in the surgical field itself (e.g., ease of use, adaptability, predictability), and those that arise in the course of long term use within the body (e.g., biocompatibility, moisture cure characteristics, tissue congruity and conformability, retention, wear characteristics, and physical-mechanical properties).
- the system involves the preparation and use of partially cured components that can be formed outside the body, for insertion and placement into the body, and that can then be further formed within the joint site in order to enhance conformance.
- partially cured components that can be formed outside the body, for insertion and placement into the body, and that can then be further formed within the joint site in order to enhance conformance.
- the ability to finally form one or more components in situ provides various additional benefits, such as increased control over the overall size and shape of the final prosthesis, improved shape and compliance of the surface apposing natural bone, and finally, improved shape and compliance of the opposite, articulating surface.
- the word "cure”, and inflections thereof, will refer to the extent to which a curable biomaterial, as used to form a component of this invention, has begun or completed whatever physical- chemical reactions may be contemplated in the course of fully forming the component, at the surgical site, for long term use in situ .
- the biomaterial can be considered as uncured (as in component parts that have not yet been mixed or compositions that have not yet been activated), or it can be partially cured (e.g., wherein the components have been mixed, or compositions activated, under conditions suitable to begin the curing process), or it can be fully cured (e. g., in which case, whatever chemical reactions may have occurred have substantially subsided).
- uncured compositions are sterile, storage stable, and often flowable, though are typically not yet formed or capable of being formed.
- Curing compositions generally begin as flowable compositions, but become nonflowable over a finite time period as they begin to gel or set. Curing compositions can also be minimally formed, e.g., outside the body by the use of molds and/or suitable shaping tools, and/or within the body, as by the initial positioning of the component on supporting bone and by the repositioning of opposing, articulating bone surfaces. Thereafter, it is contemplated that certain compositions of this invention can be further formed, over time, as by the gradual effect of articulating bone in the course of long term use.
- the word "form”, and inflections and variations thereof, will refer to the manner and extent to which a component has been sized and shaped, in either a general and/or specific manner, for use at a joint site.
- the forming of such a component can occur either ex vivo and/or in vivo, as well as in a general manner (e.g., by the use of an ex vivo mold or tools) and/or a specific manner (e.g., by final curing in apposition to supporting bone and/or opposing articulating bone surfaces), as well as combinations thereof.
- a component can be "specifically” formed in this manner in order to conform the component (and particularly its surfaces) to the corresponding specific shapes and dimensions of bone in situ , including both supporting bone surfaces and/or opposing (e.g., articulating) bone surfaces.
- Such specific conformation can be used to improve a variety of characteristics of the final implant, including comfort, mechanical performance, and/or long term stability.
- Such conformation can also include aspects in which one or more components, or the composite prosthesis, are "conformed” in correspondence with the joint site (e.g., by final shaping and curing processes that occur in situ ).
- Such conformation can also include aspects in which the components, or prosthesis itself, are adapted to be "deformed” within the site, as by the application of force.
- a substantially fully formed component can be provided to have sufficient mechanical properties (e.g., strength and resilience) to permit it to be inserted into a joint site and effectively deformed under normal anatomic forces
- a substantially convex component can be deformed to assume the corresponding concave shape in situ , in , while retaining sufficient resilient strength to tend towards its original convex shape (e.g., analogous to the manner in which a locking washer can be deformed in use, while tending toward its original shape).
- a final knee component is adapted to be deformed under conditions of use within the body (e.g., under physiologic load), while maintaining desired size and tibial congruency, and in a manner that provides desired fit and thickness for desired angular correction.
- a "preformed” component will generally refer to a component that is at least partially formed ex vivo , as by the surgeon's selection and use of an appropriately sized ex vivo mold.
- a preformed component can be specifically formed as well, including in an ex vivo fashion, as by the use of a customized mold that is itself reflective of the particular dimensions and contours of the intended joint site.
- Such customized molds can be prepared, for instance, by the use of external imaging means, and/or by the appropriate use of negative and/or positive molds taken at the tissue site.
- the preformed component is specifically formed, in whole or in part, by being positioned in situ , prior to the completion of the curing process, and in apposition to both supporting bone and opposing bone surfaces.
- any such component or prosthesis can be adapted to be deformed in order to improve its retention and/or performance in situ , e.g., resiliently deformed upon release of distracting forces and repositioning of the opposing bone surface.
- a preformed composition is provided, formed initially by the ex vivo onset of cure, in which the composition can be implanted within on the order of 10 seconds to several days of the onset of cure, preferably within about 30 seconds to about 10 minutes, and more preferably within about one to about five minutes, while maintaining a surface exotherm of less than about 50°C, and more preferably less than about 45°C once positioned within the body.
- preferred preformed components of this invention are adapted to be finally shaped, for a period of between about 10 seconds and one or more hours, and more preferably between about one minute and about five minutes.
- the lower limit is defined largely by the time it takes to effectively reposition bone, or otherwise re-establish suitable force on the implant.
- the upper limit is generally defined by the susceptibility of the implanted composition to further deformation or shaping. Such final shaping is generally accomplished, at least in part, under the force brought about.by repositioning articulating bone surfaces.
- the partially cured composition is implanted under conditions that permit it to deform less than about 15%, preferably less than about 10%, and most preferably less than about 5%, under physiologic forces, while maintaining tibial congruency and imparting desired angular correction.
- a particularly preferred preformed component of this invention can be implanted within an initial about one to about five minutes of the onset of its formation, and once implanted can be further molded or formed for a further period of about one to about five additional minutes, in a manner that permits the resultant implant to substantially retain a desired final form and function.
- the system of the present invention thereby provides the surgeon with a variety of options, based on the manner in which these curing and forming processes are correlated.
- the surgeon is provided with a composition adapted to be partially cured and generally formed ex vivo , and then promptly inserted into the body and positioned at the joint site, where it can be finally, and specifically, formed in the course of becoming fully cured.
- the present system simplifies the preparation process considerably, e.g., by lessening or avoiding potential problems (such as curing in the presence of moisture, and surface exotherm in the presence of tissue) that can arise when a comparable composition is mixed and delivered to the joint site while it is still flowable.
- potential problems such as curing in the presence of moisture, and surface exotherm in the presence of tissue
- the present system permits such prostheses to be not only formed, but also manipulated and inserted into the joint (e.g., through an incision of between about 1 cm and about 3 cm). Once inserted, the prosthesis can be positioned, and further formed in situ , all within a reasonable time frame. In fact, it has been found that the procedure is amenable to outpatient use and even regional anesthesia.
- a system of the disclosure can avoid the use of such processes as the drilling anchor holes into the underlying bone, distraction of the knee joint, ligament release, leveling of the tibial plateau, and the various other procedures typically involved with delivering the biomaterial directly to the joint site in still flowable form.
- the prosthesis of the present invention provides a combination of properties such as the extent of congruence with underlying bone, wear characteristics, fracture toughness, and avoidance of fibrillated articular cartilage, that meets or exceeds the combination of properties obtained using a comparable biomaterial in flowable form, delivered and largely cured in situ .
- a balloon can be filled with a biomaterial as described herein, and inserted and positioned within the acetabulum, prior to or following filling, to provide a soft, conformable, durable lining for the placement of a hip prosthetic portion.
- the system involves the preparation and use of one or more partially or fully cured component(s) formed outside the body, for insertion and placement into the body and optionally further fitting and securing at the joint site.
- preformed component(s) typically require less manipulation at the bedside and allow for alternative methods of terminal sterilization, and final inspection and release at the manufacturing site.
- the system e.g., preformed component(s) and/or curable biomaterial and mold
- a final prosthesis in vivo, that provides a first major surface in apposition to and retained upon the supporting bone itself, and a second (generally substantially parallel and opposite) major surface adapted to provide a wear surface for opposing (e.g., articulating) bone.
- the final prosthesis is maintained in a desired position upon the supporting bone surface in a manner suitable for its intended use, e.g., by the use of one or more anchor points, by the use of adhesive or other suitable interface materials, by the use of sutures, staples, and the like, and/or by a mechanical lock achieved by the combination of a bone-contacting surface suitably conformed or conformable to the terrain of supporting bone, together with the retaining (and optionally including deforming) effect achieved upon repositioning opposing articulating bone surface.
- the first and second major surfaces can be provided in any suitable manner, for instance, 1) by the preparation and insertion of a single partially cured and generally preformed component into the joint, preferably under conditions that permit the component to become further, and specifically, formed in vivo , 2) by adding a flowable biomaterial to an initial preformed component (e.g., in the shape of a balloon or open mold) positioned at the tissue site, 3) by placing one or more fully cured and preformed components at the tissue site and optionally further fitting, adapting and/or securing the component(s) as needed, and/or 4) by assembling one or more preformed components in situ (e. g., side by side in an interlocking fashion upon the surface) such that the assembled components cooperate to provide the first and second major surfaces.
- a flowable biomaterial e.g., in the shape of a balloon or open mold
- the method and system of this invention include the optional use of various additional materials and/or steps, e.g., to prepare the bone surface itself, to provide suitable interfaces (e.g., adhesive interfaces and/or protrusions that can be further secured to the joint site or by smoothing of the femoral condyle or tibial plateau as needed), to treat one or more surfaces in order to provide them with different or improved properties as compared to the inherent properties of the material providing the surface, and the like.
- suitable interfaces e.g., adhesive interfaces and/or protrusions that can be further secured to the joint site or by smoothing of the femoral condyle or tibial plateau as needed
- suitable interfaces e.g., adhesive interfaces and/or protrusions that can be further secured to the joint site or by smoothing of the femoral condyle or tibial plateau as needed
- suitable interfaces e.g., adhesive interfaces and/or protrusions that can be further secured to the joint site
- the partially or fully cured preformed component(s) can themselves each provide uniform or non-uniform properties, and can be provided in a plurality or range of styles and sizes. These components can be designed to conform to lateral or medial compartments, or both, and to right or left knees, or both. In a preferred embodiment, all embodiments can be inserted into the joint site in a minimally invasive fashion.
- minimally invasive in this context, it is meant that the procedure of sizing, inserting, positioning and forming the prosthesis, in situ, can preferably be accomplished without the need for open, invasive incisions of the type conventionally used for inserting total knee prostheses.
- the partially cured preformed components can be further formed and fully cured in vivo to enhance compliance with the joint site.
- the surface of the partially or fully cured preformed component(s) can also be modified to provide any desired properties (e.g., promote adhesion), such as by the design and use of polymers themselves or by surface treatment of the fully cured or curing embodiments to provide suitable reactive groups such as amines, hydroxyl groups, or other reactive or hydrogen bonding functionalities.
- the partially cured preformed component or fully cured component, including balloons or composite materials can be provided with appropriate surface coatings, e.g., biologically active agents to promote desired tissue interactions, including tissue or cellular adhesion, such as those selected from the group consisting of cytokines, hydroxyapatite, collagen, and combinations thereof.
- partially cured, and generally preformed components are inserted into the joint site, and there further and specifically formed to enhance compliance.
- fully cured components in the shape of a balloon or open mold are employed to provide a final composite material by inserting the balloon or mold into the joint and there filling it with a biomaterial that cures in situ and conforms with the joint site.
- the fully cured component(s) are provided and inserted into the joint either singly or piecemeal and optionally further fitted and secured in vivo .
- the invention provides an open ex vivo mold, adapted to approximate the desired dimensions of the joint site, and to receive a curable biomaterial.
- a suitable mold can be formed, for instance, from the use of conventional materials such as silicone materials, that permit the curing biomaterial component to be easily and entirely removed at the desired time.
- the mold can itself be provided with a coating or release liner, including those that can be integrated, in whole or in part, with the component thus formed.
- the biomaterial can be removed from the mold and inserted into the joint site, under conditions suitable to permit it to be further and finally formed in vivo to enhance conformance with the joint site.
- additional ex vivo forming steps or features can be performed, e.g., by imparting desired curvature and femoral glide paths, prior to inserting and final forming in vivo .
- various structures and/or materials can be incorporated into and/or onto the component itself, to enhance its placement, retention and/or performance in situ .
- the mold itself can be provided in a form sufficient to impart various integral structural features, such as tibial "tabs", adapted to provide or improve the retention of the component at the tissue site.
- tabs can be provided in the form of one or more protrusions integral with the mold itself and adapted to be positioned within and/or affixed to the soft tissue and/or bone in vivo . Examples of such tabs are shown, for instance, in Figure 1 , where reference number 18 depicts a raised posterior portion.
- An insertable component can also be provided with one or more ancillary portions or protrusions formed of materials other than that used to form the bulk of the component itself.
- sutures or fibrous materials can be incorporated into or onto the bulk material, for use in improving the initial and/or long term retention of the component in situ , e.g, by tethering the prosthesis at the joint site and in a desired position.
- Such other materials can be temporarily positioned into or upon the mold itself, for instance, or otherwise provided, in a manner that permits them to become integrated into the biomaterial as it fills the mold and becomes partially cured ex vivo .
- the protrusions can be used to tether the implant, by securing them to the surrounding soft tissue and/or bone by use of adhesives, sutures, screws, pins, staples or the like or combinations thereof.
- the materials can provide both an immediate fixation function, and optionally also a desired long term function, by permitting them to be either absorbed by the body over time, and/or to permit or encourage fibrous tissue ingrowth for long term fixation.
- the reinforcing material can be provided in any suitable form, e.g., as fibers (e.g., sutures) or as a uniform woven or non-woven fabric, optionally including one or more reinforcing fibers or layers.
- a suitable non-woven fabric for instance, is preferably a material such as is commercially available under the trade name Trevira Spunbond from Hoechst Celanese Corporation.
- the non-woven fabric is generally composed of continuous thermoplastic fiber, needle punched together to yield a felt-like fabric.
- other materials such as polyester staple mat, glass fiber mat, as well as other organic and inorganic fiber mats and fabrics can be employed.
- Reinforcing fibers can be included within the woven or non-woven fabric, or provided as separate layers of a composite.
- Such fiber layers can preferably include a directional reinforcing fiber layer of organic or inorganic structural reinforcing fibers such as fiberglass, carbon fibers, aramid fibers which is available from DuPont Corporation under the trade name Kevlar, linear polyethylene or polypropylene fibers such as is commercially available from Allied-Signal, Inc. (now Honeywell) under the trade name Spectra, or polyester fibers.
- the phrase "reinforcing fiber” can include any fiber which, when used in its own right or added to a composite fabric material, retains or enhances desired structural properties.
- the fibers can be randomly oriented, or preferentially, they can be oriented in one or more directions. While a number of specific types of materials have been given for use as the reinforcing fiber layer, it will be appreciated by those of ordinary skill in the art that other equivalent-type reinforcing fiber layers can be employed in the practice of the invention.
- a reinforcing fiber layer can be itself used to secure the prosthesis, or can be attached to a woven or non-woven fiber layer having a number of interstices or pores.
- the reinforcing fiber layer and other fiber layers are secured to each other mechanically, as by conventional stitching, needle punching, stapling or buttons. In the case of certain applications, adhesives can also be used.
- a partially cured preformed component (and/or ancillary portions incorporated therein) can also be provided with suitable means to improve its ability to retain the component in situ , e.g., by the use of surface characteristics that provide improved chemical interactions with the joint site. Such interactions can be achieved by the judicious use of bulk material compositions themselves and/or the use of adhesives or other suitable interface materials.
- the partially cured, preformed, component can also be physically modified to increase its interactions with joint site, as by surface roughening, etching or cross-hatching, which would tend to provide increased surface area, and in turn, improved mechanical retention.
- a partially cured, preformed, component can also be retained by external means that are otherwise secured to the surrounding bone and/or soft tissue by use of adhesives, sutures, screws, pins, staples or the like or combinations thereof.
- the partially cured preformed component can be provided with suitable means as well, intended to improve or alter either its compliance and/or interactions with the opposing bone surface.
- the system includes a partially cured preformed component that is first molded outside of the joint site and adapted to be delivered to a tissue site and there positioned in a fixed position.
- the mold can be of an open or closed configuration (and/or can involve a one- or multi-step molding process), adapted to preform one or both major surfaces, respectively.
- the partially cured component is adapted to be initially fit and positioned within the joint site, and to thereafter become better conformed to the specific dimensions and/or terrain (e.g., anatomic structure) of the joint site in vivo .
- the molds are designed to yield components that have optimum adhesion and conformance to the joint sites.
- the molds may also be heated during the ex vivo partial curing process to optimize component properties or to provide a component that is more formable in vivo .
- the system involves the preparation and use of one or more fully or partially cured component(s) formed outside the body, for insertion and placement into the body and optionally further fitting and securing at the joint site.
- the invention provides a single preformed component that is inserted into the joint site and optionally further fitted or secured as needed.
- the invention provides a plurality of preformed components, formed of the same or different materials, and adapted to be delivered and positioned at the tissue site in a manner that provides a final composite.
- the components can be combined at the site in any suitable fashion, e.g., by providing a mechanical lock and/or by the use of interfacial materials such as adhesive layers.
- the components can be combined in any suitable fashion, e.g., as layers upon the bone, or as individual side-by-side components adapted to traverse the bone surface when combined.
- the use of preformed component(s) can require less manipulation at the bedside and allow for alternative methods of terminal sterilization, and final inspection and release at the manufacturing site.
- the various means of retaining partially cured preformed components, discussed herein, can be adapted to work with fully cured preformed components.
