EP3218401B1 - Predicting response to a vegf antagonist - Google Patents
Predicting response to a vegf antagonist Download PDFInfo
- Publication number
- EP3218401B1 EP3218401B1 EP15802244.2A EP15802244A EP3218401B1 EP 3218401 B1 EP3218401 B1 EP 3218401B1 EP 15802244 A EP15802244 A EP 15802244A EP 3218401 B1 EP3218401 B1 EP 3218401B1
- Authority
- EP
- European Patent Office
- Prior art keywords
- cancer
- patient
- vegf
- antibody
- tumor
- Prior art date
- Legal status (The legal status is an assumption and is not a legal conclusion. Google has not performed a legal analysis and makes no representation as to the accuracy of the status listed.)
- Active
Links
Images
Classifications
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K16/00—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies
- C07K16/18—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans
- C07K16/22—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans against growth factors ; against growth regulators
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K45/00—Medicinal preparations containing active ingredients not provided for in groups A61K31/00 - A61K41/00
- A61K45/06—Mixtures of active ingredients without chemical characterisation, e.g. antiphlogistics and cardiaca
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K39/395—Antibodies; Immunoglobulins; Immune serum, e.g. antilymphocytic serum
- A61K39/39533—Antibodies; Immunoglobulins; Immune serum, e.g. antilymphocytic serum against materials from animals
- A61K39/39558—Antibodies; Immunoglobulins; Immune serum, e.g. antilymphocytic serum against materials from animals against tumor tissues, cells, antigens
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/33—Heterocyclic compounds
- A61K31/335—Heterocyclic compounds having oxygen as the only ring hetero atom, e.g. fungichromin
- A61K31/337—Heterocyclic compounds having oxygen as the only ring hetero atom, e.g. fungichromin having four-membered rings, e.g. taxol
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/33—Heterocyclic compounds
- A61K31/395—Heterocyclic compounds having nitrogen as a ring hetero atom, e.g. guanethidine or rifamycins
- A61K31/41—Heterocyclic compounds having nitrogen as a ring hetero atom, e.g. guanethidine or rifamycins having five-membered rings with two or more ring hetero atoms, at least one of which being nitrogen, e.g. tetrazole
- A61K31/4164—1,3-Diazoles
- A61K31/4188—1,3-Diazoles condensed with other heterocyclic ring systems, e.g. biotin, sorbinil
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/33—Heterocyclic compounds
- A61K31/395—Heterocyclic compounds having nitrogen as a ring hetero atom, e.g. guanethidine or rifamycins
- A61K31/435—Heterocyclic compounds having nitrogen as a ring hetero atom, e.g. guanethidine or rifamycins having six-membered rings with one nitrogen as the only ring hetero atom
- A61K31/47—Quinolines; Isoquinolines
- A61K31/4738—Quinolines; Isoquinolines ortho- or peri-condensed with heterocyclic ring systems
- A61K31/4745—Quinolines; Isoquinolines ortho- or peri-condensed with heterocyclic ring systems condensed with ring systems having nitrogen as a ring hetero atom, e.g. phenantrolines
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/33—Heterocyclic compounds
- A61K31/395—Heterocyclic compounds having nitrogen as a ring hetero atom, e.g. guanethidine or rifamycins
- A61K31/495—Heterocyclic compounds having nitrogen as a ring hetero atom, e.g. guanethidine or rifamycins having six-membered rings with two or more nitrogen atoms as the only ring heteroatoms, e.g. piperazine or tetrazines
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/33—Heterocyclic compounds
- A61K31/395—Heterocyclic compounds having nitrogen as a ring hetero atom, e.g. guanethidine or rifamycins
- A61K31/495—Heterocyclic compounds having nitrogen as a ring hetero atom, e.g. guanethidine or rifamycins having six-membered rings with two or more nitrogen atoms as the only ring heteroatoms, e.g. piperazine or tetrazines
- A61K31/505—Pyrimidines; Hydrogenated pyrimidines, e.g. trimethoprim
- A61K31/513—Pyrimidines; Hydrogenated pyrimidines, e.g. trimethoprim having oxo groups directly attached to the heterocyclic ring, e.g. cytosine
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/33—Heterocyclic compounds
- A61K31/395—Heterocyclic compounds having nitrogen as a ring hetero atom, e.g. guanethidine or rifamycins
- A61K31/495—Heterocyclic compounds having nitrogen as a ring hetero atom, e.g. guanethidine or rifamycins having six-membered rings with two or more nitrogen atoms as the only ring heteroatoms, e.g. piperazine or tetrazines
- A61K31/505—Pyrimidines; Hydrogenated pyrimidines, e.g. trimethoprim
- A61K31/519—Pyrimidines; Hydrogenated pyrimidines, e.g. trimethoprim ortho- or peri-condensed with heterocyclic rings
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/33—Heterocyclic compounds
- A61K31/555—Heterocyclic compounds containing heavy metals, e.g. hemin, hematin, melarsoprol
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/70—Carbohydrates; Sugars; Derivatives thereof
- A61K31/7028—Compounds having saccharide radicals attached to non-saccharide compounds by glycosidic linkages
- A61K31/7034—Compounds having saccharide radicals attached to non-saccharide compounds by glycosidic linkages attached to a carbocyclic compound, e.g. phloridzin
- A61K31/704—Compounds having saccharide radicals attached to non-saccharide compounds by glycosidic linkages attached to a carbocyclic compound, e.g. phloridzin attached to a condensed carbocyclic ring system, e.g. sennosides, thiocolchicosides, escin, daunorubicin
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/70—Carbohydrates; Sugars; Derivatives thereof
- A61K31/7042—Compounds having saccharide radicals and heterocyclic rings
- A61K31/7052—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides
- A61K31/706—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides containing six-membered rings with nitrogen as a ring hetero atom
- A61K31/7064—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides containing six-membered rings with nitrogen as a ring hetero atom containing condensed or non-condensed pyrimidines
- A61K31/7068—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides containing six-membered rings with nitrogen as a ring hetero atom containing condensed or non-condensed pyrimidines having oxo groups directly attached to the pyrimidine ring, e.g. cytidine, cytidylic acid
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K33/00—Medicinal preparations containing inorganic active ingredients
- A61K33/24—Heavy metals; Compounds thereof
- A61K33/243—Platinum; Compounds thereof
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
- A61K38/16—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof
- A61K38/17—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof from animals; from humans
- A61K38/19—Cytokines; Lymphokines; Interferons
- A61K38/21—Interferons [IFN]
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
- A61K38/16—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof
- A61K38/17—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof from animals; from humans
- A61K38/19—Cytokines; Lymphokines; Interferons
- A61K38/21—Interferons [IFN]
- A61K38/212—IFN-alpha
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P1/00—Drugs for disorders of the alimentary tract or the digestive system
- A61P1/04—Drugs for disorders of the alimentary tract or the digestive system for ulcers, gastritis or reflux esophagitis, e.g. antacids, inhibitors of acid secretion, mucosal protectants
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P11/00—Drugs for disorders of the respiratory system
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P13/00—Drugs for disorders of the urinary system
- A61P13/12—Drugs for disorders of the urinary system of the kidneys
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P15/00—Drugs for genital or sexual disorders; Contraceptives
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P25/00—Drugs for disorders of the nervous system
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P35/00—Antineoplastic agents
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P43/00—Drugs for specific purposes, not provided for in groups A61P1/00-A61P41/00
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K16/00—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies
- C07K16/18—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans
- C07K16/28—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans against receptors, cell surface antigens or cell surface determinants
- C07K16/30—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from animals or humans against receptors, cell surface antigens or cell surface determinants from tumour cells
- C07K16/3069—Reproductive system, e.g. ovaria, uterus, testes, prostate
-
- G—PHYSICS
- G01—MEASURING; TESTING
- G01N—INVESTIGATING OR ANALYSING MATERIALS BY DETERMINING THEIR CHEMICAL OR PHYSICAL PROPERTIES
- G01N33/00—Investigating or analysing materials by specific methods not covered by groups G01N1/00 - G01N31/00
- G01N33/48—Biological material, e.g. blood, urine; Haemocytometers
- G01N33/50—Chemical analysis of biological material, e.g. blood, urine; Testing involving biospecific ligand binding methods; Immunological testing
- G01N33/53—Immunoassay; Biospecific binding assay; Materials therefor
- G01N33/574—Immunoassay; Biospecific binding assay; Materials therefor for cancer
- G01N33/57407—Specifically defined cancers
- G01N33/57449—Specifically defined cancers of ovaries
-
- G—PHYSICS
- G01—MEASURING; TESTING
- G01N—INVESTIGATING OR ANALYSING MATERIALS BY DETERMINING THEIR CHEMICAL OR PHYSICAL PROPERTIES
- G01N33/00—Investigating or analysing materials by specific methods not covered by groups G01N1/00 - G01N31/00
- G01N33/48—Biological material, e.g. blood, urine; Haemocytometers
- G01N33/50—Chemical analysis of biological material, e.g. blood, urine; Testing involving biospecific ligand binding methods; Immunological testing
- G01N33/53—Immunoassay; Biospecific binding assay; Materials therefor
- G01N33/577—Immunoassay; Biospecific binding assay; Materials therefor involving monoclonal antibodies binding reaction mechanisms characterised by the use of monoclonal antibodies; monoclonal antibodies per se are classified with their corresponding antigens
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K2039/505—Medicinal preparations containing antigens or antibodies comprising antibodies
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K2300/00—Mixtures or combinations of active ingredients, wherein at least one active ingredient is fully defined in groups A61K31/00 - A61K41/00
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K2317/00—Immunoglobulins specific features
- C07K2317/20—Immunoglobulins specific features characterized by taxonomic origin
- C07K2317/24—Immunoglobulins specific features characterized by taxonomic origin containing regions, domains or residues from different species, e.g. chimeric, humanized or veneered
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K2317/00—Immunoglobulins specific features
- C07K2317/70—Immunoglobulins specific features characterized by effect upon binding to a cell or to an antigen
- C07K2317/76—Antagonist effect on antigen, e.g. neutralization or inhibition of binding
-
- G—PHYSICS
- G01—MEASURING; TESTING
- G01N—INVESTIGATING OR ANALYSING MATERIALS BY DETERMINING THEIR CHEMICAL OR PHYSICAL PROPERTIES
- G01N2333/00—Assays involving biological materials from specific organisms or of a specific nature
- G01N2333/435—Assays involving biological materials from specific organisms or of a specific nature from animals; from humans
- G01N2333/705—Assays involving receptors, cell surface antigens or cell surface determinants
- G01N2333/70596—Molecules with a "CD"-designation not provided for elsewhere in G01N2333/705
-
- G—PHYSICS
- G01—MEASURING; TESTING
- G01N—INVESTIGATING OR ANALYSING MATERIALS BY DETERMINING THEIR CHEMICAL OR PHYSICAL PROPERTIES
- G01N2333/00—Assays involving biological materials from specific organisms or of a specific nature
- G01N2333/435—Assays involving biological materials from specific organisms or of a specific nature from animals; from humans
- G01N2333/705—Assays involving receptors, cell surface antigens or cell surface determinants
- G01N2333/71—Assays involving receptors, cell surface antigens or cell surface determinants for growth factors; for growth regulators
-
- G—PHYSICS
- G01—MEASURING; TESTING
- G01N—INVESTIGATING OR ANALYSING MATERIALS BY DETERMINING THEIR CHEMICAL OR PHYSICAL PROPERTIES
- G01N2800/00—Detection or diagnosis of diseases
- G01N2800/52—Predicting or monitoring the response to treatment, e.g. for selection of therapy based on assay results in personalised medicine; Prognosis
Definitions
- the present invention is directed to methods for identifying patients that will benefit from treatment with a VEGF antagonist, e.g., an anti-VEGF antibody.
- a VEGF antagonist e.g., an anti-VEGF antibody.
- Angiogenesis is necessary for cancer development, regulating not only primary tumor size and growth, but also impacting invasive and metastatic potential. Accordingly, the mechanisms mediating angiogenic processes have been investigated as potential targets for directed anti-cancer therapies.
- VEGF vascular endothelial growth factor
- the use of angiogenesis inhibitors in the clinic has shown success, not all patients respond or fully respond to this therapy. The mechanism(s) underlying such incomplete response is unknown. Therefore, there is a need for the identification of patient subgroups sensitive or responsive to anti-angiogenic cancer therapy.
- Bevacizumab (Avastin®) is a recombinant humanized monoclonal IgG1 antibody that specifically binds to and blocks the biological effects of VEGF. Bevacizumab has been approved in Europe for the treatment of the advanced stages of five common types of cancer: colorectal cancer, breast cancer, non-small cell lung cancer (NSCLC), ovarian cancer, and kidney cancer, which collectively cause over 2.5 million deaths each year. In the United States, bevacizumab was the first anti-angiogenesis therapy approved by the FDA, and it is now approved for the treatment of five tumor types: colorectal cancer, NSCLC, brain cancer (glioblastoma), kidney cancer (renal cell carcinoma), and cervical cancer.
- NSCLC non-small cell lung cancer
- ovarian cancer ovarian cancer
- kidney cancer which collectively cause over 2.5 million deaths each year.
- bevacizumab was the first anti-angiogenesis therapy approved by the FDA, and it is now approved for the treatment of five tumor types:
- bevacizumab Over half a million patients have been treated with bevacizumab so far, and a comprehensive clinical program with over 450 clinical trials is investigating the further use of bevacizumab in the treatment of multiple cancer types (including colorectal, breast, NSCLC, brain, gastric, ovarian, and prostate cancers) in different settings (e.g., advanced or early stage disease).
- cancer types including colorectal, breast, NSCLC, brain, gastric, ovarian, and prostate cancers
- Bevacizumab has shown promise as a co-therapeutic, demonstrating efficacy when combined with a broad range of chemotherapies and other anti-cancer treatments.
