WO2010141861A1 - Synthetic glucopyranosyl lipid adjuvants - Google Patents
Synthetic glucopyranosyl lipid adjuvants Download PDFInfo
- Publication number
- WO2010141861A1 WO2010141861A1 PCT/US2010/037466 US2010037466W WO2010141861A1 WO 2010141861 A1 WO2010141861 A1 WO 2010141861A1 US 2010037466 W US2010037466 W US 2010037466W WO 2010141861 A1 WO2010141861 A1 WO 2010141861A1
- Authority
- WO
- WIPO (PCT)
- Prior art keywords
- gla
- mmol
- antigen
- compound
- vaccine
- Prior art date
Links
- -1 glucopyranosyl lipid Chemical class 0.000 title claims description 50
- 239000002671 adjuvant Substances 0.000 title description 66
- 239000000203 mixture Substances 0.000 claims abstract description 186
- 229960005486 vaccine Drugs 0.000 claims abstract description 84
- 238000000034 method Methods 0.000 claims abstract description 69
- 150000001875 compounds Chemical class 0.000 claims abstract description 67
- 230000028993 immune response Effects 0.000 claims abstract description 50
- 239000008194 pharmaceutical composition Substances 0.000 claims abstract description 24
- 150000003839 salts Chemical class 0.000 claims abstract description 15
- 230000002708 enhancing effect Effects 0.000 claims abstract description 6
- 239000000427 antigen Substances 0.000 claims description 143
- 108091007433 antigens Proteins 0.000 claims description 142
- 102000036639 antigens Human genes 0.000 claims description 142
- 125000000217 alkyl group Chemical group 0.000 claims description 19
- 239000002253 acid Substances 0.000 claims description 18
- 125000000524 functional group Chemical group 0.000 claims description 12
- 239000000546 pharmaceutical excipient Substances 0.000 claims description 11
- 238000003259 recombinant expression Methods 0.000 claims description 11
- 239000013598 vector Substances 0.000 claims description 9
- 239000003937 drug carrier Substances 0.000 claims description 7
- 230000004936 stimulating effect Effects 0.000 claims description 6
- 230000015788 innate immune response Effects 0.000 claims description 4
- 241000701161 unidentified adenovirus Species 0.000 claims description 4
- 239000013603 viral vector Substances 0.000 claims description 4
- 241001529453 unidentified herpesvirus Species 0.000 claims description 3
- 241001430294 unidentified retrovirus Species 0.000 claims description 3
- 241000702421 Dependoparvovirus Species 0.000 claims description 2
- 241000713666 Lentivirus Species 0.000 claims description 2
- 239000013604 expression vector Substances 0.000 claims description 2
- YGPZYYDTPXVBRA-RTDBHSBRSA-N [(2r,3s,4r,5r,6s)-2-[[(2r,3r,4r,5s,6r)-3-[[(3r)-3-dodecanoyloxytetradecanoyl]amino]-6-(hydroxymethyl)-5-phosphonooxy-4-[(3r)-3-tetradecanoyloxytetradecanoyl]oxyoxan-2-yl]oxymethyl]-3,6-dihydroxy-5-[[(3r)-3-hydroxytetradecanoyl]amino]oxan-4-yl] (3r)-3-hydr Chemical compound O1[C@H](CO)[C@@H](OP(O)(O)=O)[C@H](OC(=O)C[C@@H](CCCCCCCCCCC)OC(=O)CCCCCCCCCCCCC)[C@@H](NC(=O)C[C@@H](CCCCCCCCCCC)OC(=O)CCCCCCCCCCC)[C@@H]1OC[C@@H]1[C@@H](O)[C@H](OC(=O)C[C@H](O)CCCCCCCCCCC)[C@@H](NC(=O)C[C@H](O)CCCCCCCCCCC)[C@@H](O)O1 YGPZYYDTPXVBRA-RTDBHSBRSA-N 0.000 abstract description 95
- 230000001939 inductive effect Effects 0.000 abstract description 4
- XEKOWRVHYACXOJ-UHFFFAOYSA-N Ethyl acetate Chemical compound CCOC(C)=O XEKOWRVHYACXOJ-UHFFFAOYSA-N 0.000 description 159
- YMWUJEATGCHHMB-UHFFFAOYSA-N Dichloromethane Chemical compound ClCCl YMWUJEATGCHHMB-UHFFFAOYSA-N 0.000 description 114
- VLKZOEOYAKHREP-UHFFFAOYSA-N n-Hexane Chemical class CCCCCC VLKZOEOYAKHREP-UHFFFAOYSA-N 0.000 description 94
- OKKJLVBELUTLKV-UHFFFAOYSA-N Methanol Chemical compound OC OKKJLVBELUTLKV-UHFFFAOYSA-N 0.000 description 51
- 239000003921 oil Substances 0.000 description 45
- 235000019198 oils Nutrition 0.000 description 44
- 239000000243 solution Substances 0.000 description 44
- RTZKZFJDLAIYFH-UHFFFAOYSA-N Diethyl ether Chemical compound CCOCC RTZKZFJDLAIYFH-UHFFFAOYSA-N 0.000 description 42
- 210000004027 cell Anatomy 0.000 description 42
- 238000005160 1H NMR spectroscopy Methods 0.000 description 37
- UIIMBOGNXHQVGW-UHFFFAOYSA-M Sodium bicarbonate Chemical compound [Na+].OC([O-])=O UIIMBOGNXHQVGW-UHFFFAOYSA-M 0.000 description 37
- 239000000839 emulsion Substances 0.000 description 35
- 108090000623 proteins and genes Proteins 0.000 description 34
- 208000015181 infectious disease Diseases 0.000 description 33
- 239000000047 product Substances 0.000 description 33
- XLYOFNOQVPJJNP-UHFFFAOYSA-N water Substances O XLYOFNOQVPJJNP-UHFFFAOYSA-N 0.000 description 33
- 206010028980 Neoplasm Diseases 0.000 description 32
- 102000004169 proteins and genes Human genes 0.000 description 32
- 108090000765 processed proteins & peptides Proteins 0.000 description 27
- 239000007787 solid Substances 0.000 description 27
- 102000002689 Toll-like receptor Human genes 0.000 description 24
- 108020000411 Toll-like receptor Proteins 0.000 description 24
- 238000010898 silica gel chromatography Methods 0.000 description 22
- 201000011510 cancer Diseases 0.000 description 21
- 201000008827 tuberculosis Diseases 0.000 description 21
- 208000023275 Autoimmune disease Diseases 0.000 description 20
- 241000282414 Homo sapiens Species 0.000 description 20
- 201000004792 malaria Diseases 0.000 description 20
- 230000004044 response Effects 0.000 description 20
- CQLSSOINHTZFKU-UHFFFAOYSA-N 2-decanoyloxytetradecanoic acid Chemical compound CCCCCCCCCCCCC(C(O)=O)OC(=O)CCCCCCCCC CQLSSOINHTZFKU-UHFFFAOYSA-N 0.000 description 19
- WQZGKKKJIJFFOK-GASJEMHNSA-N Glucose Chemical compound OC[C@H]1OC(O)[C@H](O)[C@@H](O)[C@@H]1O WQZGKKKJIJFFOK-GASJEMHNSA-N 0.000 description 19
- 208000037265 diseases, disorders, signs and symptoms Diseases 0.000 description 19
- 239000000706 filtrate Substances 0.000 description 19
- 102000004196 processed proteins & peptides Human genes 0.000 description 19
- QTBSBXVTEAMEQO-UHFFFAOYSA-N Acetic acid Chemical compound CC(O)=O QTBSBXVTEAMEQO-UHFFFAOYSA-N 0.000 description 18
- JUJWROOIHBZHMG-UHFFFAOYSA-N Pyridine Chemical compound C1=CC=NC=C1 JUJWROOIHBZHMG-UHFFFAOYSA-N 0.000 description 18
- ZMANZCXQSJIPKH-UHFFFAOYSA-N Triethylamine Chemical compound CCN(CC)CC ZMANZCXQSJIPKH-UHFFFAOYSA-N 0.000 description 18
- 239000000556 agonist Substances 0.000 description 18
- 230000000694 effects Effects 0.000 description 18
- 239000011541 reaction mixture Substances 0.000 description 18
- 102000004127 Cytokines Human genes 0.000 description 17
- 108090000695 Cytokines Proteins 0.000 description 17
- 241000701806 Human papillomavirus Species 0.000 description 17
- VYPSYNLAJGMNEJ-UHFFFAOYSA-N Silicium dioxide Chemical compound O=[Si]=O VYPSYNLAJGMNEJ-UHFFFAOYSA-N 0.000 description 17
- 201000010099 disease Diseases 0.000 description 17
- 238000009472 formulation Methods 0.000 description 17
- 210000000987 immune system Anatomy 0.000 description 17
- 230000003308 immunostimulating effect Effects 0.000 description 17
- 229910000030 sodium bicarbonate Inorganic materials 0.000 description 17
- 108010074328 Interferon-gamma Proteins 0.000 description 16
- 238000006243 chemical reaction Methods 0.000 description 16
- 238000001914 filtration Methods 0.000 description 16
- 239000007788 liquid Substances 0.000 description 16
- 229920001184 polypeptide Polymers 0.000 description 16
- 238000002360 preparation method Methods 0.000 description 16
- 229910052938 sodium sulfate Inorganic materials 0.000 description 16
- PMZURENOXWZQFD-UHFFFAOYSA-L Sodium Sulfate Chemical compound [Na+].[Na+].[O-]S([O-])(=O)=O PMZURENOXWZQFD-UHFFFAOYSA-L 0.000 description 15
- 210000001744 T-lymphocyte Anatomy 0.000 description 15
- YXFVVABEGXRONW-UHFFFAOYSA-N Toluene Chemical compound CC1=CC=CC=C1 YXFVVABEGXRONW-UHFFFAOYSA-N 0.000 description 15
- 241000700605 Viruses Species 0.000 description 15
- 229930182490 saponin Natural products 0.000 description 15
- 235000017709 saponins Nutrition 0.000 description 15
- 150000007949 saponins Chemical class 0.000 description 15
- 229920006395 saturated elastomer Polymers 0.000 description 15
- CSNNHWWHGAXBCP-UHFFFAOYSA-L Magnesium sulfate Chemical compound [Mg+2].[O-][S+2]([O-])([O-])[O-] CSNNHWWHGAXBCP-UHFFFAOYSA-L 0.000 description 14
- 238000004587 chromatography analysis Methods 0.000 description 14
- 230000003053 immunization Effects 0.000 description 14
- 238000002649 immunization Methods 0.000 description 14
- 239000003607 modifier Substances 0.000 description 14
- 244000052769 pathogen Species 0.000 description 14
- 239000002904 solvent Substances 0.000 description 14
- 210000001519 tissue Anatomy 0.000 description 14
- 241001465754 Metazoa Species 0.000 description 13
- 108091034117 Oligonucleotide Proteins 0.000 description 13
- 239000012267 brine Substances 0.000 description 13
- PRAKJMSDJKAYCZ-UHFFFAOYSA-N dodecahydrosqualene Natural products CC(C)CCCC(C)CCCC(C)CCCCC(C)CCCC(C)CCCC(C)C PRAKJMSDJKAYCZ-UHFFFAOYSA-N 0.000 description 13
- 230000014509 gene expression Effects 0.000 description 13
- 239000000568 immunological adjuvant Substances 0.000 description 13
- 230000006698 induction Effects 0.000 description 13
- HPALAKNZSZLMCH-UHFFFAOYSA-M sodium;chloride;hydrate Chemical compound O.[Na+].[Cl-] HPALAKNZSZLMCH-UHFFFAOYSA-M 0.000 description 13
- 241000725303 Human immunodeficiency virus Species 0.000 description 12
- 239000007832 Na2SO4 Substances 0.000 description 12
- 238000003556 assay Methods 0.000 description 12
- CTMZLDSMFCVUNX-VMIOUTBZSA-N cytidylyl-(3'->5')-guanosine Chemical group O=C1N=C(N)C=CN1[C@H]1[C@H](O)[C@H](OP(O)(=O)OC[C@@H]2[C@H]([C@@H](O)[C@@H](O2)N2C3=C(C(N=C(N)N3)=O)N=C2)O)[C@@H](CO)O1 CTMZLDSMFCVUNX-VMIOUTBZSA-N 0.000 description 12
- 239000003153 chemical reaction reagent Substances 0.000 description 11
- 150000002632 lipids Chemical class 0.000 description 11
- 238000004519 manufacturing process Methods 0.000 description 11
- 150000007523 nucleic acids Chemical group 0.000 description 11
- 235000017557 sodium bicarbonate Nutrition 0.000 description 11
- 239000000725 suspension Substances 0.000 description 11
- 238000011282 treatment Methods 0.000 description 11
- YYGNTYWPHWGJRM-UHFFFAOYSA-N (6E,10E,14E,18E)-2,6,10,15,19,23-hexamethyltetracosa-2,6,10,14,18,22-hexaene Chemical compound CC(C)=CCCC(C)=CCCC(C)=CCCC=C(C)CCC=C(C)CCC=C(C)C YYGNTYWPHWGJRM-UHFFFAOYSA-N 0.000 description 10
- VHYFNPMBLIVWCW-UHFFFAOYSA-N 4-Dimethylaminopyridine Chemical compound CN(C)C1=CC=NC=C1 VHYFNPMBLIVWCW-UHFFFAOYSA-N 0.000 description 10
- 102100037850 Interferon gamma Human genes 0.000 description 10
- JLCPHMBAVCMARE-UHFFFAOYSA-N [3-[[3-[[3-[[3-[[3-[[3-[[3-[[3-[[3-[[3-[[3-[[5-(2-amino-6-oxo-1H-purin-9-yl)-3-[[3-[[3-[[3-[[3-[[3-[[5-(2-amino-6-oxo-1H-purin-9-yl)-3-[[5-(2-amino-6-oxo-1H-purin-9-yl)-3-hydroxyoxolan-2-yl]methoxy-hydroxyphosphoryl]oxyoxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(5-methyl-2,4-dioxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxyoxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(5-methyl-2,4-dioxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(5-methyl-2,4-dioxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(5-methyl-2,4-dioxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methyl [5-(6-aminopurin-9-yl)-2-(hydroxymethyl)oxolan-3-yl] hydrogen phosphate Polymers Cc1cn(C2CC(OP(O)(=O)OCC3OC(CC3OP(O)(=O)OCC3OC(CC3O)n3cnc4c3nc(N)[nH]c4=O)n3cnc4c3nc(N)[nH]c4=O)C(COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3CO)n3cnc4c(N)ncnc34)n3ccc(N)nc3=O)n3cnc4c(N)ncnc34)n3ccc(N)nc3=O)n3ccc(N)nc3=O)n3ccc(N)nc3=O)n3cnc4c(N)ncnc34)n3cnc4c(N)ncnc34)n3cc(C)c(=O)[nH]c3=O)n3cc(C)c(=O)[nH]c3=O)n3ccc(N)nc3=O)n3cc(C)c(=O)[nH]c3=O)n3cnc4c3nc(N)[nH]c4=O)n3cnc4c(N)ncnc34)n3cnc4c(N)ncnc34)n3cnc4c(N)ncnc34)n3cnc4c(N)ncnc34)O2)c(=O)[nH]c1=O JLCPHMBAVCMARE-UHFFFAOYSA-N 0.000 description 10
- 108020001507 fusion proteins Proteins 0.000 description 10
- 102000037865 fusion proteins Human genes 0.000 description 10
- 230000001717 pathogenic effect Effects 0.000 description 10
- 239000000741 silica gel Substances 0.000 description 10
- 229910002027 silica gel Inorganic materials 0.000 description 10
- TUHBEKDERLKLEC-UHFFFAOYSA-N squalene Natural products CC(=CCCC(=CCCC(=CCCC=C(/C)CCC=C(/C)CC=C(C)C)C)C)C TUHBEKDERLKLEC-UHFFFAOYSA-N 0.000 description 10
- 241000699670 Mus sp. Species 0.000 description 9
- ZMXDDKWLCZADIW-UHFFFAOYSA-N N,N-Dimethylformamide Chemical compound CN(C)C=O ZMXDDKWLCZADIW-UHFFFAOYSA-N 0.000 description 9
- 241000223960 Plasmodium falciparum Species 0.000 description 9
- BHEOSNUKNHRBNM-UHFFFAOYSA-N Tetramethylsqualene Natural products CC(=C)C(C)CCC(=C)C(C)CCC(C)=CCCC=C(C)CCC(C)C(=C)CCC(C)C(C)=C BHEOSNUKNHRBNM-UHFFFAOYSA-N 0.000 description 9
- 230000000890 antigenic effect Effects 0.000 description 9
- 230000015572 biosynthetic process Effects 0.000 description 9
- 238000001514 detection method Methods 0.000 description 9
- 238000000338 in vitro Methods 0.000 description 9
- 238000001727 in vivo Methods 0.000 description 9
- 229940035032 monophosphoryl lipid a Drugs 0.000 description 9
- 244000045947 parasite Species 0.000 description 9
- UMJSCPRVCHMLSP-UHFFFAOYSA-N pyridine Natural products COC1=CC=CN=C1 UMJSCPRVCHMLSP-UHFFFAOYSA-N 0.000 description 9
- 229940031439 squalene Drugs 0.000 description 9
- 208000030507 AIDS Diseases 0.000 description 8
- HEDRZPFGACZZDS-UHFFFAOYSA-N Chloroform Chemical compound ClC(Cl)Cl HEDRZPFGACZZDS-UHFFFAOYSA-N 0.000 description 8
- 229940046168 CpG oligodeoxynucleotide Drugs 0.000 description 8
- 108700006640 OspA Proteins 0.000 description 8
- FAPWRFPIFSIZLT-UHFFFAOYSA-M Sodium chloride Chemical compound [Na+].[Cl-] FAPWRFPIFSIZLT-UHFFFAOYSA-M 0.000 description 8
- 150000001412 amines Chemical class 0.000 description 8
- 239000002585 base Substances 0.000 description 8
- 239000003795 chemical substances by application Substances 0.000 description 8
- 230000001965 increasing effect Effects 0.000 description 8
- 230000002458 infectious effect Effects 0.000 description 8
- 108020004707 nucleic acids Proteins 0.000 description 8
- 102000039446 nucleic acids Human genes 0.000 description 8
- 239000012074 organic phase Substances 0.000 description 8
- 239000012071 phase Substances 0.000 description 8
- 125000006239 protecting group Chemical group 0.000 description 8
- 239000001397 quillaja saponaria molina bark Substances 0.000 description 8
- 230000002829 reductive effect Effects 0.000 description 8
- 238000003786 synthesis reaction Methods 0.000 description 8
- LFQSCWFLJHTTHZ-UHFFFAOYSA-N Ethanol Chemical compound CCO LFQSCWFLJHTTHZ-UHFFFAOYSA-N 0.000 description 7
- 101000669447 Homo sapiens Toll-like receptor 4 Proteins 0.000 description 7
- VEXZGXHMUGYJMC-UHFFFAOYSA-N Hydrochloric acid Chemical compound Cl VEXZGXHMUGYJMC-UHFFFAOYSA-N 0.000 description 7
- 102100039360 Toll-like receptor 4 Human genes 0.000 description 7
- 238000007792 addition Methods 0.000 description 7
- 210000004369 blood Anatomy 0.000 description 7
- 239000008280 blood Substances 0.000 description 7
- SQQXRXKYTKFFSM-UHFFFAOYSA-N chembl1992147 Chemical compound OC1=C(OC)C(OC)=CC=C1C1=C(C)C(C(O)=O)=NC(C=2N=C3C4=NC(C)(C)N=C4C(OC)=C(O)C3=CC=2)=C1N SQQXRXKYTKFFSM-UHFFFAOYSA-N 0.000 description 7
- 239000012230 colorless oil Substances 0.000 description 7
- 239000003085 diluting agent Substances 0.000 description 7
- 239000002158 endotoxin Substances 0.000 description 7
- 229940124669 imidazoquinoline Drugs 0.000 description 7
- 230000036039 immunity Effects 0.000 description 7
- 238000002347 injection Methods 0.000 description 7
- 239000007924 injection Substances 0.000 description 7
- 229910052943 magnesium sulfate Inorganic materials 0.000 description 7
- 239000002245 particle Substances 0.000 description 7
- 235000000346 sugar Nutrition 0.000 description 7
- 238000002560 therapeutic procedure Methods 0.000 description 7
- 238000002255 vaccination Methods 0.000 description 7
- HUGDBOLAOLFPKW-KFMIKNBQSA-N (2R)-3-decanoyloxy-2-phenacyltetradecanoic acid Chemical compound CCCCCCCCCCCC([C@@H](CC(=O)C1=CC=CC=C1)C(=O)O)OC(=O)CCCCCCCCC HUGDBOLAOLFPKW-KFMIKNBQSA-N 0.000 description 6
- HZNVUJQVZSTENZ-UHFFFAOYSA-N 2,3-dichloro-5,6-dicyano-1,4-benzoquinone Chemical compound ClC1=C(Cl)C(=O)C(C#N)=C(C#N)C1=O HZNVUJQVZSTENZ-UHFFFAOYSA-N 0.000 description 6
- NGNBDVOYPDDBFK-UHFFFAOYSA-N 2-[2,4-di(pentan-2-yl)phenoxy]acetyl chloride Chemical compound CCCC(C)C1=CC=C(OCC(Cl)=O)C(C(C)CCC)=C1 NGNBDVOYPDDBFK-UHFFFAOYSA-N 0.000 description 6
- KPVQNXLUPNWQHM-RBEMOOQDSA-N 3-acetylpyridine adenine dinucleotide Chemical compound CC(=O)C1=CC=C[N+]([C@H]2[C@@H]([C@H](O)[C@@H](COP([O-])(=O)OP(O)(=O)OC[C@@H]3[C@H]([C@@H](O)[C@@H](O3)N3C4=NC=NC(N)=C4N=C3)O)O2)O)=C1 KPVQNXLUPNWQHM-RBEMOOQDSA-N 0.000 description 6
- FQKGSCOHCDSKAC-UHFFFAOYSA-N 4-[3-cyanopropyl(dimethoxy)silyl]butanenitrile Chemical compound N#CCCC[Si](OC)(CCCC#N)OC FQKGSCOHCDSKAC-UHFFFAOYSA-N 0.000 description 6
- QGZKDVFQNNGYKY-UHFFFAOYSA-N Ammonia Chemical compound N QGZKDVFQNNGYKY-UHFFFAOYSA-N 0.000 description 6
- 108010012236 Chemokines Proteins 0.000 description 6
- 102000019034 Chemokines Human genes 0.000 description 6
- 108020004414 DNA Proteins 0.000 description 6
- QOSSAOTZNIDXMA-UHFFFAOYSA-N Dicylcohexylcarbodiimide Chemical compound C1CCCCC1N=C=NC1CCCCC1 QOSSAOTZNIDXMA-UHFFFAOYSA-N 0.000 description 6
- 238000002965 ELISA Methods 0.000 description 6
- 108060008682 Tumor Necrosis Factor Proteins 0.000 description 6
- 102000000852 Tumor Necrosis Factor-alpha Human genes 0.000 description 6
- HVYWMOMLDIMFJA-DPAQBDIFSA-N cholesterol Chemical compound C1C=C2C[C@@H](O)CC[C@]2(C)[C@@H]2[C@@H]1[C@@H]1CC[C@H]([C@H](C)CCCC(C)C)[C@@]1(C)CC2 HVYWMOMLDIMFJA-DPAQBDIFSA-N 0.000 description 6
- 238000010511 deprotection reaction Methods 0.000 description 6
- 230000001900 immune effect Effects 0.000 description 6
- 239000010410 layer Substances 0.000 description 6
- 229920006008 lipopolysaccharide Polymers 0.000 description 6
- 210000002540 macrophage Anatomy 0.000 description 6
- UOZZAMWODZQSOA-CQSZACIVSA-N methyl (3r)-3-hydroxytetradecanoate Chemical compound CCCCCCCCCCC[C@@H](O)CC(=O)OC UOZZAMWODZQSOA-CQSZACIVSA-N 0.000 description 6
- 239000012044 organic layer Substances 0.000 description 6
- 230000003389 potentiating effect Effects 0.000 description 6
- 229940002612 prodrug Drugs 0.000 description 6
- 239000000651 prodrug Substances 0.000 description 6
- 230000000638 stimulation Effects 0.000 description 6
- 239000006188 syrup Substances 0.000 description 6
- 235000020357 syrup Nutrition 0.000 description 6
- 238000012360 testing method Methods 0.000 description 6
- 239000003053 toxin Substances 0.000 description 6
- 231100000765 toxin Toxicity 0.000 description 6
- 108700012359 toxins Proteins 0.000 description 6
- NDCDVTWILZGAIG-HXUWFJFHSA-N (3r)-3-phenylmethoxytetradecanoic acid Chemical compound CCCCCCCCCCC[C@H](CC(O)=O)OCC1=CC=CC=C1 NDCDVTWILZGAIG-HXUWFJFHSA-N 0.000 description 5
- ATRNZOYKSNPPBF-UHFFFAOYSA-N 3-hydroxytetradecanoic acid Chemical compound CCCCCCCCCCCC(O)CC(O)=O ATRNZOYKSNPPBF-UHFFFAOYSA-N 0.000 description 5
- WEVYAHXRMPXWCK-UHFFFAOYSA-N Acetonitrile Chemical compound CC#N WEVYAHXRMPXWCK-UHFFFAOYSA-N 0.000 description 5
- 241000894006 Bacteria Species 0.000 description 5
- 101000831567 Homo sapiens Toll-like receptor 2 Proteins 0.000 description 5
- 206010020751 Hypersensitivity Diseases 0.000 description 5
- 102000013462 Interleukin-12 Human genes 0.000 description 5
- 108010065805 Interleukin-12 Proteins 0.000 description 5
- 208000004554 Leishmaniasis Diseases 0.000 description 5
- 241000223810 Plasmodium vivax Species 0.000 description 5
- 102100024333 Toll-like receptor 2 Human genes 0.000 description 5
- HCHKCACWOHOZIP-UHFFFAOYSA-N Zinc Chemical compound [Zn] HCHKCACWOHOZIP-UHFFFAOYSA-N 0.000 description 5
- 230000004913 activation Effects 0.000 description 5
- 230000007815 allergy Effects 0.000 description 5
- 229940037003 alum Drugs 0.000 description 5
- 101150078331 ama-1 gene Proteins 0.000 description 5
- 238000004458 analytical method Methods 0.000 description 5
- 239000000872 buffer Substances 0.000 description 5
- 239000000969 carrier Substances 0.000 description 5
- 230000001413 cellular effect Effects 0.000 description 5
- 239000002274 desiccant Substances 0.000 description 5
- 239000003599 detergent Substances 0.000 description 5
- 239000003814 drug Substances 0.000 description 5
- 150000002148 esters Chemical class 0.000 description 5
- 239000011521 glass Substances 0.000 description 5
- 210000005260 human cell Anatomy 0.000 description 5
- 230000016784 immunoglobulin production Effects 0.000 description 5
- 239000000463 material Substances 0.000 description 5
- 230000001404 mediated effect Effects 0.000 description 5
- XSLAPWFITBDFTF-JOCHJYFZSA-N methyl (3r)-3-[(4-methoxyphenyl)methoxy]tetradecanoate Chemical compound CCCCCCCCCCC[C@H](CC(=O)OC)OCC1=CC=C(OC)C=C1 XSLAPWFITBDFTF-JOCHJYFZSA-N 0.000 description 5
- 239000002480 mineral oil Substances 0.000 description 5
- 229940042472 mineral oil Drugs 0.000 description 5
- 235000010446 mineral oil Nutrition 0.000 description 5
- 238000000746 purification Methods 0.000 description 5
- 239000011780 sodium chloride Substances 0.000 description 5
- 239000003381 stabilizer Substances 0.000 description 5
- 239000000126 substance Substances 0.000 description 5
- 239000004094 surface-active agent Substances 0.000 description 5
- 229960000984 tocofersolan Drugs 0.000 description 5
- AOBORMOPSGHCAX-DGHZZKTQSA-N tocofersolan Chemical compound OCCOC(=O)CCC(=O)OC1=C(C)C(C)=C2O[C@](CCC[C@H](C)CCC[C@H](C)CCCC(C)C)(C)CCC2=C1C AOBORMOPSGHCAX-DGHZZKTQSA-N 0.000 description 5
- 239000003981 vehicle Substances 0.000 description 5
- AOSZTAHDEDLTLQ-AZKQZHLXSA-N (1S,2S,4R,8S,9S,11S,12R,13S,19S)-6-[(3-chlorophenyl)methyl]-12,19-difluoro-11-hydroxy-8-(2-hydroxyacetyl)-9,13-dimethyl-6-azapentacyclo[10.8.0.02,9.04,8.013,18]icosa-14,17-dien-16-one Chemical compound C([C@@H]1C[C@H]2[C@H]3[C@]([C@]4(C=CC(=O)C=C4[C@@H](F)C3)C)(F)[C@@H](O)C[C@@]2([C@@]1(C1)C(=O)CO)C)N1CC1=CC=CC(Cl)=C1 AOSZTAHDEDLTLQ-AZKQZHLXSA-N 0.000 description 4
- OBECRJHRCDNGOR-OAQYLSRUSA-N (3r)-3-[(4-methoxyphenyl)methoxy]tetradecanoic acid Chemical compound CCCCCCCCCCC[C@H](CC(O)=O)OCC1=CC=C(OC)C=C1 OBECRJHRCDNGOR-OAQYLSRUSA-N 0.000 description 4
- HDNMEFKWYRFSJN-OAQYLSRUSA-N (3r)-3-[(4-methoxyphenyl)methoxy]tetradecanoyl chloride Chemical compound CCCCCCCCCCC[C@H](CC(Cl)=O)OCC1=CC=C(OC)C=C1 HDNMEFKWYRFSJN-OAQYLSRUSA-N 0.000 description 4
- WLNJGOIHOQOCJP-JOCHJYFZSA-N (3r)-3-decanoyloxytetradecanoic acid Chemical compound CCCCCCCCCCC[C@H](CC(O)=O)OC(=O)CCCCCCCCC WLNJGOIHOQOCJP-JOCHJYFZSA-N 0.000 description 4
- GVJHHUAWPYXKBD-IEOSBIPESA-N (R)-alpha-Tocopherol Natural products OC1=C(C)C(C)=C2O[C@@](CCC[C@H](C)CCC[C@H](C)CCCC(C)C)(C)CCC2=C1C GVJHHUAWPYXKBD-IEOSBIPESA-N 0.000 description 4
- 0 *CC(C(*)C(C1*)C(*CC(S)I)=*)OC1OCC1OC(*)C(*C(CC(*)O)=O)C(*C(CC(*)O)=O)C1* Chemical compound *CC(C(*)C(C1*)C(*CC(S)I)=*)OC1OCC1OC(*)C(*C(CC(*)O)=O)C(*C(CC(*)O)=O)C1* 0.000 description 4
- RYHBNJHYFVUHQT-UHFFFAOYSA-N 1,4-Dioxane Chemical compound C1COCCO1 RYHBNJHYFVUHQT-UHFFFAOYSA-N 0.000 description 4
- KDCGOANMDULRCW-UHFFFAOYSA-N 7H-purine Chemical compound N1=CNC2=NC=NC2=C1 KDCGOANMDULRCW-UHFFFAOYSA-N 0.000 description 4
- CIWBSHSKHKDKBQ-JLAZNSOCSA-N Ascorbic acid Chemical compound OC[C@H](O)[C@H]1OC(=O)C(O)=C1O CIWBSHSKHKDKBQ-JLAZNSOCSA-N 0.000 description 4
- 241000606161 Chlamydia Species 0.000 description 4
- OKKJLVBELUTLKV-MZCSYVLQSA-N Deuterated methanol Chemical compound [2H]OC([2H])([2H])[2H] OKKJLVBELUTLKV-MZCSYVLQSA-N 0.000 description 4
- PEDCQBHIVMGVHV-UHFFFAOYSA-N Glycerine Chemical compound OCC(O)CO PEDCQBHIVMGVHV-UHFFFAOYSA-N 0.000 description 4
- 208000031886 HIV Infections Diseases 0.000 description 4
- 102000008070 Interferon-gamma Human genes 0.000 description 4
- 108010002350 Interleukin-2 Proteins 0.000 description 4
- 102000000588 Interleukin-2 Human genes 0.000 description 4
- 241000222722 Leishmania <genus> Species 0.000 description 4
- 102000008072 Lymphokines Human genes 0.000 description 4
- 108010074338 Lymphokines Proteins 0.000 description 4
- 241000186359 Mycobacterium Species 0.000 description 4
- JGFZNNIVVJXRND-UHFFFAOYSA-N N,N-Diisopropylethylamine (DIPEA) Chemical compound CCN(C(C)C)C(C)C JGFZNNIVVJXRND-UHFFFAOYSA-N 0.000 description 4
- 108010057466 NF-kappa B Proteins 0.000 description 4
- 102000003945 NF-kappa B Human genes 0.000 description 4
- 108700023315 OspC Proteins 0.000 description 4
- 101100431670 Rattus norvegicus Ybx3 gene Proteins 0.000 description 4
- 240000004808 Saccharomyces cerevisiae Species 0.000 description 4
- CZMRCDWAGMRECN-UGDNZRGBSA-N Sucrose Chemical compound O[C@H]1[C@H](O)[C@@H](CO)O[C@@]1(CO)O[C@@H]1[C@H](O)[C@@H](O)[C@H](O)[C@@H](CO)O1 CZMRCDWAGMRECN-UGDNZRGBSA-N 0.000 description 4
- 229930006000 Sucrose Natural products 0.000 description 4
- 230000005867 T cell response Effects 0.000 description 4
- 206010047505 Visceral leishmaniasis Diseases 0.000 description 4
- 125000002252 acyl group Chemical group 0.000 description 4
- 208000026935 allergic disease Diseases 0.000 description 4
- 229940087168 alpha tocopherol Drugs 0.000 description 4
- 150000001413 amino acids Chemical class 0.000 description 4
- 230000005875 antibody response Effects 0.000 description 4
- 239000003963 antioxidant agent Substances 0.000 description 4
- 235000006708 antioxidants Nutrition 0.000 description 4
- 239000007864 aqueous solution Substances 0.000 description 4
- 230000001363 autoimmune Effects 0.000 description 4
- 125000004432 carbon atom Chemical group C* 0.000 description 4
- 210000001151 cytotoxic T lymphocyte Anatomy 0.000 description 4
- 229940079593 drug Drugs 0.000 description 4
- 239000000284 extract Substances 0.000 description 4
- 238000003818 flash chromatography Methods 0.000 description 4
- 230000004927 fusion Effects 0.000 description 4
- 230000001976 improved effect Effects 0.000 description 4
- JVTAAEKCZFNVCJ-UHFFFAOYSA-N lactic acid Chemical compound CC(O)C(O)=O JVTAAEKCZFNVCJ-UHFFFAOYSA-N 0.000 description 4
- 231100000252 nontoxic Toxicity 0.000 description 4
- 230000003000 nontoxic effect Effects 0.000 description 4
- 239000002953 phosphate buffered saline Substances 0.000 description 4
- 235000010482 polyoxyethylene sorbitan monooleate Nutrition 0.000 description 4
- 229920000053 polysorbate 80 Polymers 0.000 description 4
- 239000003755 preservative agent Substances 0.000 description 4
- 230000001681 protective effect Effects 0.000 description 4
- 239000000523 sample Substances 0.000 description 4
- 235000011152 sodium sulphate Nutrition 0.000 description 4
- 241000894007 species Species 0.000 description 4
- 239000005720 sucrose Substances 0.000 description 4
- 230000009885 systemic effect Effects 0.000 description 4
- 231100000331 toxic Toxicity 0.000 description 4
- 230000002588 toxic effect Effects 0.000 description 4
- 235000004835 α-tocopherol Nutrition 0.000 description 4
- 239000002076 α-tocopherol Substances 0.000 description 4
- FLHQTQQOIIZYTL-LPWJVIDDSA-N (2r,3s,4r,6r)-2-(hydroxymethyl)-6-phenylmethoxyoxane-3,4-diol Chemical compound C1[C@@H](O)[C@H](O)[C@@H](CO)O[C@H]1OCC1=CC=CC=C1 FLHQTQQOIIZYTL-LPWJVIDDSA-N 0.000 description 3
- IYESSKQVAKTOQB-AREMUKBSSA-N (3r)-3-tetradecanoyloxytetradecanoic acid Chemical compound CCCCCCCCCCCCCC(=O)O[C@@H](CC(O)=O)CCCCCCCCCCC IYESSKQVAKTOQB-AREMUKBSSA-N 0.000 description 3
- MZOFCQQQCNRIBI-VMXHOPILSA-N (3s)-4-[[(2s)-1-[[(2s)-1-[[(1s)-1-carboxy-2-hydroxyethyl]amino]-4-methyl-1-oxopentan-2-yl]amino]-5-(diaminomethylideneamino)-1-oxopentan-2-yl]amino]-3-[[2-[[(2s)-2,6-diaminohexanoyl]amino]acetyl]amino]-4-oxobutanoic acid Chemical compound OC[C@@H](C(O)=O)NC(=O)[C@H](CC(C)C)NC(=O)[C@H](CCCN=C(N)N)NC(=O)[C@H](CC(O)=O)NC(=O)CNC(=O)[C@@H](N)CCCCN MZOFCQQQCNRIBI-VMXHOPILSA-N 0.000 description 3
- ATRNZOYKSNPPBF-CYBMUJFWSA-N (R)-3-hydroxytetradecanoic acid Chemical compound CCCCCCCCCCC[C@@H](O)CC(O)=O ATRNZOYKSNPPBF-CYBMUJFWSA-N 0.000 description 3
- ONBQEOIKXPHGMB-VBSBHUPXSA-N 1-[2-[(2s,3r,4s,5r)-3,4-dihydroxy-5-(hydroxymethyl)oxolan-2-yl]oxy-4,6-dihydroxyphenyl]-3-(4-hydroxyphenyl)propan-1-one Chemical compound O[C@@H]1[C@H](O)[C@@H](CO)O[C@H]1OC1=CC(O)=CC(O)=C1C(=O)CCC1=CC=C(O)C=C1 ONBQEOIKXPHGMB-VBSBHUPXSA-N 0.000 description 3
- WVDDGKGOMKODPV-UHFFFAOYSA-N Benzyl alcohol Chemical compound OCC1=CC=CC=C1 WVDDGKGOMKODPV-UHFFFAOYSA-N 0.000 description 3
- 208000006545 Chronic Obstructive Pulmonary Disease Diseases 0.000 description 3
- 108010047041 Complementarity Determining Regions Proteins 0.000 description 3
- 241000701022 Cytomegalovirus Species 0.000 description 3
- 230000006820 DNA synthesis Effects 0.000 description 3
- 102100037840 Dehydrogenase/reductase SDR family member 2, mitochondrial Human genes 0.000 description 3
- 241000224432 Entamoeba histolytica Species 0.000 description 3
- 241000588724 Escherichia coli Species 0.000 description 3
- BDAGIHXWWSANSR-UHFFFAOYSA-N Formic acid Chemical compound OC=O BDAGIHXWWSANSR-UHFFFAOYSA-N 0.000 description 3
- 241000701044 Human gammaherpesvirus 4 Species 0.000 description 3
- 241000713772 Human immunodeficiency virus 1 Species 0.000 description 3
- 102000004895 Lipoproteins Human genes 0.000 description 3
- 108090001030 Lipoproteins Proteins 0.000 description 3
- 241000124008 Mammalia Species 0.000 description 3
- 101710151805 Mitochondrial intermediate peptidase 1 Proteins 0.000 description 3
- 108091028043 Nucleic acid sequence Proteins 0.000 description 3
- 229910019142 PO4 Inorganic materials 0.000 description 3
- KDLHZDBZIXYQEI-UHFFFAOYSA-N Palladium Chemical compound [Pd] KDLHZDBZIXYQEI-UHFFFAOYSA-N 0.000 description 3
- 241000224016 Plasmodium Species 0.000 description 3
- KWYUFKZDYYNOTN-UHFFFAOYSA-M Potassium hydroxide Chemical compound [OH-].[K+] KWYUFKZDYYNOTN-UHFFFAOYSA-M 0.000 description 3
- DNIAPMSPPWPWGF-UHFFFAOYSA-N Propylene glycol Chemical compound CC(O)CO DNIAPMSPPWPWGF-UHFFFAOYSA-N 0.000 description 3
- 101710188053 Protein D Proteins 0.000 description 3
- 101710132893 Resolvase Proteins 0.000 description 3
- 241000242683 Schistosoma haematobium Species 0.000 description 3
- 241000242677 Schistosoma japonicum Species 0.000 description 3
- HEMHJVSKTPXQMS-UHFFFAOYSA-M Sodium hydroxide Chemical compound [OH-].[Na+] HEMHJVSKTPXQMS-UHFFFAOYSA-M 0.000 description 3
- 208000035896 Twin-reversed arterial perfusion sequence Diseases 0.000 description 3
- 206010067584 Type 1 diabetes mellitus Diseases 0.000 description 3
- 241000256856 Vespidae Species 0.000 description 3
- UZQJVUCHXGYFLQ-AYDHOLPZSA-N [(2s,3r,4s,5r,6r)-4-[(2s,3r,4s,5r,6r)-4-[(2r,3r,4s,5r,6r)-4-[(2s,3r,4s,5r,6r)-3,5-dihydroxy-6-(hydroxymethyl)-4-[(2s,3r,4s,5s,6r)-3,4,5-trihydroxy-6-(hydroxymethyl)oxan-2-yl]oxyoxan-2-yl]oxy-3,5-dihydroxy-6-(hydroxymethyl)oxan-2-yl]oxy-3,5-dihydroxy-6-(hy Chemical compound O([C@H]1[C@H](O)[C@@H](CO)O[C@H]([C@@H]1O)O[C@H]1[C@H](O)[C@@H](CO)O[C@H]([C@@H]1O)O[C@H]1CC[C@]2(C)[C@H]3CC=C4[C@@]([C@@]3(CC[C@H]2[C@@]1(C=O)C)C)(C)CC(O)[C@]1(CCC(CC14)(C)C)C(=O)O[C@H]1[C@@H]([C@@H](O[C@H]2[C@@H]([C@@H](O[C@H]3[C@@H]([C@@H](O[C@H]4[C@@H]([C@@H](O[C@H]5[C@@H]([C@@H](O)[C@H](O)[C@@H](CO)O5)O)[C@H](O)[C@@H](CO)O4)O)[C@H](O)[C@@H](CO)O3)O)[C@H](O)[C@@H](CO)O2)O)[C@H](O)[C@@H](CO)O1)O)[C@@H]1O[C@H](CO)[C@@H](O)[C@H](O)[C@H]1O UZQJVUCHXGYFLQ-AYDHOLPZSA-N 0.000 description 3
- 229940024606 amino acid Drugs 0.000 description 3
- 229910021529 ammonia Inorganic materials 0.000 description 3
- 238000013459 approach Methods 0.000 description 3
- 239000012298 atmosphere Substances 0.000 description 3
- 230000005784 autoimmunity Effects 0.000 description 3
- 230000001580 bacterial effect Effects 0.000 description 3
- 230000006399 behavior Effects 0.000 description 3
- 230000008901 benefit Effects 0.000 description 3
- WQZGKKKJIJFFOK-VFUOTHLCSA-N beta-D-glucose Chemical compound OC[C@H]1O[C@@H](O)[C@H](O)[C@@H](O)[C@@H]1O WQZGKKKJIJFFOK-VFUOTHLCSA-N 0.000 description 3
- 210000000601 blood cell Anatomy 0.000 description 3
- 150000001720 carbohydrates Chemical class 0.000 description 3
- 235000014633 carbohydrates Nutrition 0.000 description 3
- 235000012000 cholesterol Nutrition 0.000 description 3
- 230000016396 cytokine production Effects 0.000 description 3
- 230000034994 death Effects 0.000 description 3
- 231100000517 death Toxicity 0.000 description 3
- 238000011161 development Methods 0.000 description 3
- 230000018109 developmental process Effects 0.000 description 3
- NAGJZTKCGNOGPW-UHFFFAOYSA-K dioxido-sulfanylidene-sulfido-$l^{5}-phosphane Chemical group [O-]P([O-])([S-])=S NAGJZTKCGNOGPW-UHFFFAOYSA-K 0.000 description 3
- 230000006334 disulfide bridging Effects 0.000 description 3
- 239000000975 dye Substances 0.000 description 3
- 229940011399 escin Drugs 0.000 description 3
- 229930186222 escin Natural products 0.000 description 3
- PQVSTLUFSYVLTO-UHFFFAOYSA-N ethyl n-ethoxycarbonylcarbamate Chemical compound CCOC(=O)NC(=O)OCC PQVSTLUFSYVLTO-UHFFFAOYSA-N 0.000 description 3
- 239000012634 fragment Substances 0.000 description 3
- 239000007789 gas Substances 0.000 description 3
- 150000004676 glycans Chemical class 0.000 description 3
- 239000001963 growth medium Substances 0.000 description 3
- 238000010438 heat treatment Methods 0.000 description 3
- 208000002672 hepatitis B Diseases 0.000 description 3
- 229940088597 hormone Drugs 0.000 description 3
- 239000005556 hormone Substances 0.000 description 3
- RAXXELZNTBOGNW-UHFFFAOYSA-N imidazole Natural products C1=CNC=N1 RAXXELZNTBOGNW-UHFFFAOYSA-N 0.000 description 3
- 150000007529 inorganic bases Chemical class 0.000 description 3
- 230000000670 limiting effect Effects 0.000 description 3
- 229940040692 lithium hydroxide monohydrate Drugs 0.000 description 3
- GLXDVVHUTZTUQK-UHFFFAOYSA-M lithium hydroxide monohydrate Substances [Li+].O.[OH-] GLXDVVHUTZTUQK-UHFFFAOYSA-M 0.000 description 3
- 238000012737 microarray-based gene expression Methods 0.000 description 3
- 239000004005 microsphere Substances 0.000 description 3
- 150000007522 mineralic acids Chemical class 0.000 description 3
- 201000006417 multiple sclerosis Diseases 0.000 description 3
- 238000012243 multiplex automated genomic engineering Methods 0.000 description 3
- 239000002773 nucleotide Substances 0.000 description 3
- 125000003729 nucleotide group Chemical group 0.000 description 3
- 239000007764 o/w emulsion Substances 0.000 description 3
- 150000007524 organic acids Chemical class 0.000 description 3
- 150000007530 organic bases Chemical class 0.000 description 3
- 235000021317 phosphate Nutrition 0.000 description 3
- 210000002381 plasma Anatomy 0.000 description 3
- 239000004033 plastic Substances 0.000 description 3
- 229920003023 plastic Polymers 0.000 description 3
- 229920001223 polyethylene glycol Polymers 0.000 description 3
- 239000000244 polyoxyethylene sorbitan monooleate Substances 0.000 description 3
- 229920001282 polysaccharide Polymers 0.000 description 3
- 239000005017 polysaccharide Substances 0.000 description 3
- 238000011321 prophylaxis Methods 0.000 description 3
- 210000002307 prostate Anatomy 0.000 description 3
- 239000012047 saturated solution Substances 0.000 description 3
- 210000002966 serum Anatomy 0.000 description 3
- 239000000377 silicon dioxide Substances 0.000 description 3
- 239000002002 slurry Substances 0.000 description 3
- 229910000104 sodium hydride Inorganic materials 0.000 description 3
- 208000024891 symptom Diseases 0.000 description 3
- 230000001225 therapeutic effect Effects 0.000 description 3
- 241000712461 unidentified influenza virus Species 0.000 description 3
- 239000011701 zinc Substances 0.000 description 3
- 229910052725 zinc Inorganic materials 0.000 description 3
- HUWSZNZAROKDRZ-RRLWZMAJSA-N (3r,4r)-3-azaniumyl-5-[[(2s,3r)-1-[(2s)-2,3-dicarboxypyrrolidin-1-yl]-3-methyl-1-oxopentan-2-yl]amino]-5-oxo-4-sulfanylpentane-1-sulfonate Chemical compound OS(=O)(=O)CC[C@@H](N)[C@@H](S)C(=O)N[C@@H]([C@H](C)CC)C(=O)N1CCC(C(O)=O)[C@H]1C(O)=O HUWSZNZAROKDRZ-RRLWZMAJSA-N 0.000 description 2
- MIOPJNTWMNEORI-GMSGAONNSA-N (S)-camphorsulfonic acid Chemical compound C1C[C@@]2(CS(O)(=O)=O)C(=O)C[C@@H]1C2(C)C MIOPJNTWMNEORI-GMSGAONNSA-N 0.000 description 2
- GVJHHUAWPYXKBD-UHFFFAOYSA-N (±)-α-Tocopherol Chemical compound OC1=C(C)C(C)=C2OC(CCCC(C)CCCC(C)CCCC(C)C)(C)CCC2=C1C GVJHHUAWPYXKBD-UHFFFAOYSA-N 0.000 description 2
- GMRQFYUYWCNGIN-UHFFFAOYSA-N 1,25-Dihydroxy-vitamin D3' Natural products C1CCC2(C)C(C(CCCC(C)(C)O)C)CCC2C1=CC=C1CC(O)CC(O)C1=C GMRQFYUYWCNGIN-UHFFFAOYSA-N 0.000 description 2
- IQFYYKKMVGJFEH-OFKYTIFKSA-N 1-[(2r,4s,5r)-4-hydroxy-5-(tritiooxymethyl)oxolan-2-yl]-5-methylpyrimidine-2,4-dione Chemical compound C1[C@H](O)[C@@H](CO[3H])O[C@H]1N1C(=O)NC(=O)C(C)=C1 IQFYYKKMVGJFEH-OFKYTIFKSA-N 0.000 description 2
- WZZBNLYBHUDSHF-DHLKQENFSA-N 1-[(3s,4s)-4-[8-(2-chloro-4-pyrimidin-2-yloxyphenyl)-7-fluoro-2-methylimidazo[4,5-c]quinolin-1-yl]-3-fluoropiperidin-1-yl]-2-hydroxyethanone Chemical compound CC1=NC2=CN=C3C=C(F)C(C=4C(=CC(OC=5N=CC=CN=5)=CC=4)Cl)=CC3=C2N1[C@H]1CCN(C(=O)CO)C[C@@H]1F WZZBNLYBHUDSHF-DHLKQENFSA-N 0.000 description 2
- UPQQXPKAYZYUKO-UHFFFAOYSA-N 2,2,2-trichloroacetamide Chemical compound OC(=N)C(Cl)(Cl)Cl UPQQXPKAYZYUKO-UHFFFAOYSA-N 0.000 description 2
- PBVZQAXFSQKDKK-UHFFFAOYSA-N 3-Methoxy-3-oxopropanoic acid Chemical compound COC(=O)CC(O)=O PBVZQAXFSQKDKK-UHFFFAOYSA-N 0.000 description 2
- FJKROLUGYXJWQN-UHFFFAOYSA-N 4-hydroxybenzoic acid Chemical compound OC(=O)C1=CC=C(O)C=C1 FJKROLUGYXJWQN-UHFFFAOYSA-N 0.000 description 2
- 102000002260 Alkaline Phosphatase Human genes 0.000 description 2
- 108020004774 Alkaline Phosphatase Proteins 0.000 description 2
- 206010059313 Anogenital warts Diseases 0.000 description 2
- 241000193830 Bacillus <bacterium> Species 0.000 description 2
- 208000023328 Basedow disease Diseases 0.000 description 2
- 108030001720 Bontoxilysin Proteins 0.000 description 2
- 241000588807 Bordetella Species 0.000 description 2
- 241000589968 Borrelia Species 0.000 description 2
- 102100032367 C-C motif chemokine 5 Human genes 0.000 description 2
- 238000011740 C57BL/6 mouse Methods 0.000 description 2
- 241000222120 Candida <Saccharomycetales> Species 0.000 description 2
- 241000222122 Candida albicans Species 0.000 description 2
- 102000014914 Carrier Proteins Human genes 0.000 description 2
- 241000193403 Clostridium Species 0.000 description 2
- 208000000907 Condylomata Acuminata Diseases 0.000 description 2
- 239000004375 Dextrin Substances 0.000 description 2
- 229920001353 Dextrin Polymers 0.000 description 2
- KCXVZYZYPLLWCC-UHFFFAOYSA-N EDTA Chemical compound OC(=O)CN(CC(O)=O)CCN(CC(O)=O)CC(O)=O KCXVZYZYPLLWCC-UHFFFAOYSA-N 0.000 description 2
- 238000012286 ELISA Assay Methods 0.000 description 2
- 241000196324 Embryophyta Species 0.000 description 2
- 102000004190 Enzymes Human genes 0.000 description 2
- 108090000790 Enzymes Proteins 0.000 description 2
- 241000713800 Feline immunodeficiency virus Species 0.000 description 2
- 241000233866 Fungi Species 0.000 description 2
- 241000224466 Giardia Species 0.000 description 2
- 108010017213 Granulocyte-Macrophage Colony-Stimulating Factor Proteins 0.000 description 2
- 102100039620 Granulocyte-macrophage colony-stimulating factor Human genes 0.000 description 2
- 208000015023 Graves' disease Diseases 0.000 description 2
- 208000037357 HIV infectious disease Diseases 0.000 description 2
- 241000606768 Haemophilus influenzae Species 0.000 description 2
- 241000700721 Hepatitis B virus Species 0.000 description 2
- 241000238631 Hexapoda Species 0.000 description 2
- 101000669406 Homo sapiens Toll-like receptor 6 Proteins 0.000 description 2
- 241000701085 Human alphaherpesvirus 3 Species 0.000 description 2
- 241000701828 Human papillomavirus type 11 Species 0.000 description 2
- UFHFLCQGNIYNRP-UHFFFAOYSA-N Hydrogen Chemical compound [H][H] UFHFLCQGNIYNRP-UHFFFAOYSA-N 0.000 description 2
- AVXURJPOCDRRFD-UHFFFAOYSA-N Hydroxylamine Chemical compound ON AVXURJPOCDRRFD-UHFFFAOYSA-N 0.000 description 2
- 241000257303 Hymenoptera Species 0.000 description 2
- 108060003951 Immunoglobulin Proteins 0.000 description 2
- 102000015696 Interleukins Human genes 0.000 description 2
- 108010063738 Interleukins Proteins 0.000 description 2
- 239000004166 Lanolin Substances 0.000 description 2
- 208000016604 Lyme disease Diseases 0.000 description 2
- 101710105759 Major outer membrane porin Proteins 0.000 description 2
- 101710164702 Major outer membrane protein Proteins 0.000 description 2