- the system of this invention can be used for repairing a variety of mammalian joints, including human joints of the spine.
- preformed component(s) that contact the bone surface are preferably adapted to physically conform closely to the prepared bone surface, e.g., to its macroscopic physical contours.
- Such conformation can be provided or enhanced in any suitable manner, e.g., 1) by providing a partially cured preformed component that is first made in an ex vivo mold and then adapted or modified to conform to the surface (e.g., by further forming in vivo ), and/or 2) by use of a preformed balloon or composite mold material that is inserted into the joint site and filled with a flowable biomaterial that cures in vivo so that it conforms with the joint site and/or 3) by the use of fully cured preformed component(s) that has optimum geometry for biomaterial compliance once placed in the joint site and/or 4) by the preparation and use of a suitable (e.g., thin) interface material between bone and preformed component (e.g., adhesive, filler, or cement material), and/or 5) by the use of physical res
- Figure 1 shows a top and side perspective of a preferred preformed knee implant (10) prepared using an ex vivo mold according to the present disclosure.
- the implant provides a first major surface (12) adapted to be positioned upon the tibial surface, and a generally planar second major surface (14) adapted to be positioned against the femoral condyle.
- the second major surface in turn, is preferably provided with a femoral glide path (16) to facilitate its performance in situ , in the form of a generally central oval depression about 1 mm to about 5mm deep at its lowest point (2 mm as shown) and about 30 mm to about 50 mm in length by 10 mm to 30 mm in width (40 mm by 20 mm as shown).
- the implant is also provided with a raised tibial projection (18), adapted to catch the posterior portion of the tibial plateau.
- the implant can have dimensions on the order of between about 40 to about 60 mm in the anterior-posterior dimension, between about 30 mm to about 40 mm in the medial-lateral dimension, and a maximum thickness (at the posterior lip of between about 10 mm and about 20 mm.
- Figure 2 shows an embodiments in which a plurality of preformed components are adapted to be inserted and assembled in situ to provide the final implant (20)
- Figure 2a shows an embodiment, in which preformed components (22 through 25, respectively) are assembled in a side-by-side manner sequentially, and in situ , and upon the tibial surface.
- the matable preformed sections each provide at least a portion of the resultant bone-contacting surface and wear surface, as well as one or more portions adapted to provide a mechanical lock with one or more respective other portions.
- the mechanical lock can be achieved in any suitable manner, as by the provision of corresponding male and female portions, respectively.
- the portions can be mated, in situ, e.g., in a press fit or sliding manner, in order to attach the respective components.
- the combined components cooperate to provide both a tibial bone-contacting surface (28) and a wear surface (26).
- a final implant is provided using interlocking preformed components (show in this case as portions 31 through 33, respectively) are instead provided in a form that permits them to be stacked upon each other, e.g., by layering or sliding them onto each other, and positioned upon the surface, in situ .
- the portions can be assembled in any suitable fashion, e.g., entirely on the tissue site, entirely ex vivo, or in varying combinations as desired.
- the generally planar portions are provided with corresponding matable portions, e.g., in the form of grooves and tabs to provide a sliding fit, or a depression and corresponding projection to provide either a press fit, snap fit, or other suitable fit sufficient to prevent lateral displacement to the extent desired.
- the resultant formed prosthetic implant can be provided with various features as described herein, including desired molded portions adapted to provide better fit or performance.
- Top portion (31) is particularly well suited to provide a desirable wear surface, while one or more intermediate portions (as shown by element 32) are adapted to provide an optimal combination of such properties as thickness, cushioning, and angular correction.
- FIG. 3 As shown the lowermost portion (33) is shown with a projection (34) adapted to be retained within a corresponding anchor hole or suitable depression formed into the bone itself.
- Figures 3b and 3c provide generally bottom and top views, respectively, showing the manner in which the portions can be combined in a layered fashion.
- preformed layers are shown having protrusions adapted to be positioned in a corresponding indentation within each underlying layer (or bone), in order to form a compact stack.
- the corresponding system will typically include at least two preformed components, including the initial, bone-contacting component, and final component providing the wear surface.
- the system can provide one or more intermediate layers, e.g., the number and/or selection of which can be used to provide a final desired height to the overall composite, and/or to provide differing properties (e.g., with respect to compressibility, resilience, tissue ingrowth), and/or to provide improved retention between the first and final components.
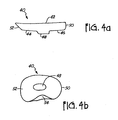
- Figure 4a shows an embodiment in which a substantially open (saucer-shaped) mold (40) is inserted into the joint site, to be filled with a corresponding curable biomateral in situ.
- the top (42) of the mold is open to receive biomaterial (not show), while the bottom (44) provides a lower major surface (46) adapted to contact bone and terminates in a filled protrusion (48) adapted to be positioned within a corresponding anchor point drilled in the bone itself.
- the anterior edge (50) of the cup is substantially perpendicular to the plane of the cup itself, while the posterior edge (52) is tapered (and optionally raised) to accommodate the corresponding shape of the tibial spine.
- the ex vivo mold accommodates a predetermined volume of biomaterial of on the order of about 5 ml to about 15 ml.
- the amount of biomaterial actually can be predetermined and controlled to correspond with the ex vivo mold volume.
- the ex vivo molds are designed for optimum sizing and conformance to the joint site and MRI software may be used to chose best mold for joint site. Implant thickness and hence angular correction can be controlled in this way.
- Figure 4b shows a bottom perspective view of the mold apparatus of Figure 4a , showing the filled protrusion (48).
- the posterior edge portion can be seen as provided with a groove or indentation (54), again to accommodate the typical shape of the corresponding tibial spine.
- the mold can be seen as assuming a generally kidney-shaped configuration, adapted to correspond with the tibial surface.
- Such a mold can be provided in a plurality of sizes, and shapes, to be selected at the time of use to accommodate the particular patient's needs and surgeon's desires.
- Figures 5a and 5b show the mold of Figure 4a being positioned upon a tibial surface ( Fig. 5a ), with the protrusion positioned within a corresponding anchor point, and (in Fig. 5b ) with the tip of a biomaterial delivery cannula (56) positioned upon it, and with flowable biomaterial (58) being shown in the course of delivery.
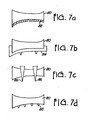
- Figure 6 shows a variety of alternative embodiments that include one or more preformed component.
- Fig. 6a shows a simple wedge shaped embodiment (60), in which the posterior portion (62) is significantly increased in size as compared to the anterior (64).
- Fig. 6b shows an implant (66) molded to provide portions (here, layers) having differing wear characteristics, including a preformed top having improved wear as compared to the separately formed bottom portion (70).
- Fig. 6c shows a plurality of components (72) adapted to be positioned and assembled in situ at the time of surgery.
- Figure 6d shows a single piece (80) as might be cut from preformed material at the time of surgery
- Figure 7 shows a variety of alternative means for anchoring a preformed component such as that shown in Fig. 6d .
- a grout (82) or other suitable interface material as shown in Fig. 7a
- a separate external retaining device (84) as shown in Fig. 7b
- the use of externally provided pins, screws, sutures, etc. as exemplified by elements (86) which generally traverse the body itself as in Fig. 7c
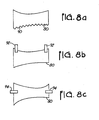
- Figure 8 shows a further variety for anchoring or stabilizing a preformed portion by the use of ancillary portions and/or surface texture, including a roughened surface (90) as in Fig. 8a ; or tabs (e.g., provided by fabric or suture like materials) as shown as elements 92 and 94 of Figs. 8b and 8c , respectively.
- ancillary portions and/or surface texture including a roughened surface (90) as in Fig. 8a ; or tabs (e.g., provided by fabric or suture like materials) as shown as elements 92 and 94 of Figs. 8b and 8c , respectively.
- the preformed components can benefit from any suitable combination of the various features and embodiments described or shown herein.
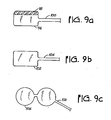
- Figure 9 shows a variety of embodiments in a substantially closed (balloon like) mold is adapted to be inserted into the joint site and filled with a corresponding curable biomaterial, the mold itself providing a preformed articulating wear surface, including Fig. 9a which shows an inflatable balloon portion (96) that includes an integral preformed wear surface and portion (98), as well as a lumen (100) adapted to fill the inflatable portion with flowable biomaterial.
- Fig. 9b shows a corresponding balloon (102) tough without a preformed portion, and including its biomaterial lumen (104).
- the balloon of this or any embodiment can include various interior and/or exterior surface coatings, and can have regions and/or layers having different desired physical-chemical properties (such as porosity).
- Fig. 9c shows a bi-compartmental closed balloon-like mold (106), wherein each compartment is adapted to conform to a respective medial or lateral tibial surface.
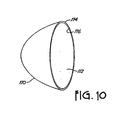
- Figure 10 shows a mold adapted for use as an acetabular mold (110) in connection with the replacement of the articulating surface in a hip, when filled with biomaterial, the mold forming a concave portion adapted to retain a corresponding femoral head.
- the mold is shown providing a thin generally cup-shaped mold adapted to be filled in any suitable form (e.g., using a removable conduit (not shown) attached to the space between inner and outer sealed layers (116 and 114, respectively) forming the mold.
- Figure 11 shows a patella-femoral joint form suitable for use in combination with the method and system of this invention.
- the form includes a silicone or other suitable pad material (122) having aluminum or other suitable stay portions (124) and terminal handle or grasping portions (126).
- the piece is formed to the femoral bone surface, with its form maintained by bending the aluminum stays.
- anchor points cut into the femoral bone if desired, the form is held tight against the bone with the upper handle held away from bone to permit the delivery of curable biopolymer between the form and the bone.
- the present application describes a method and system for the creation or modification of the wear surface using an implanted material fixed to the support structure of the original wear surface, to generally conform to the shape of the original surface in a mammal.
- a method or system where the end of the bony surface is a rotating, sliding or rolling surface, such as in the knee, finger, hip, toe, spine, wrist, elbow, shoulder, ankle, or TMJ joint The implant will function:
- the method and system of this invention can be applied to areas of aseptic necrosis, such as the nevecular bone in the wrist.
- the material to be implanted consists of a plurality of materials, such as polymers, including polyurethane, polyethyelenes, polyureas, polyacrylates, polyurethane acrylates, hydrogels, epoxies and/or hybrids of any of the above.
- the surface can be provided by any of a series of metals, including titanium, stainless steel, cobalt chrome millithium alloys and tantalum.
- Other surface materials can include various ceramics and biologic polymers.
- the implantable material for the resurfacing can be formed ex vivo and/or in vivo as an injectable material that sets up to the molded shape.
- the methods for changing state from liquid to solid state include cooling or heating, the passage of time, which allows for a change of state, or a chemical reaction between different reactants.
- the reaction can be exothermic or endothermic.
- the set-up can be light activated or chemically catalyzed or it could be heat activated. Examples of such systems include flowable polymers of two or more components, light activated polymers, and polymers cured either by catalysts or by heat, including body heat.
- Molds can be used in the form of balloons, dams or retainers. They can be used in combination with the local anatomy to produce the desired shape and geometry. Molds can be of materials that are retained and becomes part of the implant or could be removed after curing of the biomaterial component.
- the material would be semi-solid and could be shaped and then set up in vivo. This would allow for the minimally invasive application, either through an arthroscopic portal or through a small mini arthrotomy.
- the material could be synthesized ex vivo and then machined to fit using imaging to pre-determine the desired geometry and size of the implant.
- a range of implant sizes could be provided and sizing could be accomplished during the procedure.
- An ex vivo mold could be fit using molding materials and the implant could be molded on site just prior to implantation.
- Fixation methods for the implant would include biologic glues to glue the implant to the underlying surface, trapping of the implant into a cavity on the surface that causes a mechanical lock, using various anchors to the underlying structure and fixing the implant to that surface or using mold retainers and/or screws, staples, sutures or pins.
- anchors in the underlying structure may be used for fixing the implant to that surface and we may also use a tissue ingrowth system to secure anchoring.
- the patient will have a diagnosis of osteoarthritis and have loss of cartilage on the articulating surface.
- a determination will be made of the amount of correction needed for the reestablishment of a normal angle of articulation.
- the ligaments will be balanced so that there is no loss of range of motion with the implant in place and the surface will be placed in such a position that the eventual resulting surface geometry reestablishes the same plane and orientation of the original articular surface.
- Access to the site is obtained in a minimally invasive way. In a preferred embodiment, this is accomplished through arthroscopic means with arthroscopic portals. In an alternative embodiment, the access is accomplished by a mini arthrotomy with a small incision that allows access to the joint without sacrificing nerves, vessels, muscles or ligaments surrounding the joint. In the preferred embodiment fibrillated articulating cartilage that is degenerated is removed down to the subchondral surface.
- the surface is dried and prepared for appropriate anchoring. This may include anchor points that give a mechanical lock or that alternatively simply supply horizontal and lateral stability. The surface may be prepared by drying and roughening in case a tissue adhesive is used. Pre-made anchors may be installed.
- the final geometry of the implant may be determined by a dam or mold that is placed on the joint at the time the material is implanted, when the implant is installed using an in situ cured technique (in the manner shown in Figures 1 and 4 of Applicant's provisional parent application).
- a mold For pre-made material formed at the surgical site within a mold, various forms of stabilization could be used, including anchor points or titanium screws. Alternatively, the pre-made material could be made off site to the specs developed from imaging of the patient's joint surface. In a third embodiment, multiple sizes could be made off site and the selection of the appropriate implant size could be chosen at the time of surgery.
- Two alternatives shown in Figure 2 of the parent provisional application include a single segment that can be installed through a portal or a series of segments that can be installed through a portal and locked together once inside the joint. They would be placed sequentially and then anchored to the bone by anchor points cut in the bone or by screws or tissue ingrowth. Finally, a robot, a jag or other cutting fixture could be used to prepare the bony surface for the pre-made implant to a fixed geometry of the anchor point.
- Both the preformed component(s) and flowable biomaterial, if used, can be prepared from any suitable material.
- the materials include polymeric materials, having an optimal combination of such properties as biocompatibility, physical strength and durability, and compatibility with other components (and/or biomaterials) used in the assembly of a final composite.
- suitable materials for use in preparing the preformed component(s) may be the same or different from the in situ curing biomaterial, and include polyurethanes, polyethylenes, polypropylenes, Dacrons, polyureas, hydrogels, metals, ceramics, epoxies, polysiloxanes, polyacrylates, as well as biopolymers, such as collagen or collagen-based materials or the like and combinations thereof.
- suitable materials for use in preparing the flowable biomaterial include polyurethanes, polyureas, hydrogels, epoxies, polysiloxanes, polyacrylates, and combinations thereof.
- the same or different polyurethane formulations can be used to form both the preformed component(s), e.g., by an injection molding technique, as well as for the flowable biomaterial, if present.
- Suitable polyurethanes for use as either the preformed component or biomaterial can be prepared by combining: (1) a quasi-prepolymer component comprising the reaction product of one or more polyols, and one or more diisocyanates, and optionally, one or more hydrophobic additives, and (2) a curative component comprising one or more polyols, one or more chain extenders, one or more catalysts, and optionally, other ingredients such as an antioxidant, and hydrophobic additive.
- the present invention preferably provides a biomaterial in the form of a curable polyurethane composition
- a curable polyurethane composition comprising a plurality of parts capable of being mixed at the time of use in order to provide a flowable composition and initiate cure, the parts including: (1) a quasi-prepolymer component comprising the reaction product of one or more polyols, and one or more diisocyanates, optionally, one or more hydrophobic additives, and (2) a curative component comprising one or more polyols, one or more chain extenders, one or more catalysts, and optionally, other ingredients such as an antioxidant, hydrophobic additive and dye.
- the composition is sufficiently flowable to permit it to be delivered to the body, and there be fully cured under physiological conditions.
- the component parts are themselves flowable, or can be rendered flowable, in order to facilitate their mixing and use.
- the flowable biomaterial used in this invention preferably includes polyurethane prepolymer components that react either ex vivo or in situ to form solid polyurethane ("PU").
- the formed PU includes both hard and soft segments.
- the hard segments are typically comprised of stiffer oligourethane units formed from diisocyanate and chain extender, while the soft segments are typically comprised of one or more flexible polyol units. These two types of segments will generally phase separate to form hard and soft segment domains, since they tend to be incompatible with one another.
- the hard segments of the polymer can be formed by a reaction between the diisocyanate or multifunctional isocyanate and chain extender.
- suitable isocyanates for preparation of the hard segment of this invention include aromatic diisocyanates and their polymeric form or mixtures of isomers or combinations thereof, such as toluene diisocyanates, naphthalene diisocyanates, phenylene diisocyanates, xylylene diisocyanates, and diphenylmethane diisocyanates, and other aromatic polyisocyanates known in the art.
- suitable polyisocyanates for preparation of the hard segment of this invention include aliphatic and cycloaliphatic isocyanates and their polymers or mixtures or combinations thereof, such as cyclohexane diisocyanates, cyclohexyl-bis methylene diisocyanates, isophorone diisocyanates and hexamethylene diisocyanates and other aliphatic polyisocyanates. Combinations of aromatic and aliphatic or arylakyl diisocyanates can also be used.
- the isocyanate component can be provided in any suitable form, examples of which include 2,4'-diphenylmethane diisocyanate, 4,4'-diphenylmethane diisocyanate, and mixtures or combinations of these isomers, optionally together with small quantities of 2,2'-diphenylmethane diisocyanate (typical of commercially available diphenylmethane diisocyanates).
