JP5654584B2 - Correction connector for spine construction - Google Patents
Correction connector for spine construction Download PDFInfo
- Publication number
- JP5654584B2 JP5654584B2 JP2012516310A JP2012516310A JP5654584B2 JP 5654584 B2 JP5654584 B2 JP 5654584B2 JP 2012516310 A JP2012516310 A JP 2012516310A JP 2012516310 A JP2012516310 A JP 2012516310A JP 5654584 B2 JP5654584 B2 JP 5654584B2
- Authority
- JP
- Japan
- Prior art keywords
- extension
- bone
- extension system
- anchor
- rod
- Prior art date
- Legal status (The legal status is an assumption and is not a legal conclusion. Google has not performed a legal analysis and makes no representation as to the accuracy of the status listed.)
- Active
Links
- 238000012937 correction Methods 0.000 title description 12
- 238000010276 construction Methods 0.000 title description 9
- 210000000988 bone and bone Anatomy 0.000 claims description 200
- 239000007943 implant Substances 0.000 claims description 43
- 230000000149 penetrating effect Effects 0.000 claims description 5
- 238000004873 anchoring Methods 0.000 description 29
- 238000001356 surgical procedure Methods 0.000 description 14
- 238000000034 method Methods 0.000 description 13
- 125000006850 spacer group Chemical group 0.000 description 8
- 239000000463 material Substances 0.000 description 4
- 230000000295 complement effect Effects 0.000 description 3
- 230000006835 compression Effects 0.000 description 3
- 238000007906 compression Methods 0.000 description 3
- 239000012530 fluid Substances 0.000 description 3
- 230000004927 fusion Effects 0.000 description 3
- 238000002513 implantation Methods 0.000 description 3
- 238000012986 modification Methods 0.000 description 3
- 230000004048 modification Effects 0.000 description 3
- 239000004606 Fillers/Extenders Substances 0.000 description 2
- 208000002193 Pain Diseases 0.000 description 2
- 239000004696 Poly ether ether ketone Substances 0.000 description 2
- 238000013459 approach Methods 0.000 description 2
- 239000008280 blood Substances 0.000 description 2
- 210000004369 blood Anatomy 0.000 description 2
- 230000008878 coupling Effects 0.000 description 2
- 238000010168 coupling process Methods 0.000 description 2
- 238000005859 coupling reaction Methods 0.000 description 2
- 238000003780 insertion Methods 0.000 description 2
- 230000037431 insertion Effects 0.000 description 2
- 230000007246 mechanism Effects 0.000 description 2
- 229920002530 polyetherether ketone Polymers 0.000 description 2
- 238000003825 pressing Methods 0.000 description 2
- YZFVTGCKLQCIFB-UHFFFAOYSA-N C1C2C1CC(C1)C1C2 Chemical compound C1C2C1CC(C1)C1C2 YZFVTGCKLQCIFB-UHFFFAOYSA-N 0.000 description 1
- 229910001257 Nb alloy Inorganic materials 0.000 description 1
- 208000031481 Pathologic Constriction Diseases 0.000 description 1
- 208000004550 Postoperative Pain Diseases 0.000 description 1
- 238000004026 adhesive bonding Methods 0.000 description 1
- 210000003484 anatomy Anatomy 0.000 description 1
- 230000000712 assembly Effects 0.000 description 1
- 238000000429 assembly Methods 0.000 description 1
- 239000011324 bead Substances 0.000 description 1
- 238000005422 blasting Methods 0.000 description 1
- 230000003139 buffering effect Effects 0.000 description 1
- 210000000078 claw Anatomy 0.000 description 1
- 238000002316 cosmetic surgery Methods 0.000 description 1
- 238000013461 design Methods 0.000 description 1
- 239000013013 elastic material Substances 0.000 description 1
- 238000005516 engineering process Methods 0.000 description 1
- 238000000605 extraction Methods 0.000 description 1
- 238000002594 fluoroscopy Methods 0.000 description 1
- 230000035876 healing Effects 0.000 description 1
- 238000002347 injection Methods 0.000 description 1
- 239000007924 injection Substances 0.000 description 1
- 238000009434 installation Methods 0.000 description 1
- 238000005304 joining Methods 0.000 description 1
- 230000000399 orthopedic effect Effects 0.000 description 1
- 230000035515 penetration Effects 0.000 description 1
- 230000003094 perturbing effect Effects 0.000 description 1
- 230000000717 retained effect Effects 0.000 description 1
- 230000001568 sexual effect Effects 0.000 description 1
- 210000003625 skull Anatomy 0.000 description 1
- 239000007787 solid Substances 0.000 description 1
- 239000010935 stainless steel Substances 0.000 description 1
- 229910001220 stainless steel Inorganic materials 0.000 description 1
- 230000036262 stenosis Effects 0.000 description 1
- 208000037804 stenosis Diseases 0.000 description 1
- 230000003746 surface roughness Effects 0.000 description 1
- 208000024891 symptom Diseases 0.000 description 1
- 210000000115 thoracic cavity Anatomy 0.000 description 1
- -1 titanium-aluminum-niobium Chemical compound 0.000 description 1
- 238000002054 transplantation Methods 0.000 description 1
Images
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/56—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor
- A61B17/58—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor for osteosynthesis, e.g. bone plates, screws, setting implements or the like
- A61B17/68—Internal fixation devices, including fasteners and spinal fixators, even if a part thereof projects from the skin
- A61B17/70—Spinal positioners or stabilisers ; Bone stabilisers comprising fluid filler in an implant
- A61B17/7001—Screws or hooks combined with longitudinal elements which do not contact vertebrae
- A61B17/7002—Longitudinal elements, e.g. rods
- A61B17/7019—Longitudinal elements having flexible parts, or parts connected together, such that after implantation the elements can move relative to each other
- A61B17/7025—Longitudinal elements having flexible parts, or parts connected together, such that after implantation the elements can move relative to each other with a sliding joint
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/56—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor
- A61B17/58—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor for osteosynthesis, e.g. bone plates, screws, setting implements or the like
- A61B17/68—Internal fixation devices, including fasteners and spinal fixators, even if a part thereof projects from the skin
- A61B17/70—Spinal positioners or stabilisers ; Bone stabilisers comprising fluid filler in an implant
- A61B17/7001—Screws or hooks combined with longitudinal elements which do not contact vertebrae
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/56—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor
- A61B17/58—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor for osteosynthesis, e.g. bone plates, screws, setting implements or the like
- A61B17/68—Internal fixation devices, including fasteners and spinal fixators, even if a part thereof projects from the skin
- A61B17/70—Spinal positioners or stabilisers ; Bone stabilisers comprising fluid filler in an implant
- A61B17/7001—Screws or hooks combined with longitudinal elements which do not contact vertebrae
- A61B17/7002—Longitudinal elements, e.g. rods
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/16—Bone cutting, breaking or removal means other than saws, e.g. Osteoclasts; Drills or chisels for bones; Trepans
- A61B17/1662—Bone cutting, breaking or removal means other than saws, e.g. Osteoclasts; Drills or chisels for bones; Trepans for particular parts of the body
- A61B17/1671—Bone cutting, breaking or removal means other than saws, e.g. Osteoclasts; Drills or chisels for bones; Trepans for particular parts of the body for the spine
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/56—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor
- A61B17/58—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor for osteosynthesis, e.g. bone plates, screws, setting implements or the like
- A61B17/68—Internal fixation devices, including fasteners and spinal fixators, even if a part thereof projects from the skin
- A61B17/70—Spinal positioners or stabilisers ; Bone stabilisers comprising fluid filler in an implant
- A61B17/7001—Screws or hooks combined with longitudinal elements which do not contact vertebrae
- A61B17/7002—Longitudinal elements, e.g. rods
- A61B17/7004—Longitudinal elements, e.g. rods with a cross-section which varies along its length
- A61B17/7007—Parts of the longitudinal elements, e.g. their ends, being specially adapted to fit around the screw or hook heads
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/56—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor
- A61B17/58—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor for osteosynthesis, e.g. bone plates, screws, setting implements or the like
- A61B17/68—Internal fixation devices, including fasteners and spinal fixators, even if a part thereof projects from the skin
- A61B17/70—Spinal positioners or stabilisers ; Bone stabilisers comprising fluid filler in an implant
- A61B17/7001—Screws or hooks combined with longitudinal elements which do not contact vertebrae
- A61B17/7002—Longitudinal elements, e.g. rods
- A61B17/7011—Longitudinal element being non-straight, e.g. curved, angled or branched
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/56—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor
- A61B17/58—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor for osteosynthesis, e.g. bone plates, screws, setting implements or the like
- A61B17/68—Internal fixation devices, including fasteners and spinal fixators, even if a part thereof projects from the skin
- A61B17/70—Spinal positioners or stabilisers ; Bone stabilisers comprising fluid filler in an implant
- A61B17/7001—Screws or hooks combined with longitudinal elements which do not contact vertebrae
- A61B17/7032—Screws or hooks with U-shaped head or back through which longitudinal rods pass
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/56—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor
- A61B17/58—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor for osteosynthesis, e.g. bone plates, screws, setting implements or the like
- A61B17/68—Internal fixation devices, including fasteners and spinal fixators, even if a part thereof projects from the skin
- A61B17/70—Spinal positioners or stabilisers ; Bone stabilisers comprising fluid filler in an implant
- A61B17/7049—Connectors, not bearing on the vertebrae, for linking longitudinal elements together
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/56—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor
- A61B17/58—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor for osteosynthesis, e.g. bone plates, screws, setting implements or the like
- A61B17/68—Internal fixation devices, including fasteners and spinal fixators, even if a part thereof projects from the skin
- A61B17/70—Spinal positioners or stabilisers ; Bone stabilisers comprising fluid filler in an implant
- A61B17/7062—Devices acting on, attached to, or simulating the effect of, vertebral processes, vertebral facets or ribs ; Tools for such devices
- A61B17/7068—Devices comprising separate rigid parts, assembled in situ, to bear on each side of spinous processes; Tools therefor
Landscapes
- Health & Medical Sciences (AREA)
- Orthopedic Medicine & Surgery (AREA)
- Life Sciences & Earth Sciences (AREA)
- Surgery (AREA)
- Neurology (AREA)
- Heart & Thoracic Surgery (AREA)
- General Health & Medical Sciences (AREA)
- Biomedical Technology (AREA)
- Nuclear Medicine, Radiotherapy & Molecular Imaging (AREA)
- Medical Informatics (AREA)
- Molecular Biology (AREA)
- Animal Behavior & Ethology (AREA)
- Engineering & Computer Science (AREA)
- Public Health (AREA)
- Veterinary Medicine (AREA)
- Dentistry (AREA)
- Oral & Maxillofacial Surgery (AREA)
- Surgical Instruments (AREA)
- Prostheses (AREA)
Description
本願は、2009年6月17日に出願された、米国仮特許出願第61/187,902号を基礎とする優先権を主張するもので、同出願のすべての内容をここで参照によって引用する。 This application claims priority based on US Provisional Patent Application No. 61 / 187,902, filed Jun. 17, 2009, the entire contents of which are hereby incorporated by reference. .
本願による開示は、一般的には整形外科に関し、特に、既存の後部椎骨ねじ組立体をさらなるレベルへと伸ばすためのインプラント及び方法に関する。 The present disclosure relates generally to orthopedics, and more particularly to implants and methods for extending an existing posterior vertebral screw assembly to a further level.
患者の体内にある後部椎骨ねじ及びロッドの構造物を修正及び/又は延長させるために存する選択肢は、限られている。以前に脊柱手術を受けたことのある患者は、しばしば、隣接する脊柱レベルに症状を発現し、これが、しばしば疼痛を引き起こし、追加的な外科手術が必要になる。そのような追加的な脊柱の手術では、しばしば、既存のハードウェア構造物を、1又は複数のさらなる脊柱レベルにまで延長させることが必要になる。そのような症例においては、外科医は、(1)患者の既存のハードウェアと同一のハードウェアを使用して構造物を延長するのか、(2)患者の既存のいくつかのハードウェアには手を付けずにこれを残しつつ、異なるハードウェアを使用して構造物を延長するのか、あるいは、(3)患者の既存のすべてのハードウェアを取り外し、装着すべき新たな脊柱レベルを含む、新たなハードウェアと交換するのかを決定しなければならない。しかしながら、これらのアプローチには、いくつかの欠点がある。 The options that exist to modify and / or extend the posterior vertebral screw and rod structures in the patient's body are limited. Patients who have previously undergone spinal surgery often develop symptoms at adjacent spinal levels, which often cause pain and require additional surgery. Such additional spinal surgery often requires extending existing hardware structures to one or more additional spinal levels. In such cases, the surgeon may (1) extend the structure using the same hardware as the patient's existing hardware, or (2) handle some of the patient's existing hardware. Leave this without attaching and extend the structure using different hardware, or (3) remove any existing hardware of the patient and include a new spine level to be fitted You must decide whether to replace the hardware. However, these approaches have several drawbacks.
まず、患者の既存のハードウェアを、X線又は蛍光透視を介して確認し、確認されたならば、外科医は、同一の作り及び型式のハードウェアが院内で又は市場で、まだ入手可能であるのかどうかを判断しなければならない。また、外科医は、彼の技量で、既存のハードウェアを修正し、及び/又は、新たなハードウェアを追加できるか否かを判断しなければならない。というのは、既存のハードウェアシステムの修正又は据え付けは、より困難であるためである。こうした判断に基づいて、外科医は、新たなハードウェアを用いて修正することを決断するだろう。外科医は、彼の選択でハードウェアを選べるけれども、既存のハードウェアと新たなハードウェアとの間の結合を行う必要があり、そのためには、通例、すべての既存の固定された椎体と共に、新たに固定されるべき椎体を露出させるのに充分な長さの切開を行って、下にあるロッドを取り外し、新たなねじを移植し、それから、新たなロッドを、既存の移植されたロッド及び新たに移植されるロッドへ挿入する。しかしながら、そのような技術には、それまでは無症状だった、ある脊柱レベルを乱し、従って、以前には無かった疼痛をもたらす結果になり得るという懸念がある。さらに、多くの椎骨ねじシステムは、互いに互換性が無く、既存の構造物に追加するための新たなハードウェアの選択肢には著しい制限がある。仮に、外科医が、すべての既存のハードウェアを取り外して、彼の選択による新たなハードウェアと交換することを決断した場合にも、彼は、それまで無症状だった、いくつかの脊柱レベルを乱すことがある。ハードウェアを追加及び交換する、これらのいずれの選択肢も、時間がかかり、外科医が、患者の既存のハードウェアに馴染みがない場合には、特にそう言える。 First, the patient's existing hardware is confirmed via X-ray or fluoroscopy, and if confirmed, the surgeon is still able to obtain the same make and type of hardware in the hospital or on the market You must judge whether or not. The surgeon must also determine whether his skill can modify existing hardware and / or add new hardware. This is because it is more difficult to modify or install existing hardware systems. Based on these decisions, the surgeon will decide to modify with new hardware. Although the surgeon can choose the hardware at his choice, he needs to make a connection between the existing hardware and the new hardware, usually with all existing fixed vertebral bodies, Make an incision long enough to expose the vertebral body to be newly fixed, remove the underlying rod, implant a new screw, and then replace the new rod with the existing implanted rod And inserting into a newly implanted rod. However, there are concerns that such techniques may result in perturbing certain spinal levels that were previously asymptomatic and thus leading to pain that was not previously present. In addition, many vertebral screw systems are not compatible with each other and there are significant limitations on new hardware options for adding to existing structures. Even if the surgeon decides to remove all existing hardware and replace it with new hardware of his choice, he has several vertebral levels that were previously asymptomatic. May be disturbed. Either of these options of adding and replacing hardware is particularly time consuming and the surgeon is unfamiliar with the patient's existing hardware.
本発明の1つの実施形態においては、延長システムは、椎骨に結合される椎骨インプラントに機能的に結合されるべく構成されており、該インプラントは、第1の骨アンカーと、第1の骨アンカーを受け入れる第1のアンカー座部とを具備している。延長システムは、延長部材であって、本体と、本体に結合される係合部材とを含む、上記延長部材を具備している。延長システムはさらに、固定具であって、延長部材を椎骨インプラントに結合すべく構成されてなる、上記固定具を具備している。延長システムはさらに、第2の骨アンカーであって、延長部材を、椎骨に隣接して配置された、下にある骨に取り付ける、上記第2の骨アンカーを具備している。 In one embodiment of the invention, the extension system is configured to be functionally coupled to a vertebral implant that is coupled to a vertebra, the implant including a first bone anchor and a first bone anchor. And a first anchor seat. The extension system includes the extension member, the extension member including a main body and an engagement member coupled to the main body. The extension system further comprises a fixture, the fixture configured to couple the extension member to the vertebral implant. The extension system further comprises a second bone anchor that attaches the extension member to the underlying bone disposed adjacent to the vertebra.
上述した要旨並びに以下の本願の例示的実施形態についての詳細な説明は、添付図面と関連させて読むことで、より良く理解されよう。本願による修正コネクタを例証する目的で、図面には好ましい実施形態を示しているしかしながら、本願は、図示された詳細な構成及び手段に限定されるものではないことを理解されたい。 The foregoing summary, as well as the following detailed description of exemplary embodiments of the present application, will be better understood when read in conjunction with the appended drawings. For the purpose of illustrating the modified connector in accordance with the present application, it is to be understood that the preferred embodiment is illustrated in the drawings, however, the present application is not limited to the detailed arrangement and instrumentalities shown.