- 101710085938 Matrix protein Proteins 0.000 description 2
- 101710127721 Membrane protein Proteins 0.000 description 2
- 241001092142 Molina Species 0.000 description 2
- 208000031998 Mycobacterium Infections Diseases 0.000 description 2
- 241000186366 Mycobacterium bovis Species 0.000 description 2
- 241000186362 Mycobacterium leprae Species 0.000 description 2
- 241000187479 Mycobacterium tuberculosis Species 0.000 description 2
- KWYHDKDOAIKMQN-UHFFFAOYSA-N N,N,N',N'-tetramethylethylenediamine Chemical compound CN(C)CCN(C)C KWYHDKDOAIKMQN-UHFFFAOYSA-N 0.000 description 2
- 125000001429 N-terminal alpha-amino-acid group Chemical group 0.000 description 2
- 241000588653 Neisseria Species 0.000 description 2
- 241000721454 Pemphigus Species 0.000 description 2
- 102100035181 Plastin-1 Human genes 0.000 description 2
- 241000233870 Pneumocystis Species 0.000 description 2
- 108010072866 Prostate-Specific Antigen Proteins 0.000 description 2
- 102100038358 Prostate-specific antigen Human genes 0.000 description 2
- 235000009001 Quillaja saponaria Nutrition 0.000 description 2
- 241000725643 Respiratory syncytial virus Species 0.000 description 2
- 208000036284 Rhinitis seasonal Diseases 0.000 description 2
- 241000607142 Salmonella Species 0.000 description 2
- 241000242678 Schistosoma Species 0.000 description 2
- KEAYESYHFKHZAL-UHFFFAOYSA-N Sodium Chemical compound [Na] KEAYESYHFKHZAL-UHFFFAOYSA-N 0.000 description 2
- CDBYLPFSWZWCQE-UHFFFAOYSA-L Sodium Carbonate Chemical compound [Na+].[Na+].[O-]C([O-])=O CDBYLPFSWZWCQE-UHFFFAOYSA-L 0.000 description 2
- PXIPVTKHYLBLMZ-UHFFFAOYSA-N Sodium azide Chemical compound [Na+].[N-]=[N+]=[N-] PXIPVTKHYLBLMZ-UHFFFAOYSA-N 0.000 description 2
- PRXRUNOAOLTIEF-ADSICKODSA-N Sorbitan trioleate Chemical compound CCCCCCCC\C=C/CCCCCCCC(=O)OC[C@@H](OC(=O)CCCCCCC\C=C/CCCCCCCC)[C@H]1OC[C@H](O)[C@H]1OC(=O)CCCCCCC\C=C/CCCCCCCC PRXRUNOAOLTIEF-ADSICKODSA-N 0.000 description 2
- 229920002472 Starch Polymers 0.000 description 2
- 230000006052 T cell proliferation Effects 0.000 description 2
- 206010043561 Thrombocytopenic purpura Diseases 0.000 description 2
- 108010060818 Toll-Like Receptor 9 Proteins 0.000 description 2
- 229940123384 Toll-like receptor (TLR) agonist Drugs 0.000 description 2
- 102100039387 Toll-like receptor 6 Human genes 0.000 description 2
- 102100033117 Toll-like receptor 9 Human genes 0.000 description 2
- 241000244005 Wuchereria bancrofti Species 0.000 description 2
- LNUFLCYMSVYYNW-ZPJMAFJPSA-N [(2r,3r,4s,5r,6r)-2-[(2r,3r,4s,5r,6r)-6-[(2r,3r,4s,5r,6r)-6-[(2r,3r,4s,5r,6r)-6-[[(3s,5s,8r,9s,10s,13r,14s,17r)-10,13-dimethyl-17-[(2r)-6-methylheptan-2-yl]-2,3,4,5,6,7,8,9,11,12,14,15,16,17-tetradecahydro-1h-cyclopenta[a]phenanthren-3-yl]oxy]-4,5-disulfo Chemical compound O([C@@H]1[C@@H](COS(O)(=O)=O)O[C@@H]([C@@H]([C@H]1OS(O)(=O)=O)OS(O)(=O)=O)O[C@@H]1[C@@H](COS(O)(=O)=O)O[C@@H]([C@@H]([C@H]1OS(O)(=O)=O)OS(O)(=O)=O)O[C@@H]1[C@@H](COS(O)(=O)=O)O[C@H]([C@@H]([C@H]1OS(O)(=O)=O)OS(O)(=O)=O)O[C@@H]1C[C@@H]2CC[C@H]3[C@@H]4CC[C@@H]([C@]4(CC[C@@H]3[C@@]2(C)CC1)C)[C@H](C)CCCC(C)C)[C@H]1O[C@H](COS(O)(=O)=O)[C@@H](OS(O)(=O)=O)[C@H](OS(O)(=O)=O)[C@H]1OS(O)(=O)=O LNUFLCYMSVYYNW-ZPJMAFJPSA-N 0.000 description 2
- LUXUAZKGQZPOBZ-SAXJAHGMSA-N [(3S,4S,5S,6R)-3,4,5-trihydroxy-6-(hydroxymethyl)oxan-2-yl] (Z)-octadec-9-enoate Chemical compound CCCCCCCC\C=C/CCCCCCCC(=O)OC1O[C@H](CO)[C@@H](O)[C@H](O)[C@@H]1O LUXUAZKGQZPOBZ-SAXJAHGMSA-N 0.000 description 2
- SMNRFWMNPDABKZ-WVALLCKVSA-N [[(2R,3S,4R,5S)-5-(2,6-dioxo-3H-pyridin-3-yl)-3,4-dihydroxyoxolan-2-yl]methoxy-hydroxyphosphoryl] [[[(2R,3S,4S,5R,6R)-4-fluoro-3,5-dihydroxy-6-(hydroxymethyl)oxan-2-yl]oxy-hydroxyphosphoryl]oxy-hydroxyphosphoryl] hydrogen phosphate Chemical compound OC[C@H]1O[C@H](OP(O)(=O)OP(O)(=O)OP(O)(=O)OP(O)(=O)OC[C@H]2O[C@H]([C@H](O)[C@@H]2O)C2C=CC(=O)NC2=O)[C@H](O)[C@@H](F)[C@@H]1O SMNRFWMNPDABKZ-WVALLCKVSA-N 0.000 description 2
- 239000000443 aerosol Substances 0.000 description 2
- 125000003342 alkenyl group Chemical group 0.000 description 2
- 125000000304 alkynyl group Chemical group 0.000 description 2
- 230000004075 alteration Effects 0.000 description 2
- XAGFODPZIPBFFR-UHFFFAOYSA-N aluminium Chemical compound [Al] XAGFODPZIPBFFR-UHFFFAOYSA-N 0.000 description 2
- 229910052782 aluminium Inorganic materials 0.000 description 2
- 239000003708 ampul Substances 0.000 description 2
- 230000010056 antibody-dependent cellular cytotoxicity Effects 0.000 description 2
- 238000003782 apoptosis assay Methods 0.000 description 2
- 230000006907 apoptotic process Effects 0.000 description 2
- 235000010323 ascorbic acid Nutrition 0.000 description 2
- 229960005070 ascorbic acid Drugs 0.000 description 2
- 239000011668 ascorbic acid Substances 0.000 description 2
- 208000006673 asthma Diseases 0.000 description 2
- 230000002238 attenuated effect Effects 0.000 description 2
- 210000003719 b-lymphocyte Anatomy 0.000 description 2
- 244000052616 bacterial pathogen Species 0.000 description 2
- 229960001212 bacterial vaccine Drugs 0.000 description 2
- MSWZFWKMSRAUBD-UHFFFAOYSA-N beta-D-galactosamine Natural products NC1C(O)OC(CO)C(O)C1O MSWZFWKMSRAUBD-UHFFFAOYSA-N 0.000 description 2
- 229920002988 biodegradable polymer Polymers 0.000 description 2
- 239000004621 biodegradable polymer Substances 0.000 description 2
- 239000013060 biological fluid Substances 0.000 description 2
- 230000033228 biological regulation Effects 0.000 description 2
- 238000001574 biopsy Methods 0.000 description 2
- 229920001400 block copolymer Polymers 0.000 description 2
- 229940053031 botulinum toxin Drugs 0.000 description 2
- 210000004556 brain Anatomy 0.000 description 2
- 229960005084 calcitriol Drugs 0.000 description 2
- GMRQFYUYWCNGIN-NKMMMXOESA-N calcitriol Chemical compound C1(/[C@@H]2CC[C@@H]([C@]2(CCC1)C)[C@@H](CCCC(C)(C)O)C)=C\C=C1\C[C@@H](O)C[C@H](O)C1=C GMRQFYUYWCNGIN-NKMMMXOESA-N 0.000 description 2
- 239000003054 catalyst Substances 0.000 description 2
- 238000004113 cell culture Methods 0.000 description 2
- 230000024245 cell differentiation Effects 0.000 description 2
- 230000004663 cell proliferation Effects 0.000 description 2
- 230000036755 cellular response Effects 0.000 description 2
- 239000002738 chelating agent Substances 0.000 description 2
- QUWFSKKBMDKAHK-SBOJBMMISA-A chembl2103793 Chemical compound [Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].[Na+].O=C1NC(=O)C(C)=CN1[C@@H]1O[C@H](COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(N=C(N)C=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C3=C(C(NC(N)=N3)=O)N=C2)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(N=C(N)C=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C3=C(C(NC(N)=N3)=O)N=C2)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C3=C(C(NC(N)=N3)=O)N=C2)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(N=C(N)C=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C3=C(C(NC(N)=N3)=O)N=C2)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C3=C(C(NC(N)=N3)=O)N=C2)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(N=C(N)C=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C3=C(C(NC(N)=N3)=O)N=C2)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)COP([O-])(=S)O[C@@H]2[C@H](O[C@H](C2)N2C(NC(=O)C(C)=C2)=O)CO)[C@@H](O)C1 QUWFSKKBMDKAHK-SBOJBMMISA-A 0.000 description 2
- 239000003086 colorant Substances 0.000 description 2
- 239000000356 contaminant Substances 0.000 description 2
- 230000001461 cytolytic effect Effects 0.000 description 2
- IPIVAXLHTVNRBS-UHFFFAOYSA-N decanoyl chloride Chemical compound CCCCCCCCCC(Cl)=O IPIVAXLHTVNRBS-UHFFFAOYSA-N 0.000 description 2
- 230000003247 decreasing effect Effects 0.000 description 2
- 230000001419 dependent effect Effects 0.000 description 2
- 238000013461 design Methods 0.000 description 2
- 235000019425 dextrin Nutrition 0.000 description 2
- 238000003745 diagnosis Methods 0.000 description 2
- 238000002405 diagnostic procedure Methods 0.000 description 2
- 238000000502 dialysis Methods 0.000 description 2
- 238000010790 dilution Methods 0.000 description 2
- 239000012895 dilution Substances 0.000 description 2
- LOKCTEFSRHRXRJ-UHFFFAOYSA-I dipotassium trisodium dihydrogen phosphate hydrogen phosphate dichloride Chemical compound P(=O)(O)(O)[O-].[K+].P(=O)(O)([O-])[O-].[Na+].[Na+].[Cl-].[K+].[Cl-].[Na+] LOKCTEFSRHRXRJ-UHFFFAOYSA-I 0.000 description 2
- POULHZVOKOAJMA-UHFFFAOYSA-N dodecanoic acid Chemical compound CCCCCCCCCCCC(O)=O POULHZVOKOAJMA-UHFFFAOYSA-N 0.000 description 2
- 229940007078 entamoeba histolytica Drugs 0.000 description 2
- 238000003114 enzyme-linked immunosorbent spot assay Methods 0.000 description 2
- 210000003743 erythrocyte Anatomy 0.000 description 2
- 238000002474 experimental method Methods 0.000 description 2
- 239000000796 flavoring agent Substances 0.000 description 2
- IRXSLJNXXZKURP-UHFFFAOYSA-N fluorenylmethyloxycarbonyl chloride Chemical compound C1=CC=C2C(COC(=O)Cl)C3=CC=CC=C3C2=C1 IRXSLJNXXZKURP-UHFFFAOYSA-N 0.000 description 2
- 235000013355 food flavoring agent Nutrition 0.000 description 2
- 235000019253 formic acid Nutrition 0.000 description 2
- 239000012458 free base Substances 0.000 description 2
- 230000006870 function Effects 0.000 description 2
- 229940044627 gamma-interferon Drugs 0.000 description 2
- 229960002442 glucosamine Drugs 0.000 description 2
- 239000008103 glucose Substances 0.000 description 2
- RWSXRVCMGQZWBV-WDSKDSINSA-N glutathione Chemical compound OC(=O)[C@@H](N)CCC(=O)N[C@@H](CS)C(=O)NCC(O)=O RWSXRVCMGQZWBV-WDSKDSINSA-N 0.000 description 2
- 235000011187 glycerol Nutrition 0.000 description 2
- 239000003102 growth factor Substances 0.000 description 2
- 229940029575 guanosine Drugs 0.000 description 2
- 230000002949 hemolytic effect Effects 0.000 description 2
- 102000022382 heparin binding proteins Human genes 0.000 description 2
- 108091012216 heparin binding proteins Proteins 0.000 description 2
- 208000006454 hepatitis Diseases 0.000 description 2
- 231100000283 hepatitis Toxicity 0.000 description 2
- 238000004128 high performance liquid chromatography Methods 0.000 description 2
- 235000010181 horse chestnut Nutrition 0.000 description 2
- 208000033519 human immunodeficiency virus infectious disease Diseases 0.000 description 2
- 239000001257 hydrogen Substances 0.000 description 2
- 229910052739 hydrogen Inorganic materials 0.000 description 2
- 230000002163 immunogen Effects 0.000 description 2
- 102000018358 immunoglobulin Human genes 0.000 description 2
- 239000002955 immunomodulating agent Substances 0.000 description 2
- 229940121354 immunomodulator Drugs 0.000 description 2
- 229960001438 immunostimulant agent Drugs 0.000 description 2
- 239000003022 immunostimulating agent Substances 0.000 description 2
- 239000012535 impurity Substances 0.000 description 2
- 210000005007 innate immune system Anatomy 0.000 description 2
- 229910052500 inorganic mineral Inorganic materials 0.000 description 2
- 229960003130 interferon gamma Drugs 0.000 description 2
- 238000007918 intramuscular administration Methods 0.000 description 2
- 238000001990 intravenous administration Methods 0.000 description 2
- 210000003734 kidney Anatomy 0.000 description 2
- 239000004310 lactic acid Substances 0.000 description 2
- 235000014655 lactic acid Nutrition 0.000 description 2
- 229940039717 lanolin Drugs 0.000 description 2
- 235000019388 lanolin Nutrition 0.000 description 2
- 238000011031 large-scale manufacturing process Methods 0.000 description 2
- GZQKNULLWNGMCW-PWQABINMSA-N lipid A (E. coli) Chemical compound O1[C@H](CO)[C@@H](OP(O)(O)=O)[C@H](OC(=O)C[C@@H](CCCCCCCCCCC)OC(=O)CCCCCCCCCCCCC)[C@@H](NC(=O)C[C@@H](CCCCCCCCCCC)OC(=O)CCCCCCCCCCC)[C@@H]1OC[C@@H]1[C@@H](O)[C@H](OC(=O)C[C@H](O)CCCCCCCCCCC)[C@@H](NC(=O)C[C@H](O)CCCCCCCCCCC)[C@@H](OP(O)(O)=O)O1 GZQKNULLWNGMCW-PWQABINMSA-N 0.000 description 2
- 239000002502 liposome Substances 0.000 description 2
- 210000004072 lung Anatomy 0.000 description 2
- HQKMJHAJHXVSDF-UHFFFAOYSA-L magnesium stearate Chemical compound [Mg+2].CCCCCCCCCCCCCCCCCC([O-])=O.CCCCCCCCCCCCCCCCCC([O-])=O HQKMJHAJHXVSDF-UHFFFAOYSA-L 0.000 description 2
- 229940124735 malaria vaccine Drugs 0.000 description 2
- 239000002609 medium Substances 0.000 description 2
- 201000001441 melanoma Diseases 0.000 description 2
- 230000002503 metabolic effect Effects 0.000 description 2
- 230000004060 metabolic process Effects 0.000 description 2
- LXCFILQKKLGQFO-UHFFFAOYSA-N methylparaben Chemical compound COC(=O)C1=CC=C(O)C=C1 LXCFILQKKLGQFO-UHFFFAOYSA-N 0.000 description 2
- 230000000813 microbial effect Effects 0.000 description 2
- 235000010755 mineral Nutrition 0.000 description 2
- 239000011707 mineral Substances 0.000 description 2
- 230000004048 modification Effects 0.000 description 2
- 238000012986 modification Methods 0.000 description 2
- 239000002808 molecular sieve Substances 0.000 description 2
- 230000004899 motility Effects 0.000 description 2
- 208000027531 mycobacterial infectious disease Diseases 0.000 description 2
- JXTPJDDICSTXJX-UHFFFAOYSA-N n-Triacontane Natural products CCCCCCCCCCCCCCCCCCCCCCCCCCCCCC JXTPJDDICSTXJX-UHFFFAOYSA-N 0.000 description 2
- 229930014626 natural product Natural products 0.000 description 2
- 239000004006 olive oil Substances 0.000 description 2
- 235000008390 olive oil Nutrition 0.000 description 2
- CTSLXHKWHWQRSH-UHFFFAOYSA-N oxalyl chloride Chemical compound ClC(=O)C(Cl)=O CTSLXHKWHWQRSH-UHFFFAOYSA-N 0.000 description 2
- NFHFRUOZVGFOOS-UHFFFAOYSA-N palladium;triphenylphosphane Chemical compound [Pd].C1=CC=CC=C1P(C=1C=CC=CC=1)C1=CC=CC=C1.C1=CC=CC=C1P(C=1C=CC=CC=1)C1=CC=CC=C1.C1=CC=CC=C1P(C=1C=CC=CC=1)C1=CC=CC=C1.C1=CC=CC=C1P(C=1C=CC=CC=1)C1=CC=CC=C1 NFHFRUOZVGFOOS-UHFFFAOYSA-N 0.000 description 2
- 230000008506 pathogenesis Effects 0.000 description 2
- NBIIXXVUZAFLBC-UHFFFAOYSA-K phosphate Chemical compound [O-]P([O-])([O-])=O NBIIXXVUZAFLBC-UHFFFAOYSA-K 0.000 description 2
- 239000010452 phosphate Substances 0.000 description 2
- 150000004713 phosphodiesters Chemical class 0.000 description 2
- 108010049148 plastin Proteins 0.000 description 2
- 201000000317 pneumocystosis Diseases 0.000 description 2
- 229920000747 poly(lactic acid) Polymers 0.000 description 2
- 229920001606 poly(lactic acid-co-glycolic acid) Polymers 0.000 description 2
- 229940068917 polyethylene glycols Drugs 0.000 description 2
- 229920000136 polysorbate Polymers 0.000 description 2
- BWHMMNNQKKPAPP-UHFFFAOYSA-L potassium carbonate Chemical compound [K+].[K+].[O-]C([O-])=O BWHMMNNQKKPAPP-UHFFFAOYSA-L 0.000 description 2
- 239000000843 powder Substances 0.000 description 2
- 230000005522 programmed cell death Effects 0.000 description 2
- 230000000069 prophylactic effect Effects 0.000 description 2
- GRJJQCWNZGRKAU-UHFFFAOYSA-N pyridin-1-ium;fluoride Chemical compound F.C1=CC=NC=C1 GRJJQCWNZGRKAU-UHFFFAOYSA-N 0.000 description 2
- 238000003127 radioimmunoassay Methods 0.000 description 2
- 238000011084 recovery Methods 0.000 description 2
- 230000009467 reduction Effects 0.000 description 2
- 238000010992 reflux Methods 0.000 description 2
- 206010039073 rheumatoid arthritis Diseases 0.000 description 2
- 230000003248 secreting effect Effects 0.000 description 2
- 230000035945 sensitivity Effects 0.000 description 2
- 238000013207 serial dilution Methods 0.000 description 2
- 230000019491 signal transduction Effects 0.000 description 2
- URGAHOPLAPQHLN-UHFFFAOYSA-N sodium aluminosilicate Chemical compound [Na+].[Al+3].[O-][Si]([O-])=O.[O-][Si]([O-])=O URGAHOPLAPQHLN-UHFFFAOYSA-N 0.000 description 2
- 239000012312 sodium hydride Substances 0.000 description 2
- 239000007790 solid phase Substances 0.000 description 2
- 239000012453 solvate Substances 0.000 description 2
- 210000004988 splenocyte Anatomy 0.000 description 2
- 239000007921 spray Substances 0.000 description 2
- 230000007480 spreading Effects 0.000 description 2
- 238000003892 spreading Methods 0.000 description 2
- 229940032094 squalane Drugs 0.000 description 2
- 239000008107 starch Substances 0.000 description 2
- 235000019698 starch Nutrition 0.000 description 2
- 238000003756 stirring Methods 0.000 description 2
- 238000010254 subcutaneous injection Methods 0.000 description 2
- 239000007929 subcutaneous injection Substances 0.000 description 2
- 239000000375 suspending agent Substances 0.000 description 2
- 201000000596 systemic lupus erythematosus Diseases 0.000 description 2
- 125000003396 thiol group Chemical group [H]S* 0.000 description 2
- RYYWUUFWQRZTIU-UHFFFAOYSA-K thiophosphate Chemical compound [O-]P([O-])([O-])=S RYYWUUFWQRZTIU-UHFFFAOYSA-K 0.000 description 2
- 238000011200 topical administration Methods 0.000 description 2
- WJKHJLXJJJATHN-UHFFFAOYSA-N triflic anhydride Chemical compound FC(F)(F)S(=O)(=O)OS(=O)(=O)C(F)(F)F WJKHJLXJJJATHN-UHFFFAOYSA-N 0.000 description 2
- RIOQSEWOXXDEQQ-UHFFFAOYSA-N triphenylphosphine Chemical compound C1=CC=CC=C1P(C=1C=CC=CC=1)C1=CC=CC=C1 RIOQSEWOXXDEQQ-UHFFFAOYSA-N 0.000 description 2
- 235000015112 vegetable and seed oil Nutrition 0.000 description 2
- 239000008158 vegetable oil Substances 0.000 description 2
- ABJSOROVZZKJGI-OCYUSGCXSA-N (1r,2r,4r)-2-(4-bromophenyl)-n-[(4-chlorophenyl)-(2-fluoropyridin-4-yl)methyl]-4-morpholin-4-ylcyclohexane-1-carboxamide Chemical compound C1=NC(F)=CC(C(NC(=O)[C@H]2[C@@H](C[C@@H](CC2)N2CCOCC2)C=2C=CC(Br)=CC=2)C=2C=CC(Cl)=CC=2)=C1 ABJSOROVZZKJGI-OCYUSGCXSA-N 0.000 description 1
- XOLCPJGQMDBKQJ-GAWVXTGCSA-N (2R)-2-phenacyl-3-tetradecanoyloxytetradecanoic acid Chemical compound CCCCCCCCCCCCCC(=O)OC(CCCCCCCCCCC)[C@@H](CC(=O)C1=CC=CC=C1)C(=O)O XOLCPJGQMDBKQJ-GAWVXTGCSA-N 0.000 description 1
- YSTCVEONORJQDG-KWRHIPAJSA-N (2r)-2-benzyl-3-tetradecanoyloxytetradecanoic acid Chemical compound CCCCCCCCCCCCCC(=O)OC(CCCCCCCCCCC)[C@H](C(O)=O)CC1=CC=CC=C1 YSTCVEONORJQDG-KWRHIPAJSA-N 0.000 description 1
- ITOFPJRDSCGOSA-KZLRUDJFSA-N (2s)-2-[[(4r)-4-[(3r,5r,8r,9s,10s,13r,14s,17r)-3-hydroxy-10,13-dimethyl-2,3,4,5,6,7,8,9,11,12,14,15,16,17-tetradecahydro-1h-cyclopenta[a]phenanthren-17-yl]pentanoyl]amino]-3-(1h-indol-3-yl)propanoic acid Chemical compound C([C@H]1CC2)[C@H](O)CC[C@]1(C)[C@@H](CC[C@]13C)[C@@H]2[C@@H]3CC[C@@H]1[C@H](C)CCC(=O)N[C@H](C(O)=O)CC1=CNC2=CC=CC=C12 ITOFPJRDSCGOSA-KZLRUDJFSA-N 0.000 description 1
- WWTBZEKOSBFBEM-SPWPXUSOSA-N (2s)-2-[[2-benzyl-3-[hydroxy-[(1r)-2-phenyl-1-(phenylmethoxycarbonylamino)ethyl]phosphoryl]propanoyl]amino]-3-(1h-indol-3-yl)propanoic acid Chemical compound N([C@@H](CC=1C2=CC=CC=C2NC=1)C(=O)O)C(=O)C(CP(O)(=O)[C@H](CC=1C=CC=CC=1)NC(=O)OCC=1C=CC=CC=1)CC1=CC=CC=C1 WWTBZEKOSBFBEM-SPWPXUSOSA-N 0.000 description 1
- YFESOSRPNPYODN-RSMWSHJLSA-N (2s,3s,4s,5r,6r)-6-[[(4s,6ar,6bs,8r,8ar,9r,10r,14br)-9-acetyloxy-8-hydroxy-4,8a-bis(hydroxymethyl)-4,6a,6b,11,11,14b-hexamethyl-10-[(z)-2-methylbut-2-enoyl]oxy-1,2,3,4a,5,6,7,8,9,10,12,12a,14,14a-tetradecahydropicen-3-yl]oxy]-4-hydroxy-3,5-bis[[(2s,3r,4s, Chemical compound O([C@@H]1[C@H](O[C@H]([C@@H]([C@H]1O)O[C@H]1[C@@H]([C@@H](O)[C@H](O)[C@@H](CO)O1)O)OC1CC[C@]2(C)C3CC=C4[C@@]([C@@]3(CCC2[C@]1(CO)C)C)(C)C[C@@H](O)[C@@]1(CO)[C@@H](OC(C)=O)[C@@H](C(CC14)(C)C)OC(=O)C(\C)=C/C)C(O)=O)[C@@H]1O[C@H](CO)[C@@H](O)[C@H](O)[C@H]1O.O([C@@H]1[C@H](O[C@H]([C@@H]([C@H]1O)O[C@H]1[C@@H]([C@@H](O)[C@H](O)[C@@H](CO)O1)O)OC1CC[C@]2(C)C3CC=C4[C@@]([C@@]3(CCC2[C@]1(CO)C)C)(C)C[C@@H](O)[C@@]1(CO)[C@@H](OC(C)=O)[C@@H](C(CC14)(C)C)OC(=O)C(/C)=C/C)C(O)=O)[C@@H]1O[C@H](CO)[C@@H](O)[C@H](O)[C@H]1O YFESOSRPNPYODN-RSMWSHJLSA-N 0.000 description 1
- IWZSHWBGHQBIML-ZGGLMWTQSA-N (3S,8S,10R,13S,14S,17S)-17-isoquinolin-7-yl-N,N,10,13-tetramethyl-2,3,4,7,8,9,11,12,14,15,16,17-dodecahydro-1H-cyclopenta[a]phenanthren-3-amine Chemical compound CN(C)[C@H]1CC[C@]2(C)C3CC[C@@]4(C)[C@@H](CC[C@@H]4c4ccc5ccncc5c4)[C@@H]3CC=C2C1 IWZSHWBGHQBIML-ZGGLMWTQSA-N 0.000 description 1
- LCTORNIWLGOBPB-GASJEMHNSA-N (3r,4s,5s,6r)-2-amino-6-(hydroxymethyl)oxane-2,3,4,5-tetrol Chemical compound NC1(O)O[C@H](CO)[C@@H](O)[C@H](O)[C@H]1O LCTORNIWLGOBPB-GASJEMHNSA-N 0.000 description 1
- TYHGKLBJBHACOI-UHFFFAOYSA-N (4-methoxyphenyl)methyl 2,2,2-trichloroethanimidate Chemical compound COC1=CC=C(COC(=N)C(Cl)(Cl)Cl)C=C1 TYHGKLBJBHACOI-UHFFFAOYSA-N 0.000 description 1
- HEVMDQBCAHEHDY-UHFFFAOYSA-N (Dimethoxymethyl)benzene Chemical compound COC(OC)C1=CC=CC=C1 HEVMDQBCAHEHDY-UHFFFAOYSA-N 0.000 description 1
- UVNPEUJXKZFWSJ-LMTQTHQJSA-N (R)-N-[(4S)-8-[6-amino-5-[(3,3-difluoro-2-oxo-1H-pyrrolo[2,3-b]pyridin-4-yl)sulfanyl]pyrazin-2-yl]-2-oxa-8-azaspiro[4.5]decan-4-yl]-2-methylpropane-2-sulfinamide Chemical compound CC(C)(C)[S@@](=O)N[C@@H]1COCC11CCN(CC1)c1cnc(Sc2ccnc3NC(=O)C(F)(F)c23)c(N)n1 UVNPEUJXKZFWSJ-LMTQTHQJSA-N 0.000 description 1
- 125000003088 (fluoren-9-ylmethoxy)carbonyl group Chemical group 0.000 description 1
- 108091032973 (ribonucleotides)n+m Proteins 0.000 description 1
- XFQPQSJDMJVOBN-UHFFFAOYSA-N 1-[4-amino-2-(ethylaminomethyl)imidazo[4,5-c]quinolin-1-yl]-2-methylpropan-2-ol;2,2,2-trifluoroacetic acid Chemical compound OC(=O)C(F)(F)F.OC(=O)C(F)(F)F.C1=CC=CC2=C(N(C(CNCC)=N3)CC(C)(C)O)C3=C(N)N=C21 XFQPQSJDMJVOBN-UHFFFAOYSA-N 0.000 description 1
- 125000004973 1-butenyl group Chemical group C(=CCC)* 0.000 description 1
- 125000004972 1-butynyl group Chemical group [H]C([H])([H])C([H])([H])C#C* 0.000 description 1
- IXPNQXFRVYWDDI-UHFFFAOYSA-N 1-methyl-2,4-dioxo-1,3-diazinane-5-carboximidamide Chemical compound CN1CC(C(N)=N)C(=O)NC1=O IXPNQXFRVYWDDI-UHFFFAOYSA-N 0.000 description 1
- 125000006023 1-pentenyl group Chemical group 0.000 description 1
- 238000001644 13C nuclear magnetic resonance spectroscopy Methods 0.000 description 1
- KJUGUADJHNHALS-UHFFFAOYSA-N 1H-tetrazole Chemical compound C=1N=NNN=1 KJUGUADJHNHALS-UHFFFAOYSA-N 0.000 description 1
- GQHTUMJGOHRCHB-UHFFFAOYSA-N 2,3,4,6,7,8,9,10-octahydropyrimido[1,2-a]azepine Chemical compound C1CCCCN2CCCN=C21 GQHTUMJGOHRCHB-UHFFFAOYSA-N 0.000 description 1
- 125000006069 2,3-dimethyl-2-butenyl group Chemical group 0.000 description 1
- MSWZFWKMSRAUBD-IVMDWMLBSA-N 2-amino-2-deoxy-D-glucopyranose Chemical compound N[C@H]1C(O)O[C@H](CO)[C@@H](O)[C@@H]1O MSWZFWKMSRAUBD-IVMDWMLBSA-N 0.000 description 1
- YSUIQYOGTINQIN-UZFYAQMZSA-N 2-amino-9-[(1S,6R,8R,9S,10R,15R,17R,18R)-8-(6-aminopurin-9-yl)-9,18-difluoro-3,12-dihydroxy-3,12-bis(sulfanylidene)-2,4,7,11,13,16-hexaoxa-3lambda5,12lambda5-diphosphatricyclo[13.2.1.06,10]octadecan-17-yl]-1H-purin-6-one Chemical compound NC1=NC2=C(N=CN2[C@@H]2O[C@@H]3COP(S)(=O)O[C@@H]4[C@@H](COP(S)(=O)O[C@@H]2[C@@H]3F)O[C@H]([C@H]4F)N2C=NC3=C2N=CN=C3N)C(=O)N1 YSUIQYOGTINQIN-UZFYAQMZSA-N 0.000 description 1
- 125000004974 2-butenyl group Chemical group C(C=CC)* 0.000 description 1
- 125000000069 2-butynyl group Chemical group [H]C([H])([H])C#CC([H])([H])* 0.000 description 1
- 125000006029 2-methyl-2-butenyl group Chemical group 0.000 description 1
- 125000006024 2-pentenyl group Chemical group 0.000 description 1
- ASCFNMCAHFUBCO-UHFFFAOYSA-N 2-phosphoglycolic acid Chemical compound OC(=O)COP(O)(O)=O ASCFNMCAHFUBCO-UHFFFAOYSA-N 0.000 description 1
- UNSAJINGUOTTRA-UHFFFAOYSA-N 3-(3-bromophenyl)prop-2-yn-1-ol Chemical compound OCC#CC1=CC=CC(Br)=C1 UNSAJINGUOTTRA-UHFFFAOYSA-N 0.000 description 1
- FTZIQBGFCYJWKA-UHFFFAOYSA-N 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium Chemical compound S1C(C)=C(C)N=C1[N+]1=NC(C=2C=CC=CC=2)=NN1C1=CC=CC=C1 FTZIQBGFCYJWKA-UHFFFAOYSA-N 0.000 description 1
- 125000006027 3-methyl-1-butenyl group Chemical group 0.000 description 1
- OSWFIVFLDKOXQC-UHFFFAOYSA-N 4-(3-methoxyphenyl)aniline Chemical compound COC1=CC=CC(C=2C=CC(N)=CC=2)=C1 OSWFIVFLDKOXQC-UHFFFAOYSA-N 0.000 description 1
- 229940090248 4-hydroxybenzoic acid Drugs 0.000 description 1
- 108010068327 4-hydroxyphenylpyruvate dioxygenase Proteins 0.000 description 1
- RVDLHGSZWAELAU-UHFFFAOYSA-N 5-tert-butylthiophene-2-carbonyl chloride Chemical compound CC(C)(C)C1=CC=C(C(Cl)=O)S1 RVDLHGSZWAELAU-UHFFFAOYSA-N 0.000 description 1
- HBAQYPYDRFILMT-UHFFFAOYSA-N 8-[3-(1-cyclopropylpyrazol-4-yl)-1H-pyrazolo[4,3-d]pyrimidin-5-yl]-3-methyl-3,8-diazabicyclo[3.2.1]octan-2-one Chemical class C1(CC1)N1N=CC(=C1)C1=NNC2=C1N=C(N=C2)N1C2C(N(CC1CC2)C)=O HBAQYPYDRFILMT-UHFFFAOYSA-N 0.000 description 1
- 241000224422 Acanthamoeba Species 0.000 description 1
- 241000238876 Acari Species 0.000 description 1
- QTBSBXVTEAMEQO-UHFFFAOYSA-M Acetate Chemical compound CC([O-])=O QTBSBXVTEAMEQO-UHFFFAOYSA-M 0.000 description 1
- 101000768957 Acholeplasma phage L2 Uncharacterized 37.2 kDa protein Proteins 0.000 description 1
- 101000823746 Acidianus ambivalens Uncharacterized 17.7 kDa protein in bps2 3'region Proteins 0.000 description 1
- 101000916369 Acidianus ambivalens Uncharacterized protein in sor 5'region Proteins 0.000 description 1
- 101000769342 Acinetobacter guillouiae Uncharacterized protein in rpoN-murA intergenic region Proteins 0.000 description 1
- 101000823696 Actinobacillus pleuropneumoniae Uncharacterized glycosyltransferase in aroQ 3'region Proteins 0.000 description 1
- 241000456624 Actinobacteria bacterium Species 0.000 description 1
- AXNVHPCVMSNXNP-GKTCLTPXSA-N Aescin Natural products O=C(O[C@H]1[C@@H](OC(=O)C)[C@]2(CO)[C@@H](O)C[C@@]3(C)[C@@]4(C)[C@@H]([C@]5(C)[C@H]([C@](CO)(C)[C@@H](O[C@@H]6[C@@H](O[C@H]7[C@@H](O)[C@@H](O)[C@H](O)[C@@H](CO)O7)[C@@H](O)[C@H](O[C@H]7[C@H](O)[C@@H](O)[C@H](O)[C@H](CO)O7)[C@@H](C(=O)O)O6)CC5)CC4)CC=C3[C@@H]2CC1(C)C)/C(=C/C)/C AXNVHPCVMSNXNP-GKTCLTPXSA-N 0.000 description 1
- 241000157282 Aesculus Species 0.000 description 1
- 241000157280 Aesculus hippocastanum Species 0.000 description 1
- 101000786513 Agrobacterium tumefaciens (strain 15955) Uncharacterized protein outside the virF region Proteins 0.000 description 1
- 208000000884 Airway Obstruction Diseases 0.000 description 1
- 101000618005 Alkalihalobacillus pseudofirmus (strain ATCC BAA-2126 / JCM 17055 / OF4) Uncharacterized protein BpOF4_00885 Proteins 0.000 description 1
- 206010027654 Allergic conditions Diseases 0.000 description 1
- GUBGYTABKSRVRQ-XLOQQCSPSA-N Alpha-Lactose Chemical compound O[C@@H]1[C@@H](O)[C@@H](O)[C@@H](CO)O[C@H]1O[C@@H]1[C@@H](CO)O[C@H](O)[C@H](O)[C@H]1O GUBGYTABKSRVRQ-XLOQQCSPSA-N 0.000 description 1
- 239000005995 Aluminium silicate Substances 0.000 description 1
- 206010001935 American trypanosomiasis Diseases 0.000 description 1
- 241001147657 Ancylostoma Species 0.000 description 1
- 241000498253 Ancylostoma duodenale Species 0.000 description 1
- 241000243791 Angiostrongylus Species 0.000 description 1
- 102100020724 Ankyrin repeat, SAM and basic leucine zipper domain-containing protein 1 Human genes 0.000 description 1
- 241000256186 Anopheles <genus> Species 0.000 description 1
- 101100162403 Arabidopsis thaliana ALEU gene Proteins 0.000 description 1
- 240000005528 Arctium lappa Species 0.000 description 1
- 241000244185 Ascaris lumbricoides Species 0.000 description 1
- 241000228212 Aspergillus Species 0.000 description 1
- 206010050245 Autoimmune thrombocytopenia Diseases 0.000 description 1
- 101000967489 Azorhizobium caulinodans (strain ATCC 43989 / DSM 5975 / JCM 20966 / LMG 6465 / NBRC 14845 / NCIMB 13405 / ORS 571) Uncharacterized protein AZC_3924 Proteins 0.000 description 1
- 102100035526 B melanoma antigen 1 Human genes 0.000 description 1
- 241000223836 Babesia Species 0.000 description 1
- 241000193738 Bacillus anthracis Species 0.000 description 1
- 101000823761 Bacillus licheniformis Uncharacterized 9.4 kDa protein in flaL 3'region Proteins 0.000 description 1
- 101000819719 Bacillus methanolicus Uncharacterized N-acetyltransferase in lysA 3'region Proteins 0.000 description 1
- 101000789586 Bacillus subtilis (strain 168) UPF0702 transmembrane protein YkjA Proteins 0.000 description 1
- 101000792624 Bacillus subtilis (strain 168) Uncharacterized protein YbxH Proteins 0.000 description 1
- 101000790792 Bacillus subtilis (strain 168) Uncharacterized protein YckC Proteins 0.000 description 1
- 101000819705 Bacillus subtilis (strain 168) Uncharacterized protein YlxR Proteins 0.000 description 1
- 101000948218 Bacillus subtilis (strain 168) Uncharacterized protein YtxJ Proteins 0.000 description 1
- 101000718627 Bacillus thuringiensis subsp. kurstaki Putative RNA polymerase sigma-G factor Proteins 0.000 description 1
- 108020000946 Bacterial DNA Proteins 0.000 description 1
- 208000035143 Bacterial infection Diseases 0.000 description 1
- 102100021663 Baculoviral IAP repeat-containing protein 5 Human genes 0.000 description 1
- 206010005003 Bladder cancer Diseases 0.000 description 1
- 241000335423 Blastomyces Species 0.000 description 1
- 101000641200 Bombyx mori densovirus Putative non-structural protein Proteins 0.000 description 1
- 241000588779 Bordetella bronchiseptica Species 0.000 description 1
- 241000588780 Bordetella parapertussis Species 0.000 description 1
- 241000588832 Bordetella pertussis Species 0.000 description 1
- 241000589978 Borrelia hermsii Species 0.000 description 1
- 241000495356 Borrelia microti Species 0.000 description 1
- 241000589972 Borrelia sp. Species 0.000 description 1
- 241001148604 Borreliella afzelii Species 0.000 description 1
- 241000142472 Borreliella andersonii Species 0.000 description 1
- 241000589969 Borreliella burgdorferi Species 0.000 description 1
- 241001148605 Borreliella garinii Species 0.000 description 1
- 241000589893 Brachyspira hyodysenteriae Species 0.000 description 1
- 206010006187 Breast cancer Diseases 0.000 description 1
- 208000026310 Breast neoplasm Diseases 0.000 description 1
- 206010006458 Bronchitis chronic Diseases 0.000 description 1
- 241000244038 Brugia malayi Species 0.000 description 1
- COVZYZSDYWQREU-UHFFFAOYSA-N Busulfan Chemical compound CS(=O)(=O)OCCCCOS(C)(=O)=O COVZYZSDYWQREU-UHFFFAOYSA-N 0.000 description 1
- 102100031092 C-C motif chemokine 3 Human genes 0.000 description 1
- 101710155856 C-C motif chemokine 3 Proteins 0.000 description 1
- 108010074051 C-Reactive Protein Proteins 0.000 description 1
- 102100032752 C-reactive protein Human genes 0.000 description 1
- MJVIFOFQNNJMRJ-UHFFFAOYSA-N CC(/C(/C)=[O]/C)=N Chemical compound CC(/C(/C)=[O]/C)=N MJVIFOFQNNJMRJ-UHFFFAOYSA-N 0.000 description 1
- KCBAMQOKOLXLOX-BSZYMOERSA-N CC1=C(SC=N1)C2=CC=C(C=C2)[C@H](C)NC(=O)[C@@H]3C[C@H](CN3C(=O)[C@H](C(C)(C)C)NC(=O)CCCCCCCCCCNCCCONC(=O)C4=C(C(=C(C=C4)F)F)NC5=C(C=C(C=C5)I)F)O Chemical compound CC1=C(SC=N1)C2=CC=C(C=C2)[C@H](C)NC(=O)[C@@H]3C[C@H](CN3C(=O)[C@H](C(C)(C)C)NC(=O)CCCCCCCCCCNCCCONC(=O)C4=C(C(=C(C=C4)F)F)NC5=C(C=C(C=C5)I)F)O KCBAMQOKOLXLOX-BSZYMOERSA-N 0.000 description 1
- 101100454807 Caenorhabditis elegans lgg-1 gene Proteins 0.000 description 1
- 101100314454 Caenorhabditis elegans tra-1 gene Proteins 0.000 description 1
- 244000197813 Camelina sativa Species 0.000 description 1
- 241000589876 Campylobacter Species 0.000 description 1
- 241000589877 Campylobacter coli Species 0.000 description 1
- 241000589875 Campylobacter jejuni Species 0.000 description 1
- 241000222173 Candida parapsilosis Species 0.000 description 1
- 241000222178 Candida tropicalis Species 0.000 description 1
- 229920002134 Carboxymethyl cellulose Polymers 0.000 description 1
- 108010078791 Carrier Proteins Proteins 0.000 description 1
- 102100035882 Catalase Human genes 0.000 description 1
- 108010053835 Catalase Proteins 0.000 description 1
- 206010008342 Cervix carcinoma Diseases 0.000 description 1
- 208000026368 Cestode infections Diseases 0.000 description 1
- 208000022636 Cestode infectious disease Diseases 0.000 description 1
- 108010055166 Chemokine CCL5 Proteins 0.000 description 1
- 241001647372 Chlamydia pneumoniae Species 0.000 description 1
- 241001647378 Chlamydia psittaci Species 0.000 description 1
- 241000606153 Chlamydia trachomatis Species 0.000 description 1
- VEXZGXHMUGYJMC-UHFFFAOYSA-M Chloride anion Chemical compound [Cl-] VEXZGXHMUGYJMC-UHFFFAOYSA-M 0.000 description 1
- 108010049048 Cholera Toxin Proteins 0.000 description 1
- 102000009016 Cholera Toxin Human genes 0.000 description 1
- 101000947633 Claviceps purpurea Uncharacterized 13.8 kDa protein Proteins 0.000 description 1
- 241001508813 Clavispora lusitaniae Species 0.000 description 1
- 241000193163 Clostridioides difficile Species 0.000 description 1
- 241000193155 Clostridium botulinum Species 0.000 description 1
- 241000193449 Clostridium tetani Species 0.000 description 1
- 241000223203 Coccidioides Species 0.000 description 1
- 206010010071 Coma Diseases 0.000 description 1
- 208000035473 Communicable disease Diseases 0.000 description 1
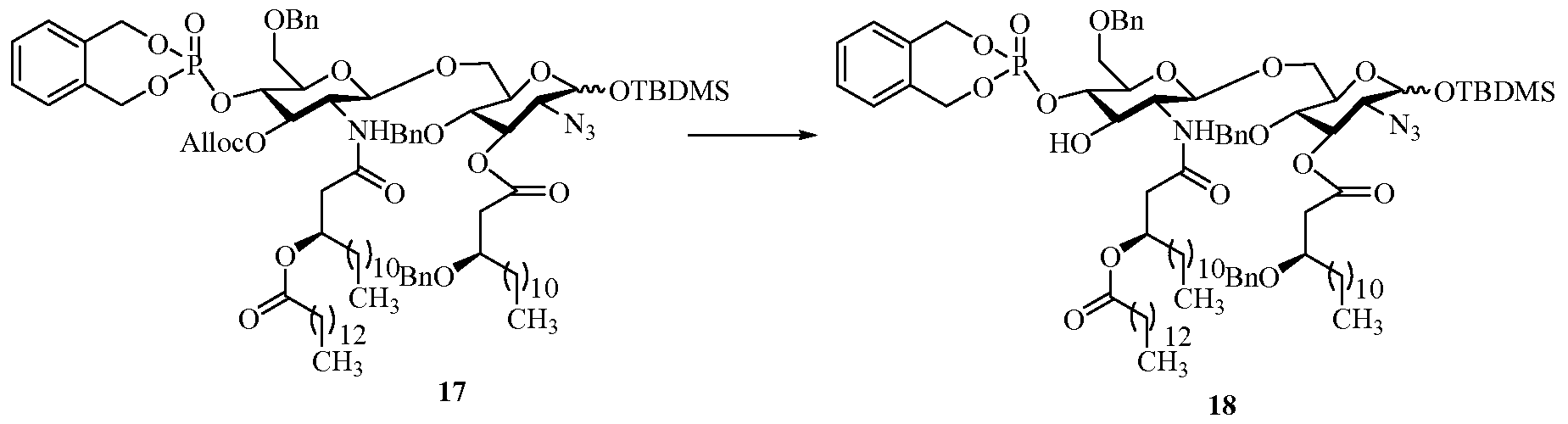
- 229940126657 Compound 17 Drugs 0.000 description 1
- 229940126639 Compound 33 Drugs 0.000 description 1
- 206010010305 Confusional state Diseases 0.000 description 1
- 206010010904 Convulsion Diseases 0.000 description 1
- RYGMFSIKBFXOCR-UHFFFAOYSA-N Copper Chemical compound [Cu] RYGMFSIKBFXOCR-UHFFFAOYSA-N 0.000 description 1
- 241000186216 Corynebacterium Species 0.000 description 1
- 241000186227 Corynebacterium diphtheriae Species 0.000 description 1
- 206010011224 Cough Diseases 0.000 description 1
- 208000011231 Crohn disease Diseases 0.000 description 1
- 241001337994 Cryptococcus <scale insect> Species 0.000 description 1
- 241000221204 Cryptococcus neoformans Species 0.000 description 1
- 241000223935 Cryptosporidium Species 0.000 description 1
- 229920000858 Cyclodextrin Polymers 0.000 description 1
- FBPFZTCFMRRESA-KVTDHHQDSA-N D-Mannitol Chemical compound OC[C@@H](O)[C@@H](O)[C@H](O)[C@H](O)CO FBPFZTCFMRRESA-KVTDHHQDSA-N 0.000 description 1
- 101710088194 Dehydrogenase Proteins 0.000 description 1
- 102100031262 Deleted in malignant brain tumors 1 protein Human genes 0.000 description 1
- 241000725619 Dengue virus Species 0.000 description 1
- 102000007577 Desmoglein 3 Human genes 0.000 description 1
- 108010032035 Desmoglein 3 Proteins 0.000 description 1
- 238000009007 Diagnostic Kit Methods 0.000 description 1
- 206010012735 Diarrhoea Diseases 0.000 description 1
- 240000001879 Digitalis lutea Species 0.000 description 1
- QRLVDLBMBULFAL-UHFFFAOYSA-N Digitonin Natural products CC1CCC2(OC1)OC3C(O)C4C5CCC6CC(OC7OC(CO)C(OC8OC(CO)C(O)C(OC9OCC(O)C(O)C9OC%10OC(CO)C(O)C(OC%11OC(CO)C(O)C(O)C%11O)C%10O)C8O)C(O)C7O)C(O)CC6(C)C5CCC4(C)C3C2C QRLVDLBMBULFAL-UHFFFAOYSA-N 0.000 description 1
- 108010053187 Diphtheria Toxin Proteins 0.000 description 1
- 102000016607 Diphtheria Toxin Human genes 0.000 description 1
- 241000255925 Diptera Species 0.000 description 1
- SNRUBQQJIBEYMU-UHFFFAOYSA-N Dodecane Natural products CCCCCCCCCCCC SNRUBQQJIBEYMU-UHFFFAOYSA-N 0.000 description 1
- 206010059866 Drug resistance Diseases 0.000 description 1
- 241000605314 Ehrlichia Species 0.000 description 1
- 206010014561 Emphysema Diseases 0.000 description 1
- 241000224431 Entamoeba Species 0.000 description 1
- 241000146407 Entamoeba coli Species 0.000 description 1
- 241000204733 Entamoeba dispar Species 0.000 description 1
- 241001133638 Entamoeba equi Species 0.000 description 1
- 241000146401 Entamoeba hartmanni Species 0.000 description 1
- 241000146402 Entamoeba polecki Species 0.000 description 1
- 241000305071 Enterobacterales Species 0.000 description 1
- 101000948901 Enterobacteria phage T4 Uncharacterized 16.0 kDa protein in segB-ipI intergenic region Proteins 0.000 description 1
- 241000498255 Enterobius vermicularis Species 0.000 description 1
- 241000194033 Enterococcus Species 0.000 description 1
- 241000194032 Enterococcus faecalis Species 0.000 description 1
- 241000194031 Enterococcus faecium Species 0.000 description 1
- 241000991587 Enterovirus C Species 0.000 description 1
- 101000805958 Equine herpesvirus 4 (strain 1942) Virion protein US10 homolog Proteins 0.000 description 1
- 241000588722 Escherichia Species 0.000 description 1
- 101000790442 Escherichia coli Insertion element IS2 uncharacterized 11.1 kDa protein Proteins 0.000 description 1
- 101000788354 Escherichia phage P2 Uncharacterized 8.2 kDa protein in gpA 5'region Proteins 0.000 description 1
- 239000001856 Ethyl cellulose Substances 0.000 description 1
- ZZSNKZQZMQGXPY-UHFFFAOYSA-N Ethyl cellulose Chemical compound CCOCC1OC(OC)C(OCC)C(OCC)C1OC1C(O)C(O)C(OC)C(CO)O1 ZZSNKZQZMQGXPY-UHFFFAOYSA-N 0.000 description 1
- 241000204939 Fasciola gigantica Species 0.000 description 1
- 241000242711 Fasciola hepatica Species 0.000 description 1
- 241000282326 Felis catus Species 0.000 description 1
- 101710154643 Filamentous hemagglutinin Proteins 0.000 description 1
- 108010040721 Flagellin Proteins 0.000 description 1
- 241000710831 Flavivirus Species 0.000 description 1
- BDAGIHXWWSANSR-UHFFFAOYSA-M Formate Chemical compound [O-]C=O BDAGIHXWWSANSR-UHFFFAOYSA-M 0.000 description 1
- 101000770304 Frankia alni UPF0460 protein in nifX-nifW intergenic region Proteins 0.000 description 1
- 108091006027 G proteins Proteins 0.000 description 1
- 102000030782 GTP binding Human genes 0.000 description 1
- 108091000058 GTP-Binding Proteins 0.000 description 1
- 101000797344 Geobacillus stearothermophilus Putative tRNA (cytidine(34)-2'-O)-methyltransferase Proteins 0.000 description 1
- 101000748410 Geobacillus stearothermophilus Uncharacterized protein in fumA 3'region Proteins 0.000 description 1
- 241000224467 Giardia intestinalis Species 0.000 description 1
- 229920001503 Glucan Polymers 0.000 description 1
- 102100041003 Glutamate carboxypeptidase 2 Human genes 0.000 description 1
- 108010024636 Glutathione Proteins 0.000 description 1
- 229930186217 Glycolipid Natural products 0.000 description 1
- 102000003886 Glycoproteins Human genes 0.000 description 1
- 108090000288 Glycoproteins Proteins 0.000 description 1
- 229920002683 Glycosaminoglycan Polymers 0.000 description 1
- NMJREATYWWNIKX-UHFFFAOYSA-N GnRH Chemical compound C1CCC(C(=O)NCC(N)=O)N1C(=O)C(CC(C)C)NC(=O)C(CC=1C2=CC=CC=C2NC=1)NC(=O)CNC(=O)C(NC(=O)C(CO)NC(=O)C(CC=1C2=CC=CC=C2NC=1)NC(=O)C(CC=1NC=NC=1)NC(=O)C1NC(=O)CC1)CC1=CC=C(O)C=C1 NMJREATYWWNIKX-UHFFFAOYSA-N 0.000 description 1
- 241001316290 Gypsophila Species 0.000 description 1
- 229940033330 HIV vaccine Drugs 0.000 description 1
- 241000606790 Haemophilus Species 0.000 description 1
- 101000772675 Haemophilus influenzae (strain ATCC 51907 / DSM 11121 / KW20 / Rd) UPF0438 protein HI_0847 Proteins 0.000 description 1
- 101000631019 Haemophilus influenzae (strain ATCC 51907 / DSM 11121 / KW20 / Rd) Uncharacterized protein HI_0350 Proteins 0.000 description 1
- 101100406392 Haemophilus influenzae (strain ATCC 51907 / DSM 11121 / KW20 / Rd) omp26 gene Proteins 0.000 description 1
- 101000768938 Haemophilus phage HP1 (strain HP1c1) Uncharacterized 8.9 kDa protein in int-C1 intergenic region Proteins 0.000 description 1
- 208000001204 Hashimoto Disease Diseases 0.000 description 1
- 208000030836 Hashimoto thyroiditis Diseases 0.000 description 1
- 206010019233 Headaches Diseases 0.000 description 1
- 241000589989 Helicobacter Species 0.000 description 1
- 108010034145 Helminth Proteins Proteins 0.000 description 1
- 208000035186 Hemolytic Autoimmune Anemia Diseases 0.000 description 1
- 208000032843 Hemorrhage Diseases 0.000 description 1
- 241000711549 Hepacivirus C Species 0.000 description 1
- 229940124872 Hepatitis B virus vaccine Drugs 0.000 description 1
- 208000005176 Hepatitis C Diseases 0.000 description 1
- 241000724675 Hepatitis E virus Species 0.000 description 1
- 241000709721 Hepatovirus A Species 0.000 description 1
- 241000282412 Homo Species 0.000 description 1
- 101000785414 Homo sapiens Ankyrin repeat, SAM and basic leucine zipper domain-containing protein 1 Proteins 0.000 description 1
- 101000874316 Homo sapiens B melanoma antigen 1 Proteins 0.000 description 1
- 101000797762 Homo sapiens C-C motif chemokine 5 Proteins 0.000 description 1
- 101000844721 Homo sapiens Deleted in malignant brain tumors 1 protein Proteins 0.000 description 1
- 101000892862 Homo sapiens Glutamate carboxypeptidase 2 Proteins 0.000 description 1
- 101000628547 Homo sapiens Metalloreductase STEAP1 Proteins 0.000 description 1
- 101000946889 Homo sapiens Monocyte differentiation antigen CD14 Proteins 0.000 description 1
- 101000874141 Homo sapiens Probable ATP-dependent RNA helicase DDX43 Proteins 0.000 description 1
- 101001136592 Homo sapiens Prostate stem cell antigen Proteins 0.000 description 1
- 101001130441 Homo sapiens Ras-related protein Rap-2a Proteins 0.000 description 1
- 101000831496 Homo sapiens Toll-like receptor 3 Proteins 0.000 description 1
- 101000669460 Homo sapiens Toll-like receptor 5 Proteins 0.000 description 1