- Other examples include aromatic polyisocyanates and their mixtures or combinations, such as are derived from phosgenation of the condensation product of aniline and formaldehyde.
- an isocyanate that has low volatility such as diphenylmethane diisocyanate, rather than more volatile materials such as toluene diisocyanate.
- An example of a particularly suitable isocyanate component is the 4,4'-diphenylmethane diisocyanate ("MDI").
- MDI 4,4'-diphenylmethane diisocyanate
- it can be provided in liquid form as a combination of 2,2'-, 2,4'- and 4,4'- isomers of MDI.
- the isocyanate is MDI and even more preferably 4,4'-diphenylmethane diisocyanate.
- chain extenders for preparation of the hard segment of this invention include, but are not limited, to short chain diols or triols and their mixtures or combinations thereof, such as 1,4-butane diol, 2-methyl-1,3-propane diol, 1,3-propane-diol ethylene glycol, diethylene glycol, glycerol, cyclohexane dimethanol, triethanol amine, and methyldiethanol amine.
- chain extenders for preparation of the hard segment of this invention include, but are not limited to, short chain diamines and their mixtures or combinations thereof, such as dianiline, toluene diamine, cyclohexyl diamine, and other short chain diamines known in the art.
- the soft segment consists of urethane terminated polyol moieties, which are formed by a reaction between the polyisocyanate or diisocyanate or polymeric diisocyanate and polyol.
- suitable diisocyanates are denoted above.
- polyols for preparation of the soft segment of this invention include but are not limited to polyalkylene oxide ethers derived form the condensation of alkylene oxides (e.g. ethylene oxide, propylene oxide, and blends thereof), as well as tetrahyrofuran based polytetramethylene ether glycols, polycaprolactone diols, polycarbonate diols and polyester diols and combinations thereof.
- the polyols are polytetrahydrofuran polyols ("PTHF”), also known as polytetramethylene oxide (“PTMO”) or polytetramethylene ether glycols (“PTMEG”).
- PTHF polytetrahydrofuran polyols
- PTMO polytetramethylene oxide
- PTMEG polytetramethylene ether glycols
- Two or more PTMO diols of different molecular weight can be used as a blend or separately, and in an independent fashion as between the different parts of the two part system.
- the solidification temperature(s) of PTMO diols is generally proportional to their molecular weights.
- the compatibility of the PTMO diols with such chain extenders as 1,4-butanediol is generally in the reverse proportion to molecular weight of the diol(s). Therefore the incorporation of the low molecular weight PTMO diols in the "curative" (part B) component, and higher molecular weight PTMO diols in the prepolymer (part A) component, can provide a two-part system that can be used at relatively low temperature.
- the PU can be chemically crosslinked, e.g., by the addition of multifunctional or branched OH-terminated crosslinking agents or chain extenders, or multifunctional isocyanates.
- suitable crosslinking agents include, but are not limited to, trimethylol propane (“TMP"), glycerol, hydroxyl terminated polybutadienes, hydroxyl terminated polybutadienes (HOPB), trimer alcohols, Castor oil polyethyleneoxide (PEO), polypropyleneoxide (PPO) and PEO-PPO triols.
- TMP trimethylol propane
- glycerol glycerol
- HOPB hydroxyl terminated polybutadienes
- trimer alcohols trimer alcohols
- PETO polyethyleneoxide
- PPO polypropyleneoxide
- PEO-PPO triols PEO-PPO triols.
- HOPB is used as the crosslinking agent.
- This chemical crosslinking augments the physical or "virtual" crosslinking of the polymer by hard segment domains that are in the glassy state at the temperature of the application.
- the optimal level of chemical cross-linking improves the compression set of the material, reduces the amount of the extractable components, and improves the biodurability of the PU.
- This can be particularly useful in relatively soft polyurethanes, such as those suitable for the repair of damaged cartilage. Reinforcement by virtual cross-links alone may not generate sufficient strength for in vivo performance in certain applications. Additional cross-linking from the soft segment, potentially generated by the use of higher functional polyols can be used to provide stiffer and less elastomeric materials. In this manner a balancing of hard and soft segments, and their relative contributions to overall properties can be achieved.
- a polymer system of the present invention preferably contains at least one or more, biocompatible catalysts that can assist in controlling the curing process, including the following periods: (1) the induction period, and (2) the curing period of the biomaterial. Together these two periods, including their absolute and relative lengths, and the rate of acceleration or cure within each period, determines the cure kinetics or profile for the composition.
- Suitable catalysts for preparation of the formed PU of this invention include, but are not limited to, tin and tertiary amine compounds or combinations thereof such as dibutyl tin dilaurate, and tin or mixed tin catalysts including those available under the tradenames "Cotin 222", “Formrez UL-22” (Witco), "dabco” (a triethylene diamine from Sigma-Aldrich), stannous octanoate, trimethyl amine, and triethyl amine.
- the catalyst is Formrez UL-22 (Witco).
- the catalyst is a combination Cotin 222 (CasChem) and dabco (Sigma-Aldrich).
- the in vivo and ex vivo cured polyurethanes of this invention can be formed by the reaction of two parts.
- Part I of which (alternatively referred to as Part A) includes a di- or multifunctional isocyanate or quasi-prepolymer which is the reaction product of one or more OH-terminated components, and one or more isocyanates.
- Part II of the polyurethane (alternatively referred to as Part B herein) is a curative component that includes of one or more chain extenders and one or more polyols, and one or more catalysts, and other additives such as antioxidants and dyes.
- the stoichiometry between Parts I (quasi-prepolymer) and II (curative component), expressed in terms of NCO:OH molar ratio of the isocyanate terminated pre-polymer (Part I) and the curative component (Part II) is preferably within the range of about 0.8 to 1.0 to 1.2 to 1.0, and more preferably from about 0.9 to 1 to about 1.1 to 1.0.
- a reactive polymer additive can be included and is selected from the group consisting of hydroxyl- or amine-terminated compounds selected from the group consisting of poybutadiene, polyisoprene, polyisobutylene, silicones, polyethylene-propylenediene, copolymers of butadiene with acryolnitrile, copolymers of butadiene with styrene, copolymers of isoprene with acrylonitrile, copolymers of isoprene with styrene, and mixtures of the above.
- Suitable compositions for use in the present invention are those polymeric materials that provide an optimal combination of properties relating to their manufacture, application, and in vivo use.
- properties include component miscibility or compatibility, processability, and the ability to be adequately sterilized or aseptically processed and stored.
- suitable materials exhibit an optimal combination of such properties as flowability, moldability, and in vivo curability.
- suitable compositions exhibit an optimal combination of such properties as strength (e.g., tensile and compressive), modulus, biocompatibility and biostability.
- the compositions When cured, the compositions demonstrate an optimal combination of properties, particularly in terms of their conformational stability and retention of physical shape, dissolution stability, biocompatibility, and physical performance, as well mechanical properties such as load-bearing strength, tensile strength, shear strength, shear fatigue resistance, impact absorption, wear resistance, and surface abrasion resistance. Such performance can be evaluated using procedures commonly accepted for the evaluation of natural tissue and joints, as well as the evaluation of materials and polymers in general.
- a preferred composition in its cured form, exhibits mechanical properties that approximate or exceed those of the natural tissue it is intended to provide or replace.
- a polymer system refers to the component or components used to prepare a polymeric composition of the present invention.
- a polymer system comprises the components necessary to form two parts: Part I being an NCO terminated pre-polymer (optionally referred to as an "isocyanate quasi-polymer").
- the quasi-polymer of Part I typically includes a polyol component, optionally in combination with a hydrophobic additive component, and an excess of an isocyanate component.
- Part II of the two component system can include one long-chain polyols, chain extenders and/or cross-linkers, together with other ingredients (e.g., catalysts, stabilizers, plasticizers, antioxidants, dyes and the like).
- Such adjuvants or ingredients can be added to or combined with any other component thereof either prior to or at the time of mixing, delivery, and/or curing.
- a polymer system of this invention is provided as a plurality of component parts and employs one or more catalysts.
- the component parts, including catalyst can be mixed to initiate cure, and then delivered, set and fully cured under conditions (e.g., time and exotherm) sufficient for its desired purpose.
- the resultant composition Upon the completion of cure, the resultant composition provides an optimal combination of properties for use in repairing or replacing injured or damaged tissue.
- the formulation provides an optimal combination of such properties as compatibility and stability of the biomaterial parts, ex vivo or in situ cure capability and characteristics (e.g., extractable levels, biocompatibility, thermal/ mechanical properties), mechanical properties (e.g., tensile, tear and fatigue properties), and biostability.
- the volume ratio of the parts can also be used to improve and affect the uncured and curing properties Compositions having two or more parts, are preferred. Where two parts are used, the relative volumes can range, for instance, from 1:10 to 10:1 (quasi-prepolymer to curative components, based on volume). A presently preferred range is between 2:1 and 1:2. As those skilled in the art will appreciate, given the present description, the optimal volume ratio is largely determined by the compatibility and the stability of part A and B.
- the viscosity of the reactive parts should provide an acceptable degree of mixing and flow rate, without causing mechanical failure of any component of the delivery system including cartridge, static mixer, gun and other components.
- the biomaterial is sufficiently flowable to permit it to be delivered (e.g., injected) into the mold or tissue site.
- the composition of both reactive parts must be such that these parts are homogeneous and phase stable in the temperature range of the application.
- the maximum temperature of the reaction exotherm is proportional to the concentration of the reactive groups in the mixed polymer. A high concentration of the reactive groups might evolve too high reaction exothermal energy and therefore cause thermal damage to the surrounding tissues.
- the reactive parts will preferably remain substantially liquid in form during mixing.
- a desired and stable volume ratio of the components can be achieved in any suitable manner, e.g., by the use of dual-compartment cartridges with constant volume ratio or by using the injectors with delivery rates independently variable for each component.
- Compatibility of the composition can also be affected (and improved) in other ways as well, e.g., by pre-heating the components prior to polymer application.
- the components of a preferred composition of this invention are preferably preheated before mixing and delivery, e.g., by heating to about 60 C to about 80 C for about 2 to about 6 hours prior to use.
- the composition parts are cooled back to about 35 C to 37 C before use in injection.
- Fully cured polymeric (e.g., polyurethane) biomaterials suitable for use in forming components of this invention provide an optimal combination of such properties as creep and abrasion resistance.
- the biomaterial provides DIN abrasion values of less than about 100 mm 3 , more preferably less than about 80 mm 3 and most preferably less than about 60 mm 3 , as determined by ASTM Test Method D5963-96 ("Standard Test Method for Rubber Property Abrasion Resistance Rotary Drum Abrader").
Landscapes
- Health & Medical Sciences (AREA)
- Orthopedic Medicine & Surgery (AREA)
- Chemical & Material Sciences (AREA)
- Life Sciences & Earth Sciences (AREA)
- Veterinary Medicine (AREA)
- Public Health (AREA)
- General Health & Medical Sciences (AREA)
- Animal Behavior & Ethology (AREA)
- Heart & Thoracic Surgery (AREA)
- Biomedical Technology (AREA)
- Engineering & Computer Science (AREA)
- Transplantation (AREA)
- Oral & Maxillofacial Surgery (AREA)
- Cardiology (AREA)
- Vascular Medicine (AREA)
- Medicinal Chemistry (AREA)
- Chemical Kinetics & Catalysis (AREA)
- Physical Education & Sports Medicine (AREA)
- Organic Chemistry (AREA)
- Polymers & Plastics (AREA)
- Surgery (AREA)
- Rheumatology (AREA)
- Nuclear Medicine, Radiotherapy & Molecular Imaging (AREA)
- Epidemiology (AREA)
- Medical Informatics (AREA)
- Molecular Biology (AREA)
- Pain & Pain Management (AREA)
- Dermatology (AREA)
- Prostheses (AREA)
- Materials For Medical Uses (AREA)
- Pharmaceuticals Containing Other Organic And Inorganic Compounds (AREA)
Applications Claiming Priority (3)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US22844400P | 2000-08-28 | 2000-08-28 | |
| US228444P | 2000-08-28 | ||
| PCT/US2001/041908 WO2002017821A2 (en) | 2000-08-28 | 2001-08-28 | Method for mammalian joint resurfacing |
Publications (2)
| Publication Number | Publication Date |
|---|---|
| EP1315470A2 EP1315470A2 (en) | 2003-06-04 |
| EP1315470B1 true EP1315470B1 (en) | 2009-07-15 |
Family
ID=22857197
Family Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP01964653A Expired - Lifetime EP1315470B1 (en) | 2000-08-28 | 2001-08-28 | System for mammalian joint resurfacing |
Country Status (7)
| Country | Link |
|---|---|
| US (6) | US20020127264A1 (enExample) |
| EP (1) | EP1315470B1 (enExample) |
| JP (1) | JP2004521666A (enExample) |
| AU (1) | AU2001285488A1 (enExample) |
| CA (1) | CA2420898A1 (enExample) |
| DE (1) | DE60139262D1 (enExample) |
| WO (1) | WO2002017821A2 (enExample) |
Families Citing this family (386)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US7468075B2 (en) | 2001-05-25 | 2008-12-23 | Conformis, Inc. | Methods and compositions for articular repair |
| US8556983B2 (en) | 2001-05-25 | 2013-10-15 | Conformis, Inc. | Patient-adapted and improved orthopedic implants, designs and related tools |