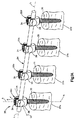
ある種の用語は、以下の説明において、便利さのためだけに使用されるが、いかなる意味でも制限的に解釈されるべきではない。例えば、骨固定組立体20は、図1Aに示すように、1又は複数の骨固定要素22と、4つの骨固定要素22a〜dを具備している。図1Bに示すように、それぞれの骨固定要素22は、軸線方向Aに沿って垂直に延在していると共に、軸線方向Aに対して垂直である放射方向Rに沿って略水平に延在している。従って、放射方向Rには、長手方向Lと、長手方向Lに対して垂直に延びる横方向LAとが含まれる。方向の用語、“長手方向”、“横方向”は、同様に、水平に延在している骨固定組立体20にも適用され、また、方向の用語、“横断方向”は、垂直方向を参照することを認識されたい。骨固定要素22は、上方の乃至後方の端部21と、下方の乃至下位の端部23とを形成しており、方向の用語、“上方”及び“下方”及びそれらの派生語は、下端23から上端21へ向けた方向と、上端21から下端23へ向けた方向とを、それぞれ参照している。
Certain terms are used in the following description for convenience only and should not be construed as limiting in any way. For example, the
用語、“内側”、“外側”、“上方”、“下方”、“遠位側”、及び“近位側”は、骨固定組立体20及びその要素の幾何学的中心に向かう又は遠ざかる方向をそれぞれ参照する。用語、“前方”、“後方”、“上位”、及び“下位”、及び関連する用語及び/又はフレーズは、参照されている人体における好ましい位置及び配向を指示し、限定を意味しない。さらに、本願の開示の如く、丸い構造物は直径を形成するけれども、丸い構造物は、代替的な構造物(例えば、多角形)と置換することができ、それらは、直径ではなく、代替的に、横断面寸法を形成することを認識されたい。本願における用語、“直径”は、特段の記載が無い限り、そうしたあらゆる代替物を包含することを意図している。用語には、上に列挙した単語のほか、それらの派生語及び類義語が含まれる。
The terms “inner”, “outer”, “upper”, “lower”, “distal”, and “proximal” refer to the direction toward or away from the geometric center of the
本願において、骨固定組立体20及びその要素についての方向の用語は、配向に関連して使用され、また、骨固定組立体20及びその要素についての実際の配向は使用中には変化することを認識されたい。例えば、軸線方向は、垂直方向に沿って延びるものとして示され、放射方向は、水平方向に沿って延びるものとして示されるけれども、様々な方向を包含する方向は、使用中には、例えば、使用中の骨固定組立体20の望ましい配向に応じて、異なってくることになる。従って、本願における方向の用語は、単に、非限定的な、明瞭性及び便宜性の目的だけのものである。
In this application, the directional terms for the
次に、図1Aを参照すると、骨固定組立体20は、複数の骨固定要素、例えば、骨固定要素22a〜dを具備し、長手軸線Lに沿って延在している脊柱固定ロッド24によって結合されている。骨固定要素22a〜dのそれぞれは、対応する椎骨27a〜dに移植された(例えば、ねじ込まれた)、骨アンカー30を具備している。骨固定要素20a〜dは、脊柱の後方領域に移植され、又は、脊柱のあらゆる適切な他の領域、例えば、椎弓根若しくはその他の脊柱領域に移植される。骨アンカー30は、ねじ、フック、又は他の構造をもった、上部載荷式の骨アンカーであって、下にある椎骨に取り付けられるように構成されたものとして、提供される。特段の記載が無い限り、骨固定組立体20とその要素とは、チタン−アルミニウム−ニオブの合金(TAN)や、インプラント等級の316Lのステンレス鋼、又はその他のあらゆる代替的なインプラント等級の材料から作られる。
Referring now to FIG. 1A, the
引き続き、図1Aを参照すると、骨固定要素22a〜dは、一般に、脊柱、例えば、腰部や、胸部、又は、頚部の椎体の後方部分に移植されるものとして開示される。これに関して、骨固定要素22a〜dがロッド24によって結合されたとき、組立体20は、椎骨(模式的に27a〜dとして示される)の相対的な位置を固定する。従って、骨固定要素22a〜dは、椎骨インプラントと称することができ、脊柱固定ロッド24は、脊柱固定ロッドと称することができ、骨固定組立体20は、椎骨インプラントと称することができる。しかしながら、骨固定組立体20はまた、例えば、関節、長骨、又は手、顔、足、四肢、及び頭蓋骨など、身体の他の部分の固定にも使用できることを認識されたい。
With continued reference to FIG. 1A,
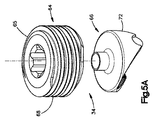
図2に示すように、脊柱固定ロッド24は、長手軸線Lに沿った細長いものであり、円筒形ないし管状の形状である本体25を具備している。長手方向Lは、骨固定組立体が脊柱に取り付けられたとき、概略、頭蓋−尾部の方向に延びる。ロッド本体25は、限定はしないが、中実な本体、中空の本体、可撓性ないし動的な本体、その他を含み、必要に応じて任意のあらゆる他の形態で良い。従って、骨固定組立体20は、何か特定の脊柱固定ロッド24を使用することに限定されないことを認識されたい。
As shown in FIG. 2, the spinal
次に、図1Bをも参照して、骨固定組立体20における骨固定要素22a〜dについて、骨固定要素22によって説明する。特に、骨固定要素22は、一般的に、椎骨インプラント75と、ロックキャップ34とを具備している。椎骨インプラント75は、骨アンカー座部26と、アンカー座部26の内側に配置されたコレット28と、コレット28に取り付けられた頭部部分33(図3参照)を有する骨アンカー30(骨ねじとして示される)とを具備しているものとして図示される。ロックキャップ34は、コレット28の上方の位置にて、アンカー座部26に据え付けられ、脊柱固定ロッド24は、コレット28とロックキャップ34との間に配置された、ロッドスロット36の中に位置している。
Next, the
図3をも参照すると、骨アンカー30は、骨ねじ又は椎骨ねじとして構成され、上端にて、拡大した曲面頭部33に結合されてなる雄ねじ軸部31を具備している。軸部31は、回転の中心軸線Bに沿って、軸線方向に延在し、椎骨27などの下にある骨に係合するために、任意の適切な直径、長さ、及びねじ部デザインを有している。変形例としては、軸部31は、望むならば、ねじ付きではなく、ピン又は爪として形成しても良い。従って、当業者は、骨アンカー30が何か特定のタイプの軸部31に限定されないことを認識するだろう。また、必要ならば、骨アンカー30を、カニューレ化及び有窓化して、開口部が、カニューレ化された軸部の中心の中空通路から外側へ放射状に延在し、注入中には骨アンカー30から流体が出るのを促し、又はアンカーに隣接する物質の摘出中にはアンカーの放射側面から中心の中空通路の中へ流体を吸引したりしても良い。
Referring also to FIG. 3, the
骨アンカー30はさらに、軸部31と頭部33との間に結合された、垂直に延在する首部35を具備している。首部35は、軸線Bに対して平行な方向において、軸方向に延在するものとして示され、頭部33の直径に比べて小さい首部直径を形成してなる、外側首部面37を具備している。
The
頭部33は、例えば、半球形曲面など、少なくとも部分的に球形の曲面を形成しているか、又は、代わりに、所望の任意の適当な曲面を形成し、詳しくは後述するように、コレット28に対する回転を容易にしている。また、頭部33は、骨アンカー30を回転させて椎骨27又はその他の下にある骨の表面に係合させるべく構成されてなるねじ回しなどの、駆動ツールの対応する先端部を受け入れるように構成された駆動面39を具備している。駆動面39は、ねじ回しのための、六角形、星形駆動パターン、フィリップスの頭部パターン、スロット、若しくは、ねじ付き駆動支柱の対応するねじを受け入れるべく構成されたねじ部、又は、所望の任意の適当な駆動ツール係合構造を形成することができる。
The
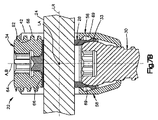
次に、図4を参照すると、アンカー座部26は、骨固定要素が下にある椎骨に移植されたときに、略前後方向へ延びるような軸線Aに沿った中心に延在してなる、略円筒形の管状本体として開示されるアンカー座部本体38を具備している。本体38は、ベース40と、ベース40から(図面では上方向に)突き出た、一対の間隔を隔てた対向するアーム42とを具備している。アーム42は、実質的な同一又は同一に構成される。アーム42は、本体38の上端である、対応する上端部46を形成し、及び上部開口部48を形成している。ベース40は、本体38の下端である下端部50を形成し、及び下部開口部52を形成している。そして、本体38は、下部開口部52から上部開口部48へと延在してなる軸線ボア54を形成している。
Referring now to FIG. 4, the
本体38は、対向する支持壁部56と、支持壁部56同士の間に結合された、一対の間隔を隔てた対向するスペーサ壁部58とを具備している。支持壁部56は、実質的な同一又は同一に構成され、スペーサ壁部58も同様に、実質的な同一又は同一に構成されている。アーム42は、それぞれの支持壁部56から突き出て、所望の形状に形成される。図示の通り、アーム42は、円弧形状であって、アンカー座部26を二等分する対称面を通る円弧の軸線をもっている。それぞれのアーム42は、その軸線のまわりの円周に、60゜〜150゜の間など、180゜未満、例えば、およそ90゜にわたって延在している。例えば、それぞれのアーム42は、その軸線のまわりの円周に、90.5゜にわたって延在する。
The main body 38 includes an opposing
従って、アーム42の隣接する円周外端部の間には、円周状にギャップGが延在する。対向するギャップGは、軸線ボア54に対して整列されている。アーム42は、放射方向に互いに対向するように配置され、ギャップGは、軸線ボア54の整列部分との組合せによって、ロッド受入れ通路36を形成し、そのサイズ及び構造は、脊柱固定ロッド24を受け入れて、脊柱固定ロッド24が骨固定要素22を通って延びるようになっている。従って、ギャップGは、長手方向に整列される。脊柱固定ロッド24は、従って、対向するギャップG及び軸線ボア54を通って延在する。アーム42は、放射方向に内側及び外側の表面60及び62をそれぞれ形成している。内側の表面60には、ねじ62が形成され、以下に述べるように、ロックキャップ34がねじ込まれるように構成されている。
Therefore, a gap G extends circumferentially between the adjacent outer circumferential ends of the
より詳しくは、図5A乃至図5Cを参照すると、ロックキャップ34は、止めねじ64と、止めねじ64に機能的に結合されるサドル部66とから構成されるものとして示されている。止めねじ64は、アーム42の内面60に形成されたねじ部62と螺合すべく構成された雄ねじ68を有してなる、略円筒形の止めねじ本体65を具備している。1つの実施形態によれば、ねじ部68及び62は、骨固定要素22の軸線Aに対して斜めに形成された、傾斜ロードフランクを組み込まれている。ロードフランクは、収束しており、ねじ部の上面とねじ部の底面とが収束するようになっている。角度は、0゜〜30゜の間であり、1つの実施形態では、約5゜である。当業者は認識するだろうが、ねじ部は、必要に応じて、任意の変形例による形態を取ることができ、それには、ネガティブロードねじや、垂直ねじ、鋸歯ねじ、その他が含まれる。
More specifically, with reference to FIGS. 5A-5C, the
雄ねじの止めねじ64は、一般的に、脊柱固定ロッド24をアンカー座部本体38に挿入するとき、ロックキャップ34の係合前に、脊柱固定ロッド24が、本体38の内部に完全に納まりないし着座する必要がないという柔軟性を提供する。止めねじ64は、脊柱固定ロッド24に当接して、アンカー座部26の内部にて締め付けられるように構成されている。ロックキャップ34は、かかる目的に望ましいように構築され、限定はしないが、それらには、雄ねじキャップや、直角回転又は部分回転のロックキャップ、ツーピースの止めねじ、その他が含まれる。
The
止めねじ64は、ねじ64の上端部から下へ向けて垂直に延びた内側凹部として提供されてなる、駆動面70を具備するものとして示されている。駆動面は、任意の適当な形状を有し、止めねじ64をアンカー座部本体38に螺着するための対応する駆動ツールと協働するように構成されている。駆動面70は、所望の任意の形状に形成することができ、例えば、ねじ回しのための、六角形外面、星形駆動パターン、フィリップスの頭部パターン、スロット、又は、ねじ付き駆動支柱の対応するねじ、その他がある。
The
引き続き、図5A乃至図5Cを参照すると、サドル66は、サドル本体72を具備し、これは、サドル本体72の底端部から上へ延びた横断凹部74を有している。凹部74は、長手方向に延びる軸線のまわりに延設された、丸い表面を形成しており、凹部74は、ロッド接触面76において、脊柱固定ロッド24を受け入れるように構成されている。ロッド接触面76は、粗さを加える所望の表面仕上げを具備し、例えば、ローレットや、ビーズブラスト、溝部、又はその他のテクスチャ仕上げであって、表面粗さを増加させ、ロッドの押通し強度を向上させるものなどがある。
With continued reference to FIGS. 5A-5C, the
サドル66は、接着や、機械的固定、その他、あらゆる所望のやり方で、止めねじ64に結合される。図示の実施形態においては、サドル66は、サドル本体72の中心から上方へ延設された心棒78を具備している。心棒78は、止めねじ本体65の下端へ向けて垂直に延在している中心ボア32に受け入れられるように構成され、リベット80又はその他の類似の固定具を用いて、中心ボアの内部に固定される。従って、サドル66は、止めねじ64に対して回転可能であり、例えば、ロックキャップ34が脊柱固定ロッド24に当接して締め付けられるときなど、止めねじ64がアンカー座部26に対して回転されるとき、脊柱固定ロッド24に自己整列される。
The
再び図4を参照すると、上述したように、アンカー座部本体38は、一対の間隔を隔てた対向する支持壁部56と、支持壁部56同士の間に結合された、一対の間隔を隔てた対向するスペーサ壁部58とを具備している。アーム42は、それぞれの支持壁部56から上方へ延在し、スペーサ壁部58がアーム42の間に配置されるようになっている。それぞれのスペーサ壁部58は、所望の形状をもった、対向する上端部84と下端部82とを形成している。上端部84は、図示の実施形態では、丸くなっていて、アーム42における上端部84及び円周状の外側端部42と隣接し、ギャップGを通る水平視にて、略U字形を形成している。従って、上端部84は、ギャップGの下端を形成する。
Referring to FIG. 4 again, as described above, the anchor seat portion main body 38 has a pair of spaced apart support
上端部84の形状は、脊柱固定ロッド24の外面と概略一致しており、上端部84は、使用中に脊柱固定ロッド24を受け入れて係合する。変形例としては、上端部84は、コレット28の上面に対して、下側にわずかに間隔を隔てており、詳しくは後述するように、使用中にコレット28が脊柱固定ロッド24を支持するようにしても良い。
The shape of the
それぞれの支持壁部56は、対向する内側及び外側の表面86及び88をそれぞれ形成している。支持壁部56及びスペーサ壁部58は、アーム42から下方向へ、中心軸線Aに向けて内方へ窄んでおり、それぞれの下端部90にて終端している。支持壁部56及びスペーサ壁部58に対向する内面86は、距離Dを形成し、これは、アーム42の放射方向に対向する内面60間の距離に比べて小さくなっている。距離Dは、骨アンカー30の頭部33の直径に比べて、小さいか、又は大きいか、のいずれかとすることができる。内面86は、下方向へ、中心軸線Aへ向けて及び互いに向けて、放射方向内方に窄んでおり、それぞれの当接壁部92を形成している、最底部かつ最内方の表面に、それぞれ結合されている。
Each
図4及び図7Aを参照すると、それぞれの当接壁部92は、それぞれ内側当接面93を形成し、それらの間に形成される距離は、首部35の直径と実質的に等しくて、当接壁部92は、骨アンカーの対向する当接面に当接すべく構成されており、これらは、骨アンカー30がアンカー座部26内に配置されたときの、首部の外面37における対向側部として示される。当接壁部92は、骨アンカー30が、アンカー座部26に対して、所望の平面内において、ピボットするのを防止ないし制限する。
Referring to FIGS. 4 and 7A, each
次に図6を参照すると、コレット28は、コレット本体45を具備し、これは、第1のないし上方の端部47であって、ロッド受入れ通路36の内部にロッドが受け入れられたとき、脊柱固定ロッド24の少なくとも一部分に接触又は支持するようなサイズ及び構造をもつものと、第2のないし下方の端部49であって、直接的に又は間接的に、骨アンカー頭部33の一部分に接触又はその他の係合をするようなサイズ及び構造をもつものと、を具備している。コレット本体45は、環状であり、これにより、上端部47と下端部49との間を通って延在する軸線ボア53を形成している。軸線ボア53は、コレット28がアンカー座部26内に据え付けられたとき、軸線ボア54に対して整列される。
Referring now to FIG. 6, the
図6、図7A、及び図7Bを参照すると、上端部47は、脊柱固定ロッド24の外面に対応する曲面ないし半球形の形状をもち、放射方向に対向し、上方を向いてなる座部51を形成しており、もって、ロッド24の少なくとも一部分(例えば、下側部分)を受入れ又はその他の支持をすべく構成されている。下端部49は、アンカー頭部33の外面に対応する曲面ないし半球形の形状をもった内面55を形成しており、従って、頭部33の少なくとも一部分を受入れ又はその他の係合をすべく構成され、頭部が、コレット28及びアンカー座部26に対して回転でき、さらに、アンカー座部26によって許容されて、コレット28に対してピボットし得るようになっている。骨アンカー30は、アンカー座部26に対して、その回転軸線Bのまわりで自由に回転でき、従って、アンカー座部26も同様に、骨アンカー30のまわりで回転できるので、ロッド受入れ通路36は、骨アンカー30を下にある骨から出し入れするように前進又は後退させることなく、脊柱固定ロッド24に対して整列される。かくして、骨アンカー30は、ロッド受入れ通路36の配向を調整する間も、下にある骨(例えば、椎骨27)への一定の挿入深さを維持できる。
Referring to FIGS. 6, 7A, and 7B, the
コレット28はさらに、一対のフランジ57を具備し、これらは、座部51の間の放射方向の位置にて、コレット本体45の上端部47から上方へ突設されている。それぞれのフランジ57からは、放射状に、ロック唇部59が延設されている。図7Aに最良に示されるように、アンカー座部26は、一対の対向する凹部61(図8A参照)を形成しており、これらは、アーム42のねじ付き内面60の下方の位置にて、支持壁部56の対向する内面86に放射方向に形成されている。手術中には、コレット28は、アンカー座部26の中に上から下へ挿入され、それにより、フランジ57は、内方へ撓み、ねじ付き内面60を通り抜け、ついには、唇部59が凹部61の上端部を通過し、かかる場所で、フランジ57はスナップバックして、唇部59は凹部61内に配置される。唇部59と凹部61の上端部との間の干渉によって、コレット28が、アンカー座部26の上端部を通って外へ出ることが防止される。凹部61はさらに、フランジ57及びロック唇部59と実質的に等しい円周長さを形成しており、コレット28は、回転についてアンカー座部26に対して所定位置に固定され、それにより、脊柱固定ロッド24がアンカー座部26に挿入されたとき、上面47が脊柱固定ロッド24に対して整列されるようになっている。
The
コレット28の下端部49は、当接壁部92同士の間の内側距離に比べて、大きい外径を形成している。従って、コレット28は、アンカー本体26の下端部を通って軸線方向下方へ通り抜けることは出来ない。下端部49は、(複数のスロットとして図示される)1又は複数のスロット67を具備し、これらは、下端部を通って放射状に延びており、骨アンカー30の頭部33をポップオーバーするように構成された、対向する複数の指部69を形成している。コレット28がアンカー座部26の中に配置されて、唇部59がそれぞれの凹部61内に配置されたとき、指部69は、当接壁部92に対して軸線方向に整列される。従って、図7A及び図7Bに示すように、コレット28及びアンカー30がアンカー座部24内に据え付けられたとき、指部69は、放射方向に拡張して、アンカー頭部33の外面及びアンカー座部26の内面と一致する。対向する指部69によって形成された内径は、アンカー頭部33の外径に比べて小さくなっており、アンカー30が、アンカー座部26から軸線の下方向へ外れるのを防止している。指部69の下端部は、当接壁部92の上方の位置にて終端している。従って、指部69は、アンカー首部35と当接壁部92との間の係合に干渉することはない。
The
