JP4336386B2 - Surgical stapling and cutting device and method of using the device - Google Patents
Surgical stapling and cutting device and method of using the device Download PDFInfo
- Publication number
- JP4336386B2 JP4336386B2 JP2008524042A JP2008524042A JP4336386B2 JP 4336386 B2 JP4336386 B2 JP 4336386B2 JP 2008524042 A JP2008524042 A JP 2008524042A JP 2008524042 A JP2008524042 A JP 2008524042A JP 4336386 B2 JP4336386 B2 JP 4336386B2
- Authority
- JP
- Japan
- Prior art keywords
- actuator
- stapling
- joint
- end effector
- articulated
- Prior art date
- Legal status (The legal status is an assumption and is not a legal conclusion. Google has not performed a legal analysis and makes no representation as to the accuracy of the status listed.)
- Active
Links
Images
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/068—Surgical staplers, e.g. containing multiple staples or clamps
- A61B17/072—Surgical staplers, e.g. containing multiple staples or clamps for applying a row of staples in a single action, e.g. the staples being applied simultaneously
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/28—Surgical forceps
- A61B17/29—Forceps for use in minimally invasive surgery
- A61B2017/2926—Details of heads or jaws
- A61B2017/2927—Details of heads or jaws the angular position of the head being adjustable with respect to the shaft
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B90/00—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges
- A61B90/50—Supports for surgical instruments, e.g. articulated arms
- A61B2090/508—Supports for surgical instruments, e.g. articulated arms with releasable brake mechanisms
Description
本発明は、医療用デバイスの分野に関し、特に、組織にステープルのラインを当てながら、これらのステープルラインの間の組織を切断することができる外科用ステープラ器具の分野に関し、更に、ステープラ器具の改良及び、連接型シャフトを含むこれらのステープラ器具の様々な構成部品を形成するプロセスの改良に関する。このデバイスは、特に、内視鏡または腹腔鏡外科手順を行う間に組織のステープリングおよび切断を行うのに用いることができる。 The present invention relates to the field of medical devices, and more particularly to the field of surgical stapler instruments that can cut tissue between staple lines while applying the staple lines to the tissue, and further improvements to the stapler instrument. And an improvement in the process of forming the various components of these stapler instruments, including articulated shafts. This device can be used, inter alia, for stapling and cutting tissue during endoscopic or laparoscopic surgical procedures.
内視鏡外科器具は、しばしば伝統的な開外科デバイスより好まれる。なぜなら、より小さい切開が、術後の回復時間と合併症を低減する傾向にあるためである。この結果、外套針のカニューラを通して所望の外科部位に遠位側端部作動体を正確に配置するのに好適な内視鏡外科器具の作動範囲に有意な開発がなされた。これらの遠位側端部作動体は、様々な方法で組織に係合して診断または治療効果をあげている(例えば、エンドカッタ、把持器、カッタ、ステープラ、クリップアプライヤ、アクセスデバイス、薬剤/遺伝子セラピィ送出デバイス、超音波、RF、レーザなどを用いたエネルギィデバイス、他)。 Endoscopic surgical instruments are often preferred over traditional open surgical devices. This is because smaller incisions tend to reduce post-operative recovery time and complications. As a result, significant developments have been made in the operating range of endoscopic surgical instruments suitable for accurately positioning the distal end effector at the desired surgical site through the cannula of the trocar. These distal end effectors engage the tissue in a variety of ways to provide diagnostic or therapeutic effects (eg, end cutters, graspers, cutters, staplers, clip appliers, access devices, drugs / Gene therapy device, energy device using ultrasound, RF, laser, etc.).
端部作動体の位置決めは、外套針によって強制される。一般的に、これらの内視鏡外科器具は、端部作動体と外科医が操作するハンドル部分との間に長いシャフトがある。この長いシャフトが、所望の深さへの挿入と、このシャフトの長軸を中心とする回転を可能にし、これによって、端部作動体を幾分位置決めすることができる。外套針を賢明に配置し、例えば、別の外套針を介して把持器を使用することで、多くの場合この位置決め量で十分である。例えば、Knodel et al.に付与された米国特許第5、465、895号などの外科用ステープリング及び切断器具は、挿入と回転によって端部作動体をうまく位置決めする内視鏡外科器具の一例である。 The positioning of the end effector is forced by the trocar. Generally, these endoscopic surgical instruments have a long shaft between the end effector and the handle portion that the surgeon manipulates. This long shaft allows insertion to the desired depth and rotation around the long axis of the shaft, thereby allowing some positioning of the end effector. This positioning is often sufficient by judicious placement of the trocar, for example by using a gripper via another trocar. For example, Knodel et al. Surgical stapling and cutting instruments such as U.S. Pat. No. 5,465,895, which is incorporated herein by reference, are examples of endoscopic surgical instruments that successfully position an end effector by insertion and rotation.
United States Surgical Corporation社によって製造され、Green et al.に付与された米国特許第6,644,532号及び第6,250,532号に記載されているステープラは、同じステップで単一の面に沿って相応して移動するレバーの作動に応じて、単一の面に沿ってステップで回動する端部作動体を具える。図31および図32を参照されたい。しかしながら、United States Surgical Corporation社のステープラは、達成できる所定の角度と、左右の回動の制限(−45°から+45°)によって制限を受け、操作に二本の手を必要とする。 Manufactured by United States Surgical Corporation, Green et al. The staplers described in U.S. Pat. Nos. 6,644,532 and 6,250,532 are responsive to actuation of a lever that moves correspondingly along a single surface in the same step. And an end effector that pivots in steps along a single plane. See FIGS. 31 and 32. However, the United States Surgical Corporation stapler is limited by the predetermined angle that can be achieved and the left and right rotation limits (-45 ° to + 45 °) and requires two hands to operate.
挿入と回転に制限されるのではなく、操作の特性に依存して、内視鏡外科器具の端部作動体の位置決めを更に調整することが望まれる。特に、端部作動体をこの器具のシャフトの長軸を横切る軸に向けることがしばしば望まれている。この器具のシャフトに対する端部作動体の横径移動は、従来より、「連接」と呼ばれている。この連接型位置決めによれば、外科医は、いくつかの場合、より容易に組織に係合させることができる。また、有利なことに、連接型位置決めによれば、器具のシャフトによってブロックされることなく、端部作動体の背後に内視鏡を配置することができる。 Rather than being limited to insertion and rotation, it is desirable to further adjust the positioning of the end effector of the endoscopic surgical instrument depending on the operating characteristics. In particular, it is often desirable to point the end effector to an axis that traverses the long axis of the instrument shaft. This lateral movement of the end effector relative to the instrument shaft is conventionally referred to as "joint". This articulated positioning allows the surgeon to more easily engage tissue in some cases. Also advantageously, articulated positioning allows the endoscope to be placed behind the end effector without being blocked by the instrument shaft.
上述した非連接型ステープリングおよび切断器具は、実用性が高く多くの外科的手順にうまく利用することができるが、端部作動体を連接する能力をもってこの動作を強化して、これによって使用に際して外科医により優れたフレキシビリティを与えることが望まれる。連接型外科器具は、一般的に、器具シャフト内で、連接ジョイントを通って縦方向に移動して、カートリッジからステープルを発射して、最も内側のステープルライン間の組織を切断する一又それ以上の発射バーを使用している。これらの外科器具の一つの共通の問題は、連接ジョイントを通る発射バーの制御である。端部作動体は、シャフトと端部作動体のエッジが連接中にぶつからないように、連接ジョイントにおいてシャフトから縦方向にスペースを空けて配置されている。このギャップは、支持材料で満たされているか、あるいは、単一または複数の発射バーに縦方向の発射負荷がかかっているときに、発射バーのジョイントの留め金が外れてしまわないような構造でなくてはならない。必要なものは、連接ジョイントを通して単一又は複数の発射バーを案内して支持する潮路構造、あるいは端部作動体が連接される時に曲がるあるいは湾曲する支持構造である。 The non-joint stapling and cutting instrument described above is highly practical and can be successfully used in many surgical procedures, but enhances this action with the ability to articulate the end effector, and thereby in use. It would be desirable to give surgeons greater flexibility. Articulated surgical instruments typically move one or more longitudinally through the articulating joint within the instrument shaft to fire staples from the cartridge and cut tissue between the innermost staple lines. Use the launch bar. One common problem with these surgical instruments is the control of the firing bar through the articulating joint. The end actuating body is arranged with a space in the vertical direction from the shaft in the articulation joint so that the shaft and the edge of the end actuating body do not collide during the articulation. This gap is either filled with support material or structured so that the launch bar joints do not come off when a single or multiple launch bars are subjected to a longitudinal firing load. Must-have. What is needed is a tidal structure that guides and supports one or more firing bars through articulating joints, or a supporting structure that bends or curves when the end effector is articulated.
Schulze et al.に付与された米国特許第5,673,840号は、エラストマ材料またはプラスチック材料で形成され、フレキシブル連接ジョイントを開示している。これはフレキシブルジョイントまたは「フレックスネック」で曲がる。発射バーは、フレックスネック内の中空チューブを通って支持され案内される。フレックスネックは、こう合閉鎖機構の一部であり、組織上でこう合部が閉じるときに、端部作動体、シャフト、発射バーに対して縦方向に移動する。次いで、ステープルが発射され組織が切断されるときに、発射バーがフレックスネック内を縦方向に移動する。 Schulze et al. U.S. Pat. No. 5,673,840 issued to U.S. Pat. No. 6,057,028 is made of an elastomeric material or a plastic material and discloses a flexible articulated joint. This bends at the flexible joint or “flex neck”. The firing bar is supported and guided through a hollow tube in the flex neck. The flex neck is part of the occlusion closure mechanism and moves longitudinally relative to the end effector, shaft and firing bar when the occlusion closes on the tissue. The firing bar then moves longitudinally within the flex neck as the staples are fired and the tissue is cut.
Oberlin et al.に付与された米国特許第5,797,537号(Richard−Allan Medical Industries、Inc.が所有)は、フレックスジョイントを中心に曲がるのではなく、ピンの回りを回動する連接ジョイントを開示している。この器具では、発射バーは、一対のスペースを空けて配置された支持プレートの間に支持されている。このプレートは、一端部がシャフトに、他端部が端部作動体に連結されている。これらの連結の少なくとも一方が、摺動可能な連結である。支持プレートは、連接面においてフレキシブルな駆動部材近傍の連接ジョイントを通って延在しており、支持プレートは、先端がこの連接面内のギャップを通って曲がり、フレキシブル発射バーは、先端がその整合位置から一方向に連接される時に、支持プレートに対して曲がる。U.S.Surgicalからの Milliman et al.に付与された米国特許第6,330,965号は、シャフトに固定的に取り付けられ、端部作動体に摺動可能に取り付けられた支持プレートの使用を教示している。 Oberlin et al. U.S. Pat. No. 5,797,537 (owned by Richard-Allan Medical Industries, Inc.) discloses an articulating joint that pivots around a pin rather than bending around a flex joint. Yes. In this instrument, the firing bar is supported between support plates arranged in a pair of spaces. This plate has one end connected to the shaft and the other end connected to the end working body. At least one of these connections is a slidable connection. The support plate extends through the articulation joint near the flexible drive member at the articulation surface, the support plate bends through the gap in the articulation surface, and the flexible launch bar aligns the tip thereof When connected in one direction from position, it bends against the support plate. U. S. Milliman et al. From Surgical. U.S. Pat. No. 6,330,965 teaches the use of a support plate fixedly attached to the shaft and slidably attached to the end effector.
これらの公知の支持プレートは、連接ジョイントを通って発射バーを案内しているが、性能を強化しうると考えられる。例えば、多くの場合、発射バーが発射の間に急速に加速して、組織を効果的に切断するのに十分な運動量を確保することが望まれる。強固に取り付けられた支持プレートは、応答において無理に移動する傾向にあり、発射バーを連接ジョイントから飛び出させる。更なる例としては、連接しているかどうかにかかわらず、器具が同じ態様で動作することが望ましい。連接時の摩擦が大きくなることは好ましくなく、発射力の変化量を用いる必要がある場合、外科医を混乱させる。 These known support plates guide the firing bar through articulated joints, but it is believed that performance can be enhanced. For example, in many cases it is desirable for the firing bar to accelerate rapidly during firing to ensure sufficient momentum to effectively cut tissue. The firmly attached support plate tends to move in response and causes the firing bar to jump out of the articulating joint. As a further example, it is desirable for the instrument to operate in the same manner regardless of whether it is articulated. Increased friction during articulation is undesirable and confuses the surgeon if it is necessary to use a variation in firing force.
この結果、連接ジョイントを介して発射バーへの支持を強化する外科器具機構用の改良した連接機構が有意に求められている。 As a result, there is a significant need for an improved articulation mechanism for a surgical instrument mechanism that enhances support to the firing bar via the articulation joint.
従って、本発明の目的は、一般的なタイプの公知のデバイスと方法の上述した欠点を克服し、連接型外科用端部作動体を提供する外科用ステープリング及び切断デバイス及びこのデバイスを使用する方法を提供することである。 Accordingly, it is an object of the present invention to overcome the above-mentioned drawbacks of common types of known devices and methods and to use a surgical stapling and cutting device and articulated device that provide an articulated surgical end effector. Is to provide a method.
上述の目的及びその他の目的を鑑みると、本発明によれば、端部作動体を制御ハンドルに連結する受動的連接ジョイントを具える、医療用デバイス端部作動体連結アッセンブリが提供されている。 In view of the above and other objects, in accordance with the present invention, a medical device end effector coupling assembly is provided that includes a passive articulation joint that couples the end effector to a control handle.
本発明の目的を鑑みると、制御ハンドルに連結された端部作動体を有する医療デバイスにおいて、当該端部作動体を制御ハンドルに連結する受動的連接ジョイントを具える作動体連結アッセンブリが提供されている。 In view of the objectives of the present invention, in a medical device having an end effector coupled to a control handle, an actuating body coupling assembly is provided that includes a passive articulating joint for coupling the end effector to the control handle. Yes.
本発明の目的を鑑みると、また、制御ハンドルと、受動的連接接続を介してこの制御ハンドルに連結した外科用端部作動体を具える、医療デバイスが提供されている。 In view of the objects of the present invention, there is also provided a medical device comprising a control handle and a surgical end effector coupled to the control handle via a passive articulation connection.
本発明の目的を鑑みると、また、制御ハンドルと、この制御ハンドルに対して受動的に連接された外科用端部作動体を具える医療用デバイスが提供されている。 In view of the object of the present invention, there is also provided a medical device comprising a control handle and a surgical end effector passively connected to the control handle.
本発明の目的を鑑みると、また、受動的連接ジョイントの第1の部分を有する制御ハンドルと、受動的連接ジョイントの第2の部分を有する外科用端部作動体を具え、この受動的連接ジョイントの第1及び第2の部分が端部作動体を制御ハンドルに連結している医療用デバイスが提供されている。 In view of the objects of the present invention, there is also provided a control handle having a first portion of a passive articulating joint and a surgical end effector having a second portion of the passive articulating joint, the passive articulating joint. A medical device is provided in which the first and second portions connect the end effector to the control handle.
本発明の目的を鑑みると、また、制御ハンドルと、端部作動体を制御ハンドルに連結する受動的連接ジョイントを有する外科用端部作動体を具える医療用デバイスが提供されている。 In view of the objects of the present invention, there is also provided a medical device comprising a surgical end effector having a control handle and a passive articulating joint coupling the end effector to the control handle.
本発明の目的を鑑みると、また、制御ハンドルと、外科用端部作動体と、この端部作動体を制御ハンドルに連結する受動的連接ジョイントを具える医療用デバイスが提供されている。 In view of the objectives of the present invention, there is also provided a medical device comprising a control handle, a surgical end effector, and a passive articulating joint connecting the end effector to the control handle.
本発明の目的を鑑みると、また、非作動状態および作動状態にある連接ジョイントアクチュエータを有する制御ハンドルと、外科用端部作動体と、この外科用端部作動体を制御ハンドルに連結する受動的連接ジョイントを具える医療用デバイスが提供されている。この連接ジョイントアクチュエータは、非作動状態にあるとき、受動的連接ジョイントを保持し、これによって端部作動体を実質的に固定された連接位置とし、作動状態にあるときに、受動的連接ジョイントを連接自在な状態に解放し、端部作動体に作用する外力に応じて、制御ハンドルに対して端部作動体を自在に連接させる。 In view of the objects of the present invention, there is also a control handle having articulated joint actuators in a non-actuated state and an actuated state, a surgical end effector, and a passive coupling the surgical end effector to the control handle. Medical devices having articulated joints are provided. The articulated joint actuator holds the passive articulated joint when inactive, thereby placing the end effector in a substantially fixed articulated position, and when in the active state, the articulated joint actuator The end actuating body is released in a freely connectable state, and the end actuating body is freely connected to the control handle in accordance with an external force acting on the end actuating body.
本発明の目的を鑑みると、また、ステープル付ステープリングデバイスと、刃付切断デバイスの少なくとも一つを有する外科用ステープリング端部作動体と、作動時にステープリングデバイスを閉じるステープラ閉鎖アクチュエータを有する制御ハンドルと、作動時にステープルの止め付けと、切断デバイスでの組織の切断の少なくとも一方を行うステープル発射アクチュエータと、非作動状態と作動状態とを有する連接型ジョイントアクチュエータと、端部作動体を制御ハンドルに連結する受動的連接型ジョイントとを具える医療用デバイスが提供されているこの端部作動体は、連接型ジョイントが作動して、連接型ジョイントアクチュエータが作動していないときに所定の連接位置に係止したときに、端部作動体にかかる力に応じて、自在に連接する。 In view of the objectives of the present invention, there is also a control having a stapled stapling device, a surgical stapling end actuator having at least one of a bladed cutting device, and a stapler closure actuator that closes the stapling device when actuated. A handle, a staple firing actuator that performs at least one of fastening a staple upon actuation and cutting of tissue with a cutting device, an articulated joint actuator having a non-actuated state and an actuated state, and a handle for controlling the end effector The end effector is provided with a passive articulating joint coupled to the end actuating body when the articulating joint is activated and the articulating joint actuator is not actuated. Depending on the force applied to the end effector. It is connected to.
本発明の一の態様によれば、外科用器具は、係止を解放して、端部作動体の連接と連接されている間の発射を可能とするハンドル部分を有している。この解放および発射機構は、シャフトを介して連接機構へ伝達される。連接機構は、ユーザが端部作動体に与える力に対応しており、シャフトの縦軸のラインの外への端部作動体の連接を可能にする。発射機構は、発射動作に対応しており、連接機構と端部作動体を介して移動させるために連結されている。発射支持デバイスによって、連接が生じると、発射機構が発射機構を支持して適所に保持することができる。 In accordance with one aspect of the present invention, the surgical instrument has a handle portion that releases the lock and allows firing while connected to the end effector connection. This release and firing mechanism is transmitted to the articulation mechanism via the shaft. The articulation mechanism corresponds to the force applied by the user to the end effector and allows the end effector to be articulated out of the longitudinal axis line of the shaft. The launch mechanism corresponds to the launch operation and is coupled to move through the articulation mechanism and the end effector. The firing support device allows the firing mechanism to support and hold the firing mechanism in place when articulation occurs.
本発明の別の特徴によれば、制御ハンドルは、非作動状態と作動状態を有する連接ジョイントアクチュエータを具え、端部作動体は、係止連接状態と、非係止連接状態を有する連接ロックを有し、連接ジョイントアクチュエータは、非作動状態から作動状態に変わったときに、連接ロックを係止連接状態から非係止連接状態に変更し、作動状態から非作動状態に変わったときに、連接ロックを非係止連接状態から係止連接状態に変更する。 According to another feature of the invention, the control handle comprises an articulated joint actuator having a non-actuated state and an actuated state, and the end effector has a locked articulated state and an articulated lock having an unlocked articulated state. The articulated joint actuator changes the articulation lock from the locked articulated state to the non-engaged articulated state when the non-actuated state changes to the actuated state, and The lock is changed from the non-locking connection state to the locking connection state.
本発明の更なる特徴によれば、ステープラ閉鎖アクチュエータとステープル発射アクチュエータが、連接ジョイントアクチュエータと異なる。 According to a further feature of the present invention, the stapler closure actuator and the staple firing actuator are different from the articulated joint actuator.
本発明の追加の特徴によれば、受動的連接ジョイントを介して制御ハンドルをステープル発射アクチュエータに連結する少なくとも一の第1のフレキシブルビームと、受動連接ジョイントを介して端部作動体を制御ハンドルに縦方向に連結する少なくとも第2のフレキシブルビームが提供されている。この第1及び第2のフレキシブルビームは、受動的連接ジョイントの連接に対応して撓む。 According to an additional feature of the invention, at least one first flexible beam coupling the control handle to the staple firing actuator via a passive articulation joint, and the end effector to the control handle via a passive articulation joint. At least a second flexible beam is provided for longitudinal connection. The first and second flexible beams bend corresponding to the articulation of the passive articulation joint.
本発明の更なる特徴によれば、制御ハンドルが第1の縦軸を有し、端部作動体が第2の縦軸を有し、制御ハンドルと、端部作動体、および受動連悦ジョイントの少なくとも一つが、整列デバイスを有する。例示的な実施例では、整列デバイスは、端部作動体にバイアスをかけて、連接ジョイントアクチュエータが作動したときに、第1及び第2の縦軸を実質的に整列させる。整列デバイスは、中央にバイアスするデバイスであっても良い。このような実施例では、中央バイアスデバイスは、第1の縦軸の対向する側に配置したばね式プランジャセットであり、これは、端部作動体を個別に押圧して、第1の縦軸に第2の縦軸を整列させている。 According to a further feature of the present invention, the control handle has a first longitudinal axis, the end effector has a second longitudinal axis, the control handle, the end effector, and the passive linkage joint. At least one of which has an alignment device. In an exemplary embodiment, the alignment device biases the end effector to substantially align the first and second longitudinal axes when the articulating joint actuator is actuated. The alignment device may be a centrally biased device. In such an embodiment, the central biasing device is a spring-loaded plunger set disposed on opposite sides of the first longitudinal axis, which individually presses the end effectors to provide the first longitudinal axis. The second vertical axis is aligned.
本発明のもう一つの利点は、移動可能な遠位側端部作動体が中央にバイアスされていることである。これは、まず遠位端が、安定位置から自由であり、次いで、周辺組織などの環境構造に対して端部作動体押圧することで新たな位置に受動的に動くことを意味する。端部作動体を安定位置から自由にするアクチュエータが解放されたときに、中央バイアスデバイス、好ましくは少なくとも一のバイアスばね、特に、対向しており、従って、中央方向にバイアス力をかける2本のバイアスばねを押圧した状態で、遠位側端部作動体が、中央位置に戻る。代替的に、中央バイアスデバイスが、クレビスにおいて端部作動体のどちらかの側部に配置したばね式プランジャセットであり、中央位置に向けて個別に端部作動体を押圧するものであってもよい。 Another advantage of the present invention is that the movable distal end effector is centrally biased. This means that the distal end is first free from a stable position and then passively moves to a new position by pressing the end effector against an environmental structure such as surrounding tissue. When the actuator that releases the end effector from the stable position is released, the central biasing device, preferably at least one biasing spring, in particular, is opposed and thus has two biasing forces in the central direction. With the bias spring pressed, the distal end effector returns to the central position. Alternatively, the central biasing device may be a spring-loaded plunger set located on either side of the end effector in the clevis and individually pressing the end effector toward the center position Good.
本発明の更なる特徴によれば、連接型ジョイントアクチュエータは、遠位側を向いた歯を有するプルロックを有しており、受動的連接ジョイントは、連接ジョイントアクチュエータが非作動状態にあるときにこの遠位側を向いた歯に相互係合する近位側を向いた歯を有するギアを有する。また、この連接型ジョイントアクチュエータは、連接型ジョイントアクチュエータが非作動状態にあるときに、近位側を向いた歯から遠位側を向いた歯の係合を解除して、端部作動体の連接ロックを解除する。 According to a further feature of the present invention, the articulating joint actuator has a pull lock with teeth facing distally, and the passive articulating joint is in this state when the articulating joint actuator is in an inoperative state. A gear having teeth facing proximally that interengage with teeth facing distally. Further, the articulated joint actuator disengages the teeth facing the distal side from the teeth facing the proximal side when the articulated joint actuator is in the non-actuated state. Release the articulation lock.
本発明の更なる特徴によれば、遠位側への移動の作動は、プルツーリリース(pull−to−release)、およびリリースツーリロック(release−relock)のトリガによって生じる。受動的な動きを制御するこのトリガは、通常は、係止されている。この係止は、トリガにおいて引っ張られることによって解放される。遠位側端部作動体が所望の位置にくると、ユーザがこのトリガを解除して、遠位側端部作動体を新しい位置に係止させる。 According to a further feature of the present invention, the actuation of the distal movement is caused by pull-to-release and release-relock triggers. This trigger that controls passive movement is normally locked. This lock is released by being pulled on the trigger. When the distal end effector is in the desired position, the user releases the trigger to lock the distal end effector in the new position.
本発明によるデバイスは、外科用ステープラおよびカッタ、あるいは特に、組織の部分を互いにステープルし、所望の時に組織を切断するのに使用することができるその他の内視鏡デバイスである。端部作動体の一の実施例では、ステープリング機能と切断機能の両方を実行する手段が、デバイスの遠位側端部作動体内に全体的に保持されている。 The device according to the invention is a surgical stapler and cutter, or in particular other endoscopic devices that can be used to staple portions of tissue together and cut tissue when desired. In one embodiment of the end effector, means for performing both stapling and cutting functions are generally retained within the distal end effector of the device.