| US8480754B2 (en) * | 2001-05-25 | 2013-07-09 | Conformis, Inc. | Patient-adapted and improved articular implants, designs and related guide tools |
| US8771365B2 (en) | 2009-02-25 | 2014-07-08 | Conformis, Inc. | Patient-adapted and improved orthopedic implants, designs, and related tools |
| US7618451B2 (en) * | 2001-05-25 | 2009-11-17 | Conformis, Inc. | Patient selectable joint arthroplasty devices and surgical tools facilitating increased accuracy, speed and simplicity in performing total and partial joint arthroplasty |
| US8545569B2 (en) | 2001-05-25 | 2013-10-01 | Conformis, Inc. | Patient selectable knee arthroplasty devices |
| US8882847B2 (en) | 2001-05-25 | 2014-11-11 | Conformis, Inc. | Patient selectable knee joint arthroplasty devices |
| US8083745B2 (en) | 2001-05-25 | 2011-12-27 | Conformis, Inc. | Surgical tools for arthroplasty |
| US20090222103A1 (en) * | 2001-05-25 | 2009-09-03 | Conformis, Inc. | Articular Implants Providing Lower Adjacent Cartilage Wear |
| US20070233269A1 (en) * | 2001-05-25 | 2007-10-04 | Conformis, Inc. | Interpositional Joint Implant |
| US9603711B2 (en) | 2001-05-25 | 2017-03-28 | Conformis, Inc. | Patient-adapted and improved articular implants, designs and related guide tools |
| US7534263B2 (en) | 2001-05-25 | 2009-05-19 | Conformis, Inc. | Surgical tools facilitating increased accuracy, speed and simplicity in performing joint arthroplasty |
| US8735773B2 (en) | 2007-02-14 | 2014-05-27 | Conformis, Inc. | Implant device and method for manufacture |
| US6045551A (en) | 1998-02-06 | 2000-04-04 | Bonutti; Peter M. | Bone suture |
| ATE439806T1 (de) | 1998-09-14 | 2009-09-15 | Univ Leland Stanford Junior | Zustandsbestimmung eines gelenks und schadenvorsorge |
| US9289153B2 (en) * | 1998-09-14 | 2016-03-22 | The Board Of Trustees Of The Leland Stanford Junior University | Joint and cartilage diagnosis, assessment and modeling |
| US7239908B1 (en) | 1998-09-14 | 2007-07-03 | The Board Of Trustees Of The Leland Stanford Junior University | Assessing the condition of a joint and devising treatment |
| US20050033424A1 (en) * | 1999-05-10 | 2005-02-10 | Fell Barry M. | Surgically implantable knee prosthesis |
| US8066776B2 (en) * | 2001-12-14 | 2011-11-29 | Btg International Limited | Tibial component |
| US6368343B1 (en) | 2000-03-13 | 2002-04-09 | Peter M. Bonutti | Method of using ultrasonic vibration to secure body tissue |
| US6447516B1 (en) | 1999-08-09 | 2002-09-10 | Peter M. Bonutti | Method of securing tissue |
| US6875235B2 (en) * | 1999-10-08 | 2005-04-05 | Bret A. Ferree | Prosthetic joints with contained compressible resilient members |
| US6702821B2 (en) | 2000-01-14 | 2004-03-09 | The Bonutti 2003 Trust A | Instrumentation for minimally invasive joint replacement and methods for using same |
| US6635073B2 (en) | 2000-05-03 | 2003-10-21 | Peter M. Bonutti | Method of securing body tissue |
| US7635390B1 (en) | 2000-01-14 | 2009-12-22 | Marctec, Llc | Joint replacement component having a modular articulating surface |
| US7104996B2 (en) | 2000-01-14 | 2006-09-12 | Marctec. Llc | Method of performing surgery |
| US6610067B2 (en) | 2000-05-01 | 2003-08-26 | Arthrosurface, Incorporated | System and method for joint resurface repair |
| US8177841B2 (en) | 2000-05-01 | 2012-05-15 | Arthrosurface Inc. | System and method for joint resurface repair |
| EP2314257B9 (en) | 2000-05-01 | 2013-02-27 | ArthroSurface, Inc. | System for joint resurface repair |
| JP2004521666A (ja) | 2000-08-28 | 2004-07-22 | アドバンスト バイオ サーフェイシズ,インコーポレイティド | 哺乳動物の関節を増強する方法およびシステム |
| US6620196B1 (en) * | 2000-08-30 | 2003-09-16 | Sdgi Holdings, Inc. | Intervertebral disc nucleus implants and methods |
| AU2001290887B2 (en) | 2000-09-14 | 2006-06-08 | The Board Of Trustees Of The Leland Stanford Junior University | Assessing condition of a joint and cartilage loss |
| CA2425120A1 (en) | 2000-09-14 | 2002-03-21 | The Board Of Trustees Of The Leland Stanford Junior University | Assessing the condition of a joint and devising treatment |
| US8439926B2 (en) | 2001-05-25 | 2013-05-14 | Conformis, Inc. | Patient selectable joint arthroplasty devices and surgical tools |
| CA2447694A1 (en) | 2001-05-25 | 2002-12-05 | Imaging Therapeutics, Inc. | Methods and compositions for articular resurfacing |
| US6482209B1 (en) | 2001-06-14 | 2002-11-19 | Gerard A. Engh | Apparatus and method for sculpting the surface of a joint |
| US7708741B1 (en) | 2001-08-28 | 2010-05-04 | Marctec, Llc | Method of preparing bones for knee replacement surgery |
| ATE317070T1 (de) * | 2001-11-23 | 2006-02-15 | Univ Duisburg Essen | Implantat |
| US6719765B2 (en) | 2001-12-03 | 2004-04-13 | Bonutti 2003 Trust-A | Magnetic suturing system and method |
| EP1474071B1 (en) * | 2002-01-22 | 2010-05-19 | ABS Corporation | Interpositional arthroplasty system |
| US7613491B2 (en) | 2002-05-22 | 2009-11-03 | Dexcom, Inc. | Silicone based membranes for use in implantable glucose sensors |
| US6942475B2 (en) * | 2002-03-13 | 2005-09-13 | Ortho Development Corporation | Disposable knee mold |
| US7922772B2 (en) * | 2002-05-24 | 2011-04-12 | Zimmer, Inc. | Implants and related methods and apparatus for securing an implant on an articulating surface of an orthopedic joint |
| US7771483B2 (en) * | 2003-12-30 | 2010-08-10 | Zimmer, Inc. | Tibial condylar hemiplasty implants, anchor assemblies, and related methods |
| US20040049283A1 (en) * | 2002-06-04 | 2004-03-11 | Tushar Patel | Medical implant and method of reducing back pain |
| US20040006393A1 (en) * | 2002-07-03 | 2004-01-08 | Brian Burkinshaw | Implantable prosthetic knee for lateral compartment |
| EP1523291B1 (en) * | 2002-07-11 | 2008-06-18 | Advanced Bio Surfaces, Inc. | Kit for interpositional arthroplasty |
| TWI231755B (en) | 2002-10-07 | 2005-05-01 | Conformis Inc | An interpositional articular implant and the method for making the same |
| US20040070107A1 (en) * | 2002-10-09 | 2004-04-15 | Pragtech, Inc. | Method of making lubricious polyacrylonitrile artificial joint components and resulting product |
| US7309361B2 (en) * | 2002-10-23 | 2007-12-18 | Wasielewski Ray C | Biologic modular tibial and femoral component augments for use with total knee arthroplasty |
| AU2003287190A1 (en) | 2002-10-23 | 2004-05-13 | Alastair J. T. Clemow | Modular femoral component for a total knee joint replacement for minimally invasive implantation |
| WO2004043305A1 (en) | 2002-11-07 | 2004-05-27 | Conformis, Inc. | Methods for determing meniscal size and shape and for devising treatment |
| ATE287307T1 (de) | 2002-11-08 | 2005-02-15 | Howmedica Osteonics Corp | Lasererzeugte poröse oberfläche |
| US20060147332A1 (en) | 2004-12-30 | 2006-07-06 | Howmedica Osteonics Corp. | Laser-produced porous structure |
| EP1575456B1 (en) * | 2002-12-20 | 2011-02-09 | Smith & Nephew, Inc. | High performance knee prostheses |
| US6916341B2 (en) * | 2003-02-20 | 2005-07-12 | Lindsey R. Rolston | Device and method for bicompartmental arthroplasty |
| US8388624B2 (en) | 2003-02-24 | 2013-03-05 | Arthrosurface Incorporated | Trochlear resurfacing system and method |
| WO2004093747A1 (en) * | 2003-04-02 | 2004-11-04 | Ortho Development Corporation | Tibial augment connector |
| WO2005016175A2 (en) * | 2003-06-27 | 2005-02-24 | Advanced Bio Surfaces, Inc. | Meniscus preserving implant method and apparatus |
| ES2338886T3 (es) * | 2003-06-27 | 2010-05-13 | Memometal Technologies Sas | Sistema de artroplastia de tobillo. |
| US20050074877A1 (en) * | 2003-07-28 | 2005-04-07 | Mao Jeremy Jian | Biological engineering of articular structures containing both cartilage and bone |
| WO2005025451A2 (en) * | 2003-09-11 | 2005-03-24 | Advanced Bio Surfaces, Inc. | Method and materials for interpositional arthroplasty implant |
| EP1684672B1 (en) | 2003-10-17 | 2020-03-25 | Smith & Nephew, Inc. | High flexion articular insert |
| US20050119752A1 (en) * | 2003-11-19 | 2005-06-02 | Synecor Llc | Artificial intervertebral disc |
| CA2593182A1 (en) | 2003-11-20 | 2006-07-13 | Arthrosurface, Inc. | System and method for retrograde procedure |
| EP2338442B1 (en) | 2003-12-11 | 2013-01-30 | Isto Technologies Inc. | Particulate cartilage system |
| US7578824B2 (en) * | 2003-12-30 | 2009-08-25 | Zimmer, Inc. | Methods and apparatus for forming a tunnel through a proximal end of a tibia |
| US8236060B2 (en) * | 2003-12-30 | 2012-08-07 | Zimmer, Inc. | Tethered joint bearing implants and systems |
| US7819878B2 (en) * | 2003-12-30 | 2010-10-26 | Zimmer, Inc. | Tibial condylar hemiplasty tissue preparation instruments and methods |
| AU2005204920B2 (en) | 2004-01-12 | 2011-03-31 | Depuy Products, Inc. | Systems and methods for compartmental replacement in a knee |
| US8535383B2 (en) | 2004-01-12 | 2013-09-17 | DePuy Synthes Products, LLC | Systems and methods for compartmental replacement in a knee |
| US8002840B2 (en) | 2004-01-12 | 2011-08-23 | Depuy Products, Inc. | Systems and methods for compartmental replacement in a knee |
| US20050171604A1 (en) * | 2004-01-20 | 2005-08-04 | Alexander Michalow | Unicondylar knee implant |
| US8323349B2 (en) * | 2004-02-17 | 2012-12-04 | The University Of Notre Dame Du Lac | Textured surfaces for orthopedic implants |
| US20050197711A1 (en) * | 2004-03-03 | 2005-09-08 | Cachia Victor V. | Catheter deliverable foot implant and method of delivering the same |
| US7338529B1 (en) | 2004-03-30 | 2008-03-04 | Biomet Manufacturing Corp. | Methods and apparatuses for enhancing prosthetic implant durability |
| US20060095115A1 (en) * | 2004-05-10 | 2006-05-04 | Youssef Bladillah | Stent and method of manufacturing same |
| EP1765201A4 (en) | 2004-06-28 | 2013-01-23 | Arthrosurface Inc | SYSTEM FOR THE BENDING AREA |
| ATE386482T1 (de) * | 2004-07-02 | 2008-03-15 | Zimmer Tech Inc | Modulare patella-implant gelenkprothese mit unterschiedlichen komponenten |
| US8852195B2 (en) * | 2004-07-09 | 2014-10-07 | Zimmer, Inc. | Guide templates for surgical implants and related methods |
| FR2875398B1 (fr) * | 2004-09-21 | 2007-07-06 | Newdeal Sa Sa | Implant articulaire d'interposition |
| US7922769B2 (en) | 2004-09-27 | 2011-04-12 | Depuy Products, Inc. | Modular glenoid prosthesis and associated method |
| US7927335B2 (en) | 2004-09-27 | 2011-04-19 | Depuy Products, Inc. | Instrument for preparing an implant support surface and associated method |
| US7892287B2 (en) | 2004-09-27 | 2011-02-22 | Depuy Products, Inc. | Glenoid augment and associated method |
| US20090088846A1 (en) | 2007-04-17 | 2009-04-02 | David Myung | Hydrogel arthroplasty device |
| US7828853B2 (en) | 2004-11-22 | 2010-11-09 | Arthrosurface, Inc. | Articular surface implant and delivery system |
| US20090132047A1 (en) * | 2004-11-30 | 2009-05-21 | Mansmann Kevin A | Anchoring systems and interfaces for flexible surgical implants for replacing cartilage |
| US20060282169A1 (en) * | 2004-12-17 | 2006-12-14 | Felt Jeffrey C | System and method for upper extremity joint arthroplasty |
| WO2006074414A2 (en) * | 2005-01-08 | 2006-07-13 | Alphaspine, Inc. | Modular disc device |
| US20060178749A1 (en) * | 2005-02-10 | 2006-08-10 | Zimmer Technology, Inc. | Modular porous implant |
| US8828080B2 (en) * | 2005-02-22 | 2014-09-09 | Barry M. Fell | Method and system for knee joint repair |
| US20230080207A1 (en) | 2005-02-25 | 2023-03-16 | Shoulder Innovations, Inc. | Methods and devices for less invasive glenoid replacement |
| US8778028B2 (en) | 2005-02-25 | 2014-07-15 | Shoulder Innovations, Inc. | Methods and devices for less invasive glenoid replacement |
| US8007538B2 (en) | 2005-02-25 | 2011-08-30 | Shoulder Innovations, Llc | Shoulder implant for glenoid replacement |
| US8696707B2 (en) * | 2005-03-08 | 2014-04-15 | Zyga Technology, Inc. | Facet joint stabilization |
| US7267690B2 (en) * | 2005-03-09 | 2007-09-11 | Vertebral Technologies, Inc. | Interlocked modular disc nucleus prosthesis |
| US20060241758A1 (en) * | 2005-04-20 | 2006-10-26 | Sdgi Holdings, Inc. | Facet spacers |
| WO2006127849A2 (en) * | 2005-05-24 | 2006-11-30 | Vertebral Technologies, Inc. | Rail-based modular disc nucleus prosthesis |
| US7655584B2 (en) * | 2005-07-29 | 2010-02-02 | Gore Enterprise Holdings, Inc. | Highly porous self-cohered web materials |
| US7604668B2 (en) | 2005-07-29 | 2009-10-20 | Gore Enterprise Holdings, Inc. | Composite self-cohered web materials |
| US7850810B2 (en) | 2005-07-29 | 2010-12-14 | Gore Enterprise Holdings, Inc. | Method of making porous self-cohered web materials |
| JP5292533B2 (ja) | 2005-08-26 | 2013-09-18 | ジンマー・インコーポレイテッド | インプラントおよび関節疾患の治療、置換および治療方法 |
| US7799087B2 (en) * | 2005-08-31 | 2010-09-21 | Zimmer Gmbh | Implant |
| US8691542B2 (en) * | 2005-09-09 | 2014-04-08 | Cytex Therapeutics, Inc. | Tissue engineering methods and compositions |
| US20070088444A1 (en) * | 2005-10-13 | 2007-04-19 | Robert A Hodorek | Method for repairing a bone defect using a formable implant which hardens in vivo |
| US7618422B2 (en) * | 2005-11-07 | 2009-11-17 | Howmedica Osteonics Corp. | Tibial augmentation guide |
| CA2640759A1 (en) | 2005-11-09 | 2007-05-18 | Zimmer Gmbh | Implant |
| US7744630B2 (en) * | 2005-11-15 | 2010-06-29 | Zimmer Spine, Inc. | Facet repair and stabilization |
| EP1951158A4 (en) * | 2005-11-21 | 2010-03-31 | Vertegen Inc | DEVICES AND METHODS FOR TREATMENT OF FACE CHAINS, UNCOVERTEBRAL JOINTS, COSTOVERTEBRUSK JOINTS AND OTHER JOINTS |
| US7766969B2 (en) * | 2005-12-05 | 2010-08-03 | Zimmer, Inc. | Modular progressive implant for a joint articulation surface |
| US8728387B2 (en) | 2005-12-06 | 2014-05-20 | Howmedica Osteonics Corp. | Laser-produced porous surface |
| DE102005063249B3 (de) * | 2005-12-21 | 2007-08-09 | Aesculap Ag & Co. Kg | Künstliches Meniskusteil |
| EP1803513B1 (en) * | 2005-12-30 | 2017-03-29 | Howmedica Osteonics Corp. | Method of manufacturing implants using laser |
| US20070179607A1 (en) * | 2006-01-31 | 2007-08-02 | Zimmer Technology, Inc. | Cartilage resurfacing implant |
| CN105030297A (zh) | 2006-02-06 | 2015-11-11 | 康复米斯公司 | 患者可选择的关节成形术装置和手术器具 |
| US8623026B2 (en) | 2006-02-06 | 2014-01-07 | Conformis, Inc. | Patient selectable joint arthroplasty devices and surgical tools incorporating anatomical relief |
| WO2007090790A2 (de) * | 2006-02-09 | 2007-08-16 | Zimmer Gmbh | Implantat |
| US8591516B2 (en) | 2006-02-27 | 2013-11-26 | Biomet Manufacturing, Llc | Patient-specific orthopedic instruments |
| US8603180B2 (en) | 2006-02-27 | 2013-12-10 | Biomet Manufacturing, Llc | Patient-specific acetabular alignment guides |
| US8858561B2 (en) | 2006-06-09 | 2014-10-14 | Blomet Manufacturing, LLC | Patient-specific alignment guide |
| US20110046735A1 (en) * | 2006-02-27 | 2011-02-24 | Biomet Manufacturing Corp. | Patient-Specific Implants |
| US9289253B2 (en) | 2006-02-27 | 2016-03-22 | Biomet Manufacturing, Llc | Patient-specific shoulder guide |
| US8092465B2 (en) | 2006-06-09 | 2012-01-10 | Biomet Manufacturing Corp. | Patient specific knee alignment guide and associated method |