- phase-Ill studies have demonstrated the beneficial effects of combining bevacizumab with standard chemotherapeutic regimens (see, e.g., Saltz et al., 2008, J. Clin. Oncol., 26:2013-2019 ; Yang et al., 2008, Clin. Cancer Res., 14:5893-5899 ; Hurwitz et al., 2004, N. Engl. J. Med., 350:2335-2342 ).
- phase-Ill studies have shown that a portion of patients experience incomplete response to the addition of bevacizumab to their chemotherapeutic regimens.
- HAN E S ET AL "Predictive and prognostic angiogenic markers in a gynecologic oncology group phase II trial of bevacizumab in recurrent and persistent ovarian or peritoneal cancer",GYNECOLOGIC ONCOLOGY, ACADEMIC PRESS, LONDON, GB, vol. 119, no. 3, 1 December 2010 (2010-12-01), pages 484-490 ,discloses high CD31-MVD as a prognostic marker for Epithelial Ovarian Cancer (EOC).
- EOC Epithelial Ovarian Cancer
- the present invention features a method of treating a patient with a cancer, the method including administering to the patient a therapeutically effective amount of a VEGF antagonist, wherein the patient's cancer has been determined to express CD31 and/or tumor VEGFA at a level more than the median level for CD31 and/or tumor VEGFA expression, respectively, in the cancer type.
- the present invention features a VEGF antagonist for use in a method of treating a patient with a cancer, wherein the patient's cancer has been determined to express CD31 and/or tumor VEGFA at a level more than the median level for CD31 and/or tumor VEGFA expression, respectively, in the cancer type, and the method comprises administering to the patient a therapeutically effective amount of the VEGF antagonist.
- the present invention features a method of identifying a patient suffering from a cancer who may benefit from administration of a VEGF antagonist, the method including: a) determining the expression level of CD31 and/or tumor VEGFA in a sample obtained from the patient, wherein expression of CD31 and/or tumor VEGFA at a level more than the median level for CD31 and/or tumor VEGFA expression, respectively, in the cancer type indicates that the patient may benefit from administration of a VEGF antagonist, and optionally b) administering the VEGF antagonist in a therapeutically effective amount to the patient.
- the present invention features a method of predicting responsiveness of a patient to administration of a VEGF antagonist for treatment of a cancer, the method including: a) determining the expression level of CD31 and/or tumor VEGFA in a sample obtained from the patient, wherein expression of CD31 and/or tumor VEGFA at a level more than the median level for CD31 and/or tumor VEGFA expression, respectively, in the cancer type indicates that the patient is more likely to be responsive to the administration of the VEGF antagonist, and optionally b) administering the VEGF antagonist in a therapeutically effective amount to the patient.
- the sample is a tumor tissue sample. In other embodiments, the sample is obtained before neoadjuvant or adjuvant therapy.
- the patient's cancer has been determined to express CD31 at a level that is more than the median level for CD31 expression in the cancer type. In particular aspects of this embodiment, the patient's cancer has been determined to express CD31 at a level that is more than the 75 th percentile for CD31 expression in the cancer type.
- the patient's cancer has been determined to express tumor VEGFA at a level that is more than the median level for tumor VEGFA expression in the cancer type. In particular aspects of this embodiment, the patient's cancer has been determined to express tumor VEGFA at a level that is more than the 75 th percentile for tumor VEGFA expression in the cancer type.
- the administration of the VEGF antagonist improves progression free survival (PFS) in the patient.
- the administration of the VEGF antagonist improves overall survival (OS) in the patient.
- the VEGF antagonist is administered in combination with one or more additional chemotherapeutic agents in a chemotherapy regimen.
- the one or more additional chemotherapeutic agents is selected from the group consisting of: a chemotherapeutic agent, HER antibody, antibody directed against a tumor associated antigen, anti-hormonal compound, cardioprotectant, cytokine, EGFR-targeted drug, anti-angiogenic agent, tyrosine kinase, inhibitor, COX inhibitor, non-steroidal anti-inflammatory drug, farnesyl trasferase inhibitor, antibody that binds oncofetal protein CA 125, Her2 vaccine, HER targeting therapy, Raf or ras inhibitor, liposomal doxorubicin, topotecan, taxane, dual tyrosine kinase inhibitor, TLK286, EMD-7200, a medicament that treats nausea, a medicament that prevents or treats skin rash or standard acne therapy, a medicament that treats or prevents diarrhea, a body temperature-reducing medicament, and a hematopoietic growth factor.
- a chemotherapeutic agent HER antibody, antibody
- the chemotherapeutic agent is gemcitabine, carboplatin, oxaliplatin, irinotecan, fluoropyrimidine (e.g., 5-FU), paclitaxel (e.g., nab-paclitaxel), docetaxel, topotecan, capecitabine, lecovorin, temozolomide, interferon-alpha, or liposomal doxorubicin (e.g., pegylated liposomal doxorubicin).
- fluoropyrimidine e.g., 5-FU
- paclitaxel e.g., nab-paclitaxel
- docetaxel e.g., topotecan
- topotecan ecitabine
- lecovorin e.g., temozolomide
- interferon-alpha e.g., interferon-alpha
- liposomal doxorubicin e.g., peg
- the chemotherapy regimen includes the administration of carboplatin and paclitaxel; carboplatin and gemcitabine; or paclitaxel, topotecan, or pegylated liposomal doxorubicin.
- the chemotherapy regimen includes the administration of capecitabine and paclitaxel; or capecitabine and docetaxel.
- the chemotherapy regimen includes the administration of temozolomide and optionally radiotherapy.
- the chemotherapy regimen includes the administration of fluropyrimidine, irinotecan, cisplatin, fluropyramidine and oxaliplatin; fluropyrimidine and irinotecan; fluropyramidine, lecovorin, and oxaliplatin; or ironotecan, fluoropyrimidine, and leucovorin.
- the chemotherapy regimen includes the administration of paclitaxel and topotecan; or paclitaxel and cisplatin.
- the chemotherapy regimen includes the administration of interferon-alpha2a.
- the present invention features a method for the prognosis of a patient suffering from cancer, the method including: a) determining the expression level of CD31 in a sample obtained from the patient, b) comparing the expression level of CD31 to the median level for CD31 in the cancer type, and c) determining a prognosis for the patient, wherein a poor prognosis is when expression of CD31 is at a level more than the medial level for CD31 expression.
- the method further includes the step of identifying the patient as likely to benefit from administration of a VEGF antagonist when the patient is determined to have a poor prognosis of survival. In yet another aspect, the method further includes the step of administering a VEGF antagonist in a therapeutically effective amount to the patient, if the patient is determine to have a poor prognosis.
- the VEGF antagonist is an anti-VEGF antibody. In preferred embodiments, the anti-VEGF antibody is bevacizumab.
- the method is carried out prior to administering an anti-cancer agent in order to provide a pre-administration prognosis of survival.
- the survival is progression free survival or overall survival.
- the present invention features a method of treating a patient with a cancer, the method including administering to the patient a therapeutically effective amount of a therapeutic agent other than a VEGF antagonist, wherein the patient's cancer has been determined to express CD31 and/or tumor VEGFA at a level less than the median level for CD31 and/or tumor VEGFA expression, respectively, in the cancer type.
- the present invention features a therapeutic agent other than a VEGF antagonist for use in a method of treating a patient with a cancer, wherein the patient's cancer has been determined to express CD31 and/or tumor VEGFA at a level less than the median level for CD31 and/or tumor VEGFA expression, respectively, in the cancer type, and the method comprises administering to the patient a therapeutically effective amount of the therapeutic agent other than a VEGF antagonist.
- the patient's cancer has been determined to express CD31 at a level that is less than the median level for CD31 expression in the cancer type. In certain aspects of this embodiment, the patient's cancer has been determined to express CD31 at a level that is less than the 25 th percentile for CD31 expression in the cancer type.
- the patient's cancer has been determined to express tumor VEGFA at a level that is less than the median level for tumor VEGFA expression in the cancer type. In certain aspects of this embodiment, the patient's cancer has been determined to express tumor VEGFA at a level that is less than the 25 th percentile for tumor VEGFA expression in the cancer type.
- the cancer is selected from the group consisting of colorectal cancer, breast cancer, non-small cell lung cancer (NSCLC), kidney cancer (renal cell carcinoma), or brain cancer (glioblastoma).
- the cancer is a gynecologic cancer selected from the group consisting of ovarian cancer, peritoneal cancer, fallopian tube cancer, cervical cancer, endometrial cancer, vaginal cancer, and vulvar cancer.
- the gynecologic cancer is ovarian cancer.
- the cancer is platinum-resistant, platinum-sensitive, advanced, refractory, or recurrent.
- the level of CD31 expression detected in the sample of the patient is used to determine the density of CD31 microvascular structures (CD31 MVD) in the cancer of the patient, and optionally wherein CD31 MVD of the patient's sample is compared to the median level of CD31 MVD in the cancer type.
- CD31 and/or tumor VEGFA expression is detected by an immunohistochemical (IHC) method.
- the VEGF antagonist is an anti-VEGF antibody.
- the anti-VEGF antibody is bevacizumab.
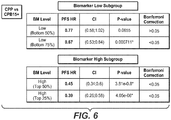
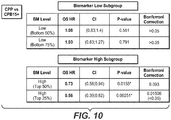
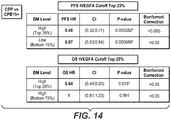
- the present invention is based in part on the finding that the tumor expression levels of CD31 and/or tumor VEGFA in a given patient, relative to the expression levels in a given population of patients having a cancer, in particular, a gynecologic cancer, such as ovarian cancer, associate with treatment effects in those patients administered an angiogenesis inhibitor in combination with a chemotherapy regimen.
- a cancer in particular, a gynecologic cancer, such as ovarian cancer
- variations in higher microvasculature density levels as measured by the number of CD31 vascular structures per mm 2
- tumor VEGFA were identified as candidate markers/predictors for improved progression-free survival (PFS) and improved overall survival (OS) of ovarian cancer patients in response to the addition of bevacizumab to carboplatin-paclitaxel chemotherapeutic regimens.
- the invention thus provides methods of treating patients with cancer (e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., metastatic breast cancer (MBC); also see below)) by administering to the patients a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab), where the patient's cancer has been determined to express CD31 MVD and/or tumor VEGFA at a level higher than the median level in the cancer type.
- cancer e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., metastatic breast cancer (MBC); also see below)
- a VEGF antagonist e.g., an anti-VEGF antibody,
- the invention also provides methods of identifying patients with cancer (e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., metastatic breast cancer (MBC); also see below)) who may benefit from administration of a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab), optionally in addition to another anti-cancer therapy, or identifying a patient who may be more responsive to treatment with a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab) by determining expression level of CD31 and/or tumor VEGFA in a tumor sample from the patient, where the VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab) is administered if the expression of CD31 MVD and/or tumor VEGFA is at a level more than the median
- Protein expression refers to conversion of the information encoded in a gene into messenger RNA (mRNA) and then to the protein.
- mRNA messenger RNA
- a sample or cell that "expresses" a protein of interest is one in which mRNA encoding the protein, or the protein, including fragments thereof, is determined to be present in the sample or cell.
- a sample, cell, tumor, or cancer which "has been determined to express” or “expresses” CD31 MVD and/or tumor VEGFA at a level more than the median level for CD31 MVD and/or tumor VEGFA expression" in a type of cancer is one in which the level of CD31 MVD and/or tumor VEGFA expression is considered a "high CD31 MVD and/or tumor VEGFA level" to a skilled person for that type of cancer.
- such level will be in the range from about 50% up to about 100% (e.g., 50%, 55%, 60%, 65%, 70%, 75%, 80%, 85%, 90%, or 95%) relative to CD31 MVD and/or tumor VEGFA levels in a population of samples, cells, tumors, or cancers of the same cancer type.
- the population that is used to arrive at the median expression level may be ovarian cancer samples generally, or subgroupings thereof, such as chemotherapy-resistant ovarian cancer, platinum-resistant ovarian cancer, as well as advanced, refractory, or recurrent ovarian cancer.
- the examples herein demonstrate how the median expression level can be determined. This may constitute an absolute value of expression.
- the cutoff for ovarian patients considered to express CD31 MVD at a high level may be about 17.78 or more (25 th percentile), about 25.19 or more (50 th percentile), about 35.8 or more (75 th percentile), etc.
- Such absolute values will be quantified in an assay under specified assay conditions, such as in an immunohistochemical (IHC) method, e.g., as disclosed herein, and most preferably the IHC assay as in Example 1.
- IHC immunohistochemical
- the level of CD31 MVD and/or tumor VEGFA expression is more than or at the 50 th percentile (e.g., the 50 th , 55 th , 60 th , 65 th , 68 th , or 70 th percentile), and most preferably more than or at the 75 th percentile (e.g., the 75 th , 76 th , 78 th , 80 th , 85 th , 90 th , or 95 th percentile).
- the 50 th percentile e.g., the 50 th , 55 th , 60 th , 65 th , 68 th , or 70 th percentile
- 75 th percentile e.g., the 75 th , 76 th , 78 th , 80 th , 85 th , 90 th , or 95 th percentile.
- cancer is or has been determined to express or “cancer expresses,” used in reference to a particular biomarker (e.g., CD31 and/or tumor VEGFA), means expression of the biomarker (e.g., CD31 and/or tumor VEGFA), as determined using a diagnostic test, any of the detection methods described herein, or the similar.
- a biomarker e.g., CD31 and/or tumor VEGFA
- expression is in endothelial cells of blood vessels within a cancer or tumor tissue, while VEGFA expression occurs in cancer or tumor cells.
