WO2011064316A2 - Mucosal delivery of peptides - Google Patents
Mucosal delivery of peptides Download PDFInfo
- Publication number
- WO2011064316A2 WO2011064316A2 PCT/EP2010/068257 EP2010068257W WO2011064316A2 WO 2011064316 A2 WO2011064316 A2 WO 2011064316A2 EP 2010068257 W EP2010068257 W EP 2010068257W WO 2011064316 A2 WO2011064316 A2 WO 2011064316A2
- Authority
- WO
- WIPO (PCT)
- Prior art keywords
- peptide
- active agent
- mucosal delivery
- delivery composition
- peptide active
- Prior art date
Links
- 0 *=CC(C*C(C1OC2(*CCOCCOCCOCCOCCOC2)O[C@@]1[C@](O)OCC(CO)O)O)O Chemical compound *=CC(C*C(C1OC2(*CCOCCOCCOCCOCCOC2)O[C@@]1[C@](O)OCC(CO)O)O)O 0.000 description 1
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K9/00—Medicinal preparations characterised by special physical form
- A61K9/0012—Galenical forms characterised by the site of application
- A61K9/0053—Mouth and digestive tract, i.e. intraoral and peroral administration
- A61K9/006—Oral mucosa, e.g. mucoadhesive forms, sublingual droplets; Buccal patches or films; Buccal sprays
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
- A61K38/02—Peptides of undefined number of amino acids; Derivatives thereof
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
- A61K38/16—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof
- A61K38/17—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof from animals; from humans
- A61K38/22—Hormones
- A61K38/26—Glucagons
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K47/00—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient
- A61K47/06—Organic compounds, e.g. natural or synthetic hydrocarbons, polyolefins, mineral oil, petrolatum or ozokerite
- A61K47/22—Heterocyclic compounds, e.g. ascorbic acid, tocopherol or pyrrolidones
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K47/00—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient
- A61K47/50—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient the non-active ingredient being chemically bound to the active ingredient, e.g. polymer-drug conjugates
- A61K47/51—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient the non-active ingredient being chemically bound to the active ingredient, e.g. polymer-drug conjugates the non-active ingredient being a modifying agent
- A61K47/54—Medicinal preparations characterised by the non-active ingredients used, e.g. carriers or inert additives; Targeting or modifying agents chemically bound to the active ingredient the non-active ingredient being chemically bound to the active ingredient, e.g. polymer-drug conjugates the non-active ingredient being a modifying agent the modifying agent being an organic compound
- A61K47/545—Heterocyclic compounds
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K9/00—Medicinal preparations characterised by special physical form
- A61K9/10—Dispersions; Emulsions
- A61K9/12—Aerosols; Foams
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P3/00—Drugs for disorders of the metabolism
- A61P3/04—Anorexiants; Antiobesity agents
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P3/00—Drugs for disorders of the metabolism
- A61P3/08—Drugs for disorders of the metabolism for glucose homeostasis
- A61P3/10—Drugs for disorders of the metabolism for glucose homeostasis for hyperglycaemia, e.g. antidiabetics
Definitions
- the disclosure relates to compositions and methods for mucosal delivery of peptides, particularly oral mucosal delivery for absorption through oral mucosal membranes.
- Peptide-based drugs are typically delivered by injection, since oral delivery by ingestion is often hindered by poor intrinsic permeability and degradation in the gastrointestinal (Gl) tract. Nevertheless, the potential therapeutic benefit remains significant, including ease of use and better overall patient compliance.
- Mucosal delivery of peptides into the blood stream of a host across various mucosal membranes, such as found in the Gl tract, lung, nasal cavity and oral cavity, is possible for a number of peptides and peptide formulations.
- the fraction of an administered dose of unchanged peptide that reaches the systemic circulation normally varies depending on the particular route of delivery, peptide and formulation.
- the non-invasive delivery of peptide drugs by mucosal routes offers significant flexibility.
- delivery of drugs via oral mucosa provides direct access to the systemic circulation through the internal jugular vein, allowing them to bypass the gut and hepatic first-pass metabolism, and enter the bloodstream for rapid on-set of effect.
- the mucosal lining in the oral cavity represents a promising topical route for the delivery of large therapeutic molecules such as insulin, interferons, and inter!eukins (Visse et al. , Eur. J. Pharm. Biopharm. (2001 ) 51 :93-109; and Sudhakar et al., J. Control. Release (2006) 1 14: 1 5-40; and Amin ef al., Drug Delivery Technology (2007) 7(3) 48, 50-55).
- mucoadhesive dosage forms also have been reported to increase resident time of the delivery system in the oral cavity (Ishida et al., Chem. Pharm. Bull. (1981 ) 29:810-816; and Senel et al., Curr. Pharm. Biotechnol. (2001 ) 2:175-186), including, for example, pelleted mucoadhesive polymeric nanoparticles (Venugopalan et al., Pharmazie (2001 ) 56:217-219), and mucoadhesive tablets (Hosny et al., Boll. Chim. Farm. (2002) 141 :210- 217).
- Mucosal dosage forms employing various solvents have also been reported, such as insulin with soybean lecithin and propanediol (Xu et al., Pharmacol. Res. (2002) 46:459 ⁇ 467), and buccal aerosol sprays and capsules using non-polar solvent (U.S. Patent No. 5,955,098).
- Pulmonary delivery formulations of a solution or suspension of various organic solvents have been reported, for example, where the solvent is a class 3 residual solvent such as ethanol, acetone, ethyl acetate, tetrahydofuran, ethyl ether, and propanol (US 6,660,715).
- mucosal delivery systems often include absorption enhancing formulations that exhibit side effects, such as causing irritation of the various mucosal linings in the mouth or airways.
- absorption enhancing formulations that exhibit side effects, such as causing irritation of the various mucosal linings in the mouth or airways.
- Another problem is the repugnant taste of many compositions, particularly for bile salts, pointing to likely issues with patient acceptance and compliance.
- a different issue relates to the volume required for delivering a sufficient amount of an active peptide ingredient for biological effect, storage stability, and reproducibility.
- compositions and methods for administering peptides that are stable, well tolerated, provide enhanced and reliable mucosal delivery, particularly oral mucosal delivery, and suitable for treatment of diseases and other adverse conditions in mammalian subjects.
- a related need exists for methods and compositions that provide efficient delivery of larger drugs such as peptides via one or more mucosal routes in therapeutic amounts, which are fast acting, easily administered, have limited adverse side effects such as mucosal irritation or tissue damage, and reproducible.
- non-aqueous pharmaceutical and diagnostic compositions of peptides which have improved stability.
- An additional need relates to the manufacture of such materials, and compositions for the same. The present disclosure addresses these and other needs.
- compositions and methods related to mucosal delivery of peptide active agents include an effective amount of a stably hydrated peptide active agent complexed with a crown compound and/or a counter ion solubilized in a non-aqueous hydrophobic vehicle at a pH different from the isoelectric point of the peptide active agent.
- compositions that include a preformed peptide complex comprising a stably hydrated peptide active agent complexed with a crown compound and/or a counter ion, wherein the performed peptide complex is dried from a solution or suspension having a pH different, optionally remote, from the isoelectric point of the peptide active agent.
- Additional compositions include an effective amount of a stably hydrated peptide active agent complexed with a counter ion solubilized in a nonaqueous hydrophobic vehicle at a pH different from the isoelectric point of the peptide active agent, wherein the stably hydrated peptide active agent complexed with a counter ion is dried from a solution or suspension having a pH different, optionally remote, from the isoelectric point of the peptide active agent, and wherein the non-aqueous hydrophobic vehicle in many embodiments comprises at least one acylglycerol and at least one organic solvent and/or lipid. Further provided are pharmaceutical and/or diagnostic preparations of the subject compositions.
- the method comprises forming a soluble peptide complex in a non-aqueous hydrophobic vehicle at a pH different from the isoelectric point of the peptide active agent, the peptide complex comprising an effective amount of a stably hydrated peptide active agent complexed with a crown compound and a counter ion.
- a method for production of a preformed peptide complex comprising a stably hydrated peptide active agent complexed with a crown compound and a counter ion, the method involving (i) forming the peptide complex in a solution or suspension having a pH different, optionally remote, from the isoelectric point of the peptide active agent, and (ii) drying the peptide complex from the solution or suspension under conditions that retain a sufficient amount of water in association with the peptide active agent to stabilize the peptide active agent, whereby the preformed peptide complex is produced.
- Another method involves solubilizing an effective amount of a stably hydrated peptide active agent compiexed with a counter ion in a non-aqueous hydrophobic vehicle at a pH different from the isoelectric point of the peptide active agent, wherein the stably hydrated peptide active agent compiexed with a counter ion is dried from a solution or suspension having a pH different, optionally remote, from the isoelectric point of the peptide active agent, and wherein the non-aqueous hydrophobic vehicle in many embodiments comprises at least one acylglycerol and at least one organic solvent and/or lipid.
- Methods for the mucosal delivery of an effective amount of a peptide active agent to a host in need thereof involve administering to a mucosal membrane of the host an effective amount of a mucosal delivery composition of the disclosure, wherein the administering delivers an effective amount of the peptide active agent into the blood stream of the host.
- the mucosal delivery composition is an oral mucosal delivery composition
- the mucosal membrane is an oral mucosal membrane.
- kits that find use in practicing the subject methods.
- the kit comprises an effective amount of a mucosal delivery composition of the disclosure, and/or components thereof each individually provided in various combinations in the kit in effective amounts capable of forming the mucosal delivery composition upon combination.
- the subject methods and compositions find use in a wide range of different applications, including the treatment of a variety of different disease conditions.
- An exemplary application illustrating a significant advantage of the methods and compositions disclosed herein is the enhanced mucosal delivery of peptides, and in particular, reliably reproducible mucosal delivery imparted by formation and use of a stably hydrated form of the peptide active agent maintained in the peptide complex and non-aqueous hydrophobic vehicle.
- compositions and methods are particularly useful for mucosal delivery of peptide hormones, such as glucagon-like peptide-1 and analogs thereof exemplified by liraglutide and exendin-4 (exenatide) that can affect blood glucose levels in vivo for treatment of diabetes, obesity, and related disorders.
- peptide hormones such as glucagon-like peptide-1 and analogs thereof exemplified by liraglutide and exendin-4 (exenatide) that can affect blood glucose levels in vivo for treatment of diabetes, obesity, and related disorders.
- specific compositions and methods are provided for mucosal delivery of a peptide active agent for treatment of diabetes, obesity, and related disorders.
- Figure 1 depicts a set of results demonstrating the effect of the type of counter ion on sublingual delivery of exendin-4 in a representative mucosal delivery composition, and reduction of glucose levels in mice as measured by intraperitoneal glucose tolerance tests (IPGTT).
- IPGTT intraperitoneal glucose tolerance tests
- Figure 2 depicts a set of results demonstrating the effect of altering vehicle pH on sublingual delivery of exendin-4 in a representative mucosal delivery composition, and reduction of glucose levels in mice as measured by IPGTT.
- Figure 3 depicts a set of results demonstrating the effect of altering the stoicheometric amounts and ratios of crown compound and counter ion to peptide on sublingual delivery of exendin-4 in representative mucosal delivery composition, and reduction of glucose levels in mice as measured by IPGTT.
- Figure 4 depicts a set of results demonstrating the effect of water content and processing conditions on sublingual delivery of exendin-4 in a representative mucosal delivery composition, and reduction of glucose levels in mice as measured by IPGTT.
- amino acid refers to any of the naturally occurring amino acids (e.g. Ala, Arg, Asn, Asp, Cys, Glu, Gin, Gly, His, Hyl, Hyp, lie, Leu, Lys, Met, Phe, Pro, Ser, Thr, Trp, Tyr, and Val) in D, L, or DL form, as well as analogues/derivatives thereof.
- Naturally occurring amino acids e.g. Ala, Arg, Asn, Asp, Cys, Glu, Gin, Gly, His, Hyl, Hyp, lie, Leu, Lys, Met, Phe, Pro, Ser, Thr, Trp, Tyr, and Val
- the side chains of naturally occurring amino acids include, for example, hydrogen (e.g., as in glycine), alkyl (e.g., as in alanine, valine, leucine, isoleucine, proline), substituted alkyl (e.g., as in threonine, serine, methionine, cysteine, aspartic acid, asparagine, glutamic acid, giutamine, arginine, and lysine), alkaryl (e.g., as in phenylalanine and tryptophan), substituted arylalkyl (e.g., as in tyrosine), and heteroarylalkyl (e.g., as in histidine).
- the amino acids includes protected or modified amino acids, such as acylated amino acids, amidated amino acids and the like.
- Analogue or “derivative” refers to without limitation any compound which has a structure derived from the structure of the compounds of the present disclosure and whose structure is sufficiently similar to those disclosed herein and based upon that similarity, would be expected, by one skilled in the art, to exhibit the same or similar activities and utilities as the claimed and/or referenced compounds.
- Bosal mucosa refers to the membrane lining the inner wall of the cheek.
- Charge complexing agent refers to a compound that forms a non- cova!ent complex with an ion, atom or ionizab!e functional group of a molecule, where the complex represents a reversible association of the complexing agent with one or more ions, atoms, or molecules through non- covalent chemical bonds.
- Complexed or charge complex refers to a reversible association of a charge complexing agent such as a crown compound that forms a non- covalent complex with an ion, atom or ionizable functional group of a molecule through non-covalent chemical bonds.
- a charge complexing agent such as a crown compound that forms a non- covalent complex with an ion, atom or ionizable functional group of a molecule through non-covalent chemical bonds.
- the term complexed or charge complex is not confined to salt or metal ions bound to a complexing agent. It relates in general to complexes between a complexing agent and an ion or ionic group on a peptide, particularly a cation or cationic group on a peptide.
- Crown compound refers to macrocyclic polydentate compounds, usually uncharged, in which three or more coordinating ring atoms (usually oxygen or nitrogen) are or may become suitably close for easy formation of chelate complexes with cationic species (excludes planar analogues, such as porphyrins). See for example: M. Hiraoka, Crown Compounds: their Characteristics and Applications, Elsevier Science Publishers, 1982; and E. Weber and F. Vogtle, Inorg. Chim. Acta (1980) 45:L65-L67.
- “Dried peptide” refers to a peptide dried by a process, such as lyophilization, spray drying, centrifugal evaporation, and air drying, and which contains residual water in association with the peptide.
- the dried peptide is typically a powder or residue that can have the appearance of a dry powder, particulate, or residue material, including an oily or moistened residue appearance.
- an “anhydrous peptide” contains essentially no water. See for example, lyophilization (e.g., Williams and Polli (1984) J, Parenteral Sci. Technol.
- Effective means adequate to accomplish a desired, expected, or intended result.
- the term “effective amount” or “pharmaceutically effective amount” as provided herein is intended to mean a non-lethal but sufficient amount of the compound to provide the desired utility.
- the effective amount is the amount which elicits a useful response (e.g., reduction of blood glucose levels below control level, or to provide for a clinically meaningful reduction in blood glucose levels).
- the exact amount required will vary from subject to subject, depending on the species, age, and general condition of the subject, the severity of the condition or disease that is being treated, the particular compound used, its mode of administration, and the like. Thus, it is not possible to specify an exact "effective amount.” However, an appropriate effective amount may be determined by one of ordinary skill in the art using only routine experimentation.
- “lonizable functional group” refers to a group on an amino acid of a peptide capable of donating or accepting a charge at a pH different from the group's pKa.
- Mucosal delivery refers to application of an active agent (such as a drug) to one or more mucosal membranes of the gastrointestinal tract (Gl), rectum, vagina, lung, nasal cavity, or oral cavity, including buccal (cheek), sublingual (under tongue), lips, gums, palates, and tongue, and passage of the active agent through the membranes covering these places and its entry into the bloodstream.
- an active agent such as a drug
- “Mucosal delivery composition” refers to a drug delivery composition or system capable of mucosal delivery of an active agent.
- Protein refers to a polyamino acid containing up to 2, 5, 10, 20, 30, 40, 50, 75, 100 or about 200 amino acid residues, which can include coded and non-coded amino acids, chemically or biochemically modified or derivatized amino acids, linear, branched or cyclic peptide, and peptides having modified backbones. Sometimes referred to as polypeptide or protein, which may be used interchangeably herein.
- peptides which comprise one or more non-naturally occurring amino acids such as beta-aianine, aipha-amino butyric acid, gamma-amino butyric acid, alpha- amino isobutyric acid, norva!ine, norleucsne, ornithine, homoserine and hydroxyproline.
- peptides in which reactive groups are modified such as the N- and C-terminus of a peptide may be chemically modified by various labeling agents, polymers such as polyethylene glycol, lipids, carbohydrates and the like, blocked by protecting groups, and the like, as well as those bearing biological modifications, such as post-translational modifications.
- “Peptide active agent” refers to a biologically active peptide or an analogue/derivative thereof, including pharmaceutically acceptable salts, solvates, hydrates, and prodrug forms thereof.
- Percent solubility value refers to the equilibrium solubility limit or maximum solubility of a molecule in a solvent or solvent system at usual room temperature, expressed as the weight percent of the molecule in the composition.
- Permeability-enhancing lipid refers to charged or neutral hydrophobic or amphiphilic small molecules that may be either solid or liquid at normal room temperature, depending on their structure and composition, may be saturated or unsaturated, branched or linear, and are capable of enhancing the permeability of mucosal membranes to absorption of peptides.
- fat-soluble vitamins such as vitamins A, D, E and K
- monoglycerides such as vitamins A, D, E and K
- diglycerides diglycerides
- phospholipids such as oleic acid
- sterols such as cholesterol
- phospholipids such as phosphatidylcholine, and the like.
- permeability-enhancing fatty acid refers to aliphatic carboxylic acids that may be saturated or unsaturated, branched or linear, and are capable of enhancing the permeability of mucosal membranes to absorption of peptides.
- Oral mucosal delivery refers to application of an active agent (such as a drug) to one or more mucosal membranes of the oral cavity, including buccal (cheek), sublingual (under tongue), Hps, gums, palates, and tongue, and passage of the active agent through the membranes covering these places and its entry into the bloodstream.
- an active agent such as a drug
- Oral mucosal delivery vehicle refers to a drug delivery system capable of oral mucosal delivery of an active agent.
- solute refers to the interaction of a solute, such as a peptide, with a solvent, such as an aqueous, organic, or an aqueous organic solution, which leads to stabilization of the solute in the solvent.
- solvent such as an aqueous, organic, or an aqueous organic solution
- solubility refers to the dynamic equilibrium state achieved when the rate of dissolution equals the rate of precipitation. The extent of the solubility of a substance in a specific solvent is measured as the saturation
- “Stably hydrated peptide active agent” refers to a peptide active agent having a water content by weight and solubility in an organic or aqueous organic solvent comparable to or greater than the dried peptide active agent, and is essentially non-aggregated and unoxidized.
- Sublingual mucosa refers to the membrane that includes the ventral surface of the tongue and the floor of the mouth.
- pharmaceutically acceptable refers to a material that is not biologically or otherwise undesirable, i.e., the material is of a medically acceptable quality and composition that may be administered to an individual along with the selected active pharmaceutical ingredient without causing any undesirable biological effects or interacting in a deleterious manner with any of the other components of the pharmaceutical composition in which it is contained.
- compositions and methods of their preparation for mucosal delivery of peptide active agents are also provided. Also provided are kits and methods of use of the subject compositions.
- compositions include a mucosal delivery composition that comprises an effective amount of a peptide complex or a peptide salt solubilized in a non-aqueous hydrophobic vehicle.
- the peptide complex includes a stably hydrated peptide active agent complexed with a crown compound and/or a counter ion, and is solubilized in the non-aqueous hydrophobic vehicle at a pH different from the pi of the peptide active agent.
- the peptide salt includes a stably hydrated peptide active agent complexed with a counter ion, and is solubilized in the non-aqueous hydrophobic vehicle at a pH different from the p/ of the peptide active agent.
- the non-aqueous hydrophobic vehicle comprises at least one acylglycerol, and at least one organic solvent and/or lipid each individually present in an amount effective to (i) soiubilize the peptide complex or peptide salt, and (ii) enhance mucosa! delivery of the peptide active agent.
- the mucosal delivery composition generally includes various solubilizing agents in non-aqueous medium, such as a medium comprising an acylglycerol and an organic solvent and/or a lipid (as described in greater detail below).
- the mucosal delivery composition and components thereof may also include one or more additional pharmaceutically acceptable excipients, such as one or more of an non-ionic surfactant, antioxidant, buffer, preservative, and the like (as described in greater detail below).
- the peptide complex or the peptide salt is preformed, wherein the preformed peptide complex or preformed peptide salt is dried from a solution or suspension having a pH different, optionally remote, from the p/ of the peptide active agent.
- the nonaqueous hydrophobic vehicle is preformed.
- the preformed non-aqueous hydrophobic vehicle is dried from a solution or suspension having a pH different, optionally remote, from the isoelectric point of the peptide active agent.
- the mucosal delivery composition is dried from a solution or suspension having a pH different, optionally remote, from the isoelectric point of the peptide active agent.
- the solution or suspension is an aqueous organic mixture.
- further embodiments are directed to a composition comprising one or more of the preformed peptide complex, the preformed peptide salt, the preformed non-aqueous hydrophobic vehicle, and combinations thereof.
- a method of producing a mucosal delivery composition comprising: forming a peptide complex or peptide salt dispersed in a non-aqueous hydrophobic vehicle at a pH different from the pi of the peptide active agent, the peptide complex comprising an effective amount of a stably hydrated peptide active agent complexed with a crown compound and a counter ion, the peptide salt comprising an effective amount of a stably hydrated peptide active agent complexed with a counter ion.
- a featured embodiment is where the peptide complex or peptide salt is solubilized at a pH different from the p/ of the peptide active agent in the nonaqueous hydrophobic vehicle.
- the forming step of the subject method comprises combining an effective amount of each component (or any effective combination thereof) of the desired mucosal delivery composition (i.e., combining an effective amount of components comprising the stably hydrated peptide active agent, the crown compound, the counter ion, and the non-aqueous hydrophobic vehicle for mucosal delivery compositions in which a crown compound is included, or combining an effective amount of the components comprising the stably hydrated peptide active agent, the counter ion, and the non-aqueous hydrophobic vehicle for mucosal delivery compositions in which a crown compound is absent).
- the forming step of the subject method comprises combining an effective amount of (i) a first composition comprising the non-aqueous hydrophobic vehicle, and (ii) a second composition comprising the peptide complex or the peptide salt.
- the forming step of the subject method comprises combining an effective amount of (i) a first composition comprising the nonaqueous hydrophobic vehicle and the peptide salt, and (ii) a second composition comprising a crown compound.
- the peptide complex or peptide salt in many embodiments is comprised as a dried powder or residue obtainable by drying a solution or suspension, the solution or suspension comprising as components therein: (i) the peptide active agent, the crown compound, and the counter ion for forming the peptide complex, or (ii) the peptide active agent, and the counter ion for forming the peptide salt; and wherein the drying is under conditions that retain a sufficient amount of water in association with the peptide active agent to produce the peptide complex or peptide salt.
- the solution or suspension is at pH different, optionally remote, from the isoelectric point of the peptide active agent.
- the solution or suspension is an aqueous organic solution or suspension.
- the peptide complex and/or the peptide salt is preformed as a dried powder or residue.
- a featured aspect is where one or more of the dried powder or residue comprising the peptide complex, the peptide salt, the peptide active agent, the crown compound, and/or the counter ion is soluble in the aqueous organic solution or suspension.
- a specific embodiment is where the dried powder or residue comprising the peptide complex, or the peptide salt is soluble in the aqueous organic solution or suspension.
- step (b) combining the preformed peptide salt of step (a) with a second composition comprising a non-aqueous hydrophobic vehicle to form the mucosal delivery composition;
- step (c) combining the preformed peptide salt of step (a) with a second composition comprising a non-aqueous hydrophobic vehicle and a crown compound to form the mucosal delivery composition; or
- step (d) combining the preformed peptide salt of step (a) with a second composition comprising a crown compound in an organic or aqueous organic solution or suspension, and (i) drying the organic or aqueous organic solution or suspension to form a preformed peptide complex under conditions that retain a sufficient amount of water in association with the peptide to maintain solvation and stability of the peptide active agent; and (ii) combining the preformed peptide complex with the non-aqueous hydrophobic vehicle to form the mucosal delivery composition.
- Methods are also provided for production of a preformed peptide complex and/or a preformed peptide salt, such as described above.
- the method involves (i) providing an aqueous organic solution or suspension comprising as components therein a peptide active agent, a crown compound, and a counter son, and (ii) drying the aqueous organic solution or suspension under conditions that retain a sufficient amount of water in association with the peptide active agent to produce the peptide complex.
- the aqueous organic solution or suspension is at a pH different, optionally remote, from the pi of the peptide active agent.
- the method involves administering to a mucosal membrane of the host an effective amount of a mucosal delivery composition of the disclosure, wherein the administering delivers an effective amount of the peptide active agent into the blood stream of the host.
- kits that find use in practicing the subject methods.
- the mucosal delivery compositions and its components are generally non-toxic and non-irritating, and facilitate enhanced and reliably reproducible mucosal delivery of the stably peptide active agent into the blood stream of the host, relative to the non-stably hydrated peptide active agent.
- the subject compositions may be administered alone or as part of a drug delivery system for delivery to one or more mucosal membranes of a host, such as administration to the oral cavity of a host for oral mucosal delivery through an oral mucosal membrane, such as a buccal membrane, sublingual membrane, or both buccal and sublingual membranes.
- the compositions can be provided in a free form, such as a liquid, gel, foam, cream, ointment, semisolid, or spray, or can comprise a device of determined physical form, such as tablets, patches, films, and troches.
- compositions and methods find use in a variety of different applications, including the treatment of a range of different disease conditions for which a given peptide active agent is indicated.
- An exemplary application illustrating a significant advantage of the methods and compositions of the disclosure is the effective and reliably reproducible oral mucosal delivery of peptide hormones such as insulin and incretin mimetic peptides that alter blood giucose levels in vivo for treatment of diabetes, obesity, and related disorders.
- the subject compositions and methods represent an important advance over the prior art.
- a significant problem overcome by the present disclosure is the reliable and reproducible mucosal delivery of peptide active agents, among other aspects.
- the present disclosure is based in part on the discovery that a remarkable improvement in the mucosal delivery of peptides can be achieved by providing a mucosal delivery composition comprising an effective amount of a stably hydrated peptide active agent complexed with a crown compound and a counter ion solubilized in a non-aqueous hydrophobic vehicle at a pH different from the isoelectric point (p/) of the peptide active agent.