再び、本発明のもう一つの利点は、ハンドルが、電子的に制御され、ユニバーサルであり、電動式であることである。ハンドルは、多数の製品構成用にプログラムされたマイクロプロセッサを具える。例えば、ステープラの場合、ハンドルは30mm、45mm、あるいは60mmのステープルカートリッジ用にプログラムされている。ステープラの遠位シャフトは、ユニバーサルハンドルに差し込む近位端を有する。この遠位シャフトは、電気的コンタクトアレイを具え、これが、接続位置においてハンドル側の合致するアレイと対応して接触する。この接触は、様々な遠位シャフトの各々でユニークなものであり、ハンドルがシャフトを「認識」して、そのシャフト用の適宜のプログラムを稼働する。ハンドルは、安全なロックアウト、ステープラ送出速度、ストロークの距離、その他のロジックを含むようにプログラムされている。このような、モジュール性によって、複数の端部作動体を有する一つのハンドルをシャフトに合致するように製造することができる。 Again, another advantage of the present invention is that the handle is electronically controlled, universal and motorized. The handle includes a microprocessor programmed for multiple product configurations. For example, in the case of a stapler, the handle is programmed for a 30 mm, 45 mm, or 60 mm staple cartridge. The distal shaft of the stapler has a proximal end that plugs into the universal handle. The distal shaft comprises an electrical contact array, which contacts correspondingly with the matching array on the handle side in the connected position. This contact is unique for each of the various distal shafts, and the handle “recognizes” the shaft and runs the appropriate program for that shaft. The handle is programmed to include safe lockout, stapler delivery speed, stroke distance, and other logic. With such modularity, a single handle having a plurality of end effectors can be manufactured to match the shaft.
デバイスの作動は、電気モータを用いて行われる。デバイスは、又、複数の電気モータによって、油圧モータまたは空気圧モータによって、あるいは、作動アッセンブリをデバイスの遠位部分に一義的にあるいは全体的に含めることができるようなあらゆる方法でフレキシブル駆動シャフトを介してエネルギィを伝達することによって、駆動させることができる。 The operation of the device is performed using an electric motor. The device may also be via a flexible drive shaft by a plurality of electric motors, by a hydraulic or pneumatic motor, or in any manner that allows the actuation assembly to be included uniquely or entirely in the distal portion of the device. It can be driven by transmitting energy.
これらの手段のいずれかによって行われた仕事は、スクリュドライブ、ギアドライブ、ウエッジ、トグル、カム、ベルト、プーリ、ケーブル、ベアリング、あるいは押出ロッドのようなものを単一で、あるいはこれらを組み合わせて所望の動きに変換することができる。特に、スクリュドライブは、電気モータの動きを線形の動きに変換するのに使用される。一の実施例では、スクリュドライブのモータが、ハンドルに設けられている。フレキシブルに回転するケーブルがモータからねじ式シャフトに連結されている。従って、モータがいずれかの方向に回転すると、フレキシブルケーブルの回転がねじ式駆動シャフトに伝わって、ステープリングアクチュエータと切断スライドが駆動シャフトの上に配置されているので、スライドの遠位側の動きによって両方の機能が実行される。第2の実施例では、モータ全体が端部作動体内に設けられており、直接にあるいはトランスミッションギアを介してスライド駆動シャフトに連結されたシャフトを有する。この場合、ハンドル内に必要なものは、オン/オフ及び駆動シャフト方向アクチュエータであり、前者はモータのオンとオフを切り替えるためのものであり、後者は、モータがスピンする方向を決定するためのものである。 The work done by any of these means can be a single thing like screw drive, gear drive, wedge, toggle, cam, belt, pulley, cable, bearing, or push rod, or a combination of these It can be converted into a desired movement. In particular, screw drives are used to convert electric motor motion into linear motion. In one embodiment, a screw drive motor is provided on the handle. A flexible rotating cable is connected from the motor to the threaded shaft. Thus, when the motor rotates in either direction, the rotation of the flexible cable is transmitted to the screw drive shaft, and the stapling actuator and cutting slide are placed on the drive shaft, so the distal movement of the slide To perform both functions. In the second embodiment, the entire motor is provided in the end working body and has a shaft connected to the slide drive shaft directly or via a transmission gear. In this case, what is needed in the handle is an on / off and drive shaft direction actuator, the former is for switching the motor on and off, and the latter is for determining the direction in which the motor spins. Is.
このデバイスは、スクリュドライブで駆動されるキャリッジを有しており、ステープラこう合を閉じる、切断刃を前進させる、ステープルを発射するといった機能を含めて、多くの機能を行う。キャリッジは、これらのタスクを行うための唯一の方法ではない。二次的なあるいは多くの仕事源が、これらの機能のいずれかを行うのに必要な仕事を提供する。 This device has a carriage driven by a screw drive and performs many functions, including functions such as closing the stapler engagement, advancing the cutting blade, and firing staples. The carriage is not the only way to perform these tasks. Secondary or many work sources provide the work necessary to perform any of these functions.
端部作動体の第2の実施例では、ステープリング及び切断作動デバイス全体が自蔵式であり、動作ジョイントの遠位側に配置されている。 In a second embodiment of the end effector, the entire stapling and cutting actuating device is self-contained and is located distal to the motion joint.
作動デバイス全体を挿入し、オペレータによって所望されるあらゆる動きあるいは制限を行う多軸「ボール」ジョイントあるいは「ユニバーサル」ジョイントによって操作することができる。 The entire actuation device can be inserted and manipulated by a multi-axis “ball” or “universal” joint that performs any movement or restriction desired by the operator.
更に、作動デバイス全体は、ハンドルから完全にフリーであり、別の角度から再度把持することができ、より良好な位置的フレキシビリティが可能である。 Furthermore, the entire actuation device is completely free from the handle and can be gripped again from another angle, allowing for better positional flexibility.
本発明の更なる特徴によれば、受動的連接ジョイントが、ボールと、カップデバイスと、当該ボールとカップデバイスを互いに係止し、係止を解除するボール−カップ係止デバイスを有するボールジョイントであり、このボール−カップ係止デバイスは、制御ハンドルが非作動状態にあるときに係止状態にあり、制御ハンドルが作動状態にあるときに係止が解除された状態になる。端部作動体は、このボールとカップデバイスの一方を有し、制御ハンドルがこのボールとカップデバイスの他方を有する。ボールは、カップデバイスに取り外し可能に連結されている。 According to a further feature of the present invention, the passive articulating joint is a ball joint having a ball, a cup device, and a ball-cup locking device that locks the ball and the cup device together and releases the locking. Yes, the ball-cup locking device is in a locked state when the control handle is in an inoperative state and is unlocked when the control handle is in an activated state. The end effector has one of the ball and cup device and the control handle has the other of the ball and cup device. The ball is removably coupled to the cup device.
本発明の更なる特徴によれば、端部作動体は、縦方向に二つの端部を有し、前記ボールが二つのボールである。この二つのボールはそれぞれ、縦方向の二つの端部の一方の上に配置されており、二つのボールは各々カップデバイスに取り外し可能に連結することができる。 According to a further feature of the present invention, the end effector has two ends in the longitudinal direction and the balls are two balls. Each of the two balls is disposed on one of the two longitudinal ends, and each of the two balls can be removably coupled to the cup device.
本発明の一の態様では、縦方向に移動する発射機構を用いて器具が端部作動体を作動させる。この発射機構は、側方支持プレートあるいは固い支持チャネルによって連接機構を介して有利に支持されている。前者の実施例では、発射機構上の負荷の発射によりよく応答するために、各支持プレートの一又はそれ以上の端部が、連接機構の一方の側に弾性あるいはバネで係合しており、従って、発射機構の座屈をより良好に防止することができる。例えば、支持プレート対は、連接機構を横切って発射機構の側面に位置し、各支持プレートは連接機構に形成されたフレーム溝にばねで係合した端部を具えており、連接機構内あるいは外の発射機構の座屈の防止を補助する。 In one aspect of the invention, the instrument activates the end effector using a longitudinally moving firing mechanism. This firing mechanism is advantageously supported via a linkage mechanism by a side support plate or a rigid support channel. In the former embodiment, one or more ends of each support plate are elastically or spring-engaged on one side of the articulation mechanism in order to respond better to the firing of the load on the firing mechanism, Therefore, the buckling of the firing mechanism can be prevented better. For example, a pair of support plates is located on the side of the launch mechanism across the articulation mechanism, and each support plate has an end engaged by a spring in a frame groove formed in the articulation mechanism, inside or outside the articulation mechanism. Helps prevent buckling of the launch mechanism.
チャネルの実施例においては、連接機構内をチャネルが浮動しており、連接がいずれかの方向で生じると発射機構のいずれかの側を支持する面を有する。従って、発射機構の座屈を防止することができる。チャネルはフロアと二つの側部を有する。支持チャネルは、連接機構内部のキャビティ内に自在に乗っている。チャネルの端部は、このキャビティの湾曲に合致するように湾曲している。支持チャネルは、連接機構内で曲がったときに発射機構に接触して支持するさまざまな内部表面を有しており、これによって、連接機構内部あるいは外部における発射機構の座屈を防止することができる。 In the channel embodiment, the channel floats within the articulation mechanism and has a surface that supports either side of the firing mechanism when the articulation occurs in either direction. Therefore, buckling of the firing mechanism can be prevented. The channel has a floor and two sides. The support channel rests freely in a cavity inside the articulation mechanism. The end of the channel is curved to match the curvature of this cavity. The support channel has various internal surfaces that contact and support the firing mechanism when bent within the articulation mechanism, thereby preventing buckling of the firing mechanism inside or outside the articulation mechanism. .
従って、さまざまなタイプの作動した診断又は治療端部作動体を、強い発射力であっても、内視鏡仕様に部品寸法を小さくしても、連接機構で座屈を生じることなく、本発明の連接型医療器具に組み込むことができる。 Therefore, the present invention does not cause buckling in the articulating mechanism even if the various types of actuated diagnosis or treatment end effectors have a strong firing force or the size of parts in the endoscope specification is reduced. Can be incorporated into any articulated medical device.
本発明の更なる態様においては、医療器具が、閉鎖動作、発射動作、連接機構の係止解除動作、及び連接動作を生じるハンドル部分を有している。これらの動作は、各々シャフトを取って伝達される。端部作動体は、ステープルまたはステープルカートリッジを受けるシャフトに連接された細長チャネルと、この細長チャネルに回動可能に連結され、シャフトからの閉鎖動作に応答する台座を具える。発射デバイスは細長デバイスと台座との間で縦方向に受けられている、遠位側にある切断デバイスを具える。発射デバイスは、ハンドルから端部作動体へ、シャフトと連接機構を介して連結されている。発射デバイスは、ステープリングを利用して、発射動作によって切断を行う。連接機構は、シャフトに対して端部作動体を移動させる。連接機構は、遠位側でシャフトに連結されており、連接ロックが解除された(すなわち、アンロック)後、及び、端部作動体に働いて連接動作を生じさせる力に応答して、端部作動体を連接させる。換言すれば、連接ロックが解除されると、端部作動体の環境に対する圧力が端部作動体をシャフトに対して連接させる。発射機構を支持するために、一対の支持プレートを連接機構にわたって発射機構の側面に位置することができる。各支持プレートは連接機構内に形成されたフレーム溝にスプリングで係合された端部を具える、あるいは、固いチャネルが連接機構にわたって発射機構を取り囲むようにしても良い。これによって、改良されたステープリングおよび切断器具が、高い発射負荷に耐える発射デバイスを含んでおり、連接時に有意に大きくなった発射力を導入することがない。 In a further aspect of the invention, the medical device has a handle portion that produces a closing action, a firing action, an unlocking action of the articulating mechanism, and an articulating action. These movements are each transmitted through the shaft. The end effector includes an elongate channel connected to a shaft that receives the staple or staple cartridge, and a pedestal that is pivotally connected to the elongate channel and is responsive to a closing action from the shaft. The firing device includes a distal cutting device that is received longitudinally between the elongate device and the pedestal. The launch device is coupled from the handle to the end effector via a shaft and articulation mechanism. The firing device uses stapling to cut by a firing action. The articulation mechanism moves the end effector relative to the shaft. The articulation mechanism is connected distally to the shaft and after the articulation lock is released (ie, unlocked) and in response to the force acting on the end effector to produce the articulation action. Connect the actuators. In other words, when the connection lock is released, the pressure on the environment of the end effector causes the end effector to be connected to the shaft. To support the firing mechanism, a pair of support plates can be positioned on the side of the firing mechanism across the articulating mechanism. Each support plate may include a spring-engaged end in a frame groove formed in the articulation mechanism, or a rigid channel may surround the firing mechanism across the articulation mechanism. Thus, the improved stapling and cutting instrument includes a firing device that can withstand high firing loads and does not introduce significantly increased firing force when articulated.
作動デバイスは、様々な長さで製造しても良く、及び/又は、腹腔鏡用あるいは内視鏡用のいずれか、あるいは両方に好適な直径に製造しても良い。交換可能なステープルカートリッジを使用することができる。また、作動デバイスは、フレキシブルな内視鏡の遠位端に取り付けるように構成することができる。 The actuation device may be manufactured in various lengths and / or may be manufactured to a diameter suitable for either laparoscopic or endoscopic or both. A replaceable staple cartridge can be used. The actuation device can also be configured to attach to the distal end of a flexible endoscope.
本発明の有意な利点は、端部作動体の動きが受動的であり、係止可能であることである。換言すると、端部作動器は、係止を解除して、次いで所望の位置に移動させ、次いで、その新しい位置に保持することができる。これらの動作は、全て片手の操作で行うことができる。内視鏡及び腹腔鏡外科手術は、外科医が両方の手を別個に使用できることが必要である。この必要性をなくすことは、外科手術をものすごく困難なものにするか、あるいは不可能にする。本発明のハンドルは、二本めの手を用いることなく移動解除/係止を作動でき、真の片手でのデバイスの操作を可能にしている。 A significant advantage of the present invention is that the end effector movement is passive and lockable. In other words, the end actuator can be unlocked and then moved to the desired position and then held in its new position. All of these operations can be performed by one-handed operation. Endoscopic and laparoscopic surgery requires that the surgeon can use both hands separately. Eliminating this need makes surgery extremely difficult or impossible. The handle of the present invention can be actuated to release / lock without using a second hand, allowing the device to be operated with a true one hand.
本発明の更なる利点は、端部作動体の軸方向の動きが別であり、手動であることである。例えば、ユーザは、挿入の前にデバイスの縦軸を中心に遠位側端部作動体を回転させることによって軸方向の動きを設定することができる。この予め設定した位置決めは、端部作動体をシャフトから離れる方向に引っ張り、次いで遠位側端部作動体を所望の方向にひねることによって生じる。この軸方向の動きは、軸外の動き(横方向の動き)と組み合わせて、遠位端で合成角を作って、端部作動体(または複数の端部作動体)の正確な位置決めを助ける。別の変形例では、ユーザは、シャフト、連接機構、及び端部作動体を含む遠位側構成部品に、ハンドルを軸方向に固定して、回転方向には自在に連結する回転デバイスを提供することによって、いつでも、動的に遠位側端部作動体をデバイスの縦軸を中心に回転させることができる。遠位側構成部品の回転は、ベル形状の回転デバイスを端部作動体から離れる方向に引っ張って生じ、次いで、所望の方向にシャフトの縦軸を中心に回転デバイスの回転が生じる。この回転運動が、端部作動体の軸外運動と組み合わされて、デバイスの遠位端に合成角を作り、端部作動体(または複数の端部作動体)の正確な位置決めを補助する。 A further advantage of the present invention is that the axial movement of the end effector is separate and manual. For example, the user can set the axial movement by rotating the distal end effector about the longitudinal axis of the device prior to insertion. This preset positioning occurs by pulling the end effector away from the shaft and then twisting the distal end effector in the desired direction. This axial movement, combined with off-axis movement (lateral movement), creates a composite angle at the distal end to aid in precise positioning of the end effector (or multiple end effectors). . In another variation, the user provides a rotating device that axially secures the handle to a distal component that includes a shaft, articulation mechanism, and end effector, and is freely coupled in the rotational direction. This allows the distal end effector to be dynamically rotated about the longitudinal axis of the device at any time. The rotation of the distal component occurs by pulling the bell-shaped rotation device away from the end effector, and then the rotation of the rotation device about the longitudinal axis of the shaft in the desired direction. This rotational motion, combined with the off-axis motion of the end effector, creates a composite angle at the distal end of the device to assist in the precise positioning of the end effector (or end effectors).
本発明の更に別の利点は、ステープラ/カッタを、標準的なフレキシブル内視鏡の端部に装着するように構成できることである。この制御は、内視鏡の作業チャネルを通って送り戻され、制御ハンドルまたは制御モジュールに合致する。 Yet another advantage of the present invention is that the stapler / cutter can be configured to attach to the end of a standard flexible endoscope. This control is sent back through the working channel of the endoscope and matches the control handle or control module.
本発明の目的を鑑みると、医療デバイスの端部作動体を操作する方法も提供されている。この方法は、連接ロックを用いて安定した位置で端部作動体の連接動作を制御する受動的連接ジョイントを維持するステップと、連接ロックの解放を作動して、受動的連接ジョイントの係止を解き、端部作動体に係る外力に応じて受動的連接ジョイントを介して端部作動体を連接動作させるステップと、を具える。 In view of the objects of the present invention, a method for operating an end effector of a medical device is also provided. The method includes maintaining a passive articulation joint that controls the articulation of the end effector in a stable position using an articulation lock, and actuating the release of the articulation lock to lock the passive articulation joint. Unwinding and articulating the end effector via a passive articulation joint in response to an external force on the end effector.
本発明の目的を鑑みると、医療デバイスの端部作動体を操作する方法が提供されており、この方法は、連接ロックによって係止状態にある受動的連接ジョイントを保持するステップと、連接ロックを作動してこの受動的連接ジョイントの係止を解き、端部作動体に作用する外力に応じて受動的連接ジョイントに連接動作をさせるステップと、を具える。 In view of the object of the present invention, a method is provided for manipulating an end effector of a medical device, the method comprising: holding a passive articulation joint that is locked by an articulation lock; Actuating to unlock the passive articulation joint and causing the passive articulation joint to actuate in response to an external force acting on the end effector.
本発明の別のモードによれば、端部作動体は、連接位置へ受動的に移動する。 According to another mode of the invention, the end effector is passively moved to the articulated position.
本発明の更なるモードによれば、端部作動体は端部作動体の一部を環境の構造に対して押圧することによって連接位置に受動的に移動する。 According to a further mode of the invention, the end effector is passively moved to the articulated position by pressing a part of the end effector against the structure of the environment.
本発明の更なるモードによれば、端部作動体を所望の連接位置に連接するために、端部作動体に力が加えられる。 According to a further mode of the invention, a force is applied to the end effector to connect the end effector to the desired articulation position.
本発明の更なるモードによれば、連接ロックの作動が取り除かれて受動的連接ジョイントを係止し、これによって、端部作動体が更に連接動作を行うことを防止する。 According to a further mode of the invention, the operation of the articulation lock is removed and the passive articulation joint is locked, thereby preventing the end effector from further articulating.
有利なことに、上述のステップの全てが片手で行われる。 Advantageously, all of the above steps are performed with one hand.
本発明の特徴と考えられるその他の特徴は、請求の範囲に記載されている。 Other features which are considered as characteristic for the invention are set forth in the appended claims.
本発明は、外科用ステープル及び切断デバイス及びこのデバイスを使用する方法として、図に示し、記載したが、さまざまな変形例と構造的な変形を、本発明の精神から外れることなく、請求の範囲の範囲および均等の範囲内で行うことができるので、図に示す詳細に限定するものではない。 Although the present invention has been shown and described in the drawings as a surgical stapling and cutting device and method of using this device, various modifications and structural variations can be made without departing from the spirit of the invention. However, the present invention is not limited to the details shown in the drawings.
本発明の構成及び操作方法は、追加の目的と利点と共に、添付の図面と共に読む場合に以下の特定の実施例の記載から最も良く理解される。 The structure and method of operation of the present invention, together with additional objects and advantages, are best understood from the following description of specific embodiments when read in conjunction with the accompanying drawings.
本発明の態様を、本発明の特定の実施例に関する以下の説明と図面に開示する。本発明の精神または範囲から外れることなく代替の実施例を考案することができる。更に、本発明の例示的な実施例のよく知られた要素は、詳細には説明しない、あるいは、本発明の関連する詳細を邪魔しないように、説明を省略する。 Aspects of the invention are disclosed in the following description and drawings relating to specific embodiments of the invention. Alternate embodiments may be devised without departing from the spirit or scope of the invention. Moreover, well-known elements of exemplary embodiments of the invention will not be described in detail or will not be described in order not to obscure the relevant details of the invention.
本発明を開示して説明する前に、ここで使用する用語は、特定の実施例を記載するだけの目的であり、限定を意図するものではない。明細書及び特許請求の範囲に使用されているように、単数形の冠詞は、コンテキストから明らかでない限り、複数の意味もあることに留意すべきである。 Prior to the disclosure and description of the present invention, the terminology used herein is for the purpose of describing particular embodiments only and is not intended to be limiting. It should be noted that as used in the specification and claims, the singular article also has multiple meanings unless the context clearly indicates otherwise.
本明細書は、新規と考えられる本発明の特徴を規定する請求の範囲で結ばれているが、本発明は、図面と併せて以下の説明を考慮することでより良く理解されると考えられる。図面には、同じ符号が用いられている。図面は、スケールどおり記載されていない。 While the specification concludes with claims that define the features of the invention believed to be novel, it is believed that the invention will be better understood in view of the following description in conjunction with the drawings. . The same reference numerals are used in the drawings. The drawings are not drawn to scale.