- 101000669402 Homo sapiens Toll-like receptor 7 Proteins 0.000 description 1
- 241000700588 Human alphaherpesvirus 1 Species 0.000 description 1
- 241000701074 Human alphaherpesvirus 2 Species 0.000 description 1
- 206010071038 Human anaplasmosis Diseases 0.000 description 1
- 241000713340 Human immunodeficiency virus 2 Species 0.000 description 1
- 241000341655 Human papillomavirus type 16 Species 0.000 description 1
- 206010022004 Influenza like illness Diseases 0.000 description 1
- 102000000589 Interleukin-1 Human genes 0.000 description 1
- 108010002352 Interleukin-1 Proteins 0.000 description 1
- 102000003814 Interleukin-10 Human genes 0.000 description 1
- 108090000174 Interleukin-10 Proteins 0.000 description 1
- 102000003816 Interleukin-13 Human genes 0.000 description 1
- 108090000176 Interleukin-13 Proteins 0.000 description 1
- 102000049772 Interleukin-16 Human genes 0.000 description 1
- 101800003050 Interleukin-16 Proteins 0.000 description 1
- 102000003810 Interleukin-18 Human genes 0.000 description 1
- 108090000171 Interleukin-18 Proteins 0.000 description 1
- 102000013264 Interleukin-23 Human genes 0.000 description 1
- 108010065637 Interleukin-23 Proteins 0.000 description 1
- 108010002386 Interleukin-3 Proteins 0.000 description 1
- 102000000646 Interleukin-3 Human genes 0.000 description 1
- 102000004388 Interleukin-4 Human genes 0.000 description 1
- 108090000978 Interleukin-4 Proteins 0.000 description 1
- 108090001005 Interleukin-6 Proteins 0.000 description 1
- 102000004889 Interleukin-6 Human genes 0.000 description 1
- 108010002586 Interleukin-7 Proteins 0.000 description 1
- 102000000704 Interleukin-7 Human genes 0.000 description 1
- 108090001007 Interleukin-8 Proteins 0.000 description 1
- 102000004890 Interleukin-8 Human genes 0.000 description 1
- 206010022998 Irritability Diseases 0.000 description 1
- 241000710842 Japanese encephalitis virus Species 0.000 description 1
- 206010023126 Jaundice Diseases 0.000 description 1
- 101000782488 Junonia coenia densovirus (isolate pBRJ/1990) Putative non-structural protein NS2 Proteins 0.000 description 1
- 102100034872 Kallikrein-4 Human genes 0.000 description 1
- 239000005909 Kieselgur Substances 0.000 description 1
- 101000811523 Klebsiella pneumoniae Uncharacterized 55.8 kDa protein in cps region Proteins 0.000 description 1
- CKLJMWTZIZZHCS-REOHCLBHSA-N L-aspartic acid Chemical compound OC(=O)[C@@H](N)CC(O)=O CKLJMWTZIZZHCS-REOHCLBHSA-N 0.000 description 1
- 101000818409 Lactococcus lactis subsp. lactis Uncharacterized HTH-type transcriptional regulator in lacX 3'region Proteins 0.000 description 1
- GUBGYTABKSRVRQ-QKKXKWKRSA-N Lactose Natural products OC[C@H]1O[C@@H](O[C@H]2[C@H](O)[C@@H](O)C(O)O[C@@H]2CO)[C@H](O)[C@@H](O)[C@H]1O GUBGYTABKSRVRQ-QKKXKWKRSA-N 0.000 description 1
- 239000005639 Lauric acid Substances 0.000 description 1
- 241000589248 Legionella Species 0.000 description 1
- 241000589242 Legionella pneumophila Species 0.000 description 1
- 208000007764 Legionnaires' Disease Diseases 0.000 description 1
- 206010057168 Leishmania infections Diseases 0.000 description 1
- 101000878851 Leptolyngbya boryana Putative Fe(2+) transport protein A Proteins 0.000 description 1
- 241000589902 Leptospira Species 0.000 description 1
- 241000589929 Leptospira interrogans Species 0.000 description 1
- 241000186781 Listeria Species 0.000 description 1
- 241000186779 Listeria monocytogenes Species 0.000 description 1
- 206010058467 Lung neoplasm malignant Diseases 0.000 description 1
- 229930195725 Mannitol Natural products 0.000 description 1
- 241000712079 Measles morbillivirus Species 0.000 description 1
- 102100026712 Metalloreductase STEAP1 Human genes 0.000 description 1
- 101000758828 Methanosarcina barkeri (strain Fusaro / DSM 804) Uncharacterized protein Mbar_A1602 Proteins 0.000 description 1
- 101001122401 Middle East respiratory syndrome-related coronavirus (isolate United Kingdom/H123990006/2012) Non-structural protein ORF3 Proteins 0.000 description 1
- 102100035877 Monocyte differentiation antigen CD14 Human genes 0.000 description 1
- 241000588621 Moraxella Species 0.000 description 1
- 241000588655 Moraxella catarrhalis Species 0.000 description 1
- 241000711386 Mumps virus Species 0.000 description 1
- 101100369076 Mus musculus Tdgf1 gene Proteins 0.000 description 1
- 241000501454 Mutillidae Species 0.000 description 1
- 208000000112 Myalgia Diseases 0.000 description 1
- 241000186367 Mycobacterium avium Species 0.000 description 1
- 241000187482 Mycobacterium avium subsp. paratuberculosis Species 0.000 description 1
- 241000187480 Mycobacterium smegmatis Species 0.000 description 1
- 241000694696 Mycobacterium tuberculosis CAS Species 0.000 description 1
- 101001055788 Mycolicibacterium smegmatis (strain ATCC 700084 / mc(2)155) Pentapeptide repeat protein MfpA Proteins 0.000 description 1
- OPFJDXRVMFKJJO-ZHHKINOHSA-N N-{[3-(2-benzamido-4-methyl-1,3-thiazol-5-yl)-pyrazol-5-yl]carbonyl}-G-dR-G-dD-dD-dD-NH2 Chemical compound S1C(C=2NN=C(C=2)C(=O)NCC(=O)N[C@H](CCCN=C(N)N)C(=O)NCC(=O)N[C@H](CC(O)=O)C(=O)N[C@H](CC(O)=O)C(=O)N[C@H](CC(O)=O)C(N)=O)=C(C)N=C1NC(=O)C1=CC=CC=C1 OPFJDXRVMFKJJO-ZHHKINOHSA-N 0.000 description 1
- 238000005481 NMR spectroscopy Methods 0.000 description 1
- 241001644525 Nastus productus Species 0.000 description 1
- 206010028813 Nausea Diseases 0.000 description 1
- 241000498270 Necator americanus Species 0.000 description 1
- 241000588652 Neisseria gonorrhoeae Species 0.000 description 1
- 241000588650 Neisseria meningitidis Species 0.000 description 1
- 208000000291 Nematode infections Diseases 0.000 description 1
- GRYLNZFGIOXLOG-UHFFFAOYSA-N Nitric acid Chemical class O[N+]([O-])=O GRYLNZFGIOXLOG-UHFFFAOYSA-N 0.000 description 1
- YPDGOXYUXQDPDJ-UHFFFAOYSA-N O=C(C1OC2)C1OCc1c2cccc1 Chemical compound O=C(C1OC2)C1OCc1c2cccc1 YPDGOXYUXQDPDJ-UHFFFAOYSA-N 0.000 description 1
- HCUVEUVIUAJXRB-UHFFFAOYSA-N OC1=C(C=C(CNC(CCCC=2SC=CC=2)=O)C=C1)OC Chemical compound OC1=C(C=C(CNC(CCCC=2SC=CC=2)=O)C=C1)OC HCUVEUVIUAJXRB-UHFFFAOYSA-N 0.000 description 1
- 241000243985 Onchocerca volvulus Species 0.000 description 1
- 101000740670 Orgyia pseudotsugata multicapsid polyhedrosis virus Protein C42 Proteins 0.000 description 1
- 101710116435 Outer membrane protein Proteins 0.000 description 1
- 108060006580 PRAME Proteins 0.000 description 1
- 102000036673 PRAME Human genes 0.000 description 1
- 208000002193 Pain Diseases 0.000 description 1
- 241001480233 Paragonimus Species 0.000 description 1
- 208000002606 Paramyxoviridae Infections Diseases 0.000 description 1
- 208000030852 Parasitic disease Diseases 0.000 description 1
- 101150111072 Pars2 gene Proteins 0.000 description 1
- 206010034133 Pathogen resistance Diseases 0.000 description 1
- 235000019483 Peanut oil Nutrition 0.000 description 1
- 108091005804 Peptidases Proteins 0.000 description 1
- 208000031845 Pernicious anaemia Diseases 0.000 description 1
- 108010081690 Pertussis Toxin Proteins 0.000 description 1
- 239000004264 Petrolatum Substances 0.000 description 1
- 241000255129 Phlebotominae Species 0.000 description 1
- 101000769182 Photorhabdus luminescens Uncharacterized protein in pnp 3'region Proteins 0.000 description 1
- 101710099976 Photosystem I P700 chlorophyll a apoprotein A1 Proteins 0.000 description 1
- 235000014676 Phragmites communis Nutrition 0.000 description 1
- 241000235645 Pichia kudriavzevii Species 0.000 description 1
- 101000983333 Plasmodium falciparum (isolate NF54) 25 kDa ookinete surface antigen Proteins 0.000 description 1
- 206010035500 Plasmodium falciparum infection Diseases 0.000 description 1
- 241000223821 Plasmodium malariae Species 0.000 description 1
- 206010035501 Plasmodium malariae infection Diseases 0.000 description 1
- 241001505293 Plasmodium ovale Species 0.000 description 1
- 206010035502 Plasmodium ovale infection Diseases 0.000 description 1
- 241000233872 Pneumocystis carinii Species 0.000 description 1
- 101710183389 Pneumolysin Proteins 0.000 description 1
- 239000002202 Polyethylene glycol Substances 0.000 description 1
- 102100035724 Probable ATP-dependent RNA helicase DDX43 Human genes 0.000 description 1
- 102100036735 Prostate stem cell antigen Human genes 0.000 description 1
- 239000004365 Protease Substances 0.000 description 1
- 102000016611 Proteoglycans Human genes 0.000 description 1
- 108010067787 Proteoglycans Proteins 0.000 description 1
- 108010010974 Proteolipids Proteins 0.000 description 1
- 102000016202 Proteolipids Human genes 0.000 description 1
- 101000961392 Pseudescherichia vulneris Uncharacterized 29.9 kDa protein in crtE 3'region Proteins 0.000 description 1
- 241000589516 Pseudomonas Species 0.000 description 1
- 101000731030 Pseudomonas oleovorans Poly(3-hydroxyalkanoate) polymerase 2 Proteins 0.000 description 1
- 101001065485 Pseudomonas putida Probable fatty acid methyltransferase Proteins 0.000 description 1
- 101710201576 Putative membrane protein Proteins 0.000 description 1
- 206010037660 Pyrexia Diseases 0.000 description 1
- 241001092473 Quillaja Species 0.000 description 1
- 241001454523 Quillaja saponaria Species 0.000 description 1
- 102100022851 Rab5 GDP/GTP exchange factor Human genes 0.000 description 1
- 102100031420 Ras-related protein Rap-2a Human genes 0.000 description 1
- 102000007056 Recombinant Fusion Proteins Human genes 0.000 description 1
- 108010008281 Recombinant Fusion Proteins Proteins 0.000 description 1
- 208000001647 Renal Insufficiency Diseases 0.000 description 1
- 101710203837 Replication-associated protein Proteins 0.000 description 1
- 102100037486 Reverse transcriptase/ribonuclease H Human genes 0.000 description 1
- 101000711023 Rhizobium leguminosarum bv. trifolii Uncharacterized protein in tfuA 3'region Proteins 0.000 description 1
- 101000948156 Rhodococcus erythropolis Uncharacterized 47.3 kDa protein in thcA 5'region Proteins 0.000 description 1
- 101000917565 Rhodococcus fascians Uncharacterized 33.6 kDa protein in fasciation locus Proteins 0.000 description 1
- 235000019774 Rice Bran oil Nutrition 0.000 description 1
- 241000606701 Rickettsia Species 0.000 description 1
- 241000606695 Rickettsia rickettsii Species 0.000 description 1
- 241000702670 Rotavirus Species 0.000 description 1
- 101000999689 Saimiriine herpesvirus 2 (strain 11) Transcriptional regulator ICP22 homolog Proteins 0.000 description 1
- 101000790284 Saimiriine herpesvirus 2 (strain 488) Uncharacterized 9.5 kDa protein in DHFR 3'region Proteins 0.000 description 1
- 241001138501 Salmonella enterica Species 0.000 description 1
- 241001354013 Salmonella enterica subsp. enterica serovar Enteritidis Species 0.000 description 1
- 241000531795 Salmonella enterica subsp. enterica serovar Paratyphi A Species 0.000 description 1
- 241000293871 Salmonella enterica subsp. enterica serovar Typhi Species 0.000 description 1
- 241000607149 Salmonella sp. Species 0.000 description 1
- 241000219287 Saponaria Species 0.000 description 1
- 241000242680 Schistosoma mansoni Species 0.000 description 1
- 241001520868 Schistosoma mekongi Species 0.000 description 1
- 206010039710 Scleroderma Diseases 0.000 description 1
- 208000034189 Sclerosis Diseases 0.000 description 1
- 108010071390 Serum Albumin Proteins 0.000 description 1
- 102000007562 Serum Albumin Human genes 0.000 description 1
- 241000607768 Shigella Species 0.000 description 1
- 241000607764 Shigella dysenteriae Species 0.000 description 1
- 241000607760 Shigella sonnei Species 0.000 description 1
- 241000700584 Simplexvirus Species 0.000 description 1
- PNUZDKCDAWUEGK-CYZMBNFOSA-N Sitafloxacin Chemical compound C([C@H]1N)N(C=2C(=C3C(C(C(C(O)=O)=CN3[C@H]3[C@H](C3)F)=O)=CC=2F)Cl)CC11CC1 PNUZDKCDAWUEGK-CYZMBNFOSA-N 0.000 description 1
- DWAQJAXMDSEUJJ-UHFFFAOYSA-M Sodium bisulfite Chemical compound [Na+].OS([O-])=O DWAQJAXMDSEUJJ-UHFFFAOYSA-M 0.000 description 1
- 101000857870 Squalus acanthias Gonadoliberin Proteins 0.000 description 1
- 241000191940 Staphylococcus Species 0.000 description 1
- 241000191963 Staphylococcus epidermidis Species 0.000 description 1
- 229930182558 Sterol Natural products 0.000 description 1
- 241000194017 Streptococcus Species 0.000 description 1
- 241000193985 Streptococcus agalactiae Species 0.000 description 1
- 101000936719 Streptococcus gordonii Accessory Sec system protein Asp3 Proteins 0.000 description 1
- 241000194019 Streptococcus mutans Species 0.000 description 1
- 241000193996 Streptococcus pyogenes Species 0.000 description 1
- 108010011834 Streptolysins Proteins 0.000 description 1
- 101000788499 Streptomyces coelicolor Uncharacterized oxidoreductase in mprA 5'region Proteins 0.000 description 1
- 101001102841 Streptomyces griseus Purine nucleoside phosphorylase ORF3 Proteins 0.000 description 1
- 101000708557 Streptomyces lincolnensis Uncharacterized 17.2 kDa protein in melC2-rnhH intergenic region Proteins 0.000 description 1
- 241000244177 Strongyloides stercoralis Species 0.000 description 1
- QAOWNCQODCNURD-UHFFFAOYSA-L Sulfate Chemical compound [O-]S([O-])(=O)=O QAOWNCQODCNURD-UHFFFAOYSA-L 0.000 description 1
- LSNNMFCWUKXFEE-UHFFFAOYSA-N Sulfurous acid Chemical compound OS(O)=O LSNNMFCWUKXFEE-UHFFFAOYSA-N 0.000 description 1
- 101710137302 Surface antigen S Proteins 0.000 description 1
- 108010002687 Survivin Proteins 0.000 description 1
- 230000024932 T cell mediated immunity Effects 0.000 description 1
- 108091008874 T cell receptors Proteins 0.000 description 1
- 102000016266 T-Cell Antigen Receptors Human genes 0.000 description 1
- 101150057833 THEG gene Proteins 0.000 description 1
- 229940124614 TLR 8 agonist Drugs 0.000 description 1
- 108700012920 TNF Proteins 0.000 description 1
- 241000244159 Taenia saginata Species 0.000 description 1
- 241000244157 Taenia solium Species 0.000 description 1
- 206010043376 Tetanus Diseases 0.000 description 1
- 108010055044 Tetanus Toxin Proteins 0.000 description 1
- 101000649826 Thermotoga neapolitana Putative anti-sigma factor antagonist TM1081 homolog Proteins 0.000 description 1
- 208000031981 Thrombocytopenic Idiopathic Purpura Diseases 0.000 description 1
- 102000009843 Thyroglobulin Human genes 0.000 description 1
- 108010034949 Thyroglobulin Proteins 0.000 description 1
- 208000024799 Thyroid disease Diseases 0.000 description 1
- 241000710771 Tick-borne encephalitis virus Species 0.000 description 1
- 102100024324 Toll-like receptor 3 Human genes 0.000 description 1
- 102100039357 Toll-like receptor 5 Human genes 0.000 description 1
- 102100039390 Toll-like receptor 7 Human genes 0.000 description 1
- QMGSCYSTMWRURP-UHFFFAOYSA-N Tomatine Natural products CC1CCC2(NC1)OC3CC4C5CCC6CC(CCC6(C)C5CCC4(C)C3C2C)OC7OC(CO)C(OC8OC(CO)C(O)C(OC9OCC(O)C(O)C9OC%10OC(CO)C(O)C(O)C%10O)C8O)C(O)C7O QMGSCYSTMWRURP-UHFFFAOYSA-N 0.000 description 1
- 241000223996 Toxoplasma Species 0.000 description 1
- 241000223997 Toxoplasma gondii Species 0.000 description 1
- 101710134694 Transcriptional regulator ICP22 homolog Proteins 0.000 description 1
- 102000010912 Transferrin-Binding Proteins Human genes 0.000 description 1
- 108010062476 Transferrin-Binding Proteins Proteins 0.000 description 1
- 241000242541 Trematoda Species 0.000 description 1
- 208000004938 Trematode Infections Diseases 0.000 description 1
- 241000589886 Treponema Species 0.000 description 1
- 241000589892 Treponema denticola Species 0.000 description 1
- 241000589884 Treponema pallidum Species 0.000 description 1
- 241000243777 Trichinella spiralis Species 0.000 description 1
- DRUIESSIVFYOMK-UHFFFAOYSA-N Trichloroacetonitrile Chemical compound ClC(Cl)(Cl)C#N DRUIESSIVFYOMK-UHFFFAOYSA-N 0.000 description 1
- 241000224526 Trichomonas Species 0.000 description 1
- 241001489151 Trichuris Species 0.000 description 1
- 235000021307 Triticum Nutrition 0.000 description 1
- 244000098338 Triticum aestivum Species 0.000 description 1
- 241000223104 Trypanosoma Species 0.000 description 1
- 241000223109 Trypanosoma cruzi Species 0.000 description 1
- 102000003425 Tyrosinase Human genes 0.000 description 1
- 108060008724 Tyrosinase Proteins 0.000 description 1
- 108010046334 Urease Proteins 0.000 description 1
- 208000006105 Uterine Cervical Neoplasms Diseases 0.000 description 1
- 241000251539 Vertebrata <Metazoa> Species 0.000 description 1
- 241000607598 Vibrio Species 0.000 description 1
- 101000827562 Vibrio alginolyticus Uncharacterized protein in proC 3'region Proteins 0.000 description 1
- 241000607626 Vibrio cholerae Species 0.000 description 1
- 101000778915 Vibrio parahaemolyticus serotype O3:K6 (strain RIMD 2210633) Uncharacterized membrane protein VP2115 Proteins 0.000 description 1
- 229930003427 Vitamin E Natural products 0.000 description 1
- 206010047700 Vomiting Diseases 0.000 description 1
- 241000710772 Yellow fever virus Species 0.000 description 1
- 241000607734 Yersinia <bacteria> Species 0.000 description 1
- 241000607447 Yersinia enterocolitica Species 0.000 description 1
- 241000607479 Yersinia pestis Species 0.000 description 1
- 241000607477 Yersinia pseudotuberculosis Species 0.000 description 1
- 241000606834 [Haemophilus] ducreyi Species 0.000 description 1
- WREOTYWODABZMH-DTZQCDIJSA-N [[(2r,3s,4r,5r)-3,4-dihydroxy-5-[2-oxo-4-(2-phenylethoxyamino)pyrimidin-1-yl]oxolan-2-yl]methoxy-hydroxyphosphoryl] phosphono hydrogen phosphate Chemical compound O[C@@H]1[C@H](O)[C@@H](COP(O)(=O)OP(O)(=O)OP(O)(O)=O)O[C@H]1N(C=C\1)C(=O)NC/1=N\OCCC1=CC=CC=C1 WREOTYWODABZMH-DTZQCDIJSA-N 0.000 description 1
- 230000002159 abnormal effect Effects 0.000 description 1
- 150000001241 acetals Chemical class 0.000 description 1
- 150000001242 acetic acid derivatives Chemical class 0.000 description 1
- DPXJVFZANSGRMM-UHFFFAOYSA-N acetic acid;2,3,4,5,6-pentahydroxyhexanal;sodium Chemical compound [Na].CC(O)=O.OCC(O)C(O)C(O)C(O)C=O DPXJVFZANSGRMM-UHFFFAOYSA-N 0.000 description 1
- 230000002378 acidificating effect Effects 0.000 description 1
- 150000007513 acids Chemical class 0.000 description 1
- 239000012190 activator Substances 0.000 description 1
- 239000004480 active ingredient Substances 0.000 description 1
- 239000008186 active pharmaceutical agent Substances 0.000 description 1
- 239000013543 active substance Substances 0.000 description 1
- 230000006978 adaptation Effects 0.000 description 1
- 102000030621 adenylate cyclase Human genes 0.000 description 1
- 108060000200 adenylate cyclase Proteins 0.000 description 1
- 230000000240 adjuvant effect Effects 0.000 description 1
- 230000002411 adverse Effects 0.000 description 1
- 230000008484 agonism Effects 0.000 description 1
- 150000001338 aliphatic hydrocarbons Chemical class 0.000 description 1
- 229930013930 alkaloid Natural products 0.000 description 1
- 230000000172 allergic effect Effects 0.000 description 1
- AZDRQVAHHNSJOQ-UHFFFAOYSA-N alumane Chemical class [AlH3] AZDRQVAHHNSJOQ-UHFFFAOYSA-N 0.000 description 1
- WNROFYMDJYEPJX-UHFFFAOYSA-K aluminium hydroxide Chemical compound [OH-].[OH-].[OH-].[Al+3] WNROFYMDJYEPJX-UHFFFAOYSA-K 0.000 description 1
- 229910021502 aluminium hydroxide Inorganic materials 0.000 description 1
- 235000012211 aluminium silicate Nutrition 0.000 description 1
- 125000003277 amino group Chemical group 0.000 description 1
- 208000007502 anemia Diseases 0.000 description 1
- 239000010775 animal oil Substances 0.000 description 1
- 208000025009 anogenital human papillomavirus infection Diseases 0.000 description 1
- 201000004201 anogenital venereal wart Diseases 0.000 description 1
- 239000003242 anti bacterial agent Substances 0.000 description 1
- 230000001093 anti-cancer Effects 0.000 description 1
- 230000036436 anti-hiv Effects 0.000 description 1
- 230000001355 anti-mycobacterial effect Effects 0.000 description 1
- 230000000798 anti-retroviral effect Effects 0.000 description 1
- 208000037908 antibody-mediated disorder Diseases 0.000 description 1
- 210000000612 antigen-presenting cell Anatomy 0.000 description 1
- 230000008350 antigen-specific antibody response Effects 0.000 description 1
- 230000003078 antioxidant effect Effects 0.000 description 1
- 239000013011 aqueous formulation Substances 0.000 description 1
- 239000012736 aqueous medium Substances 0.000 description 1
- 239000007900 aqueous suspension Substances 0.000 description 1
- 229940009098 aspartate Drugs 0.000 description 1
- 208000010668 atopic eczema Diseases 0.000 description 1
- 201000000448 autoimmune hemolytic anemia Diseases 0.000 description 1
- 230000006472 autoimmune response Effects 0.000 description 1
- 150000001540 azides Chemical class 0.000 description 1
- 210000002769 b effector cell Anatomy 0.000 description 1
- 201000008680 babesiosis Diseases 0.000 description 1
- 208000022362 bacterial infectious disease Diseases 0.000 description 1
- 239000011324 bead Substances 0.000 description 1
- 235000013871 bee wax Nutrition 0.000 description 1
- 239000012166 beeswax Substances 0.000 description 1
- 229940092738 beeswax Drugs 0.000 description 1
- 230000009286 beneficial effect Effects 0.000 description 1
- 150000008107 benzenesulfonic acids Chemical class 0.000 description 1
- 150000001558 benzoic acid derivatives Chemical class 0.000 description 1
- WPYMKLBDIGXBTP-UHFFFAOYSA-N benzoic acid group Chemical group C(C1=CC=CC=C1)(=O)O WPYMKLBDIGXBTP-UHFFFAOYSA-N 0.000 description 1
- HUZCTWYDQIQZPM-UHFFFAOYSA-N benzyl 2,2,2-trichloroethanimidate Chemical compound ClC(Cl)(Cl)C(=N)OCC1=CC=CC=C1 HUZCTWYDQIQZPM-UHFFFAOYSA-N 0.000 description 1
- 235000019445 benzyl alcohol Nutrition 0.000 description 1
- 239000011230 binding agent Substances 0.000 description 1
- 108091008324 binding proteins Proteins 0.000 description 1
- 230000003115 biocidal effect Effects 0.000 description 1
- 239000012472 biological sample Substances 0.000 description 1
- 229960000074 biopharmaceutical Drugs 0.000 description 1
- 238000001815 biotherapy Methods 0.000 description 1
- 239000012455 biphasic mixture Substances 0.000 description 1
- 201000001531 bladder carcinoma Diseases 0.000 description 1
- 230000000740 bleeding effect Effects 0.000 description 1
- 230000037396 body weight Effects 0.000 description 1
- 210000000481 breast Anatomy 0.000 description 1
- 206010006451 bronchitis Diseases 0.000 description 1
- 150000007516 brønsted-lowry acids Chemical class 0.000 description 1
- 239000007975 buffered saline Substances 0.000 description 1
- 244000309464 bull Species 0.000 description 1
- HQABUPZFAYXKJW-UHFFFAOYSA-N butan-1-amine Chemical compound CCCCN HQABUPZFAYXKJW-UHFFFAOYSA-N 0.000 description 1
- 210000004899 c-terminal region Anatomy 0.000 description 1
- 230000003185 calcium uptake Effects 0.000 description 1
- 125000000837 carbohydrate group Chemical group 0.000 description 1
- 239000001768 carboxy methyl cellulose Substances 0.000 description 1
- 150000007942 carboxylates Chemical class 0.000 description 1
- 150000001732 carboxylic acid derivatives Chemical class 0.000 description 1
- 238000000423 cell based assay Methods 0.000 description 1
- 239000001913 cellulose Substances 0.000 description 1
- 229920002678 cellulose Polymers 0.000 description 1
- 238000005119 centrifugation Methods 0.000 description 1
- 235000013339 cereals Nutrition 0.000 description 1
- 201000010881 cervical cancer Diseases 0.000 description 1
- 230000008859 change Effects 0.000 description 1
- 238000002512 chemotherapy Methods 0.000 description 1
- 210000004978 chinese hamster ovary cell Anatomy 0.000 description 1
- 108091016312 choline binding proteins Proteins 0.000 description 1
- 208000007451 chronic bronchitis Diseases 0.000 description 1
- 208000037976 chronic inflammation Diseases 0.000 description 1
- 230000006020 chronic inflammation Effects 0.000 description 1
- 150000001860 citric acid derivatives Chemical class 0.000 description 1
- 239000011248 coating agent Substances 0.000 description 1
- 238000000576 coating method Methods 0.000 description 1
- 229940110456 cocoa butter Drugs 0.000 description 1
- 235000019868 cocoa butter Nutrition 0.000 description 1
- 229910052681 coesite Inorganic materials 0.000 description 1
- 238000004737 colorimetric analysis Methods 0.000 description 1
- 238000004040 coloring Methods 0.000 description 1
- 229940125758 compound 15 Drugs 0.000 description 1
- 229940126142 compound 16 Drugs 0.000 description 1
- 229940125782 compound 2 Drugs 0.000 description 1
- 229940125810 compound 20 Drugs 0.000 description 1
- 229940126086 compound 21 Drugs 0.000 description 1
- 229940126208 compound 22 Drugs 0.000 description 1
- 229940125833 compound 23 Drugs 0.000 description 1
- 229940126214 compound 3 Drugs 0.000 description 1
- 229940125898 compound 5 Drugs 0.000 description 1
- 239000003636 conditioned culture medium Substances 0.000 description 1
- 230000001276 controlling effect Effects 0.000 description 1
- 229910052802 copper Inorganic materials 0.000 description 1
- 239000010949 copper Substances 0.000 description 1
- 230000008878 coupling Effects 0.000 description 1
- 238000010168 coupling process Methods 0.000 description 1
- 238000005859 coupling reaction Methods 0.000 description 1
- 229910052906 cristobalite Inorganic materials 0.000 description 1
- 201000003278 cryoglobulinemia Diseases 0.000 description 1
- WZHCOOQXZCIUNC-UHFFFAOYSA-N cyclandelate Chemical compound C1C(C)(C)CC(C)CC1OC(=O)C(O)C1=CC=CC=C1 WZHCOOQXZCIUNC-UHFFFAOYSA-N 0.000 description 1
- 125000004122 cyclic group Chemical group 0.000 description 1
- 125000001995 cyclobutyl group Chemical group [H]C1([H])C([H])([H])C([H])(*)C1([H])[H] 0.000 description 1
- 125000000596 cyclohexenyl group Chemical group C1(=CCCCC1)* 0.000 description 1
- 125000000113 cyclohexyl group Chemical group [H]C1([H])C([H])([H])C([H])([H])C([H])(*)C([H])([H])C1([H])[H] 0.000 description 1
- 125000002433 cyclopentenyl group Chemical group C1(=CCCC1)* 0.000 description 1
- 125000001511 cyclopentyl group Chemical group [H]C1([H])C([H])([H])C([H])([H])C([H])(*)C1([H])[H] 0.000 description 1
- 125000001559 cyclopropyl group Chemical group [H]C1([H])C([H])([H])C1([H])* 0.000 description 1
- 230000006378 damage Effects 0.000 description 1
- 230000000254 damaging effect Effects 0.000 description 1
- 230000003413 degradative effect Effects 0.000 description 1
- 210000004443 dendritic cell Anatomy 0.000 description 1
- 238000000586 desensitisation Methods 0.000 description 1
- 239000008121 dextrose Substances 0.000 description 1
- 125000000664 diazo group Chemical group [N-]=[N+]=[*] 0.000 description 1
- MHDVGSVTJDSBDK-UHFFFAOYSA-N dibenzyl ether Chemical class C=1C=CC=CC=1COCC1=CC=CC=C1 MHDVGSVTJDSBDK-UHFFFAOYSA-N 0.000 description 1
- FAVAVMFXAKZTMV-UHFFFAOYSA-N dibutylboranyl trifluoromethanesulfonate Chemical compound CCCCB(CCCC)OS(=O)(=O)C(F)(F)F FAVAVMFXAKZTMV-UHFFFAOYSA-N 0.000 description 1
- 235000014113 dietary fatty acids Nutrition 0.000 description 1
- UVYVLBIGDKGWPX-KUAJCENISA-N digitonin Chemical compound O([C@@H]1[C@@H]([C@]2(CC[C@@H]3[C@@]4(C)C[C@@H](O)[C@H](O[C@H]5[C@@H]([C@@H](O)[C@@H](O[C@H]6[C@@H]([C@@H](O[C@H]7[C@@H]([C@@H](O)[C@H](O)CO7)O)[C@H](O)[C@@H](CO)O6)O[C@H]6[C@@H]([C@@H](O[C@H]7[C@@H]([C@@H](O)[C@H](O)[C@@H](CO)O7)O)[C@@H](O)[C@@H](CO)O6)O)[C@@H](CO)O5)O)C[C@@H]4CC[C@H]3[C@@H]2[C@@H]1O)C)[C@@H]1C)[C@]11CC[C@@H](C)CO1 UVYVLBIGDKGWPX-KUAJCENISA-N 0.000 description 1
- UVYVLBIGDKGWPX-UHFFFAOYSA-N digitonine Natural products CC1C(C2(CCC3C4(C)CC(O)C(OC5C(C(O)C(OC6C(C(OC7C(C(O)C(O)CO7)O)C(O)C(CO)O6)OC6C(C(OC7C(C(O)C(O)C(CO)O7)O)C(O)C(CO)O6)O)C(CO)O5)O)CC4CCC3C2C2O)C)C2OC11CCC(C)CO1 UVYVLBIGDKGWPX-UHFFFAOYSA-N 0.000 description 1
- 230000003292 diminished effect Effects 0.000 description 1
- 150000002016 disaccharides Chemical group 0.000 description 1
- KPUWHANPEXNPJT-UHFFFAOYSA-N disiloxane Chemical class [SiH3]O[SiH3] KPUWHANPEXNPJT-UHFFFAOYSA-N 0.000 description 1
- 208000035475 disorder Diseases 0.000 description 1
- 239000002270 dispersing agent Substances 0.000 description 1
- 125000003438 dodecyl group Chemical group [H]C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])* 0.000 description 1
- 230000003828 downregulation Effects 0.000 description 1
- 208000008576 dracunculiasis Diseases 0.000 description 1
- 238000002296 dynamic light scattering Methods 0.000 description 1
- 239000012636 effector Substances 0.000 description 1
- 210000003162 effector t lymphocyte Anatomy 0.000 description 1
- 235000013601 eggs Nutrition 0.000 description 1
- 229920001971 elastomer Polymers 0.000 description 1
- 238000001962 electrophoresis Methods 0.000 description 1
- 238000004945 emulsification Methods 0.000 description 1
- 239000003995 emulsifying agent Substances 0.000 description 1
- 230000000369 enteropathogenic effect Effects 0.000 description 1
- 231100000249 enterotoxic Toxicity 0.000 description 1
- 230000002242 enterotoxic effect Effects 0.000 description 1
- 210000002919 epithelial cell Anatomy 0.000 description 1
- ZINJLDJMHCUBIP-UHFFFAOYSA-N ethametsulfuron-methyl Chemical compound CCOC1=NC(NC)=NC(NC(=O)NS(=O)(=O)C=2C(=CC=CC=2)C(=O)OC)=N1 ZINJLDJMHCUBIP-UHFFFAOYSA-N 0.000 description 1
- BEFDCLMNVWHSGT-UHFFFAOYSA-N ethenylcyclopentane Chemical compound C=CC1CCCC1 BEFDCLMNVWHSGT-UHFFFAOYSA-N 0.000 description 1
- 235000019325 ethyl cellulose Nutrition 0.000 description 1
- 229920001249 ethyl cellulose Polymers 0.000 description 1
- 125000004494 ethyl ester group Chemical group 0.000 description 1
- 125000001495 ethyl group Chemical group [H]C([H])([H])C([H])([H])* 0.000 description 1
- 125000005469 ethylenyl group Chemical group 0.000 description 1
- 230000005713 exacerbation Effects 0.000 description 1
- 235000019197 fats Nutrition 0.000 description 1
- 239000000194 fatty acid Substances 0.000 description 1
- 229930195729 fatty acid Natural products 0.000 description 1
- 150000004665 fatty acids Chemical class 0.000 description 1
- 230000002349 favourable effect Effects 0.000 description 1
- 235000021323 fish oil Nutrition 0.000 description 1
- 235000013305 food Nutrition 0.000 description 1
- 235000019264 food flavour enhancer Nutrition 0.000 description 1
- 235000003599 food sweetener Nutrition 0.000 description 1
- 238000004108 freeze drying Methods 0.000 description 1
- WIGCFUFOHFEKBI-UHFFFAOYSA-N gamma-tocopherol Natural products CC(C)CCCC(C)CCCC(C)CCCC1CCC2C(C)C(O)C(C)C(C)C2O1 WIGCFUFOHFEKBI-UHFFFAOYSA-N 0.000 description 1
- 150000002270 gangliosides Chemical class 0.000 description 1
- 229940124670 gardiquimod Drugs 0.000 description 1
- 210000001035 gastrointestinal tract Anatomy 0.000 description 1
- 239000000499 gel Substances 0.000 description 1
- 230000002068 genetic effect Effects 0.000 description 1
- 150000002307 glutamic acids Chemical class 0.000 description 1
- 229960003180 glutathione Drugs 0.000 description 1
- 230000002414 glycolytic effect Effects 0.000 description 1
- 239000004519 grease Substances 0.000 description 1
- 229940093915 gynecological organic acid Drugs 0.000 description 1
- 231100000869 headache Toxicity 0.000 description 1
- 230000036541 health Effects 0.000 description 1
- 244000000013 helminth Species 0.000 description 1
- 210000002443 helper t lymphocyte Anatomy 0.000 description 1
- 208000005252 hepatitis A Diseases 0.000 description 1
- 238000004896 high resolution mass spectrometry Methods 0.000 description 1
- 238000012766 histopathologic analysis Methods 0.000 description 1
- 238000000265 homogenisation Methods 0.000 description 1
- 201000009163 human granulocytic anaplasmosis Diseases 0.000 description 1
- 208000022340 human granulocytic ehrlichiosis Diseases 0.000 description 1
- 230000008348 humoral response Effects 0.000 description 1
- IXCSERBJSXMMFS-UHFFFAOYSA-N hydrogen chloride Substances Cl.Cl IXCSERBJSXMMFS-UHFFFAOYSA-N 0.000 description 1
- 229910000041 hydrogen chloride Inorganic materials 0.000 description 1
- FAHBNUUHRFUEAI-UHFFFAOYSA-M hydroxidooxidoaluminium Chemical compound O[Al]=O FAHBNUUHRFUEAI-UHFFFAOYSA-M 0.000 description 1
- 229960002751 imiquimod Drugs 0.000 description 1
- DOUYETYNHWVLEO-UHFFFAOYSA-N imiquimod Chemical compound C1=CC=CC2=C3N(CC(C)C)C=NC3=C(N)N=C21 DOUYETYNHWVLEO-UHFFFAOYSA-N 0.000 description 1
- 230000005965 immune activity Effects 0.000 description 1
- 230000008105 immune reaction Effects 0.000 description 1
- 230000008073 immune recognition Effects 0.000 description 1
- 238000003119 immunoblot Methods 0.000 description 1
- 229940072221 immunoglobulins Drugs 0.000 description 1
- 238000003364 immunohistochemistry Methods 0.000 description 1
- 238000010324 immunological assay Methods 0.000 description 1
- 230000001024 immunotherapeutic effect Effects 0.000 description 1
- 230000006872 improvement Effects 0.000 description 1
- 238000011534 incubation Methods 0.000 description 1
- 239000000411 inducer Substances 0.000 description 1
- 230000001524 infective effect Effects 0.000 description 1
- 230000002757 inflammatory effect Effects 0.000 description 1
- 230000028709 inflammatory response Effects 0.000 description 1
- 206010022000 influenza Diseases 0.000 description 1
- 238000001802 infusion Methods 0.000 description 1
- 230000000977 initiatory effect Effects 0.000 description 1
- 239000002198 insoluble material Substances 0.000 description 1
- 229940047122 interleukins Drugs 0.000 description 1
- 238000007913 intrathecal administration Methods 0.000 description 1
- 238000007915 intraurethral administration Methods 0.000 description 1
- 239000003456 ion exchange resin Substances 0.000 description 1
- 229920003303 ion-exchange polymer Polymers 0.000 description 1
- 230000002427 irreversible effect Effects 0.000 description 1
- 125000000959 isobutyl group Chemical group [H]C([H])([H])C([H])(C([H])([H])[H])C([H])([H])* 0.000 description 1
- 125000005468 isobutylenyl group Chemical group 0.000 description 1
- 238000002955 isolation Methods 0.000 description 1
- 125000001972 isopentyl group Chemical group [H]C([H])([H])C([H])(C([H])([H])[H])C([H])([H])C([H])([H])* 0.000 description 1
- 125000001449 isopropyl group Chemical group [H]C([H])([H])C([H])(*)C([H])([H])[H] 0.000 description 1
- 239000007951 isotonicity adjuster Substances 0.000 description 1
- 108010024383 kallikrein 4 Proteins 0.000 description 1
- NLYAJNPCOHFWQQ-UHFFFAOYSA-N kaolin Chemical compound O.O.O=[Al]O[Si](=O)O[Si](=O)O[Al]=O NLYAJNPCOHFWQQ-UHFFFAOYSA-N 0.000 description 1
- 125000000468 ketone group Chemical group 0.000 description 1
- 201000006370 kidney failure Diseases 0.000 description 1
- 230000002147 killing effect Effects 0.000 description 1
- 238000002372 labelling Methods 0.000 description 1
- 150000003893 lactate salts Chemical class 0.000 description 1
- 239000008101 lactose Substances 0.000 description 1
- 210000000265 leukocyte Anatomy 0.000 description 1
- 239000003446 ligand Substances 0.000 description 1
- 230000007774 longterm Effects 0.000 description 1
- 201000005296 lung carcinoma Diseases 0.000 description 1
- 201000003866 lung sarcoma Diseases 0.000 description 1
- 206010025135 lupus erythematosus Diseases 0.000 description 1
- 239000002932 luster Substances 0.000 description 1
- 210000004698 lymphocyte Anatomy 0.000 description 1
- 101710130522 mRNA export factor Proteins 0.000 description 1
- ZLNQQNXFFQJAID-UHFFFAOYSA-L magnesium carbonate Chemical compound [Mg+2].[O-]C([O-])=O ZLNQQNXFFQJAID-UHFFFAOYSA-L 0.000 description 1
- 239000001095 magnesium carbonate Substances 0.000 description 1
- 229910000021 magnesium carbonate Inorganic materials 0.000 description 1
- 235000019359 magnesium stearate Nutrition 0.000 description 1
- 238000012423 maintenance Methods 0.000 description 1
- 239000000594 mannitol Substances 0.000 description 1
- 235000010355 mannitol Nutrition 0.000 description 1
- 125000002960 margaryl group Chemical group [H]C([*])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])[H] 0.000 description 1
- 239000003550 marker Substances 0.000 description 1
- 238000005259 measurement Methods 0.000 description 1
- 230000007246 mechanism Effects 0.000 description 1
- 210000001806 memory b lymphocyte Anatomy 0.000 description 1
- 210000003071 memory t lymphocyte Anatomy 0.000 description 1
- 239000002207 metabolite Substances 0.000 description 1
- DSQRYVDYSWWRDB-OAQYLSRUSA-N methyl (3r)-3-phenylmethoxytetradecanoate Chemical compound CCCCCCCCCCC[C@H](CC(=O)OC)OCC1=CC=CC=C1 DSQRYVDYSWWRDB-OAQYLSRUSA-N 0.000 description 1
- 150000004702 methyl esters Chemical class 0.000 description 1
- 125000002496 methyl group Chemical group [H]C([H])([H])* 0.000 description 1
- 235000010270 methyl p-hydroxybenzoate Nutrition 0.000 description 1
- 239000004292 methyl p-hydroxybenzoate Substances 0.000 description 1
- 229960002216 methylparaben Drugs 0.000 description 1
- 239000012569 microbial contaminant Substances 0.000 description 1
- 239000003094 microcapsule Substances 0.000 description 1
- 239000003226 mitogen Substances 0.000 description 1
- 238000002156 mixing Methods 0.000 description 1
- 125000000896 monocarboxylic acid group Chemical group 0.000 description 1
- 210000001616 monocyte Anatomy 0.000 description 1
- 239000000178 monomer Substances 0.000 description 1
- 210000005087 mononuclear cell Anatomy 0.000 description 1
- 206010028417 myasthenia gravis Diseases 0.000 description 1
- 125000001421 myristyl group Chemical group [H]C([*])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])[H] 0.000 description 1
- 125000004108 n-butyl group Chemical group [H]C([H])([H])C([H])([H])C([H])([H])C([H])([H])* 0.000 description 1
- 125000001280 n-hexyl group Chemical group C(CCCCC)* 0.000 description 1
- 125000000740 n-pentyl group Chemical group [H]C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])* 0.000 description 1
- 210000000822 natural killer cell Anatomy 0.000 description 1
- 230000008693 nausea Effects 0.000 description 1
- 239000013642 negative control Substances 0.000 description 1
- 208000015122 neurodegenerative disease Diseases 0.000 description 1
- 230000007935 neutral effect Effects 0.000 description 1
- FEMOMIGRRWSMCU-UHFFFAOYSA-N ninhydrin Chemical compound C1=CC=C2C(=O)C(O)(O)C(=O)C2=C1 FEMOMIGRRWSMCU-UHFFFAOYSA-N 0.000 description 1
- 231100000344 non-irritating Toxicity 0.000 description 1
- 230000002126 nonhaemolytic effect Effects 0.000 description 1
- 239000000346 nonvolatile oil Substances 0.000 description 1
- 239000002777 nucleoside Substances 0.000 description 1
- 150000003833 nucleoside derivatives Chemical class 0.000 description 1
- 235000014571 nuts Nutrition 0.000 description 1
- 239000002674 ointment Substances 0.000 description 1
- 229940046166 oligodeoxynucleotide Drugs 0.000 description 1
- 229920001542 oligosaccharide Polymers 0.000 description 1
- 150000002482 oligosaccharides Chemical class 0.000 description 1
- 210000000056 organ Anatomy 0.000 description 1
- 235000005985 organic acids Nutrition 0.000 description 1
- 239000003960 organic solvent Substances 0.000 description 1
- 230000008520 organization Effects 0.000 description 1
- 229940099789 ospa protein Drugs 0.000 description 1
- 229940094443 oxytocics prostaglandins Drugs 0.000 description 1
- 229910052763 palladium Inorganic materials 0.000 description 1
- IPCSVZSSVZVIGE-UHFFFAOYSA-N palmitic acid group Chemical group C(CCCCCCCCCCCCCCC)(=O)O IPCSVZSSVZVIGE-UHFFFAOYSA-N 0.000 description 1
- 125000000913 palmityl group Chemical group [H]C([*])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])[H] 0.000 description 1
- 238000007911 parenteral administration Methods 0.000 description 1
- 230000001575 pathological effect Effects 0.000 description 1
- 239000013610 patient sample Substances 0.000 description 1
- 239000000312 peanut oil Substances 0.000 description 1
- 125000002958 pentadecyl group Chemical group [H]C([*])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])[H] 0.000 description 1
- 239000000813 peptide hormone Substances 0.000 description 1
- 210000005259 peripheral blood Anatomy 0.000 description 1
- 239000011886 peripheral blood Substances 0.000 description 1
- 108010021711 pertactin Proteins 0.000 description 1
- 229940066842 petrolatum Drugs 0.000 description 1
- 235000019271 petrolatum Nutrition 0.000 description 1
- LIGACIXOYTUXAW-UHFFFAOYSA-N phenacyl bromide Chemical compound BrCC(=O)C1=CC=CC=C1 LIGACIXOYTUXAW-UHFFFAOYSA-N 0.000 description 1
- 150000003904 phospholipids Chemical class 0.000 description 1
- 150000003013 phosphoric acid derivatives Chemical class 0.000 description 1
- 239000002504 physiological saline solution Substances 0.000 description 1