- the level of CD31 expression detected in a patient sample can be used to determine the density of CD31 microvascular structures (CD31 MVD) in the cancer of the patient, and optionally the CD31 MVD of the patient's sample can be compared to the median level of CD31 MVD in the cancer type.
- CD31 MVD CD31 microvascular structures
- tissue or cell sample is meant a collection of cells obtained from a tissue of a subject or patient.
- the source of the tissue or cell sample may be solid tissue as from a fresh, frozen, and/or preserved organ or tissue sample or biopsy or aspirate; blood or any blood constituents; bodily fluids such as cerebral spinal fluid, amniotic fluid, peritoneal fluid, or interstitial fluid; cells from any time in gestation or development of the subject or plasma.
- the tissue sample may also be primary or cultured cells or cell lines.
- the tissue or cell sample is obtained from a cancerous tissue/organ.
- the tissue sample may contain compounds which are not naturally intermixed with the tissue in nature such as preservatives, anticoagulants, buffers, fixatives, nutrients, antibiotics, or the like.
- a "section" of a tissue sample is meant a single part or piece of a tissue sample, e.g. a thin slice of tissue or cells cut from a tissue sample.
- tumor sample herein is a sample derived from, or comprising tumor cells from, a patient's tumor.
- tumor samples herein include, but are not limited to, tumor biopsies, circulating tumor cells, circulating plasma proteins, ascitic fluid, primary cell cultures or cell lines derived from tumors or exhibiting tumor-like properties, as well as preserved tumor samples, such as formalin-fixed, paraffin-embedded tumor samples or frozen tumor samples.
- tumor samples can include blood vessels.
- association is meant comparing, in any way, the performance and/or results of a first analysis or protocol with the performance and/or results of a second analysis or protocol. For example, one may use the results of a first analysis or protocol in carrying out a second protocols and/or one may use the results of a first analysis or protocol to determine whether a second analysis or protocol should be performed. With respect to the embodiment of gene expression analysis or protocol, one may use the results of the gene expression analysis or protocol to determine whether a specific therapeutic regimen should be performed.
- biomarker refers generally to a molecule, including a gene, protein, carbohydrate structure, or glycolipid, the expression of which in or on a mammalian tissue or cell can be detected by standard methods (or methods disclosed herein) and is predictive, diagnostic, and/or prognostic for the sensitivity of a mammalian cell or tissue to treatment regimes based on inhibition of angiogenesis using, e.g., an anti-angiogenesis agent such as a VEGF-specific inhibitor (e.g., an anti-VEGF antibody, such as bevicizumab).
- an anti-angiogenesis agent such as a VEGF-specific inhibitor
- the expression of such a biomarker is determined to be higher than that observed for a control/reference tissue or cell sample.
- Biomarkers can be determined using a high-throughput multiplexed immunoassay such as those commercially available from Rules Based Medicine, Inc. or Meso Scale Discovery. Expression of the biomarkers may also be determined using, e.g., PCR or FACS assay, an immunohistochemical assay or a gene chip-based assay.
- VEGF antagonist or "VEGF-specific antagonist” refers to a molecule capable of binding to VEGF, reducing VEGF expression levels, or neutralizing, blocking, inhibiting, abrogating, reducing, or interfering with VEGF biological activities, including, but not limited to, VEGF binding to one or more VEGF receptors, VEGF signaling, and VEGF mediated angiogenesis and endothelial cell survival or proliferation.
- a molecule capable of neutralizing, blocking, inhibiting, abrogating, reducing, or interfering with VEGF biological activities can exert its effects by binding to one or more VEGF receptor (VEGFR) (e.g., VEGFR1, VEGFR2, VEGFR3, membrane-bound VEGF receptor (mbVEGFR), or soluble VEGF receptor (sVEGFR)).
- VEGFR VEGF receptor
- mbVEGFR3 membrane-bound VEGF receptor
- sVEGFR soluble VEGF receptor
- VEGF-specific antagonists useful in the methods of the invention are polypeptides that specifically bind to VEGF, anti-VEGF antibodies and antigen-binding fragments thereof, receptor molecules and derivatives which bind specifically to VEGF thereby sequestering its binding to one or more receptors, fusions proteins (e.g., VEGF-Trap (Regeneron)), and VEGF 121 -gelonin (Peregrine).
- VEGF-Trap (Regeneron)
- Peregrine VEGF 121 -gelonin
- VEGF-specific antagonists also include antagonist variants of VEGF polypeptides, antisense nucleobase oligomers complementary to at least a fragment of a nucleic acid molecule encoding a VEGF polypeptide; small RNAs complementary to at least a fragment of a nucleic acid molecule encoding a VEGF polypeptide; ribozymes that target VEGF; peptibodies to VEGF; and VEGF aptamers.
- VEGF antagonists also include polypeptides that bind to VEGFR, anti-VEGFR antibodies, and antigen-binding fragments thereof, and derivatives which bind to VEGFR thereby blocking, inhibiting, abrogating, reducing, or interfering with VEGF biological activities (e.g., VEGF signaling), or fusions proteins.
- VEGF-specific antagonists also include nonpeptide small molecules that bind to VEGF or VEGFR and are capable of blocking, inhibiting, abrogating, reducing, or interfering with VEGF biological activities.
- VEGF activities specifically includes VEGF mediated biological activities of VEGF.
- the VEGF antagonist reduces or inhibits, by at least 10%, 20%, 30%, 40%, 50%, 60%, 70%, 80%, 90% or more, the expression level or biological activity of VEGF.
- the VEGF inhibited by the VEGF-specific antagonist is VEGF (8-109), VEGF (1-109), or VEGF 165 .
- VEGF antagonists can include, but are not limited to, anti-VEGFR2 antibodies and related molecules (e.g., ramucirumab, tanibirumab, aflibercept), anti-VEGFR1 antibodies and related molecules (e.g., icrucumab, aflibercept (VEGF Trap-Eye; EYLEA®), and ziv-aflibercept (VEGF Trap; ZALTRAP®)), bispecific VEGF antibodies (e.g., MP-0250, vanucizumab (VEGF-ANG2), and bispecific antibodies disclosed in US 2001/0236388 ), bispecific antibodies including combinations of two of anti-VEGF, anti-VEGFRl, and anti-VEGFR2 arms, anti-VEGFA antibodies (e.g., bevacizumab, sevacizumab), anti-VEGFB antibodies, anti-VEGFC antibodies (e.g., VGX-100), anti-VEGFD antibodies, and nonpeptide
- an "anti-VEGF antibody” is an antibody that binds to VEGF with sufficient affinity and specificity.
- the antibody will have a sufficiently high binding affinity for VEGF, for example, the antibody may bind hVEGF with a K d value of between 100 nM-1 pM.
- Antibody affinities may be determined, e.g., by a surface plasmon resonance based assay (such as the BIAcore assay as described in PCT Application Publication No. WO2005/012359 ); enzyme-linked immunoabsorbent assay (ELISA); and competition assays (e.g. RIA's).
- the anti-VEGF antibody can be used as a therapeutic agent in targeting and interfering with diseases or conditions wherein the VEGF activity is involved.
- the antibody may be subjected to other biological activity assays, e.g., in order to evaluate its effectiveness as a therapeutic.
- biological activity assays are known in the art and depend on the target antigen and intended use for the antibody. Examples include the HUVEC inhibition assay; tumor cell growth inhibition assays (as described in WO 89/06692 , for example); antibody-dependent cellular cytotoxicity (ADCC) and complement-mediated cytotoxicity (CDC) assays ( U.S. Pat. No.
- anti-VEGF antibody will usually not bind to other VEGF homologues such as VEGF-B or VEGF-C, nor other growth factors such as P1GF, PDGF, or bFGF.
- anti-VEGF antibody is a monoclonal antibody that binds to the same epitope as the monoclonal anti-VEGF antibody A4.6.1 produced by hybridoma ATCC HB 10709.
- the anti-VEGF antibody is a recombinant humanized anti-VEGF monoclonal antibody generated according to Presta et al. (1997) Cancer Res. 57:4593-4599 , including but not limited to the antibody known as bevacizumab (BV; AVASTIN®).
- Bevacizumab also known as “rhuMAb VEGF” or “AVASTIN®”
- rhuMAb VEGF a recombinant humanized anti-VEGF monoclonal antibody generated according to Presta et al. (1997) Cancer Res. 57:4593-4599 . It comprises mutated human IgG1 framework regions and antigen-binding complementarity-determining regions from the murine anti-hVEGF monoclonal antibody A.4.6.1 that blocks binding of human VEGF to its receptors.
- Approximately 93% of the amino acid sequence of bevacizumab, including most of the framework regions, is derived from human IgG1, and about 7% of the sequence is derived from the murine antibody A4.6.1.
- Bevacizumab has a molecular mass of about 149,000 daltons and is glycosylated. Bevacizumab and other humanized anti-VEGF antibodies are further described in U.S. Pat. No. 6,884,879 issued Feb. 26, 2005 . Additional preferred antibodies include the G6 or B20 series antibodies (e.g., G6-31, B20-4.1), as described in PCT Application Publication No. WO 2005/012359 . For additional preferred antibodies see U.S. Pat. Nos. 7,060,269 , 6,582,959 , 6,703,020 ; 6,054,297 ; WO98/45332 ; WO 96/30046 ; WO94/10202 ; EP 0666868B1 ; U.S.
- Other preferred antibodies include those that bind to a functional epitope on human VEGF comprising of residues F17, M18, D19, Y21, Y25, Q89, 191, K101, E103, and C104 or, alternatively, comprising residues F17, Y21, Q22, Y25, D63, 183, and Q89.
- antibody is used in the broadest sense and specifically covers monoclonal antibodies (including full length monoclonal antibodies), polyclonal antibodies, multispecific antibodies (e.g., bispecific antibodies), and antibody fragments so long as they exhibit the desired biological activity.
- a “blocking” antibody or an antibody “antagonist” is one which inhibits or reduces biological activity of the antigen it binds.
- a VEGF-specific antagonist antibody binds VEGF and inhibits the ability of VEGF to induce vascular endothelial cell proliferation.
- Preferred blocking antibodies or antagonist antibodies completely inhibit the biological activity of the antigen.
- multivalent antibody is used throughout this specification to denote an antibody comprising three or more antigen binding sites.
- the multivalent antibody is preferably engineered to have the three or more antigen binding sites and is generally not a native sequence IgM or IgA antibody.
- an “Fv” fragment is an antibody fragment which contains a complete antigen recognition and binding site.
- This region consists of a dimer of one heavy and one light chain variable domain in tight association, which can be covalent in nature, for example in scFv. It is in this configuration that the three CDRs of each variable domain interact to define an antigen binding site on the surface of the V H -V L dimer.
- the six CDRs or a subset thereof confer antigen binding specificity to the antibody.
- a single variable domain or half of an Fv comprising only three CDRs specific for an antigen
- the term "monoclonal antibody” as used herein refers to an antibody obtained from a population of substantially homogeneous antibodies, i.e., the individual antibodies comprising the population are identical except for possible naturally occurring mutations that may be present in minor amounts. Monoclonal antibodies are highly specific, being directed against a single antigenic site. Furthermore, in contrast to conventional (polyclonal) antibody preparations which typically include different antibodies directed against different determinants (epitopes), each monoclonal antibody is directed against a single determinant on the antigen.
- the modifier "monoclonal” indicates the character of the antibody as being obtained from a substantially homogeneous population of antibodies, and is not to be construed as requiring production of the antibody by any particular method.
- the monoclonal antibodies to be used in accordance with the present invention may be made by the hybridoma method first described by Kohler et al., Nature 256:495 (1975 ), or may be made by recombinant DNA methods (see, e.g., U.S. Patent No. 4,816,567 ).
- the "monoclonal antibodies” may also be isolated from phage antibody libraries using the techniques described in Clackson et al., Nature 352:624-628 (1991 ) and Marks et al., J. Mol. Biol. 222:581-597 (1991 ), for example.
- the monoclonal antibodies herein specifically include "chimeric" antibodies (immunoglobulins) in which a portion of the heavy and/or light chain is identical with or homologous to corresponding sequences in antibodies derived from a particular species or belonging to a particular antibody class or subclass, while the remainder of the chain(s) is identical with or homologous to corresponding sequences in antibodies derived from another species or belonging to another antibody class or subclass, as well as fragments of such antibodies, so long as they exhibit the desired biological activity ( U.S. Pat. No. 4,816,567 ; and Morrison et al., Proc. Natl. Acad. Sci. USA 81:6851-6855 (1984 )).
- chimeric antibodies immunoglobulins in which a portion of the heavy and/or light chain is identical with or homologous to corresponding sequences in antibodies derived from a particular species or belonging to a particular antibody class or subclass, while the remainder of the chain(s) is identical with or homologous to corresponding
- Humanized forms of non-human (e.g., murine) antibodies are chimeric antibodies which contain minimal sequence derived from non-human immunoglobulin.
- humanized antibodies are human immunoglobulins (recipient antibody) in which residues from a hypervariable region of the recipient are replaced by residues from a hypervariable region of a non-human species (donor antibody) such as mouse, rat, rabbit or nonhuman primate having the desired specificity, affinity, and capacity.
- donor antibody such as mouse, rat, rabbit or nonhuman primate having the desired specificity, affinity, and capacity.
- Fv framework region (FR) residues of the human immunoglobulin are replaced by corresponding non-human residues.
- humanized antibodies may comprise residues which are not found in the recipient antibody or in the donor antibody. These modifications are made to further refine antibody performance.
- the humanized antibody will comprise substantially all of at least one, and typically two, variable domains, in which all or substantially all of the hypervariable loops correspond to those of a non-human immunoglobulin and all or substantially all of the FR regions are those of a human immunoglobulin sequence.
- the humanized antibody optionally also will comprise at least a portion of an immunoglobulin constant region (Fc), typically that of a human immunoglobulin.