次に図8A乃至8Dを参照すると、椎骨インプラント75を組み立てる方法は、段階1として、骨アンカー30を、垂直下方へ軸線ボア54に通して挿入する段階を具備しており、軸部31は、アンカー座部26の下端部50における下部開口部52を延通し、アンカー頭部33は、当接壁部92の上方に配置される。この方法における、骨アンカー30をアンカー座部26に挿入するための段階は、骨アンカー30のアンカー座部26への上部載荷と称することができる。次に、段階2においては、コレット28は、軸線ボア54の中に挿入されて、所定位置に配置され、それにより、ロック唇部59は、アーム42の内面60における下端のねじ部62と係合できるようになる。次に、段階3においては、骨アンカー30に上向きの力を加えて、アンカー頭部33をコレット28の下端部49の中へ挿入する。コレット28のロック唇部59は、ねじ部62の内側にてアンカー座部26に当接して受けとめられ、ねじ28によって加えられた上向きの力が、コレット28をアンカー座部26の上側開口部から出る原因になることを防止している。段階4においては、コレット28に下向きの力が加えられ、それにより、上述したやり方で、ロック唇部59を凹部61の中へ挿入し、アンカー30及びコレット28をアンカー座部26の中に係止する。
8A-8D, the method of assembling the
使用中には、骨アンカー30は、コレット28及びアンカー座部26に対して回転可能であるから、駆動ツールを頭部33の駆動面39に係合させて、図1Aに示すように、ねじ付き軸部31を下にある骨に挿入することができる。次に、図8A乃至図8Dに示すように、アンカー座部26は、矢印Rの方向に、軸線Aを中心として、全360゜の範囲の角度に回転できて、ロッド受入れ通路36を脊柱固定ロッド24の長手軸線に対して整列させることができる。従って、椎骨インプラント75は、多軸的な椎骨インプラントと称することができ、また、骨固定要素22は、多軸的な骨固定要素と称することができる。変形例としては、骨固定要素は、軸線Aに対して一平面内における回転をアンカー座部26に許容しても良く、もって単軸的な椎骨インプラントと称されることを認識されたい。さらに、椎骨インプラントは、骨アンカー30として、ねじではなく、フックを具備しても良いことを認識されたい。ひとたび、骨アンカー30が、下にある椎骨の中の所望の深さに到達したならば、脊柱固定ロッド24を、椎骨インプラント75の中に挿入することができる。より詳しくは、脊柱固定ロッド24は、ギャップGを通して水平に、又は垂直下方向に、軸線ボア54の中に挿入される。脊柱固定ロッドは、コレット28の上端部47に着座することを認識されたい。
In use, the
引き続き図8A乃至図8Dを参照すると、いったんロッド24が椎骨インプラント75に据え付けられたならば、ロックキャップ34が組立体75に取り付けられて、アンカー組立体22が完全に組み立てられる。図示の実施形態においては、止めねじ64の雄ねじ68は、アンカー座部アーム42の雌ねじ62の中で回転し、それにより、止めねじ及びサドル66を軸線ボア54内にて軸線方向下方へ移動させる。サドル66が脊柱固定ロッド24に近づくと、サドル66は、止めねじ64に対して回転し、ロッド接触面76を脊柱固定ロッド24に対して整列せしめる。いったんサドル66が脊柱固定ロッド24に対して整列されたならば、止めねじ64を引き続き骨アンカー26に螺入して、ロックキャップ34をロッド24に対して締め付けて、それにより、ロッド24に下方向の軸線力を与える。ロックキャップ34は、ロックキャップ34に据え付けられたが、脊柱固定ロッド24に軸線力を加える前のとき、初期位置にあると言える。ロックキャップ34によってロッド24に加えられる軸線力は、コレット28へ伝達され、これにより、指部69は、支持壁部56及びスペーサ壁部58の内面86に沿って乗り上がる。
With continued reference to FIGS. 8A-8D, once the
指部69が、壁部56及び58に沿って乗り上がるとき、指部は、壁部56及び58の内面の内向きの窄みに起因して、放射方向内方へ変位し、それにより、指部69をアンカー頭部33に対して、放射方向に付勢し、又は放射方向に圧縮する。アンカー頭部33に対する指部69の放射方向の圧縮が高まると、指部69とアンカー頭部33との間に摩擦力を引き起こし、このため、アンカー座部26、コレット28、及び脊柱固定ロッド24に対する、軸線Aを中心としたアンカー30の回転は、抵抗を受ける。ロックキャップが係止位置にまで完全に締め付けられたときには、結果的に得られる摩擦力によって、アンカー30は、アンカー座部26や、コレット28、及び脊柱固定ロッド24に対して動くことが防止される。従って、ロックキャップ34は、コレット28及び骨アンカー30へ係止力を伝達するように構成され、アンカー座部26及び脊柱固定ロッド24に対して、骨アンカー30の位置を固定ないしロックする。かくして、脊柱固定ロッド24は、骨アンカー30が係合している、下にある椎骨に移植されることを認識されたい。
When the
上述した方法の段階は、必要に応じて、骨固定組立体20のそれぞれの骨固定要素について実行されることを認識されたい。さらに、骨固定要素22a〜dは、それぞれ、上述した椎骨インプラント75を具備すると述べたけれども、骨固定要素22a〜dは、脊柱固定ロッド24を下にある椎骨27に固定するために適した、あらゆる変形例によって構築された椎骨インプラントを含み得ることを認識されたい。例えば、椎骨インプラント75は、アンカー頭部33がコレット28に挿入される前に、骨アンカー30が下にある骨に移植されることを許容するようにも構築できる。1つの実施形態においては、当接壁部92にスロットが設けられ、アンカー頭部33にかぶせられて拡張するようにしている。それにより、アンカー座部26及びコレット28は、上述したやり方でアンカー30をアンカー座部26に通して下へ挿入する代わりに、上から頭部33に装着することができる。アンカー座部26を頭部33にかぶせて装着する段階は、アンカー30のアンカー座部26への底部載荷と称することができる。さらに、骨固定要素22及び椎骨インプラント75を含む骨固定組立体20について、1つの実施形態に関連させて説明したけれども、骨固定要素22及び椎骨インプラント75を含む骨固定組立体20は、複数の椎骨に移植され、脊柱固定ロッドによって結合されるのに適したあらゆる実施形態に従って構築することができることが認識されるべきであって、そのための手段は、例えば、2006年11月21に米国特許出願第11/603,428号として出願され、2007年5月24日に米国公開特許公報第2007/0118123号として刊行された文献に開示されており、同文献の内容をここで完全に参照によって引用する。
It should be appreciated that the method steps described above are performed for each bone fixation element of the
次に図9を参照すると、脊柱固定ロッド24は、骨固定組立体20によって複数の椎骨27a〜dに移植されているけれども、将来の日に、骨固定組立体20を延長して、少なくとも1つの、例えば複数の、椎骨を、椎骨27a〜dに固定することが必要になり得ることを認識されたい。例えば、少なくとも1つの、例えば複数の、下位椎骨27e〜fを、椎骨27a〜dに固定することが望ましくなることがある。代わりに又は加えて、少なくとも1つの、例えば複数の、上位椎骨27g〜hを、椎骨27a〜dに固定することが望ましくなることもある。かくして、脊柱固定ロッド24は、ここでは、既に移植された脊柱固定ロッドと称することができる。図示の通り、椎骨27aは、脊柱固定ロッド24に固定された、最も頭蓋側の椎骨であり、椎骨27dは、脊柱固定ロッド24に固定された、最も尾側の椎骨である。椎骨27gは、椎骨27aの上位にあり、椎骨27hは、椎骨27gの上位にある。椎骨27eは、椎骨27dの下位にあり、椎骨27fは、椎骨27eの下位にある。椎骨27g〜h及び27e〜fは、新たな椎骨と称される。
Referring now to FIG. 9, although the
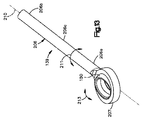
次に図10A乃至図10Dを参照すると、延長システム100は、上部載荷式の多軸的な脊柱構築延長具105を具備し、これは、既に移植された骨固定要素22の、又は新たに移植される骨固定要素の、脊柱固定ロッド24と機能的に結合するように構成されており、それまで骨固定システム20を用いて互いに結合されていた、1又は複数の椎骨を、隣接する骨に連結するものである。従って、多軸的な脊柱構築延長具105は、骨固定システム20を1又は複数の隣接する脊柱レベルに拡張するように構成されている。当業者は認識するだろうが、多軸的な脊柱構築延長具105は、既に移植されている構造物を拡張するものに限られず、最初の脊柱手術に利用して、最小限の潜在的侵襲性の態様にて、複数のレベルの患者の椎骨を固定することができる。
Referring now to FIGS. 10A-10D, the
多軸的な構築延長具105は、多軸的な延長部材139を具備し、これは、近位端141aと、これとは反対側にある遠位端141bとを形成する実質的に円筒形のロッド本体141を有してなる、ロッド140として構築されている。多軸的な延長ロッド140は、近位側ロッド本体端部141aに取り付けられたループ142として図示される係合部材と、ループ142を垂直に通って延在する開口部143とを具備している。遠位端141bは、図示の通り、ループ142と同一平面上にあっても良い。変形例としては、遠位端141bは、ループ142に対して、斜めであるか又はその他の垂直にオフセットしたものでも良い。多軸的な延長ロッド140はさらに、開口部143の内部に配置されて、ループ142に固定された、ブッシング150を具備している。延長具105はさらに、ブッシング150と(既に移植された骨固定システム20の、又は新たな骨固定システムの)アンカー座部26との両方に結合すべく構成されてなる、テーパ付き止めねじ130として図示されたテーパ付き固定具を具備していると共に、延長ロッド140を止めねじ130に係止すべく構成されたロックナット160として図示されるロック部材を具備している。
The
テーパ付き止めねじ130は、近位側部分130aと、遠位側部分130bと、近位側部分130aと遠位側部分130bとの間に配置された、中間部分130cとを具備している。止めねじ130は、近位側部分130aに、テーパの付いていない外面を具備し、これは、雄ねじ131を有しており、雄ねじは、ロックナット160の雌ねじに係合するように構成されている。テーパ付き止めねじ130の遠位側部分130bは、テーパの付いていない外面132を具備し、これは、雄ねじ133を有しており、雄ねじは、アンカー座部26の雌ねじに係合するように構成されている。止めねじ130は、中間部分130cに、テーパ付きでねじの無い外面134を具備しており、これは、ブッシング150の内面151に当接するように構成されている。テーパ付き外面134は、中間部分130cの円周が、近位側部分130aから遠位側部分130bへ向かう方向に沿って増大するように構成されている。
ブッシング150は、平坦な上位面152と、平坦な下位面153と、上位面152と下位面153との間に延在する中心長手軸線154と、平坦な上位面152と下位面153との間に延在する部分的な球形外面155と、中空てる内部156を取り囲む内面151とを具備している。ブッシング150は、外面155及び内面151を通って長手軸線に沿って延設された割れ目157を具備し、テーパ付き止めねじ130が内部156に押し込まれたとき、ブッシングの円周が拡大できるようになっている。
The
ブッシング150の内面151は、下位テーパ部151aと、上位テーパ部151bとを具備し、下位テーパ部151aは、下位面153と内面151の中間点との間に延在し、一方、上位テーパ部151bは、上位面152と内面151の中間点との間に延在している。内面151の中間点は、2つのテーパ部が交わって、頂点158を形成するような、略円形の線になっている。下位テーパ部151aと上位テーパ部151bとはそれぞれ、好ましくは、長手軸線154に対して角度を形成しており、かかる角度は、テーパ付き止めねじ130の中間部分130cの外面134のテーパ角度と合致している。
The
ブッシング150は、延長ロッド140のループ142の開口部143の中に圧入される。ブッシング150の部分的な球形の外面は、一般に、ループ142の内面の球形の幾何学形状と類似し又は同一であり、ブッシング150は、ねじ130の挿入前の初期状態においては、開口部143の内部にて多軸的に回転可能である。ひとたび、ねじ130がブッシング150に挿入されると、ねじ130のテーパ付き外面134は、ブッシングの内面151に沿って乗り上げ、割れ目157を拡大せしめ、ブッシングの外面155は、ループ142の内面に圧接されて、それにより、ループ142の内部におけるブッシング150の位置をロックする。
The
次に、再び図9をも参照すると、システム100は、例えば、図示された上位椎骨27g又は下位椎骨27eなど、隣接する椎骨に配置される、新たに移植される骨固定要素22gを具備している。多軸的な延長ロッド140は、新たに移植される骨固定要素22gのアンカー座部26に延通される、脊柱固定ロッドを提供する。かくして、多軸的な延長ロッド140は、新たに移植される骨固定要素22gと、これとは別の、例えば、既に移植された骨固定組立体20の一部分である、骨固定要素22aとの間に結合される。
Referring now again to FIG. 9, the
従って、手術中には、上部載荷式の多軸的に構築された延長具105は、既に移植されている脊柱構造物又は既に移植されている骨固定要素22aを含む骨固定組立体20を、隣接する脊柱レベルとして示された隣接する骨へと延長し、修正手術中に両者間に堅固な結合を実現する。切開は、例えば、最も頭蓋側(又は最も尾側)の、既存の脊柱構造物のレベルに隣接する、脊柱レベルにおいて、修正に必要な限度で行われる。切開は、最も端の既存の骨固定要素20と、取り付けられるべき新たな椎骨とにわたって行われ、既存の骨固定要素20におけるその他の椎骨27a〜27dにわたって切開する必要はない。というのは、既存の脊柱固定ロッド24は、取り外されないからである。まず、新たな骨固定要素22gは、ロックキャップ34を除き、隣接する脊柱レベル27gに移植される。別言すれば、新たな骨固定要素22gの椎骨インプラント75は、隣接する脊柱レベル27gに移植される。同じ切開を通して、又は第2の切開を用いて、ロックキャップ34は、最も端の、例えば、最も頭蓋側の骨固定要素22a(又は最も尾側の骨固定要素22d)から、取り外される。
Thus, during surgery, the top-loaded multi-axially constructed
次に、既に移植されている骨固定要素22aに、テーパ付き止めねじ130を結合するために、テーパ付き止めねじ130の遠位端130bにあるねじ133を、アンカー座部26の内側にねじ入れる。既に移植されている椎骨インプラント22aのロックキャップ34が取り外されたので、テーパ付き止めねじ130は、既に移植されている骨固定要素22aの多軸的な椎骨インプラント75に結合できる。次に、延長ロッド140を、既に移植されている多軸的な椎骨インプラント22aと、新たに移植される椎骨インプラント22gとの間に結合するために、ループ142の内部に保持されているブッシング150を、テーパ付き止めねじ130の中間部分のまわりに配置すると共に、延長ロッド140の他端を、新たに移植された骨固定要素22gのアンカー座部26の中へ垂直下方向に挿入する。ブッシング150の球形面155と、開口部143を形成するループ142における相補的な球形の内面147とによって、ブッシング150は、ループ142の開口部143の内部にて、多軸的に回転することが許容される。二重にテーパの付けられた、ブッシング150の内面151によって、延長ロッド140をテーパ付き止めねじ130に結合する配向には自由度が得られ、というのは、対向する向きのテーパのために、延長ロッド140は、いずれの方向からも、テーパ付き止めねじ130に結合することができ、誤った向きが存在しないためである。
Next, the
次に、ロックナット160は、例えば、ロックナット160の外面又は上位面に設けられた器具係合特徴に係合することで、テーパ付き止めねじ130の近位側ないし上位側部分130aにかぶせて螺着され、延長ロッド140とブッシング150とをテーパ付き止めねじ130の中間部分130bに対して遠位方向に押し込んで前進せしめ、その間に、ブッシング150を押し広げて、内面151のテーパと、テーパ付き止めねじ130の中間部分130cの外面134とを合致させて、締り嵌めによってロックする。次に、骨アンカー30の角度配向が、アンカー座部26に対してロックされ、且つ、延長ロッド140が、骨固定要素22に固定されるまで、ロックキャップ34を、アンカー座部26の上部にねじ込む。図10Dに示すように、延長ロッド本体141は、実質的に“S字形”であり、近位端141aは、遠位端141bに対して後方に配置される。変形例としては、延長ロッド140は、実質的に直線状であるか、又は実質的に一定の若しくは可変の曲率(図14A乃至図14C参照)をもつものでも良く、近位端141aは、遠位端141bに対して後方に配置されるように、ブッシング150は配向される。従って、近位端141aは、既存の脊柱固定ロッド24の上に据え付けることができ、一方、遠位端141bは、既存の脊柱固定ロッド24に対して実質的に整列させることができる。システム100が、固定要素22及び脊柱構築延長具105の平行な列101a及び101bを具備している場合には、対向する列について上述した取付手順を繰り返す。
The
既に移植されている骨固定組立体20を、頭蓋側ではなく、尾側に延長するためには、上部載荷式の多軸的な脊柱構築延長具105を、上述したやり方で、下位の骨固定要素22dの椎骨インプラント75に結合し、新たな骨固定要素は、椎骨27eのような下位の椎骨に固定され、延長ロッド140は、上述したやり方で、最も下位の既存の固定要素22の椎骨インプラント75と新たに移植される骨固定要素との間に結合される。
In order to extend the previously implanted
システム100の上部載荷式の可能性によれば、より侵襲性の低い、より難易度の低い、及びより時間を要しない修正手術を行うことが可能になり、これは、従来の脊柱修正手術システム及び方法が、一般的に、既に移植されている脊柱構造物の全体を分解して、隣接する脊柱レベルに融合させるために、かなりの血液流出の可能性のある別の大きな切開を用いて、より長いロッドと共に再度組み立てることを必要としていたのと比較して対照的である。システム100は、一般に、必要な切開長さを短くすると共に、手術時間、血液流出、術後の痛み、及び治癒までの時間を短縮する。さらに、第1の好ましい実施形態によるシステム100によれば、複数のレベルの脊柱ロッド組立体を構築するとき、最小限の侵襲性の技術を利用でき、というのは、比較的短い長さの延長ロッド140によって、複数の固定ねじ及び延長ロッド140を単一の小さい切開に挿入し、続いて複数のレベルにわたってロッドを積み重ね、及び比較的容易な操作で延長ロッド140を固定ねじと係合できるためである。
The top-loading possibility of
ロッド140は、緩衝機構を具備することもでき、例えば、ロッド140の1つの部分とループ142との間に、必要に応じて、追加的な動きを提供できることを認識されたい。加えて、ロッド140は、全体が弾性材料から作られ、レベル間のさらに動的な結合を提供する。例えば、ロッド本体141及び/又はループ142は、ポリエーテルエーテルケトン(PEEK)材料から構築され、隣接する多軸的な椎骨インプラント75同士の間に、緩衝又は限定的な動きを許容する。ループ142、ロッド140、ブッシング150、ロックナット160、止めねじ130、脊柱ロッド42、アンカー座部26、及び/又は、システム100のその他の要素は、互いに対する要素同士の延びすぎや過度の圧縮を防ぐために、たとえある種の構成要素が運動を許容し又は動的に構築されていたとしても、互いに対する要素の終局的な運動を限定するように構成される。
It will be appreciated that the
図11A乃至図11Cを参照すると、上述の如く、システム100について、既存の構造物を、例えば、上位椎骨27g又は下位椎骨17eなど、1つの隣接する脊柱レベルに延長するものとして説明したけれども、システム100は、さらに、2以上の上部載荷式の多軸的なカスケード構築延長具105と、対応する数の新たな骨固定要素22とを具備することもでき、システムは、それまで固定されていなかった、複数の椎骨に取り付けるためにも使用することができる。例えば、多軸的に構築された延長具105は、上述したやり方で、新たに移植される骨固定要素22gに取り付けられると共に、新たに移植される骨固定要素22は、上述したやり方で、椎体27gに対して上方にある隣接する上位椎体27hに取り付けることができる。これにより、延長ロッド140は、骨固定要素22gに取り付けられた多軸的に構築された延長具105と、椎体27hに移植された新たに移植される骨固定要素22との間を結合する。従って、カスケード構築された延長具105は、既に移植された固定システムに取り付けるのではなく、新たに移植される椎体27g及び27hに取り付けることもできることを認識されたい。
Referring to FIGS. 11A-11C, as described above, the
カスケード構築された延長具の移植は、最小限の侵襲性で行うことができ、というのは、取り付けを行うすべての椎骨レベルに沿って切開を形成するのではなく、形成された単一の切開が、単一の椎骨レベルでカニューレ管を収容できるためである。移植は、切開を通って延びるカニューレ管又は開創器を通して、それぞれの椎骨レベル毎に実行でき、管をピボットさせて又は開創器をピボット若しくは拡張させて、カスケード式に構築された延長具105の移植がされるべき隣接する椎骨レベルへのアクセスを提供する。
Transplantation of cascaded extension devices can be done with minimal invasiveness because a single incision formed rather than making incisions along all vertebral levels to be attached This is because the cannula can be accommodated at a single vertebral level. Implantation can be performed at each vertebral level through a cannula tube or retractor extending through the incision, and implantation of the