| US20150335438A1 (en) | 2006-02-27 | 2015-11-26 | Biomet Manufacturing, Llc. | Patient-specific augments |
| US8407067B2 (en) | 2007-04-17 | 2013-03-26 | Biomet Manufacturing Corp. | Method and apparatus for manufacturing an implant |
| US9113971B2 (en) | 2006-02-27 | 2015-08-25 | Biomet Manufacturing, Llc | Femoral acetabular impingement guide |
| US8864769B2 (en) | 2006-02-27 | 2014-10-21 | Biomet Manufacturing, Llc | Alignment guides with patient-specific anchoring elements |
| US8568487B2 (en) | 2006-02-27 | 2013-10-29 | Biomet Manufacturing, Llc | Patient-specific hip joint devices |
| US9345548B2 (en) | 2006-02-27 | 2016-05-24 | Biomet Manufacturing, Llc | Patient-specific pre-operative planning |
| US9907659B2 (en) | 2007-04-17 | 2018-03-06 | Biomet Manufacturing, Llc | Method and apparatus for manufacturing an implant |
| US8535387B2 (en) | 2006-02-27 | 2013-09-17 | Biomet Manufacturing, Llc | Patient-specific tools and implants |
| US9918740B2 (en) | 2006-02-27 | 2018-03-20 | Biomet Manufacturing, Llc | Backup surgical instrument system and method |
| US9173661B2 (en) | 2006-02-27 | 2015-11-03 | Biomet Manufacturing, Llc | Patient specific alignment guide with cutting surface and laser indicator |
| US9339278B2 (en) | 2006-02-27 | 2016-05-17 | Biomet Manufacturing, Llc | Patient-specific acetabular guides and associated instruments |
| US8608748B2 (en) | 2006-02-27 | 2013-12-17 | Biomet Manufacturing, Llc | Patient specific guides |
| US8377066B2 (en) | 2006-02-27 | 2013-02-19 | Biomet Manufacturing Corp. | Patient-specific elbow guides and associated methods |
| US8133234B2 (en) | 2006-02-27 | 2012-03-13 | Biomet Manufacturing Corp. | Patient specific acetabular guide and method |
| US10278711B2 (en) | 2006-02-27 | 2019-05-07 | Biomet Manufacturing, Llc | Patient-specific femoral guide |
| US8608749B2 (en) | 2006-02-27 | 2013-12-17 | Biomet Manufacturing, Llc | Patient-specific acetabular guides and associated instruments |
| US7967868B2 (en) | 2007-04-17 | 2011-06-28 | Biomet Manufacturing Corp. | Patient-modified implant and associated method |
| US7927358B2 (en) * | 2006-03-07 | 2011-04-19 | Zimmer Spine, Inc. | Spinal stabilization device |
| US9474619B2 (en) * | 2006-03-21 | 2016-10-25 | Tornier, Inc. | Glenoid component with improved fixation stability |
| US20070233268A1 (en) * | 2006-03-31 | 2007-10-04 | Depuy Products, Inc. | Interpositional knee arthroplasty |
| EP2010074A4 (en) * | 2006-04-26 | 2012-08-29 | Illuminoss Medical Inc | DEVICE AND METHOD FOR BONE GAINING |
| US7806900B2 (en) | 2006-04-26 | 2010-10-05 | Illuminoss Medical, Inc. | Apparatus and methods for delivery of reinforcing materials to bone |
| US8632601B2 (en) * | 2006-04-28 | 2014-01-21 | Zimmer, Gmbh | Implant |
| GB0609058D0 (en) * | 2006-05-09 | 2006-06-14 | Finsbury Dev Ltd | Knee prosthesis |
| US20070288021A1 (en) * | 2006-06-07 | 2007-12-13 | Howmedica Osteonics Corp. | Flexible joint implant |
| US9795399B2 (en) | 2006-06-09 | 2017-10-24 | Biomet Manufacturing, Llc | Patient-specific knee alignment guide and associated method |
| ES2568932T3 (es) | 2006-06-30 | 2016-05-05 | Smith & Nephew, Inc. | Prótesis articulada para movimiento anatómico |
| US8147861B2 (en) | 2006-08-15 | 2012-04-03 | Howmedica Osteonics Corp. | Antimicrobial implant |
| US20080058949A1 (en) * | 2006-09-06 | 2008-03-06 | Roger Ryan Dees | Implants with Transition Surfaces and Related Processes |
| US7988711B2 (en) * | 2006-09-21 | 2011-08-02 | Warsaw Orthopedic, Inc. | Low profile vertebral stabilization systems and methods |
| US8192491B2 (en) | 2006-10-09 | 2012-06-05 | Active Implants Corporation | Meniscus prosthetic device |
| WO2008045807A2 (en) | 2006-10-09 | 2008-04-17 | Active Implants Corporation | Meniscus prosthetic device |
| US20080097606A1 (en) * | 2006-10-19 | 2008-04-24 | Cragg Andrew H | Knee joint prosthesis and hyaluronate compositions for treatment of osteoarthritis |
| EP2091445B1 (en) | 2006-11-10 | 2015-03-11 | Illuminoss Medical, Inc. | Systems for internal bone fixation |
| US7879041B2 (en) | 2006-11-10 | 2011-02-01 | Illuminoss Medical, Inc. | Systems and methods for internal bone fixation |
| US9737414B2 (en) | 2006-11-21 | 2017-08-22 | Vertebral Technologies, Inc. | Methods and apparatus for minimally invasive modular interbody fusion devices |
| US9358029B2 (en) | 2006-12-11 | 2016-06-07 | Arthrosurface Incorporated | Retrograde resection apparatus and method |
| US8163549B2 (en) | 2006-12-20 | 2012-04-24 | Zimmer Orthobiologics, Inc. | Method of obtaining viable small tissue particles and use for tissue repair |
| US8663328B2 (en) * | 2006-12-21 | 2014-03-04 | Warsaw Orthopedic, Inc. | Methods for positioning a load-bearing component of an orthopedic implant device by inserting a malleable device that hardens in vivo |
| US8758407B2 (en) * | 2006-12-21 | 2014-06-24 | Warsaw Orthopedic, Inc. | Methods for positioning a load-bearing orthopedic implant device in vivo |
| US9039768B2 (en) | 2006-12-22 | 2015-05-26 | Medos International Sarl | Composite vertebral spacers and instrument |
| WO2008090468A2 (en) * | 2007-01-22 | 2008-07-31 | Zimmer, Gmbh | An implant and a method for partial replacement of joint surfaces |
| US20080234540A1 (en) * | 2007-01-31 | 2008-09-25 | Warsaw Orthopedic, Inc. | Osteochondral Implant Procedure |
| US20110093084A1 (en) * | 2007-02-09 | 2011-04-21 | Morton Troy N | Artificial joint preserving tendon and/or sesamoid bone structure |
| US8292966B2 (en) * | 2007-02-09 | 2012-10-23 | Morton Ballard Arthrotechnology, LLC. | Artificial toe joint |
| US20110093085A1 (en) * | 2007-02-09 | 2011-04-21 | Morton Troy N | Artificial joint and insert |
| AU2008216173A1 (en) * | 2007-02-14 | 2008-08-21 | Smith & Nephew, Inc. | Method and system for computer assisted surgery for bicompartmental knee replacement |
| EP2591756A1 (en) | 2007-02-14 | 2013-05-15 | Conformis, Inc. | Implant device and method for manufacture |
| US9814581B2 (en) | 2007-02-26 | 2017-11-14 | Marvin Schwartz | Mobile prosthesis for interpositional location between bone joint articular surfaces and method of use |
| US7670381B2 (en) * | 2007-02-26 | 2010-03-02 | Marvin Schwartz | Prosthesis for interpositional location between bone joint articular surfaces and method of use |
| US8506637B2 (en) | 2007-02-26 | 2013-08-13 | Marvin Schwartz | Mobile prosthesis for interpositional location between bone joint articular surfaces and method of use |
| CN104473704B (zh) | 2007-03-15 | 2017-06-16 | 矫正-空位有限公司 | 假体装置及其使用方法 |
| US8147557B2 (en) * | 2007-03-30 | 2012-04-03 | Depuy Products, Inc. | Mobile bearing insert having offset dwell point |
| US8328874B2 (en) | 2007-03-30 | 2012-12-11 | Depuy Products, Inc. | Mobile bearing assembly |
| US8142510B2 (en) | 2007-03-30 | 2012-03-27 | Depuy Products, Inc. | Mobile bearing assembly having a non-planar interface |
| US8764841B2 (en) | 2007-03-30 | 2014-07-01 | DePuy Synthes Products, LLC | Mobile bearing assembly having a closed track |
| US8147558B2 (en) | 2007-03-30 | 2012-04-03 | Depuy Products, Inc. | Mobile bearing assembly having multiple articulation interfaces |
| US20090012612A1 (en) * | 2007-04-10 | 2009-01-08 | David White | Devices and methods for push-delivery of implants |
| US20080255664A1 (en) | 2007-04-10 | 2008-10-16 | Mdesign International | Percutaneously deliverable orthopedic joint device |
| US20080255665A1 (en) * | 2007-04-11 | 2008-10-16 | Active Implants Corporation | Anchored prosthetic meniscus device |
| AU2008240191B2 (en) * | 2007-04-12 | 2013-09-19 | Zimmer, Inc. | Compositions and methods for tissue repair |
| EP1985319B1 (en) * | 2007-04-23 | 2012-06-13 | Jointsphere B.V. | Device for cartilage repair |
| WO2008157412A2 (en) | 2007-06-13 | 2008-12-24 | Conformis, Inc. | Surgical cutting guide |
| US8142886B2 (en) | 2007-07-24 | 2012-03-27 | Howmedica Osteonics Corp. | Porous laser sintered articles |
| US8979935B2 (en) * | 2007-07-31 | 2015-03-17 | Zimmer, Inc. | Joint space interpositional prosthetic device with internal bearing surfaces |
| US8343189B2 (en) | 2007-09-25 | 2013-01-01 | Zyga Technology, Inc. | Method and apparatus for facet joint stabilization |
| US7918893B2 (en) | 2007-09-30 | 2011-04-05 | Depuy Products, Inc. | Hinged orthopaedic prosthesis |
| ES2387583T3 (es) * | 2007-10-19 | 2012-09-26 | Stryker Trauma Gmbh | Sustituto de hueso sintético, procedimiento para preparar el mismo y procedimiento para rellenar una cavidad en un sustrato |
| US9427289B2 (en) | 2007-10-31 | 2016-08-30 | Illuminoss Medical, Inc. | Light source |
| US20090118833A1 (en) * | 2007-11-05 | 2009-05-07 | Zimmer Spine, Inc. | In-situ curable interspinous process spacer |
| US20090138092A1 (en) * | 2007-11-28 | 2009-05-28 | Johnston Brent W | Therapeutic Structures for Utilization in Temporomandibular Joint Replacement Systems |
| EP2288312B1 (en) | 2007-12-07 | 2016-09-28 | Zimmer Orthopaedic Surgical Products, Inc. | Spacer molds and methods therefor |
| US8403968B2 (en) | 2007-12-26 | 2013-03-26 | Illuminoss Medical, Inc. | Apparatus and methods for repairing craniomaxillofacial bones using customized bone plates |
| US7690864B2 (en) * | 2007-12-27 | 2010-04-06 | Allen Engineering Corporation | Hydraulic riding trowel with automatic load sensing system |
| US8252029B2 (en) * | 2008-02-21 | 2012-08-28 | Zimmer Gmbh | Expandable interspinous process spacer with lateral support and method for implantation |
| WO2009111481A1 (en) | 2008-03-03 | 2009-09-11 | Arthrosurface Incorporated | Bone resurfacing system and method |
| US8682052B2 (en) | 2008-03-05 | 2014-03-25 | Conformis, Inc. | Implants for altering wear patterns of articular surfaces |
| US8152846B2 (en) * | 2008-03-06 | 2012-04-10 | Musculoskeletal Transplant Foundation | Instrumentation and method for repair of meniscus tissue |
| US20090248092A1 (en) | 2008-03-26 | 2009-10-01 | Jonathan Bellas | Posterior Intervertebral Disc Inserter and Expansion Techniques |
| US8361147B2 (en) | 2008-04-09 | 2013-01-29 | Active Implants Corporation | Meniscus prosthetic devices with anti-migration features |
| US7991599B2 (en) * | 2008-04-09 | 2011-08-02 | Active Implants Corporation | Meniscus prosthetic device selection and implantation methods |
| US7611653B1 (en) * | 2008-04-09 | 2009-11-03 | Active Implants Corporation | Manufacturing and material processing for prosthetic devices |
| US8016884B2 (en) * | 2008-04-09 | 2011-09-13 | Active Implants Corporation | Tensioned meniscus prosthetic devices and associated methods |
| AU2009246474B2 (en) | 2008-05-12 | 2015-04-16 | Conformis, Inc. | Devices and methods for treatment of facet and other joints |
| US20120209396A1 (en) | 2008-07-07 | 2012-08-16 | David Myung | Orthopedic implants having gradient polymer alloys |
| US8529631B2 (en) * | 2008-07-18 | 2013-09-10 | Zimmer, Gmbh | Base component for a tibial implant |
| US9364338B2 (en) | 2008-07-23 | 2016-06-14 | Resspond Spinal Systems | Modular nucleus pulposus prosthesis |
| US8795375B2 (en) | 2008-07-23 | 2014-08-05 | Resspond Spinal Systems | Modular nucleus pulposus prosthesis |
| US9808345B2 (en) | 2008-07-24 | 2017-11-07 | Iorthopedics, Inc. | Resilient arthroplasty device |
| WO2010017282A1 (en) | 2008-08-05 | 2010-02-11 | Biomimedica, Inc. | Polyurethane-grafted hydrogels |
| US8475505B2 (en) | 2008-08-13 | 2013-07-02 | Smed-Ta/Td, Llc | Orthopaedic screws |
| US20100042213A1 (en) | 2008-08-13 | 2010-02-18 | Nebosky Paul S | Drug delivery implants |
| US9700431B2 (en) | 2008-08-13 | 2017-07-11 | Smed-Ta/Td, Llc | Orthopaedic implant with porous structural member |
| US9616205B2 (en) | 2008-08-13 | 2017-04-11 | Smed-Ta/Td, Llc | Drug delivery implants |
| US10842645B2 (en) | 2008-08-13 | 2020-11-24 | Smed-Ta/Td, Llc | Orthopaedic implant with porous structural member |
| EP2341852B1 (en) | 2008-08-29 | 2018-08-15 | SMed-TA/TD, LLC | Orthopaedic implant |
| AU2009291581A1 (en) * | 2008-09-12 | 2010-03-18 | Articulinx, Inc. | Tether-based orthopedic joint device delivery methods |
| US8257357B2 (en) * | 2008-09-23 | 2012-09-04 | Edwin Burton Hatch | Combination of a motor driven oscillating orthopedic reshaping and resurfacing tool and a surface-matching sheet metal prosthesis |
| CN102548510B (zh) | 2008-10-29 | 2015-04-01 | 捷迈骨科手术产品公司 | 具有可拆卸固定件的间隔件模具 |
| US10258473B2 (en) * | 2008-11-19 | 2019-04-16 | Softjoint Corporation | Device and method for restoring joints with artificial cartilage |
| US8241365B2 (en) | 2008-12-23 | 2012-08-14 | Depuy Products, Inc. | Shoulder prosthesis with vault-filling structure having bone-sparing configuration |
| US12383287B2 (en) | 2009-02-24 | 2025-08-12 | Microport Orthopedics Holdings, Inc. | Systems and methods for installing an orthopedic implant |
| US8808297B2 (en) | 2009-02-24 | 2014-08-19 | Microport Orthopedics Holdings Inc. | Orthopedic surgical guide |
| EP2405865B1 (en) | 2009-02-24 | 2019-04-17 | ConforMIS, Inc. | Automated systems for manufacturing patient-specific orthopedic implants and instrumentation |
| US9017334B2 (en) | 2009-02-24 | 2015-04-28 | Microport Orthopedics Holdings Inc. | Patient specific surgical guide locator and mount |
| US8808303B2 (en) | 2009-02-24 | 2014-08-19 | Microport Orthopedics Holdings Inc. | Orthopedic surgical guide |
| US9545311B2 (en) | 2009-03-05 | 2017-01-17 | Tornier, Inc. | Glenoid implant anchor post |
| US9526620B2 (en) | 2009-03-30 | 2016-12-27 | DePuy Synthes Products, Inc. | Zero profile spinal fusion cage |
| US20100256758A1 (en) * | 2009-04-02 | 2010-10-07 | Synvasive Technology, Inc. | Monolithic orthopedic implant with an articular finished surface |
| US8556972B2 (en) * | 2009-04-02 | 2013-10-15 | Sevika Holding AG | Monolithic orthopedic implant with an articular finished surface |
| US8210729B2 (en) | 2009-04-06 | 2012-07-03 | Illuminoss Medical, Inc. | Attachment system for light-conducting fibers |
| US8512338B2 (en) | 2009-04-07 | 2013-08-20 | Illuminoss Medical, Inc. | Photodynamic bone stabilization systems and methods for reinforcing bone |
| JP2012523897A (ja) | 2009-04-16 | 2012-10-11 | コンフォーミス・インコーポレイテッド | 靭帯修復のための患者固有の関節置換術の装置 |
| US9662126B2 (en) | 2009-04-17 | 2017-05-30 | Arthrosurface Incorporated | Glenoid resurfacing system and method |
| US9283076B2 (en) | 2009-04-17 | 2016-03-15 | Arthrosurface Incorporated | Glenoid resurfacing system and method |
| WO2016154393A1 (en) | 2009-04-17 | 2016-09-29 | Arthrosurface Incorporated | Glenoid repair system and methods of use thereof |
| EP2434989B1 (en) | 2009-05-29 | 2018-07-11 | Smith&Nephew, Inc. | Apparatus for performing knee arthroplasty |
| US9549820B2 (en) * | 2009-06-25 | 2017-01-24 | Zimmer, Inc. | Glenoid implant with synthetic labrum |
| US9375315B2 (en) * | 2009-07-10 | 2016-06-28 | Peter Forsell | Joint device and method |
| US9180011B2 (en) * | 2009-07-10 | 2015-11-10 | Peter Forsell | Implantable circulating lubrication system for joints |