- the stably hydrated peptide active agent complexed with a crown compound and a counter ion also referred to herein as the peptide complex, is readily prepared in situ in the non-aqueous hydrophobic vehicle or pre-formed ex situ, with the proviso that the peptide active agent is processed under conditions that retain a sufficient amount of water in association with the peptide to maintain solvation and stability of the peptide active agent.
- the peptide complex is prepared ex situ as a preformed peptide complex, and then combined with the non-aqueous hydrophobic vehicle.
- the peptide complex is prepared in situ in the non-aqueous hydrophobic vehicle, for example, by combining (i) a crown compound with (ii) a non-aqueous hydrophobic vehicle comprising the stably hydrated peptide active agent in complex with a counter ion as a peptide salt, with the proviso that the peptide active agent is processed under conditions that retain a sufficient amount of water in association with the peptide to maintain solvation and stability of the peptide active agent.
- the present disclosure is also based in part on the finding that a significant improvement in solubility of the peptide complex or peptide salt in a non-aqueous hydrophobic vehicle can be achieved when the peptide complex or peptide salt is dried from a solution or suspension at a pH different, optionally remote, from the pi of the peptide active agent.
- the mucosal delivery composition can be readily prepared in situ or ex situ utilizing such a dried peptide complex or peptide salt, with the proviso that the peptide active agent is processed under conditions that retain a sufficient amount of water in association with the peptide to maintain solvation and stability of the peptide active agent.
- the mucosal delivery composition is formed by an in situ or ex situ process as described above, reliable and reproducible mucosal delivery of the peptide active agent strongly depends on the conditions under which the composition is prepared.
- the following process of the disclosure illustrates this point, and can be characterized as involving two basic steps.
- the peptide active agent is generally provided as a performed salt that is dried (e.g., by lyophilization or spray drying) from an aqueous or aqueous organic solution or suspension (e.g., water, water/acetonitrile mixtures) having a pH different, optionally remote, from the pi of the peptide active agent.
- an aqueous or aqueous organic solution or suspension e.g., water, water/acetonitrile mixtures having a pH different, optionally remote, from the pi of the peptide active agent.
- this step is readily employed whether the preformed salt is utilized straight from purification (e.g., HPLC using water/acetonitrile mixtures in the presence of desired counter ion, such as acetic acid) or prepared from a precursor peptide salt (e.g., peptide trifluoroacetic acid) that is subjected to desalting and counter ion exchange when a different counter ion is desired (e.g., peptide salicylic acid).
- purification e.g., HPLC using water/acetonitrile mixtures in the presence of desired counter ion, such as acetic acid
- a precursor peptide salt e.g., peptide trifluoroacetic acid
- aqueous or aqueous organic solutions or suspensions e.g., water, water/acetonitrile mixtures
- the desired preformed peptide salt is eventually dried (e.g., by concentrating as a residue by centrifugal evaporation / SpeedVac, lyophilization or spray drying) from a solution or suspension having a pH different, optionally remote, from the pi of the peptide active agent, to form the desired preformed peptide salt.
- care is taken so that the peptide active agent is processed under conditions that retain a sufficient amount of water in association with the peptide to maintain solvation and stability of the peptide active agent.
- the mucosal delivery composition is then formed by either: (i) combining the dried preformed peptide salt of the first step with a crown compound (or without a crown compound in certain embodiments) and the non-aqueous hydrophobic vehicle to form the mucosal delivery composition; or (ii) (a) combining the dried preformed peptide salt of the first step with the crown compound in an organic or aqueous organic solution or suspension (e.g., methanol, water/methanol mixtures), (b) drying the organic or aqueous organic solution or suspension of step (ii)(b) (e.g., by concentrating as a residue in a centrifugal evaporator / SpeedVac), and then (c) combining the dried peptide material of step (ii)(b) (which comprises the preformed peptide complex) with the non-aqueous hydrophobic vehicle to form the mucosal delivery composition.
- care is taken so that the peptide active agent is processed under conditions
- an effective amount of one or more stabilizing excipients and/or water is optionally added to the dried peptide salt before, during, and/or after complexation with the crown compound in an amount that maintains solvation and stability of the peptide active agent.
- water can be combined with and used to first dissolve the preformed peptide salt, followed by the addition of a solvent mixture such as methanol and crown compound to aid in forming and/or maintaining the stably hydrated peptide during complexation (e.g., water added such that the final water concentration in the water-solvent mixture is in a range from 0.5%-50%, more preferably about 1 %-35%, often about 5%-25%, and typically about 10-15%, followed by drying to remove solvent).
- a solvent mixture such as methanol and crown compound
- Water also may be optionally combined with the peptide complex prior to and/or in conjunction with its combination with the non-aqueous hydrophobic vehicle (e.g., water added to the dried peptide complex prior to combination with the non-aqueous hydrophobic vehicle such that the final water concentration in the formulation mixture is about 0.1 %- 10%, usually about 0.5%-5%, and typically about 1 %-3%, with the proviso that the amount of water added is about or less than the amount capable of inducing unwanted phase separation of the formulation components).
- the non-aqueous hydrophobic vehicle e.g., water added to the dried peptide complex prior to combination with the non-aqueous hydrophobic vehicle such that the final water concentration in the formulation mixture is about 0.1 %- 10%, usually about 0.5%-5%, and typically about 1 %-3%, with the proviso that the amount of water added is about or less than the amount capable of inducing unwanted phase separation of the formulation components.
- an effective amount of one or more stabilizing excipients may be included in one or more steps of preparing the preformed peptide salt and/or peptide complex, such as in the counter ion exchange process before, during, and/or after drying, to aid in maintaining the stably hydrated peptide (e.g., a non-ionic detergent such as beta-D-octylglucoside, a tonicity modifying agent such as a mannitol, and the like). Additional water and/or one or more stabilizing excipients may be combined in the final mucosal delivery formulation as well in an amount sufficient to maintain solvation and stability of the peptide active agent.
- a non-ionic detergent such as beta-D-octylglucoside
- a tonicity modifying agent such as a mannitol, and the like.
- Additional water and/or one or more stabilizing excipients may be combined in the final mucosal delivery formulation as well in an amount sufficient to maintain solv
- the stably hydrated peptide active agent (alone or in complex with a crown compound and/or counter ion) is readily prepared by drying the desired peptide material from a solution or suspension at a pH different, optionally remote, from the p/ of the peptide active agent, with the proviso that the peptide active agent is processed under conditions that retain a sufficient amount of water in association with the peptide to maintain solvation and stability of the peptide.
- the solution or suspension can be aqueous, organic, or mixtures thereof.
- the resultant dried peptide material (e.g., peptide alone, peptide salt, or peptide complex) can be stored for later use, and/or further processed, such as combined as above with one or more of the remaining components of the mucosal delivery composition.
- the pH range of the solution or suspension from which the peptide material is dried may overlap with the p/ of the stably hydrated peptide active agent, in general, the farther away the solution or suspension's midpoint pH is from the peptide's pi, the higher the dried peptide's solubility when subsequently combined with other solvents, particularly organics and aqueous mixtures thereof, as well as the non-aqueous hydrophobic vehicle.
- the pH of the solution or suspension from which the peptide material is dried is greater than about 0.2, 0.3, 0.4, or 0.5 pH units from the pi of the peptide active agent, usually greater than about 0.6, 0.7, 0.8, or 0.9 pH units from the pi of the peptide active agent, and more usually about 1 pH unit or greater from the pi of the peptide active agent.
- the peptide active agent can be or lyophilized or dried in a stable form at a pH at which the peptide is highly charged, and in a further embodiment at a pH at which the peptide active agent is mostly charged thus owning the highest possible number of charges.
- the stably hydrated peptide active agent When the stably hydrated peptide active agent is prepared in this manner and formulated with the non-aqueous hydrophobic vehicle without further rounds of solvent exchange and/or drying, the benefit of complexation and the solution or suspension pH from which the peptide material was originally dried can effectively be maintained. However, such benefit can be lost or substantially reduced unless care is taken to maintain stable hydration of the peptide. Specifically, reliable and reproducible mucosal delivery of the peptide active agent is adversely affected if the peptide is not stably hydrated.
- stable hydration when subjecting a stably hydrated peptide active agent to further processing steps involving solvent exchange and drying (e.g., desalting, counter ion exchange, and/or preparing the preformed peptide complex ex situ), stable hydration can be achieved and/or maintained by processing the stably dried peptide active agent in, and drying the resulting peptide material from a solution or suspension at a pH different, optionally remote, from the p/ of the peptide active agent, as described above.
- solvent exchange and drying e.g., desalting, counter ion exchange, and/or preparing the preformed peptide complex ex situ
- the pH of the solution or suspension can be adjusted by the careful addition or acid and/or base to achieve a target pH, typically a target pH in the range of about 0.5 to 8.5, more often from 2.0 to about 8.0, usually about 4.0 to 8.0 (depending on the pi of the peptide active agent), with the optional inclusion of one or more additional pharmaceutically acceptable excipients, such as buffer, isotonic agent, preservative, antioxidant, and the like to aid in the maintenance of the stably hydrated peptide active agent.
- a target pH typically a target pH in the range of about 0.5 to 8.5, more often from 2.0 to about 8.0, usually about 4.0 to 8.0 (depending on the pi of the peptide active agent)
- additional pharmaceutically acceptable excipients such as buffer, isotonic agent, preservative, antioxidant, and the like to aid in the maintenance of the stably hydrated peptide active agent.
- the solution or suspension in which the pH is adjusted is water, and/or acetonitrile/water mixtures, particularly acetonitri!e/water mixtures that contain about 10%-90% acetonitrile, including about 20%-80%, 30%-70%, 40%-60%, and more particularly about 55%-65%, usually about 50:50 mixtures.
- Stabie hydration can also be achieved and/or maintained by processing the stably hydrated peptide active agent, and drying the resulting peptide material from a solution or suspension comprising aqueous, organic, or mixtures thereof, provided drying is carried out under conditions that avoid unwanted water loss, particularly by maintaining appropriate temperature, pressure and drying time (e.g., about or less than 40°C, such as about or less than 35°C, typically about or less than 32°C, for about or less than 3 hours, such as less than 2 hours, more typically less than 1 .5 hours, in a centrifugal evaporator / SpeedVac).
- appropriate temperature, pressure and drying time e.g., about or less than 40°C, such as about or less than 35°C, typically about or less than 32°C, for about or less than 3 hours, such as less than 2 hours, more typically less than 1 .5 hours, in a centrifugal evaporator / SpeedVac.
- one or more additional pharmaceutically acceptable excipients can be added for
- the various processing steps discussed above may employ solutions or suspensions that are aqueous, organic, or mixtures thereof, usually depending on the particular processing step (e.g., water, acetonitrile, methanol, ethanol, aqueous mixtures thereof etc.), or organic solvents alone.
- the solution or suspension is an aqueous alcohol, such as an aqueous methanol or aqueous ethanol, including an aqueous alcohol having a water content of about 1 % to 50% by volume, such as about 1 % to about 25%, particularly about 1 % to 15%, and more particularly about a 2 to 8% aqueous alcohol, such as an aqueous alcohol having a water content of about 5% by volume.
- Aqueous methanol solutions and suspensions are of specific interest, as methanol is the organic solvent closest to water and able to dissolve a very broad range of organic compounds. Additional mixtures are DMSO/Water and Acetonitrile/water.
- the various processing steps discussed above may be employed in any effective combination to produce the desired end composition, for example, in steps involving: (i) optional desalting of the peptide active agent; (ii) optional counter ion exchange of the peptide active agent; and/or (iii) peptide complex formation ex situ and formulation in the non-aqueous hydrophobic vehicle, and/or peptide complex formation in situ in the non-aqueous hydrophobic vehicle; with the proviso that the peptide active agent is processed under conditions that take into consideration the pi of the peptide active agent and retain a sufficient amount of water in association with the peptide to maintain solvation and stability of the peptide.
- mucosal delivery of the peptide active agent can be further improved by other aspects of the disclosure, including choice of the crown compound, counter ion, and amounts thereof, as well as choice of the non-aqueous hydrophobic vehicle, optional excipients and amounts thereof.
- the peptide active agent is complexed with a sufficient amount of a complexing agent, such as a crown and counter ion of interest, which can be present in molar excess of the peptide active agent, generally in a ratio of about 2 to 1 , 5 to 1 , 10 to 1 , 15 to 1 , 20 to 1 , 30 to 1 , 60 to 1 or greater.
- a complexing agent such as a crown and counter ion of interest
- the crown and counter ion components are complexed at a molar ratio dependent on the type and number of ionizable groups present on the peptide active agent.
- the peptide active agent comprises one or more cationic groups (e.g., primary amine, a secondary amine, a guanidinium group, and combinations thereof), the crown compound is a cation-binding crown compound (e.g., a crown ether type compound), and the counter ion is an anionic counter ion (e.g., an acidic counter ion).
- the cation-binding crown compound and the anionic counter ion are each individually present at about 0.5 to 10 stoicheometric equivalents per cationic group, more particularly about 2 to 4 stoicheometric equivalents, and most particularly about 1 to 2 stoicheometric equivalents, per cationic group.
- the cation-binding crown compound is present at about 2 stoicheometric equivalents per primary amine, secondary amine, and/or guanidinium group, and the cationic counter ion is present at about 1 stoicheometric equivalents per primary amine, secondary amine, and/or guanidinium group of the peptide active agent.
- the cationic group is associated with one or more neutralized carboxylates, which cationic group can be derived from inorganic species including but not limited to Na + , K + , Li + , Mg ++ , Ca ++ and the like.
- Another feature in addition to the pi, the peptide hydration, and the crown/counter ion amounts, is the formulation and use of a non-aqueous hydrophobic vehicle having a pH range that stabilizes the peptide complex.
- a non-aqueous hydrophobic vehicle having a pH range that stabilizes the peptide complex can be lost or substantially reduced in mucosal delivery compositions if the pH of the non-aqueous hydrophobic vehicle strays too far out of the margin for maintaining the desired solubility of the peptide complex in the vehicle.
- the pH of the non-aqueous hydrophobic vehicle has a range of about +/-1 to about +/-4 pH units, usually about +/-3 pH units, such as a pH range of about 3-6, about 4-7, about 5-8, and more about usually about +1-2 pH units, such as a pH range of about 3-5, about 4-6, about 5-7, or about 6-8, and the like.
- the final pH range of the non-aqueous hydrophobic vehicle can be adjusted, including by the addition of acid, base, buffer and/or other excipients, as well as by the addition of the peptide salt and/or peptide complex itself depending on the components and amounts in association therewith.
- the pH range of the non-aqueous hydrophobic vehicle may overlap with the pi of the peptide active agent, in general, the farther away the vehicle's midpoint pH is from the peptide's pi, the higher the peptide complex's solubility in the vehicle. Also, by forming the peptide complex either in situ or ex situ at a pH remote from the pi of the peptide active agent, the target pH is readily approached without unnecessarily having to cross over the pi of the peptide active agent upon combination of the material with the vehicle.
- the peptide salt or peptide complex can be prepared ex situ by drying the material from a solution or suspension at a pH greater than 5.0, usually at least 1 pH unit greater, again with the proviso that the peptide active agent is processed under conditions that retain a sufficient amount of water in association with the peptide to maintain solvation and stability of the peptide.
- the pH of the combined mixture can be further adjusted and/or allowed to equilibrate in the composition to achieve solvation.
- compositions such as those comprising a non-aqueous hydrophobic vehicle having at least one acylglycerol and at least one organic solvent and/or lipid, significantly enhance, and in many cases, make possible mucosal delivery of an effective amount of the peptide active agent, among other desirable aspects, including storage stability.
- the non-aqueous hydrophobic vehicle comprises at least one acylglycerol, and at least one organic solvent, and optionally at least one lipid, each individually present in an amount effective to (i) soiubilize the stably hydrated peptide active agent complexed with the crown compound and the counter ion, and (ii) enhance mucosal delivery of the peptide active agent.
- non-aqueous is intended to mean less than about 10% water, more particularly, less than about 5% water.
- the mucosal delivery composition generally includes various solubilizing agents in non-aqueous medium, such as a medium comprising an acylglycerol, and an organic solvent, and optionally a lipid such as a fatty acid or neutral lipid (as described in greater detail below).
- the mucosal delivery composition and components thereof may also include one or more additional pharmaceutically acceptable excipients (as described in greater detail below), such as one or more of a non-ionic surfactant, antioxidant, buffer, viscosity modifier, preservative, isotonic agent, chelating agent, and the like.
- additional pharmaceutically acceptable excipients as one or more of a non-ionic surfactant, antioxidant, buffer, viscosity modifier, preservative, isotonic agent, chelating agent, and the like.
- an effective amount of the stably hydrated peptide active agent complex is solubilized in a mucosal delivery composition, and thus capable of delivering of an effective amount of the peptide active agent into the blood stream of the host when administered to a mucosal membrane thereof.
- mucosal delivery of the peptide active agent as provided in the mucosal delivery compositions of the disclosure is enhanced relative to the peptide active agent that is not stably hydrated.
- the enhancement is greater than about 10%, 20%, 30%, 40%, 50%, 60%, 70%, 80%, or 90%, and usually greater than about 100% (i.e., 1-fold or greater).
- the amount of the peptide active agent that enters the blood stream of a host can be measured qualitatively and/or quantitatively, directly and/or indirectly, by various techniques known in the art, such as by chromatography (e.g., HPLC, Mass-Spectrophotometry etc.), enzymatically (measuring substrate consumption and/or modification, or product and/or byproduct production), antigen-antibody binding (e.g., Western Blot, Enzyme- Linked Immunosorbent Assay (ELISA) etc.), by biological effect (e.g., pharmacological bioavailability by indirect measure of amount of the peptide active agent that enters the blood stream, such as illustrated in the experimental section below), and the like.
- the enhancement can be readily determined.
- the mucosal delivery composition exhibits pharmacological bioavailability of the peptide active agent that is greater than about 10% relative to intrapleural (pi) administration, usually greater than about 15%, and typically about 16%, 17%, 18%, 19%, 20% or greater.
- the peptide active agent upon sublingual administration of the mucosal delivery composition has a pharmacological bioavailability of greater than about 10% relative to intrapleural administration, usually greater than about 15%, and more typically about 20% or greater.
- mucosal delivery of the peptide active agent as provided in the mucosal delivery compositions of the disclosure is enhanced and reliably reproducible relative to the peptide active agent that is not stably hydrated.
- “reliably reproducible” is intended the extent to which the measurements of a test remain consistent over repeated tests of essentially the same composition under identical conditions.
- mucosal delivery using a mucosal delivery composition of the disclosure is reliably reproducible if it yields consistent results of substantially the same measure.
- mucosal delivery of a mucosal delivery composition is unreliable if repeated tests give inconsistent results of substantially different measure.
- the stably hydrated peptide active agent has a water content by weight and solubility in an organic or aqueous organic solvent comparable to or greater than the dried peptide active agent, and is essentially non-aggregated and unoxidized.
- the stably hydrated peptide active agent has a water content by weight and solubility in an organic or aqueous organic solvent comparable to or greater than the peptide active agent dried (i) from a solution or suspension at a pH different, optionally remote, from the isoelectric point of the peptide, and (ii) under conditions that retain a sufficient amount of water to maintain solvation and stability of the peptide.
- the stably hydrated peptide active agent has a water content by weight comparable to a storage stable dried form of the peptide.
- storage stability of the dried form of the peptide is determinative when having a shelf life equal or greater than one month when stored at a temperature in the range of -20°C to 25°C.
- the storage stable dried form of the peptide is associated with one or more pharmaceutically acceptable excipients, for example, co-drying excipients such as counter ion, preservative, isotonic agent, and/or buffer.
- the water content of the stably hydrated peptide active agent relative to the anhydrous peptide can be about 0.1 % to about 50% by weight, and is usually about 0.5% to about 50%, 1 % to about 30%, 1 % to about 25%, more usually about 1 % to about 20%, about 1 % to about 15%, and typically about 1 % to about 10%, such as about 1 % to about 5%.
- Peptide hydration can be measured relative to the anhydrous peptide by standard techniques known in the art.
- water content can be measured using the Loss On Drying method and/or the Karl-Fischer method (e.g. J. A. Dean, Analytical Chemistry Handbook, Section 19, McGraw-Hill, New York, 1995, or by the United State Pharmacopeia's (USP) publication USP-NF (2004), which describes the US Food and Drug Administration (FDA) enforceable standards ((2004-USP-Chapter 921 ).
- the stably hydrated peptide active agent has a percent solubility value in a given organic or aqueous organic solvent at ambient temperature that is equal to or greater than 0.001 %, usually less than or equal to 125% of the percent solubility value, and typically less than or equal to the percent solubility value of the peptide active agent dried from a solution or suspension at a pH different, optionally remote, from the isoelectric point of the peptide.
- Solubility in organic or aqueous organic solution or suspension is readily measured as the concentration wherein adding more of the peptide does not increase its concentration in the solution or suspension. Solubility can also be estimated by visual inspection in relatively clear liquid or gel formulations (e.g., solubilized if peptide formulation is essentially limpid in appearance). pH and pi
- the pH of a subject composition is targeted so that the peptide active agent is sufficiently ionized to maintain complexation with the desired complexing agent(s), as well as capable of being soluble or re-soluble when combined in the non-aqueous hydrophobic vehicle.
- complexation with a cation-binding crown compound is favored when amino groups of the peptide are protonated (ionized).
- the pH of the subject compositions is different, often remote, from the pi of the peptide active agent in the composition, where the peptide is sufficiently ionized for complexation with the crown compound and counter ion.
- isoelectric point is intended the pH value at which the peptide active agent carries no overall net electrical charge.
- the pH is selected such that the peptide complex remains stable and soluble (or re-soluble when prepared as a dried, preformed peptide complex).
- “remote from the isoelectric point of the peptide active agent” is intended about 1 pH unit or greater from the isoelectric point of the peptide active agent.
- the pH may be above or below the isoelectric point of the peptide active agent, provided it is within a range that stabilizes the stably hydrated peptide active agent in the composition for a given end use.
- the pH is above the pi of the peptide active agent, whereas in other embodiments, the pH is below the pi of the peptide active agent.
- the pH is about 0.1 to about 4 pH units from the isoelectric point of the peptide active agent. In some embodiments, the pH is about 0.5 to about 3 pH units, including about 1 to about 2 pH units, from the isoelectric point of the peptide active agent.
- a buffer is included to maintain the pH within a given range.
- the pKa of buffer in solvent mixtures containing predominantly water are close to the water value.
- the buffer pKa changes.
- neutral weak acids such as acetic acid and anionic acids such as H 2 P0 4 " typically get weaker, and the pKa becomes larger as the proportion of organic solvent increases.
- Cationic acids such as NH 4 + get stronger, but this trend reverses at high organic concentration and they become weaker.
- the pH can be approached empirically, and/or estimated by calculation of the solution pH with reference to standard buffer solutions of known pH (e.g., Rondinini, S., Analytical Bioanalytical Chem (2004) 374(5):813-816; Bosch et al., Anal. Chem. (1996) 68(20):3651-3657; Subirats ef al., J Chrom A, (2007) 1138:203-215; Subirats et al. Separation & Purification Reviews (2007) 36(3):231 -255; and Gagliardi et al. J. Chromatography A (2005) 7077(2):159-169).
- the pKa (and isoelectric point) values of peptides under such conditions can also be determined (e.g., Sanz- Nebot er a/., J. Chromatography A (2002) 942(1 -2): 145).
- considerations for selection include buffering capacity, solubility, and ionic strength in the composition.
- optimizing the pH to increase the ratio of the ionized to the neutral form of the peptide can be accomplished in aqueous, organic, and aqueous organic solutions to favor crown and counter ion complexation.
- Peptide active agents of the present disclosure are those peptides whose mucosal delivery is facilitated or enhanced when administered in conjunction with the subject mucosal delivery compositions and methods. Whether or not a given peptide active agent is suitable for use according to the present disclosure can be readily determined, for example, using assays employed in the experimental section below.
- a peptide active agent is suitable for use in the subject methods if its mucosal delivery in conjunction with the subject non-aqueous hydrophobic vehicle of the disclosure delivers an effective amount of the agent into the blood stream of the host, particularly where such delivery is increased by 1 to 10-fold or more, such as by 50-fold or more and sometimes by 100-fold or more relative to mucosal administration of the peptide in the absence of the mucosal delivery vehicle (e.g., peptide in sterile saline solution), as determined by measuring peptide concentration present in the blood stream of a host, for example, using detection systems suitable for such purposes as discussed above and illustrated in the experimental section below.
- the peptide active agent is one whose occurrence and/or intensity of observable biological effects are increased by mucosal delivery, for example, as observed in the mouse assay described in the experimental section below.
- peptides of interest include, but are not limited to, acetalins (e.g., acetalin 1 , 2 and 3 (acetyl plus enkephalin), adrenocorticotropic hormone (ACTH) and related peptides, adipokinetic hormones (e.g., adrenomedullin), ADP-ribosylation factors (ARF), adrenomedullin peptides, Agouti related peptides, allatostatins, amylin peptides, amyloid peptides, angiotensins and related peptides, annexin, various anti-inflammatory peptides, antimicrobial and related peptides, antioxidant peptides, apelin peptides, apoptosis peptides, Bad and Bag Cell peptides, adrenal medulla peptides, basic fibroblast growth factor (bFGF), bombesins, bradykinins,
- peptide hormones which are a class of peptides that exhibit activity upon entry into the blood stream and have endocrine functions in living animals.
- peptide hormones of specific interest include, but are not limited to, glucagon, glucagon-like- peptide, insulin, somatostatin, calcitonin, parathyroid hormone, and the like, and analogues/derivatives thereof.
- the peptide active agent is a peptide hormone, for example, insulin and the incretin mimetics, such as the exendins and related analogues/derivatives (e.g., chemically synthesized and/or biologically produced exendins such as exendin-3 and exendin-4, liraglutide, glucagon-like peptide-1 (GLP-1 ), and Taspoglutide, Albiglutide.
- ZP10 (AVE0010), and various analogues/derivatives thereof.
- Naturally occurring incretins such as GLP-1 exhibit insulinotropic properties after release into the circulation from the gut.
- the actions of GLP-1 include (a) a stimulation of insulin secretion in a glucose-dependent manner, (b) a suppression of glucagon, (c) a reduction in appetite and food intake, (d) a deceleration of gastric emptying, (e) a stimulation of ⁇ -cell neogenesis, growth and differentiation in animal and tissue culture experiments, and (f) an in vitro inhibition of ⁇ -cell apoptosis induced by different toxins.