図11Aに示すように、カスケード式の延長システム100は、上部載荷式の多軸的に構築された延長具105を単独で具備しても良いし、又は、複数の既に移植された対応する骨固定要素22と組み合わせても良いことを認識されたい。複数の個別の延長ロッド140は、必要に応じて、脊柱固定ロッド24及びループ142内に保持された多軸的なブッシング150と置換することができ、望ましい角度調整能力を提供すると共に、新たに移植される骨固定要素22のアンカー座部26に、上部載荷式の結合を許容する。
As shown in FIG. 11A, the cascading
従来の頚部脊柱手術の技術では、代表的に、フックを利用しており、一般的に、フックを骨に固定するための第1の浅い軌跡と、フックを脊柱ロッド120に結合するための第2の垂直な軌跡とを必要としていた。2つの別々の軌跡は、外科的部位にアクセスするための、大きな切開を必要としていた。図11Aに示したシステム100を使用した手術方法は、一般的に、それぞれの新たに移植される骨固定要素22及び上部載荷式の多軸的に構築された延長具105を移植し、延長ロッド140を導入し、及び最後にロックナット160を締め付けるために、たった1つの軌跡だけが必要になる。それゆえに、第3の好ましい実施形態によるシステム100によれば、大きな切開に代えて、経皮的な刺し傷又は1つの小さい切開を利用することができる。システム100の移植中に使用される軌跡は、広く使用されているMagerl式の技術及び軌跡と類似したものである。
Conventional cervical spine surgery techniques typically utilize a hook, and generally a first shallow trajectory for securing the hook to the bone and a first for coupling the hook to the spinal rod 120. Required two vertical trajectories. Two separate tracks required a large incision to access the surgical site. The surgical method using the
図11C及び図11Dに示すように、システム100はさらに、列101aと列101bとを連結するように構成された一方の又は両方の横断コネクタ190及び193を具備している。横断コネクタ190は、横断コネクタロッド191と、ロッド191の両端に結合されたクランプ192とを具備しており、これらは、それぞれ、列101a及び101bにおける脊柱固定ロッド24を受け入れて固定するように構成されている。横断コネクタ193は、横断コネクタロッド194を具備し、これは、任意の適当な機械的ジョイント195を用いて一緒に結合し得る、一対のロッド部分194a及び194bを形成している。横断コネクタロッド194は、第1のロッド部分194aの外端に配置された第1のループ196aと、これに対向する第2のロッド部分194bの外端に配置された第2のループ196bとを具備している。それぞれのループ196a〜bは、延長ロッド140のループ142に関して上述したように構築できる。従って、システム100は、脊柱構築延長具105に関して改変された、すなわち、延長ロッド140の代わりに横断コネクタ193が設けられた、脊柱構築延長具105’を具備している。改変された脊柱構築延長具105’は、最も外側の骨固定要素22に、上述したようにして取り付けられ、横断コネクタロッド194は、列101a及び101bの最も外側にある椎骨インプラント75の間に結合される。
As shown in FIGS. 11C and 11D, the
次に図12を参照すると、上部載荷式の多軸的に構築された延長具105は、変形例による実施形態に従って構築できることが認識されるべきである。より詳しくは、延長具105は、上述の如く構築できるけれども、延長部材139は、プレート180として構築され、近位端181aと、長手中心軸線185に沿って近位端181aとは反対側にある遠位端181bと、を形成してなるプレート本体181を有しており、このプレート本体は、さらに、近位端181aと遠位端181bとの間に配置された中間部分181cを有している。遠位端181bは、中間部分181cに対して、矢印187の如くピボット可能になっており、取り付けられるべき、下にある骨の解剖学的な形状に一致させられる。プレート本体180は、近位端181aに結合されたループ182として示される係合部材を具備している。ループ182は、ロッド140のループ142に関して上述した如く構築され、ループ182の内部には、上述したやり方で、ブッシング150が保持されている。
Referring now to FIG. 12, it should be appreciated that the top-loaded multiaxially constructed
プレート180には、中間部分181c及び遠位端181bに、複数の開口部183が穿設され、これらは、プレート本体181の長さに沿った長手方向に間隔を隔てている。開口部183は、上述した骨固定具30などの骨固定具を受け入れるようにそれぞれ構成され、骨固定具は、圧縮ねじ又はロックねじであって、プレート本体181を、下にある骨、例えば、椎体27又は椎弓板などに直接固定する。開口部183は、骨固定具を固定位置において受け入れるサイズをもった、少なくとも1つの円形の開口部184と、少なくとも1つの長手方向に細長い開口部ないしスロット186であって、骨固定具を受け入れるサイズをもち、スロット186内にて骨固定具が並進可能であるものとを具備し、骨固定具をプレート本体181に対して締め付ける前に、骨固定具と下にある骨とを整列するのを助ける。代わりに、スロット186は、椎弓形成術中にプレート本体181内に挿入された、骨移植材料を保持しても良い。図示の実施形態においては、延長プレート180は、プレート本体の幾何学的形状を、術前又は術中に調整できるように、展性を有している。1又は複数の、あるいはすべての開口部183は、ねじ無しで良く、アンカー30がプレートを下にある骨に対して圧接できるけれども、1又は複数の、あるいはすべての開口部183は、ねじ付きにしても良く、骨アンカー30は、開口部183のねじ部と合致する相補的なねじを備え、これにより、下にある骨に対して骨アンカーを圧迫することなく、下にある骨にプレート180を固定又は係止できる。
The
手術中には、延長具105は、既に移植されている、若しくは、新たに移植された、又は新たに移植可能である、多軸的な骨固定要素22に、上述したやり方で、結合される。延長プレート180の第2の端部は、椎体の椎弓板などの骨に直接、固定される。延長プレート180を具備してなる、上部載荷式の多軸的なプレート延長具105は、一般に、移植片を含むものとして構成され、とりわけ、直視下椎弓形成術(下にある骨が同種移植片である)で、及び/又は、より長い頭蓋−尾側融合構築術で、そのようにされる。例えば、プレート180を、固定されるべき椎体27にかぶせて配置し、骨固定要素22の骨アンカー30を、相補的な開口部183に挿通することで、下にある椎骨27に対して、固定要素22とプレート180との両方を固定することができる。このように、プレートは、椎弓形成術を、単一の構造物を用いる後部融合術と組み合わせられる可能性を提供する。従来の形成術では、代表的に、そのような移植片を納めるためにケーブルを利用しているが、延長プレート180によれば、一般的に、より堅固な移植片収容方法が提供され、また、延長具105によって提供される上部載荷式の多軸的な結合の可能性は、解剖学的構造が利用できないか、又は取付箇所として機能するのに不適切である場合に、堅固な固定箇所を提供することができる。さらに、上部載荷式の取付箇所は、代表的に、今日のワイヤによる技術に比べて、組み立てるのが迅速かつ容易である。
During surgery, the
次に図10A乃至図10D及び図13を参照すると、延長具105は、延長部材139を具備し、これは、ロッド206の形態であって、近位端206aと、ロッドの中心軸線210に沿って近位端とは反対側にある、遠位端206bと、近位端206aと遠位端206bとの間に配置された中間部分206cとを形成している。ロッド206は、延長部材を具備し、これは、近位端206aに結合されるループ207として示されている。ロッド206はさらに、ブッシング150を具備し、これは、ループ142に関して上述したやり方で、ループ207内に保持される。中間部分206c及び遠位端206bは、必要に応じて、ループ207に対して斜めにオフセットさせることができる。これについて、ロッド206のキットは、中間部分206c及び/又は遠位端206bと、ループ207との間の角度が異なって形成されたものを具備することができる。
Referring now to FIGS. 10A-10D and 13, the
手術中には、延長具105は、既に移植された又は新たに移植可能な、骨固定要素22を、既に移植された椎弓板貫通ねじに結合させる。より詳しくは、ロックキャップ34を取り外して、テーパ付き止めねじ130を、上述したやり方で、既に移植されている骨固定要素22に結合させる。そして、ロッド206を、骨固定要素22と椎弓板貫通ねじとの間に結合するために、ブッシング150をテーパ付き止めねじ130の中間部分130cのまわりに配置し、遠位端206bを椎弓板貫通ねじのロッド座部の中へ配置する。椎弓板貫通ねじは、椎骨インプラント75に関して上述したように構築され、当業者に知られているように、隣接する椎骨を固定して、それらを互いに融合させるために使用される。より詳しくは、椎弓板貫通ねじは、隣接する椎骨を互いに固定するために、隣接する椎骨のファセット及び椎弓板に通して挿入される。
During surgery, the
次に、ロックナット160は、テーパ付き止めねじ130の上位ないし近位側部分130aにかぶせてねじ込まれ、それにより、延長ロッド206及びブッシング150を押圧して、テーパ付き止めねじ130の中間部分130cに対して遠位方向へ前進せしめ、そうする間に、ブッシング150は押し広げられて、ブッシング150の内側のテーパと、テーパ付き止めねじ130の中間部分の外側のテーパとを合致させて、上述の如く、締り嵌めによってこれらをロックする。次に、椎弓板貫通ねじのロックキャップ34は、椎弓板貫通ねじのアンカー座部の上部にねじ込まれ、ついには、椎弓板貫通ねじの骨アンカー30の角度的な配向が、椎弓板貫通ねじのアンカー座部26に対してロックされ、延長ロッド206が椎弓板貫通ねじ組立体にロックされる。
Next, the
延長具105は、(多軸的なループ207とブッシング150とを含む)第1の端部にて、椎弓板貫通ねじに結合され、矢印211の方向に沿ってロッド軸線210を中心として回転できると共に、矢印213の方向に沿ってねじの中心軸線Bを中心として回転することができ、それにより、多軸的な回転を提供しないプレートに対して、追加的な自由度を提供することを認識されたい。
次に図9乃至図10D及び図14A及び図14Bを参照すると、固定システム100は、脊柱の頚部領域に移植された骨固定組立体20の骨固定要素22を、後頭部253に固定されるべく構成された後頭部プレート250に、結合するように構成されている。後頭部プレート250は、当業者に公知の様々な形態を呈することができ、中心本体257を具備しており、これは、延長ロッド140の遠位端141bを受け入れるべく構成された、係合部材252を具備している。例えば、係合部材252は、中心本体257を長手方向に延通する開口部であって、延長ロッド140の遠位端141bを受け入れるサイズをもつものと、延長ロッド140に対してロックされるように構成された止めねじとを具備している。一対の後頭部プレート250は、それぞれの延長ロッド140の遠位端141bに締め付けられるものとして図示され、それぞれプレート部分250a及び250bを有し、これらは、係合部材252から外方へ突出して、互いに対向している。それぞれのプレート部分250a及び250bは、ロッド140を中心として独立して回転可能であるか、又はロッド140を中心として同調して回転可能である。加えて又は代わりに、それぞれのプレート部分250a及び250bは、中心本体257を中心として屈曲できるものでも良い。それぞれのプレート部分250a及び250bは、これらに穿設された少なくとも1つの骨固定開口部255を具備し、そのサイズは、骨固定具30、例えば、ねじ又はフックを受け入れるようになっており、プレート部分250a及び250bを、後頭部など、下にある骨に固定する。
9-10D and 14A and 14B, the
手術中には、固定組立体20は、脊柱の頚部領域に事前に移植され、骨固定要素22が、下にあるそれぞれの頚部椎骨に移植される。延長具105は、最も頭蓋側にある骨固定要素22に取り付けられ、かかる骨固定要素は、上述したやり方にて、ロックキャップ34が取り外された後に、新たに移植された若しくは移植可能な、又は既に頚部椎骨Cに移植されたものである(例えば、最も頭蓋側にある骨固定要素22の椎骨インプラント75)。延長ロッド140における、第2の、ロッド形状の遠位端141bは、当業者に公知である様々な取付機構のうち任意のものを使用して、後頭部プレート250に結合される。図示の実施形態においては、システム100は、固定要素22及び脊柱構築延長具105の、第1及び第2の縦列101a及び101bを具備し、最も頭蓋側の固定要素を、後頭部として例示されている、隣接する骨に結合させる。
During surgery, the
上部載荷式の多軸的に構築された延長具105によれば、外科医は、後頭部を頚部脊柱に結合するとき、蝶番的な能力を有し、手術は容易になり、自由度が高まる。延長ロッド140は、ループ142に対して所望の角度に事前に曲げておくことができ、その長さは、こうした用途に使用されてきた従来の蝶番ロッドに比べて短いものである。それゆえに、上部載荷式の多軸的に構築された延長具105は、その取扱い、並びに頚部脊柱と後頭部との間の結合について、より容易である。さらに、上部載荷式の多軸的に構築された延長具105によれば、外科医は、頚部脊柱形成術を行ってから、後頭部融合のためのハードウェアを追加するのが望ましいか否かを判断することができるようになるが、これは、従来の蝶番ロッドが、手術開始時に器具使用とハードウェアを確定しなければならなかったのとは対照的である。
With the top-loaded multiaxially constructed
本願では、複数の修正コネクタの実施形態が開示されたことを認識されたい。従って、脊柱固定修正コネクタのキットを提供することができ、それは、複数の修正コネクタを含み、それぞれの修正コネクタは、少なくとも1つの椎体を隣接する骨、例えば、隣接する椎体、又は後頭部に結合するように構成される。修正コネクタキット内にある複数の修正コネクタのうち、少なくとも1つの修正コネクタは、キット内にある複数の修正コネクタのうち、少なくとも1つのアンカーとは異なるように形成される。例えば、異なる修正コネクタは、異なる長さを有するか、又は異なる構造の多軸的内延長部材139を有することができる。代わりに又は加えて、異なる修正コネクタのねじ130は、テーパ付きではなくて、直線状であり、止めねじ130は、ブッシング150をそれぞれのループ内にロックせず、それにより、ブッシングは、取り付け後に、それぞれのループ内にて関節になるようにしても良い。別言すれば、ループ142は、もって多軸的な延長部材139は、ねじ130及びねじが取り付けられた椎骨インプラント75に対するロック位置において、ピボット又は関節運動をすることができる。代わりに又は加えて、ねじ130の遠位側部分130bは、ボア孔又は完全な貫通孔を具備し、これが、遠位側に配置された雌ねじを備えるようにして、既に移植された又は新たに移植される椎骨インプラント75におけるアンカー座部26の外面に設けた雄ねじと螺合するように構成し、これにより、様々な椎骨インプラント又はフックであって、雌ねじ又はロックキャップと併用すべく構成された雄ねじを具備するものに適応させても良い。
It should be appreciated that multiple correction connector embodiments have been disclosed herein. Thus, a spinal fixation correction connector kit can be provided, which includes a plurality of correction connectors, each correction connector connecting at least one vertebral body to an adjacent bone, eg, an adjacent vertebral body, or occipital region. Configured to combine. Of the plurality of correction connectors in the correction connector kit, at least one correction connector is formed different from at least one anchor of the plurality of correction connectors in the kit. For example, different correction connectors may have different lengths or differently configured polyaxial
当業者は認識するだろうが、上述した実施形態については、その広い発明的な概念から逸脱せずに、様々な変更を加えることができる。それゆえ、本発明は、開示された特定の実施形態に限定されるものではなく、本願の開示によって定められた本発明の精神及び範囲内における変形例を包含することを意図している。 Those skilled in the art will recognize that various modifications can be made to the above-described embodiments without departing from the broad inventive concept. Thus, the present invention is not intended to be limited to the particular embodiments disclosed, but is intended to encompass modifications within the spirit and scope of the present invention as defined by the present disclosure.
Claims (23)
延長部材であって、本体と、本体に結合される係合部材とを含み、延長部材は係合部材を通って延びる開口部を形成する、上記延長部材と、
開口部の中に配置されるブッシングと、
係合部材を椎骨インプラントに結合すべく構成されてなる固定具であって、この固定具は、第1のアンカー座部内に配置された脊柱固定ロッドを捕捉し、それにより、第1のアンカー座部及び脊柱固定ロッドに対して第1の骨アンカーの位置を固定するように、第1のアンカー座部に取り付けられるべく構成されてなる遠位側部分を形成する、上記固定具と、
第2の骨アンカーであって、延長部材を、椎骨に隣接して配置された、下にある骨に取り付ける、上記第2の骨アンカーと、を備え、
延長部材は、ブッシングに対して多軸的にピボット可能である、
ことを特徴とする延長システム。 An extension system configured to be operatively coupled to a vertebral implant coupled to a vertebra, the implant including a first bone anchor and a first anchor seat for receiving the first bone anchor And this extension system
An extension member comprising a body and an engagement member coupled to the body, the extension member forming an opening extending through the engagement member; and
A bushing disposed in the opening;
A fixation device configured to couple an engagement member to a vertebral implant, the fixation device capturing a spinal fixation rod disposed within the first anchor seat, thereby providing a first anchor seat. Said fixation device forming a distal portion configured to be attached to a first anchor seat so as to fix the position of the first bone anchor relative to the part and the spinal fixation rod ;
A second bone anchor, wherein the second bone anchor is attached to an underlying bone disposed adjacent to the vertebra,
The extension member is pivotable in multiple axes with respect to the bushing.
An extension system characterized by that.