- Fc immunoglobulin constant region
- a "human antibody” is one which possesses an amino acid sequence which corresponds to that of an antibody produced by a human and/or has been made using any of the techniques for making human antibodies as disclosed herein. This definition of a human antibody specifically excludes a humanized antibody comprising non-human antigen-binding residues.
- Human antibodies can be produced using various techniques known in the art. In one embodiment, the human antibody is selected from a phage library, where that phage library expresses human antibodies ( Vaughan et al. Nature Biotechnology 14:309-314 (1996 ): Sheets et al. Proc. Natl. Acad. Sci. 95:6157-6162 (1998 )); Hoogenboom and Winter, J. Mol.
- Human antibodies can also be made by introducing human immunoglobulin loci into transgenic animals, e.g., mice in which the endogenous immunoglobulin genes have been partially or completely inactivated. Upon challenge, human antibody production is observed, which closely resembles that seen in humans in all respects, including gene rearrangement, assembly, and antibody repertoire. This approach is described, for example, in U.S. Pat. Nos.
- the human antibody may be prepared via immortalization of human B lymphocytes producing an antibody directed against a target antigen (such B lymphocytes may be recovered from an individual or may have been immunized in vitro). See, e.g., Cole et al., Monoclonal Antibodies and Cancer Therapy, Alan R. Liss, p. 77 (1985 ); Boerner et al., J. Immunol., 147 (1):86-95 (1991 ); and U.S. Pat. No. 5,750,373 .
- an “isolated” polypeptide or “isolated” antibody is one that has been identified and separated and/or recovered from a component of its natural environment. Contaminant components of its natural environment are materials that would interfere with diagnostic or therapeutic uses for the polypeptide or antibody, and may include enzymes, hormones, and other proteinaceous or nonproteinaceous solutes.
- the polypeptide or antibody will be purified (1) to greater than 95% by weight of polypeptide or antibody as determined by the Lowry method, and most preferably more than 99% by weight, (2) to a degree sufficient to obtain at least 15 residues of N-terminal or internal amino acid sequence by use of a spinning cup sequenator, or (3) to homogeneity by SDS-PAGE under reducing or nonreducing conditions using Coomassie blue or, preferably, silver stain.
- Isolated polypeptide or antibody includes the polypeptide or antibody in situ within recombinant cells since at least one component of the polypeptide's natural environment will not be present. Ordinarily, however, isolated polypeptide or antibody will be prepared by at least one purification step.
- treatment refers to clinical intervention in an attempt to alter the natural course of the individual or cell being treated, and can be performed either for prophylaxis or during the course of clinical pathology. Desirable effects of treatment include preventing occurrence or recurrence of disease, alleviation of symptoms, diminishment of any direct or indirect pathological consequences of the disease, decreasing the rate of disease progression, amelioration or palliation of the disease state, and remission or improved prognosis. In some embodiments, methods and compositions of the invention are useful in attempts to delay development of a disease or disorder.
- the terms "therapeutically effective amount” or "effective amount” refer to an amount of a drug effective to treat cancer in the patient.
- the effective amount of the drug may reduce the number of cancer cells; reduce the tumor size; inhibit (i.e., slow to some extent and preferably stop) cancer cell infiltration into peripheral organs; inhibit (i.e., slow to some extent and preferably stop) tumor metastasis; inhibit, to some extent, tumor growth; and/or relieve to some extent one or more of the symptoms associated with the cancer.
- the drug may prevent growth and/or kill existing cancer cells, it may be cytostatic and/or cytotoxic.
- the effective amount may extend progression free survival (e.g.
- the therapeutically effective amount of the drug is effective to improve progression free survival (PFS) and/or overall survival (OS).
- “Survival” refers to the patient remaining alive, and includes overall survival as well as progression free survival.
- “Overall survival” refers to the patient remaining alive for a defined period of time, such as 1 year, 5 years, etc. from the time of diagnosis or treatment.
- progression-free survival in the context of the present invention refers to the length of time during and after treatment during which, according to the assessment of the treating physician or investigator, a patient's disease does not become worse, i.e., does not progress.
- a patient's progression-free survival is improved or enhanced if the patient experiences a longer length of time during which the disease does not progress as compared to the average or mean progression free survival time of a control group of similarly situated patients.
- extending survival is meant increasing overall or progression free survival in a treated patient relative to an untreated patient (i.e., relative to a patient not treated with a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab), or relative to a patient who does not express CD31 or tumor VEGFA at the designated level, and/or relative to a patient treated with an approved anti-tumor agent (such as topotecan or liposomal doxorubicin, where the cancer is ovarian cancer).
- a VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- an approved anti-tumor agent such as topotecan or liposomal doxorubicin, where the cancer is ovarian cancer
- a “fixed” or “flat” dose of a therapeutic agent herein refers to a dose that is administered to a human patient without regard for the weight (WT) or body surface area (BSA) of the patient.
- the fixed or flat dose is therefore not provided as a mg/kg dose or a mg/m 2 dose, but rather as an absolute amount of the therapeutic agent.
- a “loading" dose herein generally comprises an initial dose of a therapeutic agent administered to a patient, and is followed by one or more maintenance dose(s) thereof. Generally, a single loading dose is administered, but multiple loading doses are contemplated herein. Usually, the amount of loading dose(s) administered exceeds the amount of the maintenance dose(s) administered and/or the loading dose(s) are administered more frequently than the maintenance dose(s), so as to achieve the desired steady-state concentration of the therapeutic agent earlier than can be achieved with the maintenance dose(s).
- a “maintenance” dose or “extended” dose herein refers to one or more doses of a therapeutic agent administered to the patient over a treatment period. Usually, the maintenance doses are administered at spaced treatment intervals, such as approximately every week, approximately every 2 weeks, approximately every 3 weeks, or approximately every 4 weeks.
- a subject/patient suffering, suspected to suffer or prone to suffer from cancer e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., MBC; also see below)
- cancer e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., MBC; also see below)
- an anti-VEGF agent such as an anti-VEGF antibody, e.g., bevacizumab.
- a response may be reflected by decreased suffering from ovarian cancer, such as a diminished and/or halted tumor growth, reduction of the size of a tumor, and/or amelioration of one or more symptoms of ovarian cancer, e.g., ovarian bleeding, pain, anemia.
- the response may be reflected by decreased or diminished indices of the metastatic conversion of the cancer or indices of the cancer, e.g., the prevention of the formation of metastases or a reduction of number or size of metastases.
- a patient suffering from in accordance with the invention refers to a patient showing clinical signs of cancer (e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., metastatic MBC; also see below)).
- a gynecologic cancer e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer
- breast cancer e.g., metastatic MBC; also see below
- administering mean the administration of an angiogenesis inhibitor, e.g., an anti-VEGF antibody, such as bevacizumab, and/or a pharmaceutical composition/treatment regimen comprising an angiogenesis inhibitor, e.g., an anti-VEGF antibody, such as bevacizumab, to a patient in need of such treatment or medical intervention by any suitable means known in the art for administration of a therapeutic antibody.
- angiogenesis inhibitor e.g., an anti-VEGF antibody, such as bevacizumab
- a pharmaceutical composition/treatment regimen comprising an angiogenesis inhibitor, e.g., an anti-VEGF antibody, such as bevacizumab
- routes of administration include by oral, intravenous, intraperitoneal, subcutaneous, intramuscular, topical, intradermal, intranasal or intrabronchial administration (for example as effected by inhalation).
- parenteral administration e.g., intravenous administration.
- the preferred dosages according to the EMEA are 5 mg/kg or 10 mg/kg of body weight given once every 2 weeks or 7.5 mg/kg or 15 mg/kg of body weight given once every 3 weeks.
- the preferred dosage is 15 mg/kg given once every 3 weeks by infusion in combination with carboplatin and paclitaxel.
- the preferred dosage is 10 mg/kg given once every 2 weeks by infusion with interferon ⁇ -2a or as a monotherapy.
- the preferred dosage is 15 mg/kg given once every three weeks by infusion and administered in combination with one of the following chemotherapy regimens: paclitaxel and cisplatin or paclitaxel and topotecan.
- the preferred dosage is 10 mg/kg given once every two weeks by infusion.
- cancer and “cancerous” refer to or describe the physiological condition in mammals that is typically characterized by unregulated cell growth. Included in this definition are benign and malignant cancers. Examples of cancer include but are not limited to, carcinoma, lymphoma, blastoma, sarcoma, and leukemia.
- cancers include squamous cell cancer, lung cancer (including small-cell lung cancer, non-small cell lung cancer, adenocarcinoma of the lung, and squamous carcinoma of the lung), cancer of the peritoneum, hepatocellular cancer, gastric or stomach cancer (including gastrointestinal cancer), pancreatic cancer, glioblastoma, cervical cancer, ovarian cancer, liver cancer, bladder cancer, hepatoma, breast cancer, colon cancer, colorectal cancer, endometrial or uterine carcinoma, salivary gland carcinoma, kidney or renal cancer, liver cancer, prostate cancer, vulval cancer, thyroid cancer, hepatic carcinoma and various types of head and neck cancer, as well as B-cell lymphoma (including low grade/follicular non-Hodgkin's lymphoma (NHL); small lymphocytic (SL) NHL; intermediate grade/follicular NHL; intermediate grade diffuse NHL; high grade immunoblastic NHL; high grade lymphoblastic NHL; high grade small non-clea
- a "cancer type which is able to respond to a VEGF antagonist” is one which when treated with a VEGF antagonist, such as a VEGF antibody (e.g., bevacizumab) or small molecule inhibitor, shows a therapeutically effective benefit in the patient therewith according to any of the criteria for therapeutic effectiveness known to the skilled oncologist, including those elaborated herein, but particularly in terms of survival, including progression free survival (PFS) and/or overall survival (OS).
- a VEGF antagonist such as a VEGF antibody (e.g., bevacizumab) or small molecule inhibitor
- such cancer is selected from a gynecologic cancer (e.g., ovarian cancer, peritoneal cancer, fallopian tube cancer, cervical cancer, endometrial cancer, vaginal cancer, and vulvar cancer), breast cancer (e.g., MBC), non-small cell lung cancer (NSCLC), prostate cancer, and colorectal cancer.
- a gynecologic cancer e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, and vulvar cancer, including platinum-resistant forms of such cancers
- breast cancer e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, and vulvar cancer, including platinum-resistant forms of such cancers
- An "advanced" cancer is one which has spread outside the site or organ of origin, either by local invasion or metastasis.
- a "refractory” cancer is one which progresses even though an anti-tumor agent, such as a chemotherapeutic agent, is being administered to the cancer patient.
- An example of a refractory cancer is one which is platinum refractory.
- a "recurrent" cancer is one which has regrown, either at the initial site or at a distant site, after a response to initial therapy.
- a “patient” is a human patient.
- the patient may be a "cancer patient,” i.e., one who is suffering or at risk for suffering from one or more symptoms of cancer.
- VEGF antagonist is administered as a "single anti-tumor agent" it is the only anti-tumor agent administered to treat the cancer, i.e., it is not administered in combination with another anti-tumor agent, such as chemotherapy.
- standard of care herein is intended the anti-tumor agent or agents that are routinely used to treat a particular form of cancer.
- astandard of care is topotecan or liposomal doxorubicin.
- chemotherapeutic agent includes chemical compounds useful in the treatment of cancer.
- chemotherapeutic agents include erlotinib (TARCEVA®, Genentech/OSI Pharm.), bortezomib (VELCADE®, Millennium Pharm.), disulfiram, epigallocatechin gallate , salinosporamide A, carfilzomib, 17-AAG (geldanamycin), radicicol, lactate dehydrogenase A (LDH-A), fulvestrant (FASLODEX®, AstraZeneca), sunitib (SUTENT®, Pfizer/Sugen), letrozole (FEMARA®, Novartis), imatinib mesylate (GLEEVEC®, Novartis), finasunate (VATALANIB®, Novartis), oxaliplatin (ELOXATIN®, Sanofi), 5-FU (5-fluorouracil), leucovorin, Rapamycin (Sirol
- dynemicin including dynemicin A; bisphosphonates, such as clodronate; an esperamicin; as well as neocarzinostatin chromophore and related chromoprotein enediyne antibiotic chromophores), aclacinomysins, actinomycin, authramycin, azaserine, bleomycins, cactinomycin, carabicin, caminomycin, carzinophilin, chromomycinis, dactinomycin, daunorubicin, detorubicin, 6-diazo-5-oxo-L-norleucine, ADRIAMYCIN® (doxorubicin), morpholino-doxorubicin, cyanomorpholino-doxorubicin, 2-pyrrolino-doxorubicin and deoxydoxorubicin), epirubicin, e
- Chemotherapeutic agent also includes (i) anti-hormonal agents that act to regulate or inhibit hormone action on tumors such as anti-estrogens and selective estrogen receptor modulators (SERMs), including, for example, tamoxifen (including NOLVADEX®; tamoxifen citrate), raloxifene, droloxifene, iodoxyfene , 4-hydroxytamoxifen, trioxifene, keoxifene, LY117018, onapristone, and FARESTON® (toremifine citrate); (ii) aromatase inhibitors that inhibit the enzyme aromatase, which regulates estrogen production in the adrenal glands, such as, for example, 4(5)-imidazoles, aminoglutethimide, MEGASE® (megestrol acetate), AROMASIN® (exemestane; Pfizer), formestanie, fadrozole, RIVISOR® (vorozole), FEMARA® (
- Chemotherapeutic agent also includes antibodies such as alemtuzumab (Campath), bevacizumab (AVASTIN®, Genentech); cetuximab (ERBITUX®, Imclone); panitumumab (VECTIBIX®, Amgen), rituximab (RITUXAN®, Genentech/Biogen Idec), pertuzumab (OMNITARG®, 2C4, Genentech), trastuzumab (HERCEPTIN®, Genentech), tositumomab (Bexxar, Corixia), and the antibody drug conjugate, gemtuzumab ozogamicin (MYLOTARG®, Wyeth).