- 210000004180 plasmocyte Anatomy 0.000 description 1
- 101150106828 pmpD gene Proteins 0.000 description 1
- 229940124733 pneumococcal vaccine Drugs 0.000 description 1
- 229920001983 poloxamer Polymers 0.000 description 1
- 229920001481 poly(stearyl methacrylate) Polymers 0.000 description 1
- 229920000642 polymer Polymers 0.000 description 1
- 108091033319 polynucleotide Proteins 0.000 description 1
- 102000040430 polynucleotide Human genes 0.000 description 1
- 239000002157 polynucleotide Substances 0.000 description 1
- 229950008882 polysorbate Drugs 0.000 description 1
- 229940068968 polysorbate 80 Drugs 0.000 description 1
- 229910000027 potassium carbonate Inorganic materials 0.000 description 1
- 239000002244 precipitate Substances 0.000 description 1
- 239000002243 precursor Substances 0.000 description 1
- 230000002335 preservative effect Effects 0.000 description 1
- 230000002265 prevention Effects 0.000 description 1
- 125000002924 primary amino group Chemical group [H]N([H])* 0.000 description 1
- 230000008569 process Effects 0.000 description 1
- 230000035755 proliferation Effects 0.000 description 1
- CAEWJEXPFKNBQL-UHFFFAOYSA-N prop-2-enyl carbonochloridate Chemical compound ClC(=O)OCC=C CAEWJEXPFKNBQL-UHFFFAOYSA-N 0.000 description 1
- 125000005470 propylenyl group Chemical group 0.000 description 1
- 125000002568 propynyl group Chemical group [*]C#CC([H])([H])[H] 0.000 description 1
- 150000003180 prostaglandins Chemical class 0.000 description 1
- 244000000040 protozoan parasite Species 0.000 description 1
- 230000005180 public health Effects 0.000 description 1
- 238000003908 quality control method Methods 0.000 description 1
- 238000001959 radiotherapy Methods 0.000 description 1
- 230000009257 reactivity Effects 0.000 description 1
- 210000000664 rectum Anatomy 0.000 description 1
- 230000001105 regulatory effect Effects 0.000 description 1
- 239000003488 releasing hormone Substances 0.000 description 1
- 238000011160 research Methods 0.000 description 1
- 239000011347 resin Substances 0.000 description 1
- 229920005989 resin Polymers 0.000 description 1
- BXNMTOQRYBFHNZ-UHFFFAOYSA-N resiquimod Chemical compound C1=CC=CC2=C(N(C(COCC)=N3)CC(C)(C)O)C3=C(N)N=C21 BXNMTOQRYBFHNZ-UHFFFAOYSA-N 0.000 description 1
- 208000023504 respiratory system disease Diseases 0.000 description 1
- 230000004043 responsiveness Effects 0.000 description 1
- 230000002441 reversible effect Effects 0.000 description 1
- 238000012552 review Methods 0.000 description 1
- 239000008165 rice bran oil Substances 0.000 description 1
- 229910052707 ruthenium Inorganic materials 0.000 description 1
- CVHZOJJKTDOEJC-UHFFFAOYSA-N saccharin Chemical compound C1=CC=C2C(=O)NS(=O)(=O)C2=C1 CVHZOJJKTDOEJC-UHFFFAOYSA-N 0.000 description 1
- 235000002020 sage Nutrition 0.000 description 1
- 238000007127 saponification reaction Methods 0.000 description 1
- HFHDHCJBZVLPGP-UHFFFAOYSA-N schardinger α-dextrin Chemical compound O1C(C(C2O)O)C(CO)OC2OC(C(C2O)O)C(CO)OC2OC(C(C2O)O)C(CO)OC2OC(C(O)C2O)C(CO)OC2OC(C(C2O)O)C(CO)OC2OC2C(O)C(O)C1OC2CO HFHDHCJBZVLPGP-UHFFFAOYSA-N 0.000 description 1
- 238000007789 sealing Methods 0.000 description 1
- 125000002914 sec-butyl group Chemical group [H]C([H])([H])C([H])([H])C([H])(*)C([H])([H])[H] 0.000 description 1
- 230000000405 serological effect Effects 0.000 description 1
- 238000009589 serological test Methods 0.000 description 1
- 239000010686 shark liver oil Substances 0.000 description 1
- 229940069764 shark liver oil Drugs 0.000 description 1
- 230000035939 shock Effects 0.000 description 1
- 238000009097 single-agent therapy Methods 0.000 description 1
- 238000007390 skin biopsy Methods 0.000 description 1
- 208000017520 skin disease Diseases 0.000 description 1
- 108091029842 small nuclear ribonucleic acid Proteins 0.000 description 1
- 235000010413 sodium alginate Nutrition 0.000 description 1
- 239000000661 sodium alginate Substances 0.000 description 1
- 229940005550 sodium alginate Drugs 0.000 description 1
- WXMKPNITSTVMEF-UHFFFAOYSA-M sodium benzoate Chemical compound [Na+].[O-]C(=O)C1=CC=CC=C1 WXMKPNITSTVMEF-UHFFFAOYSA-M 0.000 description 1
- 235000010234 sodium benzoate Nutrition 0.000 description 1
- 239000004299 sodium benzoate Substances 0.000 description 1
- 229910000029 sodium carbonate Inorganic materials 0.000 description 1
- 235000019812 sodium carboxymethyl cellulose Nutrition 0.000 description 1
- 235000010267 sodium hydrogen sulphite Nutrition 0.000 description 1
- 235000010199 sorbic acid Nutrition 0.000 description 1
- 239000004334 sorbic acid Substances 0.000 description 1
- 229940075582 sorbic acid Drugs 0.000 description 1
- 230000003595 spectral effect Effects 0.000 description 1
- 210000000952 spleen Anatomy 0.000 description 1
- 239000007858 starting material Substances 0.000 description 1
- 125000004079 stearyl group Chemical group [H]C([*])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])[H] 0.000 description 1
- 150000003432 sterols Chemical class 0.000 description 1
- 235000003702 sterols Nutrition 0.000 description 1
- 229910052682 stishovite Inorganic materials 0.000 description 1
- 239000011550 stock solution Substances 0.000 description 1
- 238000007920 subcutaneous administration Methods 0.000 description 1
- 125000001424 substituent group Chemical group 0.000 description 1
- 239000000758 substrate Substances 0.000 description 1
- 229940031626 subunit vaccine Drugs 0.000 description 1
- KDYFGRWQOYBRFD-UHFFFAOYSA-L succinate(2-) Chemical compound [O-]C(=O)CCC([O-])=O KDYFGRWQOYBRFD-UHFFFAOYSA-L 0.000 description 1
- KUNICNFETYAKKO-UHFFFAOYSA-N sulfuric acid;pentahydrate Chemical compound O.O.O.O.O.OS(O)(=O)=O KUNICNFETYAKKO-UHFFFAOYSA-N 0.000 description 1
- 239000006228 supernatant Substances 0.000 description 1
- 239000000829 suppository Substances 0.000 description 1
- 230000001629 suppression Effects 0.000 description 1
- 208000032922 susceptibility to mycobacterium tuberculosis Diseases 0.000 description 1
- 238000013268 sustained release Methods 0.000 description 1
- 239000012730 sustained-release form Substances 0.000 description 1
- 239000003765 sweetening agent Substances 0.000 description 1
- 239000000454 talc Substances 0.000 description 1
- 235000012222 talc Nutrition 0.000 description 1
- 229910052623 talc Inorganic materials 0.000 description 1
- 125000000999 tert-butyl group Chemical group [H]C([H])([H])C(*)(C([H])([H])[H])C([H])([H])[H] 0.000 description 1
- 229940118376 tetanus toxin Drugs 0.000 description 1
- 229940021747 therapeutic vaccine Drugs 0.000 description 1
- 239000002562 thickening agent Substances 0.000 description 1
- 229960002175 thyroglobulin Drugs 0.000 description 1
- 210000001685 thyroid gland Anatomy 0.000 description 1
- 108040006218 thyroid-stimulating hormone receptor activity proteins Proteins 0.000 description 1
- 102000015486 thyroid-stimulating hormone receptor activity proteins Human genes 0.000 description 1
- 230000003867 tiredness Effects 0.000 description 1
- 208000016255 tiredness Diseases 0.000 description 1
- 230000024664 tolerance induction Effects 0.000 description 1
- 239000003970 toll like receptor agonist Substances 0.000 description 1
- 229940044616 toll-like receptor 7 agonist Drugs 0.000 description 1
- REJLGAUYTKNVJM-SGXCCWNXSA-N tomatine Chemical compound O([C@H]1[C@H](O)[C@@H](CO)O[C@H]([C@@H]1O[C@H]1[C@@H]([C@@H](O)[C@H](O)[C@@H](CO)O1)O)O[C@H]1[C@@H](CO)O[C@H]([C@@H]([C@H]1O)O)O[C@@H]1C[C@@H]2CC[C@H]3[C@@H]4C[C@H]5[C@@H]([C@]4(CC[C@@H]3[C@@]2(C)CC1)C)[C@@H]([C@@]1(NC[C@@H](C)CC1)O5)C)[C@@H]1OC[C@@H](O)[C@H](O)[C@H]1O REJLGAUYTKNVJM-SGXCCWNXSA-N 0.000 description 1
- 230000000699 topical effect Effects 0.000 description 1
- 239000012049 topical pharmaceutical composition Substances 0.000 description 1
- 230000001988 toxicity Effects 0.000 description 1
- 231100000419 toxicity Toxicity 0.000 description 1
- 231100000440 toxicity profile Toxicity 0.000 description 1
- 238000006276 transfer reaction Methods 0.000 description 1
- 102000027257 transmembrane receptors Human genes 0.000 description 1
- 108091008578 transmembrane receptors Proteins 0.000 description 1
- 238000011269 treatment regimen Methods 0.000 description 1
- 229940093609 tricaprylin Drugs 0.000 description 1
- 229940096911 trichinella spiralis Drugs 0.000 description 1
- 125000002889 tridecyl group Chemical group [H]C([*])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])[H] 0.000 description 1
- 229910052905 tridymite Inorganic materials 0.000 description 1
- ITMCEJHCFYSIIV-UHFFFAOYSA-N triflic acid Chemical compound OS(=O)(=O)C(F)(F)F ITMCEJHCFYSIIV-UHFFFAOYSA-N 0.000 description 1
- NQPHMXWPDCSHTE-UHFFFAOYSA-N trifluoromethanesulfonyl azide Chemical compound FC(F)(F)S(=O)(=O)N=[N+]=[N-] NQPHMXWPDCSHTE-UHFFFAOYSA-N 0.000 description 1
- UFTFJSFQGQCHQW-UHFFFAOYSA-N triformin Chemical compound O=COCC(OC=O)COC=O UFTFJSFQGQCHQW-UHFFFAOYSA-N 0.000 description 1
- FTVLMFQEYACZNP-UHFFFAOYSA-N trimethylsilyl trifluoromethanesulfonate Chemical compound C[Si](C)(C)OS(=O)(=O)C(F)(F)F FTVLMFQEYACZNP-UHFFFAOYSA-N 0.000 description 1
- VLPFTAMPNXLGLX-UHFFFAOYSA-N trioctanoin Chemical compound CCCCCCCC(=O)OCC(OC(=O)CCCCCCC)COC(=O)CCCCCCC VLPFTAMPNXLGLX-UHFFFAOYSA-N 0.000 description 1
- 229960001005 tuberculin Drugs 0.000 description 1
- 229960002109 tuberculosis vaccine Drugs 0.000 description 1
- OUYCCCASQSFEME-UHFFFAOYSA-N tyrosine Natural products OC(=O)C(N)CC1=CC=C(O)C=C1 OUYCCCASQSFEME-UHFFFAOYSA-N 0.000 description 1
- 125000002948 undecyl group Chemical group [H]C([*])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])[H] 0.000 description 1
- 125000004417 unsaturated alkyl group Chemical group 0.000 description 1
- 230000003827 upregulation Effects 0.000 description 1
- 208000010570 urinary bladder carcinoma Diseases 0.000 description 1
- 230000002477 vacuolizing effect Effects 0.000 description 1
- 244000052613 viral pathogen Species 0.000 description 1
- 230000003612 virological effect Effects 0.000 description 1
- 239000000277 virosome Substances 0.000 description 1
- 210000001835 viscera Anatomy 0.000 description 1
- 230000009278 visceral effect Effects 0.000 description 1
- 239000011709 vitamin E Substances 0.000 description 1
- 235000019165 vitamin E Nutrition 0.000 description 1
- 229940046009 vitamin E Drugs 0.000 description 1
- 230000008673 vomiting Effects 0.000 description 1
- 239000008215 water for injection Substances 0.000 description 1
- 239000001993 wax Substances 0.000 description 1
- 238000001262 western blot Methods 0.000 description 1
- 239000000080 wetting agent Substances 0.000 description 1
- 229940051021 yellow-fever virus Drugs 0.000 description 1
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/70—Carbohydrates; Sugars; Derivatives thereof
- A61K31/7024—Esters of saccharides
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K39/39—Medicinal preparations containing antigens or antibodies characterised by the immunostimulating additives, e.g. chemical adjuvants
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/66—Phosphorus compounds
- A61K31/665—Phosphorus compounds having oxygen as a ring hetero atom, e.g. fosfomycin
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/70—Carbohydrates; Sugars; Derivatives thereof
- A61K31/7016—Disaccharides, e.g. lactose, lactulose
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/70—Carbohydrates; Sugars; Derivatives thereof
- A61K31/7028—Compounds having saccharide radicals attached to non-saccharide compounds by glycosidic linkages
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K39/02—Bacterial antigens
- A61K39/04—Mycobacterium, e.g. Mycobacterium tuberculosis
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K39/12—Viral antigens
- A61K39/21—Retroviridae, e.g. equine infectious anemia virus
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K39/12—Viral antigens
- A61K39/235—Adenoviridae
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K39/12—Viral antigens
- A61K39/245—Herpetoviridae, e.g. herpes simplex virus
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K39/12—Viral antigens
- A61K39/275—Poxviridae, e.g. avipoxvirus
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K9/00—Medicinal preparations characterised by special physical form
- A61K9/10—Dispersions; Emulsions
- A61K9/107—Emulsions ; Emulsion preconcentrates; Micelles
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P31/00—Antiinfectives, i.e. antibiotics, antiseptics, chemotherapeutics
- A61P31/12—Antivirals
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P35/00—Antineoplastic agents
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P37/00—Drugs for immunological or allergic disorders
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P37/00—Drugs for immunological or allergic disorders
- A61P37/02—Immunomodulators
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P37/00—Drugs for immunological or allergic disorders
- A61P37/02—Immunomodulators
- A61P37/04—Immunostimulants
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P37/00—Drugs for immunological or allergic disorders
- A61P37/08—Antiallergic agents
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07H—SUGARS; DERIVATIVES THEREOF; NUCLEOSIDES; NUCLEOTIDES; NUCLEIC ACIDS
- C07H11/00—Compounds containing saccharide radicals esterified by inorganic acids; Metal salts thereof
- C07H11/04—Phosphates; Phosphites; Polyphosphates
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07H—SUGARS; DERIVATIVES THEREOF; NUCLEOSIDES; NUCLEOTIDES; NUCLEIC ACIDS
- C07H15/00—Compounds containing hydrocarbon or substituted hydrocarbon radicals directly attached to hetero atoms of saccharide radicals
- C07H15/02—Acyclic radicals, not substituted by cyclic structures
- C07H15/04—Acyclic radicals, not substituted by cyclic structures attached to an oxygen atom of the saccharide radical
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07H—SUGARS; DERIVATIVES THEREOF; NUCLEOSIDES; NUCLEOTIDES; NUCLEIC ACIDS
- C07H15/00—Compounds containing hydrocarbon or substituted hydrocarbon radicals directly attached to hetero atoms of saccharide radicals
- C07H15/02—Acyclic radicals, not substituted by cyclic structures
- C07H15/12—Acyclic radicals, not substituted by cyclic structures attached to a nitrogen atom of the saccharide radical
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07H—SUGARS; DERIVATIVES THEREOF; NUCLEOSIDES; NUCLEOTIDES; NUCLEIC ACIDS
- C07H15/00—Compounds containing hydrocarbon or substituted hydrocarbon radicals directly attached to hetero atoms of saccharide radicals
- C07H15/20—Carbocyclic rings
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K2039/51—Medicinal preparations containing antigens or antibodies comprising whole cells, viruses or DNA/RNA
- A61K2039/525—Virus
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K2039/555—Medicinal preparations containing antigens or antibodies characterised by a specific combination antigen/adjuvant
- A61K2039/55511—Organic adjuvants
- A61K2039/55572—Lipopolysaccharides; Lipid A; Monophosphoryl lipid A
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K2039/57—Medicinal preparations containing antigens or antibodies characterised by the type of response, e.g. Th1, Th2
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K2039/57—Medicinal preparations containing antigens or antibodies characterised by the type of response, e.g. Th1, Th2
- A61K2039/575—Medicinal preparations containing antigens or antibodies characterised by the type of response, e.g. Th1, Th2 humoral response
Definitions
- the present invention relates to the field of pharmaceutical and vaccine compositions. More specifically, embodiments described herein relate to pharmaceutical and vaccine compositions, as well as related prophylactic and therapeutic methods, wherein the compositions comprise a glucopyranosyl lipid adjuvant (GLA) as described herein.
- GLA glucopyranosyl lipid adjuvant
- Immune responses have traditionally been characterized as either humoral responses, in which antibodies specific for antigens are produced by differentiated B lymphocytes known as plasma cells, or cell mediated responses, in which various types of T lymphocytes act to eliminate antigens by a number of mechanisms.
- B lymphocytes differentiated B lymphocytes known as plasma cells
- cell mediated responses in which various types of T lymphocytes act to eliminate antigens by a number of mechanisms.
- CD4+ helper T cells that are capable of recognizing specific antigens may respond by releasing soluble mediators such as cytokines to recruit additional cells of the immune system to participate in an immune response.
- CD8+ cytotoxic T cells that are also capable of specific antigen recognition may respond by binding to and destroying or damaging an antigen-bearing cell or particle. It is known in the immunological arts to provide certain vaccines according to a variety of formulations, usually for the purpose of inducing a desired immune response in a host.
- Several strategies for eliciting specific immune responses through the administration of a vaccine to a host include immunization with heat-killed or with live, attenuated infectious pathogens such as viruses, bacteria or certain eukaryotic pathogens; immunization with a non-virulent infective agent capable of directing the expression of genetic material encoding the antigen(s) to which an immune response is desired; and immunization with subunit vaccines that contain isolated immunogens (such as proteins) from a particular pathogen in order to induce immunity against the pathogen.
- infectious pathogens such as viruses, bacteria or certain eukaryotic pathogens
- a non-virulent infective agent capable of directing the expression of genetic material encoding the antigen(s) to which an immune response is desired
- subunit vaccines that contain isolated immunogens (such as proteins) from a particular pathogen in order to induce immunity against the pathogen.
- enterobacterial lipopolysaccharide is a potent stimulator of the immune system, although its use in adjuvants has been curtailed by its toxic effects.
- LPS enterobacterial lipopolysaccharide
- MPL monophosphoryl lipid A
- a further detoxified version of MPL results from the removal of the acyl chain from the 3-position of the disaccharide backbone, and is called 3-O- deacylated monophosphoryl lipid A (3D-MPL). It can be purified and prepared by the methods taught in GB 2122204B, which reference also discloses the preparation of diphosphoryl lipid A, and 3-O-deacylated variants thereof.
- 3D-MPL has been prepared in the form of an emulsion having a small particle size less than 0.2 ⁇ m in diameter, and its method of manufacture is disclosed in WO 94/21292.
- Aqueous formulations comprising monophosphoryl lipid A and a surfactant have been described in WO9843670A2.
- Bacterial lipopolysacchahde-derived adjuvants to be formulated in adjuvant combinations may be purified and processed from bacterial sources, or alternatively they may be synthetic.
- purified monophosphoryl lipid A is described in Ribi et at 1986 ⁇ supra
- 3-O-deacylated monophosphoryl or diphosphoryl lipid A derived from Salmonella sp. is described in GB 2220211 and U.S. Pat. No. 4,912,094.
- 3D-MPL and the ⁇ (1 -6) glucosamine disaccharides as well as other purified and synthetic lipopolysaccharides have been described (WO 98/01139; U.S. Pat. No.
- WO 95/17210 discloses an adjuvant emulsion system based on squalene, ⁇ - tocopherol, and polyoxyethylene sorbitan monooleate (TWEENTM-80), formulated with the immunostimulant QS21 , and optionally including 3D-MPL.
- TWEENTM-80 polyoxyethylene sorbitan monooleate
- the use of adjuvants derived from natural products is accompanied by high production costs, inconsistency from lot to lot, difficulties associated with large-scale production, and uncertainty with respect to the presence of impurities in the compositional make-up of any given preparation.
- GLA glucopyranosyl lipid adjuvants
- the GLA compounds of the present invention have utility over a broad range of therapeutic applications where induction of specific or nonspecific immune responses is desired.
- vaccine compositions comprising one or more GLA compounds as set forth herein in combination with an antigen.
- Such vaccine compositions may be advantageously used in methods for stimulating antigen-specific immune responses in subjects in need thereof.
- pharmaceutical compositions comprising one or more GLA compounds as set forth herein, wherein the compositions are substantially devoid of antigen.
- Such pharmaceutical compositions may be advantageously used in methods for stimulating non- specific immune responses in subjects in need thereof, for example in the treatment of infection, seasonal rhinitis and the like.
- Figure 1 demonstrates IFN- ⁇ cytokine production induced in vivo following vaccination of mice with compositions of the invention comprising antigen and GLA.
- Figures 2A-2F show antibody responses induced in vivo following vaccination of mice with compositions of the invention comprising antigen and GLA.
- Figure 3 shows the NF-kB enhancement observed at different concentrations of an illustrative GLA compound of the invention (Compound IX).
- FIGS 4A-4D show the induction of immunostimulatory cytokines (MIP-1 b and TNFa) at different concentrations of an illustrative GLA compound of the invention (Compound IX).
- Monophosphoryl lipid A (MPL) and other related adjuvants are known to mediate their effects, at least in part, by acting as agonists of Toll-like receptors (TLR).
- TLR Toll-like receptors
- the glucopyranosyl lipid adjuvant (GLA) compounds of the present invention were rationally designed based upon 3D structural considerations in relation to TLR receptor stimulation. More specifically, according to the present invention, by selectively defining the acyl chain lengths of the GLA compounds of the invention such that they achieve a "flat" bottom in the three dimensional structure of the compounds, an improved fit may be achieved within the binding site of a TLR receptor, thereby resulting in enhanced TLR stimulation and enhanced immunostimulatory properties.
- the solubility of the GLA compounds of the invention is advantageously improved due to the shortened acyl chain lengths, thereby facilitating efficient and effective compound formulation.
- the acyl chain lengths are tailored to make the molecule three dimensionally "flat" along the bottom of the molecule, the compounds can be more effectively incorporated within vesicles, e.g., for liposomal formulations.
- compounds of the invention provide advantageous profiles of potency relative to toxicity.
- the compounds of the invention may be used over a broad and relatively high range of dosages for achieving a desired level of activity ⁇ e.g., adjuvant activity), while nevertheless remaining substantially non-toxic to human cells and to human patients, as assayed, for example, by the levels of tumor necrosis factor produced from human cells over a range of concentrations, which quickly rises and levels off unlike other more toxic TLR4 agonists such as lipopolysaccharide.
- This cell based assay should be predictive of lower inflammatory markers like C-reactive protein involved in adverse events in human pharmacology. The favorable potency vs.
- toxicity profile for the compounds of the invention may be particularly important, for example, when administering to children whose tolerance to cytokines may be lower, or when the compounds are used in formulations targeted at a large population where more leveled responses will translate into more consistent clinical outcomes for people with a varied responsiveness to TLR agonism.
- regulatory approval will be simplified since target dosing will be more forgiving and manufacturing simplified when the range of active pharmaceutical ingredient need not be controlled at as strict a tolerance level.
- the present invention in its many embodiments provides compounds, vaccine compositions, adjuvant compositions, pharmaceutical compositions and related formulations and methods that include synthetic GLA compounds as described herein.
- the GLA compounds represent synthetic immunomodulators which, advantageously relative to adjuvants of the prior art, and in particular, relative to natural product adjuvants, can be prepared in substantially homogeneous form.
- the GLA compounds of the invention can be prepared efficiently and economically through large-scale synthetic chemical manufacturing, unlike natural product- derived adjuvants. Because a synthetic adjuvant that is chemically synthesized from defined starting materials to obtain a chemically defined product exhibits qualitative and quantitative batch-to-batch consistency, the GLA compounds of the invention offer benefits including improved product quality control.
- GLA compounds, compositions and methods for their use include in some embodiments the use of GLA by itself with a pharmaceutically acceptable carrier or excipient for immunological adjuvant activity (e.g., non-specific immunostimulatory activity), including "adjuvanting" in which GLA administration to a subject may be wholly independent of, and/or separated temporally and/or spatially from, administration to the subject of one or more antigens against which elicitation or enhancement of an immune response ⁇ e.g., an antigen-specific response) in the subject is desired.
- Other embodiments include the use of GLA in a vaccine composition that also includes one or a plurality of antigens to which an immune response elicited or enhanced by such a vaccine is desired.
- these vaccine compositions may in certain related embodiments also include one or more toll-like receptor (TLR) agonist and/or one or a plurality of one or more of a co-adjuvant, an imidazoquinoline immune response modifier, and a double stem loop immune modifier (dSLIM).
- TLR toll-like receptor
- dSLIM double stem loop immune modifier
- a vaccine composition as provided herein may comprise GLA and one or more recombinant expression constructs each comprising a promoter operably linked to a nucleic acid sequence encoding the antigen against which elicitation or enhancement of an immune response ⁇ e.g., an antigen-specific response) in the subject is desired.
- GLA toll-like receptor
- GLA is a chemically synthesized adjuvant it can be prepared in substantially homogeneous form, which refers to a GLA preparation that is at least 80%, preferably at least 85%, more preferably at least 90%, more preferably at least 95% and still more preferably at least 96%, 97%, 98% or 99% pure with respect to the GLA molecule.
- GLA compounds of the present invention have the following formula (I):
- L 1 , L 2 , L 3 , L 4 , L 5 and L 6 are the same or different and independently -O-, -NH- or -(CH 2 )-;
- Y 2 and Y 3 are the same or different and independently -OH, -SH, or an acid functional group
- Y 4 is -OH or -SH
- Ri, R 3 , R 5 and R 6 are the same or different and independently C 8- 13 alkyl
- R 2 and R 4 are the same or different and independently C 6- n alkyl.
- Alkyl means a straight chain or branched, noncyclic or cyclic, unsaturated or saturated aliphatic hydrocarbon containing from 1 to 20 carbon atoms, and in certain preferred embodiments containing from 11 to 20 carbon atoms.
- saturated straight chain alkyls include methyl, ethyl, n- propyl, n-butyl, n-pentyl, n-hexyl, and the like, including undecyl, dodecyl, tridecyl, tetradecyl, pentadecyl, hexadecyl, heptadecyl, octadecyl, etc.; while saturated branched alkyls include isopropyl, sec-butyl, isobutyl, tert-butyl, isopentyl, and the like.
- saturated cyclic alkyls include cyclopropyl, cyclobutyl, cyclopentyl, cyclohexyl, and the like; while unsaturated cyclic alkyls include cyclopentenyl and cyclohexenyl, and the like.
- Cyclic alkyls are also referred to herein as “homocycles” or “homocyclic rings.”
- Unsaturated alkyls contain at least one double or triple bond between adjacent carbon atoms (referred to as an "alkenyl” or “alkynyl”, respectively).
- Representative straight chain and branched alkenyls include ethylenyl, propylenyl, 1 -butenyl, 2-butenyl, isobutylenyl, 1 -pentenyl, 2-pentenyl, 3-methyl-1 -butenyl, 2-methyl-2-butenyl, 2,3-dimethyl-2-butenyl, and the like; while representative straight chain and branched alkynyls include acetylenyl, propynyl, 1-butynyl, 2-butynyl, 1 -pentynyl, 2-pentynyl, 3-methyl-1 -butynyl, and the like.
- C 8 -i 3 alkyl and “C 6 -nalkyl” mean an alkyl as defined above, containing from 8-13 or 6-11 carbon atoms, respectively.
- Acid functional group means a functional group capable of donating a proton in aqueous media (i.e. a Br ⁇ nsted-Lowry acid). After donating a proton, the acid functional group becomes a negatively charged species (i.e. the conjugate base of the acid functional group).
- the present invention provides GLA compounds of formula (II), wherein Ri, R 3 , R 5 and Re are each C x alkyl, where x is constant and is selected from an integer from 8-13, and R2 and R 4 are both C x- 2 alkyl, and the GLA compounds have the following formula (III):
- the present invention provides GLA compounds of formula (III), wherein x is selected from an integer from 10-12. In other more specific embodiments, the present invention provides GLA compounds of formula (III), wherein x is 11 , and the GLA compounds have the following structure (IV):
- the invention provides GLA compounds of formula (II), wherein Li and L 3 are both -O- and L 2 and L 4 are both -NH-, and the GLA compounds have the following formula (Vl):
- the invention provides GLA compounds of formula (II), wherein Y 1 is -OP(O)(OH) 2 , Y2, Y3 and Y 4 are each OH, L 1 and L 3 are both -O-, and L 2 and L 4 are both -NH-, and the GLA compounds have the following formula (VII):
- the present invention provides GLA compounds of formula (II), wherein Y 1 is -OP(O)(OH) 2 , Y 2 , Y 3 and Y 4 are each -OH, L 1 and L 3 are both -O-, L 2 and L 4 are both -NH-, R 1 , R 3 , R 5 and R 6 each are C x alkyl where x is constant and is selected from an integer from 8-13, and R2 and R 4 are both C x- 2 alkyl, and the GLA compounds have the following formula (VIII):
- the present invention provides GLA compounds.
- the GLA compounds of the present invention may be prepared by known organic synthesis techniques, including the methods described in more detail in the Examples.
- the GLA compounds of structure (I) may be prepared by the following Reaction Schemes, wherein all substituents are as defined above unless indicated otherwise. Reaction Scheme 1
- the sugar backbone of representative GLA compounds can be prepared generally according to Reaction Scheme 1 , wherein d, G 2 , G 3 , G 4 , G 5 , G 6 , G 7 , G 8 , G 9 , and G 10 are either the same or different and independently an appropriate protecting group or hydrogen.
- An appropriate sugar, such as (i) can be purchased or prepared according to methods known to those skilled in the art.
- the functional groups of sugar (i) can then be fully protected using methods known to those skilled in the art to obtain (ii).
- an appropriate orthogonal protecting group strategy which allows for selective deprotection of the sugar functional groups may be employed.
- Suitable protecting groups include, but are not limited to silylethers, benzyl ethers, allyloxycarbonyl, acetals, Fmoc, azide, and the like. Deprotection of Gi results in free alcohol (iii) which can then be coupled with protected sugar (iv) using appropriate coupling conditions, for example CCIsCN/NaH, to obtain the desired sugar backbone (v).
- Acid compounds of structure (vi) can be purchased or prepared according to methods known to those skilled in the art. Reaction of (vi) with an appropriate reagent, such as methyl hydrogen malonate, yields ketoester (vii). Reduction of (vii) yields alcohol (viii). One skilled in the art will recognize that under appropriate conditions the keto group of (vii) may be reduced stereospecifically as exemplified in the Examples. Saponification of (viii) yields acid (ix) which can be subsequently protected to yield (x).
- GLA compounds can be prepared generally according to Reaction Scheme 3, wherein G12 and G13 are the same or different and independently represent an appropriate protecting group. Removal of the G 5 protecting group of (v) followed by reaction with acid chloride (xiv) produces (xv). Similarly, removal of theGs protecting group from (xv) followed by reaction with acid chloride (xvi) results in (xvii). Deprotection of (xvii) and reaction with acid chloride (xviii) yields (xix). Removal of G 9 and reaction with (xx) then produces the protected GLA compound (xxi). Global deprotection of (xxi) results in a compound of structure (II).
- Reaction Scheme 3 depicts the synthesis of a compound of structure (II), one skilled in the art will recognize that analogous methods may be employed to produce any compound of structure (I). In addition, one skilled in the art will also recognize that with selection of the appropriate protecting groups, the final deprotection results in the desired compound.
- the compounds of the present invention may generally be utilized as the free base or free acid. Alternatively, the compounds of this invention may be used in the form of acid or base addition salts. Acid addition salts of the free amino compounds of the present invention may be prepared by methods well known in the art, and may be formed from organic and inorganic acids. Suitable organic acids include maleic, fumaric, benzoic, ascorbic, succinic, methanesulfonic, acetic, oxalic, propionic, tartaric, salicylic, citric, gluconic, lactic, mandelic, cinnamic, aspartic, stearic, palmitic, glycolic, glutamic, and benzenesulfonic acids. Suitable inorganic acids include hydrochloric, hydrobromic, sulfuric, phosphoric, and nitric acids.
- base addition salts of the acid compounds of the present invention may be prepared by methods well known in the art, and may be formed from organic and inorganic bases.
- Suitable organic bases include, but are not limited to, thethylamine and pyridine.
- Suitable inorganic bases include, but are not limited to, sodium hydroxide, potassium hydroxide, sodium carbonate, potassium carbonate, and ammonia.
- pharmaceutically acceptable salt of structure (I) is intended to encompass any and all acceptable salt forms.
- prodrugs are also included within the context of this invention.
- Prodrugs are any covalently bonded carriers that release a compound of structure (I) in vivo when such prodrug is administered to a patient.
- Prodrugs are generally prepared by modifying functional groups in a way such that the modification is cleaved, either by routine manipulation or in vivo, yielding the parent compound.
- Prodrugs include, for example, compounds of this invention wherein hydroxy, amine or sulfhydryl groups are bonded to any group that, when administered to a patient, cleaves to form the hydroxy, amine or sulfhydryl groups.
- prodrugs include (but are not limited to) acetate, formate and benzoate derivatives of alcohol and amine functional groups of the compounds of structure (I).
- esters may be employed, such as methyl esters, ethyl esters, and the like.
- the compounds of structure (I) may have chiral centers and may occur as racemates, racemic mixtures and as individual enantiomers or diastereomers. All such isomeric forms are included within the present invention, including mixtures thereof. Furthermore, some of the crystalline forms of the compounds of structure (I) may exist as polymorphs, which are included in the present invention. In addition, some of the compounds of structure (I) may also form solvates with water or other organic solvents. Such solvates are similarly included within the scope of this invention.
- an antigen for use in certain embodiments of the herein described vaccine compositions and methods employing GLA, may be any target epitope, molecule (including a biomolecule), molecular complex (including molecular complexes that contain biomolecules), subcellular assembly, cell or tissue against which elicitation or enhancement of immunreactivity in a subject is desired.
- the term antigen will refer to a polypeptide antigen of interest.
- antigen as used herein, may also refer to a recombinant construct which encodes a polypeptide antigen of interest (e.g, an expression construct).
- the antigen may be, or may be derived from, or may be immunologically cross- reactive with, an infectious pathogen and/or an epitope, biomolecule, cell or tissue that is associated with infection, cancer, autoimmune disease, allergy, asthma, or any other condition where stimulation of an antigen-specific immune response would be desirable or beneficial.
- the vaccine formulations of the present invention contain an antigen or antigenic composition capable of eliciting an immune response against a human or other mammalian pathogen, which antigen or antigenic composition may include a composition derived from a virus such as from HIV-1 , (such as tat, nef, gp120 or gp160), human herpes viruses, such as gD or derivatives thereof or Immediate Early protein such as ICP27 from HSV1 or HSV2, cytomegalovirus ((esp.
- hepatitis virus such as hepatitis B virus (for example Hepatitis B Surface antigen or a derivative thereof), hepatitis A virus, hepatitis C virus and hepatitis E virus, or from other viral pathogens, such as paramyxoviruses: Respiratory Syncytial virus (such as F and G proteins or derivatives thereof), parainfluenza virus, measles virus, mumps virus, human papilloma viruses (for example HPV6, 11 , 16, 18, etc.), flaviviruses ⁇ e.g., Yellow Fever Virus, Dengue Virus, Tick-borne encephalitis virus, Japanese Encephalitis Virus) or Influenza virus (whole live or inactivated virus
- the vaccine formulations of the present invention contain an antigen or antigenic composition capable of eliciting an immune response against a human or other mammlian pathogen, which antigen or antigenic composition may include a composition derived from one or more bacterial pathogens such as Neisseria spp, including N. gonorrhea and N. meningitidis (for example capsular polysaccharides and conjugates thereof, transferrin-binding proteins, lactoferhn binding proteins, PiIC, adhesins); S. pyogenes (for example M proteins or fragments thereof, C5A protease, lipoteichoic acids), S. agalactiae, S. mutans: H.
- Neisseria spp including N. gonorrhea and N. meningitidis
- S. pyogenes for example M proteins or fragments thereof, C5A protease, lipoteichoic acids
- Moraxella spp including M catarrhalis, also known as Branhamella catarrhalis (for example high and low molecular weight adhesins and invasins); Bordetella spp, including B. pertussis (for example pertactin, pertussis toxin or derivatives thereof, filamentous hemagglutinin, adenylate cyclase, fimbriae), B. parapertussis and B. bronchiseptica; Mycobacterium spp., including M. tuberculosis (for example ESAT6, Antigen 85A, -B or -C), M. bovis, M. leprae, M. avium, M.
- M. tuberculosis for example ESAT6, Antigen 85A, -B or -C
- paratuberculosis M. smegmatis; Legionella spp, including L. pneumophila; Escherichia spp, including enterotoxic E. coli (for example colonization factors, heat-labile toxin or derivatives thereof, heat-stable toxin or derivatives thereof), enterohemorragic E. coli, enteropathogenic E. coli (for example Shiga toxin-like toxin or derivatives thereof); Vibrio spp, including V. cholera (for example cholera toxin or derivatives thereof); Shigella spp, including S. sonnei, S. dysenteriae, S. flexnerii; Yersinia spp, including Y.
- enterotoxic E. coli for example colonization factors, heat-labile toxin or derivatives thereof, heat-stable toxin or derivatives thereof
- enterohemorragic E. coli enteropathogenic E. coli
- Vibrio spp including V
- enterocolitica for example a Yop protein
- Y. pestis for example a Yop protein
- Campylobacter spp including C. jejuni (for example toxins, adhesins and invasins) and C. coli
- Salmonella spp including S. typhi, S. paratyphi, S. choleraesuis, S. enteritidis
- Listeria spp. including L. monocytogenes
- Helicobacter spp including H. pylori (for example urease, catalase, vacuolating toxin); Pseudomonas spp, including P.