| US8394125B2 (en) | 2009-07-24 | 2013-03-12 | Zyga Technology, Inc. | Systems and methods for facet joint treatment |
| DE102009028503B4 (de) | 2009-08-13 | 2013-11-14 | Biomet Manufacturing Corp. | Resektionsschablone zur Resektion von Knochen, Verfahren zur Herstellung einer solchen Resektionsschablone und Operationsset zur Durchführung von Kniegelenk-Operationen |
| BR112012003783A2 (pt) | 2009-08-19 | 2016-04-19 | Illuminoss Medical Inc | dispositivos e métodos para alinhamento, estabilização e distração óssea |
| WO2011032043A1 (en) | 2009-09-11 | 2011-03-17 | Articulinx, Inc. | Disc-shaped orthopedic devices |
| US8152854B2 (en) * | 2009-09-30 | 2012-04-10 | Imbriglia Joseph E | Resurfacing implant for the wrist and method of implantation thereof |
| WO2011060062A1 (en) * | 2009-11-10 | 2011-05-19 | Illuminoss Medical, Inc. | Intramedullary implants having variable fastener placement |
| US8231683B2 (en) | 2009-12-08 | 2012-07-31 | Depuy Products, Inc. | Shoulder prosthesis assembly having glenoid rim replacement structure |
| US9393129B2 (en) | 2009-12-10 | 2016-07-19 | DePuy Synthes Products, Inc. | Bellows-like expandable interbody fusion cage |
| CA2782137A1 (en) | 2009-12-11 | 2011-06-16 | Conformis, Inc. | Patient-specific and patient-engineered orthopedic implants |
| WO2011091005A2 (en) | 2010-01-22 | 2011-07-28 | Grotz R Thomas | Resilient knee implant and methods |
| US10307257B2 (en) | 2010-01-22 | 2019-06-04 | Iorthopedics, Inc. | Resilient knee implant and methods |
| US20130060334A1 (en) * | 2010-02-25 | 2013-03-07 | Orteq B.V. | Meniscus repair assembly and method |
| US8632547B2 (en) | 2010-02-26 | 2014-01-21 | Biomet Sports Medicine, Llc | Patient-specific osteotomy devices and methods |
| WO2011109836A1 (en) | 2010-03-05 | 2011-09-09 | Arthrosurface Incorporated | Tibial resurfacing system and method |
| US9233006B2 (en) | 2010-06-15 | 2016-01-12 | Zyga Technology, Inc. | Systems and methods for facet joint treatment |
| US8663293B2 (en) | 2010-06-15 | 2014-03-04 | Zyga Technology, Inc. | Systems and methods for facet joint treatment |
| US8684965B2 (en) | 2010-06-21 | 2014-04-01 | Illuminoss Medical, Inc. | Photodynamic bone stabilization and drug delivery systems |
| AU2011271681A1 (en) * | 2010-07-01 | 2013-02-21 | Sevika Holding AG | Convex concave implant |
| JP2013537451A (ja) * | 2010-08-12 | 2013-10-03 | プロストヘクシス ピーティワイ リミテッド | 人工半月と、ヒト膝関節における移植の方法 |
| CA2808528A1 (en) | 2010-08-27 | 2012-03-01 | Biomimedica, Inc. | Hydrophobic and hydrophilic interpenetrating polymer networks derived from hydrophobic polymers and methods of preparing the same |
| US20120078373A1 (en) | 2010-09-23 | 2012-03-29 | Thomas Gamache | Stand alone intervertebral fusion device |
| US20120078372A1 (en) | 2010-09-23 | 2012-03-29 | Thomas Gamache | Novel implant inserter having a laterally-extending dovetail engagement feature |
| US11529241B2 (en) | 2010-09-23 | 2022-12-20 | DePuy Synthes Products, Inc. | Fusion cage with in-line single piece fixation |
| US9271744B2 (en) | 2010-09-29 | 2016-03-01 | Biomet Manufacturing, Llc | Patient-specific guide for partial acetabular socket replacement |
| US8465548B2 (en) | 2010-11-24 | 2013-06-18 | DePuy Synthes Products, LLC | Modular glenoid prosthesis |
| US8480750B2 (en) | 2010-11-24 | 2013-07-09 | DePuy Synthes Products, LLC | Modular glenoid prosthesis |
| US9968376B2 (en) | 2010-11-29 | 2018-05-15 | Biomet Manufacturing, Llc | Patient-specific orthopedic instruments |
| US9179959B2 (en) | 2010-12-22 | 2015-11-10 | Illuminoss Medical, Inc. | Systems and methods for treating conditions and diseases of the spine |
| USD833613S1 (en) | 2011-01-19 | 2018-11-13 | Iorthopedics, Inc. | Resilient knee implant |
| WO2012112694A2 (en) | 2011-02-15 | 2012-08-23 | Conformis, Inc. | Medeling, analyzing and using anatomical data for patient-adapted implants. designs, tools and surgical procedures |
| US9241745B2 (en) | 2011-03-07 | 2016-01-26 | Biomet Manufacturing, Llc | Patient-specific femoral version guide |
| US9066716B2 (en) | 2011-03-30 | 2015-06-30 | Arthrosurface Incorporated | Suture coil and suture sheath for tissue repair |
| US8715289B2 (en) | 2011-04-15 | 2014-05-06 | Biomet Manufacturing, Llc | Patient-specific numerically controlled instrument |
| US9675400B2 (en) | 2011-04-19 | 2017-06-13 | Biomet Manufacturing, Llc | Patient-specific fracture fixation instrumentation and method |
| US8747479B2 (en) | 2011-04-26 | 2014-06-10 | Michael A. McShane | Tibial component |
| US8668700B2 (en) | 2011-04-29 | 2014-03-11 | Biomet Manufacturing, Llc | Patient-specific convertible guides |
| US8956364B2 (en) | 2011-04-29 | 2015-02-17 | Biomet Manufacturing, Llc | Patient-specific partial knee guides and other instruments |
| US9861372B2 (en) | 2011-05-27 | 2018-01-09 | Howmedica Osteonics Corp. | Prosthetic implant and associated instruments |
| US8532807B2 (en) | 2011-06-06 | 2013-09-10 | Biomet Manufacturing, Llc | Pre-operative planning and manufacturing method for orthopedic procedure |
| US9084618B2 (en) | 2011-06-13 | 2015-07-21 | Biomet Manufacturing, Llc | Drill guides for confirming alignment of patient-specific alignment guides |
| US20130001121A1 (en) | 2011-07-01 | 2013-01-03 | Biomet Manufacturing Corp. | Backup kit for a patient-specific arthroplasty kit assembly |
| US8764760B2 (en) | 2011-07-01 | 2014-07-01 | Biomet Manufacturing, Llc | Patient-specific bone-cutting guidance instruments and methods |
| JP2014524809A (ja) * | 2011-07-13 | 2014-09-25 | ザ ジェネラル ホスピタル コーポレーション ドゥーイング ビジネス アズ マサチューセッツ ジェネラル ホスピタル | 前十字靱帯代替を有する膝関節置換用の方法および装置 |
| US9775661B2 (en) | 2011-07-19 | 2017-10-03 | Illuminoss Medical, Inc. | Devices and methods for bone restructure and stabilization |
| US8597365B2 (en) | 2011-08-04 | 2013-12-03 | Biomet Manufacturing, Llc | Patient-specific pelvic implants for acetabular reconstruction |
| US9295497B2 (en) | 2011-08-31 | 2016-03-29 | Biomet Manufacturing, Llc | Patient-specific sacroiliac and pedicle guides |
| US9066734B2 (en) | 2011-08-31 | 2015-06-30 | Biomet Manufacturing, Llc | Patient-specific sacroiliac guides and associated methods |
| EP2750629B1 (en) | 2011-09-01 | 2016-07-13 | R. Thomas Grotz | Resilient interpositional arthroplasty device |
| US9248028B2 (en) | 2011-09-16 | 2016-02-02 | DePuy Synthes Products, Inc. | Removable, bone-securing cover plate for intervertebral fusion cage |
| US9386993B2 (en) | 2011-09-29 | 2016-07-12 | Biomet Manufacturing, Llc | Patient-specific femoroacetabular impingement instruments and methods |
| KR20140115294A (ko) | 2011-10-03 | 2014-09-30 | 바이오미메디카, 인코포레이티드 | 순응성 재료들을 또 다른 표면으로 앵커링하기 위한 중합체성 접착제 |
| US9289307B2 (en) | 2011-10-18 | 2016-03-22 | Ortho-Space Ltd. | Prosthetic devices and methods for using same |
| WO2013059609A1 (en) | 2011-10-19 | 2013-04-25 | Illuminoss Medical, Inc. | Systems and methods for joint stabilization |
| US9554910B2 (en) | 2011-10-27 | 2017-01-31 | Biomet Manufacturing, Llc | Patient-specific glenoid guide and implants |
| US9451973B2 (en) | 2011-10-27 | 2016-09-27 | Biomet Manufacturing, Llc | Patient specific glenoid guide |
| EP2770918B1 (en) | 2011-10-27 | 2017-07-19 | Biomet Manufacturing, LLC | Patient-specific glenoid guides |
| US9301812B2 (en) | 2011-10-27 | 2016-04-05 | Biomet Manufacturing, Llc | Methods for patient-specific shoulder arthroplasty |
| KR20130046337A (ko) | 2011-10-27 | 2013-05-07 | 삼성전자주식회사 | 멀티뷰 디바이스 및 그 제어방법과, 디스플레이장치 및 그 제어방법과, 디스플레이 시스템 |
| US9468536B1 (en) | 2011-11-02 | 2016-10-18 | Nuvasive, Inc. | Spinal fusion implants and related methods |
| KR20140113655A (ko) | 2011-11-21 | 2014-09-24 | 바이오미메디카, 인코포레이티드 | 정형외과적 임플란트를 뼈에 앵커링하기 위한 시스템, 장치, 및 방법 |
| WO2013096746A1 (en) | 2011-12-22 | 2013-06-27 | Arthrosurface Incorporated | System and method for bone fixation |
| US9408686B1 (en) | 2012-01-20 | 2016-08-09 | Conformis, Inc. | Devices, systems and methods for manufacturing orthopedic implants |
| US9237950B2 (en) | 2012-02-02 | 2016-01-19 | Biomet Manufacturing, Llc | Implant with patient-specific porous structure |
| US9364896B2 (en) | 2012-02-07 | 2016-06-14 | Medical Modeling Inc. | Fabrication of hybrid solid-porous medical implantable devices with electron beam melting technology |
| US9271836B2 (en) | 2012-03-06 | 2016-03-01 | DePuy Synthes Products, Inc. | Nubbed plate |
| US9510953B2 (en) | 2012-03-16 | 2016-12-06 | Vertebral Technologies, Inc. | Modular segmented disc nucleus implant |
| US9180010B2 (en) | 2012-04-06 | 2015-11-10 | Howmedica Osteonics Corp. | Surface modified unit cell lattice structures for optimized secure freeform fabrication |
| US9135374B2 (en) | 2012-04-06 | 2015-09-15 | Howmedica Osteonics Corp. | Surface modified unit cell lattice structures for optimized secure freeform fabrication |
| US9486226B2 (en) | 2012-04-18 | 2016-11-08 | Conformis, Inc. | Tibial guides, tools, and techniques for resecting the tibial plateau |
| US9237952B2 (en) * | 2012-04-30 | 2016-01-19 | William B. Kurtz | Total knee arthroplasty system and method |
| US20150127104A1 (en) * | 2012-05-03 | 2015-05-07 | ULTIMATE JOINT LTD. a corporation | In-situ formation of a joint replacement prosthesis |
| US9675471B2 (en) | 2012-06-11 | 2017-06-13 | Conformis, Inc. | Devices, techniques and methods for assessing joint spacing, balancing soft tissues and obtaining desired kinematics for joint implant components |
| DE112013003358T5 (de) | 2012-07-03 | 2015-03-19 | Arthrosurface, Inc. | System und Verfahren für Gelenkoberflächenersatz und -reparatur |
| US8939977B2 (en) | 2012-07-10 | 2015-01-27 | Illuminoss Medical, Inc. | Systems and methods for separating bone fixation devices from introducer |
| IN2015DN02998A (enExample) | 2012-10-18 | 2015-10-02 | Smith & Nephew Inc | |
| JP6085682B2 (ja) * | 2012-10-29 | 2017-02-22 | カーディアック ペースメイカーズ, インコーポレイテッド | 耐破断性を備える外側表面を有する縫合糸スリーブ |
| US9486622B2 (en) | 2012-11-08 | 2016-11-08 | Cardiac Pacemakers, Inc. | Fixation and strain relief element for temporary therapy delivery device |
| US10182921B2 (en) | 2012-11-09 | 2019-01-22 | DePuy Synthes Products, Inc. | Interbody device with opening to allow packing graft and other biologics |
| KR20150087273A (ko) | 2012-11-15 | 2015-07-29 | 지가 테크놀로지 인코포레이티드 | 패시트 관절 치료를 위한 시스템 및 방법 |
| USD731061S1 (en) | 2012-11-28 | 2015-06-02 | Nuvasive, Inc. | Intervertebral implant |
| US9204977B2 (en) | 2012-12-11 | 2015-12-08 | Biomet Manufacturing, Llc | Patient-specific acetabular guide for anterior approach |
| US9060788B2 (en) | 2012-12-11 | 2015-06-23 | Biomet Manufacturing, Llc | Patient-specific acetabular guide for anterior approach |
| US9687281B2 (en) | 2012-12-20 | 2017-06-27 | Illuminoss Medical, Inc. | Distal tip for bone fixation devices |
| US20140178343A1 (en) | 2012-12-21 | 2014-06-26 | Jian Q. Yao | Supports and methods for promoting integration of cartilage tissue explants |
| US9949837B2 (en) | 2013-03-07 | 2018-04-24 | Howmedica Osteonics Corp. | Partially porous bone implant keel |
| US9839438B2 (en) | 2013-03-11 | 2017-12-12 | Biomet Manufacturing, Llc | Patient-specific glenoid guide with a reusable guide holder |
| US9579107B2 (en) | 2013-03-12 | 2017-02-28 | Biomet Manufacturing, Llc | Multi-point fit for patient specific guide |
| US9826981B2 (en) | 2013-03-13 | 2017-11-28 | Biomet Manufacturing, Llc | Tangential fit of patient-specific guides |
| US9498233B2 (en) | 2013-03-13 | 2016-11-22 | Biomet Manufacturing, Llc. | Universal acetabular guide and associated hardware |
| US9517145B2 (en) | 2013-03-15 | 2016-12-13 | Biomet Manufacturing, Llc | Guide alignment system and method |
| US9492200B2 (en) | 2013-04-16 | 2016-11-15 | Arthrosurface Incorporated | Suture system and method |
| AU2014273284B2 (en) * | 2013-05-27 | 2018-12-13 | Vita Zahnfabrik H. Rauter Gmbh & Co. Kg | Prosthetic preform for producing a dental prosthetic body |
| US20150112349A1 (en) | 2013-10-21 | 2015-04-23 | Biomet Manufacturing, Llc | Ligament Guide Registration |
| US20150250472A1 (en) | 2014-03-07 | 2015-09-10 | Arthrosurface Incorporated | Delivery System for Articular Surface Implant |
| US10624748B2 (en) | 2014-03-07 | 2020-04-21 | Arthrosurface Incorporated | System and method for repairing articular surfaces |
| US11607319B2 (en) | 2014-03-07 | 2023-03-21 | Arthrosurface Incorporated | System and method for repairing articular surfaces |
| US10282488B2 (en) | 2014-04-25 | 2019-05-07 | Biomet Manufacturing, Llc | HTO guide with optional guided ACL/PCL tunnels |
| US9408616B2 (en) | 2014-05-12 | 2016-08-09 | Biomet Manufacturing, Llc | Humeral cut guide |
| US9839436B2 (en) | 2014-06-03 | 2017-12-12 | Biomet Manufacturing, Llc | Patient-specific glenoid depth control |
| US9561040B2 (en) | 2014-06-03 | 2017-02-07 | Biomet Manufacturing, Llc | Patient-specific glenoid depth control |
| US10492926B1 (en) | 2014-09-04 | 2019-12-03 | Shoulder Innovations, Inc. | Alignment guide for humeral or femoral stem replacement prostheses |
| GB201416985D0 (en) * | 2014-09-26 | 2014-11-12 | Ucb Biopharma Sprl And Bespak Europ Ltd | Housing part for an auto-injector |
| US9826994B2 (en) | 2014-09-29 | 2017-11-28 | Biomet Manufacturing, Llc | Adjustable glenoid pin insertion guide |
| US9833245B2 (en) | 2014-09-29 | 2017-12-05 | Biomet Sports Medicine, Llc | Tibial tubercule osteotomy |
| CN104352291A (zh) * | 2014-11-05 | 2015-02-18 | 上海大学 | 表面微织构型人工膝关节半月板 |
| US9820868B2 (en) | 2015-03-30 | 2017-11-21 | Biomet Manufacturing, Llc | Method and apparatus for a pin apparatus |
| CN107530541A (zh) | 2015-05-20 | 2018-01-02 | 心脏起搏器股份公司 | 用于医疗电引线的完全集成的引线稳定器及附接方法 |
| US10226262B2 (en) | 2015-06-25 | 2019-03-12 | Biomet Manufacturing, Llc | Patient-specific humeral guide designs |
| US10568647B2 (en) | 2015-06-25 | 2020-02-25 | Biomet Manufacturing, Llc | Patient-specific humeral guide designs |
| US11077228B2 (en) | 2015-08-10 | 2021-08-03 | Hyalex Orthopaedics, Inc. | Interpenetrating polymer networks |
| WO2017046647A1 (en) | 2015-09-18 | 2017-03-23 | Ortho-Space Ltd. | Intramedullary fixated subacromial spacers |
| MX2018014218A (es) * | 2016-05-26 | 2019-03-28 | Corning Optical Communications LLC | Formulacion de material para cable de fibra optica con cubierta de sobremolde. |
| EP3573806A4 (en) | 2017-01-30 | 2019-12-11 | Ortho-Space Ltd. | MACHINING MACHINE AND METHOD FOR PROCESSING DIVING MADE ARTICLES |
| US10722310B2 (en) | 2017-03-13 | 2020-07-28 | Zimmer Biomet CMF and Thoracic, LLC | Virtual surgery planning system and method |
| KR101880395B1 (ko) * | 2017-04-06 | 2018-07-19 | 성균관대학교산학협력단 | 다기능 생체이식용 구조체 및 이의 제조방법 |
| AU2018251815B2 (en) | 2017-04-14 | 2023-12-14 | Shoulder Innovations, Inc. | Total shoulder prosthesis having inset glenoid implant convertible from anatomic to reverse |
| EP3400912B1 (en) | 2017-05-10 | 2019-11-20 | Howmedica Osteonics Corporation | Patient specific composite knee replacement |
| AU2018203479B2 (en) | 2017-05-18 | 2024-04-18 | Howmedica Osteonics Corp. | High fatigue strength porous structure |