- Exendins are peptide hormones isolatable from an exocrine gland but have endocrine actions. Exendins stimulate insulin secretion in response to rising blood glucose levels, and modulate gastric emptying to slow the entry of ingested sugars into the bloodstream. Exendin- 3 is a 39-amino acid peptide that shares homology with VIP (vasoactive intestinal peptide), secretin, helospectin I and II and helodermin. It stimulates increases in cellular cAMP and amylase release from dispersed guinea pig pancreatic acini. Exendin-4, a 39-amino acid peptide originally isolated from the oral secretions of the lizard Heloderma suspectum, has been shown to share certain activities with glucagon-like-peptide-1 (GLP-1 ).
- GLP-1 glucagon-like-peptide-1
- Exenatide (the active ingredient of BYETTA® (exenatide injection), also called exendin-4) is a GLP-1 agonist that improves glucose homeostasis by mimicking the actions of naturally occurring GLP-1 . It improves glycemic control by reducing fasting and postprandial glucose concentrations through a combination of known mechanisms, including glucose-dependent insulin secretion, restoration of first-phase insulin response, regulation of glucagon secretion, delaying gastric emptying, and decreasing food intake.
- Exenatide is a subcutaneously injected incretin mimetic peptide approved for the treatment of type 2 diabetes mellitus (condition in which the body does not use insulin normally and, therefore, cannot control the amount of sugar in the blood).
- Exenatide is used in combination with metformin, a sulfonylurea, or a thiazolidinedione.
- Exenatide works by stimulating the pancreas to secrete insulin when blood sugar levels are high. Insulin helps move sugar from the blood into other body tissues where it is used for energy. Exenatide also slows the emptying of the stomach and causes a decrease in appetite.
- Exenatide is not used to treat type 1 diabetes (condition in which the body does not produce insulin and, therefore, cannot control the amount of sugar in the blood).
- Exenatide is usually injected twice a day within 60 minutes before the morning and evening meals.
- Liraglutide is a GLP-1 derivative that finds use similar to Exenatide, for example, in the treatment of type 2 diabetes. Liraglutide has a half-life after subcutaneous injection of 11-15 hours, making it suitable for once-daily dosing (in contrast to Byetta's twice daily). The prolonged action of liraglutide is achieved by a fatty acid molecule attached to the GLP-1 molecule, which binds to albumin within the subcutaneous tissue and bloodstream. The active GLP-1 is then released from albumin at a slow, consistent rate. Binding with albumin also results in slower degradation and reduced elimination of liraglutide from the circulation by the kidneys compared to GLP-1.
- peptide active agents for use in the subject methods and compositions of the disclosure may include incretin mimetics, such as GLP-1 , and various analogues/derivatives thereof including exendin-4, liraglutide, and various analogues/derivatives thereof.
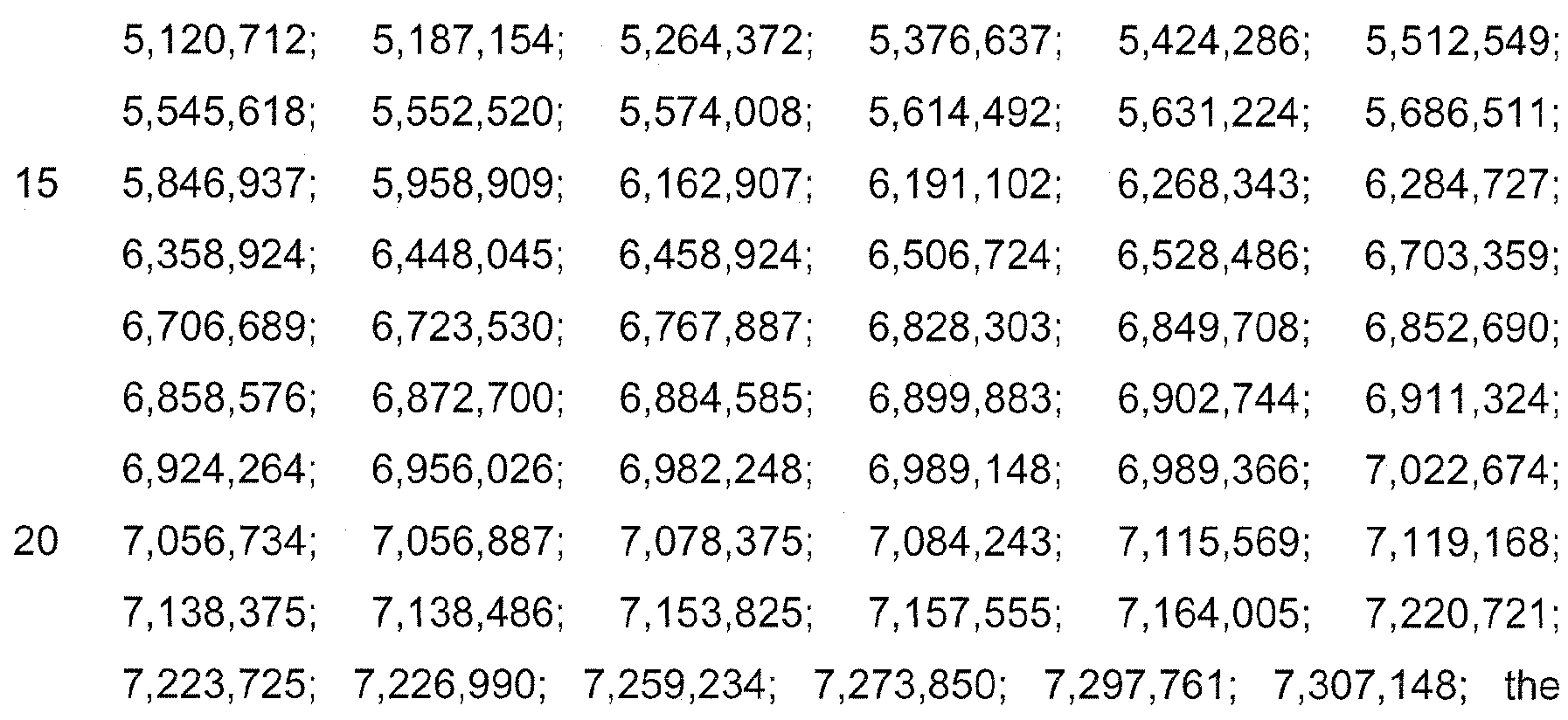
- incretin mimetics and related compounds of interest are described in U.S. Patent Nos. 5, 1 18,666
- Additional peptide active agents for use in the subject methods and compositions of the disclosure may include insulin, such as human insulin and various analogues/derivatives thereof. Insulin and related compounds of interest are described in U.S. Patent Nos. 4,51 1 ,505; 5,631 ,347; 5,646,242
- peptide active agents for use in the subject methods and compositions of the disclosure may include parathyroid hormone, or calcitonin (e.g., for the treatment of Paget's disease, hypercalcemia and osteoporosis, including natural, synthetic or recombinant human, salmon, pig or eel calcitonin).
- parathyroid hormone, calcitonin and related compounds of interest are described in U.S. Patent Nos.: 4,692,433; and RE40.850; the disclosures of which are herein incorporated by reference.
- the peptide active agent is incretin mimetic peptide.
- the incretin mimetic is exendin-4 and analogues/derivatives thereof.
- the incretin mimetic is liraglutide and analogues/derivatives thereof.
- the peptide active agent is glucagon-like peptide-1 (GLP-1 ) and analogues/derivatives thereof.
- the peptide active agent is insulin and analogues/derivatives thereof.
- the peptide active agent is other than a peptide selected from one or more of the peptides described herein, such as insulin, including peptides larger than about 50 amino acids, such as peptides larger than about 100 amino acids.
- prodrugs of the peptide active agents are, in general, functional derivatives of the compounds that are readily convertible in vivo into the required compounds.
- administering encompasses administering the compound specifically disclosed or with a compound which may not be specifically disclosed, but which converts to the specified compound in vivo after administration to the subject in need thereof.
- Conventional procedures for the selection and preparation of suitable prodrug derivatives are described, e.g., in Wermuth, "Designing Prodrugs and Bioprecursors" in Wermuth, ed. The Practice of Medicinal Chemistry, 2d Ed., pp. 561 -586 (Academic Press 2003).
- Prodrugs include peptides bearing post-translational or synthesis modification sites, enzymatic or chemically cleavable bonds, such as peptides with protease cleavable leader residues or sequences, or esters that hydrolyze in vivo (e.g., in the human body) to produce a compound described herein suitable for the present disclosure.
- Suitable ester groups include, without limitation, those derived from pharmaceutically acceptable, aliphatic carboxylic acids, particularly alkanoic, alkenoic, cycloalkanoic and alkanedioic acids.
- Illustrative esters include formates, acetates, propionates, butyrates, acrylates, citrates, succinates, and ethylsuccinates.
- the crown compounds include, for example, cyclic polyethers (crown ethers, e.g., 18-crown-6) and cyclic polyesters (crown esters, e.g., polylactones such as nonactine and tetranactine, polyglycolic or lactic esters), and analogues/derivatives thereof (e.g., WO 08/037484; Lifson et al., J. Am. Chem. Soc. (1983) 105:3866-3875; Lifson et al., J. Am. Chem. Soc.
- the crown compounds are cyclic polyethers, cyclic polyesters, and cyclic depsipeptide (where "depsipeptide” refers to crown compounds which comprise or consist of alpha-hydroxy acids and alpha-amino acids, or mixtures thereof, which are linked to each other by ester linkages between the hydroxy group of an alpha-hydroxy acid and the carboxyl group of either a hydroxy acid or an amino acid as well as by amide linkages between the amino group of an alpha-amino acid and the carboxyl group of either a hydroxy acid or an amino acid).
- Linear forms of the subject crown compounds such as a cleavage form thereof, may be employed as charge complexing agents in some aspects of the disclosure.
- the crown compound in certain embodiments comprises a biodegradable linkage.
- the biodegradable linkage is cleavable in vivo.
- biodegradable linkages of particular interest include esters, such as carboxylic acid esters (-C(O)-O-), thioesters (-C(O)-S-), orthoesters (- C(OR 1 )(OR 2 ) and (-C(OR 1 )(OR 2 )(OR 3 )), and the like.
- biodegradable linkage is an ester, and more particularly an ester selected from a carboxylic acid ester, and an orthoester.
- Crown compounds of specific interest are disclosed in the co- pending patent application entitled Orthoester derivatives of crown ethers" and having attorney docket number "R1856" filed on even date herewith, which reference is incorporated in its entirety.
- carboxylic acid ester and an orthoester crown compounds include, but are not limited to, the oxo-crowns and analogues/derivatives thereof, particularly oxo-crown ethers.
- the oxo-crown ethers comprise 4 to 8 coordinating oxygen ring atoms, 8 to 16 ring carbon atoms, and at least one oxo- substituted side chain.
- oxo-(18-crown-6) compounds and analogues/derivatives thereof such as those comprising a structure selected from oxo-(18-crown-6), oxo-(18-crown-6)-diethyl tartrate, and oxo- (18-crown-6)-diglycerol tartrate, as illustrated below.
- the counter ion allows the formation of neutrally charged species of ionizable groups of the stably hydrated peptide active agent.
- the counter ion is present in an amount in combination with the crown compound under conditions that partially neutralize, or impart overall neutrality to the stably hydrated peptide active agent.
- the counter ion is a counter ion of an acidic salt (e.g., salicylic acid, acetic acid, trifluoroacetic acid, tartaric acid, phosphoric acid, lactic acid, fumaric acid, maleic acid, citric acid, methylsulfonic acid, p-toluensulfonic acid), an amino acid (e.g., lysine, glycine, histidine, arginine), or a modified amino acid (e.g., N-acetyl-lysine-amide, N-acetyl-arginine-amide). Combinations of different counter ions are also contemplated.
- an acidic salt e.g., salicylic acid, acetic acid, trifluoroacetic acid, tartaric acid, phosphoric acid, lactic acid, fumaric acid, maleic acid, citric acid, methylsulfonic acid, p-toluensulfonic acid
- an amino acid e.g
- the counter ion is selected from an acidic salt, an amino acid, a modified amino acid, and mixtures thereof.
- an acidic salt is a hydrophilic acid or lipophilic acid.
- hydrophilic acids of interest include, but are not limited to, trifluoroacetic acid, sulfonic acid, and benzoic acid.
- lipophilic acids of particular interest included, but are not limited to, aryl and alkyl sulfonic acids, such as dodecyl-sulfonic acid and higher homologues, phosphatidylglycerol deravtives such as dilauryloylphosphatidylglycerol (DLPG), lipoic acid, and the like.
- aryl and alkyl sulfonic acids such as dodecyl-sulfonic acid and higher homologues
- phosphatidylglycerol deravtives such as dilauryloylphosphatidylglycerol (DLPG), lipoic acid, and the like.
- DLPG dilauryloylphosphatidylglycerol
- lipoic acids can be employed.
- an acidic salt that is a strong lipophilic acid, such as an alkyl sulfonic acid and higher homologues.
- the hydrophilic acid is selected from the group consist
- the lipophilic acid is dodecyl-sulfonic acid.
- relatively strong acidic counter ions such as dodecyl-sulfonic acid
- care is taken to avoid oxidation of peptides that may be susceptible, for example, by inclusion of an antioxidant, limiting the concentration of the counter ion, and so forth.
- lipophilic acids such as alkyl sulfonic acids having an alkyl chain with between 2 and 30, and usually between 8 and 10 carbon atoms are of specific interest.
- Certain phospholipids may also be employed as a counter ion in some embodiments.
- phospholipids with at least an acidic proton on the phosphate such as a phosphatidyl glycerol or phosphatidyl sugar with one acidic proton, or a phosphatidic acid with two acidic protons are of interest.
- Phospholipids comprising two alkanoic acids may either symmetric or asymmetric. In the latter case, a phospholipid molecule comprises two different fatty acids.
- the phospholipds are of natural origin, like for example phosphatidylinositol.
- the counter ion can be acids with multiple acidic valence (multi protic) or poly carboxylic acids.
- inorganic acids that include, but are not limited to, phosphoric sulfuric acid, and the like
- organic acids that include, but not limited to, bis-carboxylic aromatic acids such as Phthalic acid and Terephthalic Acid, and from alkylic oxalic acid, malonic acid, succinic acid, tartaric acid, maleic acid, fumaric acid, and the like.
- a bis carboxylic acid of choice can be used as a counter ion to generate a cationic charge with an amino group of the peptide side chain, notably Lysine and Arginine.
- a peptide active agent can be prepared having about 1 bis carboxylic acid as per amino group counter ion, and then the pH can be brought to about neutrality, from approximately pH 6 to pH 8.
- the amino groups on the peptide chain (especially Lysine and Arginine) can still be fully protonated by the first acidic moiety of the acid, and the other acid function being concomitantly ionized and amenable of forming a salt with the buffer generating an additional cationic charge, for example sodium or potassium.
- the cationic charges of peptide can be significantly increased possibly resulting in better solubility, reduced aggregation and enhanced peptide stability.
- the non-aqueous hydrophobic vehicle is generally capable of solubilizing, or maintaining the solubility of the peptide complex and/or peptide salt homogeneously dispersed therein.
- the peptide complex and/or peptide salt when combined in the non-aqueous hydrophobic vehicle may be clear or turbid in appearance, with the proviso that an effective amount of the peptide active agent is homogenously dispersed therein without unwanted precipitation and/or aggregate formation.
- the non-aqueous hydrophobic vehicle of the mucosal compositions comprises at least one acylglycerol, and at least one organic solvent and/or lipid each individually present in an amount effective to (i) solubilize the stably hydrated peptide active agent complexed with the crown compound and/or the counter ion and (ii) enhance mucosal delivery of the peptide active agent.
- the acylglycerol embodies the water insoluble esters of glycerol
- acylglycerol examples include, but are not limited to, corn oil mono-di-tridiglycerides, medium chain (C 8 -Cio) mono- and diglycerides, long-chain triglycerides (castor oil, corn oil, cottonseed oil, olive oil, peanut oil, peppermint oil, safflower oil, sesame oil, soybean oil, hydrogenated soybean oil, hydrogenated vegetable oils), and medium-chain triglycerides (such as caprylic/capric triglycerides derived from coconut oil or palm seed oil).
- Such acylglycerols are generally recognized as safe for use as direct food additives, as well as for cosmetic and pharmaceutical applications.
- the acylglycerol is selected from monoacylgycerol, diacylglycerol, and mixtures thereof.
- monoacylgycerols and diacyiglycerols that are solid or semi-solids at ambient, normal room temperature, particularly medium chain (C 8 -Ci 0 ) mono- and diacyiglycerols.
- a featured aspect is directed to the medium chain (C 8 -Cio) monoacylglycerols, such as mono-decanoyl-glycerol.
- At least one acylglycerol may be included in an amount so that the formulation is liquid, gel, or a solid or semi-solid at a desired temperature.
- a solid oral delivery formulation may employ one or more particular acylglycerols in an amount such that the formulation is a solid or semi-solid at temperature of up to about 50°C to about 55°C.
- an acylglycerol formulation can be selected that is a liquid or gel at lower temperatures than this.
- an acylglycerol formulation can be selected such that at least one acylglycerol is included in an amount to provide a formulation that is solid at 4°C, and melts at room temperature, or at or around the temperature of the host, e.g., solid at 4°C and is melted or begins melting around 37°C- 45°C.
- an acylglycerol formulation that is a solid or semisolid at temperatures less than about the body temperature of the host, such as an acylglycerol formulation that is a solid or semi-solid at less than about 37°C-45°C.
- an acylglycerol with such features can be chosen based on its melting temperature.
- acylglycerols that are solids or semisolids at ambient room temperature and having a melting temperature of about 60°C or iess, usually about 55°C or less, and more typically about 53°C or less, e.g., mono-decanoyl-glycerol, has a melting point of about 53°C.
- acylglycerols are known and commercially available.
- acylglycerols with unsaturated long alkyl chain such as mono-olein (glycerol ester with oleic acid), mono linolein, mono elaidin, mono erucate et others, which are liquids and or semi-solid at room temperature.
- mono-olein glycerol ester with oleic acid
- mono linolein mono elaidin
- mono erucate et others which are liquids and or semi-solid at room temperature.
- medium chain (C 8 -Ci 0 ) mono- and diacylgiycerols typically are solids or semi-solids at temperatures less than about the body temperature of the host, and thus have, or can be formulated to have, melting points that are less than about the body temperature of the host, usually less than about 37°C, and as such are of specific interest.
- the body temperature of the host can melt the semi-solid material, allowing for dissolution and delivery of the peptide active
- acylglycerols that are a semi-solid at temperatures less than about the body temperature of the host can be advantageously used to (1 ) reduce the volume of the mucosal delivery vehicle, since solids or semisolids have a reduced volume compared to their liquid forms, and (2) provide flexibility for solid or semi-solid dosage forms (as described in greater detail below).
- This aspect of the disclosure also aids in retaining the peptide active agent in the mucosal delivery composition to avoid unwanted leakage prior to delivery, more uniform dissolution of the peptide active agent upon delivery, enhancement of permeability in general across the mucosal membrane of interest, as well as maintaining the peptide active agent in its stably hydrated form in the mucosal delivery composition.
- the acylglycerol is a semi-solid at temperatures less than about the body temperature of the host.
- the acylglycerol is a semi-solid at ambient, normal room temperature, such as a medium chain mono- and diacylgiycerols.
- a featured aspect of the disclosure is directed to the medium chain (Ce-C- ⁇ ) mono- acylglycerols, such as mono-decanoyl-glycerol.
- a mixture of one or more saturated acylglycerols can be used with one or more long alkyl chain unsaturated acylglycerol as defined above.
- Using such mixtures permits to optimize physical/chemical properties such as, but not limited to viscosity, and melting point of the composition of the invention.
- Lipid Lipids are generally defined as hydrophobic or amphiphilic small molecules.
- lipids include fats, waxes, sterols, fat-soluble vitamins (such as vitamins A, D, E and K), monoglycerides, diglycerides, phospholipids, and others.
- the lipid component comprises an acylglycerol, for example, when the lipid is an oil, such as corn oil mono-di-tridiglyceride, long-chain triglyceride such as olive oil, castor oil, corn oil, cottonseed oil, peanut oil, peppermint oil, safflower oil, sesame oil, soybean oil, hydrogenated soybean oil, hydrogenated vegetable oils, medium- chain triglyceride such as caprylic/capric triglycerides derived from coconut oil or palm seed oil, and the like.
- oil such as corn oil mono-di-tridiglyceride, long-chain triglyceride such as olive oil, castor oil, corn oil, cottonseed oil, peanut oil, peppermint oil, safflower oil, sesame oil, soybean oil, hydrogenated soybean oil, hydrogenated vegetable oils, medium- chain triglyceride such as caprylic/capric triglycerides derived from coconut oil or palm seed oil, and the like.
- the lipid is other than an acylglycerol, such as when the lipid is a fatty acid, or a neutral lipid such as a vitamin E (e.g., ⁇ -, ⁇ -, ⁇ -, and ⁇ -tocopherols and the corresponding four tocotrienols, which are fat-soluble neutral vitamins).
- a vitamin E e.g., ⁇ -, ⁇ -, ⁇ -, and ⁇ -tocopherols and the corresponding four tocotrienols, which are fat-soluble neutral vitamins.
- the lipid includes a fatty acid, more particularly, a permeability-enhancing fatty acid that is an aliphatic carboxylic acid, which may be saturated or unsaturated, branched or linear, and may include mixtures of different fatty acids.
- fatty acids are short, medium or long.
- Short chain fatty acids are fatty acids with aliphatic tails of less than seven carbons.
- Medium chain fatty acids are fatty acids with aliphatic tails of 7-14 carbons.
- Long chain fatty acids are fatty acids with aliphatic tails 16 carbons or more.
- fatty acids of particular interest include saturated fatty acids having 7-19 carbon atoms selected from caprylic acid, octanoic acid, nonanoic acid, decanoic acid, undecanoic acid, dodecanoic acid, myristic acid, palmitic acid, stearic acid, arachidic acid, and mixtures thereof.
- unsaturated fatty acids include those having 7- 19 carbon atoms selected from palmitoieic acid, oieic acid, linoleic acid, alpha- linoleic acid, and mixtures thereof.
- Each of these fatty acids have found use in various consumables, including their use as food additives, in cosmetics, and pharmaceutical applications, and thus may be generally regarded as safe for their intended use.
- a permeability-enhancing fatty acid as an excipient of the mucosal delivery composition to aid and/or maintain the peptide active agent in its stably hydrated state.
- Permeability-enhancing fatty acids having from 7-14 carbon atoms, and particularly 7-12 carbon atoms for this purpose are of particular interest.
- a featured aspect is a permeability- enhancing fatty acid that is a saturated fatty acid selected from caprylic acid, octanoic acid, nonanoic acid, decanoic acid, undecanoic acid, dodecanoic acid.
- nonanoic acid and thus the fatty acids exhibiting its mucosal delivery properties when employed in the mucosal delivery composition of the present disclosure.
- the permeability-enhancing features of the fatty acid can be readily determined, such as illustrated herein.
- the non-aqueous hydrophobic vehicle comprises a non-aqueous solvent capable of solubilizing the stably hydrated peptide active agent complexed with the crown compound and/or the counter ion.
- the non-aqueous solvent according to the disclosure includes solvents which may be used as a constituent in a pharmaceutical or diagnostic composition and/or solvents which may be used during the course of the manufacture and formulation thereof. In other words, the medical use of such solvents is approved and/or their use does not pose a threat to the health of an individual to be treated.
- the term "non-aqueous solvent” also includes natural products such as oils, and natural product derivatives such as Cremofor EL and the like.
- the non-aqueous hydrophobic vehicle comprises at least one organic solvent.
- organic solvent is known in the art and relates to carbon-based substances commonly used in the chemical industry, capable of dissolving or dispersing one or more substances. Generally speaking, organic solvents are more lipophilic or hydrophobic than water. As a consequence, their IogP vaiues are generally greater than zero.
- Organic solvents refer to unsubstituted hydrocarbon solvents like paraffinic, aliphatic and aromatic hydrocarbons and their derivatives containing heteratoms, like oxygen (e.g., alcohols, ketones, glycol esters), halogens (e.g., carbon tetrachloride), nitrogen (e.g., DMF, dimethyl formamide and acetonitrile) or sulphur (e.g., DMSO: dimethyl sulfoxide).
- oxygen e.g., alcohols, ketones, glycol esters
- halogens e.g., carbon tetrachloride
- nitrogen e.g., DMF, dimethyl formamide and acetonitrile
- sulphur e.g., DMSO: dimethyl sulfoxide
- organic solvents are methanol, ethanol, alcohols from C 3 to do, acetonitrile, butanone, 1 ,1 ,1-trifluoroethanol (TFE), hexafluoroisopropanol (HFIP), ethyl acetate, carbon tetrachloride, butanol, dibutyl ether, diethyl ether, cyclohexane, methylene chloride (dichloromethane), hexane, butyl acetate, di-isopropyl ether, benzene, dipentyl ether, chloroform, heptane, tetrachloroethylene, toluene, hexadecane, dimethylformamide (DMF), tetrahydrofurane (THF) and dioxane.
- TFE 1 ,1 ,1-trifluoroethanol
- HFIP hexafluoroisopropanol
- At least one organic solvent is a water soluble organic solvent.
- the water-soluble organic solvent include, but are not limited to, hexaethylene glycol, polyethylene glycol 300, polyethylene glycol 400, ethanol, propylene glycol, glycerin, N-methyl-2-pyrrolidone, dimethylacetamide, and dimethylsulfoxide. Each of these components is commercially available, found in a number of pharmaceutical products, and generally regarded as safe for their intended uses.
- the water-soluble organic solvent includes or consists of a humectant, such as a diol, polyol, or mixtures thereof.
- the water-soluble organic solvent is a polar aprotic solvent.
- the water-soluble organic solvent comprises a mixture of polar aprotic solvent with humectant.
- a humectant is a hygroscopic substance having an affinity to form hydrogen bonds with molecules of water. It is typically a molecule with several hydrophilic groups, most often hydroxyl groups, but amines and carboxyl groups, sometimes esterified, can be encountered as well. Examples of humectants include glycerine, propylene glycol and glyceryl triacetate.
- Others can be polyols like the sugar alcohols erythritol, arabitol, xylitol, ribitol, mannitol, sorbitol, isomalt, maltitol, and lactitol, or polymeric polyols like polydextrose or natural extracts like quillaia, or polyethylene glycols like hexaethylene glycol (MW 282.3), polyethylene glycol 300 or polyethylene glycol 400.