- Clostridium spp. including C. tetani (for example tetanus toxin and derivative thereof), C. botulinum (for example botulinum toxin and derivative thereof), C. difficile (for example Clostridium toxins A or B and derivatives thereof); Bacillus spp., including B. anthracis (for example botulinum toxin and derivatives thereof); Corynebacterium spp., including C.
- diphtheriae for example diphtheria toxin and derivatives thereof
- Borrelia spp. including B. burgdorferi (for example OspA, OspC, DbpA, DbpB), B. garinii (for example OspA, OspC, DbpA, DbpB), B. afzelii (for example OspA, OspC, DbpA, DbpB), B. andersonii (for example OspA, OspC, DbpA, DbpB), B. hermsii; Ehrlichia spp., including E. equi and the agent of the Human Granulocytic Ehrlichiosis;
- Rickettsia spp including R. rickettsii; Chlamydia spp. including C. trachomatis (for example MOMP, heparin-binding proteins), C. pneumoniae (for example MOMP, heparin-binding proteins), C. psittaci; Leptospira spp., including L. interrogans; Treponema spp., including T. pallidum (for example the rare outer membrane proteins), T. denticola, T. hyodysenteriae; or other bacterial pathogens.
- C. trachomatis for example MOMP, heparin-binding proteins
- C. pneumoniae for example MOMP, heparin-binding proteins
- C. psittaci Leptospira spp., including L. interrogans
- Treponema spp. including T. pallidum (for example the rare outer membrane proteins), T. denticola, T. h
- the vaccine formulations of the present invention contain an antigen or antigenic composition capable of eliciting an immune response against a human or other mammalian pathogen, which antigen or antigenic composition may include a composition derived from one or more parasites (See, e.g., John, DT. and Petri, W.A., Markell and Voge's Medical Parasitology-9 th Ed., 2006, WB Saunders, Philadelphia; Bowman, D. D., Georgis' Parasitology for Veterinarians- ⁇ Ed., 2002, WB Saunders, Philadelphia) such as Plasmodium spp., including P. falciparum; Toxoplasma spp., including T.
- parasites See, e.g., John, DT. and Petri, W.A., Markell and Voge's Medical Parasitology-9 th Ed., 2006, WB Saunders, Philadelphia; Bowman, D. D., Georgis' Parasitology for Veterinarians- ⁇
- gondii for example SAG2, SAG3, Tg34
- Entamoeba spp. including E. histolytica
- Babesia spp. including B. microti
- Trypanosoma spp. including T. cruzi
- Giardia spp. including G. lamblia
- Leishmania spp. including L. major
- Pneumocystis spp. including P.
- nematode infections including, but not limited to, Enterobius vermicularis, Ascaris lumbricoides, Trichuris trichuria, Necator americanus, Ancylostoma duodenale, Wuchereria bancrofti, Brugia malayi, Onchocerca volvulus, Dracanculus medinensis, Trichinella spiralis, and Strongyloides stercoralis
- trematode infections including, but not limited to, Schistosoma mansoni, Schistosoma haematobium, Schistosoma japonicum, Schistosoma mekongi, Opistorchis sinensis, Paragonimus sp, Fasciola hepatica, Fasciola magna, Fasciola gigantic
- Certain embodiments may therefore contemplate vaccine compositions that include an antigen derived from Schisostoma spp., Schistosoma mansonii, Schistosoma haematobium, and/or Schistosoma japonicum, or derived from yeast such as Candida spp., including C. albicans; Cryptococcus spp., including C. neoformans.
- M. tuberculosis preferred specific antigens for M. tuberculosis are for example Th Ra12, Tb H9, Tb Ra35, Tb38-1 , Erd 14, DPV, MTI, MSL, mTTC2 and hTCC1 (WO 99/51748).
- Proteins for M. tuberculosis also include fusion proteins and variants thereof where at least two, preferably three polypeptides of M. tuberculosis are fused into a larger protein.
- Preferred fusions include Ra12-TbH9-Ra35, Erd14-DPV-MTI, DPV-MTI-MSL, Erd14DPV-MTI-MSL- mTCC2, Erd14-DPV-MTI-MSL, DPV-MTI-MSL-mTCC2, TbH9-DPV-MTI (WO 99151748).
- Chlamydia include for example the High Molecular Weight Protein (HWMP) (WO 99/17741 ), ORF3 (EP 366 412), CT622, CT610, pmpD, UVEB and putative membrane proteins (Pmps).
- HWMP High Molecular Weight Protein
- ORF3 EP 366 412
- CT622 CT610
- pmpD UVEB
- Pmps putative membrane proteins
- Other Chlamydia antigens of the vaccine formulation can be selected from the group described in WO 99128475.
- Preferred bacterial vaccines comprise antigens derived from Streptococcus spp, including S.
- pneumoniae for example capsular polysaccharides and conjugates thereof, PsaA, PspA, PdB, streptolysin, choline-binding proteins
- Pneumolysin Biochem Biophys Acta, 1989, 67, 1007; Rubins et al., Microbial Pathogenesis, 25, 337-342
- mutant detoxified derivatives thereof WO 90/06951 ; WO 99/03884
- Other preferred bacterial vaccines comprise antigens derived from Haemophilus spp., including H. influenzae type B (for example PRP and conjugates thereof), nontypeable H.
- influenzae for example OMP26, high molecular weight adhesins, P5, P6, protein D and lipoprotein D, and fimbrin and fimbrin derived peptides (U.S. Pat. No. 5,843,464) or multiple copy variants or fusion proteins thereof.
- the vaccine formulation of the invention comprises the HIV-1 antigen, gp120, especially when expressed in CHO cells.
- the vaccine formulation of the invention comprises gD2t as hereinabove defined.
- vaccines containing the claimed adjuvant comprise antigen derived from the Human Papilloma Virus (HPV) considered to be responsible for genital warts (HPV 6 or HPV 11 and others), and the HPV viruses responsible for cervical cancer (HPV16, HPV18 and others).
- HPV Human Papilloma Virus
- Particularly preferred forms of genital wart prophylactic, or therapeutic, vaccine comprise L1 particles or capsomers, and fusion proteins comprising one or more antigens selected from the HPV 6 and HPV 11 proteins E6, E7, L1 , and L2.
- fusion protein include L2E7 as disclosed in WO 96/26277, and proteinD(1/3)-E7 disclosed in GB 9717953.5 (PCT/EP98/05285).
- a preferred HPV cervical infection or cancer, prophylaxis or therapeutic vaccine, composition may comprise HPV 16 or 18 antigens.
- VLP virus like particle
- Such antigens, virus like particles and capsomer are perse known. See for example WO94/00152, WO94/20137, WO94/05792, and WO93/02184.
- Additional early proteins may be included alone or as fusion proteins such as E7, E2 or preferably F5 for example; particularly preferred embodiments include a VLP comprising L1 E7 fusion proteins (WO 96/11272).
- Particularly preferred HPV 16 antigens comprise the early proteins E6 or F7 in fusion with a protein D carrier to form Protein D-E6 or E7 fusions from HPV 16, or combinations thereof; or combinations of E6 or E7 with L2 (WO 96/26277).
- the HPV 16 or 18 early proteins E6 and E7 may be presented in a single molecule, preferably a Protein D-E6/E7 fusion.
- Such vaccine may optionally contain either or both E6 and E7 proteins front HPV 18, preferably in the form of a Protein D-E6 or Protein D-E7 fusion protein or Protein D E6/E7 fusion protein.
- the vaccine of the present invention may additionally comprise antigens from other HPV strains, preferably from strains HPV 31 or 33.
- Vaccines of the present invention further comprise antigens derived from parasites that cause Malaria.
- preferred antigens from Plasmodia falciparum include RTS 1 S and TRAP.
- RTS is a hybrid protein comprising substantially all the C-terminal portion of the circumsporozoite (CS) protein of P.falciparum linked via four amino acids of the preS2 portion of Hepatitis B surface antigen to the surface (S) antigen of hepatitis B virus. Its full structure is disclosed in the International Patent Application No. PCT/EP92/02591 , published as WO 93/10152 claiming priority from UK patent application No.9124390.7. When expressed in yeast RTS is produced as a lipoprotein particle, and when it is co-expressed with the S antigen from HBV it produces a mixed particle known as RTS 1 S.
- TRAP antigens are described in the International Patent Application No. PCT/GB89/00895 published as WO 90/01496.
- a preferred embodiment of the present invention is a Malaria vaccine wherein the antigenic preparation comprises a combination of the RTS 1 S and TRAP antigens.
- Other Plasmodia antigens that are likely candidates to be components of a multistage Malaria vaccine are P.
- an antigen that is derived from at least one infectious pathogen such as a bacterium, a virus or a fungus, including an Actinobacterium such as M. tuberculosis or M. leprae or another mycobacterium; a bacterium such as a member of the genus Salmonella, Neisseria, Borrelia, Chlamydia or Bordetella; a virus such as a herpes simplex virus, a human immunodeficiency virus (HIV), a feline immunodeficiency virus (FIV), cytomegalovirus, Varicella Zoster Virus, hepatitis virus, Epstein Barr Virus (EBV), respiratory syncytial virus, human papilloma virus (HPV) and a cytomegalovirus; HIV such as HIV-1 or HIV-2; a fungus such as Aspergillus, Blastomyces, Coccidioides and Pneumocysti or another mycobacterium; a bacter
- a parasite such as a protozoan, for example, a Plasmodium species including P. falciparum, P. vivax, P. malariae and P.
- ovale or another parasite such as one or more of Acanthamoeba, Entamoeba histolytica, Angiostrongylus, Schistosoma mansonii, Schistosoma haematobium, Schistosoma japonicum, Cryptosporidium, Ancylostoma, Entamoeba histolytica, Entamoeba coli, Entamoeba dispar, Entamoeba hartmanni, Entamoeba polecki, Wuchereria bancrofti, Giardia, and Leishmania.
- another parasite such as one or more of Acanthamoeba, Entamoeba histolytica, Angiostrongylus, Schistosoma mansonii, Schistosoma haematobium, Schistosoma japonicum, Cryptosporidium, Ancylostoma, Entamoeba histolytica, Entamoeba coli, Entamoeba dispar, Entam
- the antigens may include nucleic acid, pathogen derived antigen or antigenic preparations, recombinantly produced protein or peptides, and chimeric fusion proteins.
- One such antigen is OspA.
- the OspA may be a full mature protein in a lipidated form by virtue of its biosynthesis in a host cell (Lipo-OspA) or may alternatively be a non-lipidated derivative.
- non-lipidated derivatives include the non-lipidated NS1 -OspA fusion protein which has the first 81 N-terminal amino acids of the nonstructural protein (NS1 ) of the influenza virus, and the complete OspA protein, and another, MDP-OspA is a non-lipidated form of OspA carrying 3 additional N-terminal amino acids.
- compositions and methods are known in the art for identifying subjects having, or suspected of being at risk for having, an infection with an infectious pathogen as described herein.
- TB tuberculosis
- the bacteria usually attack the lungs but can also attack the kidney, spine, and brain. If not treated properly, TB disease can be fatal. The disease is spread from one person to another in the air when an infected person sneezes or coughs. In 2003, more than 14,000 cases of TB were reported in the United States.
- tuberculosis can generally be controlled using extended antibiotic therapy, such treatment is not sufficient to prevent the spread of the disease and concerns exist regarding the potential selection for antibiotic- resistant strains.
- Infected individuals may be asymptomatic, but contagious, for some time.
- compliance with the treatment regimen is critical, patient behavior is difficult to monitor.
- Some patients do not complete the course of treatment, which can lead to ineffective treatment and the development of drug resistance, (e.g., U.S. Patent 7,087,713)
- BCG Bacillus Calmette-Guehn
- Mycobacterium bovis an avirulent strain of Mycobacterium bovis.
- PPD protein-purified derivative
- T cells While macrophages have been shown to act as the principal effectors of M. tuberculosis immunity, T cells are the predominant inducers of such immunity.
- the essential role of T cells in protection against M. tuberculosis infection is illustrated by the frequent occurrence of M. tuberculosis in AIDS patients, due to the depletion of CD4 T cells associated with human immunodeficiency virus (HIV) infection.
- Mycobacterium-reactive CD4 T cells have been shown to be potent producers of gamma-interferon (IFN-gamma), which, in turn, has been shown to trigger the anti-mycobacterial effects of macrophages in mice.
- IFN-gamma gamma-interferon
- IFN-gamma While the role of IFN-gamma in humans is less clear, studies have shown that 1 ,25-dihydroxy-vitamin D3, either alone or in combination with IFN-gamma or tumor necrosis factor-alpha, activates human macrophages to inhibit M. tuberculosis infection. Furthermore, it is known that IFN-gamma stimulates human macrophages to make 1 ,25-dihydroxy-vitamin D3. Similarly, IL-12 has been shown to play a role in stimulating resistance to
- M. tuberculosis infection For a review of the immunology of M. tuberculosis infection, see Chan and Kaufmann, in Tuberculosis: Pathogenesis, Protection and Control, Bloom (ed.), ASM Press. Washington, D.C. (1994).
- Existing compounds and methods for diagnosing tuberculosis or for inducing protective immunity against tuberculosis include the use of polypeptides that contain at least one immunogenic portion of one or more Mycobacterium proteins and DNA molecules encoding such polypeptides. Diagnostic kits containing such polypeptides or DNA sequences and a suitable detection reagent may be used for the detection of Mycobacterium infection in patients and biological samples. Antibodies directed against such polypeptides are also provided. In addition, such compounds may be formulated into vaccines and/or pharmaceutical compositions for immunization against Mycobacterium infection. (U.S. Patent Nos. 6,949,246 and 6,555,653).
- Malaria is usually transmitted when a person is bitten by an infected female Anopheles mosquito. To transmit the mosquito must have been infected by having drawn blood from a person already infected with malaria. Malaria is caused by a parasite and the clinical symptoms of the disease include fever and flu-like illness, such as chills, headache, muscle aches, and tiredness. These symptoms may be accompanied by nausea, vomiting, and diarrhea. Malaria can also cause anemia and jaundice because of the loss of red blood cells. Infection with one type of malaria, Plasmodium falciparum, if not promptly treated, may cause kidney failure, seizures, mental confusion, coma, and death.
- An in vitro diagnostic method for malaria in an individual comprising placing a tissue or a biological fluid taken from an individual in contact with a molecule or polypeptide composition, wherein said molecule or polypeptide composition comprises one or more peptide sequences bearing all or part of one or more T epitopes of the proteins resulting from the infectious activity of P. falciparum, under conditions allowing an in vitro immunological reaction to occur between said composition and the antibodies that may be present in the tissue or biological fluid, and in vitro detection of the antigen- antibody complexes formed (see, e.g., U.S. Patent 7,087,231 ).
- AMA-1 ectodomain a recombinant Plasmodium falciparum (3D7) AMA-1 ectodomain have been described. Previous methods have produced a highly purified protein which retains folding and disulfide bridging of the native molecule.
- the recombinant AMA-1 is useful as a diagnostic reagentas well as in antibody production, and as a protein for use alone, or as part of, a vaccine to prevent malaria. (U.S. Patent 7,029,685)
- Polynucleotides have been described in the art that encode species-specific P. vivax malarial peptide antigens which are proteins or fragments of proteins secreted into the plasma of a susceptible mammalian host after infection, as have monoclonal or polyclonal antibodies directed against these antigens.
- the peptide antigens, monoclonal antibodies, and/or polyclonal antibodies are utilized in assays used to diagnose malaria, as well as to determine whether Plasmodium vivax is the species responsible for the infection. (U.S. Patent 6,706,872) Species-specific P.
- vivax malarial peptide antigens have also been reported which are proteins or fragments of proteins secreted into the plasma of a susceptible mammalian host after infection, as have monoclonal or polyclonal antibodies directed against these antigens.
- the peptide antigens, monoclonal antibodies, and/or polyclonal antibodies are utilized in assays used to diagnose malaria, as well as to determine whether Plasmodium vivax is the species responsible for the infection (see, e.g., U.S. Patent 6,231 ,861 ).
- a recombinant Plasmodium falciparum (3D7) AMA-1 ectodomain has also been expressed by a method that produces a highly purified protein which retains folding and disulfide bridging of the native molecule.
- the recombinant AMA-1 is useful as a diagnostic reagent, for use in antibody production, and as a vaccine.
- U.S. Patent 7,060,276 Similarly known are the expression and purification of a recombinant Plasmodium falciparum (3D7) MSP-1 4 2, which retains folding and disulfide bridging of the native molecule.
- the recombinant MSP-1 4 2 is useful as a diagnostic reagent, for use in antibody production, and as a vaccine.
- U.S. Patent 6,855,322 U.S. Patent 6,855,322
- Diagnostic methods for the detection of human malaria infections to identify a subject having or suspected of being at risk for having an infection with a malaria infectious pathogen are thus known according to these and related disclosures.
- blood samples are combined with a reagent containing 3-acetyl pyridine adenine dinucleotide (APAD), a substrate (e.g. a lactate salt or lactic acid), and a buffer.
- APAD 3-acetyl pyridine adenine dinucleotide
- substrate e.g. a lactate salt or lactic acid
- the reagent is designed to detect the presence of a unique glycolytic enzyme produced by the malaria parasite. This enzyme is known as parasite lactic acid dehydrogenase (PLDH).
- PLDH is readily distinguishable from host LDH using the above- described reagent.
- APAD is not reduced by host LDH.
- the reduced APAD may then be detected by various techniques, including spectral, fluorimetric, electrophoretic, or colorimetric analysis. Detection of the reduced APAD in the foregoing manner provides a positive indication of malaria infection ⁇ e.g., U.S. Patent 5,124,141 ).
- a polypeptide comprising a characteristic amino acid sequence derived from the Plasmodium falciparum antigen GLURP, is recognized in a test sample by a specific antibody raised against or reactive with the polypeptide.
- Leishmaniasis is a widespread parasitic disease with frequent epidemics in the Indian subcontinent, Africa, and Latin America and is a World Health Organization priority for vaccine development.
- a complex of different diseases, Leishmania parasites cause fatal infections of internal organs, as well as serious skin disease.
- One of the most devastating forms of leishmaniasis is a disfiguring infection of the nose and mouth.
- the number of cases of leishmaniasis is increasing, and it is now out of control in many areas.
- Leishmaniasis is also on the rise in some developed countries, specifically southern Europe as a result of HIV infection. Available drugs are toxic, expensive, and require long-term daily injections.
- Leishmania are protozoan parasites that inhabit macrophages or the white blood cells of the immune system.
- the parasites are transmitted by the bite of small blood sucking insects (sand flies), which are difficult to control, as they inhabit vast areas of the planet.
- Visceral leishmaniasis is the most dangerous of the three manifestations of the disease. It is estimated that about 500,000 new cases of the visceral form (kala-azar or "the killing disease") occur each year. More than 200 million people are currently at risk for contracting visceral leishmaniasis. Over 90 percent of visceral leishmaniasis cases occur in India, Bangladesh, Sudan, Brazil, and Nepal. Most of the deaths occur in children. Those with the cutaneous forms are often left permanently disfigured.
- HIV human immunodeficiency virus
- HIV human immunodeficiency virus
- the most robust solution to the problem is preventing the virus from spreading.
- Making a safe, effective, and affordable HIV vaccine is one way to reach this goal. Across the world, fewer than one in five people at high risk for HIV infection have access to effective prevention.
- the vaccine compositions and related formulations and methods of use may include an antigen that is derived from a cancer cell, as may be useful for the immunotherapeutic treatment of cancers.
- the adjuvant formulation may finds utility with tumor rejection antigens such as those for prostate, breast, colorectal, lung, pancreatic, renal or melanoma cancers.
- Exemplary cancer or cancer cell-derived antigens include MAGE 1 , 3 and MAGE 4 or other MAGE antigens such as those disclosed in WO99/40188, PRAME, BAGE, Lü (also known as NY Eos 1 ) SAGE and HAGE (WO 99/53061 ) or GAGE (Robbins and Kawakami, 1996 Current Opinions in Immunology 8, pps 628-636; Van den Eynde et al., International Journal of Clinical & Laboratory Research (1997 & 1998); Correale et al. (1997), Journal of the National Cancer Institute 89, p. 293.
- These non-limiting examples of cancer antigens are expressed in a wide range of tumor types such as melanoma, lung carcinoma, sarcoma and bladder carcinoma. See, e.g., U.S. Patent No. 6,544,518.
- tumor-specific antigens are suitable for use with GLA according to certain presently disclosed embodiments include, but are not restricted to, tumor-specific or tumor-associated gangliosides such as GM 2 , and GM 3 or conjugates thereof to carrier proteins; or an antigen for use in a GLA vaccine composition for eliciting or enhancing an anti-cancer immune response may be a self peptide hormone such as whole length Gonadotrophin hormone releasing hormone (GnRH, WO 95/20600), a short 10 amino acid long peptide, useful in the treatment of many cancers.
- prostate antigens are used, such as Prostate specific antigen (PSA), PAP, PSCA (e.g., Proc. Nat. Acad. Sci.
- PSMA or, in a preferred embodiment an antigen known as Prostase.
- Prostase e.g., Nelson, et al., Proc. Natl. Acad. Sci. USA (1999) 96: 3114-3119; Ferguson, et al. Proc. Natl. Acad. Sci. USA 1999. 96, 3114-3119; WO 98/12302; U.S. Pat. No. 5,955,306; WO 98/20117; U.S. Pat. Nos. 5,840,871 and 5,786,148; WO 00/04149.
- Other prostate specific antigens are known from WO 98/137418, and WO/004149.
- Another is STEAP PNAS 96 14523 14528 7-12 1999).
- tumor associated antigens useful in the context of the present invention include: PIu -1 (J Biol. Chem 21 A (22) 15633 -15645, 1999), HASH -1 , HasH-2, Cripto (Salomon et al Bioessays 199, 21 :61 -70, U.S. Pat. No. 5,654,140) and Criptin (U.S. Pat. No. 5,981 ,215). Additionally, antigens particularly relevant for vaccines in the therapy of cancer also comprise tyrosinase and survivin.
- GLA-containing vaccine compositions comprising a cancer antigen will be useful against any cancer characterized by tumor associated antigen expression, such as HER- 2/neu expression or other cancer-specific or cancer-associated antigens.
- Diagnosis of cancer in a subject having or suspected of being at risk for having cancer may be accomplished by any of a wide range of art- accepted methodologies, which may vary depending on a variety of factors including clinical presentation, degree of progression of the cancer, the type of cancer, and other factors.
- cancer diagnostics include histopathological, histocytochemical, immunohistocytochemical and immunohistopathological examination of patient samples (e.g., blood, skin biopsy, other tissue biopsy, surgical specimens, etc.), PCR tests for defined genetic ⁇ e.g., nucleic acid) markers, serological tests for circulating cancer- associated antigens or cells bearing such antigens, or for antibodies of defined specificity, or other methodologies with which those skilled in the art will be familiar.
- Vaccine compositions and methods according to certain embodiments of the present invention may also be used for the prophylaxis or therapy of autoimmune diseases, which include diseases, conditions or disorders wherein a host's or subject's immune system detrimentally mediates an immune response that is directed against "self tissues, cells, biomolecules (e.g., peptides, polypeptides, proteins, glycoproteins, lipoproteins, proteolipids, lipids, glycolipids, nucleic acids such as RNA and DNA, oligosaccharides, polysaccharides, proteoglycans, glycosaminoglycans, or the like, and other molecular components of the subjects cells and tissues) or epitopes (e.g., specific immunologically defined recognition structures such as those recognized by an antibody variable region complementarity determining region (CDR) or by a T cell receptor CDR.
- autoimmune diseases include diseases, conditions or disorders wherein a host's or subject's immune system detrimentally mediates an immune response that is directed
- Autoimmune diseases are thus characterized by an abnormal immune response involving either cells or antibodies, that are in either case directed against normal autologous tissues.
- Autoimmune diseases in mammals can generally be classified in one of two different categories: cell-mediated disease (i.e., T-cell) or antibody-mediated disorders.
- cell-mediated autoimmune diseases include multiple sclerosis, rheumatoid arthritis, Hashimoto thyroiditis, type I diabetes mellitus (Juvenile onset diabetes) and autoimmune uvoretinitis.
- Antibody-mediated autoimmune disorders include, but are not limited to, myasthenia gravis, systemic lupus erythematosus (or SLE), Graves' disease, autoimmune hemolytic anemia, autoimmune thrombocytopenia, autoimmune asthma, cryoglobulinemia, thrombic thrombocytopenic purpura, primary biliary sclerosis and pernicious anemia.
- the antigen(s) associated with: systemic lupus erythematosus is small nuclear ribonucleic acid proteins (snRNP); Graves' disease is the thyrotropin receptor, thyroglobulin and other components of thyroid epithelial cells (Akamizu et al., 1996; Kellerman et al., 1995; Raju et al., 1997; and Texier et al., 1992); pemphigus is cadherin-like pemphigus antigens such as desmoglein 3 and other adhesion molecules (Memar et al., 1996: Stanley, 1995; Plott et al., 1994; and Hashimoto, 1993); and thrombic thrombocytopenic purpura is antigens of platelets.
- snRNP small nuclear ribonucleic acid proteins
- Graves' disease is the thyrotropin receptor, thyroglobulin and other components of thyroid epitheli
- Autoimmunity plays a role in more than 80 different diseases, including type 1 diabetes, multiple sclerosis, lupus, rheumatoid arthritis, scleroderma, and thyroid diseases. Vigorous quantitative estimates of morbidity for most autoimmune diseases are lacking. Most recent studies done in the late 1990s reveal that autoimmune diseases are the third most common major illness in the United States; and the most common autoimmune diseases affect more than 8.5 million Americans. Current estimates of the prevalence of the disease range from 5 to 8 percent of the United States population. Most autoimmune diseases disproportionately affect women. Women are 2.7 times more likely than men to acquire an autoimmune disease. Women are more susceptible to autoimmune diseases; men appear to have higher levels of natural killer cell activity than do women. (Jacobsen et al, Clinical Immunology and Immunopathology, 84:223-243, 1997.)
- Autoimmune diseases occur when the immune system mistakes self tissues for nonself and mounts an inappropriate attack.
- the body can be affected in different ways from autoimmune diseases, including, for example, the gut (Crohn's disease) and the brain (multiple sclerosis).
- autoimmune diseases including, for example, the gut (Crohn's disease) and the brain (multiple sclerosis).
- an autoantibody attacks self-cells or self-tissues to injure their function and as a result causes autoimmune diseases, and that the autoantibody may be detected in the patient's serum prior to the actual occurrence of an autoimmune disease ⁇ e.g., appearance of clinical signs and symptoms). Detection of an autoantibody thus permits early discovery or recognition of presence or risk for developing an autoimmune disease.
- compositions of the invention will be particularly applicable in treatment of the elderly and/or the immunosuppressed, including subjects on kidney dialysis, subjects on chemo-therapy and/or radiation therapy, transplant recipients, and the like. Such individuals generally exhibit diminished immune responses to vaccines and therefore use of the compositions of the invention can enhance the immune responses achieved in these subjects.
- the antigen or antigens used in the compositions of the invention include antigens associated with respiratory diseases, such as those caused or exacerbated by bacterial infection (e.g. pneumococcal), for the prophylaxis and therapy of conditions such as chronic obstructive pulmonary disease (COPD).
- COPD chronic obstructive pulmonary disease
- COPD is defined physiologically by the presence of irreversible or partially reversible airway obstruction in patients with chronic bronchitis and/or emphysema (Am J Respir Crit Care Med. 1995 Nov;152(5 Pt 2):S77-121 ). Exacerbations of COPD are often caused by bacterial (e.g. pneumococcal) infection (Clin Microbiol Rev. 2001 Apr;14(2):336- 63).
- a composition of the invention comprises a GLA adjuvant, as described herein, in combination with the Pneumococcal vaccine Prevnar ® (Wyeth).
- compositions of the invention are used in the treatment of allergic conditions.
- the compositions are used in allergy desensitization therapy.
- Such therapy involves the stimulation of the immune system with gradually increasing doses of the substances to which a person is allergic, wherein the substances are formulated in compositions comprising GLA.
- the compositions are used in the treatment of allergies to food products, pollen, mites, cats or stinging insects (e.g., bees, hornets, yellow jackets, wasps, velvet ants, fire ants).
- certain embodiments of the present invention contemplate vaccine compositions and immunological adjuvant compositions, including pharmaceutical compositions, that include, in addition to the GLA compound(s) of the invention, one or more toll-like receptor agonist
- TLR agonist Toll-like receptors
- TLR include cell surface transmembrane receptors of the innate immune system that confer early-phase recognition capability to host cells for a variety of conserved microbial molecular structures such as may be present in or on a large number of infectious pathogens, ⁇ e.g., Armant et al., 2002 Genome Biol. 3(8):reviews3011.1-3011.6; Fearon et al., 1996 Science 272:50; Medzhitov et al., 1997 Curr. Opin. Immunol. 9:4; Luster 2002 Curr. Opin. Immunol. 14:129; Lien et al. 2003 Nat. Immunol. 4:1162; Medzhitov, 2001 Nat.
- TLR agonists which engage cell surface TLR.
- lipopolysacchahde may be a TLR agonist through TLR2 or TLR4 (Tsan et al., 2004 J. Leuk. Biol. 76:514; Tsan et al., 2004 Am. J. Physiol. Cell Physiol.
- poly(inosine-cytidine) may be a TLR agonist through TLR3 (Salem et al., 2006 Vaccine 24:5119); CpG sequences (oligodeoxynucleotides containing unmethylated cytosine-guanosine or "CpG" dinucleotide motifs, e.g., CpG 7909, Cooper et al., 2005 AIDS 19:1473; CpG 10101 Bayes et al. Methods Find Exp Clin Pharmacol 27:193; Vollmer et al.
- TLR agonists may be TLR9 (Andaloussi et a., 2006 GHa 54:526; Chen et al., 2006 J. Immunol. 177:2373); peptidoglycans may be TLR2 and/or TLR6 agonists (Soboll et al., 2006 Biol. Reprod. 75:131 ; Nakao et al., 2005 J. Immunol.
- 3M003 (4-amino-2-(ethoxymethyl)- ⁇ , ⁇ -dimethyl- 6,7,8,9-tetrahydro-1 H-imidazo[4,5-c]quinoline-1-ethanol hydrate, MoI. Wt. 318 Da from 3M Pharmaceuticals, St. Paul, MN, which is also a source of the related compounds 3M001 and 3M002; Gorden et al., 2005 J. Immunol. 174:1259) may be a TLR7 agonist (Johansen 2005 CHn. Exp. Allerg. 35:1591 ) and/or a TLR8 agonist (Johansen 2005); flagellin may be a TLR5 agonist
- TLR7 and/or TLR9 may act as TLR agonists through TLR7 and/or TLR9 (Lee et al., 2006 Proc. Nat. Acad. Sci. USA 103:1828; Horsmans et al., 2005 Hepatol. 42:724).
- Other TLR agonists are known ⁇ e.g., Schirmbeck et al., 2003 J. Immunol. 171 :5198) and may be used according to certain of the presently described embodiments.
- CpG immunostimulatory oligonucleotides containing unmethylated CpG dinucleotides
- CpG immunostimulatory oligonucleotides containing unmethylated CpG dinucleotides
- the central role of the CG motif in immunostimulation was elucidated by Krieg, Nature 374, p546 1995. Detailed analysis has shown that the CG motif has to be in a certain sequence context, and that such sequences are common in bacterial DNA but are rare in vertebrate DNA.
- the immunostimulatory sequence is often: Purine, Purine, C, G, pyhmidine, pyhmidine; wherein the dinucleotide CG motif is not methylated, but other unmethylated CpG sequences are known to be immunostimulatory and may be used in certain embodiments of the present invention.
- CpG when formulated into vaccines may be administered in free solution together with free antigen (WO 96/02555; McCluskie and Davis, supra) or covalently conjugated to an antigen (PCT Publication No. WO 98/16247), or formulated with a carrier such as aluminium hydroxide (e.g., Davis et al. supra, Brazolot-Millan et al., Proc. Natl. Acad. Sci., USA, 1998, 95(26), 15553-8).
- a carrier such as aluminium hydroxide
- the preferred oligonucleotides for use in adjuvants or vaccines of the present invention preferably contain two or more dinucleotide CpG motifs separated by at least three, more preferably at least six or more nucleotides.
- the oligonucleotides of the present invention are typically deoxynucleotides.
- the internucleotide in the oligonucleotide is phosphorodithioate, or more preferably a phosphorothioate bond, although phosphodiester and other internucleotide bonds are within the scope of the invention including oligonucleotides with mixed internucleotide linkages. Methods for producing phosphorothioate oligonucleotides or phosphorodithioate are described in U.S. Pat. Nos. 5,666,153, 5,278,302 and WO95/26204.
- oligonucleotides have sequences that are disclosed in the following publications; for certain herein disclosed embodiments the sequences preferably contain phosphorothioate modified internucleotide linkages:
- CPG 7909 Cooper et al., "CPG 7909 adjuvant improves hepatitis B virus vaccine seroprotection in antiretroviral-treated HIV-infected adults.” AIDS, 2005 Sep 23;19(14):1473-9.
- Alternative CpG oligonucleotides may comprise variants of the preferred sequences described in the above-cited publications that differ in that they have inconsequential nucleotide sequence substitutions, insertions, deletions and/or additions thereto.
- the CpG oligonucleotides utilized in certain embodiments of the present invention may be synthesized by any method known in the art ⁇ e.g., EP 468520). Conveniently, such oligonucleotides may be synthesized utilizing an automated synthesizer.
- the oligonucleotides are typically deoxynucleotides.
- the internucleotide bond in the oligonucleotide is phosphorodithioate, or more preferably phosphorothioate bond, although phosphodiesters are also within the scope of the presently contemplated embodiments.
- Oligonucleotides comprising different internucleotide linkages are also contemplated, e.g., mixed phosphorothioate phosphodiesters.
- Other internucleotide bonds which stabilize the oligonucleotide may also be used.
- Certain embodiments as provided herein include vaccine compositions and immunological adjuvant compositions, including pharmaceutical compositions, that contain, in addition to GLA compound(s), at least one co-adjuvant, which refers to a component of such compositions that has adjuvant activity but that is other than GLA.
- a co-adjuvant having such adjuvant activity includes a composition that, when administered to a subject such as a human (e.g., a human patient), a non-human primate, a mammal or another higher eukaryotic organism having a recognized immune system, is capable of altering (i.e., increasing or decreasing in a statistically significant manner, and in certain preferred embodiments, enhancing or increasing) the potency and/or longevity of an immune response.
- GLA and a desired antigen, and optionally one or more co-adjuvants may so alter, e.g., elicit or enhance, an immune response that is directed against the desired antigen which may be administered at the same time as GLA or may be separated in time and/or space (e.g., at a different anatomic site) in its administration, but certain invention embodiments are not intended to be so limited and thus also contemplate administration of GLA in a composition that does not include a specified antigen but which may also include one or more of a TLR agonist, a co-adjuvant, an imidazoquinline immune response modifier, and a double stem loop immune modifier (dSLIM).
- dSLIM double stem loop immune modifier
- co-adjuvants include compositions other than GLA that have adjuvant effects, such as saponins and saponin mimetics, including QS21 and QS21 mimetics (see, e.g., U.S. Pat. No.
- alum plant alkaloids such as tomatine, detergents such as (but not limited to) saponin, polysorbate 80, Span 85 and stearyl tyrosine, one or more cytokines (e.g., GM-CSF, IL-2, IL-7, IL-12, TNF-alpha, IFN-gamma), an imidazoquinoline immune response modifier, and a double stem loop immune modifier (dSLIM, e.g., Weeratna et al., 2005 Vaccine 23:5263).
- cytokines e.g., GM-CSF, IL-2, IL-7, IL-12, TNF-alpha, IFN-gamma
- dSLIM double stem loop immune modifier
- Detergents including saponins are taught in, e.g., U.S. Patent 6,544,518; Lacaille-Dubois, M and Wagner H. (1996 Phytomedicine 2:363-386), U.S. Pat. No. 5,057,540 , Kensil, Crit Rev Ther Drug Carrier Syst, 1996, 12 (1 - 2):1 -55, and EP 0 362 279 B1.
- Particulate structures termed Immune Stimulating Complexes (ISCOMS), comprising fractions of Quil A (saponin) are haemolytic and have been used in the manufacture of vaccines (Morein, B., EP 0 109 942 B1 ).
- Combinations of QS21 and polysorbate or cyclodextrin are also known (WO 99/10008).
- Particulate adjuvant systems comprising fractions of QuilA, such as QS21 and QS7 are described in WO 96/33739 and WO 96/11711.
- Other saponins which have been used in systemic vaccination studies include those derived from other plant species such as Gypsophila and Saponaria (Bomford et al., Vaccine, 10(9):572-577, 1992).
- Escin is another detergent related to the saponins for use in the adjuvant compositions of the embodiments herein disclosed. Escin is described in the Merck index (12 th Ed.: entry 3737) as a mixture of saponin occurring in the seed of the horse chestnut tree, Aesculus hippocastanum. Its isolation is described by chromatography and purification (Fiedler, Arzneistoff- Forsch. 4, 213 (1953)), and by ion-exchange resins (Erbring et al., U.S. Pat. No. 3,238,190). Fractions of escin (also known as aescin) have been purified and shown to be biologically active (Yoshikawa M, et al.
- Digitonin is another detergent, also being described in the Merck index (12th Ed., entry 3204) as a saponin, being derived from the seeds of Digitalis purpurea and purified according to the procedure described by Gisvold et al., J. Am. Pharm.Assoc, 1934, 23, 664; and Rubenstroth-Bauer, Physiol. Chem., 1955, 301 , 621.
- co-adjuvants for use according to certain herein disclosed embodiments include a block co-polymer or biodegradable polymer, which refers to a class of polymeric compounds with which those in the relevant art will be familiar.
- a block co-polymer or biodegradable polymer that may be included in a GLA vaccine composition or a GLA immunological adjuvant include Pluronic® L121 (BASF Corp., Mount Olive, NJ; see, e.g., Yeh et al., 1996 Pharm. Res. 13:1693; U.S. Patent No. 5,565,209), CRL1005 ⁇ e.g., Triozzi et al., 1997 Clin Cane. Res.
- poly(lactic-co-glycolic acid) PLGA
- poly(lactic acid) PLA
- poly-(D,L-lactide-co-glycolide) PLA
- polyl:C poly(See, e.g., Powell and Newman, "Vaccine design - The Subunit and Adjuvant Approach", 1995, Plenum Press, New York)
- Certain embodiments contemplate GLA vaccines and GLA immunological adjuvants that include an oil, which in some such embodiments may contribute co-adjuvant activity and in other such embodiments may additionally or alternatively provide a pharmaceutically acceptable carrier or excipient.
- oils Any number of suitable oils are known and may be selected for inclusion in vaccine compositions and immunological adjuvant compositions based on the present disclosure. Examples of such oils, by way of illustration and not limitation, include squalene, squalane, mineral oil, olive oil, cholesterol, and a mannide monooleate.
- Immune response modifiers such as imidazoquinoline immune response modifiers are also known in the art and may also be included as co- adjuvants in certain presently disclosed embodiments.
- Certain preferred imidazoquinoline immune response modifiers include, by way of non-limiting example, resiquimod (R848), imiquimod and gardiquimod (Hemmi et al., 2002 Nat. Immunol. 3:196; Gibson et al., 2002 Cell. Immunol. 218:74; Gorden et al.,
- dSLIM nucleic acid-based double stem loop immune modifiers
- one type of co-adjuvant for use with GLA as described herein may be the aluminum co-adjuvants, which are generally referred to as "alum.”
- Alum co-adjuvants are based on the following: aluminum oxy-hydroxide; aluminum hydroxyphosphoate; or various proprietary salts.
- Vaccines that use alum co-adjuvants may include vaccines for tetanus strains, HPV, hepatitis A, inactivated polio virus, and other antigens as described herein.
- Alum co-adjuvants are advantageous because they have a good safety record, augment antibody responses, stabilize antigens, and are relatively simple for large-scale production. (Edelman 2002 MoI. Biotechnol. 21 :129-148; Edelman, R. 1980 Rev. Infect. Dis. 2:370-383.)
- co-adjuvants that may be combined with GLA for effective immune stimulation include saponins and saponin mimetics, including QS21 and structurally related compounds conferring similar effects and referred to herein as QS21 mimetics.
- QS21 has been recognized as a preferred co- adjuvant.
- QS21 may comprise an HPLC purified non-toxic fraction derived from the bark of Quillaja Saponaria Molina. The production of QS21 is disclosed in U.S. Pat. No. 5,057,540. (See also U.S. Patent Nos. 6,936,255, 7,029,678 and 6,932,972.)
- GLA may also in certain embodiments be combined with "immunostimulatory complexes" known as ISCOMS (e.g., U.S. Patent Nos. 6,869,607, 6,846,489, 6,027,732, 4,981 ,684), including saponin-derived ISCOMATRIX®, which is commercially available, for example, from lscotec (Stockholm, Sweden) and CSL Ltd. (Parkville, Victoria, Australia).
- ISCOMS immunosys
- saponin-derived ISCOMATRIX® which is commercially available, for example, from lscotec (Stockholm, Sweden) and CSL Ltd. (Parkville, Victoria, Australia).
- the GLA vaccine composition may contain at least one recombinant expression construct which comprises a promoter operably linked to a nucleic acid sequence encoding an antigen.
- the recombinant expression construct is present in a viral vector, such as an adenovirus, adeno-associated virus, herpesvirus, lentivirus, poxvirus or retrovirus vector.
- a viral vector such as an adenovirus, adeno-associated virus, herpesvirus, lentivirus, poxvirus or retrovirus vector.
- Compositions and methods for making and using such expression constructs and vectors are known in the art, for the expression of polypeptide antigens as provided herein, for example, according to Ausubel et al. (Eds.), Current Protocols in Molecular Biology, 2006 John Wiley & Sons, NY.
- Non-limiting examples of recombinant expression constructs generally can be found, for instance, in U.S. Patent Nos. 6,844,192; 7,037,712; 7,052,904; 7,001 ,770; 6,106,824; 5,693,531 ; 6,613,892; 6,875,610; 7,067,310; 6,218,186; 6,783,981 ; 7,052,904; 6,783,981 ; 6,734,172; 6,713,068; 5,795,577 and 6,770,445 and elsewhere, with teachings that can be adapted to the expression of polypeptide antigens as provided herein, for use in certain presently disclosed embodiments.
- compositions for altering i.e., increasing or decreasing in a statistically significant manner, for example, relative to an appropriate control as will be familiar to persons skilled in the art
- an immune response may be any active alteration of the immune status of a host, which may include any alteration in the structure or function of one or more tissues, organs, cells or molecules that participate in maintenance and/or regulation of host immune status.
- immune responses may be detected by any of a variety of well known parameters, including but not limited to in vivo or in vitro determination of: soluble immunoglobulins or antibodies; soluble mediators such as cytokines, lymphokines, chemokines, hormones, growth factors and the like as well as other soluble small peptide, carbohydrate, nucleotide and/or lipid mediators; cellular activation state changes as determined by altered functional or structural properties of cells of the immune system, for example cell proliferation, altered motility, induction of specialized activities such as specific gene expression or cytolytic behavior; cellular differentiation by cells of the immune system, including altered surface antigen expression profiles or the onset of apoptosis (programmed cell death); or any other criterion by which the presence of an immune response may be detected.
- soluble immunoglobulins or antibodies soluble mediators such as cytokines, lymphokines, chemokines, hormones, growth factors and the like as well as other soluble small peptide, carbohydrate, nu
- Immune responses may often be regarded, for instance, as discrimination between self and non-self structures by the cells and tissues of a host's immune system at the molecular and cellular levels, but the invention should not be so limited.
- immune responses may also include immune system state changes that result from immune recognition of self molecules, cells or tissues, as may accompany any number of normal conditions such as typical regulation of immune system components, or as may be present in pathological conditions such as the inappropriate autoimmune responses observed in autoimmune and degenerative diseases.
- immune responses may also include suppression, attenuation or any other down-regulation of detectable immunity, which may be the consequence of the antigen selected, the route of antigen administration, specific tolerance induction or other factors.
- Determination of the induction of an immune response by the vaccines of the present invention may be established by any of a number of well known immunological assays with which those having ordinary skill in the art will be readily familiar.
- assays include, but need not be limited to, to in vivo or in vitro determination of: soluble antibodies; soluble mediators such as cytokines, lymphokines, chemokines, hormones, growth factors and the like as well as other soluble small peptide, carbohydrate, nucleotide and/or lipid mediators; cellular activation state changes as determined by altered functional or structural properties of cells of the immune system, for example cell proliferation, altered motility, induction of specialized activities such as specific gene expression or cytolytic behavior; cellular differentiation by cells of the immune system, including altered surface antigen expression profiles or the onset of apoptosis (programmed cell death).
- T cell proliferation can be detected by measuring the rate of DNA synthesis, and antigen specificity can be determined by controlling the stimuli (such as, for example, a specific desired antigen- or a control antigen-pulsed antigen presenting cells) to which candidate antigen-reactive T cells are exposed.
- T cells which have been stimulated to proliferate exhibit an increased rate of DNA synthesis.
- a typical way to measure the rate of DNA synthesis is, for example, by pulse-labeling cultures of T cells with tritiated thymidine, a nucleoside precursor which is incorporated into newly synthesized DNA.
- the amount of tritiated thymidine incorporated can be determined using a liquid scintillation spectrophotometer.
- Other ways to detect T cell proliferation include measuring increases in interleukin-2 (IL-2) production, Ca 2+ flux, or dye uptake, such as 3- (4,5-dimethylthiazol-2-yl)-2,5-diphenyl-tetrazolium.
- IL-2 interleukin-2
- dye uptake such as 3- (4,5-dimethylthiazol-2-yl)-2,5-diphenyl-tetrazolium.
- lymphokines such as interferon-gamma
- the relative number of T cells that can respond to a particular antigen may be quantified.
- Detection of antigen-specific antibody production may be achieved, for example, by assaying a sample (e.g., an immunoglobulin containing sample such as serum, plasma or blood) from a host treated with a vaccine according to the present invention using in vitro methodologies such as radioimmunoassay (RIA), enzyme linked immunosorbent assays (ELISA), equilibrium dialysis or solid phase immunoblotting including Western blotting.
- a sample e.g., an immunoglobulin containing sample such as serum, plasma or blood
- ELISA enzyme linked immunosorbent assays
- equilibrium dialysis solid phase immunoblotting including Western blotting.
- solid phase immunoblotting including Western blotting.
- Elaboration of soluble mediators may also be readily determined by enzyme-linked immunosorbent assay (ELISA), for example, using methods, apparatus and reagents that are readily available from commercial sources (e.g., Sigma, St. Louis, MO; see also R & D Systems 2006 Catalog, R & D Systems, Minneapolis, MN).
- ELISA enzyme-linked immunosorbent assay
- any number of other immunological parameters may be monitored using routine assays that are well known in the art. These may include, for example, antibody dependent cell-mediated cytotoxicity (ADCC) assays, secondary in vitro antibody responses, flow immunocytofluohmethc analysis of various peripheral blood or lymphoid mononuclear cell subpopulations using well established marker antigen systems, immunohistochemistry or other relevant assays.
- ADCC antibody dependent cell-mediated cytotoxicity
- the vaccine and adjuvant compositions provided herein will be capable of eliciting or enhancing in a host at least one immune response that is selected from a T H 1 -type T lymphocyte response, a T H 2-type T lymphocyte response, a cytotoxic T lymphocyte (CTL) response, an antibody response, a cytokine response, a lymphokine response, a chemokine response, and an inflammatory response.
- TTL cytotoxic T lymphocyte
- the immune response may comprise at least one of production of one or a plurality of cytokines wherein the cytokine is selected from interferon-gamma (IFN- ⁇ ), tumor necrosis factor-alpha (TNF- ⁇ ), production of one or a plurality of interleukins wherein the interleukin is selected from IL-1 , IL-2, IL-3, IL-4, IL-6, IL-8, IL-10, IL-12, IL-13, IL-16, IL-18 and IL-23, production one or a plurality of chemokines wherein the chemokine is selected from MIP-1 ⁇ , MIP-1 ⁇ , RANTES, CCL4 and CCL5, and a lymphocyte response that is selected from a memory T cell response, a memory B cell response, an effector T cell response, a cytotoxic T cell response and an effector B cell response.
- IFN- ⁇ interferon-gamma
- TNF- ⁇ tumor necrosis factor-alpha
- compositions generally comprise at least one GLA compound of the invention, and may further comprise one or more components as provided herein that are selected, for example, from antigen, TLR agonist, co-adjuvant (including optionally a cytokine, an imidazoquinoline immune response modifier and/or a dSLIM), and/or a recombinant expression construct, in combination with a pharmaceutically acceptable carrier, excipient or diluent.
- antigen TLR agonist
- co-adjuvant including optionally a cytokine, an imidazoquinoline immune response modifier and/or a dSLIM
- a recombinant expression construct in combination with a pharmaceutically acceptable carrier, excipient or diluent.
- the present invention is drawn to GLA "monotherapy" wherein GLA, as described herein, is formulated in a composition that is substantially devoid of other antigens, and is administered to a subject in order to stimulate an immune e response, e.g., a non-specific immune response, for the purpose of treating or preventing a disease or other condition, such as for treating an infection by an organism, for treating seasonal rhinitis, or the like.
- an immune e response e.g., a non-specific immune response
- the compositions and methods of the invention employ a GLA compound for stimulating an immune response in a subject.