複数の構造延長部分を備え、それぞれの構造延長部分が、
第1の下にある骨の中に移植されるべく構成された第1の骨アンカーと、第1の骨アンカーを受けるべく構成された第1の骨アンカー座部と、
近位端と、これとは反対側にあり、近位端に比べて低くなっている遠位端とを形成する本体と、近位端に結合される係合部材とを具備してなる延長部材と、
第1の骨アンカー座部に係合部材を結合するように構成されてなる固定具であって、この固定具は、第1の骨アンカー座部内に配置された脊柱固定ロッドを捕捉し、それにより、第1の骨アンカー座部及び脊柱固定ロッドに対して第1の骨アンカーの位置を固定するように、第1の骨アンカー座部に取り付けられるべく構成されてなる遠位側部分を形成する、上記固定具と、
延長部材の遠位端を第2の下にある骨に取り付けるべく構成された、第2の骨アンカーと、
を具備していることを特徴とするカスケード式延長部分システム。 A cascade extension system configured to be secured to a plurality of underlying bones, wherein the cascade extension system is
Provided with a plurality of structural extensions, each structural extension,
The first bone anchor configured to be implanted in the bone underlying the first, the first bone anchor seat portion configured to receive a first bone anchor,
An extension comprising a body forming a proximal end and a distal end opposite to and lower than the proximal end, and an engagement member coupled to the proximal end Members,
A fixture configured to couple an engagement member to a first bone anchor seat, the fixture captures a spinal fixation rod disposed within the first bone anchor seat, and To form a distal portion configured to be attached to the first bone anchor seat so as to fix the position of the first bone anchor relative to the first bone anchor seat and the spinal fixation rod. And the above fixture ,
A second bone anchor configured to attach the distal end of the extension member to the second underlying bone;
A cascading extension system comprising:
Applications Claiming Priority (3)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US18790209P | 2009-06-17 | 2009-06-17 | |
| US61/187,902 | 2009-06-17 | ||
| PCT/US2010/039037 WO2010148231A1 (en) | 2009-06-17 | 2010-06-17 | Revision connector for spinal constructs |
Publications (3)
| Publication Number | Publication Date |
|---|---|
| JP2012530550A JP2012530550A (en) | 2012-12-06 |
| JP2012530550A5 JP2012530550A5 (en) | 2014-09-11 |
| JP5654584B2 true JP5654584B2 (en) | 2015-01-14 |
Family
ID=42556671
Family Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| JP2012516310A Active JP5654584B2 (en) | 2009-06-17 | 2010-06-17 | Correction connector for spine construction |
Country Status (8)
| Country | Link |
|---|---|
| US (3) | US9510862B2 (en) |
| EP (1) | EP2442738B1 (en) |
| JP (1) | JP5654584B2 (en) |
| KR (1) | KR20120039622A (en) |
| CN (1) | CN102458279B (en) |
| BR (1) | BRPI1012921A2 (en) |
| CA (1) | CA2764841A1 (en) |
| WO (1) | WO2010148231A1 (en) |
Families Citing this family (74)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US8475495B2 (en) | 2004-04-08 | 2013-07-02 | Globus Medical | Polyaxial screw |
| US7503924B2 (en) | 2004-04-08 | 2009-03-17 | Globus Medical, Inc. | Polyaxial screw |
| US8100946B2 (en) | 2005-11-21 | 2012-01-24 | Synthes Usa, Llc | Polyaxial bone anchors with increased angulation |
| US9439681B2 (en) | 2007-07-20 | 2016-09-13 | DePuy Synthes Products, Inc. | Polyaxial bone fixation element |
| US9060813B1 (en) | 2008-02-29 | 2015-06-23 | Nuvasive, Inc. | Surgical fixation system and related methods |
| EP2160989B1 (en) * | 2008-09-05 | 2012-05-02 | BIEDERMANN MOTECH GmbH | Stabilization device for bones, in particular for the spinal column |
| PL2337512T3 (en) | 2008-09-12 | 2012-09-28 | Synthes Gmbh | Spinal stabilizing and guiding fixation system |
| KR20110081208A (en) | 2008-09-29 | 2011-07-13 | 신세스 게엠바하 | Polyaxial bottom-loading screw and rod assembly |
| BRPI0920181A2 (en) | 2008-11-03 | 2015-12-29 | Synthes Gmbh | uni-planar bone fixation set |
| JP2012523927A (en) | 2009-04-15 | 2012-10-11 | ジンテス ゲゼルシャフト ミット ベシュレンクテル ハフツング | Correction connector for spinal components |
| US11229457B2 (en) * | 2009-06-15 | 2022-01-25 | Roger P. Jackson | Pivotal bone anchor assembly with insert tool deployment |
| BRPI1012921A2 (en) | 2009-06-17 | 2016-04-05 | Synthes Gmbh | revision connector for spinal construction |
| US8246657B1 (en) | 2009-06-29 | 2012-08-21 | Nuvasive, Inc. | Spinal cross connector |
| US20110087287A1 (en) * | 2009-10-09 | 2011-04-14 | Custom Spine, Inc. | Rod-to-Rod Connector |
| WO2011053962A1 (en) * | 2009-11-02 | 2011-05-05 | Life Spine, Inc. | Laminoplasty rod system |
| US9198696B1 (en) | 2010-05-27 | 2015-12-01 | Nuvasive, Inc. | Cross-connector and related methods |
| US9044274B2 (en) * | 2010-12-01 | 2015-06-02 | Amendia, Inc. | Bone screw system |
| US9247964B1 (en) | 2011-03-01 | 2016-02-02 | Nuasive, Inc. | Spinal Cross-connector |
| US9387013B1 (en) | 2011-03-01 | 2016-07-12 | Nuvasive, Inc. | Posterior cervical fixation system |
| US8888827B2 (en) | 2011-07-15 | 2014-11-18 | Globus Medical, Inc. | Orthopedic fixation devices and methods of installation thereof |
| US9993269B2 (en) | 2011-07-15 | 2018-06-12 | Globus Medical, Inc. | Orthopedic fixation devices and methods of installation thereof |
| US9186187B2 (en) | 2011-07-15 | 2015-11-17 | Globus Medical, Inc. | Orthopedic fixation devices and methods of installation thereof |
| US9358047B2 (en) | 2011-07-15 | 2016-06-07 | Globus Medical, Inc. | Orthopedic fixation devices and methods of installation thereof |
| US9198694B2 (en) | 2011-07-15 | 2015-12-01 | Globus Medical, Inc. | Orthopedic fixation devices and methods of installation thereof |
| US9381048B2 (en) | 2011-08-31 | 2016-07-05 | DePuy Synthes Products, Inc. | Devices and methods for cervical lateral fixation |
| DE202011107821U1 (en) * | 2011-09-09 | 2012-02-23 | Humantech Germany Gmbh | Rod extension system for the extension of an existing screw-rod implant for fixation of the spine |
| US8337532B1 (en) | 2011-12-08 | 2012-12-25 | Spine Wave, Inc. | Methods for percutaneously extending an existing spinal construct |
| EP2606841B1 (en) * | 2011-12-23 | 2016-03-09 | Biedermann Technologies GmbH & Co. KG | Polyaxial bone anchoring device |
| US8906067B2 (en) * | 2012-03-21 | 2014-12-09 | Warsaw Orthopedic, Inc. | Posterior incremental spinal fixation system |
| US9968379B2 (en) * | 2012-10-04 | 2018-05-15 | Loubert S. Suddaby | Subcutaneous implantable device for gradually aligning a spine and subcutaneous implantable device for gradually lengthening a bone |
| US9259247B2 (en) | 2013-03-14 | 2016-02-16 | Medos International Sarl | Locking compression members for use with bone anchor assemblies and methods |
| CN103405269A (en) * | 2013-07-22 | 2013-11-27 | 苏州欣荣博尔特医疗器械有限公司 | Spine screw with rotary screw seat |
| KR101599603B1 (en) | 2013-08-26 | 2016-03-03 | 경북대학교 산학협력단 | Medical inserting apparatus |
| FR3018442B1 (en) | 2014-03-12 | 2016-03-25 | Safe Orthopaedics | IMPROVED ANCHOR SCREW FOR VERTEBRATES STABILIZATION AND OSTEOSYNTHESIS SYSTEM COMPRISING SUCH SCREWS |
| CN104207836A (en) * | 2014-09-04 | 2014-12-17 | 浙江嘉佑医疗器械有限公司 | Pedicle screw special for PLIF (Posterior Lumbar Interbody Fusion) |
| US9724131B2 (en) * | 2014-09-25 | 2017-08-08 | DePuy Synthes Products, Inc. | Spinal connectors and related methods |
| FR3027207A1 (en) * | 2014-10-15 | 2016-04-22 | Medicrea Int | MATERIAL OF VERTEBRAL OSTEOSYNTHESIS |
| KR101639887B1 (en) | 2014-11-11 | 2016-07-14 | 경북대학교 산학협력단 | A system for fixing cervical vertebrae and a driver used for an appratus for fixing cervical vertebrae |
| KR101608949B1 (en) | 2014-11-19 | 2016-04-04 | 경북대학교 산학협력단 | A system for fixing cervical vertebrae, an appratus for fixing cervical vertebrae and a driver used for an appratus for fixing cervical vertebrae |
| US9924972B2 (en) | 2015-02-04 | 2018-03-27 | James J. Yue | System and method for spinal fusion |
| US9717541B2 (en) | 2015-04-13 | 2017-08-01 | DePuy Synthes Products, Inc. | Lamina implants and methods for spinal decompression |
| DE102015109481A1 (en) * | 2015-06-15 | 2016-12-15 | Aesculap Ag | Pedicle screw with radially offset guide |
| KR101670768B1 (en) | 2015-07-16 | 2016-10-31 | 경북대학교 산학협력단 | Screw anchor assembly |
| US9855078B2 (en) * | 2015-10-05 | 2018-01-02 | Globus Medical, Inc. | Spinal anchoring system |
| US10874445B2 (en) | 2015-10-13 | 2020-12-29 | Kyungpook National University Industry-Academic Cooperation Foundation | Screw fixing apparatus |
| JP6921826B2 (en) * | 2015-12-15 | 2021-08-18 | マフホウズ,モハメド ラシュワン | Thigh base plate THA |
| KR101712610B1 (en) * | 2015-12-29 | 2017-03-06 | 경북대학교 산학협력단 | A rod connecter |
| US10321939B2 (en) | 2016-05-18 | 2019-06-18 | Medos International Sarl | Implant connectors and related methods |
| US10517647B2 (en) | 2016-05-18 | 2019-12-31 | Medos International Sarl | Implant connectors and related methods |
| KR101791004B1 (en) | 2016-06-08 | 2017-10-27 | 경북대학교 산학협력단 | Screw anchor assembly and a method for using the same to pedicle screw instrumentation |
| US10413330B2 (en) | 2016-08-09 | 2019-09-17 | Warsaw Orthopedic, Inc. | Spinal implant system and method |
| US10543022B2 (en) | 2016-10-11 | 2020-01-28 | Warsaw Orthopedic, Inc. | Spinal implant system and method |
| US10966760B2 (en) * | 2016-10-28 | 2021-04-06 | Warsaw Orthopedic, Inc. | Spinal implant system and method |
| US10398476B2 (en) | 2016-12-13 | 2019-09-03 | Medos International Sàrl | Implant adapters and related methods |
| US10492835B2 (en) | 2016-12-19 | 2019-12-03 | Medos International Sàrl | Offset rods, offset rod connectors, and related methods |
| US10238432B2 (en) * | 2017-02-10 | 2019-03-26 | Medos International Sàrl | Tandem rod connectors and related methods |
| US10966761B2 (en) | 2017-03-28 | 2021-04-06 | Medos International Sarl | Articulating implant connectors and related methods |
| US10561454B2 (en) | 2017-03-28 | 2020-02-18 | Medos International Sarl | Articulating implant connectors and related methods |
| US10258386B2 (en) | 2017-06-15 | 2019-04-16 | Warsaw Orthopedic, Inc. | Spinal construct and method |
| US10927835B2 (en) * | 2017-11-02 | 2021-02-23 | Emerson Climate Technologies, Inc. | Scroll compressor with scroll bolt clamp joint |
| US11076890B2 (en) | 2017-12-01 | 2021-08-03 | Medos International Sàrl | Rod-to-rod connectors having robust rod closure mechanisms and related methods |
| IT201800002749A1 (en) * | 2018-02-16 | 2019-08-16 | Orthofix Srl | Quick-connect clamp for external fixation systems |
| CN108553153A (en) * | 2018-05-15 | 2018-09-21 | 郭志良 | A kind of backbone fixation kit |
| CN110604609A (en) * | 2018-06-14 | 2019-12-24 | 港大科桥有限公司 | Bone implant device |
| US11234738B2 (en) | 2018-11-16 | 2022-02-01 | Roger P. Jackson | Pivotal bone anchor assembly having a deployable collet insert with internal pressure ring |
| CN109316231A (en) * | 2018-12-03 | 2019-02-12 | 重庆医科大学附属第二医院 | Percutaneous posterior cervical single open-door internal fixation system |
| US12082849B2 (en) | 2019-04-12 | 2024-09-10 | Orthopediatrics Corp. | Dual tether support of vertebra |
| US10918421B2 (en) * | 2019-05-07 | 2021-02-16 | Warsaw Orthopedic, Inc. | Spinal implant system and methods of use |
| US20210290272A1 (en) * | 2020-01-13 | 2021-09-23 | Xiangyang Ma | Customized posterior atlantoaxial reduction fixatorwith screws and rods |
| US11974785B2 (en) | 2020-10-16 | 2024-05-07 | Globus Medical, Inc | Band clamp implants |
| US11771475B2 (en) | 2020-10-07 | 2023-10-03 | Globus Medical, Inc. | Systems and methods for surgical procedures using band clamp implants and tensioning instruments |
| CN112155704B (en) * | 2020-10-28 | 2022-02-01 | 陈文祥 | Universal centrum repositor used in orthopedic spine operation |
| US11376046B1 (en) | 2021-02-01 | 2022-07-05 | Warsaw Orthopedic, Inc. | Spinal implant system and method |
| US11331125B1 (en) | 2021-10-07 | 2022-05-17 | Ortho Inventions, Llc | Low profile rod-to-rod coupler |
Family Cites Families (447)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US405546A (en) | 1889-06-18 | Insulator | ||
| US513630A (en) | 1894-01-30 | Detachable electric-wire-holding device | ||
| US802896A (en) | 1904-11-01 | 1905-10-24 | Nicholas W Webb | Electric lock. |
| US2005348A (en) | 1932-05-23 | 1935-06-18 | Anthony G M Michell | Nut, screw, and like article |
| US2396925A (en) | 1942-08-01 | 1946-03-19 | Adel Prec Products Corp | Subassembly conduit clip |
| US2338659A (en) | 1942-10-24 | 1944-01-04 | Adel Prec Products Corp | Conduit clip and supporting bracket |
| GB820252A (en) | 1957-10-04 | 1959-09-16 | Standard Telephones Cables Ltd | Semiconductor device |
| US3173987A (en) | 1963-03-04 | 1965-03-16 | Lumidor Products Corp | Terminal box with yoke and clip supporting means for cables |
| US3463427A (en) | 1967-08-07 | 1969-08-26 | Illinois Tool Works | Cable strap |
| US4447934A (en) | 1982-06-07 | 1984-05-15 | National Molding Corporation | Cable harness |
| US4601491A (en) | 1983-10-19 | 1986-07-22 | Vetco Offshore, Inc. | Pipe connector |
| US4719905B1 (en) | 1985-11-01 | 1995-10-31 | Acromed Corp | Apparatus and method for maintaining vertebrae in a desired relationship |
| DE3614101C1 (en) | 1986-04-25 | 1987-10-22 | Juergen Prof Dr Med Harms | Pedicle screw |
| US4805602A (en) | 1986-11-03 | 1989-02-21 | Danninger Medical Technology | Transpedicular screw and rod system |
| US4846614A (en) | 1986-12-08 | 1989-07-11 | Rolf Steinbock | Differential thread for transfer of screw thread forces |
| DE3708638A1 (en) | 1987-03-17 | 1988-09-29 | Grafelmann Hans L | SELF-CUTTING SCREW-IN BONE IMPLANT FOR DENTAL PURPOSES |
| JPH051947Y2 (en) | 1987-09-04 | 1993-01-19 | ||
| US5468241A (en) | 1988-02-18 | 1995-11-21 | Howmedica Gmbh | Support device for the human vertebral column |
| FR2633177B1 (en) | 1988-06-24 | 1991-03-08 | Fabrication Materiel Orthopedi | IMPLANT FOR A SPINAL OSTEOSYNTHESIS DEVICE, ESPECIALLY IN TRAUMATOLOGY |
| US4936851A (en) | 1988-08-26 | 1990-06-26 | Colin Electronics Co., Ltd. | Analytic bone implant |
| FR2642643B1 (en) | 1989-02-09 | 1991-05-10 | Vignaud Jean Louis | SPINAL INSTRUMENTATION FOR UNIVERSAL PEDICULAR FIXATION WITH MICROMETRIC ADJUSTMENT DIAPASON SCREW |
| CH678803A5 (en) | 1989-07-12 | 1991-11-15 | Sulzer Ag | |
| DE3923996A1 (en) | 1989-07-20 | 1991-01-31 | Lutz Biedermann | RECORDING PART FOR JOINTLY CONNECTING TO A SCREW FOR MAKING A PEDICLE SCREW |
| US5360431A (en) | 1990-04-26 | 1994-11-01 | Cross Medical Products | Transpedicular screw system and method of use |
| DE4115959C1 (en) | 1991-05-13 | 1993-04-15 | Eberle Medizintechnische Elemente Gmbh, 7131 Wurmberg, De | |
| US5116337A (en) | 1991-06-27 | 1992-05-26 | Johnson Lanny L | Fixation screw and method for ligament reconstruction |
| DE9112176U1 (en) | 1991-09-30 | 1991-11-14 | Howmedica GmbH, 2314 Schönkirchen | Vertebral body spacer |
| US5242446A (en) | 1992-01-02 | 1993-09-07 | Acromed Corporation | Connector for a spinal column corrective device |
| DE9202745U1 (en) | 1992-03-02 | 1992-04-30 | Howmedica Gmbh, 2314 Schoenkirchen | Device for bracing vertebrae of the human spine |
| US5270678A (en) * | 1992-03-06 | 1993-12-14 | Walker Magnetics Group, Inc. | Magnetic rail chuck |
| US5304178A (en) | 1992-05-29 | 1994-04-19 | Acromed Corporation | Sublaminar wire |
| DE59301618D1 (en) | 1992-06-04 | 1996-03-28 | Synthes Ag | Osteosynthetic fastener |
| US5501684A (en) | 1992-06-25 | 1996-03-26 | Synthes (U.S.A.) | Osteosynthetic fixation device |
| DE59305375D1 (en) | 1992-08-12 | 1997-03-20 | Synthes Ag | Spine fixation element |
| GB9217578D0 (en) | 1992-08-19 | 1992-09-30 | Surgicarft Ltd | Surgical implants,etc |
| DE4228909C2 (en) | 1992-08-28 | 1994-06-09 | Ethicon Gmbh | Endoscopic instrument for the application of ligature binders and ligature binders |
| US5312410A (en) | 1992-12-07 | 1994-05-17 | Danek Medical, Inc. | Surgical cable tensioner |
| DE4243951C2 (en) | 1992-12-23 | 1997-07-03 | Plus Endoprothetik Ag | Device for stiffening a spinal column section consisting of at least two vertebrae |
| US5306275A (en) | 1992-12-31 | 1994-04-26 | Bryan Donald W | Lumbar spine fixation apparatus and method |
| US5498262A (en) | 1992-12-31 | 1996-03-12 | Bryan; Donald W. | Spinal fixation apparatus and method |
| US5413576A (en) | 1993-02-10 | 1995-05-09 | Rivard; Charles-Hilaire | Apparatus for treating spinal disorder |
| FR2702362B3 (en) | 1993-02-24 | 1995-04-14 | Soprane Sa | Fixator for osteosynthesis of the lumbosacral spine. |
| DE9302700U1 (en) | 1993-02-25 | 1993-04-08 | Howmedica GmbH, 2314 Schönkirchen | Device for setting up a spine |
| DE4307576C1 (en) | 1993-03-10 | 1994-04-21 | Biedermann Motech Gmbh | Bone screw esp. for spinal column correction - has U=shaped holder section for receiving straight or bent rod |
| WO1994020029A1 (en) | 1993-03-11 | 1994-09-15 | Wilson Greatbatch Ltd. | Laparoscopic surgical grasper |
| CA2106776C (en) | 1993-03-15 | 1998-12-29 | Johannes Fridolin Schlapfer | Hook with screw for the treatment of deformities of the spine |
| US5540698A (en) | 1993-04-21 | 1996-07-30 | Amei Technologies Inc. | System and method for securing a medical cable |
| US5449361A (en) | 1993-04-21 | 1995-09-12 | Amei Technologies Inc. | Orthopedic cable tensioner |
| US5306285A (en) | 1993-04-30 | 1994-04-26 | Komet Medical | Surgical saw blade |
| EP0650344B1 (en) | 1993-05-11 | 1998-02-18 | Synthes AG, Chur | Osteo-synthetic securing component and manipulation aid therefor |
| DE4316542C1 (en) | 1993-05-18 | 1994-07-21 | Schaefer Micomed Gmbh | Osteosynthesis device |
| US5282825A (en) | 1993-06-02 | 1994-02-01 | Muck Kin C | Surgical ligaturing and animal restraining device |
| US6077262A (en) | 1993-06-04 | 2000-06-20 | Synthes (U.S.A.) | Posterior spinal implant |
| US5527183A (en) | 1993-08-18 | 1996-06-18 | Collaborative Enterprises, Inc. | Endosseous implant system |