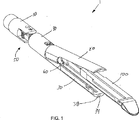
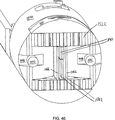
図面を詳細に、特にまず図1を参照すると、本発明によるステープリング及び切断用端部作動体1の第1の例示的実施例が示されている。端部作動体の主要部品には、クレビス10、台座20、ステープルカートリッジ100を受けるカートリッジホルダ30、アダプタスリーブ40、及び横方向移動又は連接デバイス50が含まれる。図1は、カートリッジホルダ30からのステープルカートリッジ100の着脱性を示している。
Referring now in detail to the drawings, and more particularly to FIG. 1, a first exemplary embodiment of a stapling and cutting
台座20をカートリッジホルダ30と、ステープルカートリッジ100に連結しているのは、ステープル作動及び組織切断スライド60である。スライド60は、台座20とカートリッジホルダ30に動作可能に係合しており、この二つの部品20と30を正しく整列させて保持し、カートリッジ100の中で作動したステープルが、台座20内の各ステープラ台座に当たり、台座20とカートリッジ100の間に配置された組織の回りにこのステープルを固定するようにする。スライド60の遠位側を向いた面は、組織を互いにステープルするときに、こう合20、30内に配置された組織を切断する刃62を有する。このスライドの近位側の動きが、図1乃至3に線図的に示されている。スライド60は、図1及び3に見ることができ、台座20は、スライド60の先端から外れている。しかしながら、動作中は、スライド60は、図2、特に図13に示すように、台座20に連結されていなければならない。
Connecting the
図2は、アダプタスリーブ内での移動のさまざまな特徴を見せるために、アダプタスリーブ40を取り除いた端部作動体1を示す図である。
FIG. 2 shows the
横方向移動デバイス50の二つの主要部品の第1の部品が、図1乃至3に明らかである。近位側部品52は、近位側スプロケット522と、中間スプライン加工コネクタ524、及び遠位側ロッド526を具える。例示的な実施例では、中間スプライン加工コネクタ524は、図2に明瞭に示すように、4本の遠位側に突出した歯5242を有する。
The first of the two main parts of the
また、図2には、引っ張りケーブルアダプタ70が示されている。この引っ張りケーブルアダプタ70は、近位側側部が引っ張りケーブル110(破線)に連結されており、遠位側側部がカートリッジホルダ30に連結されている。従って、引っ張りケーブルアダプタ70を用いて、台座20に対してカートリッジホルダ30を押したり引いたりして、これによって、カートリッジホルダ30の動きに応じて、台座20が開位置から閉位置へ、あるいは、反対に回動する。台座20の近位端は、両側部にカムフォロワ22を有する。カートリッジホルダ30の近位端は、両側部に二つのカム面32を規定しており、各カムフォロワ22を受けるように整列している。従って、遠位方向あるいは近位方向へのカートリッジホルダの動きによって、台座20に対応する開回動または閉回動が生じる。
Also shown in FIG. 2 is a
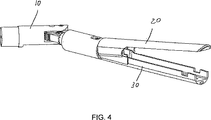
図4は、クレビス10に対するステープラ20、30の横方向の連接動作を示す図である。
FIG. 4 is a diagram illustrating a lateral connecting operation of the
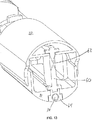
図5乃至8では、アダプタスリーブ40と、クレビス10を含む全ての部品がワイヤフレームで示されており、これによって、内部の特徴がわかる。クレビス10は、4つのルーメンを具えており、その内の二つが図5に示されており、図6および図7には、4つのルーメン全てが示されている。これらのルーメンの内、第1のルーメン12は、端部作動体横方向移動係止ピン120の遠位側及び近位側への移動を制御する、図示しないシャフトを含むように形成されている。このピン120は、図8及び図9にまず示されている。二つの横方向ルーメン14は、引っ張りケーブルアダプタ70を近位側に移動させる引っ張りワイヤを受けるような形状をしている(引っ張りケーブルアダプタ70の遠位側への移動は、バネによって生じる)。二つのルーメン14の他のルーメンは、余分なルーメンであり、追加の器具をいくつでも受けることができる。駆動ケーブルルーメン16は、4つのルーメンの最後のルーメンであり、スライド60の動きを制御する駆動スクリュ34(図1参照)を回転させるフレキシブル駆動ケーブルを受けるように構成されている。
In FIGS. 5-8, the
駆動ケーブルルーメン16の遠位端において、クレビス20は、横方向移動係止ピン120を受ける長円キャビティ18を規定している。図6乃至9は、特に、このキャビティ18の例示的な形状を示す。横方向移動係止ピン120は円周形状が長円形であるため、ピン120はスプロケット522の歯に整列した位置から回転しない。
At the distal end of the
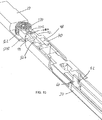
また、図5に示すクレビス10の先端側の下には、二つの復心ばね130が見える。これらのばね130は、図6乃至9、特に図10にも示されている。ばね130間の望ましくない相互作用を防ぐために、バネ130を挟んで分離プレート140が設けられている。図10は、間に分離プレート140を有する二つのバネ130を示す図である。
Also, two decentering
透明のスリーブ40の下側の機構は、図7乃至10でよりよく説明される。スリーブ40は、二つの外側構造と、二つの内部ボアを規定している。第1の外側構造は、近位側シリンダ42である。近位側シリンダ42は、その近位端にスプライン構造422を規定している。これらのスプライン構造422は、近位側部分52の中間のスプライン付コネクタ524に合致して相互作用する。近位側シリンダ42は、第1のボア44も規定しており、これは、近位側部分52の遠位側ロッド526を受けるような形状をしている。ロッド526と第1のボア44の内側面との間には円筒状の半径方向クリアランスが、ケーブルアダプタ70の近位端と第1のボア44の近位内側面との間は縦方向クリアランスがある。この筒状クリアランスは、明瞭化のために図示していない第1の筒状バイアスデバイス(例えば、コイルばね)を受けることができる。第1のバイアスデバイスは、アダプタスリーブ40の最も近位側端部に近位側を向いた力をかける位置にある。このような構成において、第1のバイアスデバイスによってかかる力が、遠位側スプライン構造422を近位側スプライン構造5242に向けて、これに対して押圧する。
The mechanism below the
スリーブ40の第2の外側構造は、遠位側シリンダ46である。この遠位側シリンダ46は、そこで引っ張りケーブルアダプタ70を受ける形状をしている第2のボア48を規定する。引っ張りケーブルアダプタ70も、近位側部分52の遠位ロッド526を受ける形状の内側ボア72を規定している。この構造を明確にするために、ロッド526は、図9において破線で内側ボア72に完全に延在している様子が示されている。作動時は、ロッド526は、内側ボア72内へ完全に延在する。内側ボア72は、同軸であり、例示的な実施例では、第1のボア44と同じ内径を有する。従って、ロッド526と内側ボア72の内側面との間には円筒状半径方向のクリアランスがあり、ケーブルアダプタ70の遠位側表面と、内側ボア72の内側遠位側表面との間には縦方向のクリアランスがある。これは、第2の筒状バイアスデバイス(例えば、コイルスプリング)を収容する形状をしているためであり、明瞭にするために図には示していない。第2のバイアスデバイスは、引っ張りケーブルアダプタ70に対して遠位側に向けたバイアス力を与えるように設けられている。このような力は、こう合20、30を開位置に保つ。従って、こう合20、30は安定した開位置を有する。
The second outer structure of the
中間部分を設けることなく、図示しない二つのバイアスデバイスが連結しており、従って、単一のバネを形成している。しかしながら、二つのバイアスデバイスは相互作用しないことが望ましい。なぜなら、スプライン部分の分離によって、キャリッジに望ましくない力がかかり、キャリッジホルダ30の動きがスプライン部分の連結を緩めることがあるからである。従って、引っ張りケーブルアダプタ70の近位端表面と、第2のボア48の遠位端表面とによって規定される筒状キャビティ74内の二つのバイアスデバイス間に、図示しないワッシャが配置されている。図7は、このワッシャを保持するための近位側側部を特に示す図であり、このワッシャはそこを通る遠位側ロッド526を受けるだけの形状をしている。従って、ワッシャが引っ張りケーブルアダプタ70とスリーブ40との間にはまるので、二つのバネが外れ、互いに独立したバイアス力を提供する。
Without providing an intermediate portion, two bias devices (not shown) are connected, thus forming a single spring. However, it is desirable that the two bias devices do not interact. This is because the separation of the spline portion applies an undesirable force to the carriage, and the movement of the
図11および12の下側の図は、スライド60の駆動シャフト34と、カートリッジホルダ30内の適所に駆動シャフト34を保持する近位側アイドラブッシュ36を示す。アイドラブッシュ36のこの位置では、駆動シャフト34にはねじがついていない。しかしながら、アイドラブッシュ36の近位側では、駆動シャフト34に、駆動シャフト34の遠位端へ延在するねじが設けられている(図示せず)。図11及び12は、駆動シャフト34の対向する端部上にスラストベアリング38を示していないが、図1は、このベアリング38を明確に示している。図11、12、及び13には、駆動ナット64の形状をしたスライド60の底部が示されている。例示的な実施例では、この駆動ナット64は、スライド60の刃62から分離された一部であるが、刃62の底部に固定的に連結されている。図に示す形状の駆動ナット64は、ダンベル形状の断面を有し、ねじの上にかかる力をいくらか軽減している。図11では、駆動ナット64は、台座20が開位置にある近位側位置にある。図12および13は、反対に、台座20が部分的に閉じた位置にある中間位置の駆動ナット64を示す。
The lower view of FIGS. 11 and 12 shows the
図13は、刃62と駆動ナット64を具えるスライド60の形状と構造を示すのに特に有益である。
FIG. 13 is particularly useful for showing the shape and structure of a
図14及び図15に示す端部作動体のほぼ縦軸に沿った水平断面は、遠位ロッド526の周囲のボアを示すのに特に有益である。また、ロッド526は、引っ張りケーブルアダプタ70のボア72の遠位側表面への経路全体に延在しているが、明瞭にするために、そのようには示されていない。ロッド526の近位端の周囲には、アダプタスリーブ46内の第1のボア44がある。第1のボア44のすぐ遠位側に、その中のワッシャを受けるキャビティ74があり、キャビティ74のすぐ遠位側には、第2のバイアスデバイスを受ける引っ張りケーブルアダプタ70の内側ボア72がある。
The horizontal cross section along the generally longitudinal axis of the end effector shown in FIGS. 14 and 15 is particularly useful to show the bore around the
図16に示す端部作動体の縦軸にほぼ沿った縦断面は、駆動ナット64と駆動シャフト34の間の連結を示すのに特に有益である。同様に、明瞭可のために、引っ張りケーブルアダプタ70内のボア72の近位側表面への全ての経路に延在しているロッド526は示されていない。
A longitudinal section generally along the longitudinal axis of the end effector shown in FIG. 16 is particularly useful to show the connection between the
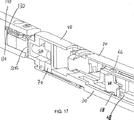
図17に示す端部作動体の縦軸にほぼ沿った縦断面は、スライド60と台座20及びカートリッジホルダ30との間の連結を見るのに特に有益である。二つの上側ウイング66は、台座20内の溝内に配置されており、二つの下側ウイング68は、下側ウイング68と駆動ナット64によって形成されたI字形状の上側保持表面を形成している。
A longitudinal section generally along the longitudinal axis of the end effector shown in FIG. 17 is particularly useful for viewing the connection between the
図18乃至24は、本発明に係るステープリングデバイスの縦方向の全寸法を示す図であり、遠位側端部作動体1と、作動ハンドル2の第1の例示的実施例を示す。図60に示すように、こう合20、30は開位置で安定している。
FIGS. 18-24 are diagrams illustrating all longitudinal dimensions of a stapling device according to the present invention, showing a first exemplary embodiment of a
引っ張りケーブルアダプタ70で終端している引っ張りケーブルの近位端に親指トリガが連結している。従って、親指トリガ3が作動すると(図19参照)、カートリッジホルダ30が近位方向に引っ張られる。カム面32の形状によって、カムフォロワ22が移動し、これによって、台座20をほぼステープリング位置に回動させる。上述したとおり、カートリッジホルダ30、従って、ステープルカートリッジ100に対して台座20を確実に正しい平行方向に向けるのは親指トリガ3ではない。むしろ、正しい平行方向を確実にしているのはスライド60である。
A thumb trigger is connected to the proximal end of the pull cable that terminates in the
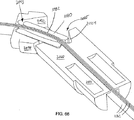
図20乃至22は、端部作動体1が横方向においてどのように受動的に連接しているかを示す図である。人差し指トリガ4を押すと、横方向移動係止ピン120が後側に移動して、スプロケット522から外れる。端部作動体1に何ら力が加わらなければ、二つの復心ばね130によって、端部作動体1は、図18及び19に示すように、軸方向に整列した方向に残る。しかしながら、外からの力が端部作動体1に与えられると(図20に示すように)、横方向に自在である端部作動体1は、スプロケット522の軸を中心に、例えば、図20に示すほぼ45度左の位置、あるいは、その他の方向といった、どの位置へでも回動できる。例えば図22を参照されたい。人差し指トリガ4を解放すると、スプロケット522の二本の歯の間の係止ピン120の遠位端を戻すことによって、横方向の動きは防止される。このように、図21及び22に例示するように、端部作動体は、多数の横方向に連接した位置に係止させることができる。明瞭可のために、ステープルカートリッジ100は図18ないし24には記載されていないことに留意されたい。
20 to 22 are diagrams showing how the
図23と24は、端部作動体の軸方向の回転制御を示す図である。このような軸方向の回転制御は、アダプタスリーブ40と横方向の移動デバイス50のそれぞれの二つのスプライン構造422、5242によって提供される。図23では、スプライン構造が係合しており、台座20は、ハンドルに対して90度の位置にある。スプライン構造の係合をはずすために、第1のバイアスデバイスに打ち勝つ十分な力が端部作動体1にかかり、スプライン構造422、5242が分離する。次いで、端部作動体1が、時計方向または半時計方向に回転することができる。図68は、例えば、台座20が反時計方向に、約9時の位置に回転した状態を示す。
23 and 24 are diagrams showing the axial rotation control of the end effector. Such axial rotation control is provided by two
図1乃至3は、本発明のステープリングデバイスの電動式ステープリング機能の動作を示すのに使用することができる。図1では、スライド60が近位位置にある。可逆モータは、ハンドル内部に収納されている。3方向スイッチがモータに連結されている。中央位置にあるときに、例えば、モータがオフになる。近位側にあるときは、モータがオンになって、駆動シャフト34を回転させ、スライド60が近位方向に移動する。逆に、スイッチが遠位位置にあると、モータがオンになって、スライド60が遠位方向に移動するように駆動シャフト34を回転させる。もちろん、スイッチは、オフ位置のない、単なる2方向スイッチでも良い。
1-3 can be used to illustrate the operation of the electric stapling function of the stapling device of the present invention. In FIG. 1, slide 60 is in a proximal position. The reversible motor is housed inside the handle. A three-way switch is connected to the motor. For example, the motor is turned off when in the center position. When in the proximal side, the motor is turned on to rotate the
図25及び26は、本発明のステープリング及び切断システム200の第2の例示的実施例を示す図である。このシステム200は、電動式ステープリングアッセンブリ全体が端部作動体210に含まれている点で、第1の実施例と異なる。従って、ハンドル220は、二つの作動デバイスを必要とするのみである。第1の作動デバイス222は、ボールジョイント解除レバーであり、第2の作動デバイスは、ステープリング/切断モータオン/オフボタン224である。
25 and 26 are diagrams illustrating a second exemplary embodiment of the stapling and cutting
端部作動体210は、ボールジョイントコネクタ228におけるハンドル220の作動シャフト226の遠位端に連結されている。端部作動体210は、最も遠位端に、ボールジョイント212を有する。ボールジョイント212は、二つの対向するカップ形状クランプ2122、2124を有する。クランプ2122、2124の内側面は、ボールジョイント212の外側形状に対応する形状をしている。クランプ2122、2124は、レバー222の作動に基づいて、互いに向けてあるいは互いから離れるように移動する。
クランプ2122、2124は、閉位置において互いに対してバイアスしており、ボールジョイント212がその中に配置されている場合は、二つのクランプ2122、2124がボールジョイント212をしっかり把持する。レバー222の作動によって、クランプ2122、2124が分離し、これによって、ボールジョイント212が二つのクランプ2122、2124内で自在に回転できる。従って、レバー222が作動すると、端部作動体210は、ステープリング/切断部位近傍の組織などの環境内の構造に対する圧力に基づいて「自在」に動く。レバー222を十分に押し下げて、ボールジョイント212をクランプ2122、2124の外に完全に移動させる。従って、第1の端部作動体210が第1の部位でクランプされ、第2の端部作動体210が第2の部位でとまって切断することが所望される場合は、第1の端部作動体210は第1の端部でクランプされたままで、シャフト226を本体から取り外して、第2の端部作動体210に負荷をかけて、第2の端部作動体210を第2の部位に案内することができる。
The
第2の作動デバイス224は、ユーザが端部作動体210を用いてステープリング及び切断を行うことを所望するときに必要である。端部作動体210は、ステープリング/切断の所望の位置にあるときに、アクチュエータ224(例えば、ボタン)を押す。好ましくは、この作動が、端部作動体210内部のモータへ電力を供給する回路を接続し(あるいは遮断する)、これによってスライド60を遠位側へ移動させて、こう合のステープリングと切断機能を実行する。
The
図25は、ボールジョイント212に対していずれかの位置に端部作動体210を方向付けるための全く自在な状態を示す。図25では、端部作動体210は、右横方向に約45度の位置に、台座は約90度の位置に示されている。
FIG. 25 shows a completely free state for directing the
図27及び28は、図25と26に示す端部作動体の第2の実施例の変形例を示す図である。特に、ハンドル220は、図25と26に示すものと同じである。しかしながら、端部作動体310は異なる。特に、端部作動体310は、図25及び26に示すボールジョイント212と同じ近位側ボールジョイント312を有するが、近位側ボールジョイント312とほとんど同じ形状の第2の遠位側ボールジョイント314も有する。従って、レバー222を押し下げてボールジョイント312、314を解放すると、端部作動体310を本体内に位置させることができ、反対側の端部をクランプ2122、2124で挟むことができる。このような図27に示す方向において、開いたこう合がユーザに対向しているときに、ステープリング/切断を作動することができる。
27 and 28 are views showing a modification of the second embodiment of the end effector shown in FIGS. 25 and 26. FIG. In particular, the
端部作動体210、310を手術部位に配置することは、端部作動体210、310の開いたこう合に比較して、手術部位へのアクセスがむしろ小さいことが求められる。端部作動体310を反転させる能力によって、シングルボールジョイント端部作動体210をもっては到達できない、到達が困難であったいくつかの部位にアクセすることができる。
Placing the
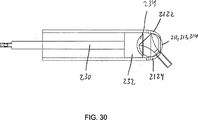
図29及び30は、図25乃至28の端部作動体210、310のボールジョイント212、312、314を保持している図25乃至28に示す外科用ステープリング及び切断デバイス200、300の作動シャフト226の最も遠位端にあるクランプ2122、2124を示す。これらの図面は、レバー222が、その遠位端にプランジャ232を有する押出ロッド230に連結されていることを示す。このプランジャ232は、最も遠位端に、ボールジョイント212、312、314の外側形状に対応する形状を持つカップ状面234を有する。従って、プランジャ232が最も遠位側位置において、ボールジョイント212、312、314と接触しているとき、ボールが捕捉され、移動あるいは回転しない。逆に、プランジャ232が図30に示すように近位側に移動すると、ボールジョイント212、312、314のボールがクランプ2122、2124の間で自在に回転する。
29 and 30 show the actuation shaft of the surgical stapling and cutting
図31乃至70に示すエンドステープラは、図1乃至30に示すエンドステープラに、様々な異なる代替及び/又は追加の特徴を加えたものである。 The end stapler shown in FIGS. 31-70 is a variety of different alternative and / or additional features to the end stapler shown in FIGS. 1-30.
図31乃至70において、明瞭化のために、先端こう合又は台座1020が示されているのは図30と40のみである。更に、台座20は、図1乃至30を参照して上記に詳述されており、従って、以下では繰り返しの説明を避ける。
In FIGS. 31-70, only the FIGS. 30 and 40 show the tip occlusion or
図31に示す例示的ハンドルは、Ethicon Endo−Surgery、Inc.社で製造されたものであり、Ethicon社のリニアカッタ、モデルECHELON60 Endopath Staplerに見ることができる。従って、このハンドルの説明は、このハンドルの部品及び機能的説明がこの技術で公開されているので、冗長であると考えられる。このような説明は、本明細書に全体的な引用として組み込まれている。 The exemplary handle shown in FIG. 31 is available from Ethicon Endo-Surgery, Inc. And can be found in Ethicon's linear cutter, model ECHELON60 Endopath Stapler. Thus, the description of the handle is considered redundant because the handle's parts and functional description are published in the art. Such description is incorporated herein by reference in its entirety.
上述したとおり、本発明のエンドステープラの遠位端は、標準ステープルカートリッジ100を収納するように構成されている。カートリッジ100も、先行する刊行物に開示されており、ここで繰り返して述べる必要はない。この刊行物は、従って、本明細書に全体的な引用として組み込まれている。
As described above, the distal end of the end stapler of the present invention is configured to house a standard
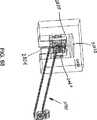
図31は、本発明のエンドステープラ1000の代替の実施例を部分的に示す図である。エンドステープラ1000のハンドル1200上の二つの遠位側作動レバーは、図31では、明確化のために隠れて見えない。
FIG. 31 is a diagram partially showing an alternative embodiment of the
ハンドル1200の遠位端は、ベル状のアクチュエータ1100を具える。これは、エンドステープラ1000の連接部分に二つの制御角度を提供する。第1に、ベルアクチュエータ1100は、ハンドル1200の遠位端上で、エンドステープラ1000の中央軸を中心に自在に回動する。ベルアクチュエータ1100は外側チューブ1100に回動可能に固定的に連接されているため、ベルアクチュエータ1100が時計方向あるいは反時計方向に回転すると、エンドステープラ1000の遠位端全体が対応して回転する。第2に、ベルアクチュエータ1100は、ハンドル1200の遠位端上で、近位方向に所定の距離を超えて移動することができる。以下に更に詳細に記載するように、ベルアクチュエータ1100の近位側の移動によって、連接ロック解放スライド120、1120の対応する動きが、遠位側端部作動体1002を伝達デバイス50、1050において連接させる。例えば、ベルアクチュエータ1100の遠位部分に位置する図示しないバイアスデバイス(例えば、圧縮ばね)を用いて、ベルアクチュエータ1100と、連接係止解除スライド1120に遠位方向にバイアスを与え、ベルアクチュエータ1100を非作動状態にしたまま、連接ロック解除スライド120、1120が動作位置あるいは係止位置に残る。図8及び9を参照されたい。このバイアスデバイスは、ベルアクチュエータ1100の内側に収納されているが、明瞭化のために図32には、示されていない。内側チューブ1130の回りの溝1139に嵌るスナップリングも示されていない。このバイアスデバイスは、ロッド引っ張りブロック1105(図34)の近位側と、スナップリングの遠位側で区切られている。このような構造では、ベルアクチュエータ1100が近位側に引っ張られると、このアクチュエータ1100がロッド引っ張りブロック1105に近位側へ力を加え、これによって、連接係止解除スライド120、1120が係止解除位置に移動する。ベルアクチュエータ1100の内面のキー孔は、形状で係止するように、ロッド引っ張りブロック1105を囲んでおり、内側チューブ1130の縦軸を中心としたベルアクチュエータ1100の回転で、ロッド引っ張りブロック1105に力がかかり、対応する回転がなされる。形状で係止するあるいは形状でフィットする連結は、要素形状自体で二つの要素を互いに連結するものであり、要素への外力によって要素を互いに係止させる力係止連結とは逆である。このように、内側チューブと、デバイス1000の遠位側アッセンブリ全体は、同様に回転する。代替の構成では、ベルアクチュエータ1100の縦の動きが、スライド120、1120を非係止状態に位置させる第1の作動と、スライド120、1120を係止状態に位置させる第2の作動とによって、標準的なボールペンと同様に機能する。
The distal end of the handle 1200 includes a bell-shaped
本発明のベルアクチュエータ1100を用いて、外科医は、エンドステープラ1000のあらゆる機能を片手で取り扱うことができる。
Using the
図32は、ハンドル1200のないエンドステープラ1000の近位端を示す図である。ベルアクチュエータ1100内で同軸に配置した押出ロッド1102は、ステープラが発射方向にあるときに、切断刃1060を移動させるのに用いる。
FIG. 32 shows the proximal end of
図33は、エンドステープラ1000の近位端における部品を示す図であり、この部品は、軸方向に固定的に、及び自在に回転するように、遠位アッセンブリをベルアクチュエータ1100に連結している。特に、内側チューブ1130(外側チューブ1110内部に配置される)は、内側チューブ連結チャンバ1134を規定する近位側エクステンション1132を有する。クラムシェル套管1131は、内側チューブ1130のエクステンション1132にほぼ等しい長さと、近位側エクステンション1132の連結チャンバ1134に対応すると套管連結チャンバ1333を有する。回転カップル1141は、連結チャンバ1133と1134の双方に対応する外側形状を有する遠位側T字型状回転リンク1143を有しており、リンク1143がエクステンション1132と套管1131との間に配置されているときに、リンク1143は自在でありそこで回転する。このカップル1141は、カップル1141の近位端上の近位側ポート1145を通ってハンドル1200の内側に固定されている。
FIG. 33 illustrates a component at the proximal end of the
一緒に配置したときに、内側チューブ1130は、カップル1141に対して軸方向に保持されているが、カップル1141とは独立して回転する。3つの連結部1130、1131、1141が、外側チューブ1110の内側に嵌るサイズなので、これらの部品が外側チューブ1110の内側に配置されると、外側チューブ1110は形状による係止連結となり、内側チューブ1130と套管1131のあらゆる分離を防止する(外側チューブ1110がこの領域を十分にカバーしている限り)。従って、ベルアクチュエータ1100が、内側チューブ1130の縦軸を中心に回転すると、内側及び外側チューブ1110、1130は、チューブ1110、1130の同軸を中心に回転可能であるが、ハンドル1200内側に縦方向に固定されているカップル1141に対しては縦方向に安定している。
When placed together, the
図34は、ハンドル1200、ベルアクチュエータ1100、および外側チューブ1110のないエンドステープラ1000の近位端を示す図である。図に示すように、内側チューブ1130は中空形状であり、ここを通って押出ロッド1102を受ける。このロッドについては、以下に詳細に述べる。これらの図面に示すように、クレビス1010とドラムスリーブ1040は、互いに、エンドステープラ1000の連接接合またはジョイント1050を形成している。
34 shows the proximal end of
この時点では、下側こう合/ステープルカートリッジホルダ1030はハンドル1200に対して縦方向に固定されている点に留意されたい。この固定は、回動可能であり、こう合を閉じる及び/又は開けるためにキー孔形状のカム面32を通って摺動するときにいくらか縦方向に移動する上側台座1020と対照的である(カム面1032について、以下に/上記に更に詳細に述べる)。
Note that at this point, the lower occlusion /
ステープルカートリッジホルダ1030とハンドル1200の縦方向に固定した連結を形成するためには、内側チューブ1130が、ステープルカートリッジホルダ1030に連結されていなければならない。しかし、同時に、ステープルカートリッジホルダ1030が内側チューブ1130の縦方向のエクステントに対して連接可能でなければならない。従って、二つの部品1030、1130の間は、軸方向には固定されているが、横方向に連接されていなければならない。
In order to form a longitudinally fixed connection between the
このような連結を提供するために、本発明は、例えば図35乃至38に示すような、少なくとも一のプルバンド1140を具える。例示的構造においては、多数のプルバンド1140が隣り合って設けられている。3つまたは4つのバンドで、二つの構造を形成している。対向する二本のプルバンド1140が、縦方向の強度はほぼ同じであるが、プルバンド1140を横方向に曲げるのに必要な力は低減する。おなじことが3本、または4本のプルバンド1140にも言える。図37は、プルバンド1140の近位端を示す図であり、この近位端は、近位側プルバンドピン1142で内側チューブ1130の遠位端に縦方向に止めつけられている。プルバンド1140と内側チューブ1130の間を強く連結するために、例えば、内側チューブ1130の遠位端とプルバンド1140の間に真鍮製の近位ガイドブロック1150を配置している。
To provide such a connection, the present invention includes at least one