- one or more diols, polyols and mixtures thereof are included in the non-aqueous hydrophobic vehicle not only to aid solubilization of the stably hydrated peptide active agent, but also as a source of OH (hydroxyl) groups, which are amenable to hydrogen bonding with the peptide to aid in stabilization.
- peptides when formulated as dried powder or residue particularly large peptides (e.g., proteins), may be dried with sugar alcohols such as mannitol to maintain folding and biological activity. This is because when formulated without water (in solution) and as dried powder or residue, it has been found that the peptides often loose biologically activity.
- a water-soluble organic solvent comprising a mixture of two or more of a polar aprotic solvent, propylene glycol, glycerol, and a polyethylene glycol.
- Glycerol (or propane-1 ,2,3-triol) is a colorless, odorless, viscous liquid is widely used in food and pharmaceutical formulations.
- glycerin or glycerine it is a sugar alcohol, and is sweet-tasting and of low toxicity.
- Glycerol has three hydrophilic alcoholic hydroxyl groups that are responsible for its solubility in water and its hygroscopic nature.
- Propylene glycol (or propane-1 ,2-diol) is a diol alcohol, usually a tasteless, odorless, and colorless clear oily liquid that is hygroscopic and miscible with water, acetone, and chloroform. Because of its low chronic oral toxicity, propylene glycol is generally recognized as safe (GRAS) for use as a direct food additive, as well as for cosmetic and pharmaceutical applications.
- GRAS groscopic and miscible with water, acetone, and chloroform.
- Polyethylene glycol (or PEG) also known as polyethylene oxide (PEO) or polyoxyethylene (POE) are polyethers.
- PEG oligomers and polymers with a molecular mass below 20,000 g/mol are PEG oligomers and polymers with a molecular mass below 20,000 g/mol, as well as various derivatives, the most common of which is a monofunctional methyl ether PEG (methoxypoly(ethylene glycol)), abbreviated mPEG.
- PEG diols having a molecular mass below 8000 g/mol, 4000 g/mol, 1000 g/mol, 800 g/mol, 700 g/mol, or 600 g/mol and particular PEG diols having a molecular mass of between about 200-500 g/mol, such as hexaethylene glycol, and the better known PEG 300 and PEG 400.
- the subject PEG compounds are generally recognized as safe for use as a direct food additive, as well as for cosmetic and pharmaceutical applications.
- Polar aprotic solvents are solvents that share ion dissolving power with protic solvents but lack an acidic hydrogen. These solvents generally have high dielectric constants and high polarity. Examples are N-methyl- pyrrolidone (or N-methyl-2-pyrrolidone), dimethyl sulfoxide, dimethylformamide, dioxane and hexamethylphosphorotriamide.
- An advantage of polar aprotic solvents in the subject compositions is their high solubizing nature and ability to maintain and/or reduce unwanted ionization of the peptide. Of specific interest is N-methyl-2-pyrrolidone.
- N-methyl-2- pyrrolidone is a very strong solubilizing agent and found as a solubilizing agent in a few commercially available pharmaceutical products. It is also found as a volatile component in roasted nuts, and is a versatile solvent miscible with water, ethyl alcohol, ether, chloroform, benzene, ethyl acetate and carbon disulfide.
- the organic solvent includes a non-ionic surfactant.
- the non-ionic surfactant can also be a non-aqueous solvent, an organic solvent, and/or a water soluble organic solvent.
- the non- ionic surfactant include, but are not limited to, polyoxyl 35 castor oil (Cremophor EL), polyoxyl 40 hydrogenated castor oil (Cremophor RH 40), and polyoxyl 60 hydrogenated castor oil (Cremophor RH 60), as well as d-a- tocopherol, polyethylene glycol 1000 succinate, polysorbate 20, polysorbate 80, Sorbitan-monolaurate (Span 20), Sorbitan monopalmitate (Span 40); Sorbitan monostearate (Span 60); Sorbitan-monooleate (Span 80), Solutol HS 15, sorbitan monooleate, poloxamer 407, Labrafil M-1944CS, Labrafil M- 2125CS, Labrasol, Gel
- the non-ionic surfactant is selected from a polyoxyethylated polyol, a polyoxyethylated polyol esterified with fatty acids, and mixtures thereof.
- the non-ionic surfactant is a polyoxyethylated polyol selected from the group consisting of polyoxyl 35 castor oil (Cremophor EL), polyoxyl 40 hydrogenated castor oil (Cremophor RH 40), polyoxyl 60 hydrogenated castor oil (Cremophor RH 60), and mixtures thereof
- the polyethoxylated polyol esterified with fatty acids is selected from the group consisting of polysorbate 20 (Tween 20), polysorbate 80 (Tween 80), and mixtures thereof.
- non-ionic surfactant is a polyoxyethylated polyol, such as a polyethoxylated castor oil, and in particular, polyoxyl 35 castor oil (Cremophor EL).
- vitamin E such as d-a-tocopherol alone or in combination with other vitamin E compounds, as it includes a moderately acidic phenol group that may benefit the subject formulations.
- the non-aqueous hydrophobic vehicle is acidic
- at least one acylglycerol is a medium chain acylglycerol
- at least one lipid comprises a short chain fatty acid and/or a medium chain fatty acid
- at least one water soluble organic solvent is a polar aprotic solvent.
- the medium chain acylglycerol is mono- decanoyl glycerol
- the short chain fatty acid is nonanoic acid
- the medium chain fatty acid is oleic acid
- the polar aprotic solvent is N-methyl-2- pyrrolidone.
- the non-aqueous hydrophobic vehicle is neutral
- at least one acylglycerol is a medium chain acylglycerol
- at least one lipid is a neutral lipid
- at least one water soluble organic solvent is a polar aprotic solvent.
- the medium chain acylglycerol is a mixture of mono-decanoyl glycerol and octanoyl glycerol
- the neutral lipid is vitamin E
- the polar aprotic solvent is propylene glycol N-methyl-2-pyrrolidone.
- the mucosal delivery composition is comprised as an emulsion, dispersion, liposome, or micelle, including a reverse micelle (as described in more detail below).
- compositions may further comprise other pharmaceutically acceptable components as excipients.
- examples of such components are well known in the art and include non-ionic surfactants, antioxidants, buffers, viscosity modifying agents, chelating agents, various types of wetting agents, dilutants, sterile solutions, and so forth (as described in more detail below).
- Non-ionic surfactants or detergents include organic compounds having a hydrophobic tail and an uncharged head group. Examples include, but are not limited to, alkyl poly(ethylene oxide), alkylphenol poly(ethylene oxide), copolymers of poly(ethylene oxide) and poly(propylene oxide) (commercially called poloxamers or poloxamines), alkyl polyglucosides such as octyl glucoside and decyl maltoside, fatty alcohols such as cetyl alcohol and oleyl alcohol, cocamide MEA, cocamide DEA, and polysorbates such as Tween 20, Tween 80, and dodecyl dimethylamine oxide, and the like. Of specific interest are non-ionic detergents such as beta-D-octylglucoside.
- antioxidants which are generally reducing agents such as thiols, melatonin, lipoic acid, uric acid, carotenes, ascorbic acid, polyphenols and the like, such as glutathione, and vitamin E, as well as enzymes such as catalase, superoxide dismutase and various peroxidases.
- antioxidants of specific interest include, but are not limited to, N- acetyl-methionine, biotin, ascorbic acid, glutathione, and vitamin E.
- the mucosal delivery composition comprises an antioxidant.
- the preformed peptide complex comprises an antioxidant.
- ascorbic acid alkanoate esters the alkyl chain thereof preferably being from C8 to C24 and being saturated or unsaturated. Such compounds may act as surfactant. As such, they may promote microemulsion and formation of microgels. Preferred compounds falling into this class such as 6-O-lauryl ascorbic acid as described in Zaino et al., Lat. Am. J.Pharm., 28, 438-442, 2009.
- An advantage of ascorbic acid alkanoate esters is that they serve not only to deliver and stabilize the peptide active agent according to the present invention, but furthermore are capable of preventing or reducing oxidation thereof. Accordingly, these compounds may serve as surfactants and/or antioxidants.
- Preferred carriers for mucosal delivery or diluents for formulation according to the disclosure include the non-aqueous solvents as discussed above.
- Compositions comprising such carriers can be formulated by well known conventional methods, taking into account the storage and dosage regimen, which can be determined by the clinical factors.
- the peptide active agent may be present in amounts between 1 ng and 10 mg/kg body weight per dose; however, doses below or above this exemplary range are envisioned, especially considering the aforementioned factors.
- Envisaged formulations furthermore comprise microspheres, liposomes, microcapsules, and nanoparticles/nanocapsules.
- compositions of to the disclosure include cyclodextrins (see, for example, Irie and Uekama (1999) or Challa et al. (2005)) and/or chitosan.
- Cyclodextrins form inclusion complexes with hydrophobic moieties present on a compound. Furthermore, they present a hydrophilic exterior surface.
- Compositions comprising cyclodextrins or chitosan may provide for a delayed release and/or a release over an extended period of time of the peptide active agent. Accordingly, compositions to be manufactured further comprises a cyclodextrins.
- Cyclodextrins are known in the art and include alpha-cyclodextrin, beta-cyclodextrin and gammacyclodextrin.
- the stably hydrated peptide active agent is in a first step complexed to form a first peptide complex, and then, in second step, the first peptide complex is complexed, to form a second layer, with cyclodextrines, more specifically be the hydrohphobic inner cavity of cyclodextrins, thereby generating in total two levels of complexations.
- Excipients may further include one or more chelators, which may also serve as an antioxidant, counter ion, and/or buffering agent and the like, depending on the particular compound.
- chelators include, but are not limited to, citric acid, phosphonates, antibiotics such as those of the tetracycline family, acrylic polymers, ascorbic acid, tetrasodium iminodisuccinate), dicarboxymethylglutamic acid, ethylenediaminedisuccinic acid (EDDS), ethylenediaminetetraacetic acid (EDTA), hepta sodium salt of diethylene triamine penta (methylene phosphonic acid)(DTPMP*Na 7 ), malic acid, nitrilotriacetic acid (NTA), nonpolar amino acids (e.g., methionine and derivatives thereof), oxalic acid, phosphoric acid, polar amino acids (e.g., arginine, asparagine, aspartic acid, glutamic acid
- Buffers such as sodium phosphate, TRIS, glycine, maleic acid, and sodium citrate
- additional excipients such as sodium phosphate, TRIS, glycine, maleic acid, and sodium citrate
- preservatives can be included to prevent or delay microbial activity (growth and metabolism).
- examples of pharmaceutically acceptable preservatives are phenol, m-cresol and a mixture of phenol and m-cresol, benzoate and derivatives thereof, and the like.
- isotonic agents in general represent a broad category of excipients, and may include, for example, a salt (e.g. sodium chloride), a sugar or sugar alcohol (i.e., a C4-C8 hydrocarbon having at least one -OH group and includes, for example, mannitol, sorbitol, inositol, galacititol, dulcitol, xylitol, and arabito), an amino acid (e.g. L-glycine, L-histidine, arginine, lysine, isoleucine, aspartic acid, tryptophan, threonine), an alditol (e.g.
- a salt e.g. sodium chloride
- a sugar or sugar alcohol i.e., a C4-C8 hydrocarbon having at least one -OH group and includes, for example, mannitol, sorbitol, inositol, galacititol,
- glycerol glycerine
- 1 ,2-propanediol propyleneglycol
- 1 ,3-propanediol 1,3- butanediol
- polyethyleneglycol e.g. PEG400
- Isotonic agents also include any sugar such as mono-, 10 di-, or polysaccharides, or water-soluble glucans, including for example fructose, glucose, mannose, sorbose, xylose, maltose, lactose, sucrose, trehalose, dextran, pullulan, dextrin, cyclodextrin, soluble starch, hydroxyethyl starch and carboxymethylcellulose-Na.
- sugar such as mono-, 10 di-, or polysaccharides, or water-soluble glucans, including for example fructose, glucose, mannose, sorbose, xylose, maltose, lactose, sucrose, trehalose, dextran, pullulan, dextrin, cyclodextrin, soluble starch, hydroxyethyl starch and carboxymethylcellulose-Na.
- excipients such as those mentioned above may be used individually or in combination. There is no fixed iimit to the amount used, as long as the excipient is soluble in the preparation and does not adversely affect the mucosal delivery composition or its components for a given end use.
- Remington The Science and Practice of Pharmacy, 19th edition, 1995. Storage Stability
- the subject mucosal delivery compositions and substituent components are prepared as storage stable preparations.
- the mucosal delivery composition, and/or pharmaceutical and/or diagnostic preparations comprising the mucosal delivery composition is storage stable.
- the preformed peptide complex is storage stable.
- the non-aqueous hydrophobic vehicle is storage stable.
- storage stable refers to compositions prepared for storage, aliquoting and/or shipping as separate and/or combined components, such as for inclusion in a kit, and particularly as a pharmaceutical and/or diagnostic formulation, which include a peptide active agent as an active ingredient, and in which the concentration of the active ingredient is effectively maintained during storage stability testing, and degradation products, oxidation products, and/or impurities which are typically observed in storage stability testing of such formulations are absent or significantly reduced during storage stability testing.
- storage stability is determined at a temperature range from about -20°C to about 80°C, about 4°C to about 70°C, about 4°C to about 60°C, about 4°C to about 50°C, about 4°C to about 40°C, or about 4°C to about 30°C.
- storage stability is determined at a relative humidity ("RH") range of greater than about 1 to 5% RH, generally from about 10% RH to about 90% RH, about 20% RH to about 65% RH, or about 30% RH to about 75% RH.
- RH relative humidity
- storage stability is determined under inert gas, such as nitrogen, argon, and the like.
- time intervals for measuring storage stability that range, for example, from about 1 week to 5 years, from about 2 weeks to about 4 months, or at intervals of 2 weeks, 4 weeks, 8 weeks, 12 weeks, 16 weeks, 6 months, and 12 months.
- storage stability of a given composition is determinative when the composition is stored under the desired conditions suitable for a given end use, and stable for a period of about or greater than about 3 to 6 months, typically about 1 year or greater. Storage stability can be assessed by various techniques well known in the art.
- storage stability can be measured qualitatively and/or quantitatively, directly and/or indirectly, by various techniques known in the art, such as by chromatography (e.g., HPLC, Mass-Spectrophotometry etc.), enzymatically (measuring substrate consumption and/or modification, or product and/or by-product production), antigen-antibody binding (e.g., Western Blot, Enzyme-Linked Immunosorbent Assay (ELISA) etc.), by biological effect (e.g., pharmacological bioavailability by indirect measure of amount of the peptide active agent that enters the blood stream, such as illustrated in the experimental section below), and the like.
- chromatography e.g., HPLC, Mass-Spectrophotometry etc.
- enzymatically measuring substrate consumption and/or modification, or product and/or by-product production
- antigen-antibody binding e.g., Western Blot, Enzyme-Linked Immunosorbent Assay (ELISA) etc.
- biological effect e.
- Storage stable pharmaceutical and/or diagnostic formulations of the subject disclosure include those which maintain the initial concentration of the peptide active agent at a level that meets or exceeds The United States Food and Drug Administration (FDA) regulatory standards for peptide pharmaceuticals.
- FDA United States Food and Drug Administration
- specific formulations of the disclosure maintain the initial concentration of the peptide active agent for a period of greater than about 6 months, and in certain embodiments, for a period of greater than about 12 months, including up to about 2 years, while the average impurity concentration is less than about 1 %, typically less than about 0.1%.
- the mucosal delivery activity in specific embodiments is reduced by 10% at the most, and the pharmacokinetic and/or pharmacological parameters do not show any substantial change.
- the peptide complex and/or peptide salt and the non-aqueous hydrophobic vehicle are combined into a single composition that is administered to the host, in yet other embodiments, the peptide complex and/or peptide salt and non-aqueous hydrophobic vehicle are each individually provided in separate compositions for subsequent combination into a single composition that is administered to the host. In additional embodiments, the peptide salt in the non-aqueous hydrophobic vehicle and/or the crown compound are each individually provided in separate compositions for subsequent combination into a single composition that is administered to the host.
- the peptide complex and/or peptide salt and non-aqueous hydrophobic vehicle can be provided in a single composition, or provided each individually in separate compositions, and various combinations thereof, including in separate reservoirs of a dosage form or device, for subsequent combination as part of a delivery system of the disclosure, or any effective variation thereof.
- the peptide complex and/or peptide salt and the other mucosal delivery composition components are each individually combined in an effective amount, i.e., a biologically relevant amounts.
- the peptide active agent comprises about 0.001 -10% by weight of the mucosal delivery composition, usually about 0.01-5%, about 0.01-3%, and more generally about 0.01-2%, with the balance being the remaining components of the mucosal delivery composition.
- compositions are combined in amounts for mucosal delivery of an effective amount of the peptide active agent.
- Such compositions therefore comprise effective mixtures of their constituent components suitable for this purpose and corresponding given end use.
- the mucosal delivery composition in general comprises an effective mixture of about 0.1-50% by weight peptide complex or peptide salt, and about 50-99.9% by weight non-aqueous hydrophobic vehicle, balance being substantially one or more additional pharmaceutically acceptable excipients.
- the non-aqueous hydrophobic vehicle comprises at least one acylglycerol, at least one organic solvent such as a water soluble organic solvent, and optionally at least one lipid.
- the peptide dried or lyophilized at the desired pH with the counter ions of choice, can be dissolved or suspended in the organic solvent, 1 % to 50% v/v to the final mixture composition, more precisely 3% to 25%, 5% to 20%, 6% to 15%v/v to the final mixture composition, optionally with water 0.1 % to 15% v/v to the organic solvent and the crown structure.
- the acylglycerol is added with optionally the second organic solvent (non-ionic surfactant) and optionally the lipid.
- the non-aqueous hydrophobic vehicle comprises at least one acylglycerol, at least one lipid, and optionally, at least one organic solvent, such as a water soluble organic solvent.
- the acylglycerol comprises up to about 80% by weight of the mucosal delivery composition, such as about 20-80%, about 30-70%, about 40-60%, and generally about 45-55%.
- the lipid component comprises about 5-60% by weight of the mucosal delivery composition, such as about 10-50%, usually about 20-40%.
- the organic solvent comprises about 1-50% by weight of the mucosal delivery composition, usually about 5-30%, and typically about 5-10%, depending on the organic solvent or system.
- the mucosal delivery composition comprises an effective mixture of about 0.1-20% by weight peptide complex or peptide salt, about 35-55% by weight acylglycerol, and about 30-50% by weight lipid, balance being substantially one or more additional pharmaceutically acceptable excipients.
- the mucosal delivery composition comprises an effective mixture of about 0.1-15% by weight peptide complex or peptide salt, about 45-55% by weight acylglycerol, and about 30-45% by weight lipid, balance being substantially one or more additional pharmaceutically acceptable excipients, where the acylglycerol is selected from a monoacylglycerol, diacylglycerol, and mixtures thereof, and the lipid is a permeability-enhancing lipid selected from a neutral lipid, a charged lipid, or a mixture thereof.
- the acylglycerol is a monoacylglycerol such as mono-decanoyl glycerol and/or octanoyl glycerol
- the permeability-enhancing lipid comprises a mixture of short chain and medium chain saturated or unsaturated fatty acids having 7-19 carbon atoms such as nonanoic acid and oleic acid, and/or comprises a neutral lipid such as vitamin E.
- the mucosal delivery composition comprises an effective mixture of about 0.1-15% by weight peptide complex or peptide salt, about 35-55% by weight acylglycerol, about 30-45% by weight lipid, and about 5-15% by weight water-soluble organic solvent, balance being substantially one or more additional pharmaceutically acceptable excipients.
- the acylglycerol is selected from a monoacylglycerol, a diacylglycerol, or mixtures thereof
- the lipid is a permeability-enhancing lipid selected from a neutral lipid, a charged lipid, or mixtures thereof
- the water-soluble organic solvent is selected from a polar solvent, and a polar aprotic solvent.
- the acylglycerol is a monoacylglycerol such as mono-decanoyl glycerol and/or octanoyi glycerol
- the permeability-enhancing lipid comprises a mixture of short chain and medium chain fatty acids such as nonanoic acid and oleic acid, or comprises a neutral lipid such as vitamin E
- the water- soluble organic solvent comprises polar solvent such as a diol or polyol, or a polar aprotic solvent such as N-methylpyrrolidone.
- the mucosal delivery composition comprises an effective mixture of about 0.1-15% by weight peptide complex or peptide salt, about 35-45% by weight water-soluble organic solvent, and about 35- 55% by weight acylglycerol, balance being substantially a non-ionic surfactant and optionally one or more additional pharmaceutically acceptable excipients, where the water-soluble organic solvent comprises a mixture of a diol and a polyol, and the acylglycerol is a monoacylglycerol.
- compositions where the diol is glycerol, the polyol is propylene glycol, and the monoacylglycerol is mono-decanoyl-glycerol and/or octanoyi glycerol.
- the non-ionic surfactant comprises about 10-30% by weight of the mucosal delivery composition, and wherein the non-ionic surfactant comprises a polyoxyethylated polyol.
- a particular polyoxyethylated poiyol of interest is polyoxyl 35 castor oil
- the mucosal delivery composition comprises an effective mixture of about 0.1-15% by weight peptide complex or peptide salt, about 5-25% by weight water-soluble organic solvent, and about 45-55% by weight acylglycerol, balance being substantially a non-ionic surfactant, a permeability-enhancing fatty acid, and optionally one or more additional pharmaceutically acceptable excipients, and wherein the water-soluble organic solvent is a polar aprotic solvent that optionally includes polyethylene glycol, and the acylglycerol is a monoacylglycerol.
- the polar aprotic solvent is N-methylpyrrolidone
- the monoacylglycerol is a medium chain monoacylglycerol such as mono- decanoyl-glycerol and/or octanoyl glycerol
- the polyethylene glycol is a short chain polyethylene glycol diol, such as a polyethylene glycol diol selected from hexaethylene glycol, PEG 300, PEG 400, and mixtures thereof.
- non-ionic surfactant comprises about 10-30% by weight of the mucosal delivery composition, and wherein the non-ionic surfactant comprises a polyoxyethylated polyol, such as polyoxyl 35 castor oil (Cremophor EL).
- a polyoxyethylated polyol such as polyoxyl 35 castor oil (Cremophor EL).
- a mucosal delivery composition that comprises an effective mixture of about 0.1-15% by weight peptide complex or peptide salt, about 5-25% by weight water-soluble organic solvent, about 45-55% by weight acylglycerol, about 15-25% by weight permeability-enhancing fatty acid, about 10-30% by weight non-ionic surfactant; balance being optionally one or more additional pharmaceutically acceptable excipients, and wherein the water- soluble organic solvent is a polar aprotic solvent that optionally includes polyethylene glycol, the acylglycerol is a monoacylglycerol, the non-ionic surfactant comprises a polyoxyethylated polyol, and wherein the permeability- enhancing fatty acid is a saturated or unsaturated fatty acid having 7-19 carbon atoms.
- the polar aprotic solvent is N-methylpyrrolidone
- the monoacylglycerol is a medium chain monoacylglycerol such as mono-decanoyl-glycerol and/or octanoyl glycerol
- the polyethylene glycol is a short chain polyethylene glycol diol (such as hexaethylene glycol, PEG 300, PEG 400, and mixtures thereof)
- the non-ionic surfactant comprises a polyoxyethylated polyol (such as polyoxyl 35 castor oil (Cremophor EL))
- the permeability-enhancing fatty acid is a saturated fatty acid selected from caprylic acid, octanoic acid, nonanoic acid, decanoic acid, undecanoic acid, dodecanoic acid, myristic acid, palmitic acid, stearic acid, arachidic acid, and mixtures thereof, and/or a an unsaturated fatty acid
- compositions in which the permeability-enhancing fatty acid is a saturated fatty acid having 7-12 carbon atoms selected from caprylic acid, octanoic acid, nonanoic acid, decanoic acid, undecanoic acid, dodecanoic acid, and mixtures thereof.
- a particular embodiment is such a composition where the permeability-enhancing fatty acid is nonanoic acid.
- a featured composition comprises a non-aqueous hydrophobic vehicle that is a combination of a monoacylglycerol such as mono-decanoyl- glycerol and/or octanoyl glycerol, a mixture of saturated or unsaturated permeability enhancing fatty acids having 7-21 or 7-19 carbon atoms such as nonionic and oleic acid, and a polar aprotic solvent such as N-methyl-2- pyrrolidone.
- a monoacylglycerol such as mono-decanoyl- glycerol and/or octanoyl glycerol
- saturated or unsaturated permeability enhancing fatty acids having 7-21 or 7-19 carbon atoms such as nonionic and oleic acid
- a polar aprotic solvent such as N-methyl-2- pyrrolidone
- a featured composition comprises a non-aqueous hydrophobic vehicle that is a combination of glycerol, propylene glycol, a monoacylglycerol such as mono-decanoyl-glycerol and/or octanoyl glycerol, a polyethoxylated polyol such as polyoxyethylated 35 castor oil (Cremophor EL), and optionally a short chain PEG diol such as hexaethylene glycol, PEG 300 or PEG 400.
- a non-aqueous hydrophobic vehicle that is a combination of glycerol, propylene glycol, a monoacylglycerol such as mono-decanoyl-glycerol and/or octanoyl glycerol, a polyethoxylated polyol such as polyoxyethylated 35 castor oil (Cremophor EL), and optionally a short chain PEG diol such
- a featured composition comprises a non-aqueous hydrophobic vehicle that is a combination of N-methyl-2-pyrrolidone, a monoacylglycerol such as mono-decanoyl-glycerol and/or octanoyl glycerol, a polyethoxylated polyol such as polyoxyethylated 35 castor oil (Cremophor EL), a medium chain saturated fatty acid such as nonanoic acid, and optionally a short chain PEG dioi such as hexaethylene glycol, PEG 300 or PEG 400.
- a non-aqueous hydrophobic vehicle that is a combination of N-methyl-2-pyrrolidone, a monoacylglycerol such as mono-decanoyl-glycerol and/or octanoyl glycerol, a polyethoxylated polyol such as polyoxyethylated 35 castor oil (Cremophor EL
- a featured aspect is where the peptide active agent in the above formulations is human insulin, exendin-4, or Iiraglutide (or pharmaceutically acceptable analogues/derivatives thereof), and the composition further comprises an antioxidant such as N-acetyl-methionine, and preferably a buffer.
- a preferred organic solvent to be used for the compositions of the invention is a polyol.
- Preferred polyols are propylene glycol and glycerol or a mixture of the two.
- the LogP of the propylene glycol and glycerol are both negative and about in the range of the water, thus being a preferred replacement for water.