| US10940016B2 (en) | 2017-07-05 | 2021-03-09 | Medos International Sarl | Expandable intervertebral fusion cage |
| US10806529B2 (en) | 2017-07-20 | 2020-10-20 | Mako Surgical Corp. | System and method for robotically assisting a surgical procedure |
| CA3108761A1 (en) | 2017-08-04 | 2019-02-07 | Arthrosurface Incorporated | Multicomponent articular surface implant |
| US12138172B2 (en) | 2018-04-30 | 2024-11-12 | Shoulder Innovations, Inc. | Inset/onlay glenoid, porous coated convertible glenoid, and humeral heads with textured undersides |
| US10736748B2 (en) | 2018-05-02 | 2020-08-11 | Depuy Ireland Unlimited Company | Orthopaedic prosthetic system for a hinged-knee prosthesis |
| WO2020006239A1 (en) | 2018-06-27 | 2020-01-02 | Illuminoss Medical, Inc. | Systems and methods for bone stabilization and fixation |
| US10869950B2 (en) | 2018-07-17 | 2020-12-22 | Hyalex Orthopaedics, Inc. | Ionic polymer compositions |
| US11648058B2 (en) | 2018-09-24 | 2023-05-16 | Simplify Medical Pty Ltd | Robotic system and method for bone preparation for intervertebral disc prosthesis implantation |
| US11160672B2 (en) | 2018-09-24 | 2021-11-02 | Simplify Medical Pty Ltd | Robotic systems and methods for distraction in intervertebral disc prosthesis implantation |
| US11819424B2 (en) | 2018-09-24 | 2023-11-21 | Simplify Medical Pty Ltd | Robot assisted intervertebral disc prosthesis selection and implantation system |
| US11033396B2 (en) | 2019-02-05 | 2021-06-15 | Depuy Ireland Unlimited Company | Orthopaedic prosthetic system for a rotating hinged-knee prosthesis |
| US11116641B2 (en) | 2019-02-05 | 2021-09-14 | Depuy Ireland Unlimited Company | Orthopaedic prosthetic system for a rotating hinged-knee prosthesis |
| US20220151795A1 (en) | 2019-03-11 | 2022-05-19 | Shoulder Innovations, Inc. | Total reverse shoulder systems and methods |
| USD977643S1 (en) | 2019-03-12 | 2023-02-07 | Shoulder Innovations, Inc. | Humeral stem implant |
| WO2020186099A1 (en) | 2019-03-12 | 2020-09-17 | Arthrosurface Incorporated | Humeral and glenoid articular surface implant systems and methods |
| JP2022531871A (ja) | 2019-05-29 | 2022-07-12 | ライト メディカル テクノロジー インコーポレイテッド | 置換足関節の脛骨インプラント部品を受容するための脛骨の準備 |
| CN110934667A (zh) * | 2019-12-20 | 2020-03-31 | 王俊瑞 | 一种软骨保护垫 |
| WO2021146015A1 (en) | 2020-01-17 | 2021-07-22 | Wright Medical Technology, Inc. | Guidance tools, systems, and methods |
| US11642226B2 (en) | 2020-05-01 | 2023-05-09 | Ensemble Orthopedics, Inc. | Implantable interpositional orthopedic pain management |
| US12290443B2 (en) * | 2020-05-01 | 2025-05-06 | Ensemble Orthopedics, Inc. | Implantable interpositional orthopedic pain management |
| EP4208111B1 (en) | 2020-09-04 | 2025-08-27 | DePuy Synthes Products, Inc. | Temporary antimicrobial cement spacer, assembly, kit, and method of manufacture |
| US12440227B2 (en) | 2021-02-24 | 2025-10-14 | Wright Medical Technology, Inc. | Preparing a tibia for receiving tibial implant component of a replacement ankle |
| CN113069245B (zh) * | 2021-03-18 | 2024-08-27 | 重庆熙科医疗科技有限公司 | 一种髌骨假体及其设计与制备方法 |
| CN116159185B (zh) * | 2022-12-26 | 2024-04-09 | 烟台德胜海洋生物科技有限公司 | 复合脱细胞基质材料及其制备方法 |
| WO2024186934A1 (en) * | 2023-03-06 | 2024-09-12 | Ensemble Orthopedics, Inc. | Implantable interpositional orthopedic pain management |
Citations (2)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| WO1991016867A1 (en) * | 1990-05-07 | 1991-11-14 | Regen Corporation | Prosthetic intervertebral disc |
| US5306308A (en) * | 1989-10-23 | 1994-04-26 | Ulrich Gross | Intervertebral implant |
Family Cites Families (153)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US3030951A (en) * | 1959-04-10 | 1962-04-24 | Michael P Mandarino | Methods and materials for orthopedic surgery |
| CA992255A (en) | 1971-01-25 | 1976-07-06 | Cutter Laboratories | Prosthesis for spinal repair |
| US3728742A (en) * | 1971-06-18 | 1973-04-24 | Howmedica | Knee or elbow prosthesis |
| US3848601A (en) | 1972-06-14 | 1974-11-19 | G Ma | Method for interbody fusion of the spine |
| US3815599A (en) * | 1973-03-02 | 1974-06-11 | W Deyerle | Femoral shaft surgical rasp for use in hip prosthesis surgery |
| US4081866A (en) * | 1977-02-02 | 1978-04-04 | Howmedica, Inc. | Total anatomical knee prosthesis |
| US4203444A (en) * | 1977-11-07 | 1980-05-20 | Dyonics, Inc. | Surgical instrument suitable for closed surgery such as of the knee |
| CA1146301A (en) | 1980-06-13 | 1983-05-17 | J. David Kuntz | Intervertebral disc prosthesis |
| US4502161A (en) | 1981-09-21 | 1985-03-05 | Wall W H | Prosthetic meniscus for the repair of joints |
| US4463141A (en) * | 1981-11-30 | 1984-07-31 | E. I. Du Pont De Nemours And Company | Polyether carbonate diols and polyurethanes prepared therefrom |
| US4476293A (en) | 1981-11-30 | 1984-10-09 | E. I. Du Pont De Nemours And Company | Polymeric carbonate diols of copolyether glycols and polyurethanes prepared therefrom |
| US4456745A (en) * | 1982-05-24 | 1984-06-26 | Ethyl Corporation | Polyurethanes prepared from polycarbonates |
| US4477604A (en) * | 1982-09-20 | 1984-10-16 | Oechsle Iii Sixtus J | Polyurethane compositions and their use as luting agents |
| DE3318730A1 (de) * | 1983-05-21 | 1984-11-22 | Akzo Gmbh, 5600 Wuppertal | Biokompatible polyurethane |
| US4722948A (en) * | 1984-03-16 | 1988-02-02 | Dynatech Corporation | Bone replacement and repair putty material from unsaturated polyester resin and vinyl pyrrolidone |
| DE3433264C2 (de) | 1984-09-11 | 1986-10-02 | S + G Implants GmbH, 2400 Lübeck | Tibiateil für eine Kniegelenk-Endoprothese |
| US4743256A (en) | 1985-10-04 | 1988-05-10 | Brantigan John W | Surgical prosthetic implant facilitating vertebral interbody fusion and method |
| US4647643A (en) * | 1985-11-08 | 1987-03-03 | Becton, Dickinson And Company | Soft non-blocking polyurethanes |
| US4651736A (en) * | 1986-02-01 | 1987-03-24 | Bruce Sanders | Methods for temporomandibular joint small incision surgery |
| US4834757A (en) | 1987-01-22 | 1989-05-30 | Brantigan John W | Prosthetic implant |
| US4743632A (en) * | 1987-02-25 | 1988-05-10 | Pfizer Hospital Products Group, Inc. | Polyetherurethane urea polymers as space filling tissue adhesives |
| DE3717060A1 (de) * | 1987-05-21 | 1988-12-01 | Bayer Ag | Polyether-polycarbonat-diole, ihre herstellung und verwendung als ausgangsprodukte fuer polyurethankunststoffe |
| US5306311A (en) * | 1987-07-20 | 1994-04-26 | Regen Corporation | Prosthetic articular cartilage |
| US4772287A (en) | 1987-08-20 | 1988-09-20 | Cedar Surgical, Inc. | Prosthetic disc and method of implanting |
| US4880610A (en) * | 1988-04-20 | 1989-11-14 | Norian Corporation | In situ calcium phosphate minerals--method and composition |
| US4911718A (en) | 1988-06-10 | 1990-03-27 | University Of Medicine & Dentistry Of N.J. | Functional and biocompatible intervertebral disc spacer |
| US5484437A (en) | 1988-06-13 | 1996-01-16 | Michelson; Gary K. | Apparatus and method of inserting spinal implants |
| US5772661A (en) | 1988-06-13 | 1998-06-30 | Michelson; Gary Karlin | Methods and instrumentation for the surgical correction of human thoracic and lumbar spinal disease from the antero-lateral aspect of the spine |
| CA1333209C (en) | 1988-06-28 | 1994-11-29 | Gary Karlin Michelson | Artificial spinal fusion implants |
| US5609635A (en) | 1988-06-28 | 1997-03-11 | Michelson; Gary K. | Lordotic interbody spinal fusion implants |
| US5545229A (en) | 1988-08-18 | 1996-08-13 | University Of Medicine And Dentistry Of Nj | Functional and biocompatible intervertebral disc spacer containing elastomeric material of varying hardness |
| US4873308A (en) * | 1988-09-30 | 1989-10-10 | Medtronic, Inc. | Biostable, segmented aliphatic polyurethanes and process therefor |
| US4938763B1 (en) * | 1988-10-03 | 1995-07-04 | Atrix Lab Inc | Biodegradable in-situ forming implants and method of producing the same |
| FR2639823A1 (fr) | 1988-12-06 | 1990-06-08 | Garcia Alain | Remplacement du nucleus du disque intervertebral par un polyurethane polymerise in situ |
| US4872452A (en) | 1989-01-09 | 1989-10-10 | Minnesota Mining And Manufacturing Company | Bone rasp |
| US4969888A (en) * | 1989-02-09 | 1990-11-13 | Arie Scholten | Surgical protocol for fixation of osteoporotic bone using inflatable device |
| US5007940A (en) * | 1989-06-09 | 1991-04-16 | American Medical Systems, Inc. | Injectable polymeric bodies |
| US5263987A (en) * | 1989-08-25 | 1993-11-23 | Shah Mrugesh K | Method and apparatus for arthroscopically replacing a bone joint |
| US5082803A (en) * | 1989-09-21 | 1992-01-21 | Asahi Kogaku Kogyo Kabushiki Kaisha | Process for producing bone prosthesis |
| US5067964A (en) * | 1989-12-13 | 1991-11-26 | Stryker Corporation | Articular surface repair |
| US5254662A (en) * | 1990-09-12 | 1993-10-19 | Polymedia Industries, Inc. | Biostable polyurethane products |
| US5192326A (en) | 1990-12-21 | 1993-03-09 | Pfizer Hospital Products Group, Inc. | Hydrogel bead intervertebral disc nucleus |
| US5047055A (en) | 1990-12-21 | 1991-09-10 | Pfizer Hospital Products Group, Inc. | Hydrogel intervertebral disc nucleus |
| US5192327A (en) | 1991-03-22 | 1993-03-09 | Brantigan John W | Surgical prosthetic implant for vertebrae |
| JP3007903B2 (ja) * | 1991-03-29 | 2000-02-14 | 京セラ株式会社 | 人工椎間板 |
| NL9101159A (nl) | 1991-07-03 | 1993-02-01 | Industrial Res Bv | Vormvast te maken uitzetbare ring, cylinder of huls. |
| US5329846A (en) | 1991-08-12 | 1994-07-19 | Bonutti Peter M | Tissue press and system |
| US5143942A (en) * | 1991-10-28 | 1992-09-01 | Ethyl Corporation | Polyurethanes |
| US5166115A (en) * | 1991-10-28 | 1992-11-24 | Brown William R | Polyurethanes |
| US5344459A (en) | 1991-12-03 | 1994-09-06 | Swartz Stephen J | Arthroscopically implantable prosthesis |
| US5509934A (en) * | 1992-02-28 | 1996-04-23 | Osteonics Corp. | Prosthetic knee tibial component constructed of synthetic polymeric material |
| JPH05298662A (ja) * | 1992-04-14 | 1993-11-12 | Fuji Photo Film Co Ltd | 磁気記録媒体用結合剤および磁気記録媒体 |
| US5344458A (en) * | 1992-08-06 | 1994-09-06 | Bonutti Peter M | Arthroplasty component |
| EP0621020A1 (de) | 1993-04-21 | 1994-10-26 | SULZER Medizinaltechnik AG | Zwischenwirbelprothese und Verfahren zum Implantieren einer derartigen Prothese |
| FR2709949B1 (fr) | 1993-09-14 | 1995-10-13 | Commissariat Energie Atomique | Prothèse de disque intervertébral. |
| US5397364A (en) | 1993-10-12 | 1995-03-14 | Danek Medical, Inc. | Anterior interbody fusion device |
| DE4339895C1 (de) * | 1993-11-23 | 1995-03-23 | Plus Endoprothetik Ag | System für die Ausbildung einer Kniegelenk-Endoprothese |
| US6140452A (en) * | 1994-05-06 | 2000-10-31 | Advanced Bio Surfaces, Inc. | Biomaterial for in situ tissue repair |
| US6248131B1 (en) * | 1994-05-06 | 2001-06-19 | Advanced Bio Surfaces, Inc. | Articulating joint repair |
| US5888220A (en) * | 1994-05-06 | 1999-03-30 | Advanced Bio Surfaces, Inc. | Articulating joint repair |
| US5556429A (en) * | 1994-05-06 | 1996-09-17 | Advanced Bio Surfaces, Inc. | Joint resurfacing system |
| US5571189A (en) | 1994-05-20 | 1996-11-05 | Kuslich; Stephen D. | Expandable fabric implant for stabilizing the spinal motion segment |
| US6187048B1 (en) | 1994-05-24 | 2001-02-13 | Surgical Dynamics, Inc. | Intervertebral disc implant |
| US5562736A (en) | 1994-10-17 | 1996-10-08 | Raymedica, Inc. | Method for surgical implantation of a prosthetic spinal disc nucleus |
| US5824093A (en) | 1994-10-17 | 1998-10-20 | Raymedica, Inc. | Prosthetic spinal disc nucleus |
| US5860973A (en) | 1995-02-27 | 1999-01-19 | Michelson; Gary Karlin | Translateral spinal implant |
| US5989289A (en) | 1995-10-16 | 1999-11-23 | Sdgi Holdings, Inc. | Bone grafts |
| ATE200409T1 (de) | 1995-10-20 | 2001-04-15 | Synthes Ag | Zwischenwirbel-implantat mit käfig und rotationskörper |
| ATE203886T1 (de) | 1995-10-20 | 2001-08-15 | Synthes Ag | Zwischenwirbel-implantat |
| US5725531A (en) * | 1995-12-27 | 1998-03-10 | Shapiro; Jules S. | Reaming device |
| EP0826347B1 (de) | 1996-08-24 | 2002-12-11 | CERASIV GmbH INNOVATIVES KERAMIK-ENGINEERING | Gelenkprothese |
| DE29615920U1 (de) * | 1996-09-12 | 1998-01-15 | Waldemar Link GmbH & Co, 22339 Hamburg | Gelenkendoprothese |
| CA2269342C (en) | 1996-10-23 | 2006-09-12 | Sdgi Holdings, Inc. | Spinal spacer |
| EP0873145A2 (en) | 1996-11-15 | 1998-10-28 | Advanced Bio Surfaces, Inc. | Biomaterial system for in situ tissue repair |
| US6033438A (en) | 1997-06-03 | 2000-03-07 | Sdgi Holdings, Inc. | Open intervertebral spacer |
| US5855167A (en) * | 1997-07-21 | 1999-01-05 | Hay & Forage Industries | End of round bale twine guide |
| US6511509B1 (en) | 1997-10-20 | 2003-01-28 | Lifenet | Textured bone allograft, method of making and using same |
| US6079868A (en) * | 1997-12-18 | 2000-06-27 | Advanced Bio Surfaces, Inc. | Static mixer |
| US6258125B1 (en) | 1998-08-03 | 2001-07-10 | Synthes (U.S.A.) | Intervertebral allograft spacer |
| US6143033A (en) | 1998-01-30 | 2000-11-07 | Synthes (Usa) | Allogenic intervertebral implant |
| US6224631B1 (en) | 1998-03-20 | 2001-05-01 | Sulzer Spine-Tech Inc. | Intervertebral implant with reduced contact area and method |
| US6241769B1 (en) | 1998-05-06 | 2001-06-05 | Cortek, Inc. | Implant for spinal fusion |
| DE19823325C1 (de) * | 1998-05-26 | 2000-03-23 | Werner Scholz | Kniegelenk-Endoprothesensystem |
| US6251140B1 (en) | 1998-05-27 | 2001-06-26 | Nuvasive, Inc. | Interlocking spinal inserts |
| US6224630B1 (en) | 1998-05-29 | 2001-05-01 | Advanced Bio Surfaces, Inc. | Implantable tissue repair device |
| US6270528B1 (en) | 1998-08-06 | 2001-08-07 | Sdgi Holdings, Inc. | Composited intervertebral bone spacers |
| US6159211A (en) | 1998-10-22 | 2000-12-12 | Depuy Acromed, Inc. | Stackable cage system for corpectomy/vertebrectomy |
| US6174311B1 (en) | 1998-10-28 | 2001-01-16 | Sdgi Holdings, Inc. | Interbody fusion grafts and instrumentation |
| US6183517B1 (en) | 1998-12-16 | 2001-02-06 | Loubert Suddaby | Expandable intervertebral fusion implant and applicator |
| US6206923B1 (en) | 1999-01-08 | 2001-03-27 | Sdgi Holdings, Inc. | Flexible implant using partially demineralized bone |
| US6146422A (en) | 1999-01-25 | 2000-11-14 | Lawson; Kevin Jon | Prosthetic nucleus replacement for surgical reconstruction of intervertebral discs and treatment method |
| US6245108B1 (en) | 1999-02-25 | 2001-06-12 | Spineco | Spinal fusion implant |
| US6113638A (en) | 1999-02-26 | 2000-09-05 | Williams; Lytton A. | Method and apparatus for intervertebral implant anchorage |
| ES2257044T3 (es) * | 1999-04-02 | 2006-07-16 | Barry M. Fell | Protesis de rodilla implantable quirurgicamente. |
| US6206927B1 (en) * | 1999-04-02 | 2001-03-27 | Barry M. Fell | Surgically implantable knee prothesis |
| US6558421B1 (en) * | 2000-09-19 | 2003-05-06 | Barry M. Fell | Surgically implantable knee prosthesis |
| US7341602B2 (en) * | 1999-05-10 | 2008-03-11 | Fell Barry M | Proportioned surgically implantable knee prosthesis |