プルバンド1140は、図35に示すように、連接ジョイント1050の全長にわたっており、図38に示すように、遠位ガイドブロック1160に連結されている。遠位ガイドブロック1160(これも、例えば真鍮でできている)は、ステープルカートリッジホルダ1030の近位端の上の少なくとも一の溝に嵌る少なくとも一の突起を有する。以降の図面は、遠位ガイドブロック1160をステープルカートリッジホルダ1030に連結する手段を示しており、最終的に、ステープルカートリッジホルダ1030は、ハンドルに軸方向には固定的に連結されているが、内側チューブ1130に対しては連接できる。図38に示すように、遠位側プルバンドピン1144は、プルバンド1140を遠位ガイドブロック1160に軸方向に係止している。
The
こう合20、30の動きに関する第1の実施例が上述されている。ここでは、ステープルカートリッジ30は軸方向に移動し、台座20は相対的に静止している。図31、及び以下に示すようにエンドステープラ1000の構成では、操作上反対に移動する。
The first embodiment relating to the movement of the
ステープルカートリッジホルダ1030がハンドル1200に対して縦方向に固定されていることを鑑みると、二つのこう合20、30;1020、1030を閉じるアッセンブリがなくてはならない。従って、閉鎖は、以下に述べるように、上側こう合/台座1020の移動によって行われる。
In view of the fact that the
ハンドル1200の2本のレバーのうちの第1のレバー(例えば、近位側ハンドル)は、外側チューブ1110に操作可能に連結されており、第1のレバーが圧縮され/作動すると、外側チューブ1110を遠位側に動かす。クレビス1010、連接ジョイント1050、及びドラムスリーブ1040は、外側チューブ1110に軸方向に固定的に連結されているため(また、外側チューブ1110が内側チューブ1130に沿って縦方向にスライド可能であるため)、第1のレバーの作動で、ドラムスリーブ1040を遠位側に移動させる。
A first lever (eg, proximal handle) of the two levers of handle 1200 is operably coupled to outer tube 1110, and when the first lever is compressed / actuated, outer tube 1110. Move distally. The
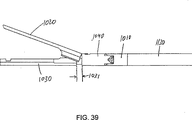
図39は、開状態にある台座1020を示す図である。ここに見られるように、ギャップ1031は、ドラムスリーブ1040の遠位端と、ステープルカートリッジホルダ1030底部の近位シェルフとの間にギャップ1031がある。この方向において、ドラムスリーブ1040、クレビス1010、及び外側チューブ1110は、シェルフからある距離、近位側に配置されている。
FIG. 39 shows the
図40は、閉状態にある台座1020を示す図である。ここに示すように、ドラムスリーブ1040とステープルカートリッジホルダ1030の近位シェルフとの間にはギャップ1031がない。この方向において、ドラムスリーブ1040、クレビス1010、外側チューブ1110は、ドラムスリーブ1040がシェルフと接触する位置にある。
FIG. 40 shows the
ハンドル1200に対するステープルカートリッジホルダ1030の軸方向に固定された位置と反対に、また、ドラムスリーブ1040の移動と同様に、ナイフ60、1060は、縦軸に沿ってハンドル1200に対して移動しなければならない。図35、36、及び38乃至41は、ハンドル1200のナイフ移動構造に対するナイフ1060の軸方向に変位可能な連結を示す。
Opposite to the axially fixed position of the
図35を参照すると、押出ロッド1102がハンドル1200から延在しており、ハンドル1200の第2の図示しないレバー(例えば、遠位側レバー)に連結されている。押出ロッド1102の遠位端は、押出ピン1122を通って少なくとも一のフレキシブルなナイフ刃1062の遠位端に連結されている。このナイフ刃1062の遠位端は、切断刃1060の近位側に連結されており、切断刃1060は、押出ロッドの1102の対応する動きを追って遠位側あるいは近位側に移動する。ナイフ刃1062は、近位側に上方向に延在するフランジ1064を有し、これは、押出ロッドピン1122を受けるボアを収納している。押出ロッド1102とナイフ刃1062との間のこの軸外連結によって遠位方向に押されると、ナイフ刃1062の遠位端に下側に力が加わり、従って、例えば図36及び図42に示すように、押出ロッド刃サポート1070の内側の位置に留まる。
Referring to FIG. 35, a
ナイフ刃1062は十分にフレキシブルであり、連接ジョイント105が曲がるいずれの方向にも曲がる。従って、ナイフ刃1062も、支持されていなければ屈曲するのに十分にフレキシブルである。本発明は、従って、図36及び42に示す押出ロッド−刃サポート1070を提供する。ここで、押出ロッド−刃サポート1070の近位端は、矩形ナイフ刃1062を摺動可能に支持する矩形刃チャネル1072を明らかにしている。また、押出ロッド1102の湾曲した(例えば円筒形)の外面を摺動可能に支持する、湾曲した押出ロッドチャネル1074が示されている。このように、押出ロッド−刃サポート1070は、押出ロッド1102がサポート1070内部にある位置で押出ロッド1102を支持しており、また、ナイフ刃1062がサポート1070内部にある位置で、ナイフ刃1062を支持している。
The
図36は、サポート1070の連結と、近位ガイドブロック1150に対する関係を示す。
FIG. 36 shows the connection of the
プルバンド1140と同様に、一又はそれ以上のナイフブレード1062を並べることができる。このような構成において、複数のブレード1062は同じ縦方向の剛性を有するが、連接ジョイント1050に曲げがある場合にはより大きな可撓性を提供する。
As with the
図41に明らかなものは、こう合1020、1030の連接を係止する連接ロック解除スライド1120である。
What is apparent in FIG. 41 is an articulated
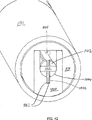
図42乃至50は、エンドステープラ1000の縦軸に直交する面に沿った、ハンドル1200の筒状部分遠位側の縦断面を示す図である。
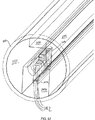
FIGS. 42 to 50 are longitudinal sectional views of the distal end of the cylindrical portion of the handle 1200 taken along a plane orthogonal to the longitudinal axis of the
図42は、ナイフ刃1062と押出ロッドピン1122の連結ジャンクションの断面を示す。押出ロッドピン1122は、2枚の隣接する刃1062と押出ロッド1102の全体を通過するが、押出ロッドの外側面の外へは延在しない。この図面は、内側及び外側チューブ1130、1110及び押出ロッド−刃サポート1070の関係も示している。また、この図から明らかなことは、係止解除スライド1120のロックを解除するのに使用する解除押出ロッド1104である。解除プルロッド1104の縦方向のエキスステントは、まず、図35に示されており、また、図36、37、41、52および53にも示されている。特に、図41は、外側部品は隠されているが、プルロッド1104がどのようにベルアクチュエータ1100を連接係止解除スライド1120に連結しているかを示す。図37に示すように、連接係止解除スライド1120の遠位端を通り、遠位端の回りに巻き付けられているプルロッド1104の遠位端で、解除プルロッド1104は、ベルアクチュエータ1100と連接係止解除スライド1120の間の縦方向の固定的連結を行う。このように、ベルアクチュエータ1100は近位側に移動するときに、連接係止解除スライド1120が対応して近位方向に移動し、連接係止解除スライド1120の遠位側の歯1121とスプロケット1522のスポーク1041を分離する。特に、図46と52を参照されたい。プルロッド1104と連接係止解除スライド1120の間の巻かれている連結は、例示的実施例にすぎない。その他の形状による係止、力による係止連結も同様に可能である。
FIG. 42 shows a cross section of the connecting junction between the
図43は、プルバンド1140と内側チューブ1130によるピンジョイントの連結を示す。上述したとおり、近位側プルバンドピン1142は、刃1062、近位ガイドブロック1150、及び内側チューブ1130を全体的に通過しているが、外側チューブ1110には及ばない。
FIG. 43 shows the connection of the pin joint by the
図44は、連接係止解除スライド1120の近位端のすぐ近位側の領域を示す。この例示的実施例では、プルバンド1140が二本の刃1062の上に配置されている。プルバンド1140と刃1062のうちの少なくとも一方を支持するために、一対のハンモック1066がプルバンド1140と刃1062の連接部分の側部に沿って配置されている。例えば、図50に示すように、各ハンモック1066はU字形状(縦断面に沿って)をしており、各ハンモック1066の近位側アームは、クレビス1010の近位側面を中心に曲がっており、各ハンモック1066の遠位側アームは、ドラムスリーブ1040内のキャッチ面を中心に曲がっている。
FIG. 44 shows the region immediately proximal to the proximal end of the articulating
クレビス1010内部には、2本のスプリングロッド1012が配置されており、この回りに各スプリングロッドカラー1014がある。このカラーは、縦軸に向けて及び縦軸に沿って連接ジョイント1050のアッセンブリ遠位側全体を横方向にバイアスするように機能する。スプリングロッドとカラー1012、1014については、以下に更に詳細に述べる。
Two
図45は、プルロッド1104(この図には示されていない)の曲がった部分を受ける連接係止解除スライド1120の中央の開領域を示す。また、キャビティ1016も示されており、この中に図示しないスプリングロッド1012のバイアスばねが入っている。この断面領域には、二本のナイフ刃1062の上に配置された二本のプルバンド1140の部分が含まれている。
FIG. 45 shows the central open region of the articulating
図46は、スプリングロッド1012がカム面1018に対して作動している開領域を示す。カム面1018は、アーチ形状をしており、スプリングロッド1012とカム面1018間の接触が常に、スプリングロッド1012の最も遠位側の表面に垂直な軸方向に作用する。例えば、図56を参照されたい。このような構成において、遠位側連接アッセンブリ(例えば、台座1020、ステープルカートリッジホルダ1030、ドラムスリーブ1040)を内側及び外側チューブ1130、1110の縦軸に対してバイアスするためにカム面1018に対してスプリングロッド1012によって与えられる力は、常に、連接テープルカートリッジホルダ1030の連接軸を中心に同じ半径にある。このような構成の利点の一つは、どのような場合でもスプリングロッド1012に横方向に力がかからないことであり、この場合、スプリングロッド1012の最も遠位端が、カム面1018をとらえて係止することができる。
FIG. 46 shows the open region where the
図47は、エンドステープラ連接ジョイント1050内の領域を断面で示す。再び、二本のプルバンド1140と、二本の刃1062、及び二つのハンモック1066の一部がこの領域に含まれている。上側及び下側軸パック1152がドラムスリーブ1040の表面上及び下のオリフィス1042内に挿入されている。連接ジョイント1050におけるドラムスリーブ1040に対するクレビス1010の連結は、上部と底部において対称である。パック1152は、ドラムスリーブ1040の近位端の上部と底部において、オリフィス1042に挿入される。この方向において、アッセンブリはクレビス1040の遠位端に挿入され、スクリュ孔1011をパック1152の中央ねじ付きボア1153に整列させる。整列したときに、スクリュ1013がパック1152に螺合して、ドラムスリーブ1040をクレビス1010に軸方向に固定すると共に、ドラムスリーブ1040を二本のスクリュ1013の縦軸によって規定される軸を中心に連接させる。
FIG. 47 shows the area within the end stapler articulating joint 1050 in cross section. Again, two pull
図48は、遠位側プルバンドピンジョイントの領域を示す。この領域では、プルバンド1140の遠位側端部が、遠位側ガイドブロック1160のボア内に配置されている遠位側プルバンドピン1144で固定されている。遠位側ガイドブロック1160は、ステープルカートリッジホルダ1030内に配置されており、上述したようにそこに固定されている。
FIG. 48 shows the region of the distal pull band pin joint. In this region, the distal end of the
図49は、切断刃1060のすぐ近位側の領域を示しており、切断刃1060の近位側オリフィス内の二本のナイフ刃1062の固定した連結を示す。この図も、台座1020を回動させてステープルカートリッジホルダ1030に対して移動させるカム面1032を明確に示している。
FIG. 49 shows the region just proximal of the
図50は、スプリングロッド1012を通る縦断面を示す。この図では、ハンモック1066の縦方向のエクステント全体が見られる。ハンモック1066の遠位側部分は、ハンモック1066の遠位端近傍の垂直軸を中心に連接している。図50では、スプリングロッド1012とハンモック1066の間に実質的にギャップが存在する。ハンモック1066がなければ、薄いナイフ刃1062が曲がって、これらのギャップ内で反ったり、あるいは曲がる可能性がある。ハンモック1066をこれらの間に配置することによって、ナイフ刃1062の許されない曲がりが生じすることを防ぐ。図51は、このような目的で作ったテストベッドにおける、ハンモック1066と刃1062の極端に曲がっているエクステントを示す図である。上側ハンモック1066は、臨界的曲がり領域におけるカーブの内側表面を追従しているので、図51に関して上側の曲がりには用いられていない。対照的に、下側ハンモック1066が、ナイフ刃1062(例示的実施例では二本)がテストベッドのギャップ内へ許されない曲がりが生じることを実質的に防ぐために用いられている。各ハンモック1066は、両側にしっかりと保持されており、実質的に非弾性材料(例えば、ステンレススチール)でできているので、その間に曲がったナイフ刃1062を支持するスリングまたは「ハンモック」を形成する。
FIG. 50 shows a longitudinal section through the
図52は、連接係止解除スライド1120を通る断面を示す図であり、解除プルロッド1104のスライド1120内への遠位側連結曲がりを明確に示している。このような構成では、係止解除プルロッド1104の近位側への変位によって、スライド1120が対応して近位側に変位し、スライド1120の歯1121をドラムスリーブ1040の近位側の対応する歯1041間から解除する。図示しないバイアスデバイスによって、連接係止解除スライド1120に遠位側のバイアスがかかる。このバイアスデバイスは、中空1123内にあり、中空1123の遠位端と、クレビス1010に対して固定されているブロック1124に対して押圧している。
FIG. 52 shows a cross section through the articulated unlocking
図35は、解除プルロッド1104とハンドル1200との間の連結を示す。ロッドプルブロック1105は、プルロッド1104を受けるための縦方向のボア1107を有する。ロッドプルブロック1105は、横方向のボア1109も有しており、ロッドプルブロック1105内にプルロッド1104を固定するために、そこで図示しないスクリュセットを受ける。ベルアクチュエータ1100の内側部分は、ロッドプルブロックと係合し、ベルアクチュエータ1100が近位側に移動すると、ロッドプルブロック1105(例えば、キー孔などの形状嵌合連結など)を近位側に偏位させるような形状をしている。
FIG. 35 shows the connection between the
図53は、遠位端から見たエンドステープラの遠位部分の分解斜視図である。 FIG. 53 is an exploded perspective view of the distal portion of the end stapler as viewed from the distal end.
図34乃至53に示すクレビス1010は、一体型である。代替的に、クレビス1010を、二等分にモールドすることができる。このような場合、パック1152を除いて、代わりに、二等分したクレビスの各部分を形成し、これによって、スクリュ1013を不要とすることができる。なぜなら、外側チューブ1110は、クレビス1010の近位端に取り付けるときに、二等分したものを互いに保持するからである。このような構成が、図54以下のエンドステープラの実施例に記載されている。
The
図54は、端部作動体の第4実施例の内部部品をいくつか示す図である。台座1020は、ステープルカートリッジホルダ1030の反対側に配置されており、閉リング1040は、ステープルカートリッジホルダ1030の近位端を囲んでいる。内側及び外側チューブ1130、1110は除去されており、連接係止解除スライド1120、押出ロッド1102、および押出ロッド刃サポート1070をはっきり見ることができる。スクリーンドア1103が、押出ロッド1102の周囲で、内側及び外側チューブ1130、1110、及びベルアクチュエータ1100の内側に装着されている。ハンドル1200とベルアクチュエータ1100は、明瞭化のための取り除かれている。スクリーンドア1103は、ナイフ/切断刃1060が遠位方向に移動するのみなので、押出ロッド1102の動きを一方向(遠位側)のみに制限している。
FIG. 54 is a diagram showing some internal components of the fourth embodiment of the end effector. The
二等分したクレビスは、図55及び56に最も良く示されている。これらの図面では、外側チューブ1110は除かれており、図54に示す端部作動体の様々な内部構造を示す。図55の分解図において、プルバンド1140のステープルカートリッジホルダ1030への連結が明らかである。図示しないピン(図59も参照されたい)は、ホルダ1030の第1の近位側フランジと、第1のスペーサ1170と、プルバンド1140の遠位側フランジと、第2のスペーサ1170と、ホルダ1030の第2の対向する近位側フランジとを、それぞれ、通っている。図59に示すような閉鎖リング1040は、ピンをここに保持して、これらの部品の縦方向の連結を提供する。
The bisected clevis is best shown in FIGS. In these drawings, the outer tube 1110 has been removed to show the various internal structures of the end effector shown in FIG. In the exploded view of FIG. 55, the connection of
ナイフ/切断刃1060の様々な構造も、図55に明らかである。歯1060は、ナイフ刃1062の遠位端を連結する近位側溝1061を有する。例示的な実施例は、溝1061と遠位端が、キー孔形状の係止を形成している。刃1060の上側ハーフは、上側台座1020の底面内の対応する溝に嵌る外側形状を有する二つの対向するガイドウイング1063を有する。刃1060の下側ハーフも、二つの対向するガイドウイング1065を有する。ホルダ1030は、下側ウイング1065をそこに受けるために、上側表面内に溝を有する。これらの二対のウイング1063、1065によって、刃1060が切断及びステープリング手順中にそこに沿って移動しているときに、台座1020とホルダ1030が確実に、固定した平行位置にある。刃1060の下側ハーフには、近位側に延在するフランジ1067が配置されている。板ばね1090が、リベット1036によってステープルカートリッジホルダ1030に取り付けられている。板ばね1090と、刃1060のその他の特徴を、以下により詳細に記載する。
Various configurations of the knife /
図55及び56は、また、二等分したクレビス2010、2020の様々な部品を示す。図56及び58に見られるように、クレビスの上側ハーフ2010の内側表面は、二つのキャビティ2011を規定しており、これらのキャビティは各々、スプリングロッド1012と、このスプリングロッド1012用の図示しないバイアスデバイスとを収納する。図に示す例示的実施例では、クレビスの上側ハーフ2010が、スプリングロッド1012用のキャビティ2011全体を規定しており、クレビスの下側ハーフ2020は、バイアスデバイスを収容するためだけのキャビティの底部分2021を規定している。これらのクレビスハーフ2010、2020は、ドッグボーンクレビスの二つの部分2030、2040の各々の上の連接ボス2031、2041をそこで受けるための連接ポート2012、2022を規定している。
Figures 55 and 56 also show the various parts of the
図56及び57は、外側チューブ1110内の構造の縦方向の連結を示す。押出ロッド刃サポート1070は、内側チューブ1130の下側チャネル内に配置されている。この押出ロッド刃サポート1070も、狭い近位側ネック1074と比較的広い遠位側ヘッド1075を有する遠位エクステンション1071を有する。クレビスの下側ハーフ2020の底部にある対応する溝2023によって、遠位側エクステンション1071は、クレビスハーフ2020、従って、クレビスの残りのハーフに、縦方向に固定することができる。
56 and 57 show the longitudinal connection of the structure within the outer tube 1110. Extrusion
外側チューブ1110とクレビスの下側ハーフ2020は、スプリングロッドキャビティ2011内のスプリングロッド1012の構造を示すために、図56では取り除かれている。再び、スプリングロッドバイアスデバイス(例えば、コイルスプリング)は、明瞭にするために、キャビティ2011には示されていない。様々な部品を取り除いて、プルバンド1140の連接エクステントが図56に明確に示されている。クレビスの上側ハーフ2010内部のプルバンド1140用支持面は、図58の断平面に見ることができる。上側ドッグボーンクレビス2030は、二つの対向する支持面2032を有し、この面は各々が、非連接プルバンド1140の中央線に対して同じ鋭角をなしている。同様に、クレビスの上側ハーフ2010は、二つの対向する面2013を有し、これらの面も、各々、非連接プルバンド1140の中央線に対して鋭角を成している。
The outer tube 1110 and the
図55及び58に、クレビスの下側ハーフ2020の内側に向かう方向の反対側の図を示す。ナイフ刃1062用連接部が、下側ドッグボーンクレビス2040内部のドッグボーン1080用支持面2042、及びクレビスの下側ハーフ2010内部のドッグボーン1080用支持面2024と共に示されている。また、この方向においては、ドッグボーンガイド1080用ガイド面及び支持面を見ることができる。図57では、下側ドッグボーンクレビスが、キドニー形状の遠位側ドッグボーン凹部2043を有し、クレビスの下側ハーフ2010がキドニー形状の近位側ドッグボーン凹部2025を有することわかる。これらの凹部2025、2043及び面2024、2042は、図66にも示されており、以下に詳細に説明する。図59、62及び66に更に見られる特徴は、左右の面1082を有するドッグボーンガイド1080の内側通路であり、これを以下に更に詳細に説明する。
55 and 58 show views on the opposite side of the clevis
ドッグボーンガイド1080の遠位端が、図59の縦断面図に示されている。遠位側ドッグボーン凹部2043は、ドッグボーンガイド1080の遠位端を収納しており、非連接時には、ドッグボーンガイド1080が下側ドッグボーンクレビス2040の支持面2042に接触しない。
The distal end of the
ドッグボーンガイド1080の遠位端用近位側ハウジングが図60に示されている。近位側ドッグボーン凹部2025の構造をより明らかにするために、ドッグボーンガイド1080をこれらの構造から取り除いている。
A proximal housing for the distal end of the
凹部2025、2043の両方が、ここに配置されたドッグボーンガイド1080の下側延在部を共に、図57の水平方向の、縦断面に示されている。ここには、押出ロッド刃サポート1070、切断刃1060、及びステープルスレッド102(取り外し可能なステープルカートリッジ100の一部である)の下側構造が示されている。これらの構造を、図61及び62に拡大して示す。
Both
図63、64および65は、ナイフ刃1060閉鎖構造を示す図である。換言すると、ステープルカートリッジ100がないとき、あるいはすでに発射されたステープルカートリッジがステープルカートリッジホルダ1030内にあるときに、ナイフ刃1060が前進しないようにする安全装置である。理解を容易にするために、この図に示されているステープルカートリッジ100の部分のみが、ステープルスレッド102である。
63, 64 and 65 are views showing a
ナイフ刃1060は、ステープルスレッド102が発射用意位置にあるとき、すなわち、スレッド102が図65に示す位置にあるときにのみ、遠位側に移動できるようにするべきである。スレッド102がこの位置にないときは、二つの事態を意味する。すなわち、ホルダ1030内にステープルカートリッジ100がないか、あるいはスレッド102がすでに遠位側に移動している、換言すると、ロード済みステープルカートリッジ100によって部分的あるいは完全な発射がすでに成されたという事態である。従って、スレッド102には、閉塞接触面104が設けられており、刃1060には、対応する形状の接触ノーズ1069が設けられている。この時点において、下側ガイドウイング1065は、刃1060が遠位側にエッジ1035をすぎて移動するまでカートリッジホルダ1030内のフロア1034に乗らない。このような構成によって、スレッド102が刃1060の遠位端になく、ノーズ1069をたたかない場合、下側ガイドウイング1065がエッジ1035のすぐ近位側の凹部1037を追跡し、フロア1034の上に進む代わりに、エッジ1035をたたいて刃1060が更に前側に移動することを止める。スレッド102が存在しないときにこのような接触を補助するために、ステープルカートリッジ1030は、板ばね1090を有する(リベット1036によって取り付けられている)。上向きに固定されており、フランジ1067を下向きに押圧している板ばね1090(少なくとも、フランジ1067が板ばね1090の遠位端の遠位側にくるまで)によって、下向きの力が刃1060にかかり、ウイング1065を凹部1037に押し下げる。このように、スレッド102が存在することなく刃1060が遠位側に進むと、ウイング1065を凹部1037の下側カーブを追跡して、ウイング1065の遠位エッジがエッジ1035に当たるときに、止まってこれ以上遠位側に移動しないようにする。図63は、例えば、遠位エッジ1035と二つの立ち上がりボス1038を示す。このボスは、エッジ1035の高さに延在して、スレッド102が内場合にウイング1065がエッジ1035を超えて押されることがないようにする。
The
図66は、クレビスの下側ハーフ2020と下側ドッグボーンクレビス2040内のドッグボーン1080の例示的な動きを示す図である。図66の完全に左側に曲がった位置では、ドッグボーン1080の遠位側底部突出部が、遠位側ドッグボーン凹部2043内の回転位置にあり、近位側底部突出部が、近位側ドッグボーン凹部2025内の回転位置にある。重要なことは、ドッグボーン1080の左側垂直面が、左側ドッグボーン支持面2024、2042の上でほぼ完全に支持されていることである。凹部2025、2043の形状、及びドッグボーン1080の底部突出部は、ドッグボーン1080の伸張あるいは圧縮がなく、端に、端部作動体の連接が生じるときに左から右へ揺れ動くように選択される。
FIG. 66 is a diagram illustrating exemplary movement of the
三本の並んだナイフ刃1062が、クレビスの下側ハーフ2020、2040の左側のアーチ状位置内において、図66に図示されている。左側に曲がると、ナイフ刃1062がドッグボーン1080の右側内側面1082に押しつけられる。従って、内側面1082は、端部作動体が曲がるであろうエクステントに応じた形状をしている。本発明の特徴を画のに制限があるため、刃1062は、ほぼカーブした方向に概略的に示されているだけである。
Three side-by-
ナイフ刃1062のいくつかの特徴をよりよく理解するために、押出ロッド1102と押出ロッド刃サポート1070との近位側連結の拡大図が図67に示されている。同軸に整列したナイフ刃1062と押出ロッド1102を有する構造を想像することが可能であるが、例えば図41、67に示すオフセット連結が用いられる。上述したとおり、ナイフ刃1062の長さが、ナイフ刃1062が、押出ロッド刃サポート1070内で刃チャンネル1072へ完全に押し下げることが好ましいものにする。図41は、刃1062をチャネル1072にバイアスするオフセット連結の第1の実施例を示す。図67は、このオフセット連結の第2の実施例を示す。この第2の実施例では、刃1062が、第1の実施例(横方向押出ピン1122で連結されている)のように押出ロッド1102に固定的に連結されていない。代わりに、押出ロッド1102にチャンバ1108が形成されており、この中に刃1062の近位端が挿入される。チャンバ1108を、刃1062を軸方向に縦に保持する(例えば、横方向オフセット)形状に形成することによって、固定的な連結が不要になる。この実施例では、チャンバ1108が縦断面においてほぼL字形状であり、このような横方向のオフセットを提供しているが、様々な異なる形状であっても良い。
To better understand some features of the
プルバンド1140の遠位側連結が図59に特によく示されている。このような構成では、左右のアーチが、二つ、三つ、四つ、あるいはそれ以上の隣接するプルバンド1140の各々を曲げる。各プルバンド1140は固定長を有しており、またプルバンド1140が側部に沿って互いに積み重なっているので、所定の方向のアーチが、差はわずかであるにしても、各プルバンド1140を異なる方向に曲げる。このような曲がりの差を補償するための、遠位側連結の代替の実施例が、図68乃至70に示されている。明瞭化と、簡単にするために、これらの図面には上側ドッグボーンクレビス2030の一部のみを略図で示す。
The distal connection of the
この代替の実施例では、第1の実施例のスペーサ1170を置き換えている。ここでは、5本のプルバンド1140が側部に並べて配置されている。上側ドッグボーンクレビス2030が、内側ボア2033(例えば円形ボア)を規定しており、この中に、ボア2033の内側形状に対応する外側形状を有するピストン2050が挿入される。ボア2033は、近位側窓2034を具えており、これを通ってプルバンド1140がボア2033内に突出している。窓2034は、プルバンド1140の全幅とほぼ同じ幅(わずかにこれより大きいが)を有する。
In this alternative embodiment, the
ピストン2050は、横方向ボアを有し、この中に、近位側プルバンドピン2060が螺合している。このピンはピストン2050と、及び各プルバンド1140の遠位側プルバンドボア1145と螺合するときに、軸として機能する。図70を参照されたい。ピストン2050の内部2051は、重なったプルバンド1140の幅に対応する形状を有していない。代わりに、プルバンド1140の遠位端を受ける内側開口が、ウイング付きの水平方向断面形状を有する。
端部作動体が連接するときに、プルバンド1140の遠位端が曲がってカーブになる。プルバンド1140などの隣接する平行プレートが共に曲がって、外側プレートが、中央あるいは内側プレートと異なる方向に移動する。この不均質な動きは、ウイング付開口2051と、楕円形状の遠位側プルバンドボア1145によって補償される。端部作動体が連接すると、プルバンド1140にかかる曲げ力が、上側ドッグボーンクレビス2030のボア2033内でピストン2050を回動させる。端部作動体が連接するほど、ピストン2050が、完全な連接が外側プルバンド1140をウイング付開口2051の内側面に対して押圧するまで、更に回動する。この時点で、各プルバンド1140の近位端は整列するが、図68ないし70に示す遠位端は整列しない。卵形開口1145の存在によって、プルバンド1140は互いに対して若干移動することができる。
When the end effectors are articulated, the distal end of the
上述した説明及び図面は、本発明の原理、好ましい実施例、及び操作モードを示すものである。しかしながら、本発明は、上述した特定の実施例に限定されると介すべきではない。上述の実施例の更なる変形例は、当業者には自明である。 The foregoing description and drawings illustrate the principles, preferred embodiments, and modes of operation of the present invention. However, the invention should not be construed as limited to the specific embodiments described above. Further variations of the above-described embodiments will be apparent to those skilled in the art.
従って、上述の実施例は、限定ではなく、例示であると考えるべきである。従って、当業者が特許請求の範囲によって規定される本発明の範囲から外れることなくこれらの実施例の変形例を作ることができることは自明である。 Accordingly, the above embodiments should be considered as illustrative rather than limiting. Thus, it will be apparent to one skilled in the art that modifications may be made to these embodiments without departing from the scope of the invention as defined by the appended claims.