| FR2709246B1 (en) | 1993-08-27 | 1995-09-29 | Martin Jean Raymond | Dynamic implanted spinal orthosis. |
| DE4329220A1 (en) | 1993-08-31 | 1995-03-09 | Volkmar Dipl Ing Dr Me Jansson | Medical wire-twisting forceps |
| US5395374A (en) | 1993-09-02 | 1995-03-07 | Danek Medical, Inc. | Orthopedic cabling method and apparatus |
| DE9314297U1 (en) | 1993-09-22 | 1994-04-14 | Schäfer micomed GmbH, 73614 Schorndorf | Bone surgery holding device |
| AU693498B2 (en) | 1993-11-19 | 1998-07-02 | Cross Medical Products, Inc. | Rod anchor seat having sliding closure member |
| US5466237A (en) | 1993-11-19 | 1995-11-14 | Cross Medical Products, Inc. | Variable locking stabilizer anchor seat and screw |
| WO1995022294A1 (en) | 1994-02-17 | 1995-08-24 | Surgical Accessories, Inc. | Fastener and tensioner for bone securing cable |
| DE9402839U1 (en) | 1994-02-22 | 1994-04-14 | Howmedica GmbH, 24232 Schönkirchen | Device for setting up a spine with damaged vertebrae |
| US5536270A (en) | 1994-02-24 | 1996-07-16 | Pioneer Laboratories, Inc. | Cable system for bone securance |
| US5545168A (en) | 1994-03-11 | 1996-08-13 | Burke; Dennis W. | Apparatus for both tensioning and crimping a surgical wire |
| AU689846B2 (en) | 1994-03-29 | 1998-04-09 | Zimmer Gmbh | Screw made of biodegradable material for bone surgery purposes, and screwdriver suitable therefor |
| AU4089697A (en) | 1994-05-25 | 1998-03-19 | Roger P Jackson | Apparatus and method for spinal fixation and correction of spinal deformities |
| DE9409123U1 (en) | 1994-06-04 | 1994-09-01 | Howmedica GmbH, 24232 Schönkirchen | Device for stabilizing or compressing or distracting sections of the spine |
| JP3267451B2 (en) | 1994-07-29 | 2002-03-18 | 株式会社パイオラックス | Band clip |
| FR2724553B1 (en) | 1994-09-15 | 1996-12-20 | Tornier Sa | EXTERNAL OR INTERNAL FIXER FOR THE REPAIR OF FRACTURES OR ARTHROPLASTIES OF THE SKELETON |
| CA2156027C (en) | 1994-10-04 | 2006-07-18 | Keith Ratcliff | Surgical retractor |
| JPH08112291A (en) | 1994-10-17 | 1996-05-07 | Terumo Corp | Screw fixing system |
| US5620443A (en) | 1995-01-25 | 1997-04-15 | Danek Medical, Inc. | Anterior screw-rod connector |
| US5605457A (en) | 1995-02-13 | 1997-02-25 | Crystal Medical Technology, A Division Of Folsom Metal Products, Inc. | Implant connector |
| US5643260A (en) | 1995-02-14 | 1997-07-01 | Smith & Nephew, Inc. | Orthopedic fixation system |
| US5605458A (en) | 1995-03-06 | 1997-02-25 | Crystal Medical Technology, A Division Of Folsom Metal Products, Inc. | Negative load flank implant connector |
| FR2731344B1 (en) | 1995-03-06 | 1997-08-22 | Dimso Sa | SPINAL INSTRUMENTATION ESPECIALLY FOR A ROD |
| US5562661A (en) | 1995-03-16 | 1996-10-08 | Alphatec Manufacturing Incorporated | Top tightening bone fixation apparatus |
| US5669911A (en) | 1995-04-13 | 1997-09-23 | Fastenetix, L.L.C. | Polyaxial pedicle screw |
| US5882350A (en) | 1995-04-13 | 1999-03-16 | Fastenetix, Llc | Polyaxial pedicle screw having a threaded and tapered compression locking mechanism |
| US5888204A (en) | 1996-04-15 | 1999-03-30 | Fastenetix, Llc | Acetabular cup having capped polyaxial locking screws |
| US6780186B2 (en) | 1995-04-13 | 2004-08-24 | Third Millennium Engineering Llc | Anterior cervical plate having polyaxial locking screws and sliding coupling elements |
| US5520690A (en) | 1995-04-13 | 1996-05-28 | Errico; Joseph P. | Anterior spinal polyaxial locking screw plate assembly |
| US5607304A (en) | 1995-04-17 | 1997-03-04 | Crystal Medical Technology, A Division Of Folsom Metal Products, Inc. | Implant connector |
| EP0837656B1 (en) | 1995-07-13 | 2003-12-03 | Fastenetix, L.L.C. | A polyaxial locking mechanism |
| US5554157A (en) | 1995-07-13 | 1996-09-10 | Fastenetix, L.L.C. | Rod securing polyaxial locking screw and coupling element assembly |
| US5549608A (en) | 1995-07-13 | 1996-08-27 | Fastenetix, L.L.C. | Advanced polyaxial locking screw and coupling element device for use with rod fixation apparatus |
| US5584834A (en) | 1995-07-13 | 1996-12-17 | Fastenetix, L.L.C. | Polyaxial locking screw and coupling element assembly for use with side loading rod fixation apparatus |
| US5586984A (en) | 1995-07-13 | 1996-12-24 | Fastenetix, L.L.C. | Polyaxial locking screw and coupling element assembly for use with rod fixation apparatus |
| US5609594A (en) | 1995-07-13 | 1997-03-11 | Fastenetix Llc | Extending hook and polyaxial coupling element device for use with side loading road fixation devices |
| US5578033A (en) | 1995-07-13 | 1996-11-26 | Fastenetix, L.L.C. | Advanced polyaxial locking hook and coupling element device for use with side loading rod fixation devices |
| US5609593A (en) | 1995-07-13 | 1997-03-11 | Fastenetix, Llc | Advanced polyaxial locking hook and coupling element device for use with top loading rod fixation devices |
| US5733285A (en) | 1995-07-13 | 1998-03-31 | Fastenetix, Llc | Polyaxial locking mechanism |
| US5575792A (en) | 1995-07-14 | 1996-11-19 | Fastenetix, L.L.C. | Extending hook and polyaxial coupling element device for use with top loading rod fixation devices |
| US5601429A (en) | 1995-08-11 | 1997-02-11 | Blacklock; Gordon D. | Dental implant anchor |
| US5645544A (en) * | 1995-09-13 | 1997-07-08 | Danek Medical, Inc. | Variable angle extension rod |
| US6273914B1 (en) * | 1995-09-28 | 2001-08-14 | Sparta, Inc. | Spinal implant |
| US5683392A (en) | 1995-10-17 | 1997-11-04 | Wright Medical Technology, Inc. | Multi-planar locking mechanism for bone fixation |
| US5688273A (en) | 1995-10-23 | 1997-11-18 | Fastenetix, Llc. | Spinal implant apparatus having a single central rod and plow hooks |
| US5810818A (en) | 1995-10-23 | 1998-09-22 | Fastenetix, Llc | Spinal hook implant having a low blade and S swivel hook |
| DE29600879U1 (en) | 1996-01-19 | 1996-03-28 | Howmedica GmbH, 24232 Schönkirchen | Spinal implant |
| US5704939A (en) | 1996-04-09 | 1998-01-06 | Justin; Daniel F. | Intramedullary skeletal distractor and method |
| US5667508A (en) | 1996-05-01 | 1997-09-16 | Fastenetix, Llc | Unitary locking cap for use with a pedicle screw |
| FR2748387B1 (en) | 1996-05-13 | 1998-10-30 | Stryker France Sa | BONE FIXATION DEVICE, IN PARTICULAR TO THE SACRUM, IN OSTEOSYNTHESIS OF THE SPINE |
| US5683404A (en) | 1996-06-05 | 1997-11-04 | Metagen, Llc | Clamp and method for its use |
| DE19627864C2 (en) | 1996-07-11 | 2003-05-08 | Aesculap Ag & Co Kg | Surgical jig |
| US5694760A (en) | 1996-07-19 | 1997-12-09 | General Electric Company | Cumbustor lean flameout control |
| US5797911A (en) | 1996-09-24 | 1998-08-25 | Sdgi Holdings, Inc. | Multi-axial bone screw assembly |
| US5879350A (en) | 1996-09-24 | 1999-03-09 | Sdgi Holdings, Inc. | Multi-axial bone screw assembly |
| US5885286A (en) | 1996-09-24 | 1999-03-23 | Sdgi Holdings, Inc. | Multi-axial bone screw assembly |
| US5964760A (en) | 1996-10-18 | 1999-10-12 | Spinal Innovations | Spinal implant fixation assembly |
| US5863293A (en) | 1996-10-18 | 1999-01-26 | Spinal Innovations | Spinal implant fixation assembly |
| US5782831A (en) | 1996-11-06 | 1998-07-21 | Sdgi Holdings, Inc. | Method an device for spinal deformity reduction using a cable and a cable tensioning system |
| US5728098A (en) | 1996-11-07 | 1998-03-17 | Sdgi Holdings, Inc. | Multi-angle bone screw assembly using shape-memory technology |
| ATE234046T1 (en) | 1996-12-12 | 2003-03-15 | Synthes Ag | DEVICE FOR CONNECTING A LONG SUPPORT TO A PEDICLE SCREW |
| US6485494B1 (en) | 1996-12-20 | 2002-11-26 | Thomas T. Haider | Pedicle screw system for osteosynthesis |
| US6001098A (en) | 1997-01-17 | 1999-12-14 | Howmedica Gmbh | Connecting element for spinal stabilizing system |
| EP0954247B1 (en) | 1997-01-22 | 2005-11-23 | Synthes Ag Chur | Device for connecting a longitudinal bar to a pedicle screw |
| US5899940A (en) | 1997-02-11 | 1999-05-04 | Carchidi; Joseph Edward | Maxillofacial anchoring system for alveolar and small bone skeletal distraction |
| US5951287A (en) | 1997-04-17 | 1999-09-14 | Hawkinson; Roy T. | Dental implant failed fastener recovery systems, devices and methods |
| US6248105B1 (en) | 1997-05-17 | 2001-06-19 | Synthes (U.S.A.) | Device for connecting a longitudinal support with a pedicle screw |
| DE19720782B4 (en) | 1997-05-17 | 2004-12-09 | Synthes Ag Chur, Chur | Device for connecting a side member to a pedicle screw |
| EP2199973A3 (en) | 1997-06-09 | 2010-09-08 | Seiko Epson Corporation | An image processing apparatus and method, and an image evaluation device and method |
| DE29710484U1 (en) | 1997-06-16 | 1998-10-15 | Howmedica GmbH, 24232 Schönkirchen | Receiving part for a holding component of a spinal implant |
| US5961329A (en) | 1997-07-02 | 1999-10-05 | Stucki-Mccormick; Suzanne U. | Combination distraction dental implant and method of use |
| US5891145A (en) | 1997-07-14 | 1999-04-06 | Sdgi Holdings, Inc. | Multi-axial screw |
| FR2767263B1 (en) | 1997-08-13 | 1999-10-01 | Aesculap Jbs | CLAMPS FOR VERTEBRAL OSTEOSYNTHESIS SYSTEM |
| US6217331B1 (en) | 1997-10-03 | 2001-04-17 | Implant Innovations, Inc. | Single-stage implant system |
| US6017177A (en) | 1997-10-06 | 2000-01-25 | Mcgard, Inc. | Multi-tier security fastener |
| FR2771918B1 (en) | 1997-12-09 | 2000-04-21 | Dimso Sa | CONNECTOR FOR SPINAL OSTEOSYNTHESIS DEVICE |
| US6010503A (en) | 1998-04-03 | 2000-01-04 | Spinal Innovations, Llc | Locking mechanism |
| DE29806563U1 (en) | 1998-04-09 | 1998-06-18 | Howmedica GmbH, 24232 Schönkirchen | Pedicle screw and assembly aid for it |
| DE19822802C2 (en) | 1998-05-20 | 2001-11-08 | Medicon Eg Chirurgiemechaniker | Device for distraction of bone segments, especially in the jaw area |
| US6565565B1 (en) | 1998-06-17 | 2003-05-20 | Howmedica Osteonics Corp. | Device for securing spinal rods |
| DE29810798U1 (en) | 1998-06-17 | 1999-10-28 | SCHÄFER micomed GmbH, 73035 Göppingen | Osteosynthesis device |
| EP1109502B1 (en) | 1998-09-11 | 2006-03-15 | Synthes AG Chur | Variable angle spinal fixation system |
| ES2221195T3 (en) | 1998-09-29 | 2004-12-16 | Synthes Ag Chur | DEVICE FOR JOINING A LONGITUDINAL SUPPORT WITH A MEDIUM FOR BONE FIXATION. |
| US6126662A (en) | 1998-10-09 | 2000-10-03 | Carmichael; Robert P. | Bone implant |
| CA2249948C (en) | 1998-10-09 | 2006-04-04 | Donald R. Johnson | Bone implant |
| US6296642B1 (en) | 1998-11-09 | 2001-10-02 | Sdgi Holdings, Inc. | Reverse angle thread for preventing splaying in medical devices |
| US6482208B1 (en) | 1998-11-25 | 2002-11-19 | Alliance Orthopedic, Inc. | Fracture reduction clamp |
| ES2245047T3 (en) | 1998-11-26 | 2005-12-16 | Synthes Ag Chur | BONE SCREW. |
| FR2789886B1 (en) | 1999-02-18 | 2001-07-06 | Dimso Sa | DISTRACTION / CONTRACTION DEVICE FOR A SPINAL OSTEOSYNTHESIS SYSTEM |
| DE29903342U1 (en) | 1999-02-24 | 1999-06-02 | Grzibek, Egbert, 97534 Waigolshausen | Fixing element for holding elements of spinal implants |
| DE19912364B4 (en) | 1999-03-19 | 2004-10-07 | Peter Brehm | pedicle screw |
| FR2796545B1 (en) | 1999-07-22 | 2002-03-15 | Dimso Sa | POLY-AXIAL LINK FOR OSTEOSYNTHESIS SYSTEM, ESPECIALLY FOR THE RACHIS |
| DE19936286C2 (en) | 1999-08-02 | 2002-01-17 | Lutz Biedermann | bone screw |
| ES2153331B1 (en) | 1999-08-05 | 2001-09-01 | Traiber S A | INTERVERTEBRAL FIXING SYSTEM FOR COLUMN TREATMENTS. |
| US6280442B1 (en) | 1999-09-01 | 2001-08-28 | Sdgi Holdings, Inc. | Multi-axial bone screw assembly |
| US6378289B1 (en) | 1999-11-19 | 2002-04-30 | Pioneer Surgical Technology | Methods and apparatus for clamping surgical wires or cables |
| ATE275877T1 (en) | 1999-11-25 | 2004-10-15 | Ct Pulse Orthopedics Ltd | SURGICAL INSTRUMENT FOR TENSIONING A CABLE-LIKE TENSIONING ELEMENT |
| CN1191791C (en) | 2000-01-13 | 2005-03-09 | 库尔斯恩蒂斯股份公司 | Device for detachably clamping a longitudinal carrier in a surgical implant |
| US6508820B2 (en) | 2000-02-03 | 2003-01-21 | Joel Patrick Bales | Intramedullary interlock screw |
| DE10005385A1 (en) | 2000-02-07 | 2001-08-09 | Ulrich Gmbh & Co Kg | Pedicle screw |
| US6443953B1 (en) | 2000-02-08 | 2002-09-03 | Cross Medical Products, Inc. | Self-aligning cap nut for use with a spinal rod anchor |
| US6224598B1 (en) | 2000-02-16 | 2001-05-01 | Roger P. Jackson | Bone screw threaded plug closure with central set screw |
| US6514255B1 (en) | 2000-02-25 | 2003-02-04 | Bret Ferree | Sublaminar spinal fixation apparatus |
| US20050209592A1 (en) | 2000-05-11 | 2005-09-22 | Fridolin Schlapfer | Plug-type connection for releasably connecting two bodies |
| US6440132B1 (en) | 2000-05-24 | 2002-08-27 | Roger P. Jackson | Open head bone screw closure with threaded boss |
| ATE476929T1 (en) | 2000-06-30 | 2010-08-15 | Warsaw Orthopedic Inc | INTERVERBEL CONNECTION DEVICE |
| US6482207B1 (en) | 2000-07-13 | 2002-11-19 | Fastenetix, Llc | Efficient assembling modular locking pedicle screw |
| EP1174092A3 (en) | 2000-07-22 | 2003-03-26 | Corin Spinal Systems Limited | A pedicle attachment assembly |
| US7833250B2 (en) | 2004-11-10 | 2010-11-16 | Jackson Roger P | Polyaxial bone screw with helically wound capture connection |
| US6554831B1 (en) | 2000-09-01 | 2003-04-29 | Hopital Sainte-Justine | Mobile dynamic system for treating spinal disorder |
| US6533226B2 (en) | 2000-09-14 | 2003-03-18 | Hellermanntyton Corporation | Saddle mount |
| US6485491B1 (en) | 2000-09-15 | 2002-11-26 | Sdgi Holdings, Inc. | Posterior fixation system |
| US6755829B1 (en) | 2000-09-22 | 2004-06-29 | Depuy Acromed, Inc. | Lock cap anchor assembly for orthopaedic fixation |
| EP1192908A3 (en) | 2000-10-02 | 2004-05-26 | Howmedica Osteonics Corp. | System and method for spinal reconstruction |
| DE20018390U1 (en) | 2000-10-27 | 2001-01-18 | Wenzler Medizintechnik GmbH, 78665 Frittlingen | Cutting pliers |
| DE10055888C1 (en) | 2000-11-10 | 2002-04-25 | Biedermann Motech Gmbh | Bone screw, has connector rod receiving part with unsymmetrically arranged end bores |
| US6524311B2 (en) | 2000-12-01 | 2003-02-25 | Robert W. Gaines, Jr. | Method and apparatus for performing spinal procedures |
| US6368321B1 (en) | 2000-12-04 | 2002-04-09 | Roger P. Jackson | Lockable swivel head bone screw |
| US6454768B1 (en) | 2000-12-05 | 2002-09-24 | Roger P. Jackson | Removable gripping set screw |
| US6726687B2 (en) | 2000-12-08 | 2004-04-27 | Jackson Roger P | Closure plug for open-headed medical implant |
| US6454772B1 (en) | 2000-12-08 | 2002-09-24 | Roger P. Jackson | Set screw for medical implant with gripping side slots |
| DE50100793D1 (en) | 2000-12-27 | 2003-11-20 | Biedermann Motech Gmbh | Screw for connecting to a rod |
| WO2002054966A2 (en) | 2001-01-12 | 2002-07-18 | Depuy Acromed, Inc. | Polyaxial screw with improved locking |
| US6558387B2 (en) | 2001-01-30 | 2003-05-06 | Fastemetix, Llc | Porous interbody fusion device having integrated polyaxial locking interference screws |
| US6451021B1 (en) | 2001-02-15 | 2002-09-17 | Third Millennium Engineering, Llc | Polyaxial pedicle screw having a rotating locking element |
| AU2002245473A1 (en) | 2001-02-26 | 2002-09-12 | Federal-Mogul Powertrain, Inc | Rigidized protective sleeving |
| FR2822053B1 (en) * | 2001-03-15 | 2003-06-20 | Stryker Spine Sa | ANCHORING MEMBER WITH SAFETY RING FOR SPINAL OSTEOSYNTHESIS SYSTEM |
| US6802844B2 (en) | 2001-03-26 | 2004-10-12 | Nuvasive, Inc | Spinal alignment apparatus and methods |
| DE10115014A1 (en) | 2001-03-27 | 2002-10-24 | Biedermann Motech Gmbh | anchoring element |
| US6641588B2 (en) | 2001-05-08 | 2003-11-04 | Medtronic, Inc. | Surgical tool for tensioning a cranial-flap clamp |
| US6770075B2 (en) | 2001-05-17 | 2004-08-03 | Robert S. Howland | Spinal fixation apparatus with enhanced axial support and methods for use |
| EP1269929A1 (en) | 2001-06-20 | 2003-01-02 | Copf jun., Franz | Connection system for the spinal fusion of the lumbar column |
| FR2827499B1 (en) | 2001-07-20 | 2004-05-07 | Henry Graf | INTERVERTEBRAL LINK DEVICE |
| US6520963B1 (en) | 2001-08-13 | 2003-02-18 | Mckinley Lawrence M. | Vertebral alignment and fixation assembly |
| US6932597B2 (en) | 2001-09-12 | 2005-08-23 | Norbert Abels | Self-ligating orthodontic brackets including a metal ligation cover hingedly connected to a bracket base |
| US6974460B2 (en) | 2001-09-14 | 2005-12-13 | Stryker Spine | Biased angulation bone fixation assembly |
| FR2830433B1 (en) | 2001-10-04 | 2005-07-01 | Stryker Spine | ASSEMBLY FOR OSTEOSYNTHESIS OF THE SPINACH COMPRISING AN ANCHORING MEMBER HEAD AND A TOOL FOR HEAD FIXING |
| US6800079B2 (en) | 2002-03-15 | 2004-10-05 | Lock-N-Stitch, Inc. | Orthopedic stabilization device and method |
| US6783527B2 (en) | 2001-10-30 | 2004-08-31 | Sdgi Holdings, Inc. | Flexible spinal stabilization system and method |
| US7766947B2 (en) | 2001-10-31 | 2010-08-03 | Ortho Development Corporation | Cervical plate for stabilizing the human spine |
| US6695852B2 (en) | 2001-10-31 | 2004-02-24 | Spineology, Inc. | Tension tools for tension band clip |
| US20060079892A1 (en) | 2001-10-31 | 2006-04-13 | Suranjan Roychowdhury | Adjustable tandem connectors for corrective devices for the spinal column and other bones and joints |
| DE10157814B4 (en) | 2001-11-27 | 2004-12-02 | Biedermann Motech Gmbh | Closure device for securing a rod-shaped element in a holding element connected to a shaft |
| FR2832620B1 (en) | 2001-11-27 | 2004-01-23 | Eurosurgical | CONNECTOR FOR VERTEBRAL ANCHORAGE SYSTEM |