| US6048345A (en) * | 1999-04-08 | 2000-04-11 | Joseph J. Berke | Motorized reciprocating surgical file apparatus and method |
| US6110210A (en) | 1999-04-08 | 2000-08-29 | Raymedica, Inc. | Prosthetic spinal disc nucleus having selectively coupled bodies |
| AU4348400A (en) | 1999-04-16 | 2000-11-02 | Nuvasive, Inc. | Systems for securing facet joints together |
| AU4810800A (en) | 1999-04-26 | 2000-11-10 | Li Medical Technologies, Inc. | Prosthetic apparatus and method |
| US7491235B2 (en) | 1999-05-10 | 2009-02-17 | Fell Barry M | Surgically implantable knee prosthesis |
| US6866684B2 (en) * | 1999-05-10 | 2005-03-15 | Barry M. Fell | Surgically implantable knee prosthesis having different tibial and femoral surface profiles |
| US6923831B2 (en) * | 1999-05-10 | 2005-08-02 | Barry M. Fell | Surgically implantable knee prosthesis having attachment apertures |
| US20050033424A1 (en) | 1999-05-10 | 2005-02-10 | Fell Barry M. | Surgically implantable knee prosthesis |
| US6893463B2 (en) * | 1999-05-10 | 2005-05-17 | Barry M. Fell | Surgically implantable knee prosthesis having two-piece keyed components |
| US6911044B2 (en) * | 1999-05-10 | 2005-06-28 | Barry M. Fell | Surgically implantable knee prosthesis having medially shifted tibial surface |
| US6855165B2 (en) * | 1999-05-10 | 2005-02-15 | Barry M. Fell | Surgically implantable knee prosthesis having enlarged femoral surface |
| US7297161B2 (en) | 1999-05-10 | 2007-11-20 | Fell Barry M | Surgically implantable knee prosthesis |
| US6966928B2 (en) * | 1999-05-10 | 2005-11-22 | Fell Barry M | Surgically implantable knee prosthesis having keels |
| US6371990B1 (en) | 1999-10-08 | 2002-04-16 | Bret A. Ferree | Annulus fibrosis augmentation methods and apparatus |
| US6419704B1 (en) | 1999-10-08 | 2002-07-16 | Bret Ferree | Artificial intervertebral disc replacement methods and apparatus |
| AU5701200A (en) | 1999-07-02 | 2001-01-22 | Petrus Besselink | Reinforced expandable cage |
| US6368324B1 (en) * | 1999-09-24 | 2002-04-09 | Medtronic Xomed, Inc. | Powered surgical handpiece assemblies and handpiece adapter assemblies |
| US6264695B1 (en) | 1999-09-30 | 2001-07-24 | Replication Medical, Inc. | Spinal nucleus implant |
| US6342075B1 (en) * | 2000-02-18 | 2002-01-29 | Macarthur A. Creig | Prosthesis and methods for total knee arthroplasty |
| US6740093B2 (en) | 2000-02-28 | 2004-05-25 | Stephen Hochschuler | Method and apparatus for treating a vertebral body |
| EP1263331B1 (en) | 2000-03-10 | 2015-09-16 | Smith & Nephew, Inc. | Apparatus for use in arthroplasty on a knee joint |
| US6482234B1 (en) | 2000-04-26 | 2002-11-19 | Pearl Technology Holdings, Llc | Prosthetic spinal disc |
| JP2004521666A (ja) | 2000-08-28 | 2004-07-22 | アドバンスト バイオ サーフェイシズ,インコーポレイティド | 哺乳動物の関節を増強する方法およびシステム |
| US20020026244A1 (en) | 2000-08-30 | 2002-02-28 | Trieu Hai H. | Intervertebral disc nucleus implants and methods |
| US20050154463A1 (en) | 2000-08-30 | 2005-07-14 | Trieu Hal H. | Spinal nucleus replacement implants and methods |
| US6620196B1 (en) | 2000-08-30 | 2003-09-16 | Sdgi Holdings, Inc. | Intervertebral disc nucleus implants and methods |
| US6468311B2 (en) | 2001-01-22 | 2002-10-22 | Sdgi Holdings, Inc. | Modular interbody fusion implant |
| US6595998B2 (en) | 2001-03-08 | 2003-07-22 | Spinewave, Inc. | Tissue distraction device |
| DE10152567A1 (de) | 2001-10-24 | 2003-05-08 | Tutogen Medical Gmbh | Implantat |
| US6855167B2 (en) | 2001-12-05 | 2005-02-15 | Osteotech, Inc. | Spinal intervertebral implant, interconnections for such implant and processes for making |
| US20030171812A1 (en) | 2001-12-31 | 2003-09-11 | Ilan Grunberg | Minimally invasive modular support implant device and method |
| US6726720B2 (en) | 2002-03-27 | 2004-04-27 | Depuy Spine, Inc. | Modular disc prosthesis |
| US20060106462A1 (en) | 2002-04-16 | 2006-05-18 | Tsou Paul M | Implant material for minimally invasive spinal interbody fusion surgery |
| US7291171B2 (en) | 2002-05-10 | 2007-11-06 | Ferree Bret A | Artificial disc replacement (ADR) using elastic tether member |
| US20040010318A1 (en) | 2002-05-15 | 2004-01-15 | Ferree Bret A. | Conformable endplates for artificial disc replacement (ADR) devices and other applications |
| US6817284B2 (en) | 2002-06-14 | 2004-11-16 | Lyco Manufacturing, Inc. | Food processing apparatus, transport mechanism, bucket and method |
| US20040006393A1 (en) * | 2002-07-03 | 2004-01-08 | Brian Burkinshaw | Implantable prosthetic knee for lateral compartment |
| US20040054413A1 (en) | 2002-09-16 | 2004-03-18 | Howmedica Osteonics Corp. | Radiovisible hydrogel intervertebral disc nucleus |
| US7824444B2 (en) | 2003-03-20 | 2010-11-02 | Spineco, Inc. | Expandable spherical spinal implant |
| WO2004098466A2 (en) | 2003-05-02 | 2004-11-18 | Smart Disc, Inc. | Artificial spinal disk |
| US20040220672A1 (en) | 2003-05-03 | 2004-11-04 | Shadduck John H. | Orthopedic implants, methods of use and methods of fabrication |
| WO2004103152A2 (en) | 2003-05-16 | 2004-12-02 | Spine Wave, Inc. | Tissue distraction device |
| US7008452B2 (en) | 2003-06-26 | 2006-03-07 | Depuy Acromed, Inc. | Dual durometer elastomer artificial disc |
| US20050015150A1 (en) | 2003-07-17 | 2005-01-20 | Lee Casey K. | Intervertebral disk and nucleus prosthesis |
| US7901459B2 (en) | 2004-01-09 | 2011-03-08 | Warsaw Orthopedic, Inc. | Split spinal device and method |
| US7250060B2 (en) | 2004-01-27 | 2007-07-31 | Sdgi Holdings, Inc. | Hybrid intervertebral disc system |
| EP1729678A4 (en) | 2004-02-06 | 2011-08-10 | Georgia Tech Res Inst | BEARING BIOCOMPATIBLE DEVICE |
| WO2006034436A2 (en) | 2004-09-21 | 2006-03-30 | Stout Medical Group, L.P. | Expandable support device and method of use |
| US8048083B2 (en) | 2004-11-05 | 2011-11-01 | Dfine, Inc. | Bone treatment systems and methods |
| CN101098667A (zh) | 2004-11-15 | 2008-01-02 | 光碟-O-特克医学科技有限公司 | 例如盘状物的组装假体 |
| US20060142858A1 (en) | 2004-12-16 | 2006-06-29 | Dennis Colleran | Expandable implants for spinal disc replacement |
| JP2008526459A (ja) | 2005-01-19 | 2008-07-24 | ネクスジェン スパイン、インク. | エラストマー椎間板プロテーゼ |
| US20060247778A1 (en) | 2005-01-26 | 2006-11-02 | Ferree Bret A | Intradiscal devices including spacers facilitating posterior-lateral and other insertion approaches |
| WO2006091838A2 (en) | 2005-02-24 | 2006-08-31 | Morphogeny, Llc | Linked slideable and interlockable rotatable components |
| US7267690B2 (en) | 2005-03-09 | 2007-09-11 | Vertebral Technologies, Inc. | Interlocked modular disc nucleus prosthesis |
| US9737414B2 (en) | 2006-11-21 | 2017-08-22 | Vertebral Technologies, Inc. | Methods and apparatus for minimally invasive modular interbody fusion devices |
-
2001
- 2001-08-28 JP JP2002522799A patent/JP2004521666A/ja active Pending
- 2001-08-28 DE DE60139262T patent/DE60139262D1/de not_active Expired - Lifetime
- 2001-08-28 CA CA002420898A patent/CA2420898A1/en not_active Abandoned
- 2001-08-28 EP EP01964653A patent/EP1315470B1/en not_active Expired - Lifetime
- 2001-08-28 AU AU2001285488A patent/AU2001285488A1/en not_active Abandoned
- 2001-08-28 WO PCT/US2001/041908 patent/WO2002017821A2/en not_active Ceased
-
2002
- 2002-03-15 US US10/098,601 patent/US20020127264A1/en not_active Abandoned
- 2002-04-12 US US10/121,455 patent/US20020183850A1/en not_active Abandoned
- 2002-06-12 US US10/167,963 patent/US6652587B2/en not_active Expired - Lifetime
-
2003
- 2003-11-24 US US10/722,019 patent/US7320709B2/en not_active Expired - Lifetime
-
2007
- 2007-12-10 US US11/953,203 patent/US7914582B2/en not_active Expired - Fee Related
-
2009
- 2009-06-05 US US12/479,402 patent/US8100979B2/en not_active Expired - Fee Related
Patent Citations (2)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US5306308A (en) * | 1989-10-23 | 1994-04-26 | Ulrich Gross | Intervertebral implant |
| WO1991016867A1 (en) * | 1990-05-07 | 1991-11-14 | Regen Corporation | Prosthetic intervertebral disc |
Also Published As
| Publication number | Publication date |
|---|---|
| US20040107000A1 (en) | 2004-06-03 |
| EP1315470A2 (en) | 2003-06-04 |
| WO2002017821A2 (en) | 2002-03-07 |
| AU2001285488A1 (en) | 2002-03-13 |
| US7914582B2 (en) | 2011-03-29 |
| US20020183850A1 (en) | 2002-12-05 |
| US20020173852A1 (en) | 2002-11-21 |
| US8100979B2 (en) | 2012-01-24 |
| US7320709B2 (en) | 2008-01-22 |
| US6652587B2 (en) | 2003-11-25 |
| US20080234820A1 (en) | 2008-09-25 |
| WO2002017821A3 (en) | 2002-11-21 |
| DE60139262D1 (de) | 2009-08-27 |
| JP2004521666A (ja) | 2004-07-22 |
| WO2002017821A9 (en) | 2003-02-13 |
| US20100145457A1 (en) | 2010-06-10 |
| US20020127264A1 (en) | 2002-09-12 |
| CA2420898A1 (en) | 2002-03-07 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| EP1315470B1 (en) | System for mammalian joint resurfacing | |
| EP1474071B1 (en) | Interpositional arthroplasty system | |
| US6306177B1 (en) | Biomaterial system for in situ tissue repair | |
| US6140452A (en) | Biomaterial for in situ tissue repair | |
| US20050043808A1 (en) | Knee joint prosthesis | |
| US20070067032A1 (en) | Meniscus preserving implant method and apparatus | |
| US20060282169A1 (en) | System and method for upper extremity joint arthroplasty | |
| US20110029084A1 (en) | Foam prosthesis for spinal disc | |
| WO2009117737A2 (en) | Methods, devices and compositions for adhering hydrated polymer implants to bone | |
| WO2006096889A2 (en) | Materials, devices, and methods for in-situ formation of composite intervertebral implants | |
| WO2005025451A2 (en) | Method and materials for interpositional arthroplasty implant | |
| AU2003205319A1 (en) | Interpositional arthroplasty system and method | |
| MXPA04007061A (en) | Interpositional arthroplasty system and method | |
| CA2243154A1 (en) | Biomaterial system for in situ tissue repair |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| PUAI | Public reference made under article 153(3) epc to a published international application that has entered the european phase |
Free format text: ORIGINAL CODE: 0009012 |
|
| 17P | Request for examination filed |
Effective date: 20030326 |
|
| AK | Designated contracting states |
Designated state(s): AT BE CH CY DE DK ES FI FR GB GR IE IT LI LU MC NL PT SE TR |
|
| AX | Request for extension of the european patent |
Extension state: AL LT LV MK RO SI |
|
| 17Q | First examination report despatched |
Effective date: 20040319 |
|
| RAP1 | Party data changed (applicant data changed or rights of an application transferred) |
Owner name: DISC DYNAMICS, INC. |
|
| R17C | First examination report despatched (corrected) |
Effective date: 20040319 |
|
| GRAP | Despatch of communication of intention to grant a patent |
Free format text: ORIGINAL CODE: EPIDOSNIGR1 |
|
| RTI1 | Title (correction) |
Free format text: SYSTEM FOR MAMMALIAN JOINT RESURFACING |
|
| GRAS | Grant fee paid |
Free format text: ORIGINAL CODE: EPIDOSNIGR3 |
|
| GRAA | (expected) grant |
Free format text: ORIGINAL CODE: 0009210 |
|
| AK | Designated contracting states |
Kind code of ref document: B1 Designated state(s): AT BE CH CY DE DK ES FI FR GB GR IE IT LI LU MC NL PT SE TR |
|
| REG | Reference to a national code |
Ref country code: CH Ref legal event code: EP Ref country code: GB Ref legal event code: FG4D |
|
| REG | Reference to a national code |
Ref country code: IE Ref legal event code: FG4D |
|
| REF | Corresponds to: |
Ref document number: 60139262 Country of ref document: DE Date of ref document: 20090827 Kind code of ref document: P |
|
| NLV1 | Nl: lapsed or annulled due to failure to fulfill the requirements of art. 29p and 29m of the patents act | ||
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: AT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20090715 Ref country code: SE Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20090715 Ref country code: ES Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20091026 Ref country code: FI Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20090715 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: NL Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20090715 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: PT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20091115 Ref country code: MC Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20090831 |
|
| REG | Reference to a national code |
Ref country code: CH Ref legal event code: PL |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: LI Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20090831 Ref country code: CH Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20090831 Ref country code: DK Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20090715 |
|
| PLBE | No opposition filed within time limit |
Free format text: ORIGINAL CODE: 0009261 |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: NO OPPOSITION FILED WITHIN TIME LIMIT |
|
| 26N | No opposition filed |
Effective date: 20100416 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: IE Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20090828 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: GR Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20091016 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: IT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20090715 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: LU Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20090828 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: TR Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20090715 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: CY Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20090715 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: FR Payment date: 20110811 Year of fee payment: 11 Ref country code: GB Payment date: 20110722 Year of fee payment: 11 Ref country code: DE Payment date: 20110831 Year of fee payment: 11 |
|
| PGFP | Annual fee paid to national office [announced via postgrant information from national office to epo] |
Ref country code: BE Payment date: 20110916 Year of fee payment: 11 |
|
| BERE | Be: lapsed |
Owner name: DISC DYNAMICS, INC. Effective date: 20120831 |
|
| GBPC | Gb: european patent ceased through non-payment of renewal fee |
Effective date: 20120828 |
|
| REG | Reference to a national code |
Ref country code: FR Ref legal event code: ST Effective date: 20130430 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: BE Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20120831 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: DE Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20130301 Ref country code: GB Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20120828 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: FR Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20120831 |
|
| REG | Reference to a national code |
Ref country code: DE Ref legal event code: R119 Ref document number: 60139262 Country of ref document: DE Effective date: 20130301 |