本発明の実施例の利点は、本発明の好ましい実施例の以下の詳細な説明から明らかである。この説明は、添付の図面と共に考慮すべきである。
Claims (18)
ステープリングアクチュエータと;
前記ステープリングアクチュエータと異なり、非作動状態と作動状態を有する連接ジョイントアクチュエータと;
前記ステープリングアクチュエータと前記連接ジョイントアクチュエータを収納し、遠位端を有する第1の縦軸を画定する本体と;
を具える制御ハンドルと;
台座と;
近位端と;
第2の縦軸と;
少なくとも一のステープルを有するステープラカートリッジと;
前記ステープリングアクチュエータと、前記台座と、前記ステープラカートリッジに動作可能に連結しており、前記ステープリングアクチュエータが作動するときに少なくとも一のステープルをステープリングする台座カートリッジ制御デバイスと;を具える外科用ステープリング端部作動体と;
前記ステープリング端部作動体を前記制御ハンドルに連結し、連接軸を中心に連接する受動的連接ジョイントと;
前記受動的連接ジョイントを介して、前記受動的連接ジョイントの連接に対応する態様で撓む前記ステープリングアクチュエータの一部と;を具え、
前記連接ジョイントアクチュエータが:
前記非作動状態にあるときに、前記受動的連接ジョイントと、これによって、前記端部作動体を実質的に固定された連接位置に保持し;
前記作動状態にあるときに、前記受動的連接ジョイントを自在に連接する状態に解放して、前記端部作動体に作用する外力に応じて前記端部作動体を自在に連接させ;
前記本体の遠位端と前記端部作動体の前記近位端のうちの一方の第1の部分に配置され、当該第1の部分が一対のプランジャキャビティを画定するセンタリング装置と;
前記本体の遠位端と前記端部作動体の前記近位端のうちの他方の第2の部分に配置され、前記センタリング装置が一対の予負荷バネバイアスプランジャであって、各々が前記プランジャキャビティに配置され、前記プランジャを前記第2の部分の方向へ当該部分に対してバイアスして、前記連接ジョイントアクチュエータが前記作動状態にある時に前記第1及び第2の縦軸を実質的に整列させる整合面とを具えることを特徴とする、医療デバイス。In medical devices;
A stapling actuator;
An articulated joint actuator having a non-actuated state and an actuated state, unlike the stapling actuator;
A body that houses the stapling actuator and the articulating joint actuator and that defines a first longitudinal axis having a distal end;
A control handle comprising:
With pedestal;
The proximal end;
A second vertical axis;
A stapler cartridge having at least one staple;
Surgical comprising: the stapling actuator; the pedestal; and a pedestal cartridge control device operatively coupled to the stapler cartridge and stapling at least one staple when the stapling actuator is activated. A stapling end actuating body;
A passive articulation joint coupling the stapling end actuating body to the control handle and articulating about a articulation axis;
A portion of the stapling actuator that bends via the passive articulation joint in a manner corresponding to the articulation of the passive articulation joint;
The articulated joint actuator is:
Holding the passive articulation joint and thereby the end effector in a substantially fixed articulated position when in the inoperative state;
When in the actuated state, the passive articulation joint is released into a freely articulated state, and the end effector is freely articulated in response to an external force acting on the end effector;
A centering device disposed at a first portion of one of the distal end of the body and the proximal end of the end effector, the first portion defining a pair of plunger cavities;
Disposed at a second portion of the other of the distal end of the body and the proximal end of the end effector, wherein the centering device is a pair of preloaded spring biased plungers, each being a plunger cavity And biasing the plunger in the direction of the second portion relative to the portion to substantially align the first and second longitudinal axes when the articulated joint actuator is in the activated state. A medical device comprising an alignment surface.
前記制御ハンドルの前記ステープリングアクチュエータが:
作動時に、前記台座と前記ステープリングカートリッジを閉じるステープラ閉鎖アクチュエータと;
作動時に、少なくとも一のステープルをステープリングし、前記切断デバイスで切断するステープル発射アクチュエータと;
を具え:
前記ステープラ閉鎖アクチュエータと前記ステープル発射アクチュエータが前記連接ジョイントアクチュエータと異なることを特徴とする医療デバイス。The medical device of claim 1, wherein the surgical stapling end effector comprises a bladed cutting device;
The stapling actuator of the control handle is:
A stapler closing actuator for closing the pedestal and the stapling cartridge in operation;
A staple firing actuator that, in operation, staples at least one staple and cuts with the cutting device;
With:
The medical device, wherein the stapler closing actuator and the staple firing actuator are different from the articulated joint actuator.
前記連接ジョイントアクチュエータが遠位側を向いた歯を有するプルロックを具え;
前記ステープリング端部作動体が:
前記連接ジョイントアクチュエータが非作動状態にあるときに、前記遠位側を向いた歯に相互係合して;
前記連接ジョイントアクチュエータが前記作動状態にあるときに、遠位側を向いた歯からの係合が解除されて、これによって、前記受動的連接ジョイントを前記自在な連接状態に解放する;近位側を向いた歯を有するギアを具えることを特徴とする医療デバイス。In the medical device of claim 1:
The articulating joint actuator comprises a pull lock having teeth facing distally;
The stapling end effector is:
When the articulating joint actuator is in an inoperative state, interengaging with the distally facing teeth;
When the articulated joint actuator is in the actuated state, the engagement from the teeth facing distally is released, thereby releasing the passive articulated joint to the free articulated state; A medical device comprising a gear having teeth facing toward it.
ステープリングアクチュエータと;
前記ステープリングアクチュエータと異なり、非作動状態と作動状態を有する連接ジョイントアクチュエータと;
前記ステープリングアクチュエータと前記連接ジョイントアクチュエータを収納し、遠位端を有する第1の縦軸を画定する本体と;
を具える制御ハンドルと;
台座と;
近位端と;
第2の縦軸と;
少なくとも一のステープルを有するステープラカートリッジと;
前記ステープリングアクチュエータと、前記台座と、前記ステープラカートリッジに動作可能に連結しており、前記ステープリングアクチュエータが作動するときに少なくとも一のステープルをステープリングする台座カートリッジ制御デバイスと、
連接ロックと、
を具える外科用ステープリング端部作動体と;
前記ステープリング端部作動体を前記制御ハンドルに連結し、連接軸を中心に連接する受動的連接ジョイントと;
前記受動的連接ジョイントを通り、前記受動的連接ジョイントの連接に対応する態様で撓む前記ステープリングアクチュエータの一部と;を具え、
前記連接ジョイントアクチュエータが:
前記非作動状態にあるときに、前記連接係止に連結されて、これによって、前記端部作動体を適所に保持する前記受動的連接ジョイントを所定の連接位置に係止して;
前記作動状態にあるときに、前記連接係止からの連結を解除して、これによって、前記端部作動体に作用する外力に応じて自在に連接させる前記受動的連接ジョイントを連接的に解放し;
前記本体の遠位端と前記端部作動体の前記近位端のうちの一方の第1の部分に配置され、当該第1の部分が一対のプランジャキャビティを画定するセンタリング装置と;
前記本体の遠位端と前記端部作動体の前記近位端のうちの他方の第2の部分に配置され、前記センタリング装置が一対の予負荷バネバイアスプランジャであって、各々が前記プランジャキャビティに配置され、前記プランジャを前記第2の部分の方向へ当該部分に対してバイアスして、前記連接ジョイントアクチュエータが前記作動状態にある時に前記第1及び第2の縦軸を実質的に整列させる整合面とを具えることを特徴とする、医療デバイス。In medical devices:
A stapling actuator;
An articulated joint actuator having a non-actuated state and an actuated state, unlike the stapling actuator;
A body that houses the stapling actuator and the articulating joint actuator and that defines a first longitudinal axis having a distal end;
A control handle comprising:
With pedestal;
The proximal end;
A second vertical axis;
A stapler cartridge having at least one staple;
A pedestal cartridge control device operatively coupled to the stapling actuator, the pedestal, and the stapler cartridge for stapling at least one staple when the stapling actuator is activated;
Articulated locks,
A surgical stapling end actuator comprising:
A passive articulation joint coupling the stapling end actuating body to the control handle and articulating about a articulation axis;
A portion of the stapling actuator that passes through the passive articulation joint and flexes in a manner corresponding to the articulation of the passive articulation joint;
The articulated joint actuator is:
When in the non-actuated state, coupled to the articulation lock, thereby locking the passive articulation joint holding the end effector in place;
When in the actuated state, the connection from the articulation lock is released, thereby disengaging the passive articulation joint that is freely articulated according to the external force acting on the end effector. ;
A centering device disposed at a first portion of one of the distal end of the body and the proximal end of the end effector, the first portion defining a pair of plunger cavities;
Disposed at a second portion of the other of the distal end of the body and the proximal end of the end effector, wherein the centering device is a pair of preloaded spring biased plungers, each being a plunger cavity And biasing the plunger in the direction of the second portion relative to the portion to substantially align the first and second longitudinal axes when the articulated joint actuator is in the activated state. A medical device comprising an alignment surface.
前記制御ハンドルの前記ステープリングアクチュエータが:
作動時に、前記台座と前記ステープリングカートリッジを閉じるステープラ閉鎖アクチュエータと;
作動時に、少なくとも一のステープルをステープリングし、前記切断デバイスで切断するステープル発射アクチュエータと;
を具え:
前記ステープラ閉鎖アクチュエータと前記ステープル発射アクチュエータが前記連接ジョイントアクチュエータと異なることを特徴とする医療デバイス。The medical device of claim 9, wherein the surgical stapling end effector comprises a bladed cutting device;
The stapling actuator of the control handle is:
A stapler closing actuator for closing the pedestal and the stapling cartridge in operation;
A staple firing actuator that, in operation, staples at least one staple and cuts with the cutting device;
With:
The medical device, wherein the stapler closing actuator and the staple firing actuator are different from the articulated joint actuator.
前記連接ジョイントアクチュエータが遠位側を向いた歯付プルロックを有しており、
前記連接係止が:
前記連接ジョイントアクチュエータが前記非作動状態にあるときに前記遠位側を向いた歯と相互に係合し;
前記連接ジョイントが前記作動状態にあるときに、前記遠位側を向いた歯からの係合が解除されて、これによって前記受動的連接ジョイントを解放して、外力に応じて自在に連接する;
近位側を向いた歯のついたギアを有していることを特徴とする医療デバイス。The medical device according to claim 9, wherein
The articulating joint actuator has a toothed pull lock facing distally;
The articulated lock is:
Interacting with the distally facing teeth when the articulating joint actuator is in the inoperative state;
When the articulating joint is in the activated state, the disengagement from the distally facing teeth is released, thereby releasing the passive articulating joint and freely articulating in response to external forces;
A medical device comprising a gear with teeth facing proximally.
ステープリングアクチュエータと;
前記ステープリングアクチュエータと異なり、前記連接ジョイントアクチュエータが静止している非作動状態と、前記連接ジョイントアクチュエータが近位方向に移動する作動状態を有するプルツーリリースおよびリリースツーリロック連接ジョイントアクチュエータと;
前記ステープリングアクチュエータと前記連接ジョイントアクチュエータを収納し、遠位端を有する第1の縦軸を画定する本体と;
を具える制御ハンドルと;
台座と;
近位端と;
第2の縦軸と;
少なくとも一のステープルを有するステープラカートリッジと;
前記ステープリングアクチュエータと、前記台座と、前記ステープラカートリッジに動作可能に連結しており、前記ステープリングアクチュエータが作動するときに少なくとも一のステープルをステープリングする台座カートリッジ制御デバイスと、
連接係止と、
を具える外科用ステープリング端部作動体と;
前記ステープリング端部作動体を前記制御ハンドルに連接し、連接軸を中心に前記ステープリング端部作動体を連接する受動的連接ジョイント;
前記受動的連接ジョイントを通り、前記受動的連接ジョイントの連接に対応する態様で撓む前記ステープリングアクチュエータの一部と;を具え、
前記連接ジョイントアクチュエータが:
前記非連接状態で静止しているときに、前記連接ロックに連結されて、これによって、前記受動的連接ジョイントを前記端部作動体を適所に保持する所定の連接位置に係止し;
前記連接状態で近位側に移動するときに、前記連接係止からの連結を解除して、これによって、前記受動的連接ジョイントを前記端部作動体にかかる外力に応じて自在に連接させるように連接的に解放し;
前記本体の遠位端と前記端部作動体の前記近位端のうちの一方の第1の部分に配置され、当該第1の部分が一対のプランジャキャビティを画定するセンタリング装置と;
前記本体の遠位端と前記端部作動体の前記近位端のうちの他方の第2の部分に配置され、前記センタリング装置が一対の予負荷バネバイアスプランジャであって、各々が前記プランジャキャビティに配置され、前記プランジャを前記第2の部分の方向へ当該部分に対してバイアスして、前記連接ジョイントアクチュエータが前記作動状態にある時に前記第1及び第2の縦軸を実質的に整列させる整合面とを具えることを特徴とする、医療デバイス。In medical devices:
A stapling actuator;
Unlike the stapling actuator, a pull-to-release and release-to-relock articulated joint actuator having an inoperative state in which the articulated joint actuator is stationary and an actuated state in which the articulated joint actuator moves proximally;
A body that houses the stapling actuator and the articulating joint actuator and that defines a first longitudinal axis having a distal end;
A control handle comprising:
With pedestal;
The proximal end;
A second vertical axis;
A stapler cartridge having at least one staple;
A pedestal cartridge control device operatively coupled to the stapling actuator, the pedestal, and the stapler cartridge for stapling at least one staple when the stapling actuator is activated;
Articulated locking;
A surgical stapling end actuator comprising:
A passive articulation joint that articulates the stapling end effector to the control handle and articulates the stapling end effector about a articulation axis;
A portion of the stapling actuator that passes through the passive articulation joint and flexes in a manner corresponding to the articulation of the passive articulation joint;
The articulated joint actuator is:
Coupled to the articulation lock when stationary in the non-articulated state, thereby locking the passive articulation joint in a predetermined articulation position that holds the end effector in place;
When moving to the proximal side in the connected state, the connection from the connection lock is released, so that the passive connection joint is freely connected according to the external force applied to the end effector. Release articulated;
A centering device disposed at a first portion of one of the distal end of the body and the proximal end of the end effector, the first portion defining a pair of plunger cavities;
Disposed at a second portion of the other of the distal end of the body and the proximal end of the end effector, wherein the centering device is a pair of preloaded spring biased plungers, each being a plunger cavity And biasing the plunger in the direction of the second portion relative to the portion to substantially align the first and second longitudinal axes when the articulated joint actuator is in the activated state. A medical device comprising an alignment surface.
ステープリングアクチュエータと;
前記ステープリングアクチュエータと別に、係止状態と非係止状態を有する連接の係止を解除する手段と;
前記ステープリングアクチュエータと前記連接の係止を解除する手段を収納し、遠位端を有する第1の縦軸を画定する本体と;
を具える制御ハンドルと:
台座と;
近位端と;
第2の縦軸と;
少なくとも一のステープルを有するステープラカートリッジと;
前記ステープリングアクチュエータと、前記台座と、前記ステープラカートリッジに動作可能に連結しており、前記ステープリングアクチュエータが作動するときに少なくとも一のステープルをステープリングする台座カートリッジ制御デバイスと、
を具える外科用ステープリング端部作動体と;
前記制御ハンドルに対して前記ステープリング端部作動体を受動的に連接する手段と;
前記受動的連接ジョイントを通り、前記受動的連接ジョイントの連接に対応する態様で撓む前記ステープリングアクチュエータの一部と;を具え、
前記連接の係止を解除する手段が:
前記係止状態にあるときに、前記端部作動体を実質的に固定した連接位置に保持し;
前記非係止状態にあるときに、前記端部作動体に作用する外力に応じて前記端部作動体を解放して自在に連接させる;
前記本体の遠位端と前記端部作動体の前記近位端のうちの一方の第1の部分に配置され、当該第1の部分が一対のプランジャキャビティを画定するセンタリング装置と;
前記本体の遠位端と前記端部作動体の前記近位端のうちの他方の第2の部分に配置され、前記センタリング装置が一対の予負荷バネバイアスプランジャであって、各々が前記プランジャキャビティに配置され、前記プランジャを前記第2の部分の方向へ当該部分に対してバイアスして、前記連接ジョイントアクチュエータが前記作動状態にある時に前記第1及び第2の縦軸を実質的に整列させる整合面とを具えることを特徴とする、医療デバイス。In medical devices:
A stapling actuator;
Apart from the stapling actuator, means for releasing the interlocking of the connection having the locked state and the unlocked state;
A body containing a means for unlocking the stapling actuator and the articulation and defining a first longitudinal axis having a distal end;
Control handle with:
With pedestal;
The proximal end;
A second vertical axis;
A stapler cartridge having at least one staple;
A pedestal cartridge control device operatively coupled to the stapling actuator, the pedestal, and the stapler cartridge for stapling at least one staple when the stapling actuator is activated;
A surgical stapling end actuator comprising:
Means for passively connecting the stapling end effector to the control handle;
A portion of the stapling actuator that passes through the passive articulation joint and flexes in a manner corresponding to the articulation of the passive articulation joint;
Means for unlocking the linkage is:
Holding the end effector in a substantially fixed articulated position when in the locked state;
When in the unlocked state, the end effector is released and freely connected in accordance with an external force acting on the end effector;
A centering device disposed at a first portion of one of the distal end of the body and the proximal end of the end effector, the first portion defining a pair of plunger cavities;
Disposed at a second portion of the other of the distal end of the body and the proximal end of the end effector, wherein the centering device is a pair of preloaded spring biased plungers, each being a plunger cavity And biasing the plunger in the direction of the second portion relative to the portion to substantially align the first and second longitudinal axes when the articulated joint actuator is in the activated state. A medical device comprising an alignment surface.
Applications Claiming Priority (7)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US70264305P | 2005-07-26 | 2005-07-26 | |
| US60/702,643 | 2005-07-26 | ||
| US76000006P | 2006-01-18 | 2006-01-18 | |
| US60/760,000 | 2006-01-18 | ||
| US81195006P | 2006-06-08 | 2006-06-08 | |
| US60/811,950 | 2006-06-08 | ||
| PCT/US2006/028752 WO2007016060A2 (en) | 2005-07-26 | 2006-07-25 | Surgical stapling and cutting device and method for using the device |
Related Child Applications (2)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| JP2008257807A Division JP4611410B2 (en) | 2005-07-26 | 2008-10-02 | Surgical stapling and cutting device and method of using the device |
| JP2009118008A Division JP5020995B2 (en) | 2005-07-26 | 2009-05-14 | Surgical stapling and cutting device and method of using the device |
Publications (2)
| Publication Number | Publication Date |
|---|---|
| JP2009507526A JP2009507526A (en) | 2009-02-26 |
| JP4336386B2 true JP4336386B2 (en) | 2009-09-30 |
Family
ID=39167223
Family Applications (12)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| JP2008524042A Active JP4336386B2 (en) | 2005-07-26 | 2006-07-25 | Surgical stapling and cutting device and method of using the device |
| JP2008257807A Active JP4611410B2 (en) | 2005-07-26 | 2008-10-02 | Surgical stapling and cutting device and method of using the device |
| JP2009118008A Active JP5020995B2 (en) | 2005-07-26 | 2009-05-14 | Surgical stapling and cutting device and method of using the device |
| JP2011111900A Active JP5623980B2 (en) | 2005-07-26 | 2011-05-18 | Surgical stapling and cutting device and method of using the device |
| JP2011111899A Active JP5686373B2 (en) | 2005-07-26 | 2011-05-18 | Surgical stapling and cutting device and method of using the device |
| JP2013120535A Active JP5889834B2 (en) | 2005-07-26 | 2013-06-07 | Surgical stapling and cutting device and method of using the device |
| JP2015168464A Active JP5969670B2 (en) | 2005-07-26 | 2015-08-28 | Surgical stapling and cutting device and method of using the device |
| JP2016051247A Active JP6622120B2 (en) | 2005-07-26 | 2016-03-15 | Surgical stapling and cutting device and method of using the device |
| JP2017019295A Active JP6298185B2 (en) | 2005-07-26 | 2017-02-06 | Surgical stapling and cutting device and method of using the device |
| JP2017156785A Active JP7001389B2 (en) | 2005-07-26 | 2017-08-15 | Surgical stapling and cutting device and how to use this device |
| JP2018198534A Active JP7090528B2 (en) | 2005-07-26 | 2018-10-22 | Surgical stapling and cutting device and how to use this device |
| JP2020081760A Active JP7130697B2 (en) | 2005-07-26 | 2020-05-07 | Surgical stapling and cutting device and method of using this device |
Family Applications After (11)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| JP2008257807A Active JP4611410B2 (en) | 2005-07-26 | 2008-10-02 | Surgical stapling and cutting device and method of using the device |
| JP2009118008A Active JP5020995B2 (en) | 2005-07-26 | 2009-05-14 | Surgical stapling and cutting device and method of using the device |
| JP2011111900A Active JP5623980B2 (en) | 2005-07-26 | 2011-05-18 | Surgical stapling and cutting device and method of using the device |
| JP2011111899A Active JP5686373B2 (en) | 2005-07-26 | 2011-05-18 | Surgical stapling and cutting device and method of using the device |
| JP2013120535A Active JP5889834B2 (en) | 2005-07-26 | 2013-06-07 | Surgical stapling and cutting device and method of using the device |
| JP2015168464A Active JP5969670B2 (en) | 2005-07-26 | 2015-08-28 | Surgical stapling and cutting device and method of using the device |
| JP2016051247A Active JP6622120B2 (en) | 2005-07-26 | 2016-03-15 | Surgical stapling and cutting device and method of using the device |
| JP2017019295A Active JP6298185B2 (en) | 2005-07-26 | 2017-02-06 | Surgical stapling and cutting device and method of using the device |
| JP2017156785A Active JP7001389B2 (en) | 2005-07-26 | 2017-08-15 | Surgical stapling and cutting device and how to use this device |
| JP2018198534A Active JP7090528B2 (en) | 2005-07-26 | 2018-10-22 | Surgical stapling and cutting device and how to use this device |
| JP2020081760A Active JP7130697B2 (en) | 2005-07-26 | 2020-05-07 | Surgical stapling and cutting device and method of using this device |
Country Status (1)
| Country | Link |
|---|---|
| JP (12) | JP4336386B2 (en) |
Families Citing this family (477)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US20070084897A1 (en) | 2003-05-20 | 2007-04-19 | Shelton Frederick E Iv | Articulating surgical stapling instrument incorporating a two-piece e-beam firing mechanism |
| US9060770B2 (en) | 2003-05-20 | 2015-06-23 | Ethicon Endo-Surgery, Inc. | Robotically-driven surgical instrument with E-beam driver |
| US8215531B2 (en) | 2004-07-28 | 2012-07-10 | Ethicon Endo-Surgery, Inc. | Surgical stapling instrument having a medical substance dispenser |
| US11896225B2 (en) | 2004-07-28 | 2024-02-13 | Cilag Gmbh International | Staple cartridge comprising a pan |
| US20070194079A1 (en) | 2005-08-31 | 2007-08-23 | Hueil Joseph C | Surgical stapling device with staple drivers of different height |
| US7669746B2 (en) | 2005-08-31 | 2010-03-02 | Ethicon Endo-Surgery, Inc. | Staple cartridges for forming staples having differing formed staple heights |
| US11246590B2 (en) | 2005-08-31 | 2022-02-15 | Cilag Gmbh International | Staple cartridge including staple drivers having different unfired heights |
| US9237891B2 (en) | 2005-08-31 | 2016-01-19 | Ethicon Endo-Surgery, Inc. | Robotically-controlled surgical stapling devices that produce formed staples having different lengths |
| US11484312B2 (en) | 2005-08-31 | 2022-11-01 | Cilag Gmbh International | Staple cartridge comprising a staple driver arrangement |
| US10159482B2 (en) | 2005-08-31 | 2018-12-25 | Ethicon Llc | Fastener cartridge assembly comprising a fixed anvil and different staple heights |
| US7934630B2 (en) | 2005-08-31 | 2011-05-03 | Ethicon Endo-Surgery, Inc. | Staple cartridges for forming staples having differing formed staple heights |
| US20070106317A1 (en) | 2005-11-09 | 2007-05-10 | Shelton Frederick E Iv | Hydraulically and electrically actuated articulation joints for surgical instruments |
| US8820603B2 (en) | 2006-01-31 | 2014-09-02 | Ethicon Endo-Surgery, Inc. | Accessing data stored in a memory of a surgical instrument |
| US20110006101A1 (en) | 2009-02-06 | 2011-01-13 | EthiconEndo-Surgery, Inc. | Motor driven surgical fastener device with cutting member lockout arrangements |
| US7845537B2 (en) | 2006-01-31 | 2010-12-07 | Ethicon Endo-Surgery, Inc. | Surgical instrument having recording capabilities |
| US8708213B2 (en) | 2006-01-31 | 2014-04-29 | Ethicon Endo-Surgery, Inc. | Surgical instrument having a feedback system |
| US11224427B2 (en) | 2006-01-31 | 2022-01-18 | Cilag Gmbh International | Surgical stapling system including a console and retraction assembly |
| US9861359B2 (en) | 2006-01-31 | 2018-01-09 | Ethicon Llc | Powered surgical instruments with firing system lockout arrangements |
| US11793518B2 (en) | 2006-01-31 | 2023-10-24 | Cilag Gmbh International | Powered surgical instruments with firing system lockout arrangements |
| US11278279B2 (en) | 2006-01-31 | 2022-03-22 | Cilag Gmbh International | Surgical instrument assembly |
| US8186555B2 (en) | 2006-01-31 | 2012-05-29 | Ethicon Endo-Surgery, Inc. | Motor-driven surgical cutting and fastening instrument with mechanical closure system |
| US20110024477A1 (en) | 2009-02-06 | 2011-02-03 | Hall Steven G | Driven Surgical Stapler Improvements |
| US20110290856A1 (en) | 2006-01-31 | 2011-12-01 | Ethicon Endo-Surgery, Inc. | Robotically-controlled surgical instrument with force-feedback capabilities |
| US20120292367A1 (en) | 2006-01-31 | 2012-11-22 | Ethicon Endo-Surgery, Inc. | Robotically-controlled end effector |
| US7753904B2 (en) | 2006-01-31 | 2010-07-13 | Ethicon Endo-Surgery, Inc. | Endoscopic surgical instrument with a handle that can articulate with respect to the shaft |
| US8992422B2 (en) | 2006-03-23 | 2015-03-31 | Ethicon Endo-Surgery, Inc. | Robotically-controlled endoscopic accessory channel |