- the GLA is in the form of a spray, optionally provided in a kit.
- the GLA may be preferably formulated in a stable emulsion.
- a composition comprising a GLA compound of the invention in a stable emulsion substantially devoid of other antigens.
- the pharmaceutical composition is a vaccine composition that comprises both GLA and an antigen and may further comprise one or more components, as provided herein, that are selected from TLR agonist, co-adjuvant (including, e.g., a cytokine, an imidazoquinoline immune response modifier and/or a dSLIM) and the like and/or a recombinant expression construct, in combination with a pharmaceutically acceptable carrier, excipient or diluent.
- TLR agonist including, e.g., a cytokine, an imidazoquinoline immune response modifier and/or a dSLIM
- co-adjuvant including, e.g., a cytokine, an imidazoquinoline immune response modifier and/or a dSLIM
- a recombinant expression construct in combination with a pharmaceutically acceptable carrier, excipient or diluent.
- Illustrative carriers will be nontoxic to recipients at the dosages and concentrations employed.
- GLA-plus-nucleic acid-based vaccines or for vaccines comprising GLA plus an antigen, about 0.001 ⁇ g/kg to about 100 mg/kg body weight will generally be administered, typically by the intradermal, subcutaneous, intramuscular or intravenous route, or by other routes.
- the dosage is about 0.001 ⁇ g/kg to about 1 mg/kg. In another specific embodiment, the dosage is about 0.001 to about 50 ⁇ g/kg. In another specific embodiment, the dosage is about 0.001 to about 15 ⁇ g/kg.
- the amount of GLA administered is about 0.01 ⁇ g/dose to about 5 mg/dose. In another specific embodiment, the amount of GLA administered is about 0.1 ⁇ g/dose to about 1 mg/dose. In another specific embodiment, the amount of GLA administered is about 0.1 ⁇ g/dose to about 100 ⁇ g/dose. In another specific embodiment, the GLA administered is about 0.1 ⁇ g/dose to about 10 ⁇ g/dose. It will be evident to those skilled in the art that the number and frequency of administration will be dependent upon the response of the host. "Pharmaceutically acceptable carriers" for therapeutic use are well known in the pharmaceutical art, and are described, for example, in Remingtons Pharmaceutical Sciences, Mack Publishing Co. (A. R. Gennaro edit. 1985).
- sterile saline and phosphate-buffered saline at physiological pH may be used.
- Preservatives, stabilizers, dyes and even flavoring agents may be provided in the pharmaceutical composition.
- sodium benzoate, sorbic acid and esters of p-hydroxybenzoic acid may be added as preservatives. ]d_. at 1449.
- antioxidants and suspending agents may be used, k ⁇
- “Pharmaceutically acceptable salt” refers to salts of the compounds of the present invention derived from the combination of such compounds and an organic or inorganic acid (acid addition salts) or an organic or inorganic base (base addition salts).
- the compositions of the present invention may be used in either the free base or salt forms, with both forms being considered as being within the scope of the present invention.
- compositions may be in any form which allows for the composition to be administered to a patient.
- the composition may be in the form of a solid, liquid or gas (aerosol).
- routes of administration include, without limitation, oral, topical, parenteral ⁇ e.g., sublingually or buccally), sublingual, rectal, vaginal, and intranasal ⁇ e.g., as a spray).
- parenteral as used herein includes iontophoretic ⁇ e.g., U.S. 7,033,598; 7,018,345; 6,970,739), sonophoretic ⁇ e.g., U.S.
- a composition as described herein is administered intradermal ⁇ by a technique selected from iontophoresis, microcavitation, sonophoresis or microneedles.
- compositions that will be administered to a patient take the form of one or more dosage units, where for example, a tablet may be a single dosage unit, and a container of one or more compounds of the invention in aerosol form may hold a plurality of dosage units.
- an excipient and/or binder may be present.
- examples are sucrose, kaolin, glycerin, starch dextrins, sodium alginate, carboxymethylcellulose and ethyl cellulose.
- Coloring and/or flavoring agents may be present.
- a coating shell may be employed.
- the composition may be in the form of a liquid, e.g., an elixir, syrup, solution, emulsion or suspension.
- the liquid may be for oral administration or for delivery by injection, as two examples.
- preferred compositions contain one or more of a sweetening agent, preservatives, dye/colorant and flavor enhancer.
- a surfactant, preservative, wetting agent, dispersing agent, suspending agent, buffer, stabilizer and isotonic agent may be included.
- a liquid pharmaceutical composition as used herein, whether in the form of a solution, suspension or other like form, may include one or more of the following carriers or excipients: sterile diluents such as water for injection, saline solution, preferably physiological saline, Ringer's solution, isotonic sodium chloride, fixed oils such as squalene, squalane, mineral oil, a mannide monooleate, cholesterol, and/or synthetic mono or digylcerides which may serve as the solvent or suspending medium, polyethylene glycols, glycerin, propylene glycol or other solvents; antibacterial agents such as benzyl alcohol or methyl paraben; antioxidants such as ascorbic acid or sodium bisulfite; chelating agents such as ethylenediaminetetraacetic acid; buffers such as acetates, citrates or phosphates and agents for the adjustment of tonicity such as sodium chloride or dextrose.
- the parenteral preparation can be enclosed in
- a pharmaceutical or vaccine composition of the invention comprises a stable aqueous suspension of less than 0.2um and further comprises at least one component selected from the group consisting of phospholipids, fatty acids, surfactants, detergents, saponins, fluorodated lipids, and the like.
- composition of the invention is formulated in a manner which can be aerosolized.
- a vaccine or pharmaceutical composition such as delivery vehicles including but not limited to aluminum salts, water-in-oil emulsions, biodegradable oil vehicles, oil- in-water emulsions, biodegradable microcapsules, and liposomes.
- delivery vehicles including but not limited to aluminum salts, water-in-oil emulsions, biodegradable oil vehicles, oil- in-water emulsions, biodegradable microcapsules, and liposomes.
- additional immunostimulatory substances for use in such vehicles are also described above and may include N-acetylmuramyl-L-alanine- D-isoglutamine (MDP), glucan, IL-12, GM-CSF, gamma interferon and IL-12.
- the carrier preferably comprises water, saline, alcohol, a fat, a wax or a buffer.
- the carrier preferably comprises water, saline, alcohol, a fat, a wax or a buffer.
- any of the above carriers or a solid carrier such as mannitol, lactose, starch, magnesium stearate, sodium saccharine, talcum, cellulose, glucose, sucrose, and magnesium carbonate, may be employed.
- Biodegradable microspheres e.g., polylactic galactide
- suitable biodegradable microspheres are disclosed, for example, in U.S. Patent Nos. 4,897,268 and 5,075,109. In this regard, it is preferable that the microsphere be larger than approximately 25 microns.
- compositions may also contain diluents such as buffers, antioxidants such as ascorbic acid, low molecular weight (less than about 10 residues) polypeptides, proteins, amino acids, carbohydrates including glucose, sucrose or dextrins, chelating agents such as EDTA, glutathione and other stabilizers and excipients.
- diluents such as buffers, antioxidants such as ascorbic acid, low molecular weight (less than about 10 residues) polypeptides, proteins, amino acids, carbohydrates including glucose, sucrose or dextrins, chelating agents such as EDTA, glutathione and other stabilizers and excipients.
- Neutral buffered saline or saline mixed with nonspecific serum albumin are exemplary appropriate diluents.
- product may be formulated as a lyophilizate using appropriate excipient solutions ⁇ e.g., sucrose) as diluents.
- compositions capable of delivering nucleic acid molecules encoding desired antigens.
- compositions include recombinant viral vectors (e.g., retroviruses (see WO 90/07936, WO 91/02805, WO 93/25234, WO 93/25698, and WO 94/03622), adenovirus (see Berkner, Biotechniques 6:616-627, 1988; Li et al., Hum. Gene Ther. 4:403-409, 1993; Vincent et al., Nat. Genet. 5:130- 134, 1993; and KoIIs et al., Proc. Natl. Acad. Sci.
- retroviruses see WO 90/07936, WO 91/02805, WO 93/25234, WO 93/25698, and WO 94/03622
- adenovirus see Berkner, Biotechniques 6:616-627, 1988; Li et al.,
- the DNA may be linked to killed or inactivated adenovirus (see Curiel et al., Hum. Gene Ther. 3:147-154, 1992; Cotton et al., Proc. Natl. Acad. Sci.
- compositions include DNA-ligand (see Wu et al., J. Biol. Chem. 264:16985- 16987, 1989) and lipid-DNA combinations (see Feigner et al., Proc. Natl. Acad. Sci. USA 84:7413-7417, 1989).
- ex vivo procedures may be used in which cells are removed from a host, modified, and placed into the same or another host animal. It will be evident that one can utilize any of the compositions noted above for introduction of antigen-encoding nucleic acid molecules into tissue cells in an ex vivo context. Protocols for viral, physical and chemical methods of uptake are well known in the art.
- the present invention is useful for enhancing or eliciting, in a host, a patient or in cell culture, an immune response.
- the term "patient” refers to any warm-blooded animal, preferably a human.
- a patient may be afflicted with an infectious disease, cancer, such as breast cancer, or an autoimmune disease, or may be normal (i.e., free of detectable disease and/or infection).
- a "cell culture” is any preparation containing immunocompetent cells or isolated cells of the immune system (including, but not limited to, T cells, macrophages, monocytes, B cells and dendritic cells).
- Such cells may be isolated by any of a variety of techniques well known to those of ordinary skill in the art (e.g., Ficoll-hypaque density centrifugation).
- the cells may (but need not) have been isolated from a patient afflicted with cancer, and may be reintroduced into a patient after treatment.
- a liquid composition intended for either parenteral or oral administration should contain an amount of GLA vaccine composition such that a suitable dosage will be obtained. Typically, this amount is at least 0.01 wt% of an antigen in the composition. When intended for oral administration, this amount may be varied to be between 0.1 and about 70% of the weight of the composition. Preferred oral compositions contain between about 4% and about 50% of the antigen. Preferred compositions and preparations are prepared so that a parenteral dosage unit contains between 0.01 to 1 % by weight of active composition.
- the pharmaceutical composition may be intended for topical administration, in which case the carrier may suitably comprise a solution, emulsion, ointment or gel base.
- the base for example, may comprise one or more of the following: petrolatum, lanolin, polyethylene glycols, beeswax, mineral oil, diluents such as water and alcohol, and emulsifiers and stabilizers.
- Thickening agents may be present in a pharmaceutical composition for topical administration.
- the composition may include a transdermal patch or iontophoresis device.
- Topical formulations may contain a concentration of the antigen ⁇ e.g., GLA-antigen vaccine composition) or GLA ⁇ e.g., immunological adjuvant composition; GLA is available from Avanti Polar Lipids, Inc., Alabaster, AL; e.g., product number 699800) of from about 0.1 to about 10% w/v (weight per unit volume).
- GLA is available from Avanti Polar Lipids, Inc., Alabaster, AL; e.g., product number 699800
- the composition may be intended for rectal administration, in the form, e.g., of a suppository which will melt in the rectum and release the drug.
- the composition for rectal administration may contain an oleaginous base as a suitable nonirritating excipient.
- bases include, without limitation, lanolin, cocoa butter and polyethylene glycol.
- the vaccine compositions/ adjuvants may be administered through use of insert(s), bead(s), timed-release formulation(s), patch(es) or fast-release formulation(s).
- kits comprising the herein described GLA vaccine compositions and/or GLA immunological adjuvant compositions, which may be provided in one or more containers.
- all components of the GLA vaccine compositions and/or GLA immunological adjuvant compositions are present together in a single container, but the invention embodiments are not intended to be so limited and also contemplate two or more containers in which, for example, a GLA immunological adjuvant composition is separate from, and not in contact with, the antigen component.
- administering may be performed beneficially, whilst in other cases such administration may beneficially be separated temporally and/or spatially ⁇ e.g., at a different anatomical site) from administration of the antigen, whilst in still other cases administration to the subject is beneficially conducted of a GLA vaccine composition as described herein and containing both antigen and GLA, and optionally other herein described components as well.
- a container according to such kit embodiments may be any suitable container, vessel, vial, ampule, tube, cup, box, bottle, flask, jar, dish, well of a single-well or multi-well apparatus, reservoir, tank, or the like, or other device in which the herein disclosed compositions may be placed, stored and/or transported, and accessed to remove the contents.
- a container may be made of a material that is compatible with the intended use and from which recovery of the contained contents can be readily achieved.
- Preferred examples of such containers include glass and/or plastic sealed or re-sealable tubes and ampules, including those having a rubber septum or other sealing means that is compatible with withdrawal of the contents using a needle and syringe.
- Such containers may, for instance, by made of glass or a chemically compatible plastic or resin, which may be made of, or may be coated with, a material that permits efficient recovery of material from the container and/or protects the material from, e.g., degradative conditions such as ultraviolet light or temperature extremes, or from the introduction of unwanted contaminants including microbial contaminants.
- the containers are preferably sterile or stehlizable, and made of materials that will be compatible with any carrier, excipient, solvent, vehicle or the like, such as may be used to suspend or dissolve the herein described vaccine compositions and/or immunological adjuvant compositions and/or antigens and/or recombinant expression constructs, etc.
- Emulsion systems may also be used in formulating compositions of the present invention.
- many single or multiphase emulsion systems have been described.
- Oil in water emulsion adjuvants per se have been suggested to be useful as adjuvant composition (EP 0 399 843B), also combinations of oil in water emulsions and other active agents have been described as adjuvants for vaccines (WO 95/17210; WO 98/56414; WO 99/12565; WO 99/11241 ).
- Other oil emulsion adjuvants have been described, such as water in oil emulsions (U.S. Pat. No. 5,422,109; EP O 480 982 B2) and water in oil in water emulsions (U.S. Pat. No.
- a composition of the invention comprises an emulsion of oil in water wherein the GLA is incorporated in the oil phase.
- a composition of the invention comprises an emulsion of oil in water wherein the GLA is incorporated in the oil phase and wherein an additional component is present, such as a co-adjuvant, TLR agonist, or the like, as described herein.
- the oil phase of the emulsion system preferably comprises a metabolizable oil.
- metabolizable oil is well known in the art. Metabolizable can be defined as "being capable of being transformed by metabolism” (Dorland's illustrated Medical Dictionary, W. B. Saunders Company, 25th edition (1974)).
- the oil may be any vegetable oil, fish oil, animal oil or synthetic oil, which is not toxic to the recipient and is capable of being transformed by metabolism. Nuts (such as peanut oil), seeds, and grains are common sources of vegetable oils. Synthetic oils are also part of this invention and can include commercially available oils such as NEOBEE® and others.
- Squalene (2,6,10,15,19,23-Hexamethyl-2,6,10,14,18,22- tetracosahexaene), for example, is an unsaturated oil which is found in large quantities in shark-liver oil, and in lower quantities in olive oil, wheat germ nil, rice bran oil, and yeast, and is a particularly preferred oil for use in this invention.
- Squalene is a metabolizable oil virtue of the fact that it is an intermediate in the biosynthesis of cholesterol (Merck index, 10th Edition, entry no.8619).
- Particularly preferred oil emulsions are oil in water emulsions, and in particular squalene in water emulsions.
- the most preferred oil emulsion adjuvants of the present invention comprise an antioxidant, which is preferably the oil .alpha.-tocopherol (vitamin E, EP 0 382 271 B1 ).
- an antioxidant which is preferably the oil .alpha.-tocopherol (vitamin E, EP 0 382 271 B1 ).
- WO 95/17210 and WO 99/11241 disclose emulsion adjuvants based on squalene, alpha-tocopherol, and TWEEN® 80, optionally formulated with the immunostimulants QS21 and/or 3D-MPL (which are discussed above).
- WO 95/17210 and WO 99/11241 disclose emulsion adjuvants based on squalene, alpha-tocopherol, and TWEEN® 80, optionally formulated with the immunostimulants QS21 and/or 3D-MPL (which are discussed above).
- 99/12565 discloses an improvement to these squalene emulsions with the addition of a sterol into the oil phase.
- a triglyceride such as tricaprylin (C27H5OO6), may be added to the oil phase in order to stabilize the emulsion (WO 98/56414).
- the size of the oil droplets found within the stable oil in water emulsion are preferably less than 1 micron, may be in the range of substantially 30-600 nm, preferably substantially around 30-500 nm in diameter, and most preferably substantially 150-500 nm in diameter, and in particular about 150 nm in diameter as measured by photon correlation spectroscopy.
- the oil droplets by number should be within the preferred ranges, more preferably more than 90% and most preferably more than 95% of the oil droplets by number are within the defined size ranges
- the amounts of the components present in the oil emulsions of the present invention are conventionally in the range of from 2 to 10% oil, such as squalene; and when present, from 2 to 10% alpha tocopherol; and from 0.3 to 3% surfactant, such as polyoxyethylene sorbitan monooleate.
- the ratio of oil: alpha tocopherol is equal or less than 1 as this provides a more stable emulsion.
- Span 85 may also be present at a level of about 1 %. In some cases it may be advantageous that the vaccines of the present invention will further contain a stabilizer.
- the method comprises the mixing the oil phase with a surfactant such as a PBS/TWEEN80® solution, followed by homogenization using a homogenizer.
- a surfactant such as a PBS/TWEEN80® solution
- a homogenizer for instance, a method that comprises passing the mixture once, twice or more times through a syringe needle would be suitable for homogenizing small volumes of liquid.
- the emulsification process in a microfluidizer M110S microfluidics machine, maximum of 50 passes, for a period of 2 minutes at maximum pressure input of 6 bar (output pressure of about 850 bar)
- This adaptation could be achieved by routine experimentation comprising the measurement of the resultant emulsion until a preparation was achieved with oil droplets of the required diameter.
- the following Examples are offered by way of illustration and nottation.
- Glucose amine 1 (2.04 g, 9.45 mmol), sodium hydrogencarbonate (3.21 g, 38.22 mmol), and copper(ll) sulfate pentahydrate (90.5 mg, 0.362 mmol) were dissolved in water (12.3 mL).
- the triflic azide stock solution prepared above (21 mL) was added, followed by the addition of methanol (81 mL) to yield a homogeneous system.
- the blue mixture was stirred vigorously at room temperature. Complete consumption of the amine was monitored by TLC (ninhydrin stain) and is also indicated by a color change of the mixture from blue to green.
- the solvents were removed in vacuo with a rotary evaporator keeping the temperature strictly below 25 0 C.
- Acetic acid (0.30 mL, 5.2 mmol) was added dropwise to a stirred suspension of 7 (700 mg, 1.04 mmol) and zinc powder (676 mg, 10.4 mmol) in DCM (15 mL).
- the reaction mixture was stirred at room temperature for 4 h, after which it was diluted with ethyl acetate (50 mL).
- the solids were removed by filtration and washed with ethyl acetate (2 x 10 mL).
- the combined filtrates were washed with saturated aqueous NaHCO3 (2 x 40 mL) and brine (2 x 40 mL).
- ⁇ /V-Dicyclohexylcarbodiimide (230 mg, 1.11 mmol) was added to a stirred solution of (RJ-S-dodecanoyl-tetradecanoic acid (see preparation below, compound 40) (381 mg, 0.81 mmol) in DCM (10 ml_). After the reaction mixture was stirred for 10 min, the free amine (648 mg, 0.699 mmol) in DCM (10 ml_) was added, and stirring was continued for another 12 h. The insoluble materials were removed by filtration, and the residue was washed with DCM (2 ⁇ 2 ml_).
- Tetrakis(triphenylphosphine)palladiunn (228 mg, 0.198 mmol) was added to a solution of 17 (1.66 g, 0.980 mmol), D-BuNH 2 (0.19 ml_, 1.97 mmol), and HCOOH (74.5 ⁇ l_, 1.98 mmol) in THF (20 ml_). After the reaction mixture was stirred at room temperature for 20 min, it was diluted with DCM (40 ml_), and washed successively with water (40 ml_), saturated aqueous NaHCO3 (2 x 40 ml_), and brine (40 ml_). The organic phase was dried (MgSO 4 ) and filtered.
- EXAMPLE 18 TERT-BUTYLDIMETHYLSILYL-6-O- ⁇ 6-O-BENZYL-2-DEOXY-4-O-(1 ,5- DIHYDRO-3-OXO-3 ⁇ . 5 -3H-2,4,3-BENZODIOXAPHOSPHEPIN-3YL)-2-r(R)-3-
- Compound 15 (1.23 g, 1.07 mmol) was acylated in a manner similar to the synthesis of compound 16 (Example 14) using (DCC, 430 mg, 2.08 mmol), required lipid (Compound 40, Example 36, 630 mg, 1.59 mmol), and triethylamine (161 mg, 1.59 mmol) to provide 20 (1.05 g, 81 %) as a colorless oil.
- Compound 20 (1.43 g, 1.18 mmol) was acylated in a manner similar to the synthesis of compound 17 (Example 15) using (DCC, 453 mg, 2.20 mmol), required lipid (477 mg, 1.43 mmol), and ⁇ /, ⁇ /-dimethyl-4- aminopyridine (67 mg, 0.548 mmol) to provide 21 (1.60 g, 83%) as a colorless oil.
- Compound 22 (1.25 g, 0.811 mmol) was acylated in a manner similar to the synthesis of compound 19 (Example 17) using (DCC, 335 mg, 1.62 mmol), required lipid (Compound 34, Example 32, 386 mg, 1.06 mmol), and ⁇ /, ⁇ /-dimethyl-4-aminopyridine (50 mg, 0.41 mmol) to provide 23 (440 mg, 29%) as a colorless oil.
- Ester 31 (1.3 g, 3.73 mmol) was dissolved in THF/MeOH/CH 3 CN mixture (v/v/v, 1/1/1 , 90 mL). Lithium hydroxide monohydrate (235 mg, 5.6 mmol) as a solution in water (30 mL) was added, and the mixture stirred overnight. The solvent amount was reduced in vacuo to about 30 ml_. To the remaining aqueous solution was added 1 M hydrochloric acid to bring the pH down to 3. The aqueous layer was extracted with diethyl ether (3 * 40 ml_). The combined organic extracts were dried over sodium sulfate. The drying agent was removed by filtration, and the solvents removed using a rotary evaporator.
- Ester 32 (4.01 g, 10.4 mmol) was dissolved in THF/MeOH/CH 3 CN mixture (v/v/v, 1/1/1 , 90 ml_). Lithium hydroxide monohydrate (874 mg, 20.8 mmol) as a solution in water (30 mL) was added, and the mixture stirred overnight. The solvent amount was reduced in vacuo to about 30 mL. To the remaining aqueous solution was added hydrochloric acid (1 M) to bring the pH down to 3. The aqueous layer was extracted with diethyl ether (3 * 40 mL). The combined organic extracts were dried over sodium sulfate. The drying agent was removed by filtration and the solvents removed using a rotary evaporator.
- Ester 39 (10.15 g, 20.77 mmol) was dissolved in acetic acid (100 ml_). Zinc (15.5 g, 237 mmol) was added, and the mixture heated to reflux for 4 h. The acetic acid was removed under vacuum and the residue azeotroped with toluene to dryness. The residue was purified by chromatography on silica gel (120 g RediSep column, eluting with a gradient of 0% through 60% ethyl acetate/hexanes over 50 min, 85 mL/min) to give the product 40 (7.2 g, 89%) as a colorless liquid.
- the reactor was then charged with a final portion of H 2 (60 psi) stirred (600 rpm) and heated to 50 0 C for 20 h. The reactor was then cooled to room temperature and the mixture concentrated in vacuo. The resulting residue was purified by silica gel chromatography, eluting with a gradient of 0% through 50% ethyl acetate/hexanes to provide 42 (3.97 g, 74%) as an off-white solid.
- Lithium hydroxide monohydrate (1.98 g, 47.2 mmol) was added to a solution of (R)-methyl 3-hydroxytetradecanoate (42, 8.17 g, 31.5 mmol) in THF (66 mL) and water (66 mL) and stirred at room temperature for 2 h. The mixture was then diluted with diethyl ether (1 L) and the pH adjusted to ⁇ 3 with a solution of hydrochloric acid (1 N). The solution was then extracted with diethyl ether (200 mL), and the organic fractions were combined and dried over Na 2 SO 4 .
- Zinc dust (24.42 g, 373.3 mmol) was added to a solution of 46 (16.28 g, 28.42 mmol) in acetic acid (150 ml_). The mixture was then heated to reflux (115 0 C) for 3 h. The mixture was then concentrated in vacuo, and the residual pyridine removed by dissolving the residue in toluene (100 ml_) and concentrating in vacuo.
- Compound IX was used in a vaccine containing a Mycobacterium tuberculosis antigenic polypeptide referred to as ID83. Standard immunological methodologies and reagents were employed (Current Protocols in Immunology, Coligan et al. (Eds.) 2006 John Wiley & Sons, NY).
- mice (four C57BL/6 animals per group) were immunized three times at three-week intervals with ID83 antigen (8 ⁇ g per animal for each immunization) in water, ID83 antigen (8 ⁇ g per animal for each immunization) formulated in a stable emulsion vehicle, or ID83 antigen (8 ⁇ g per animal for each immunization) formulated in a stable emulsion containing (i) GLA-SE (10 ⁇ g per animal for each immunization), or (ii) Compound IX (10 ⁇ g per animal for each immunization).
- mice were bled to evaluate antigen-specific antibody (IgGI and lgG2c) responses.
- IgGI and lgG2c antigen-specific antibody
- mice were sacrificed and spleens collected to analyze T cell- dependent IFN- ⁇ cytokine responses to in vitro antigen stimulation by ELISPOT according to published methods (Id.).
- IFN- ⁇ cytokine responses have been associated with a TH1 protective phenotype against M. tuberculosis infection.
- Figure 1 shows ELISPOT data of anti-ID83 IFN- ⁇ cytokine production induced in mice three weeks after the third immunization using ID83 antigen and ID83 component antigens (Rv2608, Rv1813 and Rv3620) formulated with a stable emulsion (SE) of 10 ⁇ g Compound IX, compared to ID83 formulated in GLA-SE, SE or water. Means and SEM of IFN- ⁇ secreting cells per million of splenocytes in each group are shown.
- GLA-SE refers to a stable emulsion of a compound as described in co-owned U.S. Patent Publication No. 20080131466, wherein R 1 , R 3 , R 5 and R 6 are Cn linear alkyl; and R 2 and R 4 are Ci 3 linear alkyl.
- ID83 + Compound IX vaccination induced robust ID83 antigen- specific cytokine responses, while little or no such responses were observed in the ID83 + water or ID83 + SE control groups.
- Similar levels of IFN- ⁇ secreting cells were elicited in splenocytes purified from mice immunized with ID83 + Compound IX or ID83 + GLA-SE upon restimulation with the ID83 component antigens, Rv2608, Rv1813 and Rv3620.
- Compound IX in a stable oil formulation with M. tuberculosis vaccine antigen candidate ID83 induced predominantly antigen- specific immune responses of the cellular type (T cell) associated with the protective TH 1 phenotype.
- mice (four C57BL/6 animals per group) were immunized three times at three-week intervals with the ID83 antigen (8 ⁇ g per animal for each immunization) used alone or formulated in a stable emulsion containing Compound IX (10 ⁇ g per animal for each immunization).
- Sera were collected by bleeding animals one week after each immunization, and serum levels of IgGI and lgG2c antibodies specific for ID83 were examined by ELISA according to published methods (Id.)
- Predominance of either IgGI or lgG2c antibody isotype is associated with TH2 or TH1 responses, respectively. It has been demonstrated that a TH1 response is necessary for protection against Mycobacterium tuberculosis infection.
- ID83 in water induced predominantly antigen-specific IgGI antibody.
- ID83 + SE, ID83 + Compound IX-SE or ID83 + GLA-SE vaccination induced higher lgG2c antibody titers, and converted the phenotype to a mixed lgG1 :lgG2c antigen-specific antibody response.
- This example demonstrates the immunostimulatory activity of Compound IX in human cells.
- Compound IX was tested in vitro using HEK 293 cells (InvivoGen) with expression vectors encoding 1 ) TLR4, MD-2, and CD14, or 2) TLR2 and TLR6 to define compound activity and dependence on TLR4, and to exclude activation of TLR2.
- HEK 293 cell lines were further stably transfected with the NF-kB reporter vector pNifty-2 such that alkaline phosphatase is secreted into the growth media upon activation of the TLR signaling pathway.
- Transfected cell lines were plated at 5x10 4 cells per well in a 96-well plates and stimulated for 16-24 hours cultured in medium containing serial dilutions of Compound IX and other adjuvants.
- Secreted alkaline phosphatase activity was measured in the culture media using QUANTIBIue® assay (InvivoGen). The data was measured as enhancement of NF-kB above the PBS negative control.
- Compound IX showed greater than two-fold enhancement of NF-kB at concentrations as low as 0.1 ⁇ g/ml ( Figure 3). The results of these experiments demonstrated clear TLR4 agonist activity for Compound IX that did not appear to be associated with induction of TLR2.
- Compound IX was designed based on structural considerations of the reported atomic structure of MD2 and TLR4. As such, the fact that it binds and elicits a profile that is similar to that of a commercially approved TLR4 agonist (MPL®) is a surprising and unexpected result. More specifically, the profile for Compound IX advantageously plateaus rapidly as concentrations are increased, before one would expect the cytokine levels to rise to a point where negative side effects may exert themselves. Thus, it is expected that Compound IX and other illustrative compounds of the invention can be safely administered over a broad range of concentrations, which is highly desirable in the context of reproducibility of clinical outcomes among patients and for the safety in ranging a dose for adults and children. In this respect, the lower cytokine activity for Compound IX is a surprising and desirable result that will further facilitate its safe use in clinical formulations.
- human whole blood cells were stimulated with Compound IX and ELISA assays were performed to detect the induction of immunostimulatory cytokines.
- Serial dilutions (1 :5) of Compound IX and other adjuvants were performed with phosphate buffered saline in a 96 well plate for a total of 7 dilutions.
- 100 ⁇ l of fresh Iy drawn human blood from two different donors were mixed and incubated with 100 ⁇ l of adjuvant dilutions.
Landscapes
- Health & Medical Sciences (AREA)
- Life Sciences & Earth Sciences (AREA)
- Chemical & Material Sciences (AREA)
- General Health & Medical Sciences (AREA)
- Medicinal Chemistry (AREA)
- Pharmacology & Pharmacy (AREA)
- Animal Behavior & Ethology (AREA)
- Public Health (AREA)
- Veterinary Medicine (AREA)
- Immunology (AREA)
- Organic Chemistry (AREA)
- Epidemiology (AREA)
- Engineering & Computer Science (AREA)
- Microbiology (AREA)
- Mycology (AREA)
- Molecular Biology (AREA)
- Virology (AREA)
- Chemical Kinetics & Catalysis (AREA)
- General Chemical & Material Sciences (AREA)
- Nuclear Medicine, Radiotherapy & Molecular Imaging (AREA)
- Biochemistry (AREA)
- Biotechnology (AREA)
- Genetics & Genomics (AREA)
- Bioinformatics & Cheminformatics (AREA)
- Communicable Diseases (AREA)
- Crystallography & Structural Chemistry (AREA)
- Pulmonology (AREA)
- Hematology (AREA)
- Dispersion Chemistry (AREA)
- Oncology (AREA)
- Medicines Containing Antibodies Or Antigens For Use As Internal Diagnostic Agents (AREA)
- Pharmaceuticals Containing Other Organic And Inorganic Compounds (AREA)
- Medicines That Contain Protein Lipid Enzymes And Other Medicines (AREA)
- Saccharide Compounds (AREA)
- Medicines Containing Material From Animals Or Micro-Organisms (AREA)
Abstract
Description
Claims
Priority Applications (19)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| BRPI1011072-0A BRPI1011072B1 (en) | 2009-06-05 | 2010-06-04 | GLA COMPOUND, VACCINE AND PHARMACEUTICAL COMPOSITIONS INCLUDING SUCH COMPOUND, AS WELL AS THEIR USE TO STIMULATE, INDUCE OR EMPHASIZE AN IMMUNE RESPONSE IN AN INDIVIDUAL |
| JP2012514187A JP5830015B2 (en) | 2009-06-05 | 2010-06-04 | Synthetic glucopyranosyl lipid adjuvant |
| ES10784178.5T ES2606563T3 (en) | 2009-06-05 | 2010-06-04 | Synthetic glycopyranosyl lipid adjuvants and vaccine compositions containing the same |
| SI201031333A SI2437753T1 (en) | 2009-06-05 | 2010-06-04 | Synthetic glucopyranosyl lipid adjuvants and vaccine compositions containing them |
| DK10784178.5T DK2437753T3 (en) | 2009-06-05 | 2010-06-04 | Synthetic glucopyranosyl lipid adjuvants and vaccine compositions containing them |
| AU2010256461A AU2010256461B2 (en) | 2009-06-05 | 2010-06-04 | Synthetic glucopyranosyl lipid adjuvants |
| CA2764374A CA2764374C (en) | 2009-06-05 | 2010-06-04 | Synthetic glucopyranosyl lipid adjuvants |
| LTEP10784178.5T LT2437753T (en) | 2009-06-05 | 2010-06-04 | Synthetic glucopyranosyl lipid adjuvants and vaccine compositions containing them |
| EP10784178.5A EP2437753B1 (en) | 2009-06-05 | 2010-06-04 | Synthetic glucopyranosyl lipid adjuvants and vaccine compositions containing them |
| CN201080034214.0A CN102481312B (en) | 2009-06-05 | 2010-06-04 | Synthetic Glucopyranosyl Lipid Adjuvants |
| EP16186377.4A EP3124491B1 (en) | 2009-06-05 | 2010-06-04 | Synthetic glucopyranosyl lipid adjuvants and vaccine compositions as well as pharmaceutical compositions containing them |
| MX2011012836A MX2011012836A (en) | 2009-06-05 | 2010-06-04 | Synthetic glucopyranosyl lipid adjuvants. |
| RU2011152602/04A RU2560182C2 (en) | 2009-06-05 | 2010-06-04 | Synthetic glucopyranosyllipid adjuvants |
| MX2014009221A MX360448B (en) | 2009-06-05 | 2010-06-04 | Synthetic glucopyranosyl lipid adjuvants. |
| IL216669A IL216669A (en) | 2009-06-05 | 2011-11-29 | Synthetic glucopyranosyl lipid adjuvants |
| IL242992A IL242992B (en) | 2009-06-05 | 2015-12-09 | Synthetic glucopyranosyl lipid adjuvants |
| CY20161100990T CY1118347T1 (en) | 2009-06-05 | 2016-10-05 | GLYCOPYRANOZYL-Lipid Synthetic Immunosuppressants and Vaccine Compositions Containing them |
| HRP20161585TT HRP20161585T1 (en) | 2009-06-05 | 2016-11-29 | Synthetic glucopyranosyl lipid adjuvants and vaccine compositions containing them |
| SM201600437T SMT201600437B (en) | 2009-06-05 | 2016-11-29 | SYNTHETIC GLUCOPYRANOSILE-BASED ADIUVANTS AND VACCINAL COMPOSITIONS THAT CONTAIN THEM |
Applications Claiming Priority (2)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US18470309P | 2009-06-05 | 2009-06-05 | |
| US61/184,703 | 2009-06-05 |
Publications (1)
| Publication Number | Publication Date |
|---|---|
| WO2010141861A1 true WO2010141861A1 (en) | 2010-12-09 |
Family
ID=43298190
Family Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| PCT/US2010/037466 WO2010141861A1 (en) | 2009-06-05 | 2010-06-04 | Synthetic glucopyranosyl lipid adjuvants |
Country Status (22)
| Country | Link |
|---|---|
| US (4) | US8722064B2 (en) |
| EP (2) | EP2437753B1 (en) |
| JP (3) | JP5830015B2 (en) |
| CN (2) | CN102481312B (en) |
| AU (1) | AU2010256461B2 (en) |
| BR (1) | BRPI1011072B1 (en) |
| CA (1) | CA2764374C (en) |
| CY (1) | CY1118347T1 (en) |
| DK (1) | DK2437753T3 (en) |
| ES (1) | ES2606563T3 (en) |
| HR (1) | HRP20161585T1 (en) |
| HU (1) | HUE031051T2 (en) |
| IL (2) | IL216669A (en) |
| LT (1) | LT2437753T (en) |
| MX (2) | MX360448B (en) |
| PL (1) | PL2437753T3 (en) |
| PT (1) | PT2437753T (en) |
| RU (3) | RU2560182C2 (en) |
| SI (1) | SI2437753T1 (en) |
| SM (1) | SMT201600437B (en) |
| TW (2) | TWI549688B (en) |
| WO (1) | WO2010141861A1 (en) |
Cited By (23)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| WO2012112691A1 (en) | 2011-02-15 | 2012-08-23 | Immune Design Corp. | Methods for enhancing immunogen specific immune responses by vectored vaccines |
| US8343512B2 (en) | 2006-09-26 | 2013-01-01 | Infectious Disease Research Institute | Treatment of allergic conditions using a composition containing synthetic adjuvant |
| EP2647387A1 (en) * | 2012-04-04 | 2013-10-09 | Nitto Denko Corporation | Vaccine Composition |
| US8609114B2 (en) | 2006-09-26 | 2013-12-17 | Infectious Diesease Research Institute | Methods of using a vaccine composition containing synthetic adjuvant |
| US8957047B2 (en) | 2013-04-18 | 2015-02-17 | Immune Design Corp. | GLA monotherapy for use in cancer treatment |
| US9017698B2 (en) | 2013-09-25 | 2015-04-28 | Sequoia Sciences, Inc. | Compositions of vaccines and adjuvants and methods for the treatment of urinary tract infections |
| WO2015112485A1 (en) * | 2014-01-21 | 2015-07-30 | Immune Design Corp. | Compositions for use in the treatment of allergic conditions |
| WO2015123496A1 (en) | 2014-02-14 | 2015-08-20 | Immune Design Corp. | Immunotherapy of cancer through combination of local and systemic immune stimulation |
| US9149522B2 (en) | 2013-09-25 | 2015-10-06 | Sequoia Sciences, Inc. | Compositions of vaccines and adjuvants and methods for the treatment of urinary tract infections |
| US9149521B2 (en) | 2013-09-25 | 2015-10-06 | Sequoia Sciences, Inc. | Compositions of vaccines and adjuvants and methods for the treatment of urinary tract infections |
| US9463198B2 (en) | 2013-06-04 | 2016-10-11 | Infectious Disease Research Institute | Compositions and methods for reducing or preventing metastasis |
| US9480740B2 (en) | 2009-06-05 | 2016-11-01 | Infectious Disease Research Institute | Synthetic glucopyranosyl lipid adjuvants |
| US9878037B2 (en) | 2013-09-25 | 2018-01-30 | Sequoia Sciences, Inc. | Compositions of vaccines and adjuvants and methods for the treatment of urinary tract infections |
| US9895435B2 (en) | 2012-05-16 | 2018-02-20 | Immune Design Corp. | Vaccines for HSV-2 |
| EP2694099B1 (en) * | 2011-04-08 | 2019-10-16 | Immune Design Corp. | Immunogenic compositions and methods of using the compositions for inducing humoral and cellular immune responses |
| EP3563834A1 (en) * | 2012-02-07 | 2019-11-06 | Infectious Disease Research Institute | Improved adjuvant formulations comprising tlr4 agonists and methods of using the same |
| US10940198B2 (en) | 2016-12-26 | 2021-03-09 | Mogam Institute For Biomedical Research | Herpes zoster vaccine composition |
| WO2021067785A1 (en) | 2019-10-02 | 2021-04-08 | Janssen Vaccines & Prevention B.V | Staphylococcus peptides and methods of use |
| WO2021097347A1 (en) | 2019-11-15 | 2021-05-20 | Infectious Disease Research Institute | Rig-i agonist and adjuvant formulation for tumor treatment |
| US11207403B2 (en) | 2017-09-13 | 2021-12-28 | Sanofi Pasteur | Human cytomegalovirus immunogenic composition |
| WO2022136952A1 (en) | 2020-12-23 | 2022-06-30 | Infectious Disease Research Institute | Solanesol vaccine adjuvants and methods of preparing same |
| US11458209B2 (en) | 2020-03-23 | 2022-10-04 | Hdt Bio Corp. | Compositions and methods for delivery of nucleic acid-lipid nanoparticle complexes encoding for viral RNA polymerase region and protein antigen |
| US11679163B2 (en) | 2019-09-20 | 2023-06-20 | Hdt Bio Corp. | Compositions and methods for delivery of RNA |
Families Citing this family (55)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| CA2744987C (en) | 2008-12-02 | 2018-01-16 | Chiralgen, Ltd. | Method for the synthesis of phosphorus atom modified nucleic acids |
| AU2010270714B2 (en) | 2009-07-06 | 2015-08-13 | Wave Life Sciences Ltd. | Novel nucleic acid prodrugs and methods use thereof |
| CN102946900A (en) | 2010-03-11 | 2013-02-27 | 免疫设计公司 | Vaccines for pandemic influenza |
| EP2620428B1 (en) | 2010-09-24 | 2019-05-22 | Wave Life Sciences Ltd. | Asymmetric auxiliary group |
| US20120288515A1 (en) | 2011-04-27 | 2012-11-15 | Immune Design Corp. | Synthetic long peptide (slp)-based vaccines |
| SG10201700554VA (en) | 2011-07-19 | 2017-03-30 | Wave Life Sciences Pte Ltd | Methods for the synthesis of functionalized nucleic acids |
| US20140328876A1 (en) * | 2011-11-18 | 2014-11-06 | Variation Biotechnologies Inc. | Synthetic derivatives of mpl and uses thereof |
| EP3984551A1 (en) | 2011-12-02 | 2022-04-20 | Rhode Island Hospital | Vaccine for falciparum malaria |
| SG11201407875UA (en) | 2012-06-08 | 2014-12-30 | Aduro Biotech | Compostions and methods for cancer immunotherapy |
| SG11201500239VA (en) | 2012-07-13 | 2015-03-30 | Wave Life Sciences Japan | Asymmetric auxiliary group |
| BR112015000723A2 (en) * | 2012-07-13 | 2017-06-27 | Shin Nippon Biomedical Laboratories Ltd | chiral nucleic acid adjuvant |
| WO2014012081A2 (en) | 2012-07-13 | 2014-01-16 | Ontorii, Inc. | Chiral control |
| WO2014093936A1 (en) | 2012-12-13 | 2014-06-19 | Aduro Biotech, Inc. | Compositions comprising cyclic purine dinucleotides having defined stereochemistries and methods for their preparation and use |
| CN105358158A (en) | 2013-04-29 | 2016-02-24 | 纪念斯隆-凯特琳癌症中心 | Compositions and methods for altering second messenger signaling |
| JP2016518140A (en) | 2013-05-03 | 2016-06-23 | ザ リージェンツ オブ ザ ユニバーシティ オブ カリフォルニア | Method for inducing cyclic dinucleotide of type I interferon |
| RS59500B1 (en) | 2013-05-18 | 2019-12-31 | Aduro Biotech Inc | Compositions and methods for activating "stimulator of interferon gene"-dependent signalling |
| US9549944B2 (en) | 2013-05-18 | 2017-01-24 | Aduro Biotech, Inc. | Compositions and methods for inhibiting “stimulator of interferon gene”—dependent signalling |
| WO2015017652A1 (en) | 2013-07-31 | 2015-02-05 | Memorial Sloan-Kettering Cancer Center | Sting crystals and modulators |
| WO2015035010A1 (en) * | 2013-09-05 | 2015-03-12 | Immune Design Corp. | Vaccine compositions for drug addiction |
| CN105530953A (en) | 2013-10-03 | 2016-04-27 | 日东电工株式会社 | Injectable vaccine composition |
| EP3053593A4 (en) | 2013-10-03 | 2017-07-05 | Nitto Denko Corporation | Nasal mucosal vaccine composition |
| AU2014330337A1 (en) | 2013-10-03 | 2016-03-17 | Nitto Denko Corporation | Mucosal vaccine composition |
| TW201601752A (en) | 2013-10-03 | 2016-01-16 | Nitto Denko Corp | Mucosal vaccine composition |
| US11801223B2 (en) | 2013-12-31 | 2023-10-31 | Access To Advanced Health Institute | Single vial vaccine formulations |
| US10149905B2 (en) | 2014-01-15 | 2018-12-11 | Shin Nippon Biomedical Laboratories, Ltd. | Chiral nucleic acid adjuvant having antitumor effect and antitumor agent |
| JPWO2015108046A1 (en) | 2014-01-15 | 2017-03-23 | 株式会社新日本科学 | Chiral nucleic acid adjuvant and antiallergic agent having antiallergic action |