- antibodies such as alemtuzumab (Campath), bevacizumab (AVASTIN®, Genentech); cetuximab (ERBITUX®, Imclone); panitumumab (VECTIBIX®, Amgen), rituximab
- Additional humanized monoclonal antibodies with therapeutic potential as agents in combination with the compounds of the invention include: apolizumab, aselizumab, atlizumab, bapineuzumab, bivatuzumab mertansine, cantuzumab mertansine, cedelizumab, certolizumab pegol, cidfusituzumab, cidtuzumab, daclizumab, eculizumab, efalizumab, epratuzumab, erlizumab, felvizumab, fontolizumab, gemtuzumab ozogamicin, inotuzumab ozogamicin, ipilimumab, labetuzumab, lintuzumab, matuzumab, mepolizumab, motavizumab, motovizumab, natalizumab, nimotuzumab, nolovizum
- Chemotherapeutic agent also includes "EGFR inhibitors,” which refers to compounds that bind to or otherwise interact directly with EGFR and prevent or reduce its signaling activity, and is alternatively referred to as an "EGFR antagonist.”
- EGFR inhibitors refers to compounds that bind to or otherwise interact directly with EGFR and prevent or reduce its signaling activity
- Examples of such agents include antibodies and small molecules that bind to EGFR.
- antibodies which bind to EGFR include MAb 579 (ATCC CRL HB 8506), MAb 455 (ATCC CRL HB8507), MAb 225 (ATCC CRL 8508), MAb 528 (ATCC CRL 8509) (see, US Patent No. 4,943 , 533, Mendelsohn et al.
- chimerized 225 C225 or Cetuximab; ERBUTIX®
- H225 reshaped human 225
- IMC-11F8 a fully human, EGFR-targeted antibody (Imclone); antibodies that bind type II mutant EGFR ( US Patent No. 5,212,290 ); humanized and chimeric antibodies that bind EGFR as described in US Patent No.
- EMD 55900 Stragliotto et al. Eur. J. Cancer 32A:636-640 (1996 )
- EMD7200 (matuzumab) a humanized EGFR antibody directed against EGFR that competes with both EGF and TGF-alpha for EGFR binding (EMD/Merck); human EGFR antibody, HuMax-EGFR (GenMab); fully human antibodies known as E1.1, E2.4, E2.5, E6.2, E6.4, E2.11, E6. 3 and E7.6.
- the anti-EGFR antibody may be conjugated with a cytotoxic agent, thus generating an immunoconjugate (see, e.g., EP659,439A2 , Merck Patent GmbH).
- EGFR antagonists include small molecules such as compounds described in US Patent Nos: 5,616,582 , 5,457,105 , 5,475,001 , 5,654,307 , 5,679,683 , 6,084,095 , 6,265,410 , 6,455,534 , 6,521,620 , 6,596,726 , 6,713,484 , 5,770,599 , 6,140,332 , 5,866,572 , 6,399,602 , 6,344,459 , 6,602,863 , 6,391,874 , 6,344,455 , 5,760,041 , 6,002,008 , and 5,747,498 , as well as the following PCT publications: WO98/14451 , WO98/50038 , WO99/09016 , and WO99/24037 .
- EGFR antagonists include OSI-774 (CP-358774, erlotinib, TARCEVA® Genentech/OSI Pharmaceuticals); PD 183805 (CI 1033, 2-propenamide, N-[4-[(3-chloro-4-fluorophenyl)amino]-7-[3-(4-morpholinyl)propoxy]-6-quinazolinyl]-, dihydrochloride, Pfizer Inc.); ZD1839, gefitinib (IRESSA®) 4-(3'-Chloro-4'-fluoroanilino)-7-methoxy-6-(3-morpholinopropoxy)quinazoline, AstraZeneca); ZM 105180 ((6-amino-4-(3-methylphenyl-amino)-quinazoline, Zeneca); BIBX-1382 (N8-(3-chloro-4-fluoro-phenyl)-N2-(1-methyl-piperid
- Chemotherapeutic agents also include "tyrosine kinase inhibitors" including the EGFR-targeted drugs noted in the preceding paragraph; small molecule HER2 tyrosine kinase inhibitor such as TAK165 available from Takeda; CP-724,714, an oral selective inhibitor of the ErbB2 receptor tyrosine kinase (Pfizer and OSI); dual-HER inhibitors such as EKB-569 (available from Wyeth) which preferentially binds EGFR but inhibits both HER2 and EGFR-overexpressing cells; lapatinib (GSK572016; available from Glaxo-SmithKline), an oral HER2 and EGFR tyrosine kinase inhibitor; PKI-166 (available from Novartis); pan-HER inhibitors such as canertinib (CI-1033; Pharmacia); Raf-1 inhibitors such as antisense agent ISIS-5132 available from ISIS Pharmaceuticals which inhibit Raf-1 signaling; non-HER targeted
- Chemotherapeutic agents also include dexamethasone, interferons, colchicine, metoprine, cyclosporine, amphotericin, metronidazole, alemtuzumab, alitretinoin, allopurinol, amifostine, arsenic trioxide, asparaginase, BCG live, bevacuzimab, bexarotene, cladribine, clofarabine, darbepoetin alfa, denileukin, dexrazoxane, epoetin alfa, elotinib, filgrastim, histrelin acetate, ibritumomab, interferon alfa-2a, interferon alfa-2b, lenalidomide, levamisole, mesna, methoxsalen, nandrolone, nelarabine, nofetumomab, oprelvekin,
- platinum-based chemotherapeutic agent or “platin” is meant an antineoplastic drug that is a coordination complex of platinum.
- platinum-based chemotherapeutic agents include carboplatin, cisplatin, and oxaliplatinum.
- platinum-based chemotherapy therapy with one or more platinum-based chemotherapeutic agent, optionally in combination with one or more other chemotherapeutic agents.
- chemotherapy-resistant cancer cancer in a patient that has progressed while the patient is receiving a chemotherapy regimen (i.e., the patient is "chemotherapy refractory"), or the patient has progressed within 12 months (for instance, within 6 months) after completing a chemotherapy regimen.
- platinum-resistant cancer cancer in a patient that has progressed while receiving platinum-based chemotherapy (i.e., the patient is “platinum refractory"), or the patient has progressed within 12 months (for instance, within 6 months) after completing a platinum-based chemotherapy regimen.
- radiation therapy is meant the use of directed gamma rays or beta rays to induce sufficient damage to a cell so as to limit its ability to function normally or to destroy the cell altogether. It will be appreciated that there will be many ways known in the art to determine the dosage and duration of treatment. Typical treatments are given as a one-time administration and typical dosages range from 10 to 200 units (Grays) per day.
- Clinical benefit can be measured by assessing various endpoints, e.g., inhibition, to some extent, of disease progression, including slowing down and complete arrest; reduction in the number of disease episodes and/or symptoms; reduction in lesion size; inhibition (i.e., reduction, slowing down or complete stopping) of disease cell infiltration into adjacent peripheral organs and/or tissues; inhibition (i.e.
- the invention herein provides methods for treating patients with a type of cancer that is able to respond to a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab), involving administering a therapeutically effective amount of the antagonist to the patient, wherein the patient's cancer has been determined to express CD31 MVD and/or tumor VEGFA at a level more than the median level for CD31 MVD and/or tumor VEGFA expression in the cancer type.
- the patient's cancer has been determined to express CD31 MVD and/or tumor VEGFA at a level which is more than the 50 th percentile, most preferably greater than the 75 th percentile for CD31 and/or tumor VEGFA expression in the cancer type.
- the invention provides methods for treating patients with a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., MBC), involving administering a therapeutically effective amount of a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab) to the patient, wherein the patient's cancer has been determined to express CD31 MVD at a level more than the median level for CD31 MVD expression in the cancer, and/or wherein the patient's cancer sample has been determined to express CD31 MVD at a level which is greater than the 75 th percentile for CD31 expression the cancer, and/or expresses tumor VEGFA at a level that is greater than the median level, and/or wherein the patient's cancer sample has been determined to express tumor VEGFA at a level which is greater than the 75 th percentile for tumor VEG
- the invention provides methods for selecting a therapy for patients with a type of cancer that is able to respond to the administration of a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab), optionally in combination with one or more additional chemotherapeutic agents, involving determining CD31 MVD and/or tumor VEGFA expression in a cancer sample from the patient and selecting a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab) if the cancer sample has been determined to have CD31 MVD and/or express tumor VEGFA at a level greater than the median level for CD31 MVD and/or tumor VEGFA expression in the cancer type.
- a VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- the cancer type is a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., MBC), including platinum-resistant and/or advanced, refractory and/or recurrent forms thereof.
- the chemotherapeutic agent(s) can optionally be carboplatin and/or paclitaxel.
- cancer types that can be treated with a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab) are listed in the definition section, above.
- Preferred cancer types include gynecologic cancers (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, and vulvar cancer).
- the cancer that is treated is advanced, refractory, recurrent, chemotherapy-resistant, and/or platinum-resistant cancer.
- a VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- one or more chemotherapeutic agents e.g., carboplatin and/or paclitaxel
- therapy with the VEGF antagonist extends survival at least about 20% more than survival achieved by administering an approved anti-tumor agent, or standard of care, for the cancer being treated.
- the patient has a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., MBC).
- a gynecologic cancer e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer
- breast cancer e.g., MBC
- the patient may optionally have an advanced, refractory, recurrent, chemotherapy-resistant, and/or platinum-resistant form of the cancer.
- the VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- one or more chemotherapeutic agents e.g., carboplatin and/or paclitaxel
- intravenous administration e.g., as a bolus or by continuous infusion over a period of time, by intramuscular, intraperitoneal, intracerobrospinal, subcutaneous, intra-articular, intrasynovial, intrathecal, oral, topical, or inhalation routes.
- Intravenous administration of the antibody is preferred.
- VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- chemotherapeutic agent will depend on the type of cancer to be treated, as defined above, the severity and course of the cancer, whether the antibody is administered for preventive or therapeutic purposes, previous therapy, the patient's clinical history and response to the drug, and the discretion of the attending physician.
- VEGF antagonist e.g., bevacizumab
- a fixed dose of the VEGF antagonist is administered.
- the fixed dose may suitably be administered to the patient at one time or over a series of treatments. Where a fixed dose is administered, preferably it is in the range from about 20 mg to about 2000 mg of the inhibitor.
- the fixed dose may be approximately 420 mg, approximately 525 mg, approximately 840 mg, or approximately 1050 mg of the inhibitor (e.g., an anti-VEGF antibody, such as bevacizumab).
- a series of doses are administered, these may, for example, be administered approximately every week, approximately every 2 weeks, approximately every 3 weeks, or approximately every 4 weeks, but preferably approximately every 3 weeks.
- the fixed doses may, for example, continue to be administered until disease progression, adverse event, or other time as determined by the physician. For example, from about two, three, or four, up to about 17 or more fixed doses may be administered.
- one or more loading dose(s) of the VEGF antagonist are administered, followed by one or more maintenance dose(s).
- a plurality of the same dose is administered to the patient.
- a fixed dose of a VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- a fixed dose of a VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- loading dose is administered, followed by one or more doses of approximately 420 mg (maintenance dose(s)) of the antagonist.
- the maintenance doses are preferably administered about every 3 weeks, for a total of at least two doses, up to 17 or more doses.
- one or more fixed dose(s) of approximately 1050 mg of the VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- the VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- one, two or more of the fixed doses are administered, e.g., for up to one year (17 cycles), and longer as desired.
- a fixed dose of approximately 1050 mg of the VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- a loading dose is administered as a loading dose
- one or more maintenance dose(s) of approximately 525 mg.
- About one, two, or more maintenance doses may be administered to the patient every 3 weeks according to this embodiment.
- VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- chemotherapeutic agent may be administered as a single anti-tumor agent
- the patient is optionally treated with a combination of the inhibitor (or chemotherapeutic agent), and one or more (additional) chemotherapeutic agent(s).
- chemotherapeutic agents herein include: gemcitabine, carboplatin, oxaliplatin, irinotecan, fluoropyrimidine (e.g., 5-FU), paclitaxel (e.g., nab-paclitaxel), docetaxel, topotecan, capecitabine, temozolomide, interferon-alpha, and/or liposomal doxorubicin (e.g., pegylated liposomal doxorubicin).
- at least one of the chemotherapeutic agents is carboplatin or paclitaxel.
- the combined administration includes co-administration or concurrent administration, using separate formulations or a single pharmaceutical formulation, and consecutive administration in either order, wherein preferably there is a time period while both (or all) active agents simultaneously exert their biological activities.
- the chemotherapeutic agent may be administered prior to, or following, administration of the VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab).
- the timing between at least one administration of the chemotherapeutic agent and at least one administration of the VEGF antagonist is preferably approximately 1 month or less, and most preferably approximately 2 weeks or less.
- the chemotherapeutic agent and the inhibitor are administered concurrently to the patient, in a single formulation or separate formulations.
- Treatment with the combination of the chemotherapeutic agent (e.g., carboplatin and/or paclitaxel) and the VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab) may result in a synergistic, or greater than additive, therapeutic benefit to the patient.
- chemotherapeutic agents for combining with the VEGF antagonist include: a chemotherapeutic agent such as a platinum compound (e.g., carboplatin), a taxol such as paclitaxel or docetaxel, topotecan, or liposomal doxorubicin.
- a chemotherapeutic agent such as a platinum compound (e.g., carboplatin), a taxol such as paclitaxel or docetaxel, topotecan, or liposomal doxorubicin.