| US8236010B2 (en) | 2006-03-23 | 2012-08-07 | Ethicon Endo-Surgery, Inc. | Surgical fastener and cutter with mimicking end effector |
| US8322455B2 (en) | 2006-06-27 | 2012-12-04 | Ethicon Endo-Surgery, Inc. | Manually driven surgical cutting and fastening instrument |
| US10568652B2 (en) | 2006-09-29 | 2020-02-25 | Ethicon Llc | Surgical staples having attached drivers of different heights and stapling instruments for deploying the same |
| US10130359B2 (en) | 2006-09-29 | 2018-11-20 | Ethicon Llc | Method for forming a staple |
| US7506791B2 (en) | 2006-09-29 | 2009-03-24 | Ethicon Endo-Surgery, Inc. | Surgical stapling instrument with mechanical mechanism for limiting maximum tissue compression |
| US8652120B2 (en) | 2007-01-10 | 2014-02-18 | Ethicon Endo-Surgery, Inc. | Surgical instrument with wireless communication between control unit and sensor transponders |
| US8684253B2 (en) | 2007-01-10 | 2014-04-01 | Ethicon Endo-Surgery, Inc. | Surgical instrument with wireless communication between a control unit of a robotic system and remote sensor |
| US11291441B2 (en) | 2007-01-10 | 2022-04-05 | Cilag Gmbh International | Surgical instrument with wireless communication between control unit and remote sensor |
| US8701958B2 (en) | 2007-01-11 | 2014-04-22 | Ethicon Endo-Surgery, Inc. | Curved end effector for a surgical stapling device |
| US11039836B2 (en) | 2007-01-11 | 2021-06-22 | Cilag Gmbh International | Staple cartridge for use with a surgical stapling instrument |
| US20090001130A1 (en) | 2007-03-15 | 2009-01-01 | Hess Christopher J | Surgical procedure using a cutting and stapling instrument having releasable staple-forming pockets |
| US8893946B2 (en) | 2007-03-28 | 2014-11-25 | Ethicon Endo-Surgery, Inc. | Laparoscopic tissue thickness and clamp load measuring devices |
| US8931682B2 (en) | 2007-06-04 | 2015-01-13 | Ethicon Endo-Surgery, Inc. | Robotically-controlled shaft based rotary drive systems for surgical instruments |
| US11857181B2 (en) | 2007-06-04 | 2024-01-02 | Cilag Gmbh International | Robotically-controlled shaft based rotary drive systems for surgical instruments |
| US7588176B2 (en) * | 2007-06-18 | 2009-09-15 | Ethicon Endo-Surgery, Inc. | Surgical cutting instrument with improved closure system |
| US7753245B2 (en) | 2007-06-22 | 2010-07-13 | Ethicon Endo-Surgery, Inc. | Surgical stapling instruments |
| US8408439B2 (en) * | 2007-06-22 | 2013-04-02 | Ethicon Endo-Surgery, Inc. | Surgical stapling instrument with an articulatable end effector |
| US11849941B2 (en) | 2007-06-29 | 2023-12-26 | Cilag Gmbh International | Staple cartridge having staple cavities extending at a transverse angle relative to a longitudinal cartridge axis |
| US7905381B2 (en) | 2008-09-19 | 2011-03-15 | Ethicon Endo-Surgery, Inc. | Surgical stapling instrument with cutting member arrangement |
| US8561870B2 (en) | 2008-02-13 | 2013-10-22 | Ethicon Endo-Surgery, Inc. | Surgical stapling instrument |
| US9179912B2 (en) | 2008-02-14 | 2015-11-10 | Ethicon Endo-Surgery, Inc. | Robotically-controlled motorized surgical cutting and fastening instrument |
| US8573465B2 (en) | 2008-02-14 | 2013-11-05 | Ethicon Endo-Surgery, Inc. | Robotically-controlled surgical end effector system with rotary actuated closure systems |
| US7819298B2 (en) | 2008-02-14 | 2010-10-26 | Ethicon Endo-Surgery, Inc. | Surgical stapling apparatus with control features operable with one hand |
| US8636736B2 (en) | 2008-02-14 | 2014-01-28 | Ethicon Endo-Surgery, Inc. | Motorized surgical cutting and fastening instrument |
| US7866527B2 (en) | 2008-02-14 | 2011-01-11 | Ethicon Endo-Surgery, Inc. | Surgical stapling apparatus with interlockable firing system |
| BRPI0901282A2 (en) | 2008-02-14 | 2009-11-17 | Ethicon Endo Surgery Inc | surgical cutting and fixation instrument with rf electrodes |
| US8758391B2 (en) | 2008-02-14 | 2014-06-24 | Ethicon Endo-Surgery, Inc. | Interchangeable tools for surgical instruments |
| US8657174B2 (en) | 2008-02-14 | 2014-02-25 | Ethicon Endo-Surgery, Inc. | Motorized surgical cutting and fastening instrument having handle based power source |
| US11272927B2 (en) | 2008-02-15 | 2022-03-15 | Cilag Gmbh International | Layer arrangements for surgical staple cartridges |
| US9615826B2 (en) | 2010-09-30 | 2017-04-11 | Ethicon Endo-Surgery, Llc | Multiple thickness implantable layers for surgical stapling devices |
| US20090206131A1 (en) | 2008-02-15 | 2009-08-20 | Ethicon Endo-Surgery, Inc. | End effector coupling arrangements for a surgical cutting and stapling instrument |
| PL3476312T3 (en) | 2008-09-19 | 2024-03-11 | Ethicon Llc | Surgical stapler with apparatus for adjusting staple height |
| US11648005B2 (en) | 2008-09-23 | 2023-05-16 | Cilag Gmbh International | Robotically-controlled motorized surgical instrument with an end effector |
| US8210411B2 (en) | 2008-09-23 | 2012-07-03 | Ethicon Endo-Surgery, Inc. | Motor-driven surgical cutting instrument |
| US9005230B2 (en) | 2008-09-23 | 2015-04-14 | Ethicon Endo-Surgery, Inc. | Motorized surgical instrument |
| US9386983B2 (en) | 2008-09-23 | 2016-07-12 | Ethicon Endo-Surgery, Llc | Robotically-controlled motorized surgical instrument |
| US8608045B2 (en) | 2008-10-10 | 2013-12-17 | Ethicon Endo-Sugery, Inc. | Powered surgical cutting and stapling apparatus with manually retractable firing system |
| US8517239B2 (en) | 2009-02-05 | 2013-08-27 | Ethicon Endo-Surgery, Inc. | Surgical stapling instrument comprising a magnetic element driver |
| US8444036B2 (en) | 2009-02-06 | 2013-05-21 | Ethicon Endo-Surgery, Inc. | Motor driven surgical fastener device with mechanisms for adjusting a tissue gap within the end effector |
| EP2393430A1 (en) | 2009-02-06 | 2011-12-14 | Ethicon Endo-Surgery, Inc. | Driven surgical stapler improvements |
| US8220688B2 (en) | 2009-12-24 | 2012-07-17 | Ethicon Endo-Surgery, Inc. | Motor-driven surgical cutting instrument with electric actuator directional control assembly |
| US8851354B2 (en) | 2009-12-24 | 2014-10-07 | Ethicon Endo-Surgery, Inc. | Surgical cutting instrument that analyzes tissue thickness |
| US8608046B2 (en) | 2010-01-07 | 2013-12-17 | Ethicon Endo-Surgery, Inc. | Test device for a surgical tool |
| WO2011111271A1 (en) | 2010-03-11 | 2011-09-15 | オリンパスメディカルシステムズ株式会社 | Forceps suitable for intraperitoneal manipulations and technique of using forceps suitable for intraperitoneal manipulations |
| US8783543B2 (en) | 2010-07-30 | 2014-07-22 | Ethicon Endo-Surgery, Inc. | Tissue acquisition arrangements and methods for surgical stapling devices |
| US8360296B2 (en) | 2010-09-09 | 2013-01-29 | Ethicon Endo-Surgery, Inc. | Surgical stapling head assembly with firing lockout for a surgical stapler |
| US9289212B2 (en) | 2010-09-17 | 2016-03-22 | Ethicon Endo-Surgery, Inc. | Surgical instruments and batteries for surgical instruments |
| US8632525B2 (en) | 2010-09-17 | 2014-01-21 | Ethicon Endo-Surgery, Inc. | Power control arrangements for surgical instruments and batteries |
| US8733613B2 (en) | 2010-09-29 | 2014-05-27 | Ethicon Endo-Surgery, Inc. | Staple cartridge |
| US9332974B2 (en) | 2010-09-30 | 2016-05-10 | Ethicon Endo-Surgery, Llc | Layered tissue thickness compensator |
| US9307989B2 (en) | 2012-03-28 | 2016-04-12 | Ethicon Endo-Surgery, Llc | Tissue stapler having a thickness compensator incorportating a hydrophobic agent |
| US9386988B2 (en) | 2010-09-30 | 2016-07-12 | Ethicon End-Surgery, LLC | Retainer assembly including a tissue thickness compensator |
| US9314246B2 (en) | 2010-09-30 | 2016-04-19 | Ethicon Endo-Surgery, Llc | Tissue stapler having a thickness compensator incorporating an anti-inflammatory agent |
| US10945731B2 (en) | 2010-09-30 | 2021-03-16 | Ethicon Llc | Tissue thickness compensator comprising controlled release and expansion |
| US11812965B2 (en) | 2010-09-30 | 2023-11-14 | Cilag Gmbh International | Layer of material for a surgical end effector |
| US20120080336A1 (en) | 2010-09-30 | 2012-04-05 | Ethicon Endo-Surgery, Inc. | Staple cartridge comprising staples positioned within a compressible portion thereof |
| US9277919B2 (en) | 2010-09-30 | 2016-03-08 | Ethicon Endo-Surgery, Llc | Tissue thickness compensator comprising fibers to produce a resilient load |
| US9364233B2 (en) | 2010-09-30 | 2016-06-14 | Ethicon Endo-Surgery, Llc | Tissue thickness compensators for circular surgical staplers |
| US11298125B2 (en) | 2010-09-30 | 2022-04-12 | Cilag Gmbh International | Tissue stapler having a thickness compensator |
| EP2621356B1 (en) | 2010-09-30 | 2018-03-07 | Ethicon LLC | Fastener system comprising a retention matrix and an alignment matrix |
| US10405854B2 (en) | 2010-09-30 | 2019-09-10 | Ethicon Llc | Surgical stapling cartridge with layer retention features |
| US9629814B2 (en) | 2010-09-30 | 2017-04-25 | Ethicon Endo-Surgery, Llc | Tissue thickness compensator configured to redistribute compressive forces |
| US11925354B2 (en) | 2010-09-30 | 2024-03-12 | Cilag Gmbh International | Staple cartridge comprising staples positioned within a compressible portion thereof |
| US9301753B2 (en) | 2010-09-30 | 2016-04-05 | Ethicon Endo-Surgery, Llc | Expandable tissue thickness compensator |
| US9211120B2 (en) | 2011-04-29 | 2015-12-15 | Ethicon Endo-Surgery, Inc. | Tissue thickness compensator comprising a plurality of medicaments |
| US9220501B2 (en) | 2010-09-30 | 2015-12-29 | Ethicon Endo-Surgery, Inc. | Tissue thickness compensators |
| US9517063B2 (en) | 2012-03-28 | 2016-12-13 | Ethicon Endo-Surgery, Llc | Movable member for use with a tissue thickness compensator |
| US8695866B2 (en) | 2010-10-01 | 2014-04-15 | Ethicon Endo-Surgery, Inc. | Surgical instrument having a power control circuit |
| US9089330B2 (en) | 2011-03-14 | 2015-07-28 | Ethicon Endo-Surgery, Inc. | Surgical bowel retractor devices |
| CA2834649C (en) | 2011-04-29 | 2021-02-16 | Ethicon Endo-Surgery, Inc. | Staple cartridge comprising staples positioned within a compressible portion thereof |
| US11207064B2 (en) | 2011-05-27 | 2021-12-28 | Cilag Gmbh International | Automated end effector component reloading system for use with a robotic system |
| US9072535B2 (en) | 2011-05-27 | 2015-07-07 | Ethicon Endo-Surgery, Inc. | Surgical stapling instruments with rotatable staple deployment arrangements |
| US9050084B2 (en) | 2011-09-23 | 2015-06-09 | Ethicon Endo-Surgery, Inc. | Staple cartridge including collapsible deck arrangement |
| US9044230B2 (en) | 2012-02-13 | 2015-06-02 | Ethicon Endo-Surgery, Inc. | Surgical cutting and fastening instrument with apparatus for determining cartridge and firing motion status |
| MX350846B (en) | 2012-03-28 | 2017-09-22 | Ethicon Endo Surgery Inc | Tissue thickness compensator comprising capsules defining a low pressure environment. |
| RU2644272C2 (en) | 2012-03-28 | 2018-02-08 | Этикон Эндо-Серджери, Инк. | Limitation node with tissue thickness compensator |
| CN104321024B (en) | 2012-03-28 | 2017-05-24 | 伊西康内外科公司 | Tissue thickness compensator comprising a plurality of layers |
| US9101358B2 (en) | 2012-06-15 | 2015-08-11 | Ethicon Endo-Surgery, Inc. | Articulatable surgical instrument comprising a firing drive |
| US9649111B2 (en) | 2012-06-28 | 2017-05-16 | Ethicon Endo-Surgery, Llc | Replaceable clip cartridge for a clip applier |
| RU2636861C2 (en) | 2012-06-28 | 2017-11-28 | Этикон Эндо-Серджери, Инк. | Blocking of empty cassette with clips |
| US20140001231A1 (en) | 2012-06-28 | 2014-01-02 | Ethicon Endo-Surgery, Inc. | Firing system lockout arrangements for surgical instruments |
| BR112014032776B1 (en) | 2012-06-28 | 2021-09-08 | Ethicon Endo-Surgery, Inc | SURGICAL INSTRUMENT SYSTEM AND SURGICAL KIT FOR USE WITH A SURGICAL INSTRUMENT SYSTEM |
| US11278284B2 (en) | 2012-06-28 | 2022-03-22 | Cilag Gmbh International | Rotary drive arrangements for surgical instruments |
| US9226751B2 (en) | 2012-06-28 | 2016-01-05 | Ethicon Endo-Surgery, Inc. | Surgical instrument system including replaceable end effectors |
| US9289256B2 (en) | 2012-06-28 | 2016-03-22 | Ethicon Endo-Surgery, Llc | Surgical end effectors having angled tissue-contacting surfaces |
| US9204879B2 (en) | 2012-06-28 | 2015-12-08 | Ethicon Endo-Surgery, Inc. | Flexible drive member |
| KR101379964B1 (en) | 2012-09-12 | 2014-04-01 | 가톨릭대학교 산학협력단 | Forceps for partial turbinectomy |
| US9386985B2 (en) | 2012-10-15 | 2016-07-12 | Ethicon Endo-Surgery, Llc | Surgical cutting instrument |
| US9386984B2 (en) | 2013-02-08 | 2016-07-12 | Ethicon Endo-Surgery, Llc | Staple cartridge comprising a releasable cover |
| US9421003B2 (en) | 2013-02-18 | 2016-08-23 | Covidien Lp | Apparatus for endoscopic procedures |
| US9216013B2 (en) | 2013-02-18 | 2015-12-22 | Covidien Lp | Apparatus for endoscopic procedures |
| BR112015021098B1 (en) | 2013-03-01 | 2022-02-15 | Ethicon Endo-Surgery, Inc | COVERAGE FOR A JOINT JOINT AND SURGICAL INSTRUMENT |
| RU2669463C2 (en) | 2013-03-01 | 2018-10-11 | Этикон Эндо-Серджери, Инк. | Surgical instrument with soft stop |
| US20140246475A1 (en) | 2013-03-01 | 2014-09-04 | Ethicon Endo-Surgery, Inc. | Control methods for surgical instruments with removable implement portions |
| US20140263552A1 (en) | 2013-03-13 | 2014-09-18 | Ethicon Endo-Surgery, Inc. | Staple cartridge tissue thickness sensor system |
| US9332987B2 (en) | 2013-03-14 | 2016-05-10 | Ethicon Endo-Surgery, Llc | Control arrangements for a drive member of a surgical instrument |
| US9629629B2 (en) | 2013-03-14 | 2017-04-25 | Ethicon Endo-Surgey, LLC | Control systems for surgical instruments |
| US9332984B2 (en) | 2013-03-27 | 2016-05-10 | Ethicon Endo-Surgery, Llc | Fastener cartridge assemblies |
| US9795384B2 (en) | 2013-03-27 | 2017-10-24 | Ethicon Llc | Fastener cartridge comprising a tissue thickness compensator and a gap setting element |
| US9572577B2 (en) | 2013-03-27 | 2017-02-21 | Ethicon Endo-Surgery, Llc | Fastener cartridge comprising a tissue thickness compensator including openings therein |
| US9826976B2 (en) | 2013-04-16 | 2017-11-28 | Ethicon Llc | Motor driven surgical instruments with lockable dual drive shafts |
| BR112015026109B1 (en) | 2013-04-16 | 2022-02-22 | Ethicon Endo-Surgery, Inc | surgical instrument |
| US9574644B2 (en) | 2013-05-30 | 2017-02-21 | Ethicon Endo-Surgery, Llc | Power module for use with a surgical instrument |
| US9924942B2 (en) | 2013-08-23 | 2018-03-27 | Ethicon Llc | Motor-powered articulatable surgical instruments |
| MX369362B (en) | 2013-08-23 | 2019-11-06 | Ethicon Endo Surgery Llc | Firing member retraction devices for powered surgical instruments. |
| US9839428B2 (en) | 2013-12-23 | 2017-12-12 | Ethicon Llc | Surgical cutting and stapling instruments with independent jaw control features |
| US9687232B2 (en) | 2013-12-23 | 2017-06-27 | Ethicon Llc | Surgical staples |
| US20150173756A1 (en) | 2013-12-23 | 2015-06-25 | Ethicon Endo-Surgery, Inc. | Surgical cutting and stapling methods |
| US9724092B2 (en) | 2013-12-23 | 2017-08-08 | Ethicon Llc | Modular surgical instruments |
| US9642620B2 (en) | 2013-12-23 | 2017-05-09 | Ethicon Endo-Surgery, Llc | Surgical cutting and stapling instruments with articulatable end effectors |
| US9681870B2 (en) * | 2013-12-23 | 2017-06-20 | Ethicon Llc | Articulatable surgical instruments with separate and distinct closing and firing systems |
| US9962161B2 (en) | 2014-02-12 | 2018-05-08 | Ethicon Llc | Deliverable surgical instrument |
| US9693777B2 (en) | 2014-02-24 | 2017-07-04 | Ethicon Llc | Implantable layers comprising a pressed region |
| BR112016019387B1 (en) | 2014-02-24 | 2022-11-29 | Ethicon Endo-Surgery, Llc | SURGICAL INSTRUMENT SYSTEM AND FASTENER CARTRIDGE FOR USE WITH A SURGICAL FIXING INSTRUMENT |
| US9913642B2 (en) | 2014-03-26 | 2018-03-13 | Ethicon Llc | Surgical instrument comprising a sensor system |
| US10004497B2 (en) | 2014-03-26 | 2018-06-26 | Ethicon Llc | Interface systems for use with surgical instruments |
| US20150272580A1 (en) | 2014-03-26 | 2015-10-01 | Ethicon Endo-Surgery, Inc. | Verification of number of battery exchanges/procedure count |
| BR112016021943B1 (en) | 2014-03-26 | 2022-06-14 | Ethicon Endo-Surgery, Llc | SURGICAL INSTRUMENT FOR USE BY AN OPERATOR IN A SURGICAL PROCEDURE |
| US9804618B2 (en) | 2014-03-26 | 2017-10-31 | Ethicon Llc | Systems and methods for controlling a segmented circuit |
| JP6636452B2 (en) | 2014-04-16 | 2020-01-29 | エシコン エルエルシーEthicon LLC | Fastener cartridge including extension having different configurations |
| US20150297225A1 (en) | 2014-04-16 | 2015-10-22 | Ethicon Endo-Surgery, Inc. | Fastener cartridges including extensions having different configurations |
| US10561422B2 (en) | 2014-04-16 | 2020-02-18 | Ethicon Llc | Fastener cartridge comprising deployable tissue engaging members |
| CN106456159B (en) | 2014-04-16 | 2019-03-08 | 伊西康内外科有限责任公司 | Fastener cartridge assembly and nail retainer lid arragement construction |
| US10206677B2 (en) | 2014-09-26 | 2019-02-19 | Ethicon Llc | Surgical staple and driver arrangements for staple cartridges |
| CN106456158B (en) | 2014-04-16 | 2019-02-05 | 伊西康内外科有限责任公司 | Fastener cartridge including non-uniform fastener |
| US10045781B2 (en) | 2014-06-13 | 2018-08-14 | Ethicon Llc | Closure lockout systems for surgical instruments |
| US9999423B2 (en) * | 2014-06-25 | 2018-06-19 | Ethicon Llc | Translatable articulation joint unlocking feature for surgical stapler |
| US10314577B2 (en) * | 2014-06-25 | 2019-06-11 | Ethicon Llc | Lockout engagement features for surgical stapler |
| US9693774B2 (en) | 2014-06-25 | 2017-07-04 | Ethicon Llc | Pivotable articulation joint unlocking feature for surgical stapler |
| BR112017004361B1 (en) | 2014-09-05 | 2023-04-11 | Ethicon Llc | ELECTRONIC SYSTEM FOR A SURGICAL INSTRUMENT |
| US10016199B2 (en) | 2014-09-05 | 2018-07-10 | Ethicon Llc | Polarity of hall magnet to identify cartridge type |
| US11311294B2 (en) | 2014-09-05 | 2022-04-26 | Cilag Gmbh International | Powered medical device including measurement of closure state of jaws |
| US10105142B2 (en) | 2014-09-18 | 2018-10-23 | Ethicon Llc | Surgical stapler with plurality of cutting elements |
| US11523821B2 (en) | 2014-09-26 | 2022-12-13 | Cilag Gmbh International | Method for creating a flexible staple line |
| JP6648119B2 (en) | 2014-09-26 | 2020-02-14 | エシコン エルエルシーEthicon LLC | Surgical stapling buttress and accessory materials |
| US10076325B2 (en) | 2014-10-13 | 2018-09-18 | Ethicon Llc | Surgical stapling apparatus comprising a tissue stop |
| US9924944B2 (en) | 2014-10-16 | 2018-03-27 | Ethicon Llc | Staple cartridge comprising an adjunct material |
| US10517594B2 (en) | 2014-10-29 | 2019-12-31 | Ethicon Llc | Cartridge assemblies for surgical staplers |
| US11141153B2 (en) | 2014-10-29 | 2021-10-12 | Cilag Gmbh International | Staple cartridges comprising driver arrangements |
| US9844376B2 (en) | 2014-11-06 | 2017-12-19 | Ethicon Llc | Staple cartridge comprising a releasable adjunct material |
| US10736636B2 (en) | 2014-12-10 | 2020-08-11 | Ethicon Llc | Articulatable surgical instrument system |
| US9844374B2 (en) | 2014-12-18 | 2017-12-19 | Ethicon Llc | Surgical instrument systems comprising an articulatable end effector and means for adjusting the firing stroke of a firing member |
| US9987000B2 (en) | 2014-12-18 | 2018-06-05 | Ethicon Llc | Surgical instrument assembly comprising a flexible articulation system |
| US9844375B2 (en) | 2014-12-18 | 2017-12-19 | Ethicon Llc | Drive arrangements for articulatable surgical instruments |
| US10188385B2 (en) | 2014-12-18 | 2019-01-29 | Ethicon Llc | Surgical instrument system comprising lockable systems |
| MX2017008108A (en) | 2014-12-18 | 2018-03-06 | Ethicon Llc | Surgical instrument with an anvil that is selectively movable about a discrete non-movable axis relative to a staple cartridge. |
| US10117649B2 (en) | 2014-12-18 | 2018-11-06 | Ethicon Llc | Surgical instrument assembly comprising a lockable articulation system |
| US9968355B2 (en) | 2014-12-18 | 2018-05-15 | Ethicon Llc | Surgical instruments with articulatable end effectors and improved firing beam support arrangements |
| US10085748B2 (en) | 2014-12-18 | 2018-10-02 | Ethicon Llc | Locking arrangements for detachable shaft assemblies with articulatable surgical end effectors |
| CN104434250B (en) * | 2014-12-30 | 2017-01-18 | 苏州天臣国际医疗科技有限公司 | Reload unit and medical stapler using same |
| US11154301B2 (en) | 2015-02-27 | 2021-10-26 | Cilag Gmbh International | Modular stapling assembly |
| US10045779B2 (en) | 2015-02-27 | 2018-08-14 | Ethicon Llc | Surgical instrument system comprising an inspection station |
| US10180463B2 (en) | 2015-02-27 | 2019-01-15 | Ethicon Llc | Surgical apparatus configured to assess whether a performance parameter of the surgical apparatus is within an acceptable performance band |
| US9993258B2 (en) | 2015-02-27 | 2018-06-12 | Ethicon Llc | Adaptable surgical instrument handle |
| US9895148B2 (en) | 2015-03-06 | 2018-02-20 | Ethicon Endo-Surgery, Llc | Monitoring speed control and precision incrementing of motor for powered surgical instruments |
| US10245033B2 (en) | 2015-03-06 | 2019-04-02 | Ethicon Llc | Surgical instrument comprising a lockable battery housing |
| US9808246B2 (en) | 2015-03-06 | 2017-11-07 | Ethicon Endo-Surgery, Llc | Method of operating a powered surgical instrument |
| JP2020121162A (en) | 2015-03-06 | 2020-08-13 | エシコン エルエルシーEthicon LLC | Time dependent evaluation of sensor data to determine stability element, creep element and viscoelastic element of measurement |
| US10687806B2 (en) | 2015-03-06 | 2020-06-23 | Ethicon Llc | Adaptive tissue compression techniques to adjust closure rates for multiple tissue types |
| US10617412B2 (en) | 2015-03-06 | 2020-04-14 | Ethicon Llc | System for detecting the mis-insertion of a staple cartridge into a surgical stapler |
| US10045776B2 (en) | 2015-03-06 | 2018-08-14 | Ethicon Llc | Control techniques and sub-processor contained within modular shaft with select control processing from handle |
| US9924961B2 (en) | 2015-03-06 | 2018-03-27 | Ethicon Endo-Surgery, Llc | Interactive feedback system for powered surgical instruments |
| US10441279B2 (en) | 2015-03-06 | 2019-10-15 | Ethicon Llc | Multiple level thresholds to modify operation of powered surgical instruments |
| US9901342B2 (en) | 2015-03-06 | 2018-02-27 | Ethicon Endo-Surgery, Llc | Signal and power communication system positioned on a rotatable shaft |
| US9993248B2 (en) | 2015-03-06 | 2018-06-12 | Ethicon Endo-Surgery, Llc | Smart sensors with local signal processing |
| US10052044B2 (en) | 2015-03-06 | 2018-08-21 | Ethicon Llc | Time dependent evaluation of sensor data to determine stability, creep, and viscoelastic elements of measures |
| US10213201B2 (en) | 2015-03-31 | 2019-02-26 | Ethicon Llc | Stapling end effector configured to compensate for an uneven gap between a first jaw and a second jaw |
| US10178992B2 (en) | 2015-06-18 | 2019-01-15 | Ethicon Llc | Push/pull articulation drive systems for articulatable surgical instruments |
| BR112017027289B1 (en) * | 2015-06-18 | 2022-10-18 | Ethicon Llc | SURGICAL INSTRUMENT |