| EP3095461A4 (en) | 2014-01-15 | 2017-08-23 | Shin Nippon Biomedical Laboratories, Ltd. | Chiral nucleic acid adjuvant having immunity induction activity, and immunity induction activator |
| MX2016009290A (en) | 2014-01-16 | 2017-02-28 | Wave Life Sciences Ltd | Chiral design. |
| WO2016011083A1 (en) | 2014-07-15 | 2016-01-21 | Immune Design Corp. | Prime-boost regimens with a tlr4 agonist adjuvant and a lentiviral vector |
| TN2017000375A1 (en) | 2015-03-10 | 2019-01-16 | Aduro Biotech Inc | Compositions and methods for activating "stimulator of interferon gene" -dependent signalling |
| TW201722472A (en) | 2015-11-27 | 2017-07-01 | Nitto Denko Corp | Vaccine pharmaceutical composition for oral administration and method for manufacturing vaccine pharmaceutical composition for oral administration |
| IL314130A (en) | 2016-05-16 | 2024-09-01 | Access To Advanced Health Inst | Formulation containing tlr agonist and methods of use |
| CN109562057A (en) | 2016-05-16 | 2019-04-02 | 传染病研究所 | Pegylated liposomal and application method |
| JP2019521095A (en) | 2016-05-21 | 2019-07-25 | インフェクシャス ディズィーズ リサーチ インスティチュート | Compositions and methods for treating secondary tuberculosis and nontuberculous mycobacterial infections |
| BR112018074352B1 (en) | 2016-06-01 | 2021-11-30 | Infectious Disease Research Institute | NANOALUME PARTICLES CONTAINING A SIZING AGENT |
| WO2018009466A1 (en) | 2016-07-05 | 2018-01-11 | Aduro Biotech, Inc. | Locked nucleic acid cyclic dinucleotide compounds and uses thereof |
| US11633411B2 (en) | 2016-10-04 | 2023-04-25 | University Of Maryland, Baltimore | Methods of treating sepsis using anti-sepsis lipid A (ASLA) based therapeutics |
| KR102028463B1 (en) * | 2016-11-25 | 2019-10-04 | 재단법인 목암생명과학연구소 | Varicella Zoster Virus Vaccines |
| UY37695A (en) | 2017-04-28 | 2018-11-30 | Novartis Ag | BIS 2’-5’-RR- (3’F-A) (3’F-A) CYCLE DINUCLEOTIDE COMPOUND AND USES OF THE SAME |
| KR102673794B1 (en) | 2017-06-15 | 2024-06-11 | 액세스 투 어드밴스드 헬스 인스티튜트 | Nanostructured lipid carriers and stable emulsions and their uses |
| CN111315406A (en) * | 2017-09-08 | 2020-06-19 | 传染病研究所 | Liposome formulations comprising saponins and methods of use thereof |
| EA202091931A1 (en) | 2018-02-12 | 2020-11-05 | Иниммьюн Корпорейшн | Toll-Like Receptor Ligands |
| WO2019175147A1 (en) | 2018-03-12 | 2019-09-19 | Janssen Vaccines & Prevention B.V. | Vaccines against intra-abdominal infections |
| AU2020240075A1 (en) | 2019-03-18 | 2021-10-14 | Janssen Pharmaceuticals, Inc. | Methods of producing bioconjugates of e. coli o-antigen polysaccharides, compositions thereof, and methods of use thereof |
| EA202192390A1 (en) | 2019-03-18 | 2021-12-03 | Янссен Фармасьютикалз, Инк. | BIOCONJUGATES OF E.COLI POLYSACCHARIDE O-ANTIGENS, METHODS FOR THEIR PRODUCTION AND METHODS FOR THEIR APPLICATION |
| CN114340665A (en) | 2019-05-25 | 2022-04-12 | 传染病研究所 | Compositions and methods for spray drying adjuvant vaccine emulsions |
| EP4090363B1 (en) | 2020-01-16 | 2024-09-04 | Janssen Pharmaceuticals, Inc. | Fimh mutant, compositions therewith and use thereof |
| US10973908B1 (en) | 2020-05-14 | 2021-04-13 | David Gordon Bermudes | Expression of SARS-CoV-2 spike protein receptor binding domain in attenuated salmonella as a vaccine |
| AU2021337493A1 (en) | 2020-09-04 | 2023-05-18 | Access To Advanced Health Institute | Co-lyophilized rna and nanostructured lipid carrier |
| WO2022058945A1 (en) | 2020-09-17 | 2022-03-24 | Janssen Pharmaceuticals, Inc. | Multivalent vaccine compositions and uses thereof |
| CA3200234A1 (en) | 2020-11-25 | 2022-06-02 | Daryl C. Drummond | Lipid nanoparticles for delivery of nucleic acids, and related methods of use |
| EP4277921A1 (en) | 2021-01-12 | 2023-11-22 | Janssen Pharmaceuticals, Inc. | Fimh mutants, compositions therewith and use thereof |
| WO2022208430A1 (en) | 2021-04-01 | 2022-10-06 | Janssen Pharmaceuticals, Inc. | Production of e. coli o18 bioconjugates |
| WO2022256740A1 (en) | 2021-06-04 | 2022-12-08 | Curia Ip Holdings, Llc | Polymeric fusion proteins and compositions for inducing an immune response against infection |
| US12064479B2 (en) | 2022-05-25 | 2024-08-20 | Akagera Medicines, Inc. | Lipid nanoparticles for delivery of nucleic acids and methods of use thereof |
Citations (185)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US3238190A (en) | 1963-10-23 | 1966-03-01 | Madaus & Co K G Fa Dr | Aescin recovery |
| US3598123A (en) | 1969-04-01 | 1971-08-10 | Alza Corp | Bandage for administering drugs |
| US3598122A (en) | 1969-04-01 | 1971-08-10 | Alza Corp | Bandage for administering drugs |
| US4286592A (en) | 1980-02-04 | 1981-09-01 | Alza Corporation | Therapeutic system for administering drugs to the skin |
| US4314557A (en) | 1980-05-19 | 1982-02-09 | Alza Corporation | Dissolution controlled active agent dispenser |
| US4379454A (en) | 1981-02-17 | 1983-04-12 | Alza Corporation | Dosage for coadministering drug and percutaneous absorption enhancer |
| US4420558A (en) | 1981-02-12 | 1983-12-13 | Janssen Pharmaceutica N.V. | Bright field light microscopic method of enumerating and characterizing subtypes of white blood cells and their precursors |
| US4420461A (en) | 1982-05-26 | 1983-12-13 | Ortho Diagnostic Systems Inc. | Agglutination-inhibition test kit for detecting immune complexes |
| GB2122204B (en) | 1982-05-26 | 1985-12-24 | Ribi Immunochem Research Inc | Refined detoxfied entoxin (lipid a) and anti-tumour compostions thereof |
| US4568343A (en) | 1984-10-09 | 1986-02-04 | Alza Corporation | Skin permeation enhancer compositions |
| EP0172581A2 (en) | 1984-08-24 | 1986-02-26 | Daiichi Seiyaku Co., Ltd. | Disaccharide derivatives |
| US4595654A (en) | 1983-11-07 | 1986-06-17 | Immunomedics Inc. | Method for detecting immune complexes in serum |
| US4614722A (en) | 1983-11-01 | 1986-09-30 | Pasula Mark J | Method and apparatus for measuring the degree of reaction between antigens and leukocyte cellular antibodies |
| EP0198474A1 (en) | 1985-04-15 | 1986-10-22 | SMITHKLINE BEECHAM BIOLOGICALS s.a. | Hepatitis B surface antigen formed by recombinant DNA techniques, vaccines, diagnostics, cell lines and methods of forming same |
| US4659659A (en) | 1985-01-22 | 1987-04-21 | Monsanto Company | Diagnostic method for diseases having an arthritic component |
| US4743540A (en) | 1983-09-27 | 1988-05-10 | Memorial Sloan-Kettering Cancer Center | Method for diagnosis of subclassifications of common varied immunodeficiency disease group |
| US4767402A (en) | 1986-07-08 | 1988-08-30 | Massachusetts Institute Of Technology | Ultrasound enhancement of transdermal drug delivery |
| US4769330A (en) | 1981-12-24 | 1988-09-06 | Health Research, Incorporated | Modified vaccinia virus and methods for making and using the same |
| US4780212A (en) | 1987-07-31 | 1988-10-25 | Massachusetts Institute Of Technology | Ultrasound enchancement of membrane permeability |
| EP0304578A1 (en) | 1987-06-22 | 1989-03-01 | Medeva Holdings B.V. | Peptide comprising hepatitis B surface antigen |
| WO1989001973A2 (en) | 1987-09-02 | 1989-03-09 | Applied Biotechnology, Inc. | Recombinant pox virus for immunization against tumor-associated antigens |
| GB2220211A (en) | 1988-06-29 | 1990-01-04 | Ribi Immunochem Research Inc | Modified lipopolysaccharides |
| US4897268A (en) | 1987-08-03 | 1990-01-30 | Southern Research Institute | Drug delivery system and method of making the same |
| WO1990001496A1 (en) | 1988-08-12 | 1990-02-22 | 3I Research Exploitation Limited | Polypeptides and dna encoding same |
| EP0366412A2 (en) | 1988-10-28 | 1990-05-02 | Exxon Chemical Patents Inc. | Graft polymers of functionalized ethylene-alpha-olefin copolymer with polypropylene, methods of preparation, and use in polypropylene compositions |
| WO1990006951A1 (en) | 1988-12-16 | 1990-06-28 | De Staat Der Nederlanden Vertegenwoordigd Door De Minister Van Welzijn, Volksgezondheid En Cultuur | Pneumolysin mutants and pneumococcal vaccines made therefrom |
| WO1990007936A1 (en) | 1989-01-23 | 1990-07-26 | Chiron Corporation | Recombinant therapies for infection and hyperproliferative disorders |
| US4948587A (en) | 1986-07-08 | 1990-08-14 | Massachusetts Institute Of Technology | Ultrasound enhancement of transbuccal drug delivery |
| US4981684A (en) | 1989-10-24 | 1991-01-01 | Coopers Animal Health Limited | Formation of adjuvant complexes |
| GB2232892A (en) | 1988-02-23 | 1991-01-02 | John Mark Tucker | Occlusive body for administering a physiologically active substance |
| EP0414374A2 (en) | 1989-07-25 | 1991-02-27 | Smithkline Biologicals S.A. | Novel antigens and methods for their preparation |
| EP0109942B1 (en) | 1982-10-18 | 1991-03-06 | Bror Morein | Immunogenic protein or peptide complex, method of producing said complex and the use thereof as an immune stimulant and as a vaccine |
| WO1991002805A2 (en) | 1989-08-18 | 1991-03-07 | Viagene, Inc. | Recombinant retroviruses delivering vector constructs to target cells |
| US5017487A (en) | 1985-04-04 | 1991-05-21 | Hoffmann-La Roche Inc. | Vaccinia DNA |
| US5057540A (en) | 1987-05-29 | 1991-10-15 | Cambridge Biotech Corporation | Saponin adjuvant |
| US5075109A (en) | 1986-10-24 | 1991-12-24 | Southern Research Institute | Method of potentiating an immune response |
| EP0468520A2 (en) | 1990-07-27 | 1992-01-29 | MITSUI TOATSU CHEMICALS, Inc. | Immunostimulatory remedies containing palindromic DNA sequences |
| US5124141A (en) | 1990-06-14 | 1992-06-23 | Flow Incorporated | Method for diagnosing malaria |
| US5147785A (en) | 1983-11-01 | 1992-09-15 | Amtl Corporation | Method and apparatus for measuring the degree of reaction between a foreign entity and white blood cells |
| US5162990A (en) | 1990-06-15 | 1992-11-10 | The United States Of America As Represented By The United States Navy | System and method for quantifying macrophage phagocytosis by computer image analysis |
| WO1993002184A1 (en) | 1991-07-19 | 1993-02-04 | The University Of Queensland | Papilloma virus vaccine |
| WO1993003709A1 (en) | 1991-08-16 | 1993-03-04 | Vical, Inc. | Composition and method for treating cystic fibrosis |
| WO1993010152A1 (en) | 1991-11-16 | 1993-05-27 | Smithkline Beecham Biologicals S.A. | HYBRID PROTEIN BETWEEN CS FROM PLASMODIUM AND HBsAG |
| US5231168A (en) | 1988-09-16 | 1993-07-27 | Statens Seruminstitut | Malaria antigen |
| EP0480981B1 (en) | 1989-07-03 | 1993-10-20 | S.E.P.P.I.C., Societe D'exploitation De Produits Pour Les Industries Chimiques | Injectable multi-phase emulsions |
| JPH05328975A (en) | 1992-06-02 | 1993-12-14 | Takara Shuzo Co Ltd | E1a-f gene |
| WO1993025234A1 (en) | 1992-06-08 | 1993-12-23 | The Regents Of The University Of California | Methods and compositions for targeting specific tissue |
| WO1993025698A1 (en) | 1992-06-10 | 1993-12-23 | The United States Government As Represented By The | Vector particles resistant to inactivation by human serum |
| WO1994000153A1 (en) | 1992-06-25 | 1994-01-06 | Smithkline Beecham Biologicals (S.A.) | Vaccine composition containing adjuvants |
| WO1994000152A1 (en) | 1992-06-25 | 1994-01-06 | Georgetown University | Papillomavirus vaccines |
| US5278302A (en) | 1988-05-26 | 1994-01-11 | University Patents, Inc. | Polynucleotide phosphorodithioates |
| WO1994003622A1 (en) | 1992-07-31 | 1994-02-17 | Imperial College Of Science, Technology & Medicine | D-type retroviral vectors, based on mpmv |
| WO1994005792A1 (en) | 1992-09-03 | 1994-03-17 | The Government Of The United States Of America, As Represented By The Secretary, Department Of Health And Human Services | Self-assembling recombinant papillomavirus capsid proteins |
| US5298396A (en) | 1989-11-15 | 1994-03-29 | National Jewish Center For Immunology And Respiratory Medicine | Method for identifying T cells disease involved in autoimmune disease |
| EP0399843B1 (en) | 1989-05-25 | 1994-07-13 | Chiron Corporation | Adjuvant formulation comprising a submicron oil droplet emulsion |
| WO1994020137A1 (en) | 1993-03-09 | 1994-09-15 | University Of Rochester | Production of human papillomavirus capsid protein and virus-like particles |
| WO1994021292A1 (en) | 1993-03-23 | 1994-09-29 | Smithkline Beecham Biologicals (S.A.) | Vaccine compositions containing 3-o deacylated monophosphoryl lipid a |
| EP0382271B1 (en) | 1989-02-04 | 1994-12-21 | Akzo Nobel N.V. | Tocols as adjuvant in vaccine |
| EP0362279B1 (en) | 1987-05-29 | 1995-01-11 | Cambridge Biotech Corporation | Saponin adjuvant |
| US5411865A (en) | 1993-01-15 | 1995-05-02 | Iasys Corporation | Method of detecting anti-leishmania parasite antibodies |
| US5422109A (en) | 1989-07-03 | 1995-06-06 | Societe D'exploitation De Produits Pour Les Industries Chimiques (S.E.P.P.I.C.) | Fluid vaccines and active principle vehicles containing a metabolizable oil |
| WO1995017209A1 (en) | 1993-12-23 | 1995-06-29 | Smithkline Beecham Biologicals (S.A.) | Vaccines |
| WO1995020600A1 (en) | 1994-01-27 | 1995-08-03 | Aphton Corp. | Immunogens against gonadotropin releasing hormone |
| WO1995026204A1 (en) | 1994-03-25 | 1995-10-05 | Isis Pharmaceuticals, Inc. | Immune stimulation by phosphorothioate oligonucleotide analogs |
| US5457041A (en) | 1994-03-25 | 1995-10-10 | Science Applications International Corporation | Needle array and method of introducing biological substances into living cells using the needle array |
| US5464387A (en) | 1991-07-24 | 1995-11-07 | Alza Corporation | Transdermal delivery device |
| WO1996002555A1 (en) | 1994-07-15 | 1996-02-01 | The University Of Iowa Research Foundation | Immunomodulatory oligonucleotides |
| WO1996011272A2 (en) | 1994-10-07 | 1996-04-18 | Medigene Gesellschaft Für Molekularbiologische Diagnostik, Theraphie Und Technologie Mbh | Papilloma virus-like particles, fusion proteins and process for producing the same |
| WO1996011711A1 (en) | 1994-10-12 | 1996-04-25 | Iscotec Ab | Saponin preparations and use thereof in iscoms |
| WO1996026277A1 (en) | 1995-02-24 | 1996-08-29 | Cantab Pharmaceuticals Research Limited | Polypeptides useful as immunotherapeutic agents and methods of polypeptide preparation |
| US5565209A (en) | 1987-03-17 | 1996-10-15 | Akzo Nobel N.V. | Adjuvant mixture |
| WO1996033739A1 (en) | 1995-04-25 | 1996-10-31 | Smithkline Beecham Biologicals S.A. | Vaccines containing a saponin and a sterol |
| US5591139A (en) | 1994-06-06 | 1997-01-07 | The Regents Of The University Of California | IC-processed microneedles |
| US5595888A (en) | 1983-12-16 | 1997-01-21 | Genentech, Inc. | Recombinant methods of making gamma interferon compositions |
| US5618275A (en) | 1995-10-27 | 1997-04-08 | Sonex International Corporation | Ultrasonic method and apparatus for cosmetic and dermatological applications |
| US5654140A (en) | 1990-05-29 | 1997-08-05 | The United States Of America As Represented By The Department Of Health And Human Services | Cloned human cripto gene and applications thereof |
| US5656016A (en) | 1996-03-18 | 1997-08-12 | Abbott Laboratories | Sonophoretic drug delivery system |
| US5666153A (en) | 1995-10-03 | 1997-09-09 | Virtual Shopping, Inc. | Retractable teleconferencing apparatus |
| US5693531A (en) | 1993-11-24 | 1997-12-02 | The United States Of America As Represented By The Department Of Health And Human Services | Vector systems for the generation of adeno-associated virus particles |
| WO1998001139A1 (en) | 1996-07-03 | 1998-01-15 | Eisai Co., Ltd. | Injections containing lipid a analogues and process for the preparation thereof |
| US5722397A (en) | 1993-11-15 | 1998-03-03 | Altea Technologies, Inc. | Enhancement of transdermal monitoring applications with ultrasound and chemical enhancers |
| WO1998012302A1 (en) | 1996-09-17 | 1998-03-26 | Millennium Pharmaceuticals, Inc. | Weight control pathway genes and uses therefor |
| WO1998016247A1 (en) | 1996-10-11 | 1998-04-23 | The Regents Of The University Of California | Immunostimulatory polynucleotide/immunomodulatory molecule conjugates |
| WO1998020117A1 (en) | 1996-11-05 | 1998-05-14 | Incyte Pharmaceuticals, Inc. | Prostate-specific kallikrein |
| US5795577A (en) | 1986-04-08 | 1998-08-18 | Transgene S.A. | Viral vector coding for a glycoprotein of the virus responsible for A.I.D.S. |
| WO1998037418A2 (en) | 1997-02-25 | 1998-08-27 | Corixa Corporation | Compounds for immunodiagnosis of prostate cancer and methods for their use |
| WO1998043670A2 (en) | 1997-04-01 | 1998-10-08 | Ribi Immunochem Research, Inc. | Aqueous immunologic adjuvant compositions of monophosphoryl lipid a |
| US5840871A (en) | 1997-01-29 | 1998-11-24 | Incyte Pharmaceuticals, Inc. | Prostate-associated kallikrein |
| US5843464A (en) | 1995-06-02 | 1998-12-01 | The Ohio State University | Synthetic chimeric fimbrin peptides |
| US5846758A (en) | 1995-11-30 | 1998-12-08 | His Excellency Ghassan I. Shaker | Method for diagnosing autoimmune diseases |
| WO1998056414A1 (en) | 1997-06-11 | 1998-12-17 | Smithkline Beecham Biologicals S.A. | Oil in water vaccine compositions |
| EP0549074B1 (en) | 1991-12-23 | 1999-01-27 | Dimminaco Ag | Adjuvants |
| WO1999003884A2 (en) | 1997-07-21 | 1999-01-28 | North American Vaccine, Inc. | Modified immunogenic pneumolysin, compositions and their use as vaccines |
| WO1999010008A1 (en) | 1997-08-29 | 1999-03-04 | Aquila Biopharmaceuticals, Inc. | Compositions comprising the adjuvant qs-21 and polysorbate or cyclodextrin as excipient |
| WO1999011241A1 (en) | 1997-09-05 | 1999-03-11 | Smithkline Beecham Biologicals S.A. | Oil in water emulsions containing saponins |
| WO1999012565A1 (en) | 1997-09-05 | 1999-03-18 | Smithkline Beecham Biologicals S.A. | Vaccines |
| US5885211A (en) | 1993-11-15 | 1999-03-23 | Spectrix, Inc. | Microporation of human skin for monitoring the concentration of an analyte |
| WO1999017741A1 (en) | 1997-10-02 | 1999-04-15 | Antex Biologics Inc. | Chlamydia protein, gene sequence and uses thereof |
| WO1999028475A2 (en) | 1997-11-28 | 1999-06-10 | Genset | Chlamydia trachomatis genomic sequence and polypeptides, fragments thereof and uses thereof, in particular for the diagnosis, prevention and treatment of infection |
| US5912166A (en) | 1995-04-21 | 1999-06-15 | Corixa Corporation | Compounds and methods for diagnosis of leishmaniasis |
| WO1999040188A2 (en) | 1998-02-05 | 1999-08-12 | Smithkline Beecham Biologicals S.A. | Tumor-associated antigen derivatives from the mage family, and nucleic acid sequences encoding them, used for the preparation of fusion proteins and of compositions for vaccinations |
| WO1999051748A2 (en) | 1998-04-07 | 1999-10-14 | Corixa Corporation | Fusion proteins of mycobacterium tuberculosis antigens and their uses |
| WO1999053061A2 (en) | 1998-04-15 | 1999-10-21 | Ludwig Institute For Cancer Research | Tumor associated nucleic acids and uses therefor |
| US5981215A (en) | 1995-06-06 | 1999-11-09 | Human Genome Sciences, Inc. | Human criptin growth factor |
| US5993800A (en) | 1995-06-05 | 1999-11-30 | Bristol-Myers Squibb Company | Methods for prolonging the expression of a heterologous gene of interest using soluble CTLA4 molecules and an antiCD40 ligand |
| US6005099A (en) | 1993-11-17 | 1999-12-21 | Laboratoires Om S.A. | Glucosamine disaccharides, method for their preparation, pharmaceutical composition comprising same, and their use |
| US6018678A (en) | 1993-11-15 | 2000-01-25 | Massachusetts Institute Of Technology | Transdermal protein delivery or measurement using low-frequency sonophoresis |
| WO2000004149A2 (en) | 1998-07-14 | 2000-01-27 | Corixa Corporation | Compositions and methods for therapy and diagnosis of prostate cancer |
| US6027732A (en) | 1996-02-21 | 2000-02-22 | Morein; Bror | Iscom or iscom-matrix comprising hydrophobic receptor molecules for antigenic substances |
| US6033928A (en) | 1993-11-02 | 2000-03-07 | Matsushita Electric Industrial Co., Ltd. | Method of manufacturing aggregate of semiconductor micro-needles |
| US6057427A (en) | 1991-11-20 | 2000-05-02 | Trustees Of Dartmouth College | Antibody to cytokine response gene 2(CR2) polypeptide |
| US6106824A (en) | 1993-08-13 | 2000-08-22 | The Rockefeller University | Expression of growth associated protein B-50/GAP-43 in vitro and in vivo |
| US6120769A (en) | 1989-11-03 | 2000-09-19 | Immulogic Pharmaceutical Corporation | Human T cell reactive feline protein (TRFP) isolated from house dust and uses therefor |
| US6218186B1 (en) | 1999-11-12 | 2001-04-17 | Trustees Of The University Of Pennsylvania | HIV-MSCV hybrid viral vector for gene transfer |
| US6231861B1 (en) | 1993-06-02 | 2001-05-15 | New York University | Plasmodium vivax blood stage antigens, antibodies, and diagnostic assays |
| US6261762B1 (en) | 1986-03-03 | 2001-07-17 | Institut Pasteur | Cloned DNA sequences related to the entire genomic RNA of human immunodeficiency virus II (HIV-2), polypeptides encoded by these DNA sequences and the use of these DNA clones polypeptides in diagnostic kits |
| US6309847B1 (en) | 1995-07-05 | 2001-10-30 | Yeda Research And Development Co. Ltd. | Method for detecting or monitoring the effectiveness of treatment of T cell mediated diseases |
| US6316183B1 (en) | 1986-01-22 | 2001-11-13 | Marc Alizon | Nucleic acid-based methods for the detection of human immunodeficiency virus type 2 (HIV-2) |
| US6322532B1 (en) | 1998-06-24 | 2001-11-27 | 3M Innovative Properties Company | Sonophoresis method and apparatus |
| US6375944B1 (en) | 1998-09-25 | 2002-04-23 | The Wistar Institute Of Anatomy And Biology | Methods and compositions for enhancing the immunostimulatory effect of interleukin-12 |
| US6472515B1 (en) | 1999-08-26 | 2002-10-29 | Biovitrum Ab | Response element |
| US6512102B1 (en) | 1998-12-31 | 2003-01-28 | Chiron Corporation | Compositions and methods of diagnosis and treatment using casein kinase I |
| US6544728B1 (en) | 1986-01-22 | 2003-04-08 | Institut Pasteur | Methods and kits for diagnosing human immunodeficiency virus type 2 (HIV-2), proteins of HIV-2, and vaccinating agents for HIV-2 |
| US6544518B1 (en) | 1999-04-19 | 2003-04-08 | Smithkline Beecham Biologicals S.A. | Vaccines |
| US6555653B2 (en) | 1997-05-20 | 2003-04-29 | Corixa Corporation | Compounds for diagnosis of tuberculosis and methods for their use |
| US6587792B1 (en) | 2000-01-11 | 2003-07-01 | Richard A. Thomas | Nuclear packing efficiency |
| US6596501B2 (en) | 1998-02-23 | 2003-07-22 | Fred Hutchinson Cancer Research Center | Method of diagnosing autoimmune disease |
| US6613892B2 (en) | 1994-07-29 | 2003-09-02 | Btg International Inc. | HSV viral vector |
| US6654462B1 (en) | 1996-12-23 | 2003-11-25 | Telefonaktiebolaget Lm Ericsson (Publ) | Line terminal circuit for controlling the common mode voltage level on a transmission line |
| US6660487B2 (en) | 1999-03-10 | 2003-12-09 | The General Hospital Corporation | Treatment of autoimmune disease |
| US6676961B1 (en) | 2002-03-06 | 2004-01-13 | Automated Carrier Technologies, Inc. | Transdermal patch assembly |
| US6682901B2 (en) | 1998-05-05 | 2004-01-27 | Adherex Technologies, Inc. | Methods for diagnosing and evaluating cancer |
| US6685699B1 (en) | 1999-06-09 | 2004-02-03 | Spectrx, Inc. | Self-removing energy absorbing structure for thermal tissue ablation |
| US6692752B1 (en) | 1999-09-08 | 2004-02-17 | Smithkline Beecham Biologicals S.A. | Methods of treating human females susceptible to HSV infection |
| US6713068B1 (en) | 1998-03-03 | 2004-03-30 | Merial | Live recombined vaccines injected with adjuvant |
| US6734172B2 (en) | 1998-11-18 | 2004-05-11 | Pacific Northwest Research Institute | Surface receptor antigen vaccines |
| US6733763B2 (en) | 1991-07-25 | 2004-05-11 | Biogen Idec Inc. | Induction of cytotoxic T-lymphocyte responses |
| US6749856B1 (en) | 1997-09-11 | 2004-06-15 | The United States Of America, As Represented By The Department Of Health And Human Services | Mucosal cytotoxic T lymphocyte responses |
| US6752995B2 (en) | 2002-04-15 | 2004-06-22 | Board Of Regents, The University Of Texas System | Nucleic acid and polypeptide sequences useful as adjuvants |
| US6770445B1 (en) | 1999-02-26 | 2004-08-03 | Pacific Northwest Research Institute | Methods and compositions for diagnosing carcinomas |
| US6783981B1 (en) | 1999-03-17 | 2004-08-31 | Oxford Biomedica (Uk) Limited | Anti-viral vectors |
| US6797276B1 (en) | 1996-11-14 | 2004-09-28 | The United States Of America As Represented By The Secretary Of The Army | Use of penetration enhancers and barrier disruption agents to enhance the transcutaneous immune response |
| US6844192B2 (en) | 2001-06-29 | 2005-01-18 | Wake Forest University | Adenovirus E4 protein variants for virus production |
| US6846489B1 (en) | 1995-04-25 | 2005-01-25 | Smithkline Beecham Biologicals S.A. | Vaccines containing a saponin and a sterol |
| US6846648B2 (en) | 2000-02-01 | 2005-01-25 | Anda Biologicals, S.A. | Method for the rapid detection of whole microorganisms on retaining membranes by use of chaotropic agents |
| US6855322B2 (en) | 2001-01-26 | 2005-02-15 | The United States Of America As Represented By The Secretary Of The Army | Isolation and purification of P. falciparum merozoite protein-142 vaccine |
| US6869607B1 (en) | 1998-01-30 | 2005-03-22 | Intercell Ag | Vaccine formulations |
| US6871477B1 (en) | 1998-04-14 | 2005-03-29 | United Pharmaceutical Manufacturing Co. Limited | Method of manufacturing transdermal patches |
| US6875610B2 (en) | 2000-05-31 | 2005-04-05 | Human Gene Therapy Research Institute | Methods and compositions for efficient gene transfer using transcomplementary vectors |
| US6893820B1 (en) | 2001-01-31 | 2005-05-17 | The Ohio State University Research Foundation | Detection of methylated CpG rich sequences diagnostic for malignant cells |
| US6908453B2 (en) | 2002-01-15 | 2005-06-21 | 3M Innovative Properties Company | Microneedle devices and methods of manufacture |
| US6911434B2 (en) * | 2002-02-04 | 2005-06-28 | Corixa Corporation | Prophylactic and therapeutic treatment of infectious and other diseases with immunoeffector compounds |
| US6919210B1 (en) | 1999-04-07 | 2005-07-19 | Hiroshi Okamoto | Method for identifying autoimmune disease, method for detecting anti-Reg protein autoantibody and diagnostics for autoimmune disease |
| US6919078B2 (en) | 1997-06-11 | 2005-07-19 | Human Genome Sciences, Inc. | Antibodies to human tumor necrosis factor receptor TR9 |
| US6929796B1 (en) | 1995-11-30 | 2005-08-16 | Regents Of The University Of Minnesota | Methods to treat undesirable immune responses |
| US6933123B2 (en) | 2001-04-05 | 2005-08-23 | Yao Xiong Hu | Peptides from the E2, E6, and E7 proteins of human papilloma viruses 16 and 18 for detecting and/or diagnosing cervical and other human papillomavirus associated cancers |
| US6932972B2 (en) | 1998-03-09 | 2005-08-23 | Smithkline Beecham Biologicals S.A. | Combined vaccine compositions |
| US6936255B1 (en) | 1999-09-07 | 2005-08-30 | Smithkline Beecham Biologicals S.A. | Vaccine composition comprising herpes simplex virus and human papilloma virus antigens |
| US6949246B2 (en) | 1995-09-01 | 2005-09-27 | Corixa Corporation | Compounds and methods for diagnosis of tuberculosis |
| US6970739B1 (en) | 1999-10-28 | 2005-11-29 | Hisamitsu Pharmaceutical Co., Inc. | Iontophoresis device |
| US6969704B1 (en) | 2000-08-25 | 2005-11-29 | The Trustees Of Columbia University In The City Of New York | Methods for suppressing early growth response—1protein (Egr-1) to reduce vascular injury in a subject |
| US6974588B1 (en) | 1999-12-07 | 2005-12-13 | Elan Pharma International Limited | Transdermal patch for delivering volatile liquid drugs |
| US6977073B1 (en) | 1997-02-07 | 2005-12-20 | Cem Cezayirli | Method for stimulating an immune response |
| US6979535B2 (en) | 1986-01-22 | 2005-12-27 | Institut Pasteur | Human immunodeficiency virus type 2 (HIV-2) env polypeptide and diagnostic assays |
| US6979730B2 (en) | 1997-03-10 | 2005-12-27 | The Regents Of The University Of California | Nucleic acids encoding prostate stem cell antigen |
| US6991791B2 (en) | 1991-03-18 | 2006-01-31 | New York University School Of Medicine | Anti-TNF antibodies and peptides of human tumor necrosis factor |
| US7001770B1 (en) | 1998-10-15 | 2006-02-21 | Canji, Inc. | Calpain inhibitors and their applications |
| US7008774B2 (en) | 1999-12-01 | 2006-03-07 | The United States Of America As Represented By The Secretary Of The Army | Practical serological assay for the clinical diagnosis of leishmaniasis |
| US7012134B2 (en) | 1998-01-26 | 2006-03-14 | Human Genome Sciences, Inc. | Dendritic enriched secreted lymphocyte activation molecule |
| US7018345B2 (en) | 2002-12-06 | 2006-03-28 | Hisamitsu Pharmaceutical Co., Inc. | Iontophoresis system |
| US7029685B2 (en) | 2001-03-26 | 2006-04-18 | The United States Of America As Represented By The Secretary Of The Army | Plasmodium falciparum AMA-1 protein and uses thereof |
| US7030232B1 (en) | 1996-09-06 | 2006-04-18 | The Regents Of The University Of California | E25A protein, methods for producing and use thereof |
| US7033598B2 (en) | 1996-11-19 | 2006-04-25 | Intrabrain International N.V. | Methods and apparatus for enhanced and controlled delivery of a biologically active agent into the central nervous system of a mammal |
| US7037712B2 (en) | 1994-07-26 | 2006-05-02 | Commonwealth Scientific And Industrial Research Organisation | DNA encoding ovine adenovirus (OAV287) and its use as a viral vector |
| US7052904B2 (en) | 2000-01-31 | 2006-05-30 | The United States Of America As Represented By The Secretary Of The Department Of Health And Human Services | Hybrid adeno-retroviral vector for the transfection of cells |
| US7060276B2 (en) | 2001-03-26 | 2006-06-13 | The United States Of America As Represented By The Secretary Of The Army | Plasmodium falciparum AMA-1 protein and uses thereof |
| US7060802B1 (en) | 2000-09-18 | 2006-06-13 | The Trustees Of Columbia University In The City Of New York | Tumor-associated marker |
| US7067310B2 (en) | 1994-12-01 | 2006-06-27 | Transgene S.A. | Method for the preparation of a viral vector by inter-molecular homologous recombination |
| US7070931B2 (en) | 1995-02-08 | 2006-07-04 | Takara Bio Inc. | Cancer control |
| US7078180B2 (en) | 2001-09-05 | 2006-07-18 | The Children's Hospital Of Philadelphia | Methods and compositions useful for diagnosis, staging, and treatment of cancers and tumors |
| US7084256B2 (en) | 1999-09-24 | 2006-08-01 | Large Scale Biology Corporation | Self antigen vaccines for treating B cell lymphomas and other cancers |
| US7087231B2 (en) | 1987-02-09 | 2006-08-08 | Institut Pasteur | Peptide sequences specific for the hepatic stages of P. falciparum bearing epitopes capable of stimulating the T lymphocytes |
| US7087713B2 (en) | 2000-02-25 | 2006-08-08 | Corixa Corporation | Compounds and methods for diagnosis and immunotherapy of tuberculosis |
| US20080131466A1 (en) * | 2006-09-26 | 2008-06-05 | Infectious Disease Research Institute | Vaccine composition containing synthetic adjuvant |
| WO2009035528A2 (en) | 2007-09-07 | 2009-03-19 | University Of Georgia Research Foundation, Inc. | Synthetic lipid a derivative |
Family Cites Families (59)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US4029762A (en) * | 1971-11-17 | 1977-06-14 | Max-Planck-Gesellschaft Zur Forderung Der Wissenschaften E.V. | Lipid A-preparation |
| US4987237A (en) * | 1983-08-26 | 1991-01-22 | Ribi Immunochem Research, Inc. | Derivatives of monophosphoryl lipid A |
| US4844894A (en) * | 1984-07-12 | 1989-07-04 | Ribi Immunochem Research Inc. | Method of inhibiting the onset of septicemia and endotoxemia |
| US4629722A (en) | 1984-07-12 | 1986-12-16 | Ribi Immunochem Research, Inc. | Method of inhibiting the onset of acute radiation syndrome |
| US5612041A (en) * | 1984-07-17 | 1997-03-18 | Chiron Corporation | Recombinant herpes simplex gD vaccine |
| US5066794A (en) * | 1984-08-24 | 1991-11-19 | Daiichi Pharmaceutical Co., Ltd. | Process for preparing a disaccharide derivative |
| US4746742A (en) | 1985-11-28 | 1988-05-24 | Toho Yakuhin Kogyo Kabushiki Kaisha | Analogs of nonreducing monosaccharide moiety of lipid A |
| US4877611A (en) | 1986-04-15 | 1989-10-31 | Ribi Immunochem Research Inc. | Vaccine containing tumor antigens and adjuvants |
| JPH0755906B2 (en) | 1986-07-01 | 1995-06-14 | 第一製薬株式会社 | Analgesic containing disaturated derivative |
| EP0324455A3 (en) | 1988-01-15 | 1991-03-27 | Hans O. Ribi | Novel polymeric immunological adjuvants |
| US5888519A (en) | 1988-06-02 | 1999-03-30 | The United States Of America As Represented By The Secretary Of The Army | Encapsulated high-concentration lipid a compositions as immunogenic agents to produce human antibodies to prevent or treat gram-negative bacterial infections |
| GB9105992D0 (en) * | 1991-03-21 | 1991-05-08 | Smithkline Beecham Biolog | Vaccine |
| DK0596032T4 (en) | 1991-07-25 | 2004-07-26 | Idec Pharma Corp | Induction of cytotoxic T lymphocyte responses |
| US5530113A (en) * | 1991-10-11 | 1996-06-25 | Eisai Co., Ltd. | Anti-endotoxin compounds |
| AU660325B2 (en) * | 1991-10-11 | 1995-06-22 | Eisai Co. Ltd. | Anti-endotoxin compounds and related molecules and methods |
| US5286718A (en) | 1991-12-31 | 1994-02-15 | Ribi Immunochem Research, Inc. | Method and composition for ameliorating tissue damage due to ischemia and reperfusion |
| US5961970A (en) | 1993-10-29 | 1999-10-05 | Pharmos Corporation | Submicron emulsions as vaccine adjuvants |
| SE9403137D0 (en) | 1994-09-20 | 1994-09-20 | Perstorp Ab | Derivatives of carbohydrates and compositions containing them |
| US5718904A (en) * | 1995-06-02 | 1998-02-17 | American Home Products Corporation | Adjuvants for viral vaccines |
| US6417172B1 (en) * | 1995-06-05 | 2002-07-09 | Eisai Co., Ltd. | Prevention and treatment of pulmonary bacterial infection or symptomatic pulmonary exposure to endotoxin by inhalation of antiendotoxin drugs |
| WO1997011708A1 (en) | 1995-09-29 | 1997-04-03 | Eisai Research Institute | Method for treating alcoholic liver disease |
| JPH10131046A (en) | 1996-10-29 | 1998-05-19 | Nikka Chem Co Ltd | Durable ph-buffering processing of fiber |
| US6491919B2 (en) | 1997-04-01 | 2002-12-10 | Corixa Corporation | Aqueous immunologic adjuvant compostions of monophosphoryl lipid A |
| US7037510B2 (en) | 1997-04-18 | 2006-05-02 | Statens Serum Institut | Hybrids of M. tuberculosis antigens |
| AU7983198A (en) | 1997-06-23 | 1999-01-04 | Ludwig Institute For Cancer Research | Improved methods for inducing an immune response |
| GB9717953D0 (en) | 1997-08-22 | 1997-10-29 | Smithkline Beecham Biolog | Vaccine |
| US6368604B1 (en) * | 1997-09-26 | 2002-04-09 | University Of Maryland Biotechnology Institute | Non-pyrogenic derivatives of lipid A |
| US6488936B1 (en) | 1998-02-12 | 2002-12-03 | Wyeth | Immunogenic composition of interleukin-12 (IL-12), alum, herpes simplex viral (HSV) antigen, and method thereof |
| ATE375803T1 (en) | 1998-05-07 | 2007-11-15 | Corixa Corp | ADJUVANT COMPOSITION AND METHODS OF USE THEREOF |
| WO2000010375A1 (en) | 1998-08-25 | 2000-03-02 | Gallenberg Ronald J | Beach cleaning apparatus and method |
| US6828155B1 (en) | 1998-09-01 | 2004-12-07 | Eisai Co., Ltd. | Method for evaluating lipid a analog-containing injections |
| JP2000095694A (en) * | 1998-09-24 | 2000-04-04 | Sankyo Co Ltd | New medical drug |
| WO2000018929A2 (en) | 1998-09-25 | 2000-04-06 | Smithkline Beecham Biologicals S.A. | Paramyxovirus vaccines |
| CA2773698C (en) * | 1998-10-16 | 2015-05-19 | Glaxosmithkline Biologicals S.A. | Adjuvant systems comprising an immunostimulant adsorbed to a metallic salt particle and vaccines thereof |
| US6261573B1 (en) | 1998-10-30 | 2001-07-17 | Avant Immunotherapeutics, Inc. | Immunoadjuvants |
| WO2000042994A2 (en) | 1999-01-21 | 2000-07-27 | North Shore-Long Island Jewish Research Institute | Inhibition of bacterial dissemination |
| AU769539B2 (en) * | 1999-01-29 | 2004-01-29 | Zoetis Services Llc | Adjuvants for use in vaccines |
| US20030170249A1 (en) | 1999-02-19 | 2003-09-11 | Hakomori Sen-Itiroh | Vaccines directed to cancer-associated carbohydrate antigens |
| WO2001036433A2 (en) | 1999-11-15 | 2001-05-25 | Biomira, Inc. | Synthetic lipid-a analogs and uses thereof |
| GB0000891D0 (en) | 2000-01-14 | 2000-03-08 | Allergy Therapeutics Ltd | Formulation |
| CN1606446A (en) | 2000-05-19 | 2005-04-13 | 科里克萨有限公司 | Method for preventing and treating communicable diseases and other diseases using monosaccharides and disaccharides |
| DE10041515A1 (en) | 2000-08-24 | 2002-03-14 | Gerold Schuler | Process for the production of ready-to-use, antigen-loaded or unloaded, cryopreserved mature dendritic cells |
| AU2002223970A1 (en) | 2000-10-06 | 2002-04-15 | H. Henrich Paradies | Kyberdrug as autovaccines with immune-regulating effects |
| NZ525320A (en) | 2000-10-18 | 2004-10-29 | Glaxosmithkline Biolog S | Combinations of immunostimulatory oligonucleotides (CpG), saponin and optionally lipopolysaccharides as potent vaccine adjuvants |
| US7727974B2 (en) * | 2001-08-10 | 2010-06-01 | Eisai R & D Management Co., Ltd. | Methods of reducing the severity of mucositis |
| US20040161776A1 (en) | 2001-10-23 | 2004-08-19 | Maddon Paul J. | PSMA formulations and uses thereof |
| CA2474402C (en) | 2002-02-04 | 2012-09-11 | Corixa Corporation | Prophylactic and therapeutic treatment of infectious and other diseases with immunoeffector compounds |
| RU2288723C2 (en) * | 2002-02-04 | 2006-12-10 | Корикса Корпорейшн | Preventive and therapeutic method for treating infectious and other diseases by applying immunoeffective compounds |
| AU2003228966C1 (en) | 2002-05-09 | 2010-05-13 | Oncothyreon Inc. | Lipid A and other carbohydrate ligand analogs |
| US20050123550A1 (en) * | 2003-05-12 | 2005-06-09 | Laurent Philippe E. | Molecules enhancing dermal delivery of influenza vaccines |
| FR2862062B1 (en) | 2003-11-06 | 2005-12-23 | Oreal | LIPID A AND TOPICAL COMPOSITION, IN PARTICULAR COSMETIC, COMPRISING IT |
| US20090181078A1 (en) * | 2006-09-26 | 2009-07-16 | Infectious Disease Research Institute | Vaccine composition containing synthetic adjuvant |
| KR101064518B1 (en) | 2007-09-21 | 2011-09-19 | 주식회사 운화 | Plant Stem Cell line Derived from Cambium of Herbaceous Plant With Storage Root and Method for Isolating the Same |
| WO2009083014A1 (en) | 2007-12-27 | 2009-07-09 | Nokia Corporation | Maintaining the integrity of configuration information of a network of access points for use in positioning an apparatus |
| EP2437753B1 (en) | 2009-06-05 | 2016-08-31 | Infectious Disease Research Institute | Synthetic glucopyranosyl lipid adjuvants and vaccine compositions containing them |
| CN104363892A (en) | 2012-02-07 | 2015-02-18 | 传染性疾病研究院 | Improved adjuvant formulations comprising tlr4 agonists and methods of using the same |
| JP5328975B2 (en) | 2012-12-19 | 2013-10-30 | ルネサスエレクトロニクス株式会社 | RF power module |
| CA2909221A1 (en) * | 2013-04-18 | 2014-10-23 | Immune Design Corp. | Gla monotherapy for use in cancer treatment |
| US9463198B2 (en) | 2013-06-04 | 2016-10-11 | Infectious Disease Research Institute | Compositions and methods for reducing or preventing metastasis |
-
2010
- 2010-06-04 EP EP10784178.5A patent/EP2437753B1/en active Active
- 2010-06-04 US US12/794,336 patent/US8722064B2/en active Active
- 2010-06-04 WO PCT/US2010/037466 patent/WO2010141861A1/en active Application Filing
- 2010-06-04 PL PL10784178T patent/PL2437753T3/en unknown
- 2010-06-04 BR BRPI1011072-0A patent/BRPI1011072B1/en active IP Right Grant
- 2010-06-04 PT PT107841785T patent/PT2437753T/en unknown
- 2010-06-04 EP EP16186377.4A patent/EP3124491B1/en active Active
- 2010-06-04 MX MX2014009221A patent/MX360448B/en unknown
- 2010-06-04 AU AU2010256461A patent/AU2010256461B2/en active Active
- 2010-06-04 CN CN201080034214.0A patent/CN102481312B/en active Active
- 2010-06-04 HU HUE10784178A patent/HUE031051T2/en unknown
- 2010-06-04 TW TW104113418A patent/TWI549688B/en active
- 2010-06-04 TW TW099118278A patent/TWI494125B/en active
- 2010-06-04 SI SI201031333A patent/SI2437753T1/en unknown
- 2010-06-04 LT LTEP10784178.5T patent/LT2437753T/en unknown
- 2010-06-04 CA CA2764374A patent/CA2764374C/en active Active
- 2010-06-04 RU RU2011152602/04A patent/RU2560182C2/en active
- 2010-06-04 ES ES10784178.5T patent/ES2606563T3/en active Active
- 2010-06-04 DK DK10784178.5T patent/DK2437753T3/en active
- 2010-06-04 MX MX2011012836A patent/MX2011012836A/en active IP Right Grant
- 2010-06-04 JP JP2012514187A patent/JP5830015B2/en active Active
- 2010-06-04 RU RU2015129468A patent/RU2732574C2/en active
- 2010-06-04 CN CN201510353412.8A patent/CN105131051B/en active Active
-
2011
- 2011-11-29 IL IL216669A patent/IL216669A/en active IP Right Grant
-
2014
- 2014-03-21 US US14/222,481 patent/US9480740B2/en active Active
-
2015
- 2015-08-19 JP JP2015162164A patent/JP2016028042A/en active Pending
- 2015-12-09 IL IL242992A patent/IL242992B/en active IP Right Grant
-
2016
- 2016-10-04 US US15/285,378 patent/US9814772B2/en active Active
- 2016-10-05 CY CY20161100990T patent/CY1118347T1/en unknown
- 2016-11-29 HR HRP20161585TT patent/HRP20161585T1/en unknown
- 2016-11-29 SM SM201600437T patent/SMT201600437B/en unknown
-
2017
- 2017-03-03 JP JP2017040574A patent/JP6251431B2/en active Active
- 2017-10-10 US US15/729,512 patent/US10632191B2/en active Active
-
2020
- 2020-09-10 RU RU2020129844A patent/RU2020129844A/en unknown
Patent Citations (198)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US3238190A (en) | 1963-10-23 | 1966-03-01 | Madaus & Co K G Fa Dr | Aescin recovery |
| US3598123A (en) | 1969-04-01 | 1971-08-10 | Alza Corp | Bandage for administering drugs |
| US3598122A (en) | 1969-04-01 | 1971-08-10 | Alza Corp | Bandage for administering drugs |
| US3598122B1 (en) | 1969-04-01 | 1982-11-23 | ||
| US4286592A (en) | 1980-02-04 | 1981-09-01 | Alza Corporation | Therapeutic system for administering drugs to the skin |
| US4314557A (en) | 1980-05-19 | 1982-02-09 | Alza Corporation | Dissolution controlled active agent dispenser |
| US4420558A (en) | 1981-02-12 | 1983-12-13 | Janssen Pharmaceutica N.V. | Bright field light microscopic method of enumerating and characterizing subtypes of white blood cells and their precursors |
| US4379454A (en) | 1981-02-17 | 1983-04-12 | Alza Corporation | Dosage for coadministering drug and percutaneous absorption enhancer |
| US4769330A (en) | 1981-12-24 | 1988-09-06 | Health Research, Incorporated | Modified vaccinia virus and methods for making and using the same |
| US4420461A (en) | 1982-05-26 | 1983-12-13 | Ortho Diagnostic Systems Inc. | Agglutination-inhibition test kit for detecting immune complexes |
| GB2122204B (en) | 1982-05-26 | 1985-12-24 | Ribi Immunochem Research Inc | Refined detoxfied entoxin (lipid a) and anti-tumour compostions thereof |
| EP0109942B1 (en) | 1982-10-18 | 1991-03-06 | Bror Morein | Immunogenic protein or peptide complex, method of producing said complex and the use thereof as an immune stimulant and as a vaccine |
| US4743540A (en) | 1983-09-27 | 1988-05-10 | Memorial Sloan-Kettering Cancer Center | Method for diagnosis of subclassifications of common varied immunodeficiency disease group |
| US5147785A (en) | 1983-11-01 | 1992-09-15 | Amtl Corporation | Method and apparatus for measuring the degree of reaction between a foreign entity and white blood cells |
| US4614722A (en) | 1983-11-01 | 1986-09-30 | Pasula Mark J | Method and apparatus for measuring the degree of reaction between antigens and leukocyte cellular antibodies |
| US4595654A (en) | 1983-11-07 | 1986-06-17 | Immunomedics Inc. | Method for detecting immune complexes in serum |
| US5595888A (en) | 1983-12-16 | 1997-01-21 | Genentech, Inc. | Recombinant methods of making gamma interferon compositions |