- the stably hydrated peptide active agent is complexed with (i) a crown compound selected from an 18-crown-6 and oxo crown analogues/derivatives thereof, and (ii) a counter ion selected from salicylic acid, acetic acid, phosphate, sodium, potassium, N- acetyl-lysine-amide, N-acetyl-arginine-amide, and mixtures thereof, wherein the pH of the composition is different from the isoelectric point of the peptide active agent, particularly where the pH of the composition is remote from the isoelectric point of the peptide active agent, and more particularly where the composition includes a buffer.
- a crown compound selected from an 18-crown-6 and oxo crown analogues/derivatives thereof
- a counter ion selected from salicylic acid, acetic acid, phosphate, sodium, potassium, N- acetyl-lysine-amide, N-acetyl-arginine-amide
- Salicylic acid and acetic acid are of specific interest for many embodiments.
- the level of each component that makes up these mixtures is described in detail above, and in the experimental section below, and partially dependent on benefits sought by the formulator, and thus may also beneficially include one or more additional pharmaceutically acceptable excipients.
- compositions described above can be used directly or adapted in other dosage forms for mucosal administration for use in the subject methods.
- the compositions can be dosed in a variety of product forms and, or package delivery options.
- the compositions of the present disclosure provide improved activity while minimizing potential side effects.
- the stably hydrated peptide active agent is typically in complex with a crown compound and/or a counter ion, however, the free form of the stably hydrated peptide active agent is also useful in the present disclosure.
- the mucosal delivery compositions of the disclosure contain the stably hydrated peptide active agent in an essentially non-aggregated and non-oxidized form.
- non-aqueous hydrophobic vehicle of interest is normally a semi-solid, gel or liquid at ambient or room temperatures based on the selection of the components of the composition described above. Accordingly, there are mixtures of these components that are particularly preferred for certain embodiments of the present disclosure.
- compositions comprising a non-aqueous hydrophobic vehicle composed of a mixture of an acylglycerol, fatty acids, and a water soluble organic solvent, are provided that have different melting points.
- the mucosal delivery composition can be readily provided as a liquid or as a gel or solid dosage form designed to dissolve in the mouth of mammal.
- a non-aqueous hydrophobic vehicle of specific interest comprises about 8% by weight NMP, about 50% by weight mono-decanoyl glycerol, about 20% by weight nonanoic acid, and about 15% by weight oleic acid.
- This mixture is a solid at 19-20°C, definitely a liquid a 38-40°C, but soft or beginning to melt at 25-30°C.
- a solid formulation of this composition can be made by exposure to a cold plate or mold, where the liquid is placed in well on the cold plate to solidify and form a pill structure. When placed in the mouth of a mammal, it melts in about 1 minute.
- the formulation can be adjusted to increase percentage of mono-dodecanol glycerol (10-15% more to increase melting temp by about 2-3°C) to increase melting temperature of the formulation.
- nonanoic acid is liquid whereas decanoic acid is solid at room temperature, and oleic acid is liquid at room temperature and solid at 4°C
- the length of the fatty acid can be increased, e.g., add or substitute decanoic acid for nonanoic to form a mucosal delivery composition having a melting point of about 35°C to 40°C.
- formulation of the non-aqueous hydrophobic vehicle is afforded great flexibility in terms of dosage form design when employed in combination with a stably hydrated peptide complex of the disclosure.
- the mucosal delivery composition is a pharmaceutical and/or diagnostic composition which may include one or more additional pharmaceutically acceptable excipients, with the proviso that such excipients are compatible with maintaining the peptide complex.
- Pharmaceutically and/or diagnostically acceptable excipients are also well-known to those who are skilled in the art and are readily available. The choice of excipient will be determined in part by the particular composition, as well as by the particular method used to administer the composition. Accordingly, there are a wide variety of suitable formulations of the pharmaceutical and/or diagnostic compositions of the present disclosure.
- the peptide complex or peptide salt combined with the non-aqueous hydrophobic vehicle can be used alone (i.e., 100% by weight of the pharmaceutical and/or diagnostic composition), or admixed with conventional pharmaceutically and/or diagnostically acceptable carriers and excipients if desired and used in the form of solutions, tablets, capsules, elixirs, suspensions, syrups, wafers, and the like.
- Such pharmaceutical compositions contain, in certain embodiments, up to about 99.975% by weight of the peptide complex combined with the non-aqueous hydrophobic vehicle, depending on the dosage form and intended end use.
- the pharmaceutical and/or diagnostic composition will generally contain from about 0.001 to 10% of the stably hydrated peptide active agent, typically about 0.05% to 5% of the stably hydrated peptide active agent, usually about 0.01 to 3% of the stably hydrated peptide active agent, and more generally, about 0.1 % to 2% of the stably hydrated peptide active agent for a given unit dose.
- the peptide complex combined with the nonaqueous hydrophobic vehicle of the present disclosure will comprise from about 60% to about 99.975%, usually from 70% to about 99% and most often from about 85% to about 98% by weight of the pharmaceutical composition.
- the pharmaceutical and/or diagnostic compositions may be administered alone or as part of a drug delivery system that maintains the peptide formulation in a drug transferring relationship with a target mucosal membrane, such as an oral mucosal membrane like a buccal membrane and/or sublingual membrane.
- a target mucosal membrane such as an oral mucosal membrane like a buccal membrane and/or sublingual membrane.
- the peptide formulation can be in a free form, such as a liquid, gel, cream, foam, ointment, or semi-solid, or can comprise a device of determined physical form, such as spray, tablets, patches, and troches, for example, as described in U.S. Patent Nos.
- compositions of the disclosure may also be used in combination with other active agents as excipients in this context, including incorporation of the peptide active agent with a non-peptide active agent, or two or more peptide active agents, and so forth, in the same composition.
- compositions of the disclosure may find more beneficial use for specific routes of administration involving mucosal surfaces, including oral mucosal membranes, airway surfaces, gut and the like.
- pharmaceutical compositions for oral mucosal delivery are of specific interest, particularly pharmaceutical compositions for buccal and/or sublingual delivery.
- pharmaceutical and/or diagnostic compositions of the disclosure that comprise a stably hydrated peptide active agent in an oral mucosal delivery vehicle are of particular interest.
- the pharmaceutical and/or diagnostic composition may optionally contain other pharmaceutically and/or diagnostically acceptable components, such a buffers, surfactants, antioxidants, bacteriostats, viscosity modifying agents, suspending agents, solubilizers, stabilizers preservatives and the like.
- a buffers such as a buffers, surfactants, antioxidants, bacteriostats, viscosity modifying agents, suspending agents, solubilizers, stabilizers preservatives and the like.
- the formulations can be presented in unit-dose or multi-dose sealed containers, such as ampules and vials, spray containers, tablets and the like, or can be stored in a freeze-dried (lyophilized) condition requiring only the addition of a suitable sterile liquid excipient immediately prior to use.
- Extemporaneous solutions and suspensions can be prepared from sterile powders, granules, and tablets of the kind previously described.
- unit dosage forms for oral administration such as semi-solids, gels, syrups, elixirs, tablets and suspensions may be provided wherein each dosage unit, for example, teaspoonful, tablespoonful, or tablet, contains a predetermined amount of the composition containing the peptide active agent in the mucosal delivery vehicle.
- unit dosage form refers to physically discrete units suitable as unitary dosages for human and animal subjects, each unit containing a predetermined quantity of compounds of the present disclosure calculated in an amount sufficient to produce the desired effect in association with a pharmaceutically acceptable diluent, carrier or vehicle.
- the specifications for the novel unit dosage forms of the present disclosure depend on the particular compound employed and the effect to be achieved, and the pharmacodynamics associated with each compound in the host.
- dose levels can vary as a function of the specific compound, the nature of the delivery vehicle, and the like. Suitable dosages for a given compound are readily determinable by those of skill in the art by a variety of means.
- the dose administered to an animal, particularly a human, in the context of the present disclosure should be sufficient to cause a prophylactic or therapeutic response in the animal over a reasonable time frame.
- dosage will depend on a variety of factors including the strength of the particular compound employed, the condition of the animal, and the body weight of the animal, as well as the severity of the illness and the stage of the disease.
- the size of the dose will also be determined by the existence, nature, and extent of any adverse side-effects that might accompany the administration of a particular compound. Suitable doses and dosage regimens can be determined by comparisons to agents that are known to cause the desired response.
- the mucosal delivery composition is comprised as a dosage form selected from the group consisting of buccal, sublingual, and a combination thereof.
- the subject methods find use in a variety of applications. Examples include as reagents, diagnostics, and pharmaceutical agents for treatment of a host of interest.
- the methods of treatment involve administering a composition of the disclosure to a mucosal membrane of a host in need thereof, such as for the treatment of a host suffering from disease or condition treatable by a peptide active agent.
- An aspect of the subject methods is that an effective amount of the composition is administered to deliver an effective amount of the peptide active agent into the blood stream of the host.
- the mucosal delivery composition is an oral mucosal delivery composition
- the mucosal membrane is an oral mucosal membrane.
- a method of mucosal delivery of an effective amount of a peptide active agent to a host in need thereof comprising: administering to a mucosal membrane of the host an effective amount of a mucosal delivery composition and/or peptide complex of the disclosure, wherein the administering delivers an effective amount of the peptide active agent into the blood stream of the host.
- the mucosal membrane is an oral mucosal membrane, such as an oral mucosal membrane selected from the group consisting of buccal, sublingual, and combinations thereof.
- sublingual administration of the composition results in a pharmacological bioavailability of the peptide active agent that is greater than about 10%, preferably greater than about 15%, and more preferably about 20% or greater, relative to intrapleural (pi) administration.
- the peptide active agent is generally one that is capable of mucosal delivery in the subject formulations.
- the methods are methods of modulating at least one cellular function associated with the peptide active agent.
- the subject methods and compositions find use in known applications of many peptide active agents, such as in treating diseases or disorders that are capable of being treated using the peptide active agent.
- Use of the subject compositions of the present disclosure is of particular utility in, for example, the treatment of diseases and disorders where a gradual (e.g., gastrointestinal mucosal delivery) or rapid (e.g., oral mucosal delivery) onset of effect is desired, without the need for injection.
- the subject methods and compositions find particular use in therapeutic applications in which administration of a given peptide active agent is indicated.
- the peptide active agent is a peptide hormone, such as insulin, calcitonin, parathyroid hormone, an incretin mimetic peptide such as a glucagon-like peptide, and the like.
- a representative therapeutic application is in the treatment of diabetes, obesity and related conditions using a composition of the disclosure in which the peptide active agent is, for instance, insulin, and/or an incretin mimetic peptide, such as exendin-4 or liraglutide.
- treatment is meant that at least an amelioration of the symptoms associated with the condition afflicting the host is achieved, where amelioration is used in a broad sense to refer to at least a reduction in the magnitude of a parameter, e.g. symptom, associated with the condition being treated.
- amelioration also includes situations where the pathological condition, or at least symptoms associated therewith, are completely inhibited, e.g., prevented from happening, or stopped, e.g. terminated, such that the host no longer suffers from the condition, or at least the symptoms that characterize the condition.
- a specific application of interest is the use of peptide active agents in the mucosal delivery vehicle compositions of the disclosure, particularly insulin, exendin-4, glucagon-like peptide 1 , liraglutide, and analogues/derivatives thereof, to decrease blood glucose levels in the host.
- the condition is type II diabetes.
- Another specific application of interest is the use of peptide active agents in the mucosal delivery vehicle compositions of the disclosure, particularly exendin-4, liraglutide, and analogues/derivatives thereof, for the reduction of the weight of the host.
- a method for the treatment of a host in need thereof an effective amount of a pharmaceutical agent of the disclosure that comprises a peptide active agent selected from insulin, exendin-4, liraglutide, glucagon-like peptide 1 , and analogues/derivatives thereof.
- a pharmaceutical agent of the disclosure that comprises a peptide active agent selected from insulin, exendin-4, liraglutide, glucagon-like peptide 1 , and analogues/derivatives thereof.
- Reduction of blood glucose levels is characterized by the prevention, mitigation, or reduction of the likelihood of onset of hyperglycemia resulting from elevated blood glucose levels.
- Reduction of weight is characterized by the prevention, mitigation, or reduction of the likelihood of onset of obesity or weight gain resulting from one or more of elevated blood glucose levels, gastric emptying, and food intake.
- This includes, for example, treatment of a host in need thereof with an effective amount of an GLP active agent in an mucosal delivery vehicle of the disclosure to reduce blood glucose levels, delay gastric emptying, and/or decrease food intake in the host.
- GLP active agent is intended exendin-4, liraglutide, and pharmaceutically acceptable analogues/derivatives thereof.
- hyperglycemia can easily be assessed by standard techniques known in the art, such as by measuring blood glucose levels.
- gastric emptying, decrease in food intake, and the weight of a host can be readily determined.
- the effect of treatment with the GLP active agent can readily be determined using any, or all, of these test systems.
- hosts are treatable according to the subject methods.
- Such hosts are "mammals” or “mammalian,” where these terms are used broadly to describe organisms which are within the class mammalia, including the orders carnivore (e.g., dogs and cats), rodentia (e.g., mice, guinea pigs, and rats), and primates (e.g., humans, chimpanzees, and monkeys).
- the subjects will be humans.
- the hosts will be subjects that have been diagnosed for and are, therefore, in need of administration of the active agent.
- the methods may include diagnosing the subject for the presence of the disease condition to be treated by administration of the peptide active agent.
- the dose administered to an animal, particularly a human, in the context of the present disclosure should be sufficient to affect a prophylactic or therapeutic response in the animal over a reasonable time frame.
- dosage will depend on a variety of factors including the strength of the particular peptide active agent employed, the dose of the peptide active agent, the dosing regimen used for peptide active agent, the condition of the animal, and the body weight of the animal, as well as the severity of the illness and the stage of the disease.
- the size of the dose will also be determined by the existence, nature, and extent of any adverse side-effects that might accompany the administration of a particular peptide active agent. This will generally follow the dose and dosing profile for treatment of a condition for which the peptide active agent is indicated and/or empirically determined following routine methods.
- exendin-4 and liraglutide can be used in combination with metformin, a sulfonylurea, or a thiazolidinedione, as well as in conjunction with standard insulin therapy to manage blood glucose levels for type II diabetes.
- standard therapies for example, exendin-4 and liraglutide can be used in combination with metformin, a sulfonylurea, or a thiazolidinedione, as well as in conjunction with standard insulin therapy to manage blood glucose levels for type II diabetes.
- Such treatment regiments are well known to those of ordinary skill in the art.
- a featured embodiment is the use of a mucosal delivery composition that is an oral mucosal delivery composition of the disclosure, and wherein the oral mucosal delivery composition comprises a peptide active agent selected from insulin, exendin-4, liraglutide, glucagon-like peptide 1 , and analogues/derivatives thereof, for treatment of a host in need thereof, for instance, to treat one or more conditions described above for these compounds.
- a peptide active agent selected from insulin, exendin-4, liraglutide, glucagon-like peptide 1 , and analogues/derivatives thereof
- kits and systems comprising one or more compositions of the present disclosure, as well as those that find use in practicing the subject methods, as described above.
- the kit comprises an effective amount of a mucosal delivery composition, and/or components thereof that are each individually separate and/or provided in various combinations in the kit in effective amounts capable of forming the mucosal delivery composition upon combination.
- the kit comprises: (i) a first composition comprising the stably hydrated peptide active agent complexed with the crown compound and the counter ion, and (ii) a second composition comprising the non-aqueous hydrophobic vehicle.
- kits comprises: (i) a first composition comprising the stably hydrated peptide active agent complexed with the counter ion in the non-aqueous hydrophobic vehicle, and (ii) a second composition comprising the crown compound.
- a first composition comprising the stably hydrated peptide active agent complexed with the counter ion in the non-aqueous hydrophobic vehicle
- a second composition comprising the crown compound.
- Kits and systems for practicing the subject methods may include one or more pharmaceutical and/or diagnostic formulations.
- the kits may include a single pharmaceutical and/or diagnostic composition, present as one or more unit dosages, where the composition includes the peptide active agent predisposed in the mucosal delivery composition.
- the kits may include two or more separate pharmaceutical and/or diagnostic compositions, each containing either the stably hydrated peptide active agent in complex with the crown and counter ion, or non-aqueous hydrophobic composition, and any effective variation thereof.
- the mucosal delivery composition employed in, or capable of being formed by, the kits and systems of the disclosure is an oral mucosal delivery composition.
- the subject kits may further include instructions for practicing the subject methods. These instructions may be present in the subject kits in a variety of forms, one or more of which may be present in the kit.
- One form in which these instructions may be present is as printed information on a suitable medium or substrate, e.g., a piece or pieces of paper on which the information is printed, in the packaging of the kit, in a package insert, etc.
- Yet another means would be a computer readable medium, e.g., diskette, CD, etc., on which the information has been recorded.
- Yet another means that may be present is a website address which may be used via the internet to access the information at a removed site. Any convenient means may be present in the kits.
- kits includes as a first component (a) instructions for using a pharmaceutical and/or diagnostic composition of the present disclosure, and as a second component (b) a pharmaceutical and/or diagnostic composition of the present disclosure.
- Kits of specific interest are those that include a pharmaceutical and/or diagnostic composition of the disclosure and suitable for practicing the subject methods of the disclosure, such as for reducing blood glucose levels, delaying gastric emptying, and/or reducing food intake in a host.
- system refers to a collection of the components of a peptide formulation of the disclosure, present in a single or disparate composition, that are brought together for the purpose of practicing the subject methods.
- peptide or peptide forms brought together and admixed with a mucosal delivery vehicle or its components for administering to a host, according to the present disclosure, are a system according to the present disclosure.
- the subject methods and compositions for peptide delivery directly through mucosal membranes offer advantages over other routes of administration.
- a particular route of interest is via oral mucosal delivery.
- drugs administered through oral mucosal membranes have a rapid onset of action, provide therapeutic plasma levels, avoid first pass effect of hepatic metabolism, and avoid exposure of the drug to the hostile Gl environment. Additional advantages include easy access to the membrane sites so that the drug can be applied, localized and removed easily. Further, there is a good potential for prolonged delivery of large molecules through these membranes.
- the oral mucosa in general has excellent accessibility, an expanse of smooth muscle, and a relatively immobile mucosa, and is hence suitable for the administration of retentive dosage forms.
- Direct access to the systemic circulation through the internal jugular vein allows drugs to bypass the hepatic first-pass metabolism, leading to high bioavailability.
- Other advantages include low enzymatic activity, suitability for drug excipients that mildly and reversibly damage or irritate the mucosa, painless administration, easy drug withdrawal, facility to include a permeation enhancer/enzyme inhibitor or pH modifier in the formulation, and versatility in the design of multidirectional or unidirectional release systems for local or systemic action.
- the mucosa lining the oral cavity represents an important topical route for the delivery of large therapeutic compounds such as peptides in accordance with the present disclosure.
- oral mucosal or other mucosal delivery routes may offer certain advantages over injection and other modes of administration including convenience and speed of delivery, as well as by reducing or elimination of compliance problems and side effects that attend delivery by injection.
- Peptides were optionally desalted by Reverse Phase High Performance Chromatography (RP-HPLC) (solvents were water and acetonitrile in the presence of 1 % acetic acid) and lyophilized (i.e., freeze dried at less than room temperature). Depending on the p/ of the molecule, the molecule is either utilized as it is in lyophilized form, or when required, re-dissolved or suspended in water or water/acetonitrile mixtures. The pH of the obtained solution or suspension was then brought to a desired value ranging from 4 to 7.5 such that the pH was sufficiently different from the p/ of the molecule to insure solubility in various solvents employed in subsequent counter ion exchange and/or complexing reactions.
- RP-HPLC Reverse Phase High Performance Chromatography
- glucagon-like peptides such as exendin-4 and liraglutide were prepared by the careful and/or gradual addition of a base to obtain the desired pH (e.g., sodium or potassium bicarbonate, amino acids as Lys or Arg and protected derivatives such as N-acetylated and/or amidated versions).
- the desired pH e.g., sodium or potassium bicarbonate, amino acids as Lys or Arg and protected derivatives such as N-acetylated and/or amidated versions.
- the desired pH e.g., sodium or potassium bicarbonate, amino acids as Lys or Arg and protected derivatives such as N-acetylated and/or amidated versions.
- the desired pH e.g., sodium or potassium bicarbonate, amino acids as Lys or Arg and protected derivatives such as N-acetylated and/or amidated versions.
- the obtained solution or suspension was if necessary filtered through a 0.45 prn filter and lyophilized at this given pH ranging from
- Stabilizing excipients such as mannitol may also be included in the solvent for RP-HPLC, and/or in the water/acetonitrile mixtures following RP- HPLC, provided the excipient(s) is added in an amount that dissolves in the mixture (typically 0,1 -20%).
- Peptide counter ion (usually acetate counter ion) was alternatively substituted by acidic compounds such as salicylic acid, different substituted or not benzoic acid derivatives, oxalic acid, sulfonates, sulfates such as lauryl sulfate, phosphatidylglycerol derivatives such as dilaurylphosphatidyl glycerol (DLPG), phosphoric acid, trifluoroacetic acid or chloride.
- acidic compounds such as salicylic acid, different substituted or not benzoic acid derivatives, oxalic acid, sulfonates, sulfates such as lauryl sulfate, phosphatidylglycerol derivatives such as dilaurylphosphatidyl glycerol (DLPG), phosphoric acid, trifluoroacetic acid or chloride.
- acidic compounds such as salicylic acid, different substituted or not benzoic acid derivatives, ox
- the peptide acetate was converted to salicylate salt by the following treatment.
- Salicylic acid 138.12 g/mol
- ACN/H 2 0 50/50 mixture was dissolved in ACN/H 2 0 50/50 mixture to give the mother solution.
- Fixed volume of this latter solution containing fixed quantity of salicylic acid in a ratio of 1 to n equivalents regarding peptide/protein basic amino acid content
- a small amount of a non-ionic detergent such as beta-D-octylglucoside 0.05% to 10%, more preferably 0.1 % to 5%
- mannitol 10-20% final concentration in the formulation mixture
- glycerol 1 % final concentration in the formulation mixture
- the obtained solution was dried/concentrated for 1 hour using a centrifugal evaporator / SpeedVac (at 25°C-40°C, typically around 35°C), then ACN/H 2 0 50/50 was added and this solution dried/concentrated by SpeedVac (at 25°C-40°C, typically around 35°C) for an additional hour, affording peptide salicylate as a white solid.
- STEP 3 Preparation of the peptide-crown compound complex
- the peptide salt was dissolved in MeOH or MeOH/hbO mixtures (water content ranging from 1 to 15%) and appropriate amount of cyclic crown compound dissolved in MeOH or MeOH/H 2 0 mixtures added (containing fixed quantity of crown compound in a ratio of 1 to n equivalents regarding peptide/protein basic amino acid content).
- the obtained solution was dried/concentrated for 1 hour in a SpeedVac (at 25°C-40°C, typically around 35°C), to generate an oily residue comprising the peptide sa!t-crown compound complex.
- an organic solvent such as DMSO, NMP or propylene glycol
- a viscous non-aqueous hydrophobic formulation vehicle was added to peptide-crown compound complex and the resulting mixture vortexed then heated at 40°C for 10 minutes. The obtained limpid preparation was then stored at +4°C.
- Formulation 1 The formulation vehicle was prepared by adding NMP
- the mixture has a phi of between 3.0 and 5.0 (typically around 3.5 - 4.0, depending on addition of Ac-Met-OH anti-oxidant, which is acidic), which could be adjusted by the addition of acid or base and/or buffered depending on the pi of the peptide, and was added to the peptide- crown complex.
- the NMP can be substituted by 14 ⁇ of propylene-glycol, or glycerol or a mixture of the two and the peptide complex forms in situ in the organic solvent. Then the vehicle comprising oleic acid (40 ⁇ ), nonanoic acid (50 ⁇ ) and decanoyl glycerol (130 mg) is added to the peptide complex in the polyol organic mixture.
- Formulation 2 The formulation vehicle was prepared by adding NMP
- Formulation 3 The formulation vehicle was prepared by adding octanoyl glycerol (50 mg), NMP (25 ⁇ ), and vitamin E (50 ⁇ ) to decanoyl glycerol (130 mg). The obtained mixture was heated at 40-45°C in a water bath for complete solubilization. In the case of peptide sequences including residues susceptible to oxidation, 0.25 mg N-acetyl-methionine-amide (Ac- Met-NH 2 ) (190.27 g/mol) for 100 ⁇ formulation mixture were then added as anti-oxidizing agent, and the mixture was heated at 40-45°C in a water bath till a limpid solution was obtained.
- octanoyl glycerol 50 mg
- NMP 25 ⁇
- vitamin E 50 ⁇
- Formulation 3 The formulation vehicle was prepared by adding octanoyl glycerol (50 mg), NMP (25 ⁇ ), and vitamin E (50 ⁇ ) to decano
- the mixture without the peptide has a pH estimated of between 5.5. and 7.0, which could be adjusted by the addition of acid or base and/or buffered depending on the p/ of the peptide, and was added to the peptide-crown complex.
- Formulation 4 The formulation vehicle was prepared by adding a mixture of span 20 (60 ⁇ ) and oleic acid (50 ⁇ ) to decanoyl glycerol (1 10 mg). The obtained mixture was heated at about 45°C in a water bath for complete solubilization. In this case, the peptide complex was obtained by dissolving the peptide in 14 ⁇ propylene glycol containing the crown compound. After 15 mn at room temperature, the formulation vehicle was added to the peptide-crown complex in propylene glycol.
- Formulation 5 The formulation vehicle was prepared by adding a mixture of span 20 (60 ⁇ ), Monolinolein (mono acylglycerol of linoleic acid) (50 ⁇ ) and decanoyl glycerol (1 10 mg). The obtained mixture was heated at about 45°C in a water bath for complete solubilization. In this case, the peptide complex was obtained by dissolving the peptide in 14 ⁇ propylene glycol containing the crown compound. After 15 min at room temperature, the formulation vehicle was added to the peptide-crown complex in propylene glycol.
- non-aqueous hydrophobic vehicles i.e., Formulations 1 to 5
- one or more components may be eliminated or replaced by analogous compounds for other formulations.
- other anti-oxidizing agents such as biotin, biotin ethyl ester or vitamin C can be used.
- Mucosal delivery formulations containing parathyroid hormone, exendin-4, liraglutide, or human insulin were pre-screened for solubility, stability, and/or sublingual mucosal delivery in mice and/or rats using various crown compounds, counter ions, and non-aqueous hydrophobic vehicles in general.
- Representative crown compounds included 18-crown-6, oxo-(18- crown-6), oxo-(18-crown-6)-diethyl tartrate, and oxo-(18-crown-6)-diglycerol tartrate.