| KR20240027156A (en) * | 2015-08-06 | 2024-02-29 | 어플라이드 메디컬 리소시스 코포레이션 | Surgical stapler having locking articulation joint |
| US10835249B2 (en) | 2015-08-17 | 2020-11-17 | Ethicon Llc | Implantable layers for a surgical instrument |
| JP6828018B2 (en) | 2015-08-26 | 2021-02-10 | エシコン エルエルシーEthicon LLC | Surgical staple strips that allow you to change the characteristics of staples and facilitate filling into cartridges |
| US10433845B2 (en) | 2015-08-26 | 2019-10-08 | Ethicon Llc | Surgical staple strips for permitting varying staple properties and enabling easy cartridge loading |
| US10172973B2 (en) * | 2015-08-31 | 2019-01-08 | Ethicon Llc | Surgical adjuncts and medicants for promoting lung function |
| US10194936B2 (en) * | 2015-08-31 | 2019-02-05 | Ethicon Endo-Surgery, Llc | Adjunct material for delivery to stomach tissue |
| US10357252B2 (en) | 2015-09-02 | 2019-07-23 | Ethicon Llc | Surgical staple configurations with camming surfaces located between portions supporting surgical staples |
| MX2022006192A (en) | 2015-09-02 | 2022-06-16 | Ethicon Llc | Surgical staple configurations with camming surfaces located between portions supporting surgical staples. |
| US10085751B2 (en) | 2015-09-23 | 2018-10-02 | Ethicon Llc | Surgical stapler having temperature-based motor control |
| US10076326B2 (en) | 2015-09-23 | 2018-09-18 | Ethicon Llc | Surgical stapler having current mirror-based motor control |
| US10327769B2 (en) | 2015-09-23 | 2019-06-25 | Ethicon Llc | Surgical stapler having motor control based on a drive system component |
| US10105139B2 (en) | 2015-09-23 | 2018-10-23 | Ethicon Llc | Surgical stapler having downstream current-based motor control |
| US10363036B2 (en) | 2015-09-23 | 2019-07-30 | Ethicon Llc | Surgical stapler having force-based motor control |
| US10238386B2 (en) | 2015-09-23 | 2019-03-26 | Ethicon Llc | Surgical stapler having motor control based on an electrical parameter related to a motor current |
| US10299878B2 (en) | 2015-09-25 | 2019-05-28 | Ethicon Llc | Implantable adjunct systems for determining adjunct skew |
| US10980539B2 (en) | 2015-09-30 | 2021-04-20 | Ethicon Llc | Implantable adjunct comprising bonded layers |
| US10271849B2 (en) | 2015-09-30 | 2019-04-30 | Ethicon Llc | Woven constructs with interlocked standing fibers |
| US11690623B2 (en) | 2015-09-30 | 2023-07-04 | Cilag Gmbh International | Method for applying an implantable layer to a fastener cartridge |
| US11890015B2 (en) | 2015-09-30 | 2024-02-06 | Cilag Gmbh International | Compressible adjunct with crossing spacer fibers |
| US10265068B2 (en) | 2015-12-30 | 2019-04-23 | Ethicon Llc | Surgical instruments with separable motors and motor control circuits |
| US10292704B2 (en) | 2015-12-30 | 2019-05-21 | Ethicon Llc | Mechanisms for compensating for battery pack failure in powered surgical instruments |
| US10368865B2 (en) | 2015-12-30 | 2019-08-06 | Ethicon Llc | Mechanisms for compensating for drivetrain failure in powered surgical instruments |
| US11213293B2 (en) | 2016-02-09 | 2022-01-04 | Cilag Gmbh International | Articulatable surgical instruments with single articulation link arrangements |
| CN108882932B (en) | 2016-02-09 | 2021-07-23 | 伊西康有限责任公司 | Surgical instrument with asymmetric articulation configuration |
| US10245029B2 (en) | 2016-02-09 | 2019-04-02 | Ethicon Llc | Surgical instrument with articulating and axially translatable end effector |
| US10448948B2 (en) | 2016-02-12 | 2019-10-22 | Ethicon Llc | Mechanisms for compensating for drivetrain failure in powered surgical instruments |
| US11224426B2 (en) | 2016-02-12 | 2022-01-18 | Cilag Gmbh International | Mechanisms for compensating for drivetrain failure in powered surgical instruments |
| US10258331B2 (en) | 2016-02-12 | 2019-04-16 | Ethicon Llc | Mechanisms for compensating for drivetrain failure in powered surgical instruments |
| US10617413B2 (en) | 2016-04-01 | 2020-04-14 | Ethicon Llc | Closure system arrangements for surgical cutting and stapling devices with separate and distinct firing shafts |
| US11284890B2 (en) | 2016-04-01 | 2022-03-29 | Cilag Gmbh International | Circular stapling system comprising an incisable tissue support |
| US10376263B2 (en) | 2016-04-01 | 2019-08-13 | Ethicon Llc | Anvil modification members for surgical staplers |
| US20170281186A1 (en) | 2016-04-01 | 2017-10-05 | Ethicon Endo-Surgery, Llc | Surgical stapling system comprising a contourable shaft |
| US10531874B2 (en) | 2016-04-01 | 2020-01-14 | Ethicon Llc | Surgical cutting and stapling end effector with anvil concentric drive member |
| US10492783B2 (en) | 2016-04-15 | 2019-12-03 | Ethicon, Llc | Surgical instrument with improved stop/start control during a firing motion |
| US10357247B2 (en) | 2016-04-15 | 2019-07-23 | Ethicon Llc | Surgical instrument with multiple program responses during a firing motion |
| US10335145B2 (en) | 2016-04-15 | 2019-07-02 | Ethicon Llc | Modular surgical instrument with configurable operating mode |
| US11607239B2 (en) | 2016-04-15 | 2023-03-21 | Cilag Gmbh International | Systems and methods for controlling a surgical stapling and cutting instrument |
| US11179150B2 (en) | 2016-04-15 | 2021-11-23 | Cilag Gmbh International | Systems and methods for controlling a surgical stapling and cutting instrument |
| US10828028B2 (en) | 2016-04-15 | 2020-11-10 | Ethicon Llc | Surgical instrument with multiple program responses during a firing motion |
| US10405859B2 (en) | 2016-04-15 | 2019-09-10 | Ethicon Llc | Surgical instrument with adjustable stop/start control during a firing motion |
| US10426467B2 (en) | 2016-04-15 | 2019-10-01 | Ethicon Llc | Surgical instrument with detection sensors |
| US10456137B2 (en) | 2016-04-15 | 2019-10-29 | Ethicon Llc | Staple formation detection mechanisms |
| US11317917B2 (en) | 2016-04-18 | 2022-05-03 | Cilag Gmbh International | Surgical stapling system comprising a lockable firing assembly |
| US20170296173A1 (en) | 2016-04-18 | 2017-10-19 | Ethicon Endo-Surgery, Llc | Method for operating a surgical instrument |
| US10363037B2 (en) | 2016-04-18 | 2019-07-30 | Ethicon Llc | Surgical instrument system comprising a magnetic lockout |
| USD826405S1 (en) | 2016-06-24 | 2018-08-21 | Ethicon Llc | Surgical fastener |
| CN109310431B (en) | 2016-06-24 | 2022-03-04 | 伊西康有限责任公司 | Staple cartridge comprising wire staples and punch staples |
| USD850617S1 (en) | 2016-06-24 | 2019-06-04 | Ethicon Llc | Surgical fastener cartridge |
| US10702270B2 (en) | 2016-06-24 | 2020-07-07 | Ethicon Llc | Stapling system for use with wire staples and stamped staples |
| USD847989S1 (en) | 2016-06-24 | 2019-05-07 | Ethicon Llc | Surgical fastener cartridge |
| WO2018060411A1 (en) * | 2016-09-30 | 2018-04-05 | Koninklijke Philips N.V. | Control handle for steerable medical devices |
| US11134942B2 (en) | 2016-12-21 | 2021-10-05 | Cilag Gmbh International | Surgical stapling instruments and staple-forming anvils |
| US10675025B2 (en) | 2016-12-21 | 2020-06-09 | Ethicon Llc | Shaft assembly comprising separately actuatable and retractable systems |
| US10687810B2 (en) | 2016-12-21 | 2020-06-23 | Ethicon Llc | Stepped staple cartridge with tissue retention and gap setting features |
| US20180168633A1 (en) | 2016-12-21 | 2018-06-21 | Ethicon Endo-Surgery, Llc | Surgical stapling instruments and staple-forming anvils |
| US20180168648A1 (en) | 2016-12-21 | 2018-06-21 | Ethicon Endo-Surgery, Llc | Durability features for end effectors and firing assemblies of surgical stapling instruments |
| US11684367B2 (en) | 2016-12-21 | 2023-06-27 | Cilag Gmbh International | Stepped assembly having and end-of-life indicator |
| US10610224B2 (en) | 2016-12-21 | 2020-04-07 | Ethicon Llc | Lockout arrangements for surgical end effectors and replaceable tool assemblies |
| JP7010956B2 (en) | 2016-12-21 | 2022-01-26 | エシコン エルエルシー | How to staple tissue |
| US20180168615A1 (en) | 2016-12-21 | 2018-06-21 | Ethicon Endo-Surgery, Llc | Method of deforming staples from two different types of staple cartridges with the same surgical stapling instrument |
| JP6983893B2 (en) | 2016-12-21 | 2021-12-17 | エシコン エルエルシーEthicon LLC | Lockout configuration for surgical end effectors and replaceable tool assemblies |
| US10568626B2 (en) | 2016-12-21 | 2020-02-25 | Ethicon Llc | Surgical instruments with jaw opening features for increasing a jaw opening distance |
| US10675026B2 (en) | 2016-12-21 | 2020-06-09 | Ethicon Llc | Methods of stapling tissue |
| US10695055B2 (en) | 2016-12-21 | 2020-06-30 | Ethicon Llc | Firing assembly comprising a lockout |
| US10758230B2 (en) | 2016-12-21 | 2020-09-01 | Ethicon Llc | Surgical instrument with primary and safety processors |
| US10945727B2 (en) | 2016-12-21 | 2021-03-16 | Ethicon Llc | Staple cartridge with deformable driver retention features |
| US10888322B2 (en) | 2016-12-21 | 2021-01-12 | Ethicon Llc | Surgical instrument comprising a cutting member |
| US10682138B2 (en) | 2016-12-21 | 2020-06-16 | Ethicon Llc | Bilaterally asymmetric staple forming pocket pairs |
| US20180168623A1 (en) | 2016-12-21 | 2018-06-21 | Ethicon Endo-Surgery, Llc | Surgical stapling systems |
| US10426471B2 (en) | 2016-12-21 | 2019-10-01 | Ethicon Llc | Surgical instrument with multiple failure response modes |
| US10485543B2 (en) | 2016-12-21 | 2019-11-26 | Ethicon Llc | Anvil having a knife slot width |
| MX2019007311A (en) | 2016-12-21 | 2019-11-18 | Ethicon Llc | Surgical stapling systems. |
| US10993715B2 (en) | 2016-12-21 | 2021-05-04 | Ethicon Llc | Staple cartridge comprising staples with different clamping breadths |
| US11419606B2 (en) | 2016-12-21 | 2022-08-23 | Cilag Gmbh International | Shaft assembly comprising a clutch configured to adapt the output of a rotary firing member to two different systems |
| US10667810B2 (en) | 2016-12-21 | 2020-06-02 | Ethicon Llc | Closure members with cam surface arrangements for surgical instruments with separate and distinct closure and firing systems |
| US10307215B2 (en) * | 2017-02-02 | 2019-06-04 | Ethicon Llc | Locking articulating robotic surgical tools |
| US10881399B2 (en) | 2017-06-20 | 2021-01-05 | Ethicon Llc | Techniques for adaptive control of motor velocity of a surgical stapling and cutting instrument |
| US11071554B2 (en) | 2017-06-20 | 2021-07-27 | Cilag Gmbh International | Closed loop feedback control of motor velocity of a surgical stapling and cutting instrument based on magnitude of velocity error measurements |
| USD879809S1 (en) | 2017-06-20 | 2020-03-31 | Ethicon Llc | Display panel with changeable graphical user interface |
| US10888321B2 (en) | 2017-06-20 | 2021-01-12 | Ethicon Llc | Systems and methods for controlling velocity of a displacement member of a surgical stapling and cutting instrument |
| US10327767B2 (en) | 2017-06-20 | 2019-06-25 | Ethicon Llc | Control of motor velocity of a surgical stapling and cutting instrument based on angle of articulation |
| US11382638B2 (en) | 2017-06-20 | 2022-07-12 | Cilag Gmbh International | Closed loop feedback control of motor velocity of a surgical stapling and cutting instrument based on measured time over a specified displacement distance |
| US10881396B2 (en) | 2017-06-20 | 2021-01-05 | Ethicon Llc | Surgical instrument with variable duration trigger arrangement |
| US10779820B2 (en) | 2017-06-20 | 2020-09-22 | Ethicon Llc | Systems and methods for controlling motor speed according to user input for a surgical instrument |
| US11517325B2 (en) | 2017-06-20 | 2022-12-06 | Cilag Gmbh International | Closed loop feedback control of motor velocity of a surgical stapling and cutting instrument based on measured displacement distance traveled over a specified time interval |
| US10624633B2 (en) | 2017-06-20 | 2020-04-21 | Ethicon Llc | Systems and methods for controlling motor velocity of a surgical stapling and cutting instrument |
| US10813639B2 (en) | 2017-06-20 | 2020-10-27 | Ethicon Llc | Closed loop feedback control of motor velocity of a surgical stapling and cutting instrument based on system conditions |
| US11090046B2 (en) | 2017-06-20 | 2021-08-17 | Cilag Gmbh International | Systems and methods for controlling displacement member motion of a surgical stapling and cutting instrument |
| US10307170B2 (en) | 2017-06-20 | 2019-06-04 | Ethicon Llc | Method for closed loop control of motor velocity of a surgical stapling and cutting instrument |
| US10980537B2 (en) | 2017-06-20 | 2021-04-20 | Ethicon Llc | Closed loop feedback control of motor velocity of a surgical stapling and cutting instrument based on measured time over a specified number of shaft rotations |
| US10390841B2 (en) | 2017-06-20 | 2019-08-27 | Ethicon Llc | Control of motor velocity of a surgical stapling and cutting instrument based on angle of articulation |
| US11653914B2 (en) | 2017-06-20 | 2023-05-23 | Cilag Gmbh International | Systems and methods for controlling motor velocity of a surgical stapling and cutting instrument according to articulation angle of end effector |
| USD890784S1 (en) | 2017-06-20 | 2020-07-21 | Ethicon Llc | Display panel with changeable graphical user interface |
| US10646220B2 (en) | 2017-06-20 | 2020-05-12 | Ethicon Llc | Systems and methods for controlling displacement member velocity for a surgical instrument |
| US10368864B2 (en) | 2017-06-20 | 2019-08-06 | Ethicon Llc | Systems and methods for controlling displaying motor velocity for a surgical instrument |
| USD879808S1 (en) | 2017-06-20 | 2020-03-31 | Ethicon Llc | Display panel with graphical user interface |
| US11141154B2 (en) | 2017-06-27 | 2021-10-12 | Cilag Gmbh International | Surgical end effectors and anvils |
| US10772629B2 (en) | 2017-06-27 | 2020-09-15 | Ethicon Llc | Surgical anvil arrangements |
| US11266405B2 (en) | 2017-06-27 | 2022-03-08 | Cilag Gmbh International | Surgical anvil manufacturing methods |
| US11324503B2 (en) | 2017-06-27 | 2022-05-10 | Cilag Gmbh International | Surgical firing member arrangements |
| US10993716B2 (en) | 2017-06-27 | 2021-05-04 | Ethicon Llc | Surgical anvil arrangements |
| US10856869B2 (en) | 2017-06-27 | 2020-12-08 | Ethicon Llc | Surgical anvil arrangements |
| US10211586B2 (en) | 2017-06-28 | 2019-02-19 | Ethicon Llc | Surgical shaft assemblies with watertight housings |
| US11259805B2 (en) | 2017-06-28 | 2022-03-01 | Cilag Gmbh International | Surgical instrument comprising firing member supports |
| USD851762S1 (en) | 2017-06-28 | 2019-06-18 | Ethicon Llc | Anvil |
| US11564686B2 (en) | 2017-06-28 | 2023-01-31 | Cilag Gmbh International | Surgical shaft assemblies with flexible interfaces |
| US11389161B2 (en) | 2017-06-28 | 2022-07-19 | Cilag Gmbh International | Surgical instrument comprising selectively actuatable rotatable couplers |
| USD854151S1 (en) | 2017-06-28 | 2019-07-16 | Ethicon Llc | Surgical instrument shaft |
| US10716614B2 (en) | 2017-06-28 | 2020-07-21 | Ethicon Llc | Surgical shaft assemblies with slip ring assemblies with increased contact pressure |
| US11246592B2 (en) | 2017-06-28 | 2022-02-15 | Cilag Gmbh International | Surgical instrument comprising an articulation system lockable to a frame |
| US10765427B2 (en) | 2017-06-28 | 2020-09-08 | Ethicon Llc | Method for articulating a surgical instrument |
| EP3420947B1 (en) | 2017-06-28 | 2022-05-25 | Cilag GmbH International | Surgical instrument comprising selectively actuatable rotatable couplers |
| US10786253B2 (en) | 2017-06-28 | 2020-09-29 | Ethicon Llc | Surgical end effectors with improved jaw aperture arrangements |
| USD906355S1 (en) | 2017-06-28 | 2020-12-29 | Ethicon Llc | Display screen or portion thereof with a graphical user interface for a surgical instrument |
| US10903685B2 (en) | 2017-06-28 | 2021-01-26 | Ethicon Llc | Surgical shaft assemblies with slip ring assemblies forming capacitive channels |
| US10398434B2 (en) | 2017-06-29 | 2019-09-03 | Ethicon Llc | Closed loop velocity control of closure member for robotic surgical instrument |
| US11007022B2 (en) | 2017-06-29 | 2021-05-18 | Ethicon Llc | Closed loop velocity control techniques based on sensed tissue parameters for robotic surgical instrument |
| US10932772B2 (en) | 2017-06-29 | 2021-03-02 | Ethicon Llc | Methods for closed loop velocity control for robotic surgical instrument |
| US10258418B2 (en) | 2017-06-29 | 2019-04-16 | Ethicon Llc | System for controlling articulation forces |
| US10898183B2 (en) | 2017-06-29 | 2021-01-26 | Ethicon Llc | Robotic surgical instrument with closed loop feedback techniques for advancement of closure member during firing |
| US11304695B2 (en) | 2017-08-03 | 2022-04-19 | Cilag Gmbh International | Surgical system shaft interconnection |
| US11471155B2 (en) | 2017-08-03 | 2022-10-18 | Cilag Gmbh International | Surgical system bailout |
| US11944300B2 (en) | 2017-08-03 | 2024-04-02 | Cilag Gmbh International | Method for operating a surgical system bailout |
| USD907647S1 (en) | 2017-09-29 | 2021-01-12 | Ethicon Llc | Display screen or portion thereof with animated graphical user interface |
| US10729501B2 (en) | 2017-09-29 | 2020-08-04 | Ethicon Llc | Systems and methods for language selection of a surgical instrument |
| USD917500S1 (en) | 2017-09-29 | 2021-04-27 | Ethicon Llc | Display screen or portion thereof with graphical user interface |
| USD907648S1 (en) | 2017-09-29 | 2021-01-12 | Ethicon Llc | Display screen or portion thereof with animated graphical user interface |
| US10743872B2 (en) | 2017-09-29 | 2020-08-18 | Ethicon Llc | System and methods for controlling a display of a surgical instrument |
| US11399829B2 (en) | 2017-09-29 | 2022-08-02 | Cilag Gmbh International | Systems and methods of initiating a power shutdown mode for a surgical instrument |
| US10796471B2 (en) | 2017-09-29 | 2020-10-06 | Ethicon Llc | Systems and methods of displaying a knife position for a surgical instrument |
| US10765429B2 (en) | 2017-09-29 | 2020-09-08 | Ethicon Llc | Systems and methods for providing alerts according to the operational state of a surgical instrument |
| US11134944B2 (en) | 2017-10-30 | 2021-10-05 | Cilag Gmbh International | Surgical stapler knife motion controls |
| US11090075B2 (en) | 2017-10-30 | 2021-08-17 | Cilag Gmbh International | Articulation features for surgical end effector |
| US10779903B2 (en) | 2017-10-31 | 2020-09-22 | Ethicon Llc | Positive shaft rotation lock activated by jaw closure |
| US10842490B2 (en) | 2017-10-31 | 2020-11-24 | Ethicon Llc | Cartridge body design with force reduction based on firing completion |
| WO2019114495A1 (en) * | 2017-12-14 | 2019-06-20 | 苏州天臣国际医疗科技有限公司 | Staple cartridge assembly and medical stapler using same |
| US10687813B2 (en) | 2017-12-15 | 2020-06-23 | Ethicon Llc | Adapters with firing stroke sensing arrangements for use in connection with electromechanical surgical instruments |
| US10779825B2 (en) | 2017-12-15 | 2020-09-22 | Ethicon Llc | Adapters with end effector position sensing and control arrangements for use in connection with electromechanical surgical instruments |
| US10743874B2 (en) | 2017-12-15 | 2020-08-18 | Ethicon Llc | Sealed adapters for use with electromechanical surgical instruments |
| US11071543B2 (en) | 2017-12-15 | 2021-07-27 | Cilag Gmbh International | Surgical end effectors with clamping assemblies configured to increase jaw aperture ranges |
| US10828033B2 (en) | 2017-12-15 | 2020-11-10 | Ethicon Llc | Handheld electromechanical surgical instruments with improved motor control arrangements for positioning components of an adapter coupled thereto |
| US10966718B2 (en) | 2017-12-15 | 2021-04-06 | Ethicon Llc | Dynamic clamping assemblies with improved wear characteristics for use in connection with electromechanical surgical instruments |
| US10869666B2 (en) | 2017-12-15 | 2020-12-22 | Ethicon Llc | Adapters with control systems for controlling multiple motors of an electromechanical surgical instrument |
| US11197670B2 (en) | 2017-12-15 | 2021-12-14 | Cilag Gmbh International | Surgical end effectors with pivotal jaws configured to touch at their respective distal ends when fully closed |
| US10779826B2 (en) | 2017-12-15 | 2020-09-22 | Ethicon Llc | Methods of operating surgical end effectors |
| US11006955B2 (en) | 2017-12-15 | 2021-05-18 | Ethicon Llc | End effectors with positive jaw opening features for use with adapters for electromechanical surgical instruments |
| US11033267B2 (en) | 2017-12-15 | 2021-06-15 | Ethicon Llc | Systems and methods of controlling a clamping member firing rate of a surgical instrument |
| US10743875B2 (en) | 2017-12-15 | 2020-08-18 | Ethicon Llc | Surgical end effectors with jaw stiffener arrangements configured to permit monitoring of firing member |
| US11045270B2 (en) | 2017-12-19 | 2021-06-29 | Cilag Gmbh International | Robotic attachment comprising exterior drive actuator |
| USD910847S1 (en) | 2017-12-19 | 2021-02-16 | Ethicon Llc | Surgical instrument assembly |
| US10835330B2 (en) | 2017-12-19 | 2020-11-17 | Ethicon Llc | Method for determining the position of a rotatable jaw of a surgical instrument attachment assembly |
| US10716565B2 (en) | 2017-12-19 | 2020-07-21 | Ethicon Llc | Surgical instruments with dual articulation drivers |
| US11020112B2 (en) | 2017-12-19 | 2021-06-01 | Ethicon Llc | Surgical tools configured for interchangeable use with different controller interfaces |
| US10729509B2 (en) | 2017-12-19 | 2020-08-04 | Ethicon Llc | Surgical instrument comprising closure and firing locking mechanism |
| US11076853B2 (en) | 2017-12-21 | 2021-08-03 | Cilag Gmbh International | Systems and methods of displaying a knife position during transection for a surgical instrument |
| US11147547B2 (en) | 2017-12-21 | 2021-10-19 | Cilag Gmbh International | Surgical stapler comprising storable cartridges having different staple sizes |
| US11311290B2 (en) | 2017-12-21 | 2022-04-26 | Cilag Gmbh International | Surgical instrument comprising an end effector dampener |
| US11129680B2 (en) | 2017-12-21 | 2021-09-28 | Cilag Gmbh International | Surgical instrument comprising a projector |
| CN108938031B (en) * | 2018-07-31 | 2023-08-04 | 江苏健瑞宝医疗科技股份有限公司 | Head adjusting mechanism of intra-cavity cutting anastomat |
| USD914878S1 (en) | 2018-08-20 | 2021-03-30 | Ethicon Llc | Surgical instrument anvil |
| US11045192B2 (en) | 2018-08-20 | 2021-06-29 | Cilag Gmbh International | Fabricating techniques for surgical stapler anvils |
| US11253256B2 (en) | 2018-08-20 | 2022-02-22 | Cilag Gmbh International | Articulatable motor powered surgical instruments with dedicated articulation motor arrangements |
| US11039834B2 (en) | 2018-08-20 | 2021-06-22 | Cilag Gmbh International | Surgical stapler anvils with staple directing protrusions and tissue stability features |
| US11324501B2 (en) | 2018-08-20 | 2022-05-10 | Cilag Gmbh International | Surgical stapling devices with improved closure members |
| US11291440B2 (en) | 2018-08-20 | 2022-04-05 | Cilag Gmbh International | Method for operating a powered articulatable surgical instrument |
| US10912559B2 (en) | 2018-08-20 | 2021-02-09 | Ethicon Llc | Reinforced deformable anvil tip for surgical stapler anvil |