| DE10157969C1 (en) | 2001-11-27 | 2003-02-06 | Biedermann Motech Gmbh | Element used in spinal and accident surgery comprises a shaft joined to a holding element having a U-shaped recess with two free arms having an internal thread with flanks lying at right angles to the central axis of the holding element |
| US6887275B2 (en) | 2001-12-15 | 2005-05-03 | Ace Surgical Supply Co., Inc. | Maxillofacial anchoring system for alveolar and small bone skeletal distraction |
| DE10164323C1 (en) | 2001-12-28 | 2003-06-18 | Biedermann Motech Gmbh | Bone screw has holder element joined to shaft and possessing two free arms , with inner screw, slot, external nut, cavity and shoulder cooperating with attachment |
| US6641586B2 (en) | 2002-02-01 | 2003-11-04 | Depuy Acromed, Inc. | Closure system for spinal fixation instrumentation |
| US7066937B2 (en) | 2002-02-13 | 2006-06-27 | Endius Incorporated | Apparatus for connecting a longitudinal member to a bone portion |
| US7163538B2 (en) * | 2002-02-13 | 2007-01-16 | Cross Medical Products, Inc. | Posterior rod system |
| US20040006342A1 (en) * | 2002-02-13 | 2004-01-08 | Moti Altarac | Posterior polyaxial plate system for the spine |
| US7008227B2 (en) | 2002-03-04 | 2006-03-07 | Carmichael Robert P | Self-drilling implant |
| DE10213855A1 (en) | 2002-03-27 | 2003-10-16 | Biedermann Motech Gmbh | Bone anchoring device for stabilizing bone segments and receiving part of a bone anchoring device |
| US7842073B2 (en) | 2002-04-18 | 2010-11-30 | Aesculap Ii, Inc. | Screw and rod fixation assembly and device |
| US6740086B2 (en) | 2002-04-18 | 2004-05-25 | Spinal Innovations, Llc | Screw and rod fixation assembly and device |
| AUPS226402A0 (en) | 2002-05-13 | 2002-06-13 | Advanced Metal Coatings Pty Limited | An ablation catheter |
| DE20207785U1 (en) | 2002-05-17 | 2003-09-25 | GEOMED Medizin-Technik GmbH & Co., 78532 Tuttlingen | Surgical cutter, has cavities in opposing cutting edges forming locating cavity for object being cut |
| DE20207851U1 (en) | 2002-05-21 | 2002-10-10 | Metz-Stavenhagen, Peter, Dr.med., 34537 Bad Wildungen | Anchoring element for fastening a rod of a device for setting up a human or animal spine to a vertebral bone |
| AU2003233587B2 (en) | 2002-05-21 | 2008-12-18 | Warsaw Orthopedic, Inc. | Vertebrae bone anchor and cable for coupling it to a rod |
| DE50300788D1 (en) | 2002-05-21 | 2005-08-25 | Spinelab Gmbh Wabern | Elastic stabilization system for spinal columns |
| US7306603B2 (en) | 2002-08-21 | 2007-12-11 | Innovative Spinal Technologies | Device and method for percutaneous placement of lumbar pedicle screws and connecting rods |
| DE10246177A1 (en) | 2002-10-02 | 2004-04-22 | Biedermann Motech Gmbh | Anchor element consists of screw with head, bone-thread section on shank and holder joining rod-shaped part to screw. with cavities in wall, and thread-free end of shank |
| US7131467B2 (en) | 2002-10-24 | 2006-11-07 | Pilling Weck Incorporated | Instrument for applying a tie to two items and method of making same |
| EP2366349B1 (en) | 2002-10-30 | 2017-04-05 | Zimmer Spine, Inc. | Spinal stabilization system insertion |
| US8162989B2 (en) | 2002-11-04 | 2012-04-24 | Altus Partners, Llc | Orthopedic rod system |
| SE522397C2 (en) | 2002-11-05 | 2004-02-03 | Volvo Lastvagnar Ab | Cable duct for a vehicle and method for mounting a cabling on a vehicle |
| US20040199169A1 (en) | 2002-11-20 | 2004-10-07 | Koons Kirk C. | Cable clamp tool for surgical applications |
| DE10256095B4 (en) | 2002-12-02 | 2004-11-18 | Biedermann Motech Gmbh | Element with a shaft and an associated holding element for connecting to a rod |
| AU2002368445B2 (en) * | 2002-12-06 | 2006-10-05 | Synthes Gmbh | Device for stabilising bones |
| US20040111088A1 (en) | 2002-12-06 | 2004-06-10 | Picetti George D. | Multi-rod bone attachment member |
| US6843791B2 (en) | 2003-01-10 | 2005-01-18 | Depuy Acromed, Inc. | Locking cap assembly for spinal fixation instrumentation |
| US7094240B2 (en) * | 2003-01-10 | 2006-08-22 | Sdgi Holdings, Inc. | Flexible member tensioning instruments and methods |
| US20040162558A1 (en) | 2003-02-18 | 2004-08-19 | Hegde Sajan K. | Spinal plate having an integral rod connector portion |
| DE10310540B3 (en) | 2003-03-11 | 2004-08-19 | Biedermann Motech Gmbh | Anchoring element for bone or spinal column surgery has threaded shaft and cylindrical reception part for coupling with rod having U-shaped seating with screw threads at ends of its arms |
| US20040186473A1 (en) | 2003-03-21 | 2004-09-23 | Cournoyer John R. | Spinal fixation devices of improved strength and rigidity |
| WO2004089245A2 (en) | 2003-04-04 | 2004-10-21 | Theken Surgical, Llc | Bone anchor |
| US6964666B2 (en) | 2003-04-09 | 2005-11-15 | Jackson Roger P | Polyaxial bone screw locking mechanism |
| US20070016200A1 (en) | 2003-04-09 | 2007-01-18 | Jackson Roger P | Dynamic stabilization medical implant assemblies and methods |
| US6716214B1 (en) | 2003-06-18 | 2004-04-06 | Roger P. Jackson | Polyaxial bone screw with spline capture connection |
| DE50302889D1 (en) | 2003-04-24 | 2006-05-18 | Zimmer Gmbh Winterthur | Instrument system for pedicle screws |
| US7615068B2 (en) | 2003-05-02 | 2009-11-10 | Applied Spine Technologies, Inc. | Mounting mechanisms for pedicle screws and related assemblies |
| US7354442B2 (en) | 2003-05-05 | 2008-04-08 | Warsaw Orthopedic, Inc. | Bone anchor and methods of using the same |
| US7377923B2 (en) | 2003-05-22 | 2008-05-27 | Alphatec Spine, Inc. | Variable angle spinal screw assembly |
| US7270665B2 (en) * | 2003-06-11 | 2007-09-18 | Sdgi Holdings, Inc. | Variable offset spinal fixation system |
| US7322981B2 (en) | 2003-08-28 | 2008-01-29 | Jackson Roger P | Polyaxial bone screw with split retainer ring |
| US8137386B2 (en) | 2003-08-28 | 2012-03-20 | Jackson Roger P | Polyaxial bone screw apparatus |
| US7087057B2 (en) | 2003-06-27 | 2006-08-08 | Depuy Acromed, Inc. | Polyaxial bone screw |
| US7291151B2 (en) | 2003-07-25 | 2007-11-06 | Traiber, S.A. | Vertebral fixation device for the treatment of spondylolisthesis |
| US6981973B2 (en) | 2003-08-11 | 2006-01-03 | Mckinley Laurence M | Low profile vertebral alignment and fixation assembly |
| EP1673024B1 (en) | 2003-08-20 | 2014-04-09 | Warsaw Orthopedic, Inc. | Multi-axial orthopedic device and system, e.g. for spinal surgery |
| JP4146316B2 (en) | 2003-09-02 | 2008-09-10 | 矢崎総業株式会社 | Protector |
| US20050080415A1 (en) | 2003-10-14 | 2005-04-14 | Keyer Thomas R. | Polyaxial bone anchor and method of spinal fixation |
| US7276005B2 (en) * | 2003-10-14 | 2007-10-02 | Nissan Motor Co., Ltd. | Wheel drive system for independently driving right and left wheels of vehicle |
| DE10349046A1 (en) | 2003-10-17 | 2005-06-02 | Newfrey Llc, Newark | Holder for elongated objects, in particular cables |
| US7645282B2 (en) | 2003-11-20 | 2010-01-12 | Osseus, Llc | Method and device for cutting surgical wire or cable |
| US7527638B2 (en) | 2003-12-16 | 2009-05-05 | Depuy Spine, Inc. | Methods and devices for minimally invasive spinal fixation element placement |
| AU2004311447A1 (en) | 2003-12-30 | 2005-07-21 | Depuy Spine Sarl | Bone anchor assemblies |
| US20050143737A1 (en) * | 2003-12-31 | 2005-06-30 | John Pafford | Dynamic spinal stabilization system |
| US7678137B2 (en) | 2004-01-13 | 2010-03-16 | Life Spine, Inc. | Pedicle screw constructs for spine fixation systems |
| US20050177179A1 (en) | 2004-02-10 | 2005-08-11 | Baynham Bret O. | Surgical cable system |
| US7993373B2 (en) | 2005-02-22 | 2011-08-09 | Hoy Robert W | Polyaxial orthopedic fastening apparatus |
| US8562649B2 (en) * | 2004-02-17 | 2013-10-22 | Gmedelaware 2 Llc | System and method for multiple level facet joint arthroplasty and fusion |
| US7163539B2 (en) | 2004-02-27 | 2007-01-16 | Custom Spine, Inc. | Biased angle polyaxial pedicle screw assembly |
| US7862594B2 (en) | 2004-02-27 | 2011-01-04 | Custom Spine, Inc. | Polyaxial pedicle screw assembly |
| US7819902B2 (en) * | 2004-02-27 | 2010-10-26 | Custom Spine, Inc. | Medialised rod pedicle screw assembly |
| DE102004010382B4 (en) | 2004-03-03 | 2006-04-20 | Biedermann Motech Gmbh | Bone anchoring element for anchoring in a bone or in a vertebra and its use in a stabilizing device |
| DE102004010380A1 (en) | 2004-03-03 | 2005-09-22 | Biedermann Motech Gmbh | Anchoring element and stabilizing device for the dynamic stabilization of vertebrae or bones with such an anchoring element |
| US7491221B2 (en) * | 2004-03-23 | 2009-02-17 | Stryker Spine | Modular polyaxial bone screw and plate |
| US7717939B2 (en) * | 2004-03-31 | 2010-05-18 | Depuy Spine, Inc. | Rod attachment for head to head cross connector |
| US8236028B2 (en) | 2004-03-31 | 2012-08-07 | Depuy Spine Sarl | Spinal rod connector |
| US7503924B2 (en) | 2004-04-08 | 2009-03-17 | Globus Medical, Inc. | Polyaxial screw |
| US8475495B2 (en) | 2004-04-08 | 2013-07-02 | Globus Medical | Polyaxial screw |
| JP4845344B2 (en) * | 2004-04-14 | 2011-12-28 | ユニ・チャーム株式会社 | Disposable diapers |
| US7648520B2 (en) | 2004-04-16 | 2010-01-19 | Kyphon Sarl | Pedicle screw assembly |
| WO2005102195A1 (en) | 2004-04-20 | 2005-11-03 | Allez Spine, Llc | Pedicle screw assembly |
| GB2414674B (en) | 2004-06-04 | 2009-08-12 | John Burke | Apparatus for the correction of skeletal deformities |
| US7935135B2 (en) | 2004-06-09 | 2011-05-03 | Zimmer Spine, Inc. | Spinal fixation device |
| US7857834B2 (en) | 2004-06-14 | 2010-12-28 | Zimmer Spine, Inc. | Spinal implant fixation assembly |
| US7744634B2 (en) | 2004-06-15 | 2010-06-29 | Warsaw Orthopedic, Inc. | Spinal rod system |
| US7264621B2 (en) | 2004-06-17 | 2007-09-04 | Sdgi Holdings, Inc. | Multi-axial bone attachment assembly |
| WO2006005198A1 (en) | 2004-07-12 | 2006-01-19 | Synthes Gmbh | Device for the dynamic fixation of bones |
| US7572281B2 (en) | 2004-08-06 | 2009-08-11 | Depuy Spine, Inc. | Instrument for guiding a rod into an implant in a spinal fixation system |
| US7186255B2 (en) | 2004-08-12 | 2007-03-06 | Atlas Spine, Inc. | Polyaxial screw |
| US20060149265A1 (en) | 2004-09-07 | 2006-07-06 | Anthony James | Minimal thickness bone plate locking mechanism |
| US20060052818A1 (en) | 2004-09-08 | 2006-03-09 | Drake Daniel H | Surgical clamp and cutting blade |
| US8469966B2 (en) | 2004-09-23 | 2013-06-25 | Smith & Nephew, Inc. | Systems, methods, and apparatuses for tensioning an orthopedic surgical cable |
| US7896906B2 (en) * | 2004-12-30 | 2011-03-01 | Depuy Spine, Inc. | Artificial facet joint |
| US8267969B2 (en) | 2004-10-20 | 2012-09-18 | Exactech, Inc. | Screw systems and methods for use in stabilization of bone structures |
| US20080154277A1 (en) | 2004-10-26 | 2008-06-26 | Scott Machalk | Tool apparatus for locking a spinal rod in an anchoring device therefor |
| US8926672B2 (en) | 2004-11-10 | 2015-01-06 | Roger P. Jackson | Splay control closure for open bone anchor |
| US20060111779A1 (en) | 2004-11-22 | 2006-05-25 | Orthopedic Development Corporation, A Florida Corporation | Minimally invasive facet joint fusion |
| US8444681B2 (en) | 2009-06-15 | 2013-05-21 | Roger P. Jackson | Polyaxial bone anchor with pop-on shank, friction fit retainer and winged insert |
| US8308782B2 (en) | 2004-11-23 | 2012-11-13 | Jackson Roger P | Bone anchors with longitudinal connecting member engaging inserts and closures for fixation and optional angulation |
| US9216041B2 (en) | 2009-06-15 | 2015-12-22 | Roger P. Jackson | Spinal connecting members with tensioned cords and rigid sleeves for engaging compression inserts |
| US9168069B2 (en) | 2009-06-15 | 2015-10-27 | Roger P. Jackson | Polyaxial bone anchor with pop-on shank and winged insert with lower skirt for engaging a friction fit retainer |
| JP4573163B2 (en) | 2004-11-29 | 2010-11-04 | 株式会社ニコン | Autofocus device and autofocus adjustment method |
| US7306606B2 (en) | 2004-12-15 | 2007-12-11 | Orthopaedic Innovations, Inc. | Multi-axial bone screw mechanism |
| US7744636B2 (en) | 2004-12-16 | 2010-06-29 | Aesculap Ii, Inc. | Locking mechanism |
| CA2601916C (en) | 2005-01-18 | 2012-10-02 | Synthes (U.S.A.) | Angularly stable device for mutually fixing a longitudinal carrier with a bone fixation element |
| US7445627B2 (en) | 2005-01-31 | 2008-11-04 | Alpinespine, Llc | Polyaxial pedicle screw assembly |
| WO2006088452A2 (en) | 2005-02-11 | 2006-08-24 | Innovative Spinal Design | Surgical cable system |
| US7476239B2 (en) | 2005-05-10 | 2009-01-13 | Jackson Roger P | Polyaxial bone screw with compound articulation |
| US7951172B2 (en) | 2005-03-04 | 2011-05-31 | Depuy Spine Sarl | Constrained motion bone screw assembly |
| US20060217717A1 (en) | 2005-03-24 | 2006-09-28 | Dale Whipple | Methods and devices for stabilizing a bone anchor |
| US20060229611A1 (en) | 2005-03-30 | 2006-10-12 | Sdgi Holdings, Inc. | Spinal rod connector |
| US20060235385A1 (en) | 2005-03-31 | 2006-10-19 | Dale Whipple | Low profile polyaxial screw |
| US7708762B2 (en) | 2005-04-08 | 2010-05-04 | Warsaw Orthopedic, Inc. | Systems, devices and methods for stabilization of the spinal column |
| JP2006288864A (en) | 2005-04-13 | 2006-10-26 | Padoru:Kk | Bone fixture for surgical operation |
| BRPI0610255A2 (en) | 2005-04-25 | 2010-11-23 | Synthes Gmbh | bone anchor for attaching a fixture to a bone and vertebra, combination of bone anchor and fixture to retain adjacent vertebrae, and method of mounting a bone anchor |
| DE102005019362A1 (en) | 2005-04-26 | 2006-11-02 | Deere & Company, Moline | Electric interface device for transmitting electric power between vehicle and implement has measuring apparatus that is allocated to vehicle interface or actuator which is assigned to vehicle interface |
| EP1876975A2 (en) | 2005-04-27 | 2008-01-16 | James Marino | Mono-planar pedilcle screw method, system, and kit |
| US20060247668A1 (en) | 2005-04-28 | 2006-11-02 | Park Kee B | Surgical tool |
| JP3721189B1 (en) | 2005-05-02 | 2005-11-30 | アルフレッサファーマ株式会社 | Tightening device for bone fastening cable |
| DE102005021879B4 (en) | 2005-05-04 | 2007-04-12 | Aesculap Ag & Co. Kg | Orthopedic anchoring element and osteosynthesis device |
| WO2006135555A2 (en) | 2005-06-08 | 2006-12-21 | Accelerated Innovation, Llc | Vertebral facet stabilizer |
| US7547319B2 (en) | 2005-06-15 | 2009-06-16 | Ouroboros Medical | Mechanical apparatus and method for artificial disc replacement |
| JP4950519B2 (en) | 2005-06-30 | 2012-06-13 | キヤノン株式会社 | Optical wavelength conversion device, optical wavelength conversion method, and image forming apparatus using the same |
| EP1741396B1 (en) | 2005-07-08 | 2009-09-23 | BIEDERMANN MOTECH GmbH | Bone anchoring device |
| CN101252888A (en) | 2005-07-18 | 2008-08-27 | D·M·全 | Bi-polar bone screw assembly |
| WO2007012025A2 (en) * | 2005-07-19 | 2007-01-25 | Stephen Ritland | Rod extension for extending fusion construct |
| US7628799B2 (en) | 2005-08-23 | 2009-12-08 | Aesculap Ag & Co. Kg | Rod to rod connector |
| JP4417307B2 (en) | 2005-08-26 | 2010-02-17 | 理研ビタミン株式会社 | Dessert mix |
| FR2890850B1 (en) | 2005-09-20 | 2009-04-17 | Abbott Spine Sa | VERTEBRAL FASTENING SYSTEM |
| FR2890851B1 (en) | 2005-09-21 | 2008-06-20 | Abbott Spine Sa | ANCILLARY TO TENSION A FLEXIBLE LINK. |
| WO2007038351A2 (en) | 2005-09-23 | 2007-04-05 | Synthes (Usa) | Installation tools and system for bone support apparatus |
| WO2007041265A1 (en) | 2005-09-30 | 2007-04-12 | Paradigm Spine, Llc | Hinged polyaxial screw and methods of use |
| ES2436101T3 (en) * | 2005-10-07 | 2013-12-27 | Alphatec Spine, Inc. | Adjustable occipital plate |
| USD527678S1 (en) | 2005-10-13 | 2006-09-05 | Exhart Environmental Systems, Inc. | Fanciful fish novelty |
| US8075599B2 (en) | 2005-10-18 | 2011-12-13 | Warsaw Orthopedic, Inc. | Adjustable bone anchor assembly |
| US8002806B2 (en) | 2005-10-20 | 2011-08-23 | Warsaw Orthopedic, Inc. | Bottom loading multi-axial screw assembly |
| US7722651B2 (en) | 2005-10-21 | 2010-05-25 | Depuy Spine, Inc. | Adjustable bone screw assembly |
| GB0521582D0 (en) * | 2005-10-22 | 2005-11-30 | Depuy Int Ltd | An implant for supporting a spinal column |
| US7803174B2 (en) | 2005-11-04 | 2010-09-28 | Warsaw Orthopedic, Inc. | Dorsal adjusting multi-rod connector |
| US8100946B2 (en) | 2005-11-21 | 2012-01-24 | Synthes Usa, Llc | Polyaxial bone anchors with increased angulation |
| WO2007067443A2 (en) | 2005-12-08 | 2007-06-14 | Alphaspine, Inc. | Percutaneous screw assembly |
| US8029546B2 (en) | 2005-12-15 | 2011-10-04 | Warsaw Orthopedic, Inc. | Variable angle offset spinal connector assembly |
| DE102005061074A1 (en) | 2005-12-21 | 2007-06-28 | Mahle International Gmbh | Piston for combustion engine e.g. diesel engine, has radially outward oriented wall zone of cooling channel formed by ring carrier |
| GB0600662D0 (en) | 2006-01-13 | 2006-02-22 | Depuy Int Ltd | Spinal support rod kit |
| US20070191844A1 (en) | 2006-01-31 | 2007-08-16 | Sdgi Holdings, Inc. | In-series, dual locking mechanism device |
| EP1815812B1 (en) | 2006-02-03 | 2009-07-29 | Spinelab AG | Spinal implant |
| US8029545B2 (en) * | 2006-02-07 | 2011-10-04 | Warsaw Orthopedic Inc. | Articulating connecting member and anchor systems for spinal stabilization |
| US20070233091A1 (en) | 2006-02-23 | 2007-10-04 | Naifeh Bill R | Multi-level spherical linkage implant system |
| US7828829B2 (en) | 2006-03-22 | 2010-11-09 | Pioneer Surgical Technology Inc. | Low top bone fixation system and method for using the same |
| US7867255B2 (en) | 2006-04-07 | 2011-01-11 | Warsaw Orthopedic, Inc. | Spinal rod connector system and method for a bone anchor |