| EP0172581A2 (en) | 1984-08-24 | 1986-02-26 | Daiichi Seiyaku Co., Ltd. | Disaccharide derivatives |
| US4568343A (en) | 1984-10-09 | 1986-02-04 | Alza Corporation | Skin permeation enhancer compositions |
| US4659659A (en) | 1985-01-22 | 1987-04-21 | Monsanto Company | Diagnostic method for diseases having an arthritic component |
| US5017487A (en) | 1985-04-04 | 1991-05-21 | Hoffmann-La Roche Inc. | Vaccinia DNA |
| EP0198474A1 (en) | 1985-04-15 | 1986-10-22 | SMITHKLINE BEECHAM BIOLOGICALS s.a. | Hepatitis B surface antigen formed by recombinant DNA techniques, vaccines, diagnostics, cell lines and methods of forming same |
| US6979535B2 (en) | 1986-01-22 | 2005-12-27 | Institut Pasteur | Human immunodeficiency virus type 2 (HIV-2) env polypeptide and diagnostic assays |
| US6544728B1 (en) | 1986-01-22 | 2003-04-08 | Institut Pasteur | Methods and kits for diagnosing human immunodeficiency virus type 2 (HIV-2), proteins of HIV-2, and vaccinating agents for HIV-2 |
| US6316183B1 (en) | 1986-01-22 | 2001-11-13 | Marc Alizon | Nucleic acid-based methods for the detection of human immunodeficiency virus type 2 (HIV-2) |
| US6261762B1 (en) | 1986-03-03 | 2001-07-17 | Institut Pasteur | Cloned DNA sequences related to the entire genomic RNA of human immunodeficiency virus II (HIV-2), polypeptides encoded by these DNA sequences and the use of these DNA clones polypeptides in diagnostic kits |
| US5795577A (en) | 1986-04-08 | 1998-08-18 | Transgene S.A. | Viral vector coding for a glycoprotein of the virus responsible for A.I.D.S. |
| US4948587A (en) | 1986-07-08 | 1990-08-14 | Massachusetts Institute Of Technology | Ultrasound enhancement of transbuccal drug delivery |
| US4767402A (en) | 1986-07-08 | 1988-08-30 | Massachusetts Institute Of Technology | Ultrasound enhancement of transdermal drug delivery |
| US5075109A (en) | 1986-10-24 | 1991-12-24 | Southern Research Institute | Method of potentiating an immune response |
| US7087231B2 (en) | 1987-02-09 | 2006-08-08 | Institut Pasteur | Peptide sequences specific for the hepatic stages of P. falciparum bearing epitopes capable of stimulating the T lymphocytes |
| US5565209A (en) | 1987-03-17 | 1996-10-15 | Akzo Nobel N.V. | Adjuvant mixture |
| US5057540A (en) | 1987-05-29 | 1991-10-15 | Cambridge Biotech Corporation | Saponin adjuvant |
| EP0362279B1 (en) | 1987-05-29 | 1995-01-11 | Cambridge Biotech Corporation | Saponin adjuvant |
| EP0304578A1 (en) | 1987-06-22 | 1989-03-01 | Medeva Holdings B.V. | Peptide comprising hepatitis B surface antigen |
| US4780212A (en) | 1987-07-31 | 1988-10-25 | Massachusetts Institute Of Technology | Ultrasound enchancement of membrane permeability |
| US4897268A (en) | 1987-08-03 | 1990-01-30 | Southern Research Institute | Drug delivery system and method of making the same |
| WO1989001973A2 (en) | 1987-09-02 | 1989-03-09 | Applied Biotechnology, Inc. | Recombinant pox virus for immunization against tumor-associated antigens |
| GB2232892A (en) | 1988-02-23 | 1991-01-02 | John Mark Tucker | Occlusive body for administering a physiologically active substance |
| US5278302A (en) | 1988-05-26 | 1994-01-11 | University Patents, Inc. | Polynucleotide phosphorodithioates |
| GB2220211A (en) | 1988-06-29 | 1990-01-04 | Ribi Immunochem Research Inc | Modified lipopolysaccharides |
| US4912094A (en) | 1988-06-29 | 1990-03-27 | Ribi Immunochem Research, Inc. | Modified lipopolysaccharides and process of preparation |
| US4912094B1 (en) | 1988-06-29 | 1994-02-15 | Ribi Immunochem Research Inc. | Modified lipopolysaccharides and process of preparation |
| WO1990001496A1 (en) | 1988-08-12 | 1990-02-22 | 3I Research Exploitation Limited | Polypeptides and dna encoding same |
| US5231168A (en) | 1988-09-16 | 1993-07-27 | Statens Seruminstitut | Malaria antigen |
| EP0366412A2 (en) | 1988-10-28 | 1990-05-02 | Exxon Chemical Patents Inc. | Graft polymers of functionalized ethylene-alpha-olefin copolymer with polypropylene, methods of preparation, and use in polypropylene compositions |
| WO1990006951A1 (en) | 1988-12-16 | 1990-06-28 | De Staat Der Nederlanden Vertegenwoordigd Door De Minister Van Welzijn, Volksgezondheid En Cultuur | Pneumolysin mutants and pneumococcal vaccines made therefrom |
| WO1990007936A1 (en) | 1989-01-23 | 1990-07-26 | Chiron Corporation | Recombinant therapies for infection and hyperproliferative disorders |
| EP0382271B1 (en) | 1989-02-04 | 1994-12-21 | Akzo Nobel N.V. | Tocols as adjuvant in vaccine |
| EP0399843B1 (en) | 1989-05-25 | 1994-07-13 | Chiron Corporation | Adjuvant formulation comprising a submicron oil droplet emulsion |
| EP0480982B2 (en) | 1989-07-03 | 1997-11-12 | S.E.P.P.I.C., Societe D'exploitation De Produits Pour Les Industries Chimiques | Vaccines and vectors with liquid active principles containing an oil which can be metabolised |
| US5424067A (en) | 1989-07-03 | 1995-06-13 | Societe D'exploitation De Produits Pour Les Industries Chimiques (S.E.P.P.I.C.) | Injectable multi-phase emulsions |
| US5422109A (en) | 1989-07-03 | 1995-06-06 | Societe D'exploitation De Produits Pour Les Industries Chimiques (S.E.P.P.I.C.) | Fluid vaccines and active principle vehicles containing a metabolizable oil |
| EP0480981B1 (en) | 1989-07-03 | 1993-10-20 | S.E.P.P.I.C., Societe D'exploitation De Produits Pour Les Industries Chimiques | Injectable multi-phase emulsions |
| EP0414374A2 (en) | 1989-07-25 | 1991-02-27 | Smithkline Biologicals S.A. | Novel antigens and methods for their preparation |
| WO1991002805A2 (en) | 1989-08-18 | 1991-03-07 | Viagene, Inc. | Recombinant retroviruses delivering vector constructs to target cells |
| US4981684A (en) | 1989-10-24 | 1991-01-01 | Coopers Animal Health Limited | Formation of adjuvant complexes |
| US6120769A (en) | 1989-11-03 | 2000-09-19 | Immulogic Pharmaceutical Corporation | Human T cell reactive feline protein (TRFP) isolated from house dust and uses therefor |
| US5298396A (en) | 1989-11-15 | 1994-03-29 | National Jewish Center For Immunology And Respiratory Medicine | Method for identifying T cells disease involved in autoimmune disease |
| US5654140A (en) | 1990-05-29 | 1997-08-05 | The United States Of America As Represented By The Department Of Health And Human Services | Cloned human cripto gene and applications thereof |
| US5124141A (en) | 1990-06-14 | 1992-06-23 | Flow Incorporated | Method for diagnosing malaria |
| US5162990A (en) | 1990-06-15 | 1992-11-10 | The United States Of America As Represented By The United States Navy | System and method for quantifying macrophage phagocytosis by computer image analysis |
| EP0468520A2 (en) | 1990-07-27 | 1992-01-29 | MITSUI TOATSU CHEMICALS, Inc. | Immunostimulatory remedies containing palindromic DNA sequences |
| US6991791B2 (en) | 1991-03-18 | 2006-01-31 | New York University School Of Medicine | Anti-TNF antibodies and peptides of human tumor necrosis factor |
| WO1993002184A1 (en) | 1991-07-19 | 1993-02-04 | The University Of Queensland | Papilloma virus vaccine |
| US5464387A (en) | 1991-07-24 | 1995-11-07 | Alza Corporation | Transdermal delivery device |
| US6733763B2 (en) | 1991-07-25 | 2004-05-11 | Biogen Idec Inc. | Induction of cytotoxic T-lymphocyte responses |
| WO1993003709A1 (en) | 1991-08-16 | 1993-03-04 | Vical, Inc. | Composition and method for treating cystic fibrosis |
| WO1993010152A1 (en) | 1991-11-16 | 1993-05-27 | Smithkline Beecham Biologicals S.A. | HYBRID PROTEIN BETWEEN CS FROM PLASMODIUM AND HBsAG |
| US6057427A (en) | 1991-11-20 | 2000-05-02 | Trustees Of Dartmouth College | Antibody to cytokine response gene 2(CR2) polypeptide |
| EP0549074B1 (en) | 1991-12-23 | 1999-01-27 | Dimminaco Ag | Adjuvants |
| JPH05328975A (en) | 1992-06-02 | 1993-12-14 | Takara Shuzo Co Ltd | E1a-f gene |
| WO1993025234A1 (en) | 1992-06-08 | 1993-12-23 | The Regents Of The University Of California | Methods and compositions for targeting specific tissue |
| WO1993025698A1 (en) | 1992-06-10 | 1993-12-23 | The United States Government As Represented By The | Vector particles resistant to inactivation by human serum |
| WO1994000152A1 (en) | 1992-06-25 | 1994-01-06 | Georgetown University | Papillomavirus vaccines |
| WO1994000153A1 (en) | 1992-06-25 | 1994-01-06 | Smithkline Beecham Biologicals (S.A.) | Vaccine composition containing adjuvants |
| EP0761231B1 (en) | 1992-06-25 | 2000-01-12 | SMITHKLINE BEECHAM BIOLOGICALS s.a. | Vaccine composition containing adjuvants |
| WO1994003622A1 (en) | 1992-07-31 | 1994-02-17 | Imperial College Of Science, Technology & Medicine | D-type retroviral vectors, based on mpmv |
| WO1994005792A1 (en) | 1992-09-03 | 1994-03-17 | The Government Of The United States Of America, As Represented By The Secretary, Department Of Health And Human Services | Self-assembling recombinant papillomavirus capsid proteins |
| US5411865A (en) | 1993-01-15 | 1995-05-02 | Iasys Corporation | Method of detecting anti-leishmania parasite antibodies |
| US5719263A (en) | 1993-01-15 | 1998-02-17 | Corixa Corporation | 230Kd antigen present in Leishmania species |
| WO1994020137A1 (en) | 1993-03-09 | 1994-09-15 | University Of Rochester | Production of human papillomavirus capsid protein and virus-like particles |
| WO1994021292A1 (en) | 1993-03-23 | 1994-09-29 | Smithkline Beecham Biologicals (S.A.) | Vaccine compositions containing 3-o deacylated monophosphoryl lipid a |
| US6706872B1 (en) | 1993-06-02 | 2004-03-16 | New York University | Polynucleotides encoding Plasmodium vivax blood stage antigens |
| US6231861B1 (en) | 1993-06-02 | 2001-05-15 | New York University | Plasmodium vivax blood stage antigens, antibodies, and diagnostic assays |
| US6106824A (en) | 1993-08-13 | 2000-08-22 | The Rockefeller University | Expression of growth associated protein B-50/GAP-43 in vitro and in vivo |
| US6033928A (en) | 1993-11-02 | 2000-03-07 | Matsushita Electric Industrial Co., Ltd. | Method of manufacturing aggregate of semiconductor micro-needles |
| US6018678A (en) | 1993-11-15 | 2000-01-25 | Massachusetts Institute Of Technology | Transdermal protein delivery or measurement using low-frequency sonophoresis |
| US5722397A (en) | 1993-11-15 | 1998-03-03 | Altea Technologies, Inc. | Enhancement of transdermal monitoring applications with ultrasound and chemical enhancers |
| US5885211A (en) | 1993-11-15 | 1999-03-23 | Spectrix, Inc. | Microporation of human skin for monitoring the concentration of an analyte |
| US6005099A (en) | 1993-11-17 | 1999-12-21 | Laboratoires Om S.A. | Glucosamine disaccharides, method for their preparation, pharmaceutical composition comprising same, and their use |
| EP0729473B1 (en) | 1993-11-17 | 2000-08-23 | OM Pharma | Glucosamine disaccharides, method for their preparation, pharmaceutical composition comprising same, and their use |
| US5693531A (en) | 1993-11-24 | 1997-12-02 | The United States Of America As Represented By The Department Of Health And Human Services | Vector systems for the generation of adeno-associated virus particles |
| WO1995017209A1 (en) | 1993-12-23 | 1995-06-29 | Smithkline Beecham Biologicals (S.A.) | Vaccines |
| WO1995017210A1 (en) | 1993-12-23 | 1995-06-29 | Smithkline Beecham Biologicals (S.A.) | Vaccines |
| US7029678B2 (en) | 1993-12-23 | 2006-04-18 | Smithkline Beecham Biologicals (S.A.) | Vaccines |
| WO1995020600A1 (en) | 1994-01-27 | 1995-08-03 | Aphton Corp. | Immunogens against gonadotropin releasing hormone |
| US5457041A (en) | 1994-03-25 | 1995-10-10 | Science Applications International Corporation | Needle array and method of introducing biological substances into living cells using the needle array |
| WO1995026204A1 (en) | 1994-03-25 | 1995-10-05 | Isis Pharmaceuticals, Inc. | Immune stimulation by phosphorothioate oligonucleotide analogs |
| US5591139A (en) | 1994-06-06 | 1997-01-07 | The Regents Of The University Of California | IC-processed microneedles |
| WO1996002555A1 (en) | 1994-07-15 | 1996-02-01 | The University Of Iowa Research Foundation | Immunomodulatory oligonucleotides |
| US7037712B2 (en) | 1994-07-26 | 2006-05-02 | Commonwealth Scientific And Industrial Research Organisation | DNA encoding ovine adenovirus (OAV287) and its use as a viral vector |
| US6613892B2 (en) | 1994-07-29 | 2003-09-02 | Btg International Inc. | HSV viral vector |
| WO1996011272A2 (en) | 1994-10-07 | 1996-04-18 | Medigene Gesellschaft Für Molekularbiologische Diagnostik, Theraphie Und Technologie Mbh | Papilloma virus-like particles, fusion proteins and process for producing the same |
| WO1996011711A1 (en) | 1994-10-12 | 1996-04-25 | Iscotec Ab | Saponin preparations and use thereof in iscoms |
| US7067310B2 (en) | 1994-12-01 | 2006-06-27 | Transgene S.A. | Method for the preparation of a viral vector by inter-molecular homologous recombination |
| US7070931B2 (en) | 1995-02-08 | 2006-07-04 | Takara Bio Inc. | Cancer control |
| WO1996026277A1 (en) | 1995-02-24 | 1996-08-29 | Cantab Pharmaceuticals Research Limited | Polypeptides useful as immunotherapeutic agents and methods of polypeptide preparation |
| US5912166A (en) | 1995-04-21 | 1999-06-15 | Corixa Corporation | Compounds and methods for diagnosis of leishmaniasis |
| WO1996033739A1 (en) | 1995-04-25 | 1996-10-31 | Smithkline Beecham Biologicals S.A. | Vaccines containing a saponin and a sterol |
| US6846489B1 (en) | 1995-04-25 | 2005-01-25 | Smithkline Beecham Biologicals S.A. | Vaccines containing a saponin and a sterol |
| US5843464A (en) | 1995-06-02 | 1998-12-01 | The Ohio State University | Synthetic chimeric fimbrin peptides |
| US5993800A (en) | 1995-06-05 | 1999-11-30 | Bristol-Myers Squibb Company | Methods for prolonging the expression of a heterologous gene of interest using soluble CTLA4 molecules and an antiCD40 ligand |
| US5981215A (en) | 1995-06-06 | 1999-11-09 | Human Genome Sciences, Inc. | Human criptin growth factor |
| US6309847B1 (en) | 1995-07-05 | 2001-10-30 | Yeda Research And Development Co. Ltd. | Method for detecting or monitoring the effectiveness of treatment of T cell mediated diseases |
| US6949246B2 (en) | 1995-09-01 | 2005-09-27 | Corixa Corporation | Compounds and methods for diagnosis of tuberculosis |
| US5666153A (en) | 1995-10-03 | 1997-09-09 | Virtual Shopping, Inc. | Retractable teleconferencing apparatus |
| US5618275A (en) | 1995-10-27 | 1997-04-08 | Sonex International Corporation | Ultrasonic method and apparatus for cosmetic and dermatological applications |
| US5846758A (en) | 1995-11-30 | 1998-12-08 | His Excellency Ghassan I. Shaker | Method for diagnosing autoimmune diseases |
| US6929796B1 (en) | 1995-11-30 | 2005-08-16 | Regents Of The University Of Minnesota | Methods to treat undesirable immune responses |
| US6027732A (en) | 1996-02-21 | 2000-02-22 | Morein; Bror | Iscom or iscom-matrix comprising hydrophobic receptor molecules for antigenic substances |
| US5656016A (en) | 1996-03-18 | 1997-08-12 | Abbott Laboratories | Sonophoretic drug delivery system |
| WO1998001139A1 (en) | 1996-07-03 | 1998-01-15 | Eisai Co., Ltd. | Injections containing lipid a analogues and process for the preparation thereof |
| US7030232B1 (en) | 1996-09-06 | 2006-04-18 | The Regents Of The University Of California | E25A protein, methods for producing and use thereof |
| US5955306A (en) | 1996-09-17 | 1999-09-21 | Millenium Pharmaceuticals, Inc. | Genes encoding proteins that interact with the tub protein |
| WO1998012302A1 (en) | 1996-09-17 | 1998-03-26 | Millennium Pharmaceuticals, Inc. | Weight control pathway genes and uses therefor |
| WO1998016247A1 (en) | 1996-10-11 | 1998-04-23 | The Regents Of The University Of California | Immunostimulatory polynucleotide/immunomodulatory molecule conjugates |
| WO1998020117A1 (en) | 1996-11-05 | 1998-05-14 | Incyte Pharmaceuticals, Inc. | Prostate-specific kallikrein |
| US5786148A (en) | 1996-11-05 | 1998-07-28 | Incyte Pharmaceuticals, Inc. | Polynucleotides encoding a novel prostate-specific kallikrein |
| US6797276B1 (en) | 1996-11-14 | 2004-09-28 | The United States Of America As Represented By The Secretary Of The Army | Use of penetration enhancers and barrier disruption agents to enhance the transcutaneous immune response |
| US7033598B2 (en) | 1996-11-19 | 2006-04-25 | Intrabrain International N.V. | Methods and apparatus for enhanced and controlled delivery of a biologically active agent into the central nervous system of a mammal |
| US6654462B1 (en) | 1996-12-23 | 2003-11-25 | Telefonaktiebolaget Lm Ericsson (Publ) | Line terminal circuit for controlling the common mode voltage level on a transmission line |
| US5840871A (en) | 1997-01-29 | 1998-11-24 | Incyte Pharmaceuticals, Inc. | Prostate-associated kallikrein |
| US6977073B1 (en) | 1997-02-07 | 2005-12-20 | Cem Cezayirli | Method for stimulating an immune response |
| WO1998037418A2 (en) | 1997-02-25 | 1998-08-27 | Corixa Corporation | Compounds for immunodiagnosis of prostate cancer and methods for their use |
| US6979730B2 (en) | 1997-03-10 | 2005-12-27 | The Regents Of The University Of California | Nucleic acids encoding prostate stem cell antigen |
| WO1998043670A2 (en) | 1997-04-01 | 1998-10-08 | Ribi Immunochem Research, Inc. | Aqueous immunologic adjuvant compositions of monophosphoryl lipid a |
| US6555653B2 (en) | 1997-05-20 | 2003-04-29 | Corixa Corporation | Compounds for diagnosis of tuberculosis and methods for their use |
| US6919078B2 (en) | 1997-06-11 | 2005-07-19 | Human Genome Sciences, Inc. | Antibodies to human tumor necrosis factor receptor TR9 |
| WO1998056414A1 (en) | 1997-06-11 | 1998-12-17 | Smithkline Beecham Biologicals S.A. | Oil in water vaccine compositions |
| WO1999003884A2 (en) | 1997-07-21 | 1999-01-28 | North American Vaccine, Inc. | Modified immunogenic pneumolysin, compositions and their use as vaccines |
| WO1999010008A1 (en) | 1997-08-29 | 1999-03-04 | Aquila Biopharmaceuticals, Inc. | Compositions comprising the adjuvant qs-21 and polysorbate or cyclodextrin as excipient |
| WO1999011241A1 (en) | 1997-09-05 | 1999-03-11 | Smithkline Beecham Biologicals S.A. | Oil in water emulsions containing saponins |
| WO1999012565A1 (en) | 1997-09-05 | 1999-03-18 | Smithkline Beecham Biologicals S.A. | Vaccines |
| US6749856B1 (en) | 1997-09-11 | 2004-06-15 | The United States Of America, As Represented By The Department Of Health And Human Services | Mucosal cytotoxic T lymphocyte responses |
| WO1999017741A1 (en) | 1997-10-02 | 1999-04-15 | Antex Biologics Inc. | Chlamydia protein, gene sequence and uses thereof |
| WO1999028475A2 (en) | 1997-11-28 | 1999-06-10 | Genset | Chlamydia trachomatis genomic sequence and polypeptides, fragments thereof and uses thereof, in particular for the diagnosis, prevention and treatment of infection |
| US7012134B2 (en) | 1998-01-26 | 2006-03-14 | Human Genome Sciences, Inc. | Dendritic enriched secreted lymphocyte activation molecule |
| US6869607B1 (en) | 1998-01-30 | 2005-03-22 | Intercell Ag | Vaccine formulations |
| WO1999040188A2 (en) | 1998-02-05 | 1999-08-12 | Smithkline Beecham Biologicals S.A. | Tumor-associated antigen derivatives from the mage family, and nucleic acid sequences encoding them, used for the preparation of fusion proteins and of compositions for vaccinations |
| US6596501B2 (en) | 1998-02-23 | 2003-07-22 | Fred Hutchinson Cancer Research Center | Method of diagnosing autoimmune disease |
| US6713068B1 (en) | 1998-03-03 | 2004-03-30 | Merial | Live recombined vaccines injected with adjuvant |
| US6932972B2 (en) | 1998-03-09 | 2005-08-23 | Smithkline Beecham Biologicals S.A. | Combined vaccine compositions |
| WO1999051748A2 (en) | 1998-04-07 | 1999-10-14 | Corixa Corporation | Fusion proteins of mycobacterium tuberculosis antigens and their uses |
| US6871477B1 (en) | 1998-04-14 | 2005-03-29 | United Pharmaceutical Manufacturing Co. Limited | Method of manufacturing transdermal patches |
| WO1999053061A2 (en) | 1998-04-15 | 1999-10-21 | Ludwig Institute For Cancer Research | Tumor associated nucleic acids and uses therefor |
| US6682901B2 (en) | 1998-05-05 | 2004-01-27 | Adherex Technologies, Inc. | Methods for diagnosing and evaluating cancer |
| US6322532B1 (en) | 1998-06-24 | 2001-11-27 | 3M Innovative Properties Company | Sonophoresis method and apparatus |
| WO2000004149A2 (en) | 1998-07-14 | 2000-01-27 | Corixa Corporation | Compositions and methods for therapy and diagnosis of prostate cancer |
| US6375944B1 (en) | 1998-09-25 | 2002-04-23 | The Wistar Institute Of Anatomy And Biology | Methods and compositions for enhancing the immunostimulatory effect of interleukin-12 |
| US7001770B1 (en) | 1998-10-15 | 2006-02-21 | Canji, Inc. | Calpain inhibitors and their applications |
| US6734172B2 (en) | 1998-11-18 | 2004-05-11 | Pacific Northwest Research Institute | Surface receptor antigen vaccines |
| US6512102B1 (en) | 1998-12-31 | 2003-01-28 | Chiron Corporation | Compositions and methods of diagnosis and treatment using casein kinase I |
| US6770445B1 (en) | 1999-02-26 | 2004-08-03 | Pacific Northwest Research Institute | Methods and compositions for diagnosing carcinomas |
| US6660487B2 (en) | 1999-03-10 | 2003-12-09 | The General Hospital Corporation | Treatment of autoimmune disease |
| US6783981B1 (en) | 1999-03-17 | 2004-08-31 | Oxford Biomedica (Uk) Limited | Anti-viral vectors |
| US6919210B1 (en) | 1999-04-07 | 2005-07-19 | Hiroshi Okamoto | Method for identifying autoimmune disease, method for detecting anti-Reg protein autoantibody and diagnostics for autoimmune disease |
| US6544518B1 (en) | 1999-04-19 | 2003-04-08 | Smithkline Beecham Biologicals S.A. | Vaccines |
| US6685699B1 (en) | 1999-06-09 | 2004-02-03 | Spectrx, Inc. | Self-removing energy absorbing structure for thermal tissue ablation |
| US6472515B1 (en) | 1999-08-26 | 2002-10-29 | Biovitrum Ab | Response element |
| US6936255B1 (en) | 1999-09-07 | 2005-08-30 | Smithkline Beecham Biologicals S.A. | Vaccine composition comprising herpes simplex virus and human papilloma virus antigens |
| US6692752B1 (en) | 1999-09-08 | 2004-02-17 | Smithkline Beecham Biologicals S.A. | Methods of treating human females susceptible to HSV infection |
| US7084256B2 (en) | 1999-09-24 | 2006-08-01 | Large Scale Biology Corporation | Self antigen vaccines for treating B cell lymphomas and other cancers |
| US6970739B1 (en) | 1999-10-28 | 2005-11-29 | Hisamitsu Pharmaceutical Co., Inc. | Iontophoresis device |
| US6218186B1 (en) | 1999-11-12 | 2001-04-17 | Trustees Of The University Of Pennsylvania | HIV-MSCV hybrid viral vector for gene transfer |
| US7008774B2 (en) | 1999-12-01 | 2006-03-07 | The United States Of America As Represented By The Secretary Of The Army | Practical serological assay for the clinical diagnosis of leishmaniasis |
| US6974588B1 (en) | 1999-12-07 | 2005-12-13 | Elan Pharma International Limited | Transdermal patch for delivering volatile liquid drugs |
| US6587792B1 (en) | 2000-01-11 | 2003-07-01 | Richard A. Thomas | Nuclear packing efficiency |
| US7052904B2 (en) | 2000-01-31 | 2006-05-30 | The United States Of America As Represented By The Secretary Of The Department Of Health And Human Services | Hybrid adeno-retroviral vector for the transfection of cells |
| US6846648B2 (en) | 2000-02-01 | 2005-01-25 | Anda Biologicals, S.A. | Method for the rapid detection of whole microorganisms on retaining membranes by use of chaotropic agents |
| US7087713B2 (en) | 2000-02-25 | 2006-08-08 | Corixa Corporation | Compounds and methods for diagnosis and immunotherapy of tuberculosis |
| US6875610B2 (en) | 2000-05-31 | 2005-04-05 | Human Gene Therapy Research Institute | Methods and compositions for efficient gene transfer using transcomplementary vectors |
| US6969704B1 (en) | 2000-08-25 | 2005-11-29 | The Trustees Of Columbia University In The City Of New York | Methods for suppressing early growth response—1protein (Egr-1) to reduce vascular injury in a subject |
| US7060802B1 (en) | 2000-09-18 | 2006-06-13 | The Trustees Of Columbia University In The City Of New York | Tumor-associated marker |
| US6855322B2 (en) | 2001-01-26 | 2005-02-15 | The United States Of America As Represented By The Secretary Of The Army | Isolation and purification of P. falciparum merozoite protein-142 vaccine |
| US6893820B1 (en) | 2001-01-31 | 2005-05-17 | The Ohio State University Research Foundation | Detection of methylated CpG rich sequences diagnostic for malignant cells |
| US7060276B2 (en) | 2001-03-26 | 2006-06-13 | The United States Of America As Represented By The Secretary Of The Army | Plasmodium falciparum AMA-1 protein and uses thereof |
| US7029685B2 (en) | 2001-03-26 | 2006-04-18 | The United States Of America As Represented By The Secretary Of The Army | Plasmodium falciparum AMA-1 protein and uses thereof |
| US6933123B2 (en) | 2001-04-05 | 2005-08-23 | Yao Xiong Hu | Peptides from the E2, E6, and E7 proteins of human papilloma viruses 16 and 18 for detecting and/or diagnosing cervical and other human papillomavirus associated cancers |
| US6844192B2 (en) | 2001-06-29 | 2005-01-18 | Wake Forest University | Adenovirus E4 protein variants for virus production |
| US7078180B2 (en) | 2001-09-05 | 2006-07-18 | The Children's Hospital Of Philadelphia | Methods and compositions useful for diagnosis, staging, and treatment of cancers and tumors |
| US6908453B2 (en) | 2002-01-15 | 2005-06-21 | 3M Innovative Properties Company | Microneedle devices and methods of manufacture |
| US6911434B2 (en) * | 2002-02-04 | 2005-06-28 | Corixa Corporation | Prophylactic and therapeutic treatment of infectious and other diseases with immunoeffector compounds |
| US6676961B1 (en) | 2002-03-06 | 2004-01-13 | Automated Carrier Technologies, Inc. | Transdermal patch assembly |
| US6752995B2 (en) | 2002-04-15 | 2004-06-22 | Board Of Regents, The University Of Texas System | Nucleic acid and polypeptide sequences useful as adjuvants |
| US7018345B2 (en) | 2002-12-06 | 2006-03-28 | Hisamitsu Pharmaceutical Co., Inc. | Iontophoresis system |
| US20080131466A1 (en) * | 2006-09-26 | 2008-06-05 | Infectious Disease Research Institute | Vaccine composition containing synthetic adjuvant |
| WO2009035528A2 (en) | 2007-09-07 | 2009-03-19 | University Of Georgia Research Foundation, Inc. | Synthetic lipid a derivative |
Non-Patent Citations (109)
| Title |
|---|
| "Dorland's illustrated Medical Dictionary, 25th edition", 1974, W. B. SAUNDERS COMPANY |
| A.R. GENNARO: "Remingtons Pharmaceutical Sciences", 1985, MACK PUBLISHING CO. |
| AM J RESPIR CRIT CARE MED., vol. 152, no. 5, November 1995 (1995-11-01), pages S77 - 121 |
| ANDALOUSSI, GLIA, vol. 54, 2006, pages 526 |
| ARMANT ET AL., GENOME BIOL., vol. 3, no. 8, 2002, pages 3011.1 - 3011.6 |
| AUSUBEL ET AL.: "Current Protocols in Molecular Biology", 2006, JOHN WILEY & SONS |
| BADARO ET AL., J. INF. DIS., vol. 173, 1996, pages 758 - 761 |
| BADARO, R. ET AL., AM. J. TROP. MED. HYG, vol. 35, 1986 |
| BAYES ET AL., METHODS FIND EXP CLIN PHARMACO/, vol. 27, pages 193 |
| BAYES ET AL.: "Gateways to clinical trials", METHODS FIND. EXP. CLIN. PHARMACOL., vol. 27, no. 3, April 2005 (2005-04-01), pages 193 - 219 |
| BERKNER, BIOTECHNIQUES, vol. 6, 1988, pages 616 - 627 |
| BEUTLER ET AL., NATURE, vol. 320, 1986, pages 584 |
| BIOCHEM BIOPHYS ACTA, vol. 67, 1989, pages 1007 |
| BOMFORD ET AL., VACCINE, vol. 10, no. 9, 1992, pages 572 - 577 |
| BOWMAN, D.D.: "Georgis' Parasitology for Veterinarians-8th Ed.,", 2002, WB SAUNDERS |
| BRAY, R. S. ET AL., TRANS. R. SOC. TROP. MED. HYG., vol. 60, 1966, pages 605 - 609 |
| BRAZOLOT-MILLAN ET AL., PROC. NATL. ACAD. SCI., USA, vol. 95, no. 26, 1998, pages 15553 - 8 |
| CHAN; KAUFMANN: "Tuberculosis: Pathogenesis, Protection and Control", 1994, ASM PRESS |
| CHEN ET AL., J. IMMUNOL., vol. 177, 2006, pages 2373 |
| CHOUDHARY, A. ET AL., TRANS. R. SOC. TROP. MED. HYG., vol. 84, 1990, pages 363 - 366 |
| CHOUDHARY, S. ET AL., J. COMM. DIS., vol. 24, 1992, pages 32 - 36 |
| CLIN MICROBIOL REV., vol. 14, no. 2, April 2001 (2001-04-01), pages 336 - 63 |
| COLIGAN ET AL.: "Current Protocols in Immunology", 2006, JOHN WILEY & SONS |
| COOPER ET AL., AIDS, vol. 19, 2005, pages 1473 |
| COOPER ET AL.: "CPG 7909 adjuvant improves hepatitis B virus vaccine seroprotection in antiretroviral-treated HIV-infected adults.", AIDS, vol. 19, no. 14, 23 September 2005 (2005-09-23), pages 1473 - 9 |
| CORREALE ET AL., JOURNAL OF THE NATIONAL CANCER INSTITUTE, vol. 89, 1997, pages 293 |
| COTTON ET AL., PROC. NATL. ACAD. SCI. USA, vol. 89, 1992, pages 6094 |
| CURIEL ET AL., HUM. GENE THER., vol. 3, 1992, pages 147 - 154 |
| DATTA ET AL., J. IMMUNOL., vol. 170, 2003, pages 4102 |
| DAVIS ET AL., J. IMMUNOL, vol. 160, no. 2, 1998, pages 870 - 876 |
| DENG ET AL., J. IMMUNOL., vol. 173, 2004, pages 5148 |
| EDELMAN, MOL. BIOTECHNOL., vol. 21, 2002, pages 129 - 148 |
| EDELMAN, R., REV. INFECT. DIS., vol. 2, 1980, pages 370 - 383 |
| EL-ON, J. ET AL., EXPER. PARASITOL., vol. 47, 1979, pages 254 - 269 |
| FEARON ET AL., SCIENCE, vol. 272, 1996, pages 50 |
| FELGNER ET AL., PROC. NATL. ACAD. SCI. USA, vol. 84, 1989, pages 7413 - 7417 |
| FERGUSON ET AL., PROC. NATL. ACAD. SCI. USA, vol. 96, 1999, pages 3114 - 3119 |
| FEUILLET ET AL., PROC. NAT. ACAD.,SCI. USA, vol. 103, 2006, pages 12487 |
| FIEDLER, ARZNEIMITTEL-FORSCH, vol. 4, 1953, pages 213 |
| GLUCK, VACCINE, vol. 10, 1992, pages 915 - 920 |
| GORDEN ET AL., J. IMMUNOL., vol. 174, 2005, pages 1259 |
| GORSKI ET AL.: "Autoimmunity", 2001, KLUWER ACADEMIC PUBLISHERS |
| GREEN; REED, SCIENCE, vol. 281, 1998, pages 1309 |
| HILGERS ET AL., INT. ARCH. ALLERGY IMMUNOL., vol. 79, no. 4, 1986, pages 392 - 6 |
| HILGERS, IMMUNOLOGY, vol. 60, no. 1, 1987, pages 141 - 6 |
| HORSMANS ET AL., HEPATOL, vol. 42, 2005, pages 724 |
| J BIOL. CHEM, vol. 274, no. 22, 1999, pages 15633 - 15645 |
| J. KNABIEIN: "Modern Biopharmaceuticals", 6 December 2005, JOHN WILEY & SONS, pages: 183 - 200 |
| JACOBSEN ET AL., CLINICAL IMMUNOLOGY AND IMMUNOPATHOLOGY, vol. 84, 1997, pages 223 - 243 |
| JOHANSEN, CLIN. EXP. ALLERG., vol. 35, 2005, pages 1591 |
| JOHN, D.T.; PETRI, W.A.: "Markell and Voge's Medical Parasitology-9", 2006, WB SAUNDERS |
| KAISHO ET AL., MICROBES INFECT., vol. 6, 2004, pages 1388 |
| KENSIL ET AL., J. IMMUNOLOGY, vol. 146, 1991, pages 431 - 437 |
| KENSIL, CRIT REV THER DRUG CARRIER SYST, vol. 12, no. 1-2, 1996, pages 1 - 55 |
| KOLLS ET AL., PROC. NATL. ACAD. SCI. USA, vol. 91, 1994, pages 215 - 219 |
| KRIEG, NATURE, vol. 374, 1995, pages 546 |
| KRIEGLER ET AL., CELL, vol. 53, 1988, pages 45 - 53 |
| LACAILLE-DUBOIS, M; WAGNER H., PHYTOMEDICINE, vol. 2, 1996, pages 363 - 386 |
| LEE ET AL., PROC. NAT. ACAD. SCI. USA, vol. 103, 2006, pages 1828 |
| LEFKOVITS: "Immunology Methods Manual: The Comprehensive Sourcebook of Techniques", 1998 |
| LI ET AL., HUM. GENE THER., vol. 4, 1993, pages 403 - 409 |
| LIEN ET AL., NAT. IMMUNOL., vol. 4, 2003, pages 1162 |
| LIN ET AL., SHOCK, vol. 24, 2005, pages 206 |
| LIU, NATURE MEDICINE, vol. 4, no. 5, 1998, pages 515 |
| LUSTER, CURR. OPIN. IMMUNOL., vol. 14, 2002, pages 129 |
| MCCLUSKIE; DAVIS, J. IMMUNOL., vol. 161, no. 9, 1998, pages 4463 - 6 |
| MEDZHITOV ET AL., CURR. OPIN. IMMUNOL., vol. 9, 1997, pages 4 |
| MEDZHITOV, NAT. REV. IMMUNOL., vol. 1, 2001, pages 135 |
| MERCK: "Merck index, 10th Edition", article "entry no.8619" |
| MISHELL AND SHIGII: "Selected Methods in Cellular Immunology", 1979, FREEMAN PUBLISHING |
| MONTMINY S. ET AL.: "Virulence factors of Yersinia pestis are overcome by a strong lipopolysaccharide response", NATURE IMMUNOLOGY, NATURE PUBLISHING GROUP, vol. 7, no. 10, 1 October 2006 (2006-10-01), pages 1066 - 1073, XP002448153, DOI: doi:10.1038/ni1386 |
| NAKAO ET AL., J. IMMUNOL., vol. 174, 2005, pages 1566 |
| NELSON ET AL., PROC. NATL. ACAD. SCI. USA, vol. 96, 1999, pages 3114 - 3119 |
| PNAS, vol. 96, 1999 |
| POWELL; NEWMAN: "Vaccine design - The Subunit and Adjuvant Approach", 1995, PLENUM PRESS |
| PROC. NAT. ACAD. SCI. USA, vol. 95, 1998, pages 1735 - 1740 |
| RADBRUCH AND LIPSKY, P.E.: "Current Concepts in Autoimmunity and Chronic Inflammation (Curr. Top. Microbiol. and Immunol.)", 2001, SPRINGER |
| REED, S. G. ET AL., AM. J. TROP. MED. HYG., vol. 43, 1990, pages 632 - 639 |
| RIBI ET AL.: "Immunology and Immunopharmacology of Bacterial Endotoxins", 1986, PLENUM PUBL. CORP., pages: 407 - 419 |
| ROBBINS; KAWAKAMI, CURRENT OPINIONS IN IMMUNOLOGY, vol. 8, 1996, pages 628 - 636 |
| ROSE ET AL.: "Manual of Clinical Laboratory Immunology, 5th Ed.,", 1997, AMERICAN SOCIETY OF MICROBIOLOGY |
| RUBINS ET AL., MICROBIAL PATHOGENESIS, vol. 25, pages 337 - 342 |
| SALEM ET AL., VACCINE, vol. 24, 2006, pages 5119 |
| SALOMON ET AL., BIOESSAYS, vol. 199, no. 21, pages 61 - 70 |
| SCHIRMBECK ET AL., J. IMMUNOL., vol. 171, 2003, pages 5198 |
| SCHMIDT ET AL., ALLERGY, vol. 61, 2006, pages 56 |
| SCHNUR, L. F. ET AL., ISRL. J. MED. SCI., vol. 8, 1972, pages 932 - 942 |
| SENALDI ET AL., J. IMMUNOL. METHODS, vol. 193, 1996, pages 9 5 |
| SERGEIEV, V. P. ET AL., MED. PARASITOL., vol. 38, 1969, pages 208 - 212 |
| SMITH ET AL., J BIOL CHEM., vol. 262, 1987, pages 6951 |
| SOBOLL ET AL., BIOL. REPROD., vol. 75, 2006, pages 131 |
| TAKEDA ET AL., ANN REV IMMUNOL., vol. 21, 2003, pages 335 |
| TAKEDA ET AL., INT. IMMUNOL., vol. 17, 2005, pages 1 |
| TSAN ET AL., AM. J. PHYSIOL. CELL PHYSIOL., vol. 286, 2004, pages C739 |
| TSAN ET AL., J. LEUK. BIOL., vol. 76, 2004, pages 514 |
| VAN DEN EYNDE ET AL., INTERNATIONAL JOURNAL OF CLINICAL & LABORATORY RESEARCH, 1997 |
| VINCENT ET AL., NAT. GENET, vol. 5, 1993, pages 130 - 134 |
| VOLLMER ET AL., ANTIMICROB. AGENTS CHEMOTHER, vol. 48, 2004, pages 2314 |
| VOLLMER ET AL., EXPERT OPINION ON BIOLOGICAL THERAPY, vol. 5, pages 673 |
| VOLLMER J.: "Progress in drug development of immunostimulatory CpG oligodeoxynucleotide ligands for TLR9", EXPERT OPINION ON BIOLOGICAL THERAPY, vol. 5, no. 5, May 2005 (2005-05-01), pages 673 - 682, XP009155270, DOI: doi:10.1517/14712598.5.5.673 |
| WANG ET AL., PROC. NATL. ACAD. SCI. USA, vol. 84, 1987, pages 7851 |
| WASLYLYK ET AL., EUR. J BIOCH., vol. 211, no. 7, 1993, pages 18 |
| WEERATNA ET AL., VACCINE, vol. 23, 2005, pages 5263 |
| WEIHRAUCH ET AL., CLIN CANCER RES., vol. 11, no. 16, 2005, pages 5993 - 6001 |
| WEIR: "Handbook of Experimental Immunology", 1986, BLACKWELL SCIENTIFIC |
| WU ET AL., J. BIOL. CHEM., vol. 264, 1989, pages 16985 - 16987 |
| YOSHIKAWA M ET AL., CHEM PHARM BULL (TOKYO, vol. 44, no. 8, August 1996 (1996-08-01), pages 1454 - 1464 |
| YOSHIYUKI F. ET AL.: "Synthesis of Rubrivivax gelatinosus Lipid A and Analogues for Investigation of the Structural Basis for Immunostimulating and Inhibitory Activities", BULLETIN OF THE CHEMICAL SOCIETY OF JAPAN, vol. 81, no. 7, pages 796 - 819, XP055042391, DOI: doi:10.1246/bcsj.81.796 |
| ZIJLSTRA ET AL., TRANS. R. SOC. TROP. MED. HYG., vol. 91, 1997, pages 671 - 673 |
Cited By (52)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US8840908B2 (en) | 2006-09-26 | 2014-09-23 | Infectious Disease Research Institute | Vaccine composition containing synthetic adjuvant |
| US9907845B2 (en) | 2006-09-26 | 2018-03-06 | Infectious Disease Research Institute | Methods of using a vaccine composition containing synthetic adjuvant |
| US10765736B2 (en) | 2006-09-26 | 2020-09-08 | Infectious Disease Research Institute | Vaccine composition containing synthetic adjuvant |
| US9987355B2 (en) | 2006-09-26 | 2018-06-05 | Infectious Disease Research Institute | Vaccine composition containing synthetic adjuvant |
| US9950063B2 (en) | 2006-09-26 | 2018-04-24 | Infectious Disease Research Institute | Vaccine composition containing synthetic adjuvant |
| US8609114B2 (en) | 2006-09-26 | 2013-12-17 | Infectious Diesease Research Institute | Methods of using a vaccine composition containing synthetic adjuvant |
| US8343512B2 (en) | 2006-09-26 | 2013-01-01 | Infectious Disease Research Institute | Treatment of allergic conditions using a composition containing synthetic adjuvant |
| US10792359B2 (en) | 2006-09-26 | 2020-10-06 | Infectious Disease Research Institute | Methods of using a vaccine composition containing synthetic adjuvant |
| US9480740B2 (en) | 2009-06-05 | 2016-11-01 | Infectious Disease Research Institute | Synthetic glucopyranosyl lipid adjuvants |
| US9814772B2 (en) | 2009-06-05 | 2017-11-14 | Infectious Disease Research Institute | Synthetic glucopyranosyl lipid adjuvants |
| US10632191B2 (en) | 2009-06-05 | 2020-04-28 | Infectious Disease Research Institute | Synthetic glucopyranosyl lipid adjuvants |
| WO2012112691A1 (en) | 2011-02-15 | 2012-08-23 | Immune Design Corp. | Methods for enhancing immunogen specific immune responses by vectored vaccines |
| EP2694099B1 (en) * | 2011-04-08 | 2019-10-16 | Immune Design Corp. | Immunogenic compositions and methods of using the compositions for inducing humoral and cellular immune responses |
| EP3563834A1 (en) * | 2012-02-07 | 2019-11-06 | Infectious Disease Research Institute | Improved adjuvant formulations comprising tlr4 agonists and methods of using the same |
| JP2015028092A (en) * | 2012-04-04 | 2015-02-12 | 日東電工株式会社 | Vaccine composition |
| JP2013231026A (en) * | 2012-04-04 | 2013-11-14 | Nitto Denko Corp | Vaccine composition |
| EP3031468A1 (en) * | 2012-04-04 | 2016-06-15 | Nitto Denko Corporation | Vaccine composition |
| EP2647387A1 (en) * | 2012-04-04 | 2013-10-09 | Nitto Denko Corporation | Vaccine Composition |
| EP3485904A1 (en) * | 2012-04-04 | 2019-05-22 | Nitto Denko Corporation | Vaccine composition |
| US9498527B2 (en) | 2012-04-04 | 2016-11-22 | Nitto Denko Corporation | Vaccine composition |
| KR20130112790A (en) * | 2012-04-04 | 2013-10-14 | 닛토덴코 가부시키가이샤 | Vaccine composition |
| KR102103606B1 (en) | 2012-04-04 | 2020-04-22 | 닛토덴코 가부시키가이샤 | Vaccine composition |
| US9895435B2 (en) | 2012-05-16 | 2018-02-20 | Immune Design Corp. | Vaccines for HSV-2 |
| US8957047B2 (en) | 2013-04-18 | 2015-02-17 | Immune Design Corp. | GLA monotherapy for use in cancer treatment |
| US8962593B2 (en) | 2013-04-18 | 2015-02-24 | Immune Design Corp. | GLA monotherapy for use in cancer treatment |
| US10993956B2 (en) | 2013-04-18 | 2021-05-04 | Immune Design Corp. | GLA monotherapy for use in cancer treatment |
| US10342815B2 (en) | 2013-04-18 | 2019-07-09 | Immune Design Corp. | GLA monotherapy for use in cancer treatment |
| EP3650028A1 (en) | 2013-06-04 | 2020-05-13 | Infectious Disease Research Institute | Compositions and methods for reducing or preventing metastasis |
| US9463198B2 (en) | 2013-06-04 | 2016-10-11 | Infectious Disease Research Institute | Compositions and methods for reducing or preventing metastasis |
| US9149521B2 (en) | 2013-09-25 | 2015-10-06 | Sequoia Sciences, Inc. | Compositions of vaccines and adjuvants and methods for the treatment of urinary tract infections |
| US9017698B2 (en) | 2013-09-25 | 2015-04-28 | Sequoia Sciences, Inc. | Compositions of vaccines and adjuvants and methods for the treatment of urinary tract infections |
| US9878037B2 (en) | 2013-09-25 | 2018-01-30 | Sequoia Sciences, Inc. | Compositions of vaccines and adjuvants and methods for the treatment of urinary tract infections |
| US9149522B2 (en) | 2013-09-25 | 2015-10-06 | Sequoia Sciences, Inc. | Compositions of vaccines and adjuvants and methods for the treatment of urinary tract infections |
| US20160030459A1 (en) * | 2014-01-21 | 2016-02-04 | Immune Design Corp. | Compositions and methods for treating allergic conditions |
| WO2015112485A1 (en) * | 2014-01-21 | 2015-07-30 | Immune Design Corp. | Compositions for use in the treatment of allergic conditions |
| WO2015123496A1 (en) | 2014-02-14 | 2015-08-20 | Immune Design Corp. | Immunotherapy of cancer through combination of local and systemic immune stimulation |
| EP3542816A1 (en) | 2014-02-14 | 2019-09-25 | Immune Design Corp. | Immunotherapy of cancer through combination of local and systemic immune stimulation |
| US10940198B2 (en) | 2016-12-26 | 2021-03-09 | Mogam Institute For Biomedical Research | Herpes zoster vaccine composition |
| US11207403B2 (en) | 2017-09-13 | 2021-12-28 | Sanofi Pasteur | Human cytomegalovirus immunogenic composition |
| US11524069B2 (en) | 2017-09-13 | 2022-12-13 | Sanofi Pasteur | Human cytomegalovirus immunogenic composition |
| US11679163B2 (en) | 2019-09-20 | 2023-06-20 | Hdt Bio Corp. | Compositions and methods for delivery of RNA |
| WO2021067785A1 (en) | 2019-10-02 | 2021-04-08 | Janssen Vaccines & Prevention B.V | Staphylococcus peptides and methods of use |
| WO2021097347A1 (en) | 2019-11-15 | 2021-05-20 | Infectious Disease Research Institute | Rig-i agonist and adjuvant formulation for tumor treatment |
| US11559584B2 (en) | 2020-03-23 | 2023-01-24 | Hdt Bio Corp. | Compositions and methods for delivery of RNA |
| US11534497B2 (en) | 2020-03-23 | 2022-12-27 | Hdt Bio Corp. | Compositions and methods for delivery of RNA |
| US11458209B2 (en) | 2020-03-23 | 2022-10-04 | Hdt Bio Corp. | Compositions and methods for delivery of nucleic acid-lipid nanoparticle complexes encoding for viral RNA polymerase region and protein antigen |
| US11648321B2 (en) | 2020-03-23 | 2023-05-16 | Hdt Bio Corp. | Compositions and methods for delivery of RNA |
| US11648322B2 (en) | 2020-03-23 | 2023-05-16 | Hdt Bio Corp. | Compositions and methods for delivery of RNA |
| US11654200B2 (en) | 2020-03-23 | 2023-05-23 | Hdt Bio Corp. | Compositions and methods for delivery of RNA |
| US11752218B2 (en) | 2020-03-23 | 2023-09-12 | Hdt Bio Corp. | Nucleic acid-small diameter and liquid core nanoparticle complexed compositions |
| US11896677B2 (en) | 2020-03-23 | 2024-02-13 | Hdt Bio Corp. | Compositions and methods for delivery of RNA |
| WO2022136952A1 (en) | 2020-12-23 | 2022-06-30 | Infectious Disease Research Institute | Solanesol vaccine adjuvants and methods of preparing same |
Also Published As
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| US10632191B2 (en) | Synthetic glucopyranosyl lipid adjuvants | |
| US9907845B2 (en) | Methods of using a vaccine composition containing synthetic adjuvant |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| WWE | Wipo information: entry into national phase |
Ref document number: 201080034214.0 Country of ref document: CN |
|
| 121 | Ep: the epo has been informed by wipo that ep was designated in this application |
Ref document number: 10784178 Country of ref document: EP Kind code of ref document: A1 |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 2764374 Country of ref document: CA Ref document number: MX/A/2011/012836 Country of ref document: MX |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 2010256461 Country of ref document: AU Ref document number: 2012514187 Country of ref document: JP |
|
| NENP | Non-entry into the national phase |
Ref country code: DE |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 10056/DELNP/2011 Country of ref document: IN |
|
| REEP | Request for entry into the european phase |
Ref document number: 2010784178 Country of ref document: EP |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 2010784178 Country of ref document: EP |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 2011152602 Country of ref document: RU |
|
| ENP | Entry into the national phase |
Ref document number: 2010256461 Country of ref document: AU Date of ref document: 20100604 Kind code of ref document: A |
|
| REG | Reference to national code |
Ref country code: BR Ref legal event code: B01A Ref document number: PI1011072 Country of ref document: BR |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 242992 Country of ref document: IL |
|
| ENP | Entry into the national phase |
Ref document number: PI1011072 Country of ref document: BR Kind code of ref document: A2 Effective date: 20111202 |