- Representative counter ions included TFA, acetate, salicylic acid, DLPG, C 12 H 25 0S0 3 H, C 14 H 2 9S0 3 H, and C 8 H3 7 S0 3 H.
- Representative nonaqueous hydrophobic vehicles included vehicle Formulations 1 , 2 and 3. All peptides were detected in the blood stream to different degrees.
- Exendin-4 (having a calculated isoelectric point of about 5.0) was chosen for further detailed studies, which were carried out in accordance with the procedures and formulations described above in Experimental Section I unless otherwise indicated. Illustrative studies are reported below. III. ANIMAL STUDIES WITH REPRESENTATIVE MUCOSAL DELIVERY FORMULATIONS
- mice or rats used in these studies were age- and sex-matched from the same litter or family for each individual study. All procedures were conducted according to approved protocols and guidelines following standard procedures. Studies for mice are detailed below, and are representative of the rat studies.
- Blood samples were collected at various time points after treatment, and blood glucose levels determined by the glucose oxidase method following standard procedures. All animals remained anesthetized throughout blood collection. Changes in plasma glucose in mice were used to indicate the appearance of bioactive amounts of peptide test articles.
- Test articles were stored at 4°C, and then warmed to 37°C prior to administration. Data were analyzed and reported as mean ⁇ S.E.M. unless otherwise indicated.
- SA DLPG and salicylic acid
- SA are more acidic than acetic acid
- DLPG 610 g/mol, 0.66 mg
- 0.66 mg DLPG diauryloylphosphatidylglycerol
- An additional aliquot of ACN/H 2 0 50/50 was then added followed by drying by speedvac for 1 hour at approximately 35°C.
- Salicylic acid (138.12 g/mol, 0.15 mg) 1.5 mg salicylic acid was dissolved in 100 ⁇ ! ACN/H 2 0 50/50 mixture to give the mother solution. 10 ⁇ of this latter solution were then added to 0.76 mg exendin-4 acetate dissolved in 50 ⁇ ACN/H 2 0 50/50 followed by speedvac 2 x 1 hour as above at approximately 35°C, affording exendin-4 salicylate as a white solid.
- Exendin-4 salts from step A were dissolved in MeOH (50 ⁇ ) and 10 mg 18-crown-6 in 100 ⁇ MeOH were added followed by speedvac 1 hour at approximately 35°C to yield an oily residue.
- Approximately 80 ⁇ of the vehicle Formulation 1 was added to the exendin-4-crown complexes from Step A to obtain approximately 90 ⁇ of formulations F1 , F2 and F3, which were vortexed then heated at 40°C for 10 minutes.
- the obtained preparations were then stored at +4°C until use.
- the formulations were warmed to 37°C, and then 3 ⁇ (approximately 6 nmols exendin-4 test article) of the F1 , F2 and F3 mixtures were administered sublingually to mice.
- the as-administered mucosal delivery composition of Table 1 (with data illustrated in Figure 1 ): 208 stoicheometric equivalents of crown to peptide (i.e., approximately 35 crown molecules per basic amino group), 6 stoicheometric equivalents of counter ion to peptide (i.e., 1 counter ion molecule per basic amino group), resulting in a ratio of 35 crowns per 1 counter ion.
- Table 1 Mucosal delivery compositions as administered ( Figure 1 )
- Figure 2 shows the effect of altering the pH of the non-aqueous hydrophobic vehicle and composition on sublingual administration of exendin- 4.
- Figure 2 Key: F4 exendin-4 peptide with acetate counter ion and oxo-(18- crown-6)-diethyl tartrate ("ST5") crown compound formed in MeOH 100% and speedvac for 1 hour at approximately 35°C, followed by incorporation in Formulation 3.
- F4 exendin-4 peptide with acetate counter ion and oxo-(18- crown-6)-diethyl tartrate (“ST5") crown compound formed in MeOH 100% and speedvac for 1 hour at approximately 35°C, followed by incorporation in Formulation 3.
- the as-administered mucosal delivery composition of Table 2 (with data illustrated in Figure 2): 50 stoicheometric equivalents of crown to peptide (i.e., approximately 8 crown molecules per basic amino group), 12 stoicheometric equivalents of counter ion to peptide (i.e., 2 counter ion molecule per basic amino group), resulting in a ratio of 4 crowns per 1 counter ion.
- Formulation contains 40 nmols Ac-Met-OH
- Figure 2 show that the exendin-4 peptide complex in vehicle Formulation 3 results in reduced sublingual delivery compared to when formulated in a more acidic vehicle such as Formulation 1 , the latter also being further away from the pi of the peptide.
- Exendin-4 contains four primary amines (1 for N-terminus, 2 for the two lysines, and 1 for arginine), and two secondary amines (1 for histidine, and 1 for arginine), for a total of six basic amino groups ionizable under acidic conditions.
- the exendin-4 amino acid sequence is as follows:
- Figure 3 shows the results of adjusting stoicheometric equivalents of counter ion and crown compound (oxo-(18-crown-6) diethyl tartrate) on mucosal delivery in vehicle Formulation 1 .
- a summary of the as-administered mucosal delivery composition is provided in Table 3.
- Figure 4 shows the effect of water content on mucosal delivery of exendin-4.
- Figure 4 Key: F1 exendin-4 peptide complex formed in MeOH 100% and speedvac for 1 hour at approximately 35°C, followed by incorporation in Formulation 1 .
- F2 exendin-4 peptide complex formed in MeOH 100% and speedvac for 1 hour and 20 minutes at approximately 35°C, followed by incorporation in Formulation 1.
- F3 exendin-4 peptide complex formed in MeOH 5% water and speedvac for 1 hour at approximately 35°C, followed by incorporation in Formulation 1 .
- the as-administered mucosal delivery composition of Table 4 (with data illustrated in Figure 4): 12 stoicheometric equivalents of crown to peptide (i.e., approximately 2 crown molecules per basic amino group), 6 stoicheometric equivalents of counter ion to peptide (i.e., 1 counter ion molecule per basic amino group), resulting in a ratio of 2 crowns per 1 counter ion.
- Vehicle Formulation 1 containing 40 nmols Ac-Met-OH
- the data shows that reducing the water content by standard centrifugal evaporation or for longer times decreases biological activity compared to peptide complex formation in a mixed aqueous-methanol solution. Also, reducing the water content may alter the system pH and/or pi of the peptide active agent.
- Multiple additional data sets revealed similar results consistent with the finding that water content of the peptide and pH/p/ of the system is important for activity, including improved solubility in organic solvent and the non-aqueous hydrophobic vehicle when the peptide and/or peptide complex is dried from a solution or suspension having a pH different, typically remote from the pi of the peptide.
- the results demonstrate that selection of the crown compound, counter ion, amounts and ratios of crown to counter ion and ionizable amino groups of the peptide, as well as components and amounts thereof of the non-aqueous hydrophobic vehicle, inclusion of particular excipients, antioxidants and the like, can be exploited to improve or enhance mucosal delivery of peptides, among other aspects such as storage-stability and dosage form.
- the compositions can be readily tailored for multiple different peptides and applications.
Landscapes
- Health & Medical Sciences (AREA)
- Chemical & Material Sciences (AREA)
- Life Sciences & Earth Sciences (AREA)
- Medicinal Chemistry (AREA)
- Pharmacology & Pharmacy (AREA)
- Animal Behavior & Ethology (AREA)
- General Health & Medical Sciences (AREA)
- Public Health (AREA)
- Veterinary Medicine (AREA)
- Epidemiology (AREA)
- Engineering & Computer Science (AREA)
- Bioinformatics & Cheminformatics (AREA)
- Immunology (AREA)
- Dispersion Chemistry (AREA)
- Proteomics, Peptides & Aminoacids (AREA)
- General Chemical & Material Sciences (AREA)
- Chemical Kinetics & Catalysis (AREA)
- Diabetes (AREA)
- Endocrinology (AREA)
- Oil, Petroleum & Natural Gas (AREA)
- Nutrition Science (AREA)
- Physiology (AREA)
- Gastroenterology & Hepatology (AREA)
- Zoology (AREA)
- Nuclear Medicine, Radiotherapy & Molecular Imaging (AREA)
- Obesity (AREA)
- Organic Chemistry (AREA)
- Hematology (AREA)
- Emergency Medicine (AREA)
- Child & Adolescent Psychology (AREA)
- Medicines That Contain Protein Lipid Enzymes And Other Medicines (AREA)
- Medicinal Preparation (AREA)
Abstract
Description
Claims
Priority Applications (8)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| JP2012540439A JP5892940B2 (en) | 2009-11-25 | 2010-11-25 | Mucosal delivery composition comprising a peptide complexed with a crown compound and / or counterion |
| CN201080062361.9A CN102770152B (en) | 2009-11-25 | 2010-11-25 | The mucosal delivery of peptides |
| AU2010323117A AU2010323117B2 (en) | 2009-11-25 | 2010-11-25 | Mucosal delivery compositions comprising a peptide complexed with a crown comppound and/or a counter ion |
| BR112012012945-7A BR112012012945A2 (en) | 2009-11-25 | 2010-11-25 | MUCOSAL RELEASE COMPOSITION, ITS PRODUCTION METHOD, PRE-FORMED PEPTIDE COMPLEX, KIT AND USE OF AN ACTIVE PEPTIDE AGENT |
| EP10781909A EP2504019A2 (en) | 2009-11-25 | 2010-11-25 | Mucosal delivery composition comprising a peptide complexed with a crown compound and/or a counter ion |
| US13/512,001 US9445992B2 (en) | 2009-11-25 | 2010-11-25 | Mucosal delivery compositions comprising a peptide complexed with a crown compound and/or a counter ion |
| CA2782056A CA2782056C (en) | 2009-11-25 | 2010-11-25 | Mucosal delivery of peptides |
| IL220022A IL220022A (en) | 2009-11-25 | 2012-05-28 | Mucosal delivery compositions comprising a peptide complexed with a crown compound and/or a counter ion |
Applications Claiming Priority (2)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US26432409P | 2009-11-25 | 2009-11-25 | |
| US61/264,324 | 2009-11-25 |
Publications (2)
| Publication Number | Publication Date |
|---|---|
| WO2011064316A2 true WO2011064316A2 (en) | 2011-06-03 |
| WO2011064316A3 WO2011064316A3 (en) | 2012-01-05 |
Family
ID=44066984
Family Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| PCT/EP2010/068257 WO2011064316A2 (en) | 2009-11-25 | 2010-11-25 | Mucosal delivery of peptides |
Country Status (9)
| Country | Link |
|---|---|
| US (1) | US9445992B2 (en) |
| EP (1) | EP2504019A2 (en) |
| JP (1) | JP5892940B2 (en) |
| CN (1) | CN102770152B (en) |
| AU (1) | AU2010323117B2 (en) |
| BR (1) | BR112012012945A2 (en) |
| CA (1) | CA2782056C (en) |
| IL (1) | IL220022A (en) |
| WO (1) | WO2011064316A2 (en) |
Cited By (2)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| JP2014516969A (en) * | 2011-05-25 | 2014-07-17 | アリスジェン ソシエテ アノニム | Mucosal administration of drugs |
| WO2017140770A1 (en) | 2016-02-19 | 2017-08-24 | Forschungszentrum Borstel Leibniz-Zentrum Für Medizin Und Biowissenschaften | Means and methods for treating bacterial infections |
Families Citing this family (4)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US9782344B2 (en) * | 2013-08-22 | 2017-10-10 | Zp Opco, Inc. | Stable glucagon peptide formulations |
| WO2015027173A1 (en) * | 2013-08-22 | 2015-02-26 | Zp Opco, Inc. | Stable glucagon peptide formulations |
| US10564140B2 (en) * | 2017-04-10 | 2020-02-18 | BUFFERAD Illinois Inc. | Diffusion cell testing methods and system containing biphasic receptor fluids |
| WO2024040356A1 (en) * | 2022-08-25 | 2024-02-29 | The University Of British Columbia | Mucoadhesive pharmaceutical dosage form for unidirectional release of peptide therapeutic particles |
Citations (164)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US4226848A (en) | 1979-03-05 | 1980-10-07 | Teijin Limited | Method and preparation for administration to the mucosa of the oral or nasal cavity |
| US4292299A (en) | 1978-11-06 | 1981-09-29 | Teijin Limited | Slow-releasing medical preparation to be administered by adhering to a wet mucous surface |
| US4511505A (en) | 1979-04-13 | 1985-04-16 | Shionogi & Co., Ltd. | Semi-synthesis of human insulin |
| US4517173A (en) | 1980-09-26 | 1985-05-14 | Nippon Soda Co. Ltd. | Mucous membrane-adhering film preparation and process for its preparation |
| US4552751A (en) | 1980-10-17 | 1985-11-12 | Ono Pharmaceutical Co., Ltd. | Long-lasting multi-layered film preparation |
| US4572832A (en) | 1982-10-07 | 1986-02-25 | Grelan Pharmaceutical Co., Ltd. | Soft buccal |
| US4615697A (en) | 1983-11-14 | 1986-10-07 | Bio-Mimetics, Inc. | Bioadhesive compositions and methods of treatment therewith |
| US4671953A (en) | 1985-05-01 | 1987-06-09 | University Of Utah Research Foundation | Methods and compositions for noninvasive administration of sedatives, analgesics, and anesthetics |
| US4692433A (en) | 1983-10-12 | 1987-09-08 | The Regents Of The University Of California | Method and composition for regulating serum calcium levels of mammals |
| US4713243A (en) | 1986-06-16 | 1987-12-15 | Johnson & Johnson Products, Inc. | Bioadhesive extruded film for intra-oral drug delivery and process |
| US4863737A (en) | 1985-05-01 | 1989-09-05 | University Of Utah | Compositions and methods of manufacture of compressed powder medicaments |
| US4900554A (en) | 1986-12-24 | 1990-02-13 | Teikoku Seiyaku Co., Ltd. | Adhesive device for application to body tissue |
| US4915948A (en) | 1987-08-31 | 1990-04-10 | Warner-Lambert Company | Tablets having improved bioadhesion to mucous membranes |
| US5047244A (en) | 1988-06-03 | 1991-09-10 | Watson Laboratories, Inc. | Mucoadhesive carrier for delivery of therapeutical agent |
| US5081158A (en) | 1988-05-02 | 1992-01-14 | Zila Pharmaceuticals, Inc. | Compositions and in situ methods for forming films on body tissue |
| US5081157A (en) | 1988-05-02 | 1992-01-14 | Zila Pharmaceuticals, Inc. | Compositions and in situ methods for forming films on body tissue |
| US5118666A (en) | 1986-05-05 | 1992-06-02 | The General Hospital Corporation | Insulinotropic hormone |
| US5120712A (en) | 1986-05-05 | 1992-06-09 | The General Hospital Corporation | Insulinotropic hormone |
| US5122127A (en) | 1985-05-01 | 1992-06-16 | University Of Utah | Apparatus and methods for use in administering medicaments by direct medicament contact to mucosal tissues |
| US5132114A (en) | 1985-05-01 | 1992-07-21 | University Of Utah Research Foundation | Compositions and methods of manufacture of compressed powder medicaments |
| US5137729A (en) | 1989-01-31 | 1992-08-11 | Nitto Denko Corporation | Drug preparation applicable to oral mucosa |
| US5187154A (en) | 1990-12-13 | 1993-02-16 | Board Of Regents, The University Of Texas System | Diagnosis and treatment of humans with diabetes or at risk to develop diabetes |
| US5192802A (en) | 1991-09-25 | 1993-03-09 | Mcneil-Ppc, Inc. | Bioadhesive pharmaceutical carrier |
| US5264372A (en) | 1991-03-15 | 1993-11-23 | Amylin Pharmaceuticals, Inc. | Receptor-based screening methods for amylin agonists and antagonists |
| US5298258A (en) | 1989-12-28 | 1994-03-29 | Nitto Denko Corporation | Acrylic oily gel bioadhesive material and acrylic oily gel preparation |
| US5346701A (en) | 1993-02-22 | 1994-09-13 | Theratech, Inc. | Transmucosal delivery of macromolecular drugs |
| US5376637A (en) | 1991-04-22 | 1994-12-27 | Sanwa Kagaku Kenkyusho Co., Ltd. | Pharmaceutical preparation containing vasoactive intestinal polypeptide or its analogue |
| US5424286A (en) | 1993-05-24 | 1995-06-13 | Eng; John | Exendin-3 and exendin-4 polypeptides, and pharmaceutical compositions comprising same |
| US5458879A (en) | 1994-03-03 | 1995-10-17 | The Procter & Gamble Company | Oral vehicle compositions |
| US5512549A (en) | 1994-10-18 | 1996-04-30 | Eli Lilly And Company | Glucagon-like insulinotropic peptide analogs, compositions, and methods of use |
| US5545618A (en) | 1990-01-24 | 1996-08-13 | Buckley; Douglas I. | GLP-1 analogs useful for diabetes treatment |
| US5552520A (en) | 1993-08-09 | 1996-09-03 | Biomeasure, Inc. | Therapeutic peptide derivatives |
| US5574008A (en) | 1994-08-30 | 1996-11-12 | Eli Lilly And Company | Biologically active fragments of glucagon-like insulinotropic peptide |
| US5578315A (en) | 1993-12-01 | 1996-11-26 | Rutgers, The State University Of New Jersey | Mucosal adhesive device for long-acting delivery of pharmaceutical combinations in oral cavity |
| US5614492A (en) | 1986-05-05 | 1997-03-25 | The General Hospital Corporation | Insulinotropic hormone GLP-1 (7-36) and uses thereof |
| US5624677A (en) | 1995-06-13 | 1997-04-29 | Pentech Pharmaceuticals, Inc. | Controlled release of drugs delivered by sublingual or buccal administration |
| WO1997015297A1 (en) | 1995-10-23 | 1997-05-01 | Theratech, Inc. | Compositions and methods for buccal delivery of pharmaceutical agents |
| US5631347A (en) | 1995-06-07 | 1997-05-20 | Eli Lilly And Company | Reducing gelation of a fatty acid-acylated protein |
| US5631224A (en) | 1992-03-19 | 1997-05-20 | Novo Nordisk A/S | Use of a peptide |
| US5646242A (en) | 1994-11-17 | 1997-07-08 | Eli Lilly And Company | Selective acylation of epsilon-amino groups |
| US5686511A (en) | 1996-06-28 | 1997-11-11 | The Valspar Corporation | Esterifying epoxy resin with carboxyl polymer and quenching |
| US5693609A (en) | 1994-11-17 | 1997-12-02 | Eli Lilly And Company | Acylated insulin analogs |
| US5700904A (en) | 1995-06-07 | 1997-12-23 | Eli Lilly And Company | Preparation of an acylated protein powder |
| US5750134A (en) | 1989-11-03 | 1998-05-12 | Riker Laboratories, Inc. | Bioadhesive composition and patch |
| US5750136A (en) | 1989-11-03 | 1998-05-12 | Riker Laboratories, Inc. | Bioadhesive composition and patch |
| US5750497A (en) | 1993-09-17 | 1998-05-12 | Novo Nordisk A/S | Acylated insulin |
| US5766620A (en) | 1995-10-23 | 1998-06-16 | Theratech, Inc. | Buccal delivery of glucagon-like insulinotropic peptides |
| US5780045A (en) | 1992-05-18 | 1998-07-14 | Minnesota Mining And Manufacturing Company | Transmucosal drug delivery device |
| US5800832A (en) | 1996-10-18 | 1998-09-01 | Virotex Corporation | Bioerodable film for delivery of pharmaceutical compounds to mucosal surfaces |
| US5827525A (en) | 1995-09-12 | 1998-10-27 | Bristol-Myers Squibb Company | Buccal delivery system for therapeutic agents |
| US5846937A (en) | 1997-03-03 | 1998-12-08 | 1149336 Ontario Inc. | Method of using exendin and GLP-1 to affect the central nervous system |
| US5855908A (en) | 1984-05-01 | 1999-01-05 | University Of Utah Research Foundation | Non-dissolvable drug-containing dosage-forms for use in the transmucosal delivery of a drug to a patient |
| US5861174A (en) | 1996-07-12 | 1999-01-19 | University Technology Corporation | Temperature sensitive gel for sustained delivery of protein drugs |
| US5869082A (en) | 1996-04-12 | 1999-02-09 | Flemington Pharmaceutical Corp. | Buccal, non-polar spray for nitroglycerin |
| US5888534A (en) | 1995-06-13 | 1999-03-30 | Pentech Pharmaceuticals, Inc. | Controlled release of drugs delivered by sublingual or buccal administration |
| WO1999016417A1 (en) | 1997-10-01 | 1999-04-08 | Flemington Pharmaceutical Corporation | Buccal, polar and non-polar spray or capsule |
| US5908637A (en) | 1994-06-15 | 1999-06-01 | Minnesota Mining And Manufacturing Co. | Transmucosal delivery system |
| US5955098A (en) | 1996-04-12 | 1999-09-21 | Flemington Pharmaceutical Corp. | Buccal non polar spray or capsule |
| US5955097A (en) | 1996-10-18 | 1999-09-21 | Virotex Corporation | Pharmaceutical preparation applicable to mucosal surfaces and body tissues |
| US6011007A (en) | 1993-09-17 | 2000-01-04 | Novo Nordisk A/S | Acylated insulin |
| US6051551A (en) | 1997-10-31 | 2000-04-18 | Eli Lilly And Company | Method for administering acylated insulin |
| US6103266A (en) | 1998-04-22 | 2000-08-15 | Tapolsky; Gilles H. | Pharmaceutical gel preparation applicable to mucosal surfaces and body tissues |
| US6103226A (en) | 1994-08-12 | 2000-08-15 | Arch Development Corporation | Genetically engineered cells that produce produce L. Dopa |
| US6110486A (en) | 1996-04-12 | 2000-08-29 | Flemington Pharmaceuticals Co. | Buccal polar spray or capsule |
| US6117446A (en) | 1999-01-26 | 2000-09-12 | Place; Virgil A. | Drug dosage unit for buccal administration of steroidal active agents |
| US6159931A (en) | 1998-09-29 | 2000-12-12 | The Ohio State University | Lipid-modified insulin incorporated liposomes for selectively delivering cytotoxic agents to hepatoma cells |
| US6162895A (en) | 1996-12-26 | 2000-12-19 | Poly-Med, Inc. | Peracylated insulin compositions and process for making the same |
| US6191102B1 (en) | 1996-11-05 | 2001-02-20 | Eli Lilly And Company | Use of GLP-1 analogs and derivatives administered peripherally in regulation of obesity |
| US6193997B1 (en) | 1998-09-27 | 2001-02-27 | Generex Pharmaceuticals Inc. | Proteinic drug delivery system using membrane mimetics |
| US6214375B1 (en) | 1996-07-16 | 2001-04-10 | Generex Pharmaceuticals, Inc. | Phospholipid formulations |
| US6221378B1 (en) | 1998-02-10 | 2001-04-24 | Generex Pharmaceuticals Incorporated | Mixed micellar delivery system and method of preparation |
| US6231882B1 (en) | 1998-02-10 | 2001-05-15 | Generex Pharmaceuticals Inc. | Mixed micellar delivery system and method of preparation |
| US6268335B1 (en) | 1997-10-24 | 2001-07-31 | Eli Lilly And Company | Insoluble insulin compositions |
| US6268343B1 (en) | 1996-08-30 | 2001-07-31 | Novo Nordisk A/S | Derivatives of GLP-1 analogs |
| US6271200B1 (en) | 1998-12-21 | 2001-08-07 | Generex Pharmaceuticals Inc. | Proteinic drug delivery system using aerosolized membrane-mimetic amphiphiles |
| US6284727B1 (en) | 1993-04-07 | 2001-09-04 | Scios, Inc. | Prolonged delivery of peptides |
| US6290987B1 (en) | 1998-09-27 | 2001-09-18 | Generex Pharmaceuticals, Inc. | Mixed liposome pharmaceutical formulation with amphiphiles and phospholipids |
| US6294153B1 (en) | 1998-12-21 | 2001-09-25 | Generex Pharmaceuticals, Inc. | Aerosol pharmaceutical formulation for pulmonary and nasal delivery |
| US6309633B1 (en) | 1999-06-19 | 2001-10-30 | Nobex Corporation | Amphiphilic drug-oligomer conjugates with hydroyzable lipophile components and methods for making and using the same |
| US6312665B1 (en) | 1998-12-21 | 2001-11-06 | Generex Pharmaceuticals Incorporated | Aerosol formulations for buccal and pulmonary application |
| US6315984B1 (en) | 1999-03-19 | 2001-11-13 | Generex Pharmaceuticals, Inc. | Pressurized container having an aerosolized pharmaceutical composition |
| US6350458B1 (en) | 1998-02-10 | 2002-02-26 | Generex Pharmaceuticals Incorporated | Mixed micellar drug deliver system and method of preparation |