- chemotherapeutic agents for combining with the VEGF antagonist include: chemotherapeutic agents such as carboplatin and paclitaxel.
- chemotherapeutic agents for combining with the VEGF antagonist include: chemotherapeutic agents such as carboplatin and gemcitabine.
- chemotherapeutic agents for combining with the VEGF antagonist include: a chemotherapeutic agent such as paclitaxel, topotecan, or pegylated liposomal doxorubicin.
- chemotherapeutic agents for combining with the VEGF antagonist include: chemotherapeutic agents such as capecitabine, and a taxol such as paclitaxel (e.g., nab-paclitaxel) or docetaxel.
- chemotherapeutic agents for combining with the VEGF antagonist include: chemotherapeutic agents such as temozolomide, optionally in combination with radiotherapy.
- chemotherapeutic agents for combining with the VEGF antagonist include: chemotherapeutic agents such as a fluoropyrimidine (e.g., 5-FU), paclitaxel, cisplatin, topotecan, irinotecan, fluoropyrimidine-oxaliplatin, fluoropyrimidine-irinotecan, FOLFOX4 (5-FU, lecovorin, oxaliplatin), and IFL (ironotecan, 5-FU, leucovorin).
- chemotherapeutic agents such as a fluoropyrimidine (e.g., 5-FU), paclitaxel, cisplatin, topotecan, irinotecan, fluoropyrimidine-oxaliplatin, fluoropyrimidine-irinotecan, FOLFOX4 (5-FU, lecovorin, oxaliplatin), and IFL (ironotecan, 5-FU, leucovorin).
- chemotherapeutic agents for combining with the VEGF antagonist include: chemotherapeutic agents such as interferon-alpha2a.
- chemotherapeutic agents for combining with the VEGF antagonist include: chemotherapeutic agents such as paclitaxel, cisplatin, topotecan, paclitaxel in combination with cisplatin, and paclitaxel in combination with topotecan.
- a chemotherapeutic agent if administered, is usually administered at dosages known therefore, or optionally lowered due to combined action of the drugs or negative side effects attributable to administration of the chemotherapeutic agent. Preparation and dosing schedules for such chemotherapeutic agents may be used according to manufacturers' instructions or as determined empirically by the skilled practitioner. Where the chemotherapeutic agent is paclitaxel, preferably, it is administered at a dose between about 130 mg/m 2 to 200 mg/m 2 (for example approximately 175 mg/m 2 ), for instance, over 3 hours, once every 3 weeks.
- the chemotherapeutic agent is carboplatin
- it is administered by calculating the dose of carboplatin using the Calvert formula which is based on a patient's preexisting renal function or renal function and desired platelet nadir. Renal excretion is the major route of elimination for carboplatin.
- the use of this dosing formula as compared to empirical dose calculation based on body surface area, allows compensation for patient variations in pretreatment renal function that might otherwise result in either underdosing (in patients with above average renal function) or overdosing (in patients with impaired renal function).
- the target AUC of 4-6 mg/mL/min using single agent carboplatin appears to provide the most appropriate dose range in previously treated patients.
- VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- chemotherapeutic agent other therapeutic regimens may be combined therewith.
- a second (third, fourth, etc.) chemotherapeutic agent(s) may be administered, wherein the second chemotherapeutic agent is an antimetabolite chemotherapeutic agent, or a chemotherapeutic agent that is not an antimetabolite.
- the second chemotherapeutic agent may be a taxane (such as paclitaxel or docetaxel), capecitabine, or platinum-based chemotherapeutic agent (such as carboplatin, cisplatin, or oxaliplatin), anthracycline (such as doxorubicin, including, liposomal doxorubicin), topotecan, pemetrexed, vinca alkaloid (such as vinorelbine), and TLK 286. "Cocktails" of different chemotherapeutic agents may be administered.
- a taxane such as paclitaxel or docetaxel
- capecitabine or platinum-based chemotherapeutic agent
- platinum-based chemotherapeutic agent such as carboplatin, cisplatin, or oxaliplatin
- anthracycline such as doxorubicin, including, liposomal doxorubicin
- topotecan pemetrexed
- VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- chemotherapeutic agent include any one or more of: a HER inhibitor, HER dimerization inhibitor (for example, a growth inhibitory HER2 antibody such as trastuzumab, or a HER2 antibody which induces apoptosis of a HER2-overexpressing cell, such as 7C2, 7F3 or humanized variants thereof); an antibody directed against a different tumor associated antigen, such as EGFR, HER3, HE R4; anti-hormonal compound, e.g., an anti-estrogen compound such as tamoxifen, or an aromatase inhibitor; a cardioprotectant (to prevent or reduce any myocardial dysfunction associated with the therapy); a cytokine; an EGFR-targeted drug (such as TARCEVA® IRESSA® or cetuximab); a tyrosine kina
- a HER inhibitor for example,
- Suitable dosages for any of the above-noted co-administered agents are those presently used and may be lowered due to the combined action (synergy) of the agent and inhibitor.
- the patient may be subjected to surgical removal of tumors and/or cancer cells, and/or radiation therapy.
- the administered antibody is a naked antibody.
- the VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- administered may be conjugated with a cytotoxic agent.
- the conjugated and/or antigen to which it is bound is/are internalized by the cell, resulting in increased therapeutic efficacy of the conjugate in killing the cancer cell to which it binds.
- the cytotoxic agent targets or interferes with nucleic acid in the cancer cell. Examples of such cytotoxic agents include maytansinoids, calicheamicins, ribonucleases, and DNA endonucleases.
- the VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- the VEGF antagonist can be administered by gene therapy. See, for example, WO 96/07321 published Mar. 14, 1996 concerning the use of gene therapy to generate intracellular antibodies.
- nucleic acid (optionally contained in a vector) into the patient's cells; in vivo and ex vivo.
- the nucleic acid is injected directly into the patient, usually at the site where the antibody is required.
- the patient's cells are removed, the nucleic acid is introduced into these isolated cells and the modified cells are administered to the patient either directly or, for example, encapsulated within porous membranes which are implanted into the patient (see, e.g. U.S. Pat. Nos. 4,892,538 and 5,283,187 ).
- the techniques vary depending upon whether the nucleic acid is transferred into cultured cells in vitro, or in vivo in the cells of the intended host.
- nucleic acid transfer techniques suitable for the transfer of nucleic acid into mammalian cells in vitro include the use of liposomes, electroporation, microinjection, cell fusion, DEAE-dextran, the calcium phosphate precipitation method, etc.
- a commonly used vector for ex vivo delivery of the gene is a retrovirus.
- the currently preferred in vivo nucleic acid transfer techniques include transfection with viral vectors (such as adenovirus, Herpes simplex I virus, or adeno-associated virus) and lipid-based systems (useful lipids for lipid-mediated transfer of the gene are DOTMA, DOPE and DC-Chol, for example).
- the nucleic acid source with an agent that targets the target cells, such as an antibody specific for a cell surface membrane protein or the target cell, a ligand for a receptor on the target cell, etc.
- an agent that targets the target cells such as an antibody specific for a cell surface membrane protein or the target cell, a ligand for a receptor on the target cell, etc.
- proteins which bind to a cell surface membrane protein associated with endocytosis may be used for targeting and/or to facilitate uptake, e.g. capsid proteins or fragments thereof tropic for a particular cell type, antibodies for proteins which undergo internalization in cycling, and proteins that target intracellular localization and enhance intracellular half-life.
- the technique of receptor-mediated endocytosis is described, for example, by Wu et al., J. Biol. Chem.
- the present invention provides methods for improving the progression-free survival (PFS) and overall survival (OS) of patients suffering from cancer (e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer), or breast cancer (e.g., MBC; also see below)), by treatment with a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab), optionally in combination with a chemotherapy regimen.
- cancer e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer), or breast cancer (e.g., MBC; also see below)
- a VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- the invention also provides methods of identifying a patient suffering from a cancer (e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., metastatic breast cancer (MBC); also see below)) who may benefit from administration of a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab), optionally in combination with a chemotherapy regiment.
- a cancer e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., metastatic breast cancer (MBC); also see below)
- a VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- VEGF antagonists e.g., an anti-VEGF antibody, such as bevacizumab
- a chemotherapy regimen e.g., carboplatin and/or paclitaxel
- the present invention further provides for methods for assessing the sensitivity or responsiveness of a patient to a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab), optionally in combination with a chemotherapy regimen, by determining the expression level of one or more of CD31 and/or tumor VEGFA relative to control levels in patients diagnosed with cancer (e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer), or breast cancer (e.g., metastatic breast cancer (MBC); also see below)).
- cancer e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer)
- breast cancer e.g., metastatic breast cancer (MBC); also see below
- the present invention further provides methods of prognosis of a patient suffering from cancer (e.g., a gynecologic caner (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., metastatic breast cancer (MBC); also see below)) by determining the expression level of CD31 and/or tumor VEGFA in a sample obtained from the patient, comparing the level of CD31 MVD and/or tumor expression VEGFA to the median level for CD31 MVD and/or tumor VEGFA expression, respectively, in the cancer type, and determining a prognosis for the patient.
- cancer e.g., a gynecologic caner (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., metastatic breast cancer (MBC); also see below)
- a poor prognosis is when expression of CD31 MVD and/or tumor VEGFA is at a level more than the median level for CD31 and/or tumor VEGFA expression.
- the methods optionally include the step of identifying the patient as likely to benefit from administration of a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab) when the patient is determined to have a poor prognosis of survival, and further optionally include the step of administering a VEGF antagonist (e.g., an anti-VEGF antibody, such as bevacizumab) in a therapeutically effective amount to the patient, if the patient is determined to have a poor prognosis.
- a VEGF antagonist e.g., an anti-VEGF antibody, such as bevacizumab
- the present invention relates to the identification, selection, and use of biomarkers of cancer (e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., MBC; also see above)) that associate with sensitivity or responsiveness to angiogenesis inhibitors, e.g., VEGF antagonists (e.g., anti-VEGF antibodies, such as bevacizumab), optionally in combination with chemotherapeutic regimens, such as carboplatin-based chemotherapies.
- a gynecologic cancer e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer
- breast cancer e.g., MBC; also see above
- angiogenesis inhibitors e.g., VEGF antagonists (e.g., anti-VE
- the invention relates to the use of (a) tumor specific expression profile(s) of one or more of CD31 and/or tumor VEGFA relative to controls (e.g., the median) established in patients diagnosed with cancer (e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., MBC; also see above)), to identify patients sensitive or responsive to the addition of angiogenesis inhibitors, for example, VEGF antagonists (e.g., anti-VEGF antibodies, such as bevacizumab), to standard chemotherapies.
- cancer e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., MBC; also see above)
- angiogenesis inhibitors for example
- the invention further relates to methods for improving PFS and/or OS of a patient suffering from cancer (e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer) or breast cancer (e.g., MBC; also see above)), by the addition of angiogenesis inhibitors, for example, VEGF antagonists (e.g., anti-VEGF antibodies, such as bevacizumab), to standard chemotherapies, e.g., carboplatin- and/or paclitaxel-based chemotherapies, by determining (a) tumor specific expression level(s) of one or more of CD31 and/or tumor VEGFA relative to control(s) (e.g., the median) in patients diagnosed with cancer (e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometri
- the expression level of CD31 and/or tumor VEGFA may be assessed by any method known in the art suitable for determination of specific protein levels in a patient sample, and is preferably determined by an immunohistochemical ("IHC") method employing antibodies specific for CD31 and/or tumor VEGFA.
- IHC immunohistochemical
- Such methods are well known and routinely implemented in the art, and corresponding commercial antibodies and/or kits are readily available.
- commercially available antibodies/test kits for VEGFA and CD31 can be obtained from Abcam, Inc. (Cambridge, Mass., U.S.A.) as clone SP28, and from Dako A/S (Glostrup, Denmark), as clone JC70A, respectively.
- the expression levels of the marker/indicator proteins of the invention are assessed using the reagents and/or protocol recommendations of the antibody or kit manufacturer.
- the skilled person will also be aware of further means for determining the expression level of CD31 and/or tumor VEGFA by IHC methods. Therefore, the expression level of one or more of the markers/indicators of the invention can be routinely and reproducibly determined by a person skilled in the art without undue burden.
- the invention also encompasses the testing of patient samples in a specialized laboratory that can ensure the validation of testing procedures.
- the expression level of CD31 and/or tumor VEGFA is assessed in a biological sample that contains or is suspected to contain cancer cells.
- the sample may be, for example, an ovarian tissue resection, an ovarian tissue biopsy, or a metastatic lesion obtained from a patient suffering from, suspected to suffer from, or diagnosed with cancer (e.g., a gynecologic cancer, in particular ovarian cancer).
- the sample is a sample of ovarian tissue, a resection or biopsy of an ovarian tumor, a known or suspected metastatic ovarian cancer lesion or section, or a blood sample, e.g., a peripheral blood sample, known or suspected to comprise circulating cancer cells, e.g., ovarian cancer cells.
- the sample may comprise both cancer cells, i.e., tumor cells, and non-cancerous cells, and, in certain embodiments, comprises both cancerous and non-cancerous cells.
- the sample comprises both cancer/tumor cells and non-cancerous cells that are endothelial cells.
- a pathologist can readily discern cancer cells from non-cancerous, e.g., endothelial cells, as well as determine vessel number within a sample, e.g., by staining the sample for detection of an endothelial cell marker, e.g., CD31.
- the expression level of one or more endothelial cell markers may also be determined, which level correlates with vessel number.
- Methods of obtaining biological samples including tissue resections, biopsies, and body fluids, e.g., blood samples comprising cancer/tumor cells are well known in the art.
- the sample obtained from the patient is collected prior to beginning any chemotherapeutic regimen or therapy, e.g., therapy for the treatment of cancer or the management or amelioration of a symptom thereof. Therefore, in some embodiments, the sample is collected before the administration of chemotherapeutics or the start of a chemotherapy regimen.