| US10842492B2 (en) | 2018-08-20 | 2020-11-24 | Ethicon Llc | Powered articulatable surgical instruments with clutching and locking arrangements for linking an articulation drive system to a firing drive system |
| US10856870B2 (en) | 2018-08-20 | 2020-12-08 | Ethicon Llc | Switching arrangements for motor powered articulatable surgical instruments |
| US11207065B2 (en) | 2018-08-20 | 2021-12-28 | Cilag Gmbh International | Method for fabricating surgical stapler anvils |
| US11083458B2 (en) | 2018-08-20 | 2021-08-10 | Cilag Gmbh International | Powered surgical instruments with clutching arrangements to convert linear drive motions to rotary drive motions |
| US10779821B2 (en) | 2018-08-20 | 2020-09-22 | Ethicon Llc | Surgical stapler anvils with tissue stop features configured to avoid tissue pinch |
| US11696761B2 (en) | 2019-03-25 | 2023-07-11 | Cilag Gmbh International | Firing drive arrangements for surgical systems |
| US11172929B2 (en) | 2019-03-25 | 2021-11-16 | Cilag Gmbh International | Articulation drive arrangements for surgical systems |
| US11147551B2 (en) | 2019-03-25 | 2021-10-19 | Cilag Gmbh International | Firing drive arrangements for surgical systems |
| US11147553B2 (en) | 2019-03-25 | 2021-10-19 | Cilag Gmbh International | Firing drive arrangements for surgical systems |
| US11648009B2 (en) | 2019-04-30 | 2023-05-16 | Cilag Gmbh International | Rotatable jaw tip for a surgical instrument |
| US11432816B2 (en) | 2019-04-30 | 2022-09-06 | Cilag Gmbh International | Articulation pin for a surgical instrument |
| US11452528B2 (en) | 2019-04-30 | 2022-09-27 | Cilag Gmbh International | Articulation actuators for a surgical instrument |
| US11426251B2 (en) | 2019-04-30 | 2022-08-30 | Cilag Gmbh International | Articulation directional lights on a surgical instrument |
| US11903581B2 (en) | 2019-04-30 | 2024-02-20 | Cilag Gmbh International | Methods for stapling tissue using a surgical instrument |
| US11253254B2 (en) | 2019-04-30 | 2022-02-22 | Cilag Gmbh International | Shaft rotation actuator on a surgical instrument |
| US11471157B2 (en) | 2019-04-30 | 2022-10-18 | Cilag Gmbh International | Articulation control mapping for a surgical instrument |
| US11627959B2 (en) | 2019-06-28 | 2023-04-18 | Cilag Gmbh International | Surgical instruments including manual and powered system lockouts |
| US11229437B2 (en) | 2019-06-28 | 2022-01-25 | Cilag Gmbh International | Method for authenticating the compatibility of a staple cartridge with a surgical instrument |
| US11497492B2 (en) | 2019-06-28 | 2022-11-15 | Cilag Gmbh International | Surgical instrument including an articulation lock |
| US11051807B2 (en) | 2019-06-28 | 2021-07-06 | Cilag Gmbh International | Packaging assembly including a particulate trap |
| US11376098B2 (en) | 2019-06-28 | 2022-07-05 | Cilag Gmbh International | Surgical instrument system comprising an RFID system |
| US11464601B2 (en) | 2019-06-28 | 2022-10-11 | Cilag Gmbh International | Surgical instrument comprising an RFID system for tracking a movable component |
| US11553971B2 (en) | 2019-06-28 | 2023-01-17 | Cilag Gmbh International | Surgical RFID assemblies for display and communication |
| US11478241B2 (en) | 2019-06-28 | 2022-10-25 | Cilag Gmbh International | Staple cartridge including projections |
| US11426167B2 (en) | 2019-06-28 | 2022-08-30 | Cilag Gmbh International | Mechanisms for proper anvil attachment surgical stapling head assembly |
| US11298132B2 (en) | 2019-06-28 | 2022-04-12 | Cilag GmbH Inlernational | Staple cartridge including a honeycomb extension |
| US11638587B2 (en) | 2019-06-28 | 2023-05-02 | Cilag Gmbh International | RFID identification systems for surgical instruments |
| US11399837B2 (en) | 2019-06-28 | 2022-08-02 | Cilag Gmbh International | Mechanisms for motor control adjustments of a motorized surgical instrument |
| US11219455B2 (en) | 2019-06-28 | 2022-01-11 | Cilag Gmbh International | Surgical instrument including a lockout key |
| US11660163B2 (en) | 2019-06-28 | 2023-05-30 | Cilag Gmbh International | Surgical system with RFID tags for updating motor assembly parameters |
| US11684434B2 (en) | 2019-06-28 | 2023-06-27 | Cilag Gmbh International | Surgical RFID assemblies for instrument operational setting control |
| US11523822B2 (en) | 2019-06-28 | 2022-12-13 | Cilag Gmbh International | Battery pack including a circuit interrupter |
| US11298127B2 (en) | 2019-06-28 | 2022-04-12 | Cilag GmbH Interational | Surgical stapling system having a lockout mechanism for an incompatible cartridge |
| US11224497B2 (en) | 2019-06-28 | 2022-01-18 | Cilag Gmbh International | Surgical systems with multiple RFID tags |
| US11291451B2 (en) | 2019-06-28 | 2022-04-05 | Cilag Gmbh International | Surgical instrument with battery compatibility verification functionality |
| US11259803B2 (en) | 2019-06-28 | 2022-03-01 | Cilag Gmbh International | Surgical stapling system having an information encryption protocol |
| US11246678B2 (en) | 2019-06-28 | 2022-02-15 | Cilag Gmbh International | Surgical stapling system having a frangible RFID tag |
| US11771419B2 (en) | 2019-06-28 | 2023-10-03 | Cilag Gmbh International | Packaging for a replaceable component of a surgical stapling system |
| US11234698B2 (en) | 2019-12-19 | 2022-02-01 | Cilag Gmbh International | Stapling system comprising a clamp lockout and a firing lockout |
| US11304696B2 (en) | 2019-12-19 | 2022-04-19 | Cilag Gmbh International | Surgical instrument comprising a powered articulation system |
| US11931033B2 (en) | 2019-12-19 | 2024-03-19 | Cilag Gmbh International | Staple cartridge comprising a latch lockout |
| US11559304B2 (en) | 2019-12-19 | 2023-01-24 | Cilag Gmbh International | Surgical instrument comprising a rapid closure mechanism |
| US11911032B2 (en) | 2019-12-19 | 2024-02-27 | Cilag Gmbh International | Staple cartridge comprising a seating cam |
| US11529137B2 (en) | 2019-12-19 | 2022-12-20 | Cilag Gmbh International | Staple cartridge comprising driver retention members |
| US11464512B2 (en) | 2019-12-19 | 2022-10-11 | Cilag Gmbh International | Staple cartridge comprising a curved deck surface |
| US11446029B2 (en) | 2019-12-19 | 2022-09-20 | Cilag Gmbh International | Staple cartridge comprising projections extending from a curved deck surface |
| US11576672B2 (en) | 2019-12-19 | 2023-02-14 | Cilag Gmbh International | Surgical instrument comprising a closure system including a closure member and an opening member driven by a drive screw |
| US11607219B2 (en) | 2019-12-19 | 2023-03-21 | Cilag Gmbh International | Staple cartridge comprising a detachable tissue cutting knife |
| US11291447B2 (en) | 2019-12-19 | 2022-04-05 | Cilag Gmbh International | Stapling instrument comprising independent jaw closing and staple firing systems |
| US11844520B2 (en) | 2019-12-19 | 2023-12-19 | Cilag Gmbh International | Staple cartridge comprising driver retention members |
| US11701111B2 (en) | 2019-12-19 | 2023-07-18 | Cilag Gmbh International | Method for operating a surgical stapling instrument |
| US11504122B2 (en) | 2019-12-19 | 2022-11-22 | Cilag Gmbh International | Surgical instrument comprising a nested firing member |
| US11529139B2 (en) | 2019-12-19 | 2022-12-20 | Cilag Gmbh International | Motor driven surgical instrument |
| USD967421S1 (en) | 2020-06-02 | 2022-10-18 | Cilag Gmbh International | Staple cartridge |
| USD975850S1 (en) | 2020-06-02 | 2023-01-17 | Cilag Gmbh International | Staple cartridge |
| USD976401S1 (en) | 2020-06-02 | 2023-01-24 | Cilag Gmbh International | Staple cartridge |
| USD975278S1 (en) | 2020-06-02 | 2023-01-10 | Cilag Gmbh International | Staple cartridge |
| USD974560S1 (en) | 2020-06-02 | 2023-01-03 | Cilag Gmbh International | Staple cartridge |
| USD966512S1 (en) | 2020-06-02 | 2022-10-11 | Cilag Gmbh International | Staple cartridge |
| USD975851S1 (en) | 2020-06-02 | 2023-01-17 | Cilag Gmbh International | Staple cartridge |
| US20220031320A1 (en) | 2020-07-28 | 2022-02-03 | Cilag Gmbh International | Surgical instruments with flexible firing member actuator constraint arrangements |
| US20220047261A1 (en) * | 2020-08-17 | 2022-02-17 | Covidien Lp | Surgical stapling device with reload assembly having a lockout |
| USD1013170S1 (en) | 2020-10-29 | 2024-01-30 | Cilag Gmbh International | Surgical instrument assembly |
| US11517390B2 (en) | 2020-10-29 | 2022-12-06 | Cilag Gmbh International | Surgical instrument comprising a limited travel switch |
| US11931025B2 (en) | 2020-10-29 | 2024-03-19 | Cilag Gmbh International | Surgical instrument comprising a releasable closure drive lock |
| US11452526B2 (en) | 2020-10-29 | 2022-09-27 | Cilag Gmbh International | Surgical instrument comprising a staged voltage regulation start-up system |
| USD980425S1 (en) | 2020-10-29 | 2023-03-07 | Cilag Gmbh International | Surgical instrument assembly |
| US11534259B2 (en) | 2020-10-29 | 2022-12-27 | Cilag Gmbh International | Surgical instrument comprising an articulation indicator |
| US11844518B2 (en) | 2020-10-29 | 2023-12-19 | Cilag Gmbh International | Method for operating a surgical instrument |
| US11717289B2 (en) | 2020-10-29 | 2023-08-08 | Cilag Gmbh International | Surgical instrument comprising an indicator which indicates that an articulation drive is actuatable |
| US11617577B2 (en) | 2020-10-29 | 2023-04-04 | Cilag Gmbh International | Surgical instrument comprising a sensor configured to sense whether an articulation drive of the surgical instrument is actuatable |
| US11779330B2 (en) | 2020-10-29 | 2023-10-10 | Cilag Gmbh International | Surgical instrument comprising a jaw alignment system |
| US11896217B2 (en) | 2020-10-29 | 2024-02-13 | Cilag Gmbh International | Surgical instrument comprising an articulation lock |
| US11737751B2 (en) | 2020-12-02 | 2023-08-29 | Cilag Gmbh International | Devices and methods of managing energy dissipated within sterile barriers of surgical instrument housings |
| US11744581B2 (en) | 2020-12-02 | 2023-09-05 | Cilag Gmbh International | Powered surgical instruments with multi-phase tissue treatment |
| US11890010B2 (en) | 2020-12-02 | 2024-02-06 | Cllag GmbH International | Dual-sided reinforced reload for surgical instruments |
| US11678882B2 (en) | 2020-12-02 | 2023-06-20 | Cilag Gmbh International | Surgical instruments with interactive features to remedy incidental sled movements |
| US11653915B2 (en) | 2020-12-02 | 2023-05-23 | Cilag Gmbh International | Surgical instruments with sled location detection and adjustment features |
| US11849943B2 (en) | 2020-12-02 | 2023-12-26 | Cilag Gmbh International | Surgical instrument with cartridge release mechanisms |
| US11627960B2 (en) | 2020-12-02 | 2023-04-18 | Cilag Gmbh International | Powered surgical instruments with smart reload with separately attachable exteriorly mounted wiring connections |
| US11653920B2 (en) | 2020-12-02 | 2023-05-23 | Cilag Gmbh International | Powered surgical instruments with communication interfaces through sterile barrier |
| US11944296B2 (en) | 2020-12-02 | 2024-04-02 | Cilag Gmbh International | Powered surgical instruments with external connectors |
| US11925349B2 (en) | 2021-02-26 | 2024-03-12 | Cilag Gmbh International | Adjustment to transfer parameters to improve available power |
| US11950777B2 (en) | 2021-02-26 | 2024-04-09 | Cilag Gmbh International | Staple cartridge comprising an information access control system |
| US11793514B2 (en) | 2021-02-26 | 2023-10-24 | Cilag Gmbh International | Staple cartridge comprising sensor array which may be embedded in cartridge body |
| US11751869B2 (en) | 2021-02-26 | 2023-09-12 | Cilag Gmbh International | Monitoring of multiple sensors over time to detect moving characteristics of tissue |
| US11812964B2 (en) | 2021-02-26 | 2023-11-14 | Cilag Gmbh International | Staple cartridge comprising a power management circuit |
| US11730473B2 (en) | 2021-02-26 | 2023-08-22 | Cilag Gmbh International | Monitoring of manufacturing life-cycle |
| US11749877B2 (en) | 2021-02-26 | 2023-09-05 | Cilag Gmbh International | Stapling instrument comprising a signal antenna |
| US11950779B2 (en) | 2021-02-26 | 2024-04-09 | Cilag Gmbh International | Method of powering and communicating with a staple cartridge |
| US11696757B2 (en) | 2021-02-26 | 2023-07-11 | Cilag Gmbh International | Monitoring of internal systems to detect and track cartridge motion status |
| US11744583B2 (en) | 2021-02-26 | 2023-09-05 | Cilag Gmbh International | Distal communication array to tune frequency of RF systems |
| US11723657B2 (en) | 2021-02-26 | 2023-08-15 | Cilag Gmbh International | Adjustable communication based on available bandwidth and power capacity |
| US11701113B2 (en) | 2021-02-26 | 2023-07-18 | Cilag Gmbh International | Stapling instrument comprising a separate power antenna and a data transfer antenna |
| US11717291B2 (en) | 2021-03-22 | 2023-08-08 | Cilag Gmbh International | Staple cartridge comprising staples configured to apply different tissue compression |
| US11737749B2 (en) | 2021-03-22 | 2023-08-29 | Cilag Gmbh International | Surgical stapling instrument comprising a retraction system |
| US11826012B2 (en) | 2021-03-22 | 2023-11-28 | Cilag Gmbh International | Stapling instrument comprising a pulsed motor-driven firing rack |
| US11826042B2 (en) | 2021-03-22 | 2023-11-28 | Cilag Gmbh International | Surgical instrument comprising a firing drive including a selectable leverage mechanism |
| US11723658B2 (en) | 2021-03-22 | 2023-08-15 | Cilag Gmbh International | Staple cartridge comprising a firing lockout |
| US11806011B2 (en) | 2021-03-22 | 2023-11-07 | Cilag Gmbh International | Stapling instrument comprising tissue compression systems |
| US11759202B2 (en) | 2021-03-22 | 2023-09-19 | Cilag Gmbh International | Staple cartridge comprising an implantable layer |
| US11849944B2 (en) | 2021-03-24 | 2023-12-26 | Cilag Gmbh International | Drivers for fastener cartridge assemblies having rotary drive screws |
| US11849945B2 (en) | 2021-03-24 | 2023-12-26 | Cilag Gmbh International | Rotary-driven surgical stapling assembly comprising eccentrically driven firing member |
| US11786243B2 (en) | 2021-03-24 | 2023-10-17 | Cilag Gmbh International | Firing members having flexible portions for adapting to a load during a surgical firing stroke |
| US11832816B2 (en) | 2021-03-24 | 2023-12-05 | Cilag Gmbh International | Surgical stapling assembly comprising nonplanar staples and planar staples |
| US11944336B2 (en) | 2021-03-24 | 2024-04-02 | Cilag Gmbh International | Joint arrangements for multi-planar alignment and support of operational drive shafts in articulatable surgical instruments |
| US11896218B2 (en) | 2021-03-24 | 2024-02-13 | Cilag Gmbh International | Method of using a powered stapling device |
| US11793516B2 (en) | 2021-03-24 | 2023-10-24 | Cilag Gmbh International | Surgical staple cartridge comprising longitudinal support beam |
| US11903582B2 (en) | 2021-03-24 | 2024-02-20 | Cilag Gmbh International | Leveraging surfaces for cartridge installation |
| US11857183B2 (en) | 2021-03-24 | 2024-01-02 | Cilag Gmbh International | Stapling assembly components having metal substrates and plastic bodies |
| US11896219B2 (en) | 2021-03-24 | 2024-02-13 | Cilag Gmbh International | Mating features between drivers and underside of a cartridge deck |
| US11744603B2 (en) | 2021-03-24 | 2023-09-05 | Cilag Gmbh International | Multi-axis pivot joints for surgical instruments and methods for manufacturing same |
| US11786239B2 (en) | 2021-03-24 | 2023-10-17 | Cilag Gmbh International | Surgical instrument articulation joint arrangements comprising multiple moving linkage features |
| US11918217B2 (en) | 2021-05-28 | 2024-03-05 | Cilag Gmbh International | Stapling instrument comprising a staple cartridge insertion stop |
| US11877745B2 (en) | 2021-10-18 | 2024-01-23 | Cilag Gmbh International | Surgical stapling assembly having longitudinally-repeating staple leg clusters |
| US11937816B2 (en) | 2021-10-28 | 2024-03-26 | Cilag Gmbh International | Electrical lead arrangements for surgical instruments |
Family Cites Families (24)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US4566620A (en) * | 1984-10-19 | 1986-01-28 | United States Surgical Corporation | Articulated surgical fastener applying apparatus |
| US5219111A (en) * | 1991-03-11 | 1993-06-15 | Ethicon, Inc. | Pneumatically actuated linear stapling device |
| US5289963A (en) * | 1991-10-18 | 1994-03-01 | United States Surgical Corporation | Apparatus and method for applying surgical staples to attach an object to body tissue |
| US5330502A (en) * | 1992-10-09 | 1994-07-19 | Ethicon, Inc. | Rotational endoscopic mechanism with jointed drive mechanism |
| US5626587A (en) * | 1992-10-09 | 1997-05-06 | Ethicon Endo-Surgery, Inc. | Method for operating a surgical instrument |
| US5409498A (en) * | 1992-11-05 | 1995-04-25 | Ethicon, Inc. | Rotatable articulating endoscopic fastening instrument |
| US5827323A (en) * | 1993-07-21 | 1998-10-27 | Charles H. Klieman | Surgical instrument for endoscopic and general surgery |
| US5465894A (en) * | 1993-12-06 | 1995-11-14 | Ethicon, Inc. | Surgical stapling instrument with articulated stapling head assembly on rotatable and flexible support shaft |
| US5743456A (en) * | 1993-12-16 | 1998-04-28 | Stryker Corporation | Hand actuable surgical handpiece |
| US5465895A (en) * | 1994-02-03 | 1995-11-14 | Ethicon Endo-Surgery, Inc. | Surgical stapler instrument |
| US5643285A (en) * | 1994-10-18 | 1997-07-01 | Blairden Precision Instruments, Inc. | Vaginal extender for colpotomy surgery |
| US5632432A (en) * | 1994-12-19 | 1997-05-27 | Ethicon Endo-Surgery, Inc. | Surgical instrument |
| US5582615A (en) * | 1995-10-30 | 1996-12-10 | Pilling Weck, Incorporated | Handle for surgical clip applicator systems |
| US5669875A (en) * | 1996-04-16 | 1997-09-23 | United States Surgical Corporation | Endoscopic surgical apparatus with longitudinal actuation |
| US5984864A (en) * | 1997-10-07 | 1999-11-16 | Ethicon Endo-Surgery, Inc. | Tissue stabilization device for use during surgery |
| CA2319178A1 (en) * | 1998-11-24 | 2000-06-02 | Inbae Yoon | Surgical instrument with rotatably mounted offset end effector and method of using the same |
| US6506149B2 (en) * | 1999-09-07 | 2003-01-14 | Origin Medsystems, Inc. | Organ manipulator having suction member supported with freedom to move relative to its support |
| JP2001190563A (en) * | 2000-01-06 | 2001-07-17 | Olympus Optical Co Ltd | Cauter |
| JP4078518B2 (en) * | 2001-12-11 | 2008-04-23 | 株式会社コーナン・メディカル | Medical microscope |
| US20050236282A1 (en) * | 2002-08-27 | 2005-10-27 | Huska Brenda C | Compartmentalized cigarette snuffer and receptacle |
| US6755837B2 (en) * | 2002-09-23 | 2004-06-29 | Maxilon Laboratories, Inc. | Apparatus and method for harvesting bone |
| JP2004255082A (en) * | 2003-02-27 | 2004-09-16 | Olympus Corp | Surgical treatment appliance |
| ES2384974T3 (en) * | 2003-06-17 | 2012-07-16 | Tyco Healthcare Group Lp | Surgical stapling device |
| US6964363B2 (en) * | 2003-07-09 | 2005-11-15 | Ethicon Endo-Surgery, Inc. | Surgical stapling instrument having articulation joint support plates for supporting a firing bar |
-
2006
- 2006-07-25 JP JP2008524042A patent/JP4336386B2/en active Active
-
2008
- 2008-10-02 JP JP2008257807A patent/JP4611410B2/en active Active
-
2009
- 2009-05-14 JP JP2009118008A patent/JP5020995B2/en active Active
-
2011
- 2011-05-18 JP JP2011111900A patent/JP5623980B2/en active Active
- 2011-05-18 JP JP2011111899A patent/JP5686373B2/en active Active
-
2013
- 2013-06-07 JP JP2013120535A patent/JP5889834B2/en active Active
-
2015
- 2015-08-28 JP JP2015168464A patent/JP5969670B2/en active Active
-
2016
- 2016-03-15 JP JP2016051247A patent/JP6622120B2/en active Active
-
2017
- 2017-02-06 JP JP2017019295A patent/JP6298185B2/en active Active
- 2017-08-15 JP JP2017156785A patent/JP7001389B2/en active Active
-
2018
- 2018-10-22 JP JP2018198534A patent/JP7090528B2/en active Active
-
2020
- 2020-05-07 JP JP2020081760A patent/JP7130697B2/en active Active
Also Published As
| Publication number | Publication date |
|---|---|
| JP7130697B2 (en) | 2022-09-05 |
| JP2016152925A (en) | 2016-08-25 |
| JP2011200664A (en) | 2011-10-13 |
| JP7090528B2 (en) | 2022-06-24 |
| JP6622120B2 (en) | 2019-12-18 |
| JP2009507526A (en) | 2009-02-26 |
| JP2016025898A (en) | 2016-02-12 |
| JP2009213903A (en) | 2009-09-24 |
| JP2017109123A (en) | 2017-06-22 |
| JP6298185B2 (en) | 2018-03-20 |
| JP5686373B2 (en) | 2015-03-18 |
| JP7001389B2 (en) | 2022-01-19 |
| JP2019048089A (en) | 2019-03-28 |
| JP5020995B2 (en) | 2012-09-05 |
| JP2013208476A (en) | 2013-10-10 |
| JP2009056316A (en) | 2009-03-19 |
| JP2017213426A (en) | 2017-12-07 |
| JP5889834B2 (en) | 2016-03-22 |
| JP5623980B2 (en) | 2014-11-12 |
| JP2020175201A (en) | 2020-10-29 |
| JP5969670B2 (en) | 2016-08-17 |
| JP4611410B2 (en) | 2011-01-12 |
| JP2011200663A (en) | 2011-10-13 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| JP6298185B2 (en) | Surgical stapling and cutting device and method of using the device | |
| US11234695B2 (en) | Surgical stapling and cutting device |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| A975 | Report on accelerated examination |
Free format text: JAPANESE INTERMEDIATE CODE: A971005 Effective date: 20090115 |
|
| A131 | Notification of reasons for refusal |
Free format text: JAPANESE INTERMEDIATE CODE: A131 Effective date: 20090120 |
|
| A601 | Written request for extension of time |
Free format text: JAPANESE INTERMEDIATE CODE: A601 Effective date: 20090417 |
|
| A602 | Written permission of extension of time |
Free format text: JAPANESE INTERMEDIATE CODE: A602 Effective date: 20090424 |
|
| A521 | Request for written amendment filed |
Free format text: JAPANESE INTERMEDIATE CODE: A523 Effective date: 20090514 |
|
| TRDD | Decision of grant or rejection written | ||
| A01 | Written decision to grant a patent or to grant a registration (utility model) |
Free format text: JAPANESE INTERMEDIATE CODE: A01 Effective date: 20090609 |
|
| A01 | Written decision to grant a patent or to grant a registration (utility model) |
Free format text: JAPANESE INTERMEDIATE CODE: A01 |
|
| A61 | First payment of annual fees (during grant procedure) |
Free format text: JAPANESE INTERMEDIATE CODE: A61 Effective date: 20090626 |
|
| FPAY | Renewal fee payment (event date is renewal date of database) |
Free format text: PAYMENT UNTIL: 20120703 Year of fee payment: 3 |
|
| R150 | Certificate of patent or registration of utility model |
Ref document number: 4336386 Country of ref document: JP Free format text: JAPANESE INTERMEDIATE CODE: R150 Free format text: JAPANESE INTERMEDIATE CODE: R150 |
|
| FPAY | Renewal fee payment (event date is renewal date of database) |
Free format text: PAYMENT UNTIL: 20130703 Year of fee payment: 4 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |
|
| R250 | Receipt of annual fees |
Free format text: JAPANESE INTERMEDIATE CODE: R250 |