| US6358924B1 (en) | 1997-12-05 | 2002-03-19 | Eli Lilly And Company | GLP-1 formulations |
| US6375975B1 (en) | 1998-12-21 | 2002-04-23 | Generex Pharmaceuticals Incorporated | Pharmaceutical compositions for buccal and pulmonary application |
| US6432383B1 (en) | 2000-03-30 | 2002-08-13 | Generex Pharmaceuticals Incorporated | Method for administering insulin |
| US6436367B1 (en) | 1998-12-21 | 2002-08-20 | Generex Pharmaceuticals Inc. | Aerosol formulations for buccal and pulmonary application |
| WO2002064115A1 (en) | 2001-02-13 | 2002-08-22 | Korea Institute Of Science And Technology | Formulation for delivery of insulin and preparation method thereof |
| US6444641B1 (en) | 1997-10-24 | 2002-09-03 | Eli Lilly Company | Fatty acid-acylated insulin analogs |
| US6448045B1 (en) | 2000-03-10 | 2002-09-10 | The Regents Of The University Of California | Inducing insulin gene expression in pancreas cells expressing recombinant PDX-1 |
| US6451286B1 (en) | 1998-12-21 | 2002-09-17 | Generex Pharmaceuticals Incorporated | Pharmaceutical compositions for buccal and pulmonary administration comprising an alkali metal alkyl sulfate and at least three micelle-forming compounds |
| US6458924B2 (en) | 1996-08-30 | 2002-10-01 | Novo Nordisk A/S | Derivatives of GLP-1 analogs |
| US6506724B1 (en) | 1999-06-01 | 2003-01-14 | Amylin Pharmaceuticals, Inc. | Use of exendins and agonists thereof for the treatment of gestational diabetes mellitus |
| US6528486B1 (en) | 1999-07-12 | 2003-03-04 | Zealand Pharma A/S | Peptide agonists of GLP-1 activity |
| US6531448B1 (en) | 1997-12-23 | 2003-03-11 | Eli Lilly And Company | Insoluble compositions for controlling blood glucose |
| WO2003024425A1 (en) | 2001-09-19 | 2003-03-27 | Elan Pharma International, Ltd. | Nanoparticulate insulin formulations |
| US6660715B2 (en) | 1998-11-19 | 2003-12-09 | Massachusetts Institute Of Technology | Nonaqueous solutions and suspensions of macromolecules for pulmonary delivery |
| US6703359B1 (en) | 1998-02-13 | 2004-03-09 | Amylin Pharmaceuticals, Inc. | Inotropic and diuretic effects of exendin and GLP-1 |
| US6706689B2 (en) | 2000-05-19 | 2004-03-16 | Amylin Pharmaceuticals, Inc. | Treatment of acute coronary syndrome with GLP-1 |
| US6713452B2 (en) | 2001-06-04 | 2004-03-30 | Nobex Corporation | Mixtures of calcitonin drug-oligomer conjugates comprising polyalkylene glycol, uses thereof, and methods of making same |
| US6723530B1 (en) | 1997-02-05 | 2004-04-20 | Amylin Pharmaceuticals, Inc. | Polynucleotides encoding proexendin, and methods and uses thereof |
| US6767887B1 (en) | 1996-06-05 | 2004-07-27 | Roche Diagnostics Gmbh | Exendin analogues, processes for their preparation and medicaments containing them |
| US6770625B2 (en) | 2001-09-07 | 2004-08-03 | Nobex Corporation | Pharmaceutical compositions of calcitonin drug-oligomer conjugates and methods of treating diseases therewith |
| US6828297B2 (en) | 2001-06-04 | 2004-12-07 | Nobex Corporation | Mixtures of insulin drug-oligomer conjugates comprising polyalkylene glycol, uses thereof, and methods of making same |
| WO2004105790A1 (en) | 2003-06-03 | 2004-12-09 | Novo Nordisk A/S | Stabilized pharmaceutical peptide compositions |
| US6835802B2 (en) | 2001-06-04 | 2004-12-28 | Nobex Corporation | Methods of synthesizing substantially monodispersed mixtures of polymers having polyethylene glycol moieties |
| US6849708B1 (en) | 1986-05-05 | 2005-02-01 | The General Hospital Corporation | Insulinotropic hormone and uses thereof |
| US6852690B1 (en) | 1995-08-22 | 2005-02-08 | Amylin Pharmaceuticals, Inc. | Method and composition for enhanced parenteral nutrition |
| US6858576B1 (en) | 1996-08-08 | 2005-02-22 | Amylin Pharmaceuticals, Inc. | Methods for regulating gastrointestinal motility |
| US6858580B2 (en) | 2001-06-04 | 2005-02-22 | Nobex Corporation | Mixtures of drug-oligomer conjugates comprising polyalkylene glycol, uses thereof, and methods of making same |
| US6867183B2 (en) | 2001-02-15 | 2005-03-15 | Nobex Corporation | Pharmaceutical compositions of insulin drug-oligomer conjugates and methods of treating diseases therewith |
| US6869930B1 (en) | 1993-09-17 | 2005-03-22 | Novo Nordisk A/S | Acylated insulin |
| US6872700B1 (en) | 1999-01-14 | 2005-03-29 | Amylin Pharmaceuticals, Inc. | Methods for glucagon suppression |
| US6899883B2 (en) | 1994-05-12 | 2005-05-31 | London Health Sciences Centre | Treatment of diabetes |
| US6902744B1 (en) | 1999-01-14 | 2005-06-07 | Amylin Pharmaceuticals, Inc. | Exendin agonist formulations and methods of administration thereof |
| US6911324B2 (en) | 2001-10-18 | 2005-06-28 | The Regents Of The University Of California | Induction of beta cell differentiation in human cells |
| US6913903B2 (en) | 2001-09-07 | 2005-07-05 | Nobex Corporation | Methods of synthesizing insulin polypeptide-oligomer conjugates, and proinsulin polypeptide-oligomer conjugates and methods of synthesizing same |
| US6924264B1 (en) | 1999-04-30 | 2005-08-02 | Amylin Pharmaceuticals, Inc. | Modified exendins and exendin agonists |
| US6956026B2 (en) | 1997-01-07 | 2005-10-18 | Amylin Pharmaceuticals, Inc. | Use of exendins for the reduction of food intake |
| US6969508B2 (en) | 1997-10-01 | 2005-11-29 | Novadel Pharma, Inc. | Buccal, polar and non-polar spray or capsule containing drugs for treating pain |
| US6977070B2 (en) | 1997-10-01 | 2005-12-20 | Novadel Pharma, Inc. | Buccal, polar and non-polar spray or capsule containing drugs for treating disorders of the central nervous system |
| US6982248B2 (en) | 1998-10-08 | 2006-01-03 | Amylin Pharmaceuticals, Inc. | Metabolic intervention with GLP-1 to improve the function of ischemic and reperfused tissue |
| WO2006025882A2 (en) | 2004-08-25 | 2006-03-09 | The Uab Research Foundation | Absorption enhancers for drug administration |
| US7022674B2 (en) | 1999-12-16 | 2006-04-04 | Eli Lilly And Company | Polypeptide compositions with improved stability |
| WO2006037811A2 (en) | 2004-10-07 | 2006-04-13 | Novo Nordisk A/S | Protracted exendin-4 compounds |
| US7030082B2 (en) | 2001-09-07 | 2006-04-18 | Nobex Corporation | Pharmaceutical compositions of drug-oligomer conjugates and methods of treating disease therewith |
| US7030084B2 (en) | 1999-06-19 | 2006-04-18 | Nobex Corporation | Drug-oligomer conjugates with polyethylene glycol components |
| US7056734B1 (en) | 1998-08-10 | 2006-06-06 | The United States Of America As Represented By The Department Of Health And Human Services, Nih | Differentiation of non-insulin producing cells into insulin producing cells by GLP-1 or exendin-4 and uses thereof |
| US7060675B2 (en) | 2001-02-15 | 2006-06-13 | Nobex Corporation | Methods of treating diabetes mellitus |
| US7070799B1 (en) | 1998-02-10 | 2006-07-04 | Generex Pharmaceuticals, Inc. | Method for administering insulin to the buccal region |
| US7078375B1 (en) | 1996-10-25 | 2006-07-18 | Peter Mose Larsen | Diabetes-mediating proteins and therapeutic uses thereof |
| US7084243B2 (en) | 2000-06-16 | 2006-08-01 | Eli Lilly And Company | Glucagon-like peptide-1 analogs |
| US7087215B2 (en) | 1998-12-21 | 2006-08-08 | Generex Pharmaceuticals Incorporated | Methods of administering and enhancing absorption of pharmaceutical agents |
| US20060178304A1 (en) | 2003-06-03 | 2006-08-10 | Novo Nordisk A/S | Stabilized pharmaceutical peptide compositions |
| US7115561B2 (en) | 2004-09-22 | 2006-10-03 | Patterson James A | Medicament composition and method of administration |
| US7119168B2 (en) | 2002-11-18 | 2006-10-10 | Bioprospecting Nb Inc. | Paralytic peptide for use in neuromuscular therapy |
| WO2006105615A1 (en) | 2005-04-08 | 2006-10-12 | Ozpharma Pty Ltd | Buccal delivery system |
| WO2006110365A1 (en) | 2005-04-07 | 2006-10-19 | Photonic Systems, Inc. | Optical modulator with coupled coplanar strip electrode and domain inversion |
| US7138486B2 (en) | 1986-05-05 | 2006-11-21 | The General Hospital Corporation | Insulinotropic hormone derivatives and uses thereof |
| WO2006127361A2 (en) | 2005-05-23 | 2006-11-30 | Sdg, Inc. | Lipid construct for delivery of insulin to a mammal |
| WO2006135930A2 (en) | 2005-06-13 | 2006-12-21 | Nastech Pharmaceutical Company Inc. | Transmucosal delivery of peptide derivatives |
| US7157555B1 (en) | 1997-08-08 | 2007-01-02 | Amylin Pharmaceuticals, Inc. | Exendin agonist compounds |
| US7164005B2 (en) | 2002-10-17 | 2007-01-16 | Alkermes, Inc. | Microencapsulation and sustained release of biologically active polypeptides |
| US7166571B2 (en) | 2001-09-07 | 2007-01-23 | Biocon Limited | Insulin polypeptide-oligomer conjugates, proinsulin polypeptide-oligomer conjugates and methods of synthesizing same |
| US7169410B1 (en) | 1998-05-19 | 2007-01-30 | Sdg, Inc. | Targeted liposomal drug delivery system |
| WO2007014391A2 (en) | 2005-07-27 | 2007-02-01 | Nastech Pharmaceutical Company Inc. | Tight junction modulating peptide components for enhancing mucosal delivery of therapeutic agents |
| US7196059B2 (en) | 2001-09-07 | 2007-03-27 | Biocon Limited | Pharmaceutical compositions of insulin drug-oligomer conjugates and methods of treating diseases therewith |
| US7220721B1 (en) | 1997-11-14 | 2007-05-22 | Amylin Pharmaceuticals, Inc. | Exendin agonist peptides |
| US7223725B1 (en) | 1997-11-14 | 2007-05-29 | Amylin Pharmaceuticals, Inc. | Exendin agonist compounds |
| US7226990B2 (en) | 1998-02-27 | 2007-06-05 | Novo Nordisk A/S | Extendin derivatives |
| WO2007065156A2 (en) | 2005-12-02 | 2007-06-07 | Nastech Pharmaceutical Company Inc. | Pharmaceutical formulation for increased epithelial permeability of glucose-regulating peptide |
| WO2007067964A2 (en) | 2005-12-08 | 2007-06-14 | Nastech Pharmaceutical Company Inc. | Mucosal delivery of stabilized formulations of exendin |
| WO2007083146A2 (en) | 2006-01-20 | 2007-07-26 | Cambridge Enterprise Limited | The treatment of cognitive and psychotic disorders |
| US7255102B2 (en) | 2002-02-01 | 2007-08-14 | Generex Pharmaceuticals Inc. | Metered dose spray device for use with macromolecular pharmaceutical agents such as insulin |
| US7259234B2 (en) | 2003-05-15 | 2007-08-21 | Trustees Of Tufts College | Stable analogs of peptide and polypeptide therapeutics |
| US7273921B2 (en) | 2002-09-25 | 2007-09-25 | Novo Nordisk A/S | Method for producing acylated peptides |
| WO2007121256A2 (en) | 2006-04-12 | 2007-10-25 | Biodel, Inc. | Rapid acting and long acting insulin combination formulations |
| US7307148B2 (en) | 2004-04-23 | 2007-12-11 | Conjuchem Biotechnologies Inc. | Method for purification of albumin conjugates |
| WO2007146448A1 (en) | 2006-06-07 | 2007-12-21 | Nastech Pharmaceutical Company Inc. | Pharmaceutical formulations of glp-1 derivatives |
| US7312192B2 (en) | 2001-09-07 | 2007-12-25 | Biocon Limited | Insulin polypeptide-oligomer conjugates, proinsulin polypeptide-oligomer conjugates and methods of synthesizing same |
| WO2008016729A1 (en) | 2006-08-04 | 2008-02-07 | Nastech Pharmaceutical Company Inc. | Compositions for intranasal delivery of human insulin and uses thereof |
| WO2008037484A2 (en) | 2006-09-27 | 2008-04-03 | Paolo Botti | Formulations comprising cyclic compounds |
| WO2008145728A1 (en) | 2007-06-01 | 2008-12-04 | Novo Nordisk A/S | Spontaneously dispersible preconcentrates including a peptide drug in a solid or semisolid carrier |
| WO2008145732A1 (en) | 2007-06-01 | 2008-12-04 | Novo Nordisk A/S | Stable non-aqueous pharmaceutical compositions |
| USRE40850E1 (en) | 1995-07-13 | 2009-07-14 | Societe De Conseils De Recherches Et D'applications Scientifiques, S.A.S. | Analogs of parathyroid hormone |
Family Cites Families (7)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| GB8317697D0 (en) * | 1983-06-29 | 1983-08-03 | Shell Int Research | Dissolution of peptides in non-aqueous and mixed non-aqueous/aqueous solvents |
| US6080783A (en) * | 1998-09-01 | 2000-06-27 | Gum Tech International, Inc. | Method and composition for delivering zinc to the nasal membrane |
| EP1338272A1 (en) * | 1998-12-21 | 2003-08-27 | Generex Pharmaceuticals Inc. | Aerosol formulations for buccal and pulmonary application comprising chenodeoxycholate or deoxycholate |
| EP1770099A1 (en) * | 2005-09-28 | 2007-04-04 | University of Geneva | Method of producing a modified (poly)peptide |
| EP1972332A1 (en) * | 2007-03-23 | 2008-09-24 | BioAlliance Pharma | Mucosal bioadhesive slow release carrier for delivering active principles |
| AU2008248228B2 (en) * | 2007-05-01 | 2012-10-18 | Cephalon, Inc. | Composition for transmucosal delivery of polypeptides |
| EP2332929A1 (en) | 2009-11-25 | 2011-06-15 | ArisGen SA | Orthoester derivatives of crown ethers as carriers for pharmaceutical and diagnostic compositions |
-
2010
- 2010-11-25 BR BR112012012945-7A patent/BR112012012945A2/en not_active Application Discontinuation
- 2010-11-25 AU AU2010323117A patent/AU2010323117B2/en not_active Ceased
- 2010-11-25 CN CN201080062361.9A patent/CN102770152B/en active Active
- 2010-11-25 JP JP2012540439A patent/JP5892940B2/en active Active
- 2010-11-25 US US13/512,001 patent/US9445992B2/en active Active
- 2010-11-25 WO PCT/EP2010/068257 patent/WO2011064316A2/en active Application Filing
- 2010-11-25 CA CA2782056A patent/CA2782056C/en active Active
- 2010-11-25 EP EP10781909A patent/EP2504019A2/en not_active Withdrawn
-
2012
- 2012-05-28 IL IL220022A patent/IL220022A/en active IP Right Grant
Patent Citations (191)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US4292299A (en) | 1978-11-06 | 1981-09-29 | Teijin Limited | Slow-releasing medical preparation to be administered by adhering to a wet mucous surface |
| US4250163A (en) | 1979-03-05 | 1981-02-10 | Teijin Limited | Method and preparation for administration to the mucosa of the oral or nasal cavity |
| US4226848A (en) | 1979-03-05 | 1980-10-07 | Teijin Limited | Method and preparation for administration to the mucosa of the oral or nasal cavity |
| US4511505A (en) | 1979-04-13 | 1985-04-16 | Shionogi & Co., Ltd. | Semi-synthesis of human insulin |
| US4517173A (en) | 1980-09-26 | 1985-05-14 | Nippon Soda Co. Ltd. | Mucous membrane-adhering film preparation and process for its preparation |
| US4552751A (en) | 1980-10-17 | 1985-11-12 | Ono Pharmaceutical Co., Ltd. | Long-lasting multi-layered film preparation |
| US4572832A (en) | 1982-10-07 | 1986-02-25 | Grelan Pharmaceutical Co., Ltd. | Soft buccal |
| US4692433A (en) | 1983-10-12 | 1987-09-08 | The Regents Of The University Of California | Method and composition for regulating serum calcium levels of mammals |
| US4615697A (en) | 1983-11-14 | 1986-10-07 | Bio-Mimetics, Inc. | Bioadhesive compositions and methods of treatment therewith |
| US5855908A (en) | 1984-05-01 | 1999-01-05 | University Of Utah Research Foundation | Non-dissolvable drug-containing dosage-forms for use in the transmucosal delivery of a drug to a patient |
| US5132114A (en) | 1985-05-01 | 1992-07-21 | University Of Utah Research Foundation | Compositions and methods of manufacture of compressed powder medicaments |
| US5122127A (en) | 1985-05-01 | 1992-06-16 | University Of Utah | Apparatus and methods for use in administering medicaments by direct medicament contact to mucosal tissues |
| US4671953A (en) | 1985-05-01 | 1987-06-09 | University Of Utah Research Foundation | Methods and compositions for noninvasive administration of sedatives, analgesics, and anesthetics |
| US4863737A (en) | 1985-05-01 | 1989-09-05 | University Of Utah | Compositions and methods of manufacture of compressed powder medicaments |
| US7138486B2 (en) | 1986-05-05 | 2006-11-21 | The General Hospital Corporation | Insulinotropic hormone derivatives and uses thereof |
| US6849708B1 (en) | 1986-05-05 | 2005-02-01 | The General Hospital Corporation | Insulinotropic hormone and uses thereof |
| US5118666A (en) | 1986-05-05 | 1992-06-02 | The General Hospital Corporation | Insulinotropic hormone |
| US5958909A (en) | 1986-05-05 | 1999-09-28 | The General Hospital Corporation | Insulinotropic hormones and uses thereof |
| US5614492A (en) | 1986-05-05 | 1997-03-25 | The General Hospital Corporation | Insulinotropic hormone GLP-1 (7-36) and uses thereof |
| US6162907A (en) | 1986-05-05 | 2000-12-19 | The General Hospital Corporation | DNA encoding insulinotropic hormone |
| US5120712A (en) | 1986-05-05 | 1992-06-09 | The General Hospital Corporation | Insulinotropic hormone |
| US4713243A (en) | 1986-06-16 | 1987-12-15 | Johnson & Johnson Products, Inc. | Bioadhesive extruded film for intra-oral drug delivery and process |
| US4900554A (en) | 1986-12-24 | 1990-02-13 | Teikoku Seiyaku Co., Ltd. | Adhesive device for application to body tissue |
| US4915948A (en) | 1987-08-31 | 1990-04-10 | Warner-Lambert Company | Tablets having improved bioadhesion to mucous membranes |
| US5081158A (en) | 1988-05-02 | 1992-01-14 | Zila Pharmaceuticals, Inc. | Compositions and in situ methods for forming films on body tissue |
| US5081157A (en) | 1988-05-02 | 1992-01-14 | Zila Pharmaceuticals, Inc. | Compositions and in situ methods for forming films on body tissue |
| US5047244A (en) | 1988-06-03 | 1991-09-10 | Watson Laboratories, Inc. | Mucoadhesive carrier for delivery of therapeutical agent |
| US5137729A (en) | 1989-01-31 | 1992-08-11 | Nitto Denko Corporation | Drug preparation applicable to oral mucosa |
| US5750134A (en) | 1989-11-03 | 1998-05-12 | Riker Laboratories, Inc. | Bioadhesive composition and patch |
| US5750136A (en) | 1989-11-03 | 1998-05-12 | Riker Laboratories, Inc. | Bioadhesive composition and patch |
| US5298258A (en) | 1989-12-28 | 1994-03-29 | Nitto Denko Corporation | Acrylic oily gel bioadhesive material and acrylic oily gel preparation |
| US5545618A (en) | 1990-01-24 | 1996-08-13 | Buckley; Douglas I. | GLP-1 analogs useful for diabetes treatment |
| US5187154A (en) | 1990-12-13 | 1993-02-16 | Board Of Regents, The University Of Texas System | Diagnosis and treatment of humans with diabetes or at risk to develop diabetes |
| US5264372A (en) | 1991-03-15 | 1993-11-23 | Amylin Pharmaceuticals, Inc. | Receptor-based screening methods for amylin agonists and antagonists |
| US5376637A (en) | 1991-04-22 | 1994-12-27 | Sanwa Kagaku Kenkyusho Co., Ltd. | Pharmaceutical preparation containing vasoactive intestinal polypeptide or its analogue |
| US5192802A (en) | 1991-09-25 | 1993-03-09 | Mcneil-Ppc, Inc. | Bioadhesive pharmaceutical carrier |
| US5462749A (en) | 1991-09-25 | 1995-10-31 | Mcnell-Ppc, Inc. | Bioadhesive pharmaceutical carrier |
| US5314915A (en) | 1991-09-25 | 1994-05-24 | Mcneil-Ppc, Inc. | Bioadhesive pharmaceutical carrier |
| US5631224A (en) | 1992-03-19 | 1997-05-20 | Novo Nordisk A/S | Use of a peptide |
| US5780045A (en) | 1992-05-18 | 1998-07-14 | Minnesota Mining And Manufacturing Company | Transmucosal drug delivery device |
| US5346701A (en) | 1993-02-22 | 1994-09-13 | Theratech, Inc. | Transmucosal delivery of macromolecular drugs |
| US6828303B2 (en) | 1993-04-07 | 2004-12-07 | Scios, Inc. | Prolonged delivery of peptides |
| US6284727B1 (en) | 1993-04-07 | 2001-09-04 | Scios, Inc. | Prolonged delivery of peptides |
| US5424286A (en) | 1993-05-24 | 1995-06-13 | Eng; John | Exendin-3 and exendin-4 polypeptides, and pharmaceutical compositions comprising same |
| US5552520A (en) | 1993-08-09 | 1996-09-03 | Biomeasure, Inc. | Therapeutic peptide derivatives |
| US6869930B1 (en) | 1993-09-17 | 2005-03-22 | Novo Nordisk A/S | Acylated insulin |
| US6011007A (en) | 1993-09-17 | 2000-01-04 | Novo Nordisk A/S | Acylated insulin |
| US5750497A (en) | 1993-09-17 | 1998-05-12 | Novo Nordisk A/S | Acylated insulin |
| US5578315A (en) | 1993-12-01 | 1996-11-26 | Rutgers, The State University Of New Jersey | Mucosal adhesive device for long-acting delivery of pharmaceutical combinations in oral cavity |
| US5458879A (en) | 1994-03-03 | 1995-10-17 | The Procter & Gamble Company | Oral vehicle compositions |
| US6989148B2 (en) | 1994-05-12 | 2006-01-24 | John Dupre | Treatment of diabetes |
| US6899883B2 (en) | 1994-05-12 | 2005-05-31 | London Health Sciences Centre | Treatment of diabetes |
| US5908637A (en) | 1994-06-15 | 1999-06-01 | Minnesota Mining And Manufacturing Co. | Transmucosal delivery system |
| US6103226A (en) | 1994-08-12 | 2000-08-15 | Arch Development Corporation | Genetically engineered cells that produce produce L. Dopa |
| US5574008A (en) | 1994-08-30 | 1996-11-12 | Eli Lilly And Company | Biologically active fragments of glucagon-like insulinotropic peptide |
| US5512549A (en) | 1994-10-18 | 1996-04-30 | Eli Lilly And Company | Glucagon-like insulinotropic peptide analogs, compositions, and methods of use |
| US5693609A (en) | 1994-11-17 | 1997-12-02 | Eli Lilly And Company | Acylated insulin analogs |
| US5646242A (en) | 1994-11-17 | 1997-07-08 | Eli Lilly And Company | Selective acylation of epsilon-amino groups |
| US5922675A (en) | 1994-11-17 | 1999-07-13 | Eli Lilly And Company | Acylated Insulin Analogs |
| US5631347A (en) | 1995-06-07 | 1997-05-20 | Eli Lilly And Company | Reducing gelation of a fatty acid-acylated protein |
| US5700904A (en) | 1995-06-07 | 1997-12-23 | Eli Lilly And Company | Preparation of an acylated protein powder |
| US5888534A (en) | 1995-06-13 | 1999-03-30 | Pentech Pharmaceuticals, Inc. | Controlled release of drugs delivered by sublingual or buccal administration |
| US5624677A (en) | 1995-06-13 | 1997-04-29 | Pentech Pharmaceuticals, Inc. | Controlled release of drugs delivered by sublingual or buccal administration |
| USRE40850E1 (en) | 1995-07-13 | 2009-07-14 | Societe De Conseils De Recherches Et D'applications Scientifiques, S.A.S. | Analogs of parathyroid hormone |
| US6852690B1 (en) | 1995-08-22 | 2005-02-08 | Amylin Pharmaceuticals, Inc. | Method and composition for enhanced parenteral nutrition |
| US5827525A (en) | 1995-09-12 | 1998-10-27 | Bristol-Myers Squibb Company | Buccal delivery system for therapeutic agents |
| WO1997015297A1 (en) | 1995-10-23 | 1997-05-01 | Theratech, Inc. | Compositions and methods for buccal delivery of pharmaceutical agents |
| US5766620A (en) | 1995-10-23 | 1998-06-16 | Theratech, Inc. | Buccal delivery of glucagon-like insulinotropic peptides |
| US5863555A (en) | 1995-10-23 | 1999-01-26 | Theratech, Inc. | Buccal delivery of glucagon-like insulinotropic peptides |
| US5849322A (en) | 1995-10-23 | 1998-12-15 | Theratech, Inc. | Compositions and methods for buccal delivery of pharmaceutical agents |
| US6110486A (en) | 1996-04-12 | 2000-08-29 | Flemington Pharmaceuticals Co. | Buccal polar spray or capsule |