- the invention also encompasses further immunohistochemical methods for assessing the expression level of one or more of tumor CD31 and/or tumor VEGFA, such as by Western blotting and ELISA-based detection. Similar methods may be employed in alternative or additional methods for the determination of vessel number, including the determination of tumor specific expression level of one or more endothelial cell markers, e.g., CD31. As is understood in the art, the expression level of the marker/indicator proteins of the invention may also be assessed at the mRNA level by any suitable method known in the art, such as Northern blotting, real time PCR, and RT PCR.
- Immunohistochemical- and mRNA-based detection methods and systems are well known in the art and can be deduced from standard textbooks, such as Lottspeich ( Bioanalytik, Spektrum Akademisher Verlag, 1998 ) or Sambrook and Russell (Molecular Cloning: A Laboratory Manual, CSH Press, Cold Spring Harbor, N.Y., U.S.A., 2001 ).
- the described methods are of particular use for determining the expression levels of CD31 and/or tumor VEGFAin a patient or group of patients relative to control levels established in a population diagnosed with advanced stages of a cancer (e.g., a gynecologic cancer, such as ovarian cancer).
- the expression level of one or more of VEGFA and/or one or more endothelial cell markers, e.g., CD31 can also be determined on the protein level by taking advantage of immunoagglutination, immunoprecipitation (e.g., immunodiffusion, immunelectrophoresis, immune fixation), western blotting techniques (e.g., (in situ) immuno histochemistry, (in situ) immuno cytochemistry, affinitychromatography, enzyme immunoassays), and the like. Amounts of purified polypeptide in solution may also be determined by physical methods, e.g. photometry. Methods of quantifying a particular polypeptide in a mixture usually rely on specific binding, e.g., of antibodies.
- the expression level of the marker/indicator proteins according to the present invention may also be reflected in a decreased expression of the corresponding gene(s) encoding the VEGFA and/or one or more endothelial cell markers, e.g., CD31, for determination of vessel number as described herein. Therefore, a quantitative assessment of the gene product prior to translation (e.g. spliced, unspliced or partially spliced mRNA) can be performed in order to evaluate the expression of the corresponding gene(s).
- spliced, unspliced or partially spliced mRNA can be performed in order to evaluate the expression of the corresponding gene(s).
- hybridization probes for use in detecting mRNA levels and/or antibodies or antibody fragments for use in IHC methods can be labelled and visualized according to standard methods known in the art.
- Non-limiting examples of commonly used systems include the use of radiolabels, enzyme labels, fluorescent tags, biotin-avidin complexes, chemiluminescence, and the like.
- the vessel number in a tumor sample can be determined as a biomarker and an indicator of a patient sensitive or responsive to angiogenesis inhibitors, for example, VEGF antagonists (e.g., anti-VEGF antibodies, such as bevacizumab), optionally in addition to standard chemotherapies.
- cancer e.g., a gynecologic cancer (e.g., ovarian, peritoneal, fallopian tube, cervical, endometrial, vaginal, or vulvar cancer), or breast cancer (e.g., MBC; also see above)
- VEGF antagonists e.g., anti-VEGF antibodies, such as bevacizumab
- Tumor tissue samples were collected from patients with newly diagnosed, previously untreated, suboptimal advanced stage epithelial ovarian and primary peritoneal cancer, and participating in a phase III trial of carboplatin and paclitaxel plus placebo (CPP), versus carboplatin and paclitaxel plus concurrent bevacizumab followed by placebo (CPB15), versus carboplatin and paclitaxel plus concurrent and extended bevacizumab (CPT15+) ( Fig. 1 ).
- the intended to treat (ITT) population analysis included 1,852 patients and the biomarker evaluable population (BEP) population analysis included 1,438 patients.
- the BEP population includes all subjects who were randomized and having non-missing biomarker data at baseline.
- the non-biomarker population is defined as a complement to the biomarker evaluable population.
- the BEP includes patients with non-missing CD31 RNA data.
- Key demographics and baseline characteristics (including stratification variables and any variables with known prognostic significance) and efficacy outcomes were summarized by treatment groups and compared between biomarker and intended to treat (ITT) populations to investigate any potential selection biases associated with the missing status of the biomarker.
- ITT intended to treat
- ITT vs. BEP Patient Demographics CPP CPB15 CPB15+ ITT TCD31NV ITT TCD31NV ITT TCD31NV GOG Performance Status Total 625 483 625 463 623 492 0 311 (49.76%) 234 (48.45%) 314 (50.24%) 242 (52.27%) 307 (49.28%) 246(50%) 1 or 2 314 (50.24%) 249 (51.55%) 311 (49.76%) 221 (47.73%) 316 (50.72%) 246(50%) Stage Total 625 483 625 463 623 492 Stage III Optimally Debulked 219 (35.04%) 163 (33.75%) 204 (32.64%) 152 (32.83%) 216 (34.67%) 165 (33.54%) Stage III Sub-optimally Debulked 253 (40.48%) 200 (41.41%) 256 (40.96%) 183 (39.52%) 24
- CD31 Immunohistochemical staining of CD31 was used for detecting blood vessels.
- CD31 stains endothelium from different types of vessels, including lymphatic vessels and hepatic sinusoidal endothelial cells.
- the shape of the CD31-stained structures ranges from thread-like (longitudinal sectioned capillaries) to single cell-like (cross-sectioned capillaries).
- the immunohistochemical detection of CD31 (PECAM-1) was carried out using the Ventana Benchmark@ XT platform (Ventana, Arlington, Ariz. USA). Detection of CD31 was developed by using a mouse monoclonal antibody (Clone 1A10) from Ventana.
- Immunohistochemistry is a semi-quantitative method used to detect presence or absence of a target antigen (e.g., CD31) in tissue, in this case formalin-fixed, paraffin-embedded tissue.
- a target antigen e.g., CD31
- protocol number 91 using the ultra view TM Universal DAB detection kit was used.
- antigen retrieval was performed by 32 minutes of anti-CD31 antibody incubation at 37°C.
- Validation reports showing accuracy, specificity, linearity, and precision (reproducibility and repeatability) were prepared for each IHC assay. Staining of external control slides and intrinsic control elements was documented. These methods are described in more detail, as follows.
- CD31 vascular staining was evaluated by determination of the number of vessels (# per mm 2 ) and the volume fraction (as %) of the vessels in fixed tissue samples. Generally, a stereology-based method was used for systematically uniform random sampling of fields to score for the CD31 stainings. A minimum of three regions of interest (ROIs) were selected with a maximum of 15 ROIs at 20x magnification or at 40x magnification.
- ROIs regions of interest
- Grids were placed on top of the images to allow evaluation.
- the selected ROI images were then combined with the predefined grids.
- the volume fraction was estimated by counting the grid points, formed by the crossing lines of the counting grid that fall on top of the tissue, cells, or structures of interest. This fraction was representative for the volume density of the tissue, cells, or structures of interest. Typically, only the top right corner of a cross (or grid point) was considered. Grid points that lie within obvious tissue tears or outside the tumor tissue were not counted. Small necrotic zones within tumor structures were counted because they were considered a part of the tumor. Grid points that lie within the vascular lumen were also counted. Only grids in which >75% of the area consists of tissue (e.g., ⁇ 19 out of 25 grid points or ⁇ 61 out of 81 grid points), were analyzed. If this was not the case, the region was omitted from the analysis.
- a grid point was counted for Vvessel (the amount of grid points that represent vessels) when a stained endothelial cell or the vessel lumen was found to lie within the top right grid point corner.
- Vvessel the amount of grid points that represent vessels
- all other endothelial cells that made up this vessel were counted for Vvessel when they filled the top right corner of a grid point.
- a grid point was counted for V (the amount of grid points that represent other cell populations or structures) when a stained cell or structure of interest filled up the top right grid point corner. Since other cell populations or structures of interest can vary depending on the staining, the other cells or structures counted for V were defined in the scoring form.
- N number of vessels
- the outer borders of the raster grid delineate the counting chamber that has a given area.
- Vascular structures that cross the left or bottom line of the grid were not counted. If a vascular structure that was only stained within the grid but clearly the vessels crossed the border, it was not counted. In tissue sections, vessels with a clear lumen were counted. Stained structures without lumina that have a vascular appearance were also counted. For some staining assays, a further distinction between weak and strong staining intensity was required.
- the immunohistochemical detection of tumor VEGFA was carried out using the Autostainer and PT-module instruments.
- the primary antibody used to detect tumor VEGFA was R547 (abcam-ab27620 (HGX-R547).
- the antibody is a prediluted rabbit monoclonal antibody (SP28) raised against the N-terminal part of human VEGFA.
- SP28 rabbit monoclonal antibody
- the immunogen sequence used shares about 30-40% identity to other VEGF isoforms including VEGF-B, VEGF-C, and VEGF-D. Paraffin embedded tissues were stained for tumor VEGFA by following the HistoGeneX staining protocol.
- the lowest positivity that is dectected/scored was a pre-set detection limit which was determined by a specific scoring system and was set as 1% of cells that stain with the weakest staining intensity 1+, further described below. To ensure that the staining was performed in a linear area, experiments were not performed with different concentrations of the primary antibody.
- the N-universal negative control rabbit IgG from Dako (N1699) was used as a negative control.
- the IgG control was checked for VEGFA immunoreactivity and was VEGFA negative, whereas the positive samples showed clear and intense cytoplasmic VEGFA positivity in the tumor cells and in syncitiotrophoblast in human placenta. Only one negative external control per staining run was performed.
- the tumor VEGFA stainings were evaluated using a system in which the percentage of cells showing membrane, cytoplasmic, or nuclear staining were scored in combination with their staining intensity. Final results were extracted from the scoring matrix and reported.
- the part of the tissue needed to be evaluated was determined, for example, invasive part of the tumor, entire tumor, carcinoma in situ, etc.
- the cell compartment needed to be scored was determined (e.g., membrane, cytoplasmic, or nuclear). In general, the cell compartments were scored separately.
- the pattern of full basolateral or complete staining was also reported.
- the proportion (percentage) of staining was scored.
- the maximum percentage of all intensities together i.e., the sum of all percentages at all intensities
- the rule of thumb to assign intensity and percentages of the staining is: a) identify the most dominant staining intensity and assign a certain % to it; b) define the % of the lowest staining; c) divide the rest of the % between the lowest and the highest category; d) when staining positivity is between 0 and 10% accuracy of 1% is recommended; e) when staining positivity is more than 10%, accuracy of 5% is recommended.
- the number of fields scored was selected to be optimal (for large tissue samples a minimum of 10 ROI's is recommended) and selected systematically uniform random according to the stereology-based random sample method.
- the percentage of tumor cells showing each of membrane staining, cytoplasmic staining, and nuclear staining were scored using the 0, 1+, 2+, 3+ scale, and with the total being 100%.
- additional scores for the characterization of the staining pattern were also used, for example, the completeness of membrane staining.
- membrane percentage was scored, the percentage of full basolateral or complete membrane staining was estimated for each intensity.
- Full basolateral staining is only seen in well-differentiated adenocarcinoma.
- Full basolateral staining refers to the staining of the base and two sides of the cells.
- H-score for the H-score, the percentage is multiplied by the staining intensity.
- the highest H-score produced is 300.
- IHC tumor tissue immunohistochemical
- the hazard ratios indicate that patient subgroups having high levels of CD31 and/or tumor VEGFA (i.e., above median or above a 50% cutoff) gained benefit from bevacizumab treatment, whereas patient subgroups having low levels of CD31 and/or tumor VEGFA (i.e., below median or below a 50% cutoff) did not benefit with the addition of bevacizumab ( Fig. 7 ).
- the STEPP analysis shown in Fig. 11 uses a slide window approach to demonstrate the association of CD31 expression level with hazard ratios for PFS and OS.
- the hazard ratios for patients included in each subgroup were below 1.0, indicating that all patients derive some benefit from bevacizumab treatment.
- patients expressing high levels of CD31 the top 50% of the CD31 expression
- the hazard ratio for patients above -75% of the CD31 expression range were below 1.0, indicating that the greater benefit is seen only in patients above -75% of the CD31 expression range.
- Quartile analysis of treatment effects on PFS in patient subgroups based on % cutoff confirmed that, in general, patients with high levels of tumor VEGFA expression (i.e., above the specified % cutoff) benefited from treatment with bevacizumab ( Fig. 15 ).
- Quartile analysis of treatment effects on OS in patient subgroups based on % cutoff showed that high levels of tumor VEGFA expression, particularly in the 50% and 75% cutoff resulted in a marked improvement in OS when treated with bevacizumab ( Fig. 16 ).
- the STEPP analysis shown in Fig. 17 uses a slide window approach to demonstrate the association of tumor VEGFA expression level with hazard ratios for PFS and OS.
- the hazard ratios for patients included in each subgroup represented by middle solid line were below 1.0, indicating that all patients derive some benefit from bevacizumab treatment.
- OS the hazard ratio for patients above -75% of the tumor VEGFA expression range (represented by middle solid line) was below 1.0, indicating a greater benefit above -75% of the tumor VEGFA expression range ( Fig. 17 ).
- slide-window analysis suggested a higher optimal tumor VEGFA cutoff for PFS than for OS. Together, these results suggest that tumor VEGFA can serve as a predictive biomarker for improved PFS and OS and increased bevacizumab efficacy in ovarian cancer.