| DE202006006347U1 (en) | 2006-04-19 | 2006-06-14 | Veritas Ag | Holding device for at least one line |
| US7862573B2 (en) | 2006-04-21 | 2011-01-04 | Darois Roger E | Method and apparatus for surgical fastening |
| US20070270817A1 (en) | 2006-04-24 | 2007-11-22 | Sdgi Holdings, Inc. | Connector apparatus |
| US8435267B2 (en) | 2006-04-24 | 2013-05-07 | Spinefrontier Inc | Spine fixation method and apparatus |
| US20070270820A1 (en) * | 2006-04-26 | 2007-11-22 | Sdgi Holdings, Inc. | Revision fixation plate and method of use |
| US8979903B2 (en) | 2006-04-26 | 2015-03-17 | Warsaw Orthopedic, Inc. | Revision fixation plate and method of use |
| US20070270880A1 (en) | 2006-04-28 | 2007-11-22 | Lindemann Gary S | Bone screw revision tools and methods of use |
| US7909854B2 (en) | 2006-04-29 | 2011-03-22 | Warsaw Orthopedic, Inc. | Variable connector |
| US7806895B2 (en) | 2006-05-08 | 2010-10-05 | Device Evolutions Llc | Thoracic closure device and methods |
| WO2007141347A1 (en) | 2006-06-05 | 2007-12-13 | Traiber, S.L. | Device for vertebral attachment and tool for fitting of the said device |
| WO2007146032A2 (en) | 2006-06-07 | 2007-12-21 | Disc Motion Technologies, Inc. | Pedicle screw system |
| JP2009543597A (en) | 2006-07-13 | 2009-12-10 | マス モジュラー スパイン システム | Modular spinal fixation system |
| US20080021456A1 (en) | 2006-07-21 | 2008-01-24 | Depuy Spine, Inc. | Sacral or iliac cross connector |
| US20080021455A1 (en) | 2006-07-21 | 2008-01-24 | Depuy Spine, Inc. | Articulating Sacral or Iliac Connector |
| US20080039843A1 (en) | 2006-08-11 | 2008-02-14 | Abdou M S | Spinal motion preservation devices and methods of use |
| US20080058805A1 (en) | 2006-08-28 | 2008-03-06 | Microdexterity Systems, Inc. | Spinal fusion implant |
| US8317830B2 (en) * | 2006-08-29 | 2012-11-27 | Warsaw Orthopedic, Inc. | Orthopaedic screw system with linear motion |
| US7922746B2 (en) * | 2006-08-31 | 2011-04-12 | Warsaw Orthopedic, Inc. | Spinal rod extenders and methods of use |
| KR20090043569A (en) | 2006-08-31 | 2009-05-06 | 워쏘우 오르쏘페딕 인코포레이티드 | Spinal rod extenders and methods of use |
| EP2073732B1 (en) | 2006-09-26 | 2010-11-03 | Synthes GmbH | Transconnector |
| US8016862B2 (en) | 2006-09-27 | 2011-09-13 | Innovasis, Inc. | Spinal stabilizing system |
| US8167910B2 (en) | 2006-10-16 | 2012-05-01 | Innovative Delta Technology Llc | Bone screw and associated assembly and methods of use thereof |
| US7976567B2 (en) | 2006-10-18 | 2011-07-12 | Warsaw Orthopedic, Inc. | Orthopedic revision connector |
| WO2008070840A1 (en) | 2006-12-07 | 2008-06-12 | Alpinespine Llc | Press-on pedicle screw assembly |
| KR100829338B1 (en) * | 2006-12-07 | 2008-05-13 | 김수경 | Spinal stabilization apparatus |
| US20080154308A1 (en) | 2006-12-21 | 2008-06-26 | Warsaw Orthopedic, Inc. | Spinal fixation system |
| US8029544B2 (en) * | 2007-01-02 | 2011-10-04 | Zimmer Spine, Inc. | Spine stiffening device |
| AU2008206396A1 (en) | 2007-01-12 | 2008-07-24 | Lanx, Inc. | Bone fastener assembly |
| US20080188260A1 (en) | 2007-02-02 | 2008-08-07 | Motorola, Inc. | Method and apparatus for uplink power control in a communication system |
| US8097022B2 (en) | 2007-02-20 | 2012-01-17 | Warsaw Orthopedic, Inc. | Flexible coupling members for spinal stabilization members |
| EP2301456B1 (en) | 2007-02-23 | 2013-04-17 | Biedermann Technologies GmbH & Co. KG | Rod connector for stabilizing vertebrae |
| US7967849B2 (en) | 2007-04-06 | 2011-06-28 | Warsaw Orthopedic, Inc. | Adjustable multi-axial spinal coupling assemblies |
| US10603077B2 (en) | 2007-04-12 | 2020-03-31 | Globus Medical, Inc. | Orthopedic fastener for stabilization and fixation |
| US8337527B2 (en) | 2007-04-18 | 2012-12-25 | Ebi, Llc | Spinal connector |
| US7922725B2 (en) | 2007-04-19 | 2011-04-12 | Zimmer Spine, Inc. | Method and associated instrumentation for installation of spinal dynamic stabilization system |
| US8979904B2 (en) | 2007-05-01 | 2015-03-17 | Roger P Jackson | Connecting member with tensioned cord, low profile rigid sleeve and spacer with torsion control |
| US8016832B2 (en) | 2007-05-02 | 2011-09-13 | Zimmer Spine, Inc. | Installation systems for spinal stabilization system and related methods |
| US8197517B1 (en) | 2007-05-08 | 2012-06-12 | Theken Spine, Llc | Frictional polyaxial screw assembly |
| US8353937B2 (en) | 2007-05-22 | 2013-01-15 | Warsaw Orthopedic, Inc. | Spinal stabilization systems and methods |
| DK200700157U3 (en) | 2007-05-27 | 2008-09-12 | Hede Simon Christian | Plastic cable ties (cable ties) fitted with longitudinally extending metal wire / wires. This is to make radiological detection of possible. broken strips possible after implantation in animals or humans. Furthermore, to increase the mechanical strength of the strips. |
| US8080039B2 (en) | 2007-06-05 | 2011-12-20 | Spartek Medical, Inc. | Anchor system for a spine implantation system that can move about three axes |
| US8313515B2 (en) * | 2007-06-15 | 2012-11-20 | Rachiotek, Llc | Multi-level spinal stabilization system |
| KR100896043B1 (en) | 2007-06-22 | 2009-05-11 | 주식회사 지에스메디칼 | A rod clamp |
| US9439681B2 (en) | 2007-07-20 | 2016-09-13 | DePuy Synthes Products, Inc. | Polyaxial bone fixation element |
| KR20100043149A (en) | 2007-07-20 | 2010-04-28 | 신세스 게엠바하 | Polyaxial bone fixation element |
| FR2921248A1 (en) | 2007-09-25 | 2009-03-27 | Abbott Spine Sa | DEVICE FOR TIGHTENING TWO PORTIONS OF A BRAID AND INTERVERTEBRAL IMPLANT COMPRISING A BILGE, A BRAID AND A SUCH TIGHTENING DEVICE |
| US8096998B2 (en) | 2007-09-26 | 2012-01-17 | Ebi, Llc | External fixation tensioner |
| US20090088803A1 (en) | 2007-10-01 | 2009-04-02 | Warsaw Orthopedic, Inc. | Flexible members for correcting spinal deformities |
| US8147519B2 (en) | 2007-10-09 | 2012-04-03 | Warsaw Orthopedic, Inc. | Variable angle rod connectors and the methods of use |
| US8038701B2 (en) | 2007-10-22 | 2011-10-18 | K2M, Inc. | Uni-planar, taper lock bone screw |
| EP2052689B1 (en) | 2007-10-23 | 2011-12-14 | Zimmer Spine | Fixing devices and stabilization systems using said fixing devices |
| JP5455129B2 (en) | 2007-10-23 | 2014-03-26 | アルファテック スパイン, インコーポレイテッド | Spine stabilization system |
| US8398683B2 (en) | 2007-10-23 | 2013-03-19 | Pioneer Surgical Technology, Inc. | Rod coupling assembly and methods for bone fixation |
| GB0720762D0 (en) | 2007-10-24 | 2007-12-05 | Depuy Spine Sorl | Assembly for orthopaedic surgery |
| US9232968B2 (en) * | 2007-12-19 | 2016-01-12 | DePuy Synthes Products, Inc. | Polymeric pedicle rods and methods of manufacturing |
| US8366746B2 (en) * | 2008-01-03 | 2013-02-05 | Kiester P Douglas | Spine reconstruction rod extender |
| US8864798B2 (en) * | 2008-01-18 | 2014-10-21 | Globus Medical, Inc. | Transverse connector |
| WO2009097624A2 (en) | 2008-02-02 | 2009-08-06 | Texas Scottish Rite Hospital For Children | Spinal rod link reducer |
| US8298266B2 (en) | 2008-04-11 | 2012-10-30 | Warsaw Orthopedic, Inc. | Connectors for elongated surgical members and methods of use |
| US9504494B2 (en) | 2008-04-28 | 2016-11-29 | DePuy Synthes Products, Inc. | Implants for securing spinal fixation elements |
| ES2672778T3 (en) | 2008-06-11 | 2018-06-18 | K2M, Inc. | Rod reduction device |
| WO2010002466A1 (en) | 2008-07-01 | 2010-01-07 | Alphatec Spine, Inc. | A screw assembly |
| US8398684B2 (en) | 2008-07-29 | 2013-03-19 | Aflatoon Kamran | Bone anchoring member |
| US8257367B2 (en) | 2008-08-12 | 2012-09-04 | Pioneer Surgical Technology, Inc. | Surgical cable tensioning apparatus and method |
| US8252025B2 (en) | 2008-09-03 | 2012-08-28 | Zimmer Spine, Inc. | Vertebral fixation system |
| US9282998B2 (en) | 2008-09-05 | 2016-03-15 | DePuy Synthes Products, Inc. | Bone fixation assembly |
| PL2337512T3 (en) | 2008-09-12 | 2012-09-28 | Synthes Gmbh | Spinal stabilizing and guiding fixation system |
| KR20110081208A (en) | 2008-09-29 | 2011-07-13 | 신세스 게엠바하 | Polyaxial bottom-loading screw and rod assembly |
| US20100087864A1 (en) | 2008-10-03 | 2010-04-08 | Assaf Klein | Fastener assembly that fastens to polyaxial pedicle screw |
| US20100191286A1 (en) | 2008-10-03 | 2010-07-29 | Butler Jesse P | Facet compression system and related surgical methods |
| BRPI0920181A2 (en) | 2008-11-03 | 2015-12-29 | Synthes Gmbh | uni-planar bone fixation set |
| GB2465156B (en) | 2008-11-05 | 2012-09-26 | Dalmatic Lystrup As | Bone fixation system |
| JP5555711B2 (en) | 2008-11-24 | 2014-07-23 | シンピライカ スパイン, インコーポレイテッド | Methods and devices for limiting spinal segment flexion and extension |
| US8172772B2 (en) | 2008-12-11 | 2012-05-08 | Ethicon Endo-Surgery, Inc. | Specimen retrieval device |
| US8137356B2 (en) | 2008-12-29 | 2012-03-20 | Zimmer Spine, Inc. | Flexible guide for insertion of a vertebral stabilization system |
| US8998961B1 (en) | 2009-02-26 | 2015-04-07 | Lanx, Inc. | Spinal rod connector and methods |
| US8911470B2 (en) | 2012-09-04 | 2014-12-16 | A.M. Surgical, Inc. | Compact endoscopic surgical blade assembly and method of use thereof |
| US20100241172A1 (en) | 2009-03-23 | 2010-09-23 | Ashok Biyani | Pedicle screw including stationary and movable members for facilitating the surgical correction of spinal deformities |
| US9351767B2 (en) | 2009-03-24 | 2016-05-31 | Life Spine, Inc. | Supplementary spinal fixation/stabilization apparatus with dynamic inter-vertebral connection |
| US8882803B2 (en) | 2009-04-01 | 2014-11-11 | Globus Medical, Inc. | Orthopedic clamp and extension rod |
| JP2012523927A (en) | 2009-04-15 | 2012-10-11 | ジンテス ゲゼルシャフト ミット ベシュレンクテル ハフツング | Correction connector for spinal components |
| BRPI1011563A2 (en) | 2009-05-12 | 2016-04-05 | Synthes Gmbh | bone fixation with self-retaining clamp |
| US20100292736A1 (en) | 2009-05-15 | 2010-11-18 | Warsaw Orthopedic, Inc. | Linkage for Connection of Fusion and Non-Fusion Systems |
| US8382805B2 (en) | 2009-06-02 | 2013-02-26 | Alphatec Spine, Inc. | Bone screw assembly for limited angulation |
| US8430913B2 (en) * | 2009-06-10 | 2013-04-30 | Spine Wave, Inc. | Devices and methods for adding an additional level of fixation to an existing construct |
| US20100313428A1 (en) | 2009-06-12 | 2010-12-16 | Osteomed L.P. | Multifunctional Plate Cutter |
| EP2757988A4 (en) | 2009-06-15 | 2015-08-19 | Jackson Roger P | Polyaxial bone anchor with pop-on shank and winged insert with friction fit compressive collet |
| US8998959B2 (en) | 2009-06-15 | 2015-04-07 | Roger P Jackson | Polyaxial bone anchors with pop-on shank, fully constrained friction fit retainer and lock and release insert |
| BRPI1012921A2 (en) | 2009-06-17 | 2016-04-05 | Synthes Gmbh | revision connector for spinal construction |
| EP2279707A1 (en) | 2009-07-31 | 2011-02-02 | Zimmer Spine | Bone fixing system |
| EP2609883B1 (en) | 2009-08-12 | 2016-11-02 | Biedermann Technologies GmbH & Co. KG | A receiving part for receiving a rod for coupling the rod to a bone anchoring element |
| AU2010303934B2 (en) | 2009-10-05 | 2014-03-27 | Roger P. Jackson | Polyaxial bone anchor with non-pivotable retainer and pop-on shank, some with friction fit |
| US9814493B2 (en) | 2009-10-12 | 2017-11-14 | Globus Medical, Inc. | Trans-iliac connector |
| US8216245B2 (en) | 2009-10-30 | 2012-07-10 | Warsaw Orthopedic | Apparatus and method for applying sustained tension on a tether |
| GB0922614D0 (en) | 2009-12-23 | 2010-02-10 | Butterfield Forbes | Device |
| US20110276051A1 (en) | 2010-03-09 | 2011-11-10 | Vot, Llc | Tether and apparatus for performing a bone resection and method of use |
| WO2011115738A2 (en) | 2010-03-17 | 2011-09-22 | Dean Lin | System and method for pedicle screw placement in vertebral alignment |
| US9486296B2 (en) | 2010-07-08 | 2016-11-08 | Warsaw Orthopedic, Inc. | Surgical assembly with flexible arm |
| EP2624774A4 (en) | 2010-10-06 | 2014-01-15 | Simpirica Spine Inc | Device and accessories for limiting flexion |
| US8834540B2 (en) | 2010-10-20 | 2014-09-16 | Alphatec Spine, Inc. | Polyaxial bone screw with lateral connector |
| FR2968739B1 (en) | 2010-12-08 | 2012-12-28 | Implanet | DEVICE FOR TENSIONING A FLEXIBLE STRIP |
| US20140249530A1 (en) | 2011-05-11 | 2014-09-04 | George Babikian | Cerclage wire insertion device |
| US9649136B2 (en) | 2011-07-15 | 2017-05-16 | Globus Medical, Inc. | Coupling devices and methods of using the same |
| US8932296B2 (en) | 2011-09-27 | 2015-01-13 | Oak Tree Engineering Llc | Spinal rod persuader |
| US8758411B1 (en) | 2011-10-25 | 2014-06-24 | Nuvasive, Inc. | Implants and methods for treating spinal disorders |
| WO2013106217A1 (en) | 2012-01-10 | 2013-07-18 | Jackson, Roger, P. | Multi-start closures for open implants |
| US8870881B2 (en) | 2012-04-06 | 2014-10-28 | Warsaw Orthopedic, Inc. | Spinal correction system and method |
| US8911478B2 (en) | 2012-11-21 | 2014-12-16 | Roger P. Jackson | Splay control closure for open bone anchor |
| US9717533B2 (en) | 2013-12-12 | 2017-08-01 | Roger P. Jackson | Bone anchor closure pivot-splay control flange form guide and advancement structure |
| US9451993B2 (en) | 2014-01-09 | 2016-09-27 | Roger P. Jackson | Bi-radial pop-on cervical bone anchor |
-
2010
- 2010-06-17 BR BRPI1012921A patent/BRPI1012921A2/en not_active IP Right Cessation
- 2010-06-17 US US12/817,920 patent/US9510862B2/en active Active
- 2010-06-17 WO PCT/US2010/039037 patent/WO2010148231A1/en active Application Filing
- 2010-06-17 KR KR1020127000779A patent/KR20120039622A/en active IP Right Grant
- 2010-06-17 JP JP2012516310A patent/JP5654584B2/en active Active
- 2010-06-17 EP EP10728979.5A patent/EP2442738B1/en active Active
- 2010-06-17 CN CN201080025793.2A patent/CN102458279B/en active Active
- 2010-06-17 CA CA2764841A patent/CA2764841A1/en not_active Abandoned
-
2016
- 2016-11-11 US US15/349,509 patent/US11006978B2/en active Active
-
2021
- 2021-04-15 US US17/231,256 patent/US12089877B2/en active Active
Also Published As
| Publication number | Publication date |
|---|---|
| CN102458279B (en) | 2014-10-15 |
| US20100324599A1 (en) | 2010-12-23 |
| KR20120039622A (en) | 2012-04-25 |
| BRPI1012921A2 (en) | 2016-04-05 |
| US11006978B2 (en) | 2021-05-18 |
| JP2012530550A (en) | 2012-12-06 |
| EP2442738A1 (en) | 2012-04-25 |
| US9510862B2 (en) | 2016-12-06 |
| WO2010148231A1 (en) | 2010-12-23 |
| CA2764841A1 (en) | 2010-12-23 |
| EP2442738B1 (en) | 2014-04-30 |
| US20210244448A1 (en) | 2021-08-12 |
| US12089877B2 (en) | 2024-09-17 |
| CN102458279A (en) | 2012-05-16 |
| US20170112540A1 (en) | 2017-04-27 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| JP5654584B2 (en) | Correction connector for spine construction | |
| US20210251663A1 (en) | Revision connector for spinal constructs | |
| US11484348B2 (en) | Uni-planer bone fixation assembly | |
| USRE46371E1 (en) | Bone fixation assembly and method | |
| JP4119123B2 (en) | Bone screw for variable angle connection to longitudinal retainer | |
| JP4498412B2 (en) | Multi-axis pattern joining screw assembly having deflection angle | |
| US8277490B2 (en) | Translational manipulation polyaxial screw head | |
| US9498254B2 (en) | Bottom-loading bone anchor assemblies | |
| US8652178B2 (en) | Polyaxial pedicle screw assembly and method | |
| US20060200128A1 (en) | Bone anchor | |
| US20060195086A1 (en) | Integral, articulated, pedicle screw and longitudinal member for spinal osteosynthesis | |
| JP2009511171A (en) | Multi-directional moving device for fixing the spine during osteosynthesis surgery | |
| JP2003526444A (en) | Polyaxial bone anchor system | |
| JP2007516811A (en) | Bone anchor assembly and method for manufacturing bone anchor assembly | |
| JP2010504833A (en) | Transformer connector | |
| US20140343613A1 (en) | Bone anchoring member with clamp mechanism | |
| US20120035667A1 (en) | Locking mechanisms for pivoting bone anchors | |
| US20160128734A1 (en) | Threaded Setscrew Crosslink |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| A521 | Request for written amendment filed |
Free format text: JAPANESE INTERMEDIATE CODE: A523 Effective date: 20130617 |
|
| A621 | Written request for application examination |
Free format text: JAPANESE INTERMEDIATE CODE: A621 Effective date: 20130617 |
|
| A977 | Report on retrieval |
Free format text: JAPANESE INTERMEDIATE CODE: A971007 Effective date: 20140219 |
|
| A131 | Notification of reasons for refusal |
Free format text: JAPANESE INTERMEDIATE CODE: A131 Effective date: 20140224 |
|
| A601 | Written request for extension of time |
Free format text: JAPANESE INTERMEDIATE CODE: A601 Effective date: 20140520 |
|
| A602 | Written permission of extension of time |
Free format text: JAPANESE INTERMEDIATE CODE: A602 Effective date: 20140527 |
|
| A524 | Written submission of copy of amendment under article 19 pct |
Free format text: JAPANESE INTERMEDIATE CODE: A524 Effective date: 20140724 |
|
| TRDD | Decision of grant or rejection written | ||
| A01 | Written decision to grant a patent or to grant a registration (utility model) |
Free format text: JAPANESE INTERMEDIATE CODE: A01 Effective date: 20141117 |
|
| A61 | First payment of annual fees (during grant procedure) |
Free format text: JAPANESE INTERMEDIATE CODE: A61 Effective date: 20141120 |
|
| R150 | Certificate of patent or registration of utility model |
Ref document number: 5654584 Country of ref document: JP Free format text: JAPANESE INTERMEDIATE CODE: R150 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |