WO2014145672A1 - High strength and bio-absorbable magnesium alloys - Google Patents
High strength and bio-absorbable magnesium alloys Download PDFInfo
- Publication number
- WO2014145672A1 WO2014145672A1 PCT/US2014/030477 US2014030477W WO2014145672A1 WO 2014145672 A1 WO2014145672 A1 WO 2014145672A1 US 2014030477 W US2014030477 W US 2014030477W WO 2014145672 A1 WO2014145672 A1 WO 2014145672A1
- Authority
- WO
- WIPO (PCT)
- Prior art keywords
- percent
- microalloyed
- surgical device
- weight
- range
- Prior art date
Links
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L27/00—Materials for grafts or prostheses or for coating grafts or prostheses
- A61L27/02—Inorganic materials
- A61L27/04—Metals or alloys
- A61L27/047—Other specific metals or alloys not covered by A61L27/042 - A61L27/045 or A61L27/06
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L31/00—Materials for other surgical articles, e.g. stents, stent-grafts, shunts, surgical drapes, guide wires, materials for adhesion prevention, occluding devices, surgical gloves, tissue fixation devices
- A61L31/02—Inorganic materials
- A61L31/022—Metals or alloys
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L31/00—Materials for other surgical articles, e.g. stents, stent-grafts, shunts, surgical drapes, guide wires, materials for adhesion prevention, occluding devices, surgical gloves, tissue fixation devices
- A61L31/14—Materials characterised by their function or physical properties, e.g. injectable or lubricating compositions, shape-memory materials, surface modified materials
- A61L31/148—Materials at least partially resorbable by the body
-
- C—CHEMISTRY; METALLURGY
- C22—METALLURGY; FERROUS OR NON-FERROUS ALLOYS; TREATMENT OF ALLOYS OR NON-FERROUS METALS
- C22C—ALLOYS
- C22C23/00—Alloys based on magnesium
- C22C23/04—Alloys based on magnesium with zinc or cadmium as the next major constituent
-
- C—CHEMISTRY; METALLURGY
- C22—METALLURGY; FERROUS OR NON-FERROUS ALLOYS; TREATMENT OF ALLOYS OR NON-FERROUS METALS
- C22F—CHANGING THE PHYSICAL STRUCTURE OF NON-FERROUS METALS AND NON-FERROUS ALLOYS
- C22F1/00—Changing the physical structure of non-ferrous metals or alloys by heat treatment or by hot or cold working
- C22F1/002—Changing the physical structure of non-ferrous metals or alloys by heat treatment or by hot or cold working by rapid cooling or quenching; cooling agents used therefor
-
- C—CHEMISTRY; METALLURGY
- C22—METALLURGY; FERROUS OR NON-FERROUS ALLOYS; TREATMENT OF ALLOYS OR NON-FERROUS METALS
- C22F—CHANGING THE PHYSICAL STRUCTURE OF NON-FERROUS METALS AND NON-FERROUS ALLOYS
- C22F1/00—Changing the physical structure of non-ferrous metals or alloys by heat treatment or by hot or cold working
- C22F1/06—Changing the physical structure of non-ferrous metals or alloys by heat treatment or by hot or cold working of magnesium or alloys based thereon
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/064—Surgical staples, i.e. penetrating the tissue
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/064—Surgical staples, i.e. penetrating the tissue
- A61B17/0642—Surgical staples, i.e. penetrating the tissue for bones, e.g. for osteosynthesis or connecting tendon to bone
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B17/56—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor
- A61B17/58—Surgical instruments or methods for treatment of bones or joints; Devices specially adapted therefor for osteosynthesis, e.g. bone plates, screws, setting implements or the like
- A61B17/68—Internal fixation devices, including fasteners and spinal fixators, even if a part thereof projects from the skin
- A61B17/84—Fasteners therefor or fasteners being internal fixation devices
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B2017/00004—(bio)absorbable, (bio)resorbable, resorptive
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61L—METHODS OR APPARATUS FOR STERILISING MATERIALS OR OBJECTS IN GENERAL; DISINFECTION, STERILISATION OR DEODORISATION OF AIR; CHEMICAL ASPECTS OF BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES; MATERIALS FOR BANDAGES, DRESSINGS, ABSORBENT PADS OR SURGICAL ARTICLES
- A61L2430/00—Materials or treatment for tissue regeneration
- A61L2430/02—Materials or treatment for tissue regeneration for reconstruction of bones; weight-bearing implants
Definitions
- the present invention generally relates to surgical device. More specifically, the present invention relates to bio-absorbable surgical devices, including implantable devices for fixating bone and tissue and non-implantable surgical devices.
- Biodegradable plastics are also sometimes used as the fixation devices to allow repaired ligaments to heal and strengthen. As noted above, such plastic fixation devices do not properly mimic bone characteristics in terms of strength. Nor do these polymer implants encourage bone growth on their receding surface as they absorb. Stronger, tougher and stiffer materials in the current biodegradable plastics are needed for these procedures.
- Mg magnesium
- Al aluminum
- RE Rare Earth
- An alloy base and its alloying elements need to meet the following requirements of non-toxicity: minimal gas bubbling around the implant; normal hematology and serum biochemistry; good osteoconductivity and osteoinductivity; enhanced attached new bone growth of improved density and strength; good cytocompatibility; non-inflammation; good adhesion of osteoblasts; even distribution of alloying elements around the implants; and the addition of essential nutrients to the body, but not exceeding yearly safe limits.
- the present invention provides bio-absorbable fixation devices and retractors constructed of a magnesium alloy that meets the aforementioned requirements.
- the magnesium alloy and processing are specifically tuned for either the fixation device application or the retractor application.
- the fixation device application the particular magnesium alloy and process can be fine-tuned to the healing time/ strength requirements of the particular surgical repair.
- the retractor application the magnesium alloy and process can be tuned to provide the desired strength, allowing for fast absorption of any metal fragments retained within the body of the patient.
- the invention provides a Mg alloy that is hard and strong, providing durability for the entire healing process to any fixation device made of the Mg alloy.
- Magnesium (Mg) is the lightest of structural metals, at 60% of the density of Al, 38% of titanium (Ti) and 20% of stainless steel or cobalt (Co) implants.
- the elastic modulus and yield strength of Mg alloys are closer to bone than alloys used in other metallic implants - thus use of the proposed magnesium alloys maximizing stress transfer at interfaces.
- the fracture toughness of Mg alloys exceeds that of ceramics, hydroxyapatite, polymers and ceramic implants. It is also important to note that Mg is friendly to the body.
- Mg is naturally found in bone tissue and is essential to human metabolism. It is also the 4 th most abundant cation in the human body, is a co-factor for many enzymes, and stabilizes both DNA and RNA. During bio-absorption, Mg from the dissolving implant alloys is absorbed into the new attached bone. As a result, this new bone is denser and stronger than the previously fractured bone.
- the present invention therefore provides a microalloyed magnesium material for absorption in the body of a human or animal, the microalloyed magnesium material consisting of: 0.85 to 1.4 percent by weight of zinc (Zn), 0.2 to 0.5 percent by weight of calcium (Ca), 0.2 to 0.5 percent by weight of manganese (Mn) with the remainder being magnesium (Mg) and inevitable impurities.
- the combined percent of Zn, Ca and Mn microalloyed with Mg is in the range of 1.4 to 2.4 percent.
- the combined percent of Zn, Ca and Mn microalloyed with Mg is in the range of 1.5 to 2.4 percent.
- the Zn content is in the range of 0.9 to 1.3 percent by weight.
- the Ca content is in the range of 0.2 to 0.4 percent by weight.
- the Mn content is in the range of 0.2 to 0.35 percent by weight.
- nanometer-sized ordered zones including nanometer-sized ordered zones (mini prisms of 1-3 atom layers) of about 10 x 0.5 nanometers.
- the invention provides for a surgical device formed of a material for absorption into the body of a human or animal, the surgical device comprising: a body being formed of magnesium (Mg) microalloyed with zinc (Zn), calcium (Ca) and manganese (Mn) to form a microalloyed magnesium material, the microalloyed magnesium material consisting essentially of 0.85 to 1.4 percent by weight of zinc (Zn), 0.2 to 0.5 percent by weight of calcium (Ca), 0.2 to 0.5 percent by weight of manganese (Mn) with the remainder being magnesium (Mg).
- Mg magnesium
- Zn zinc
- Ca calcium
- Mn manganese
- the body is one of a screw, a plate, a stent, a staple, a wire or an implant device.
- the body is part of one of a clamp, a retractor, forceps or a non-implant device.
- the combined percent of Zn, Ca and Mn microalloyed with Mg is in the range of 1.4 to 2.4 percent.
- the combined percent of Zn, Ca and Mn microalloyed with Mg is in the range of 1.5 to 2.4 percent.
- the Zn content is in the range of 0.9 to 1.3 percent by weight.
- the Ca content is in the range of 0.2 to 0.4 percent by weight.
- the Mn content is in the range of 0.2 to 0.35 percent by weight.
- the microalloyed magnesium material has a yield strength in the range of 150 to 220 MPa.
- the microalloyed magnesium material has an elongation percentage in the range of 15 to 35 percent.
- the microalloyed magnesium material has a hardness of 60 to 84 Hv.
- the microalloyed magnesium material has a grain size of less than 5 ⁇ .
- the present invention provides for a method of manufacturing a surgical device formed at least in part of a material for absorption into the body of a human or animal, the method comprising the steps of: providing a melt of a magnesium material consisting essentially of 0.85 to 1.4 percent by weight of zinc (Zn), 0.2 to 0.5 percent by weight of calcium (Ca), 0.2 to 0.5 percent by weight of manganese (Mn) with the remainder being magnesium (Mg), the melt forming a microalloyed magnesium material; forming a casting from the microalloyed magnesium material; deforming the casting by a thermomechanical process whereby thickness of the casting is reduced an amount greater than 30 percent to form a reduced thickness wrought product; annealing the reduced thickness wrought product to form an annealed wrought product; subjecting the
- the deforming step includes rolling of the casting.
- the deforming step includes extruding of the casting.
- the extruding of the casting reduces the thickness of the casting by greater than 50 percent.
- annealing step includes annealing in the range of 300°C to 400°C.
- annealing step includes annealing for up to 4 hours.
- the quenching includes water quenching.
- hardening is performed by solid solution microalloying of Zn, Ca, and Mn with Mg.
- hardening is performed by forming nanometer- sized ordered zones (mini prisms of 1-3 atom layers) of about 10 x 0.5 nanometers.
- the hardening includes age hardening in the range of
- the forming step forms the casting into one of a screw, a plate, a stent, a staple, a wire, and an implant device.
- the forming step forms the casting into one of a clamp, a retractor, forceps or a non-implant device.
- the combined percent of Zn, Ca and Mn in the microalloyed magnesium material in the range of 1.4 to 2.4 percent.
- the combined percent of Zn, Ca and Mn in the microalloyed magnesium material is in the range of 1.5 to 2.4 percent.
- the present invention provides a method of fixating bone or tissue of a patient comprising the steps of: implanting a fixation device in a patient's body whereby the fixation device secures bone or tissue of the patient together, the fixation device being formed of magnesium (Mg) microalloyed with zinc (Zn), calcium (Ca) and manganese (Mn) to form a microalloyed magnesium material, the microalloyed magnesium material consisting essentially of 0.85 to 1.4 percent by weight of zinc (Zn), 0.2 to 0.5 percent by weight of calcium (Ca), 0.2 to 0.5 percent by weight of manganese (Mn) with the remainder being magnesium (Mg); absorbing the fixation device in the patient's body over time as the bone or tissue heals; and continuing to absorb the fixation device in the patient's body over time until the fixation device has been completely absorbed into the body of the patient, whereby surgical removal of the fixation device is not performed on the patient.
- Mg magnesium
- Zn zinc
- Ca calcium
- Mn manga
- the absorbing of the fixation device in the patient's body over time corresponds to a healing time for the bone or tissue secured by the fixation device.
- the combined percent of Zn, Ca and Mn in the microalloyed magnesium material is varied in the range of 1.5 to 2.4 percent to correspond the absorbing of the fixation device in the patient's body over time to a healing time for the bone and tissue secured by the fixation device.
- the fixation device is one of a screw, plate, sheet, wire or stent.
- Figure 1 is a graph presenting the evolution of various alloys in simulated body fluid
- Figure 2 a graph presenting the effects of rolling reduction on the evolution of H 2 from one of the alloys presented in FIG. 1 ;
- Figure 3 is an electron micrograph of an alloy showing a coarse grain boundary therein;
- Figure 4 is an electron diffraction pattern of the alloy seen in Figure 3;
- Figure 5 is a graph presenting the effects of zinc content on the evolution of H 2 from various alloys
- Figure 6 is a graph corrosion rates of one alloy with respect to two commercially available alloys
- Figure 7 is a presentation of histology data of an implant form from an alloy in accordance with the principles of the present invention.
- Figure 8 is a graph presenting corrosion data for the implant after various weeks of implantation;
- Figure 9 shows both the histology and x-ray CT images for an implant after 24 weeks.
- Figure 10 is a graph presenting the volume loss of an implant as a function of in vivo exposure over a course of weeks.
- Mg has a tendency to corrode in the body. This corrosion is an advantage with the present invention. When the Mg alloy is used in the formation of implants, the implants become temporary and do not require a secondary operation for their removal. Rather, the Mg alloy, and therefore the implants, will be absorbed by the body. This corrosion can further be beneficially utilized to provide an intra-body, electrochemical mechanism for the delivery of medicaments. Infections and inflammation will be further reduced as a result of the reduction in secondary surgeries
- alloying elements as replacements for Al and
- RE were selected to strengthen and toughen the Mg base, while serving as nutrients and having tuned corrosion rates.
- One microalloying criterion was the selection of small ternary additions all of which are strong solid solution hardeners at low levels. Such is the case with zinc (Zn), calcium (Ca) and manganese (Mn), as seen in Table I.
- nanometer-sized zones (mini prisms of 1-3 atom layers) of about 10 x 0.5 nanometers (mn) can be generated from a Mg-Zn-Ca-Mn solid solution by thermomechanical processing (TMP) and/ or heat treatment.
- TMP thermomechanical processing
- These ordered zones contain enriched contents of Zn, Ca and Mn in an ordered atomic array in the hep Mg matrix.
- These elements report to the ordered zones in order to reduce misfits resulting from their difference in atomic size and electronegativity from the Mg atom.
- the energy state of the alloy is lowered and the stability state of the alloy is increased.
- microalloying speeds hardening and minimizes over aging or over alloying that might form excessive intermetallic Ca 2 Mg 6 Zn 3 (cathodic to the Mg matrix) and/or Mg 2 Ca (anodic to that matrix) or Mg 2 Zn. If coarse Mg 2 Zn, Ca 2 Mg 6 Zn 3 and/or Mg 2 Ca phases occur in the cast alloy, these phases are dispersed in a disconnected array by the subsequent homogenization, thermomechanical processing and heat treatment steps.
- the anodic or cathodic and hydrogen generating roles of these coarse phases are decreased; resulting in a sufficient useful life in the body to fulfill their bone support mission, before the degree of absorption of the implant renders them no longer functional as a support element.
- the alloy composition and processing may be tailored to add these coarse phases to accelerate corrosion.
- Mg base and microalloying elements are all essential trace elements in the human body.
- Mg is involved in at least 300 enzymatic reactions in the body and is needed for neuromuscular transmission, for reactions involving ATP, for protein and nucleic acid synthesis and transmission of nerve signals.
- Mg is regulated in the kidney, with excess Mg excreted in urine.
- Ca accelerates bone growth.
- Zn is also recognized as a highly essential element for humans. In Zn deficiency, nearly all the physiological functions are strongly perturbed.
- Mn plays a primary role in activating multi-enzyme systems- hydrolases, kinases, transferases, decarboxylases and micondrial respiration.
- the recommended daily intake (RDI) levels are 310-420 mg/d for Mg, 1000-1300 mg/d for Ca and 8-1 1 mg/d for Zn.
- Mn can be tolerated at 0.5% in 25 g implants that dissolve in 1 year; Zn up to 1.4% in 87 g implants and Ca at 0.5% in larger implants. Microalloying all three elements afforded synergistic strengthening without exceeding the toxicity limits.
- a third strengthening mechanism embodied in the present invention is grain refinement.
- thermomechanical processing specifically by extrusion.
- Example 1 Following the concepts mentioned above and as applied to implants, several Mg based alloys (identified as alloys No. 1-6 in Table III) with non-toxic alloying additions were prepared and tested. After resistance furnace melting under Ar gas and casting in steel molds, the alloys were then homogenized for 24 hours at 400°C to dissolve large as-cast particles of Mg/Ca-Zn phases and then hot rolled at 250°C with a greater than 50% reduction to refine the grain structure. In this Example I, the tensile properties after soaking and rolling are also listed in Table III. Yield strength and ductility were low and erratic, believed to be due to grain boundary intermetallic phases.
- Example 2 As noted in Example 1, the yield strength and ductility of the subject alloys were low and erratic. An application of a special heat treatment was found to remedy this fault in Alloy No.6. Post-rolling solution annealing at 400°C, followed by water quenching was found to dissolve the grain boundary Mg/Ca- Zn phases and to retain the ternary elements in solid solution in a soft condition. By then aging at 200°C, the process activated the ordering of nanostructured phases to impart high strength and elongation to the alloy (see Table IV).
- Example 3 The annealing plus aging treatments found beneficial in Example 2
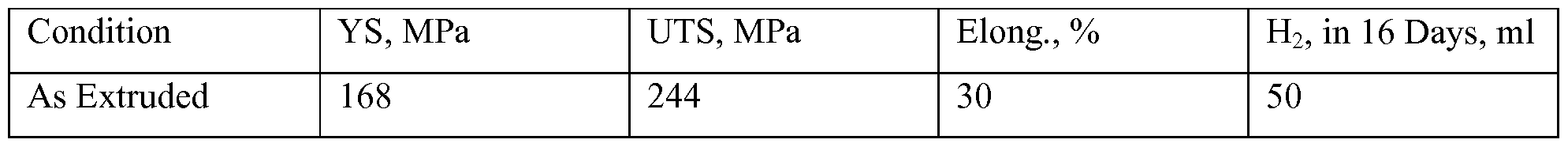
- Example 4 The above alloys, after annealing and aging, were tested in vitro in phosphate buffered saline solution, Simulated Body Fluid (SBF), at 37°C to simulate bio-absorption rate in vivo. In these tests, H 2 evolution is a direct measure of Mg alloy corrosion, and the results are presented in Table VI.
- SBF Simulated Body Fluid
- Example 5 To examine the effect of the rolling practice on the alloys, the corrosion of
- Alloy No. 3 was tested in SBF as a function of % reduction. As shown in Figure 2 and presented in Table VII, lesser rolling reductions (37-53%) showed lower corrosion rates than higher rolling reductions (77%). Further to the beneficial effect on corrosion, for Alloy No. 3, the 53% rolling reduction provided the best combination of strength and ductility.
- bio-absorption rate could be engineered by manipulation of both composition and processing so as to match the targets for either implantable devices and external components or instruments.
- Example 6 Coarse Mg/Ca- Zn phases were identified in a high Zn alloy of Mg-4.1 Zn-
- corrosion rates can be engineered in fixation devices/implants formed from the Mg based alloy.
- the Mg based alloy can be engineered such that the amount and distribution of coarse anodic and cathodic intermetallic Mg/Ca- Zn phases tailor the corrosion rates to match the desired life of any imbedded object formed from the alloy, whether the object is a fixation device/implant or other device.
- Example 7 In order to determine the effect of Mn on strength and ductility, a series of ternary microalloying heats, varying the Mn content, was prepared, rolled and treated (4 hr/400°C, WQ + 2hr/200°C) as above .
- the base of the alloy was composed of Mg-1 Zn-0.45 Ca, while Mn was varied from 0.2 to 0.6%.
- Table VIII increased amounts of Mn decreased the grain size while increasing the strength, hardness and ductility. Optimum strength and hardness were observed at 0.4% Mn. Table VIII. Effect of Mn content on Mg-1 Zn-0.45 Ca alloy, 4 hr/400°C, WQ + 2hr/200°C
- Example 8 To further affirm the effect of Mn content, in a second series of prepared, rolled and treated (4hr/400°C, WQ + 2hr/200°C) alloys, the Mn content was varied from 0.1 to 0.6 % in Alloys No.12- 16. As seen in Table IX, again, good strength and hardness were found at 0.4% Mn, with hardness decreasing at higher Mn level of 0.6%. Thus, Mn can be capped at 0.5 % to minimize any toxicity threat, since Mn has the lowest RDI levels of the alloying elements used.
- Example 9 To further affirm the negative effect of macro-alloying with Zn, as already seen in Figure 1, additional Alloys No.19 & 20 were prepared with higher Zn contents (see Table X and Figure 5) and compared to an implant alloy, Alloy No. 3. It is notable that the higher Zn contents demonstrated lower strength and/or ductility, along with accelerated corrosion, which is believed to be due to presence of coarse Mg/Ca-Zn phases. Thus, Zn is capped at 1.4%.
- Example 10 In order to determine the effect of Ca content on the strength, ductility and hardness, a series of alloys, Alloy Nos. 26, 27 and 28, were prepared and rolled as above, then subsequently treated with two differing treatments. At 0.6% Ca, excessive slag formed on the melt, but excess slag did not form at 0.2% and 0.4% Ca. As a critical test, the mechanical properties in the transverse direction to rolling are listed in Table XL (Properties in the transverse direction to rolling are usually lower than in the longitudinal direction to rolling, the latter of which is presented in the other Tables). In both the annealed and annealed + aged condition, optimum hardness and aging response were seen at 0.4% Ca. Optimum strength and elongation were also seen at 0.4% Ca. Therefore, Ca was capped at 0.5%, with a minimum of 0.2%.
- Example 1 To test an alternate process to rolling, Alloy No.21, composed of Mg-0.91
- Example 12 To test the lower limits on microalloying an additional alloy, Alloy No.22 composed of Mg-0.67 Zn-0.22 Ca-0.30 Mn (a microalloying of 1.19%, the combined amount of Zn, Ca and Mn), was extruded in the same manner as Alloy No. 21. The aging response of this extrusion is compared to that of Alloy No. 21 in Table XIII. Whereas Alloy No.21, with Mg-0.91 Zn-0.32 Ca-0.38 Mn (microalloying of 1.61%) was responsive to aging, the lower microalloying of Alloy No. 22 did not respond to age hardening. Aging increased the hardness of Alloy No.
- Example 13 To further the definition of processing and to confirm the feasibility of production on a larger scale, Alloys No. 23 and 24 were produced at the commercial production facility of Dead Sea Magnesium Ltd., located in Israel. The alloys were melted under SF 6 cover gas and cast into steel molds as 8 inch diameter 45 Kg billets. The billets were then extruded at 300°C into 1.75 and 0.75 inch round bar stock. The compositions of both alloys are listed in Table XIV and tensile properties and corrosion results of Alloy No. 23 are presented in Table XV.
- Example 14 A comparison of a Al and RE free microalloyed Alloy No. 25 of Mg-1.2
- Example 15 In Vivo Animal Study: Animal experiments were conducted on Alloy No.
- Mg-1.2 Zn-0.36 Ca-0.21 Mn The PLGA-based implant was used as a control group since the goal of the animal study was to establish that the histological reaction surrounding the Mg alloy implant caused no more harm than that of commercial polymer PLGA-based implant.
- the rabbits all also received 3 prophylactic doses of the antibiotic Baytril (enrofloxacin 2.5 - 5 mg/kg).
- the rabbits were examined for lameness, swellings, suture failure and general health condition every day. Sutures were removed in 7 - 10 days.
- the animals were euthanized by an intravenous overdose of 2ml/4.5kg dose of 240mg/ml pentobarbital after sedation.
- NAF neutral buffered formalin
- Nanotom-m (GE Sensing & Inspection Technologies GmbH). 3D-images were constructed for measuring volume loss in implant and to study morphological features of the corrosion process. 2D slice stack analysis was used to compare the volume of the implant after exposure to the volume defined by the original dimensions. (See Figure 8)
- the graph presented in Figure 10 shows a qualitative volume of magnesium screw using the 3D software tool package. Utilizing this data trend and corrosion modelling 1 , a dissolution rate of -0.9 mm/yr was determined. This is near the target rate for use of Alloy No. 25 for implanted screws.
Abstract
Description
Claims
Priority Applications (11)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| BR112015023628A BR112015023628B1 (en) | 2013-03-15 | 2014-03-17 | microalloyed magnesium material, device formed of a material, method of making a surgical device and method of fixing a material |
| CA2906876A CA2906876C (en) | 2013-03-15 | 2014-03-17 | High strength and bio-absorbable magnesium alloys |
| US14/777,159 US10022470B2 (en) | 2013-03-15 | 2014-03-17 | High-strength and bio-absorbable magnesium alloys |
| AU2014232750A AU2014232750B2 (en) | 2013-03-15 | 2014-03-17 | High strength and bio-absorbable magnesium alloys |
| ES14765401T ES2817048T3 (en) | 2013-03-15 | 2014-03-17 | High strength and bioabsorbable magnesium alloys |
| KR1020157029685A KR102246635B1 (en) | 2013-03-15 | 2014-03-17 | High strength and bio-absorbable magnesium alloys |
| EP14765401.6A EP2968656B1 (en) | 2013-03-15 | 2014-03-17 | High strength and bio-absorbable magnesium alloys |
| CN201480022585.5A CN105120907B (en) | 2013-03-15 | 2014-03-17 | The magnesium alloy of high intensity and biological absorbable |
| JP2016503407A JP6532858B2 (en) | 2013-03-15 | 2014-03-17 | High strength, bioabsorbable magnesium alloy |
| IL241608A IL241608B (en) | 2013-03-15 | 2015-09-16 | High strength and bio-absorbable magnesium alloys |
| HK16106289.9A HK1218265A1 (en) | 2013-03-15 | 2016-06-02 | High strength and bio-absorbable magnesium alloys |
Applications Claiming Priority (2)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US201361788384P | 2013-03-15 | 2013-03-15 | |
| US61/788,384 | 2013-03-15 |
Publications (1)
| Publication Number | Publication Date |
|---|---|
| WO2014145672A1 true WO2014145672A1 (en) | 2014-09-18 |
Family
ID=51538063
Family Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| PCT/US2014/030477 WO2014145672A1 (en) | 2013-03-15 | 2014-03-17 | High strength and bio-absorbable magnesium alloys |
Country Status (12)
| Country | Link |
|---|---|
| US (1) | US10022470B2 (en) |
| EP (1) | EP2968656B1 (en) |
| JP (1) | JP6532858B2 (en) |
| KR (1) | KR102246635B1 (en) |
| CN (1) | CN105120907B (en) |
| AU (1) | AU2014232750B2 (en) |
| BR (1) | BR112015023628B1 (en) |
| CA (1) | CA2906876C (en) |
| ES (1) | ES2817048T3 (en) |
| HK (1) | HK1218265A1 (en) |
| IL (1) | IL241608B (en) |
| WO (1) | WO2014145672A1 (en) |
Cited By (5)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| CN106148784A (en) * | 2015-04-20 | 2016-11-23 | 中国科学院金属研究所 | A kind of low cost room temperature high-ductility wrought magnesium alloy material and preparation technology thereof |
| WO2017112779A1 (en) * | 2015-12-21 | 2017-06-29 | The University Of Toledo | Process to produce high-strength and corrosion resistant alloy for patient-specific bioresorbable bone fixation implants and hardware |
| WO2019002277A1 (en) | 2017-06-27 | 2019-01-03 | Aap Implantate Ag | Magnesium alloy, biodegradable implant and method for producing a biodegradable implant |
| WO2019164828A1 (en) | 2018-02-20 | 2019-08-29 | Thixomat, Inc. | Improved magnesium alloy and process for making the same |
| EP3530766A4 (en) * | 2016-10-21 | 2019-09-25 | Posco | Highly molded magnesium alloy sheet and method for manufacturing same |
Families Citing this family (11)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| WO2017035072A1 (en) * | 2015-08-21 | 2017-03-02 | University Of Pittsburgh-Of The Commonwealth System Of Higher Education | Degradable magnesium-based implant devices for bone fixation |
| WO2018083998A1 (en) * | 2016-11-02 | 2018-05-11 | 国立大学法人 熊本大学 | Bioabsorbable medical device and method for producing same |
| JP6644303B2 (en) | 2017-01-10 | 2020-02-12 | 不二ライトメタル株式会社 | Magnesium alloy |
| WO2019172047A1 (en) * | 2018-03-03 | 2019-09-12 | 国立研究開発法人物質・材料研究機構 | Aging treated magnesium alloy material and method for producing same |
| CN114686739A (en) * | 2018-07-09 | 2022-07-01 | 株式会社日本医疗机器技研 | Magnesium alloy |
| JP2021019933A (en) * | 2019-07-29 | 2021-02-18 | グンゼ株式会社 | Intervertebral spacer kit |
| CN114867877A (en) * | 2019-12-02 | 2022-08-05 | 新加坡国立大学 | Biodegradable magnesium alloy |
| EP4215222A1 (en) * | 2020-11-04 | 2023-07-26 | Korea Institute Of Materials Science | High-strength, high-anticorrosive, biodegradable magnesium alloy and implant using same |
| US20220354489A1 (en) | 2021-05-10 | 2022-11-10 | Cilag Gmbh International | Absorbable staple comprising strain limiting features |
| CN114318187B (en) * | 2021-12-08 | 2022-08-05 | 中国科学院金属研究所 | Biomedical high-purity high-strength corrosion-resistant Mg-Zn-Mn magnesium alloy wire and preparation method thereof |
| CN114344550A (en) * | 2022-01-19 | 2022-04-15 | 常熟致圆微管技术有限公司 | Biodegradable medical metal magnesium and magnesium alloy medical suture and preparation method thereof |
Citations (5)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| CN101392344A (en) * | 2008-11-06 | 2009-03-25 | 上海交通大学 | Degradable Mg-Mn-Zn-Ca mulit-element magnesium alloy material in organism |
| US20090131540A1 (en) * | 2006-03-20 | 2009-05-21 | National Institute For Materials Science | Biodegradable Magnesium Based Metallic Material for Medical Use |
| CN101629260A (en) | 2008-07-18 | 2010-01-20 | 中国科学院金属研究所 | Medical absorbable Mg-Zn-Mn-Ca magnesium alloy |
| US20120269673A1 (en) * | 2009-12-07 | 2012-10-25 | Ja-Kyo Koo | Magnesium alloy |
| US20120305145A1 (en) * | 2010-02-05 | 2012-12-06 | Decker Raymond F | Method and apparatus of forming a wrought material having a refined grain structure |
Family Cites Families (12)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| KR100789632B1 (en) * | 2001-07-05 | 2007-12-27 | 주식회사 엘지생활건강 | Cosmetic for skin whitening containing a herb extract with inhibitory activity of melanin formation |
| KR100509648B1 (en) * | 2003-05-23 | 2005-08-24 | 연우인더스트리(주) | High formability the Magnesium alloy and manufacture method of the Magnesium alloy product thereof |
| JP2006061381A (en) * | 2004-08-26 | 2006-03-09 | Terumo Corp | Intravascular implant |
| DE102005060203B4 (en) * | 2005-12-14 | 2009-11-12 | Gkss-Forschungszentrum Geesthacht Gmbh | Biocompatible magnesium material, process for its preparation and its use |
| JP5053668B2 (en) * | 2007-03-15 | 2012-10-17 | テルモ株式会社 | Stent |
| DE102007061647A1 (en) * | 2007-12-20 | 2009-07-02 | Biotronik Vi Patent Ag | Implant with a body made of a biocorrodible alloy |
| US8801778B2 (en) * | 2007-12-20 | 2014-08-12 | Biotronik Vi Patent Ag | Implant with a base body of a biocorrodible alloy |
| US20090196787A1 (en) * | 2008-01-31 | 2009-08-06 | Beals Randy S | Magnesium alloy |
| CN101575682A (en) | 2009-06-04 | 2009-11-11 | 重庆大学 | Degradable biomedical complex magnesium alloy |
| AT510087B1 (en) * | 2010-07-06 | 2012-05-15 | Ait Austrian Institute Of Technology Gmbh | MAGNESIUM ALLOY |
| JP5720926B2 (en) * | 2010-10-12 | 2015-05-20 | 住友電気工業株式会社 | Magnesium alloy wire, bolt, nut and washer |
| EP2956180B1 (en) * | 2013-02-15 | 2018-08-01 | Boston Scientific Scimed, Inc. | Bioerodible magnesium alloy microstructures for endoprostheses |
-
2014
- 2014-03-17 KR KR1020157029685A patent/KR102246635B1/en active IP Right Grant
- 2014-03-17 ES ES14765401T patent/ES2817048T3/en active Active
- 2014-03-17 JP JP2016503407A patent/JP6532858B2/en active Active
- 2014-03-17 CN CN201480022585.5A patent/CN105120907B/en active Active
- 2014-03-17 AU AU2014232750A patent/AU2014232750B2/en active Active
- 2014-03-17 WO PCT/US2014/030477 patent/WO2014145672A1/en active Application Filing
- 2014-03-17 US US14/777,159 patent/US10022470B2/en active Active
- 2014-03-17 CA CA2906876A patent/CA2906876C/en active Active
- 2014-03-17 BR BR112015023628A patent/BR112015023628B1/en active IP Right Grant
- 2014-03-17 EP EP14765401.6A patent/EP2968656B1/en active Active
-
2015
- 2015-09-16 IL IL241608A patent/IL241608B/en active IP Right Grant
-
2016
- 2016-06-02 HK HK16106289.9A patent/HK1218265A1/en unknown
Patent Citations (5)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US20090131540A1 (en) * | 2006-03-20 | 2009-05-21 | National Institute For Materials Science | Biodegradable Magnesium Based Metallic Material for Medical Use |
| CN101629260A (en) | 2008-07-18 | 2010-01-20 | 中国科学院金属研究所 | Medical absorbable Mg-Zn-Mn-Ca magnesium alloy |
| CN101392344A (en) * | 2008-11-06 | 2009-03-25 | 上海交通大学 | Degradable Mg-Mn-Zn-Ca mulit-element magnesium alloy material in organism |
| US20120269673A1 (en) * | 2009-12-07 | 2012-10-25 | Ja-Kyo Koo | Magnesium alloy |
| US20120305145A1 (en) * | 2010-02-05 | 2012-12-06 | Decker Raymond F | Method and apparatus of forming a wrought material having a refined grain structure |
Non-Patent Citations (1)
| Title |
|---|
| See also references of EP2968656A4 |
Cited By (9)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| CN106148784A (en) * | 2015-04-20 | 2016-11-23 | 中国科学院金属研究所 | A kind of low cost room temperature high-ductility wrought magnesium alloy material and preparation technology thereof |
| CN106148784B (en) * | 2015-04-20 | 2019-03-19 | 中国科学院金属研究所 | A kind of low cost room temperature high-ductility wrought magnesium alloy material and its preparation process |
| WO2017112779A1 (en) * | 2015-12-21 | 2017-06-29 | The University Of Toledo | Process to produce high-strength and corrosion resistant alloy for patient-specific bioresorbable bone fixation implants and hardware |
| EP3530766A4 (en) * | 2016-10-21 | 2019-09-25 | Posco | Highly molded magnesium alloy sheet and method for manufacturing same |
| WO2019002277A1 (en) | 2017-06-27 | 2019-01-03 | Aap Implantate Ag | Magnesium alloy, biodegradable implant and method for producing a biodegradable implant |
| US20200123636A1 (en) * | 2017-06-27 | 2020-04-23 | Aap Implantate Ag | Magnesium alloy, biodegradable implant and method for producing a biodegradable implant |
| WO2019164828A1 (en) | 2018-02-20 | 2019-08-29 | Thixomat, Inc. | Improved magnesium alloy and process for making the same |
| JP2021514426A (en) * | 2018-02-20 | 2021-06-10 | チキソマット,インコーポレイテッド | Improved magnesium alloy and its manufacturing method |
| EP3755822A4 (en) * | 2018-02-20 | 2021-11-24 | Thixomat, Inc. | Improved magnesium alloy and process for making the same |
Also Published As
| Publication number | Publication date |
|---|---|
| HK1218265A1 (en) | 2017-02-10 |
| BR112015023628A2 (en) | 2017-07-18 |
| ES2817048T3 (en) | 2021-04-06 |
| IL241608B (en) | 2020-10-29 |
| BR112015023628B1 (en) | 2020-04-22 |
| AU2014232750B2 (en) | 2017-10-26 |
| JP6532858B2 (en) | 2019-06-19 |
| JP2016521312A (en) | 2016-07-21 |
| CA2906876A1 (en) | 2014-09-18 |
| KR102246635B1 (en) | 2021-04-30 |
| US10022470B2 (en) | 2018-07-17 |
| US20160022863A1 (en) | 2016-01-28 |
| AU2014232750A1 (en) | 2015-10-22 |
| EP2968656B1 (en) | 2020-06-24 |
| EP2968656A4 (en) | 2017-01-04 |
| KR20150133773A (en) | 2015-11-30 |
| CN105120907B (en) | 2018-03-30 |
| CA2906876C (en) | 2021-04-06 |
| CN105120907A (en) | 2015-12-02 |
| EP2968656A1 (en) | 2016-01-20 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| AU2014232750B2 (en) | High strength and bio-absorbable magnesium alloys | |
| US10196715B2 (en) | Magnesium alloy with adjustable degradation rate | |
| JP6840716B2 (en) | Magnesium alloy with adjustable decomposition rate | |
| Pogorielov et al. | Magnesium-based biodegradable alloys: Degradation, application, and alloying elements | |
| US10213522B2 (en) | Ultrapure magnesium alloy with adjustable degradation rate | |
| US11696976B2 (en) | Degradable magnesium-based implant devices for bone fixation | |
| Bordbar-Khiabani et al. | Emerging magnesium-based biomaterials for orthopedic implantation | |
| Niranjan et al. | Magnesium alloys as extremely promising alternatives for temporary orthopedic implants–A review | |
| Barfield et al. | The potential of magnesium alloy use in orthopaedic surgery | |
| US20230313346A1 (en) | Properties and parameters of novel biodegradable metallic alloys | |
| US11351290B1 (en) | Absorbable high-strength zinc alloy for medical implants | |
| Hong | Fundamental Study of the Design and Development of Magnesium-Zinc Based Alloys for Biodegradable Implant Devices |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| WWE | Wipo information: entry into national phase |
Ref document number: 201480022585.5 Country of ref document: CN |
|
| 121 | Ep: the epo has been informed by wipo that ep was designated in this application |
Ref document number: 14765401 Country of ref document: EP Kind code of ref document: A1 |
|
| ENP | Entry into the national phase |
Ref document number: 2906876 Country of ref document: CA Ref document number: 2016503407 Country of ref document: JP Kind code of ref document: A |
|
| NENP | Non-entry into the national phase |
Ref country code: DE |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 14777159 Country of ref document: US |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 241608 Country of ref document: IL |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 2014765401 Country of ref document: EP |
|
| ENP | Entry into the national phase |
Ref document number: 20157029685 Country of ref document: KR Kind code of ref document: A |
|
| ENP | Entry into the national phase |
Ref document number: 2014232750 Country of ref document: AU Date of ref document: 20140317 Kind code of ref document: A |
|
| REG | Reference to national code |
Ref country code: BR Ref legal event code: B01A Ref document number: 112015023628 Country of ref document: BR |
|
| ENP | Entry into the national phase |
Ref document number: 112015023628 Country of ref document: BR Kind code of ref document: A2 Effective date: 20150915 |