Landscapes
- Health & Medical Sciences (AREA)
- Life Sciences & Earth Sciences (AREA)
- Chemical & Material Sciences (AREA)
- Medicinal Chemistry (AREA)
- General Health & Medical Sciences (AREA)
- Public Health (AREA)
- Animal Behavior & Ethology (AREA)
- Veterinary Medicine (AREA)
- Pharmacology & Pharmacy (AREA)
- Epidemiology (AREA)
- Engineering & Computer Science (AREA)
- Immunology (AREA)
- Organic Chemistry (AREA)
- Bioinformatics & Cheminformatics (AREA)
- Molecular Biology (AREA)
- Proteomics, Peptides & Aminoacids (AREA)
- Biomedical Technology (AREA)
- Chemical Kinetics & Catalysis (AREA)
- General Chemical & Material Sciences (AREA)
- Nuclear Medicine, Radiotherapy & Molecular Imaging (AREA)
- Biochemistry (AREA)
- Microbiology (AREA)
- Oncology (AREA)
- Urology & Nephrology (AREA)
- Gastroenterology & Hepatology (AREA)
- Zoology (AREA)
- Genetics & Genomics (AREA)
- Biophysics (AREA)
- Mycology (AREA)
- Hematology (AREA)
- Inorganic Chemistry (AREA)
- Cell Biology (AREA)
- Physics & Mathematics (AREA)
- Pathology (AREA)
- Analytical Chemistry (AREA)
- Biotechnology (AREA)
- Food Science & Technology (AREA)
- Reproductive Health (AREA)
- General Physics & Mathematics (AREA)
- Hospice & Palliative Care (AREA)
Applications Claiming Priority (2)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US201462079787P | 2014-11-14 | 2014-11-14 | |
| PCT/US2015/059733 WO2016077227A2 (en) | 2014-11-14 | 2015-11-09 | Predicting response to a vegf antagonist |
Publications (2)
| Publication Number | Publication Date |
|---|---|
| EP3218401A2 EP3218401A2 (en) | 2017-09-20 |
| EP3218401B1 true EP3218401B1 (en) | 2020-03-04 |
Family
ID=54754748
Family Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP15802244.2A Active EP3218401B1 (en) | 2014-11-14 | 2015-11-09 | Predicting response to a vegf antagonist |
Country Status (15)
| Country | Link |
|---|---|
| US (1) | US20170226198A1 (ko) |
| EP (1) | EP3218401B1 (ko) |
| JP (1) | JP2017535548A (ko) |
| KR (1) | KR20170082537A (ko) |
| CN (1) | CN107106688A (ko) |
| AR (1) | AR102647A1 (ko) |
| AU (1) | AU2015346652A1 (ko) |
| BR (1) | BR112017009633A2 (ko) |
| CA (1) | CA2966216A1 (ko) |
| HK (1) | HK1242996A1 (ko) |
| IL (1) | IL251947A0 (ko) |
| MX (1) | MX2017006201A (ko) |
| RU (1) | RU2017120388A (ko) |
| SG (1) | SG11201703744VA (ko) |
| WO (1) | WO2016077227A2 (ko) |
Families Citing this family (3)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| CN108753984B (zh) * | 2018-08-28 | 2021-07-13 | 北京市神经外科研究所 | 预测或诊断脑恶性胶质瘤术后复发的生物标志物组合及其应用和试剂盒 |
| JPWO2021182572A1 (ko) * | 2020-03-12 | 2021-09-16 | ||
| WO2024028846A1 (en) * | 2022-08-05 | 2024-02-08 | Geistlich Pharma Ag | Combination therapy for treating cancers |
Family Cites Families (9)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| EP2277542B1 (en) * | 2001-06-01 | 2014-04-16 | Cornell Research Foundation Inc. | Modified antibodies to prostrate-specific membrane antigen and uses thereof |
| WO2003026581A2 (en) * | 2001-09-26 | 2003-04-03 | Intermune, Inc. | Pharmaceutical compositions and methods for treating cancer |
| CA2517074A1 (en) * | 2003-02-27 | 2004-09-10 | Yeda Research And Development Co., Ltd. | Nucleic acid molecules, polypeptides, antibodies and compositions containing same useful for treating and detecting influenza virus infection |
| JP2008502738A (ja) * | 2004-06-10 | 2008-01-31 | リジェネロン・ファーマシューティカルズ・インコーポレイテッド | ヒトの癌を処置するための、vegfインヒビターの使用 |
| CN104474545A (zh) * | 2010-01-19 | 2015-04-01 | 霍夫曼-拉罗奇有限公司 | 用于贝伐单抗联合疗法的基于肿瘤组织的生物标志 |
| MA34059B1 (fr) * | 2010-02-23 | 2013-03-05 | Genentech Inc | Thérapie anti-angiogénique pour le traitement du cancer des ovaires |
| SG187120A1 (en) * | 2010-07-19 | 2013-02-28 | Hoffmann La Roche | Method to identify a patient with an increased likelihood of responding to an anti-cancer therapy |
| MX2013006361A (es) * | 2010-12-09 | 2013-07-30 | Hoffmann La Roche | Agtr1 como marcador para terapias combinadas de bevacizumab. |
| WO2012118969A2 (en) * | 2011-03-01 | 2012-09-07 | The U.S.A., As Represented By The Secretary, Department Of Health And Human Services | Method of selecting cancer patients for anti-angiogenesis therapy in combination with chemotherapy |
-
2015
- 2015-11-09 SG SG11201703744VA patent/SG11201703744VA/en unknown
- 2015-11-09 AU AU2015346652A patent/AU2015346652A1/en not_active Abandoned
- 2015-11-09 MX MX2017006201A patent/MX2017006201A/es unknown
- 2015-11-09 RU RU2017120388A patent/RU2017120388A/ru not_active Application Discontinuation
- 2015-11-09 CN CN201580070085.3A patent/CN107106688A/zh active Pending
- 2015-11-09 WO PCT/US2015/059733 patent/WO2016077227A2/en active Application Filing
- 2015-11-09 KR KR1020177013270A patent/KR20170082537A/ko unknown
- 2015-11-09 BR BR112017009633A patent/BR112017009633A2/pt not_active IP Right Cessation
- 2015-11-09 EP EP15802244.2A patent/EP3218401B1/en active Active
- 2015-11-09 CA CA2966216A patent/CA2966216A1/en not_active Abandoned
- 2015-11-09 JP JP2017525946A patent/JP2017535548A/ja active Pending
- 2015-11-13 AR ARP150103707A patent/AR102647A1/es unknown
-
2017
- 2017-04-26 IL IL251947A patent/IL251947A0/en unknown
- 2017-04-28 US US15/581,448 patent/US20170226198A1/en not_active Abandoned
-
2018
- 2018-02-22 HK HK18102570.4A patent/HK1242996A1/zh unknown
Non-Patent Citations (1)
| Title |
|---|
| None * |
Also Published As
| Publication number | Publication date |
|---|---|
| US20170226198A1 (en) | 2017-08-10 |
| CN107106688A (zh) | 2017-08-29 |
| KR20170082537A (ko) | 2017-07-14 |
| RU2017120388A3 (ko) | 2019-05-30 |
| JP2017535548A (ja) | 2017-11-30 |
| WO2016077227A2 (en) | 2016-05-19 |
| EP3218401A2 (en) | 2017-09-20 |
| SG11201703744VA (en) | 2017-06-29 |
| AU2015346652A1 (en) | 2017-05-18 |
| RU2017120388A (ru) | 2018-12-14 |
| CA2966216A1 (en) | 2016-05-19 |
| HK1242996A1 (zh) | 2018-07-06 |
| WO2016077227A3 (en) | 2016-07-07 |
| AR102647A1 (es) | 2017-03-15 |
| IL251947A0 (en) | 2017-06-29 |
| BR112017009633A2 (pt) | 2017-12-19 |
| MX2017006201A (es) | 2017-07-31 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| US20220298576A1 (en) | Methods and compositions for prognosis and treatment of cancers | |
| RU2710735C2 (ru) | Композиции и способы лечения и диагностики резистентного к химиотерапии рака | |
| US11583577B2 (en) | Cancer immunotherapy by immune activation or immune modulation via Globo series antigens | |
| TWI619509B (zh) | 治療先前未經治療之ⅲ期或ⅳ期卵巢癌、輸卵管癌或原發性腹膜癌之卡鉑、太平洋紫杉醇與抗-vegf抗體之組合 | |
| EP2824457A1 (en) | Method to identify a patient with an increased likelihood of responding to an anti-cancer therapy | |
| JP2012505904A (ja) | 治療方法 | |
| US20170226198A1 (en) | Predicting response to a vegf antagonist | |
| KR20130121122A (ko) | 종양의 치료 방법 |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: THE INTERNATIONAL PUBLICATION HAS BEEN MADE |
|
| PUAI | Public reference made under article 153(3) epc to a published international application that has entered the european phase |
Free format text: ORIGINAL CODE: 0009012 |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: REQUEST FOR EXAMINATION WAS MADE |
|
| 17P | Request for examination filed |
Effective date: 20170614 |
|
| AK | Designated contracting states |
Kind code of ref document: A2 Designated state(s): AL AT BE BG CH CY CZ DE DK EE ES FI FR GB GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO RS SE SI SK SM TR |
|
| AX | Request for extension of the european patent |
Extension state: BA ME |
|
| DAV | Request for validation of the european patent (deleted) | ||
| DAX | Request for extension of the european patent (deleted) | ||
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: EXAMINATION IS IN PROGRESS |
|
| 17Q | First examination report despatched |
Effective date: 20181107 |
|
| GRAP | Despatch of communication of intention to grant a patent |
Free format text: ORIGINAL CODE: EPIDOSNIGR1 |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: GRANT OF PATENT IS INTENDED |
|
| RIC1 | Information provided on ipc code assigned before grant |
Ipc: A61K 31/513 20060101ALI20190902BHEP Ipc: A61K 31/282 20060101ALI20190902BHEP Ipc: A61K 31/4745 20060101ALI20190902BHEP Ipc: C07K 16/22 20060101AFI20190902BHEP Ipc: A61K 38/21 20060101ALI20190902BHEP Ipc: A61K 45/06 20060101ALI20190902BHEP Ipc: A61K 33/24 20190101ALI20190902BHEP Ipc: A61K 31/337 20060101ALI20190902BHEP Ipc: A61K 39/395 20060101ALI20190902BHEP Ipc: A61K 31/495 20060101ALI20190902BHEP Ipc: A61K 31/519 20060101ALI20190902BHEP Ipc: A61K 39/00 20060101ALI20190902BHEP Ipc: A61K 31/555 20060101ALI20190902BHEP Ipc: A61K 31/704 20060101ALI20190902BHEP Ipc: A61K 31/7068 20060101ALI20190902BHEP |
|
| INTG | Intention to grant announced |
Effective date: 20191001 |
|
| GRAS | Grant fee paid |
Free format text: ORIGINAL CODE: EPIDOSNIGR3 |
|
| GRAA | (expected) grant |
Free format text: ORIGINAL CODE: 0009210 |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: THE PATENT HAS BEEN GRANTED |
|
| AK | Designated contracting states |
Kind code of ref document: B1 Designated state(s): AL AT BE BG CH CY CZ DE DK EE ES FI FR GB GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO RS SE SI SK SM TR |
|
| REG | Reference to a national code |
Ref country code: GB Ref legal event code: FG4D |
|
| REG | Reference to a national code |
Ref country code: CH Ref legal event code: EP |
|
| REG | Reference to a national code |
Ref country code: AT Ref legal event code: REF Ref document number: 1240270 Country of ref document: AT Kind code of ref document: T Effective date: 20200315 |
|
| REG | Reference to a national code |
Ref country code: DE Ref legal event code: R096 Ref document number: 602015048258 Country of ref document: DE |
|
| REG | Reference to a national code |
Ref country code: IE Ref legal event code: FG4D |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: FI Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: NO Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200604 Ref country code: RS Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 |
|
| REG | Reference to a national code |
Ref country code: NL Ref legal event code: MP Effective date: 20200304 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: BG Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200604 Ref country code: GR Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200605 Ref country code: SE Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: LV Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: HR Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 |
|
| REG | Reference to a national code |
Ref country code: LT Ref legal event code: MG4D |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: NL Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: LT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: ES Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: IS Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200704 Ref country code: SK Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: RO Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: CZ Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: PT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200729 Ref country code: EE Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: SM Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 |
|
| REG | Reference to a national code |
Ref country code: AT Ref legal event code: MK05 Ref document number: 1240270 Country of ref document: AT Kind code of ref document: T Effective date: 20200304 |
|
| REG | Reference to a national code |
Ref country code: DE Ref legal event code: R097 Ref document number: 602015048258 Country of ref document: DE |
|
| PLBE | No opposition filed within time limit |
Free format text: ORIGINAL CODE: 0009261 |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: NO OPPOSITION FILED WITHIN TIME LIMIT |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: IT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: DK Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: AT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 |
|
| 26N | No opposition filed |
Effective date: 20201207 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: SI Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: PL Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 |
|
| REG | Reference to a national code |
Ref country code: DE Ref legal event code: R119 Ref document number: 602015048258 Country of ref document: DE |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: MC Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 |
|
| REG | Reference to a national code |
Ref country code: CH Ref legal event code: PL |
|
| GBPC | Gb: european patent ceased through non-payment of renewal fee |
Effective date: 20201109 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: LU Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20201109 |
|
| REG | Reference to a national code |
Ref country code: BE Ref legal event code: MM Effective date: 20201130 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: CH Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20201130 Ref country code: LI Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20201130 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: FR Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20201130 Ref country code: IE Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20201109 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: GB Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20201109 Ref country code: DE Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20210601 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: TR Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: MT Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: CY Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: MK Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 Ref country code: AL Free format text: LAPSE BECAUSE OF FAILURE TO SUBMIT A TRANSLATION OF THE DESCRIPTION OR TO PAY THE FEE WITHIN THE PRESCRIBED TIME-LIMIT Effective date: 20200304 |
|
| PG25 | Lapsed in a contracting state [announced via postgrant information from national office to epo] |
Ref country code: BE Free format text: LAPSE BECAUSE OF NON-PAYMENT OF DUE FEES Effective date: 20201130 |