| US5869082A (en) | 1996-04-12 | 1999-02-09 | Flemington Pharmaceutical Corp. | Buccal, non-polar spray for nitroglycerin |
| US5955098A (en) | 1996-04-12 | 1999-09-21 | Flemington Pharmaceutical Corp. | Buccal non polar spray or capsule |
| US6767887B1 (en) | 1996-06-05 | 2004-07-27 | Roche Diagnostics Gmbh | Exendin analogues, processes for their preparation and medicaments containing them |
| US5686511A (en) | 1996-06-28 | 1997-11-11 | The Valspar Corporation | Esterifying epoxy resin with carboxyl polymer and quenching |
| US5861174A (en) | 1996-07-12 | 1999-01-19 | University Technology Corporation | Temperature sensitive gel for sustained delivery of protein drugs |
| US6214375B1 (en) | 1996-07-16 | 2001-04-10 | Generex Pharmaceuticals, Inc. | Phospholipid formulations |
| US6858576B1 (en) | 1996-08-08 | 2005-02-22 | Amylin Pharmaceuticals, Inc. | Methods for regulating gastrointestinal motility |
| US7297761B2 (en) | 1996-08-08 | 2007-11-20 | Amylin Pharmaceuticals, Inc. | Pharmaceutical compositions containing exendins |
| US6268343B1 (en) | 1996-08-30 | 2001-07-31 | Novo Nordisk A/S | Derivatives of GLP-1 analogs |
| US6458924B2 (en) | 1996-08-30 | 2002-10-01 | Novo Nordisk A/S | Derivatives of GLP-1 analogs |
| US5800832A (en) | 1996-10-18 | 1998-09-01 | Virotex Corporation | Bioerodable film for delivery of pharmaceutical compounds to mucosal surfaces |
| US6159498A (en) | 1996-10-18 | 2000-12-12 | Virotex Corporation | Bioerodable film for delivery of pharmaceutical compounds of mucosal surfaces |
| US5955097A (en) | 1996-10-18 | 1999-09-21 | Virotex Corporation | Pharmaceutical preparation applicable to mucosal surfaces and body tissues |
| US7078375B1 (en) | 1996-10-25 | 2006-07-18 | Peter Mose Larsen | Diabetes-mediating proteins and therapeutic uses thereof |
| US7211557B2 (en) | 1996-11-05 | 2007-05-01 | Eli Lilly And Company | Use of GLP-1 analogs and derivatives administered peripherally in regulation of obesity |
| US6191102B1 (en) | 1996-11-05 | 2001-02-20 | Eli Lilly And Company | Use of GLP-1 analogs and derivatives administered peripherally in regulation of obesity |
| US6162895A (en) | 1996-12-26 | 2000-12-19 | Poly-Med, Inc. | Peracylated insulin compositions and process for making the same |
| US6989366B2 (en) | 1997-01-07 | 2006-01-24 | Amylin Pharmaceuticals, Inc. | Exendins, exendin agonists, and methods for their use |
| US7138375B2 (en) | 1997-01-07 | 2006-11-21 | Amylin Pharmaceuticals, Inc. | Use of exendins and agonists thereof for lowering plasma lipid |
| US7115569B2 (en) | 1997-01-07 | 2006-10-03 | Amylin Pharmaceuticals, Inc. | Exendins, exendin agonists, and methods for their use |
| US6956026B2 (en) | 1997-01-07 | 2005-10-18 | Amylin Pharmaceuticals, Inc. | Use of exendins for the reduction of food intake |
| US6723530B1 (en) | 1997-02-05 | 2004-04-20 | Amylin Pharmaceuticals, Inc. | Polynucleotides encoding proexendin, and methods and uses thereof |
| US5846937A (en) | 1997-03-03 | 1998-12-08 | 1149336 Ontario Inc. | Method of using exendin and GLP-1 to affect the central nervous system |
| US7157555B1 (en) | 1997-08-08 | 2007-01-02 | Amylin Pharmaceuticals, Inc. | Exendin agonist compounds |
| WO1999016417A1 (en) | 1997-10-01 | 1999-04-08 | Flemington Pharmaceutical Corporation | Buccal, polar and non-polar spray or capsule |
| US6676931B2 (en) | 1997-10-01 | 2004-01-13 | Novadel Pharma Inc. | Buccal, polar and non-polar spray or capsule |
| US6977070B2 (en) | 1997-10-01 | 2005-12-20 | Novadel Pharma, Inc. | Buccal, polar and non-polar spray or capsule containing drugs for treating disorders of the central nervous system |
| US6998110B2 (en) | 1997-10-01 | 2006-02-14 | Novadel Pharma, Inc. | Buccal, polar and non-polar spray or capsule |
| US6969508B2 (en) | 1997-10-01 | 2005-11-29 | Novadel Pharma, Inc. | Buccal, polar and non-polar spray or capsule containing drugs for treating pain |
| US6444641B1 (en) | 1997-10-24 | 2002-09-03 | Eli Lilly Company | Fatty acid-acylated insulin analogs |
| US6268335B1 (en) | 1997-10-24 | 2001-07-31 | Eli Lilly And Company | Insoluble insulin compositions |
| US6465426B2 (en) | 1997-10-24 | 2002-10-15 | Eli Lilly And Company | Insoluble insulin compositions |
| US6051551A (en) | 1997-10-31 | 2000-04-18 | Eli Lilly And Company | Method for administering acylated insulin |
| US7220721B1 (en) | 1997-11-14 | 2007-05-22 | Amylin Pharmaceuticals, Inc. | Exendin agonist peptides |
| US7223725B1 (en) | 1997-11-14 | 2007-05-29 | Amylin Pharmaceuticals, Inc. | Exendin agonist compounds |
| US6358924B1 (en) | 1997-12-05 | 2002-03-19 | Eli Lilly And Company | GLP-1 formulations |
| US6531448B1 (en) | 1997-12-23 | 2003-03-11 | Eli Lilly And Company | Insoluble compositions for controlling blood glucose |
| US6231882B1 (en) | 1998-02-10 | 2001-05-15 | Generex Pharmaceuticals Inc. | Mixed micellar delivery system and method of preparation |
| US7070799B1 (en) | 1998-02-10 | 2006-07-04 | Generex Pharmaceuticals, Inc. | Method for administering insulin to the buccal region |
| US6350458B1 (en) | 1998-02-10 | 2002-02-26 | Generex Pharmaceuticals Incorporated | Mixed micellar drug deliver system and method of preparation |
| US6221378B1 (en) | 1998-02-10 | 2001-04-24 | Generex Pharmaceuticals Incorporated | Mixed micellar delivery system and method of preparation |
| US6703359B1 (en) | 1998-02-13 | 2004-03-09 | Amylin Pharmaceuticals, Inc. | Inotropic and diuretic effects of exendin and GLP-1 |
| US7226990B2 (en) | 1998-02-27 | 2007-06-05 | Novo Nordisk A/S | Extendin derivatives |
| US6103266A (en) | 1998-04-22 | 2000-08-15 | Tapolsky; Gilles H. | Pharmaceutical gel preparation applicable to mucosal surfaces and body tissues |
| US7169410B1 (en) | 1998-05-19 | 2007-01-30 | Sdg, Inc. | Targeted liposomal drug delivery system |
| US7056734B1 (en) | 1998-08-10 | 2006-06-06 | The United States Of America As Represented By The Department Of Health And Human Services, Nih | Differentiation of non-insulin producing cells into insulin producing cells by GLP-1 or exendin-4 and uses thereof |
| US6290987B1 (en) | 1998-09-27 | 2001-09-18 | Generex Pharmaceuticals, Inc. | Mixed liposome pharmaceutical formulation with amphiphiles and phospholipids |
| US6193997B1 (en) | 1998-09-27 | 2001-02-27 | Generex Pharmaceuticals Inc. | Proteinic drug delivery system using membrane mimetics |
| US6159931A (en) | 1998-09-29 | 2000-12-12 | The Ohio State University | Lipid-modified insulin incorporated liposomes for selectively delivering cytotoxic agents to hepatoma cells |
| US6982248B2 (en) | 1998-10-08 | 2006-01-03 | Amylin Pharmaceuticals, Inc. | Metabolic intervention with GLP-1 to improve the function of ischemic and reperfused tissue |
| US6660715B2 (en) | 1998-11-19 | 2003-12-09 | Massachusetts Institute Of Technology | Nonaqueous solutions and suspensions of macromolecules for pulmonary delivery |
| US6436367B1 (en) | 1998-12-21 | 2002-08-20 | Generex Pharmaceuticals Inc. | Aerosol formulations for buccal and pulmonary application |
| US6375975B1 (en) | 1998-12-21 | 2002-04-23 | Generex Pharmaceuticals Incorporated | Pharmaceutical compositions for buccal and pulmonary application |
| US6294153B1 (en) | 1998-12-21 | 2001-09-25 | Generex Pharmaceuticals, Inc. | Aerosol pharmaceutical formulation for pulmonary and nasal delivery |
| US6451286B1 (en) | 1998-12-21 | 2002-09-17 | Generex Pharmaceuticals Incorporated | Pharmaceutical compositions for buccal and pulmonary administration comprising an alkali metal alkyl sulfate and at least three micelle-forming compounds |
| US6312665B1 (en) | 1998-12-21 | 2001-11-06 | Generex Pharmaceuticals Incorporated | Aerosol formulations for buccal and pulmonary application |
| US7087215B2 (en) | 1998-12-21 | 2006-08-08 | Generex Pharmaceuticals Incorporated | Methods of administering and enhancing absorption of pharmaceutical agents |
| US6271200B1 (en) | 1998-12-21 | 2001-08-07 | Generex Pharmaceuticals Inc. | Proteinic drug delivery system using aerosolized membrane-mimetic amphiphiles |
| US6872700B1 (en) | 1999-01-14 | 2005-03-29 | Amylin Pharmaceuticals, Inc. | Methods for glucagon suppression |
| US6902744B1 (en) | 1999-01-14 | 2005-06-07 | Amylin Pharmaceuticals, Inc. | Exendin agonist formulations and methods of administration thereof |
| US7153825B2 (en) | 1999-01-14 | 2006-12-26 | Amylin Pharmaceuticals, Inc. | Methods for glucagon suppression using modified exendins |
| US6117446A (en) | 1999-01-26 | 2000-09-12 | Place; Virgil A. | Drug dosage unit for buccal administration of steroidal active agents |
| US6315984B1 (en) | 1999-03-19 | 2001-11-13 | Generex Pharmaceuticals, Inc. | Pressurized container having an aerosolized pharmaceutical composition |
| US6350432B1 (en) | 1999-03-19 | 2002-02-26 | Generex Pharmaceuticals Incorporated | Pressurized container having an aerosolized pharmaceutical composition |
| US6924264B1 (en) | 1999-04-30 | 2005-08-02 | Amylin Pharmaceuticals, Inc. | Modified exendins and exendin agonists |
| US6506724B1 (en) | 1999-06-01 | 2003-01-14 | Amylin Pharmaceuticals, Inc. | Use of exendins and agonists thereof for the treatment of gestational diabetes mellitus |
| US7030084B2 (en) | 1999-06-19 | 2006-04-18 | Nobex Corporation | Drug-oligomer conjugates with polyethylene glycol components |
| US7169889B1 (en) | 1999-06-19 | 2007-01-30 | Biocon Limited | Insulin prodrugs hydrolyzable in vivo to yield peglylated insulin |
| US6309633B1 (en) | 1999-06-19 | 2001-10-30 | Nobex Corporation | Amphiphilic drug-oligomer conjugates with hydroyzable lipophile components and methods for making and using the same |
| US6528486B1 (en) | 1999-07-12 | 2003-03-04 | Zealand Pharma A/S | Peptide agonists of GLP-1 activity |
| US7022674B2 (en) | 1999-12-16 | 2006-04-04 | Eli Lilly And Company | Polypeptide compositions with improved stability |
| US6884585B2 (en) | 2000-03-10 | 2005-04-26 | The Regents Of The University Of California | Induction of beta cell differentiation in human cells by stimulation of the GLP-1 receptor |
| US6448045B1 (en) | 2000-03-10 | 2002-09-10 | The Regents Of The University Of California | Inducing insulin gene expression in pancreas cells expressing recombinant PDX-1 |
| US6432383B1 (en) | 2000-03-30 | 2002-08-13 | Generex Pharmaceuticals Incorporated | Method for administering insulin |
| US7056887B2 (en) | 2000-05-19 | 2006-06-06 | Amylin Pharmaceuticals, Inc. | Treatment of acute coronary syndrome with GLP-1 |
| US6706689B2 (en) | 2000-05-19 | 2004-03-16 | Amylin Pharmaceuticals, Inc. | Treatment of acute coronary syndrome with GLP-1 |
| US7084243B2 (en) | 2000-06-16 | 2006-08-01 | Eli Lilly And Company | Glucagon-like peptide-1 analogs |
| WO2002064115A1 (en) | 2001-02-13 | 2002-08-22 | Korea Institute Of Science And Technology | Formulation for delivery of insulin and preparation method thereof |
| US6867183B2 (en) | 2001-02-15 | 2005-03-15 | Nobex Corporation | Pharmaceutical compositions of insulin drug-oligomer conjugates and methods of treating diseases therewith |
| US7060675B2 (en) | 2001-02-15 | 2006-06-13 | Nobex Corporation | Methods of treating diabetes mellitus |
| US6713452B2 (en) | 2001-06-04 | 2004-03-30 | Nobex Corporation | Mixtures of calcitonin drug-oligomer conjugates comprising polyalkylene glycol, uses thereof, and methods of making same |
| US6835802B2 (en) | 2001-06-04 | 2004-12-28 | Nobex Corporation | Methods of synthesizing substantially monodispersed mixtures of polymers having polyethylene glycol moieties |
| US7084114B2 (en) | 2001-06-04 | 2006-08-01 | Nobex Corporation | Mixtures of insulin drug-oligomer comprising polyalkylene glycol |
| US6828297B2 (en) | 2001-06-04 | 2004-12-07 | Nobex Corporation | Mixtures of insulin drug-oligomer conjugates comprising polyalkylene glycol, uses thereof, and methods of making same |
| US6858580B2 (en) | 2001-06-04 | 2005-02-22 | Nobex Corporation | Mixtures of drug-oligomer conjugates comprising polyalkylene glycol, uses thereof, and methods of making same |
| US7084121B2 (en) | 2001-06-04 | 2006-08-01 | Nobex Corporation | Mixtures of calcitonin drug-oligomer conjugates comprising polyalkylene glycol, uses thereof, and methods of making same |
| US7030082B2 (en) | 2001-09-07 | 2006-04-18 | Nobex Corporation | Pharmaceutical compositions of drug-oligomer conjugates and methods of treating disease therewith |
| US6913903B2 (en) | 2001-09-07 | 2005-07-05 | Nobex Corporation | Methods of synthesizing insulin polypeptide-oligomer conjugates, and proinsulin polypeptide-oligomer conjugates and methods of synthesizing same |
| US7312192B2 (en) | 2001-09-07 | 2007-12-25 | Biocon Limited | Insulin polypeptide-oligomer conjugates, proinsulin polypeptide-oligomer conjugates and methods of synthesizing same |
| US7196059B2 (en) | 2001-09-07 | 2007-03-27 | Biocon Limited | Pharmaceutical compositions of insulin drug-oligomer conjugates and methods of treating diseases therewith |
| US7166571B2 (en) | 2001-09-07 | 2007-01-23 | Biocon Limited | Insulin polypeptide-oligomer conjugates, proinsulin polypeptide-oligomer conjugates and methods of synthesizing same |
| US6770625B2 (en) | 2001-09-07 | 2004-08-03 | Nobex Corporation | Pharmaceutical compositions of calcitonin drug-oligomer conjugates and methods of treating diseases therewith |
| WO2003024425A1 (en) | 2001-09-19 | 2003-03-27 | Elan Pharma International, Ltd. | Nanoparticulate insulin formulations |
| US6911324B2 (en) | 2001-10-18 | 2005-06-28 | The Regents Of The University Of California | Induction of beta cell differentiation in human cells |
| US7255102B2 (en) | 2002-02-01 | 2007-08-14 | Generex Pharmaceuticals Inc. | Metered dose spray device for use with macromolecular pharmaceutical agents such as insulin |
| US7273921B2 (en) | 2002-09-25 | 2007-09-25 | Novo Nordisk A/S | Method for producing acylated peptides |
| US7164005B2 (en) | 2002-10-17 | 2007-01-16 | Alkermes, Inc. | Microencapsulation and sustained release of biologically active polypeptides |
| US7119168B2 (en) | 2002-11-18 | 2006-10-10 | Bioprospecting Nb Inc. | Paralytic peptide for use in neuromuscular therapy |
| US7273850B2 (en) | 2002-11-18 | 2007-09-25 | Bioprospecting Nb Inc. | Paralytic peptide for use in neuromuscular therapy |
| US7259234B2 (en) | 2003-05-15 | 2007-08-21 | Trustees Of Tufts College | Stable analogs of peptide and polypeptide therapeutics |
| WO2004105790A1 (en) | 2003-06-03 | 2004-12-09 | Novo Nordisk A/S | Stabilized pharmaceutical peptide compositions |
| US20060178304A1 (en) | 2003-06-03 | 2006-08-10 | Novo Nordisk A/S | Stabilized pharmaceutical peptide compositions |
| US7307148B2 (en) | 2004-04-23 | 2007-12-11 | Conjuchem Biotechnologies Inc. | Method for purification of albumin conjugates |
| WO2006025882A2 (en) | 2004-08-25 | 2006-03-09 | The Uab Research Foundation | Absorption enhancers for drug administration |
| US7115561B2 (en) | 2004-09-22 | 2006-10-03 | Patterson James A | Medicament composition and method of administration |
| WO2006037811A2 (en) | 2004-10-07 | 2006-04-13 | Novo Nordisk A/S | Protracted exendin-4 compounds |
| WO2006110365A1 (en) | 2005-04-07 | 2006-10-19 | Photonic Systems, Inc. | Optical modulator with coupled coplanar strip electrode and domain inversion |
| WO2006105615A1 (en) | 2005-04-08 | 2006-10-12 | Ozpharma Pty Ltd | Buccal delivery system |
| WO2006127361A2 (en) | 2005-05-23 | 2006-11-30 | Sdg, Inc. | Lipid construct for delivery of insulin to a mammal |
| WO2006135930A2 (en) | 2005-06-13 | 2006-12-21 | Nastech Pharmaceutical Company Inc. | Transmucosal delivery of peptide derivatives |
| WO2007014391A2 (en) | 2005-07-27 | 2007-02-01 | Nastech Pharmaceutical Company Inc. | Tight junction modulating peptide components for enhancing mucosal delivery of therapeutic agents |
| WO2007065156A2 (en) | 2005-12-02 | 2007-06-07 | Nastech Pharmaceutical Company Inc. | Pharmaceutical formulation for increased epithelial permeability of glucose-regulating peptide |
| WO2007067964A2 (en) | 2005-12-08 | 2007-06-14 | Nastech Pharmaceutical Company Inc. | Mucosal delivery of stabilized formulations of exendin |
| WO2007083146A2 (en) | 2006-01-20 | 2007-07-26 | Cambridge Enterprise Limited | The treatment of cognitive and psychotic disorders |
| WO2007121256A2 (en) | 2006-04-12 | 2007-10-25 | Biodel, Inc. | Rapid acting and long acting insulin combination formulations |
| WO2007146448A1 (en) | 2006-06-07 | 2007-12-21 | Nastech Pharmaceutical Company Inc. | Pharmaceutical formulations of glp-1 derivatives |
| WO2008016729A1 (en) | 2006-08-04 | 2008-02-07 | Nastech Pharmaceutical Company Inc. | Compositions for intranasal delivery of human insulin and uses thereof |
| WO2008037484A2 (en) | 2006-09-27 | 2008-04-03 | Paolo Botti | Formulations comprising cyclic compounds |
| WO2008145728A1 (en) | 2007-06-01 | 2008-12-04 | Novo Nordisk A/S | Spontaneously dispersible preconcentrates including a peptide drug in a solid or semisolid carrier |
| WO2008145732A1 (en) | 2007-06-01 | 2008-12-04 | Novo Nordisk A/S | Stable non-aqueous pharmaceutical compositions |
Non-Patent Citations (53)
| Title |
|---|
| "Remington: The Science and Practice of Pharmacy", 1995 |
| AMIN ET AL., DRUG DELIVERY TECHNOLOGY, vol. 7, no. 3, 2007, pages 48,50 - 55 |
| AMIN ET AL., DRUG DELIVERY TECHNOLOGY, vol. 7, no. 3, 7 December 2006 (2006-12-07), pages 48,50 - 55 |
| AUNGST ET AL., INTL. J. PHARMACEUTICS, vol. 53, no. 3, 1989, pages 227 - 35 |
| AUNGST ET AL., PHARMACEUTICAL RESEARCH, vol. 5, no. 5, 1988, pages 305 - 308 |
| BERSTEIN, G., DRUG DEVELOPMENT RES., vol. 67, no. 7, 2006, pages 597 - 599 |
| BOSCH ET AL., ANAL. CHEM., vol. 68, no. 20, 1996, pages 3651 - 3657 |
| BROADHEAD ET AL., DRUG DEVEL. IND. PHARM., vol. 18, 1992, pages 1169 - 1206 |
| CARPENTER; CROWE, CRYOBIOLOGY, vol. 25, 1988, pages 459 - 470 |
| DRUKER, D.J., CURR PHARM DESIGN, vol. 7, no. 14, 2001, pages 1399 - 1412 |
| E. WEBER; F. VOGTLE, INORG. CHIM. ACTA, vol. 45, 1980, pages L65 - L67 |
| GAGLIARDI ET AL., J. CHROMATOGRAPHY A, vol. 1077, no. 2, 2005, pages 159 - 169 |
| HOSNY ET AL., BOLLETTINO CHIMICO FARMACEUTICO, vol. 141, no. 3, 2002, pages 210 - 217 |
| HOSNY, BOLL. CHIM. FARM., vol. 141, 2002, pages 210 - 217 |
| ISHIDA ET AL., CHEM. PHARM. BULL., vol. 29, 1981, pages 810 - 816 |
| J. A. DEAN: "Analytical Chemistry Handbook", 1995, MCGRAW-HILL |
| KHAFAGY ET AL., ADVANCED DRUG DELIVERY REVIEWS, vol. 59, no. 15, 2007, pages 1521 - 1546 |
| LASSMANN-VAGUE ET AL., DIABETES & METABOLISM, vol. 32, no. 5, 2006, pages 513 - 522 |
| LIFSON ET AL., J. AM. CHEM. SOC., vol. 105, 1983, pages 3866 - 3875 |
| LIFSON ET AL., J. AM. CHEM. SOC., vol. 23, 1984, pages 2577 - 2590 |
| M. HIRAOKA: "Science Publishers", 1982, ELSEVIER, article "Crown Compounds: their Characteristics and Applications" |
| MASTERS: "Spray-Drying Handbook", 1991, LONGMAN SCIENTIFIC AND TECHNICA, pages: 491 - 676 |
| MCGEARY ET AL., TETRAHEDRON, vol. 56, 2000, pages 8703 - 8713 |
| MORISHITA ET AL., INT. J. PHARM., vol. 212, 2001, pages 289 - 293 |
| MORISHITA ET AL., INTL. J. PHARMACEUTICS, vol. 212, no. 2, 2001, pages 289 - 293 |
| MUMENTHALER ET AL., PHARM. RES., vol. 11, 1994, pages 12 - 20 |
| OWENS, DR., NATURE REVIEWS DRUG DISCOVERY, vol. 1, no. 7, 2002, pages 529 - 540 |
| PATEL ET AL., DRUG DELIVERY TECHNOLOGY, vol. 6, no. 3, 2006, pages 48 - 60 |
| PILLION ET AL., J. PHARM. SCI., vol. 84, no. 11, 1995, pages 1276 - 1279 |
| PORTERO ET AL., CARBOHYDRATE POLYMERS, vol. 68, no. 4, 2007, pages 617 - 625 |
| POZZILLI ET AL., METABOLISM, CLINICAL AND EXPERIMENTAL, vol. 54, no. 7, 2005, pages 930 - 934 |
| RONDININI, S., ANALYTICAL BIOANALYTICAL CHEM, vol. 374, no. 5, 2004, pages 813 - 816 |
| ROSER, BIOPHARM., vol. 4, 1991, pages 47 - 53 |
| ROSSI ET AL., AMERICAN J. DRUG DELIVERY, vol. 3, no. 4, 2005, pages 215 - 225 |
| SADRZADEH ET AL., J. PHARM SCI, vol. 96, no. 8, 2007, pages 1925 - 1954 |
| SANZ-NEBOT ET AL., J. CHROMATOGRAPHY A, vol. 942, no. 1-2, 2002, pages 145 |
| SENEL ET AL., CURR. PHARM. BIOTECHNOL., vol. 2, 2001, pages 175 - 186 |
| STAROKADOMSKYY ET AL., INT. J. PHARM., vol. 308, 2006, pages 149 - 154 |
| STAROKADOMSKYY ET AL., INTL. J. PHARMACEUTICS, vol. 308, no. 1-2, 2006, pages 149 - 154 |
| SUBIRATS ET AL., J CHROM A, vol. 1138, 2007, pages 203 - 215 |
| SUBIRATS ET AL., SEPARATION & PURIFICATION REVIEWS, vol. 36, no. 3, 2007, pages 231 - 255 |
| SUDHAKAR ET AL., J. CONTROL. RELEASE, vol. 114, 2006, pages 15 - 40 |
| TOUITOU, E., J. CONTROLLED REL, vol. 21, 1992, pages 139 - 144 |
| VENUGOPALAN ET AL., PHARMAZIE, vol. 56, 2001, pages 217 - 219 |
| VEUILLEZ, EUR. J. PHARM. BIOPHARM., vol. 51, 2001, pages 93 - 109 |
| WERMUTH: "The Practice of Medicinal Chemistry", 2003, ACADEMIC PRESS, article "Designing Prodrugs and Bioprecursors", pages: 561 - 586 |
| WILLIAMS; POLLI, J. PARENTERAL SCI. TECHNOL., vol. 38, 1984, pages 48 - 59 |
| XU ET AL., PHARMACOL. RES., vol. 46, 2002, pages 459 - 467 |
| XU ET AL., PHARMACOLOGICAL RESEARCH, vol. 46, no. 5, 2002, pages 459 - 467 |
| YANG ET AL., CHEM. PHARM. BULL., vol. 50, 2002, pages 749 - 753 |
| YANG ET AL., CHEMICAL & PHARMACEUTICAL BULLETIN, vol. 50, no. 6, 2002, pages 749 - 753 |
| YANG ET AL., S. T.P. PHARM. SCIENCES, vol. 11, no. 6, 2001, pages 415 - 419 |
| ZAINO ET AL., LAT. AM. J.PHARM., vol. 28, 2009, pages 438 - 442 |
Cited By (2)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| JP2014516969A (en) * | 2011-05-25 | 2014-07-17 | アリスジェン ソシエテ アノニム | Mucosal administration of drugs |
| WO2017140770A1 (en) | 2016-02-19 | 2017-08-24 | Forschungszentrum Borstel Leibniz-Zentrum Für Medizin Und Biowissenschaften | Means and methods for treating bacterial infections |
Also Published As
| Publication number | Publication date |
|---|---|
| US9445992B2 (en) | 2016-09-20 |
| CN102770152B (en) | 2016-07-06 |
| WO2011064316A3 (en) | 2012-01-05 |
| JP2013512226A (en) | 2013-04-11 |
| CA2782056A1 (en) | 2011-06-03 |
| US20120302502A1 (en) | 2012-11-29 |
| CA2782056C (en) | 2021-03-09 |
| CN102770152A (en) | 2012-11-07 |
| IL220022A0 (en) | 2012-07-31 |
| IL220022A (en) | 2017-04-30 |
| AU2010323117B2 (en) | 2015-09-03 |
| AU2010323117A1 (en) | 2012-06-07 |
| JP5892940B2 (en) | 2016-03-23 |
| EP2504019A2 (en) | 2012-10-03 |
| BR112012012945A2 (en) | 2020-12-29 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| EP3204045B1 (en) | Pharmaceutical formulations for the oral delivery of peptide or protein drugs | |
| US10905744B2 (en) | Pharmaceutical formulations for the oral delivery of peptide drugs | |
| JP5628026B2 (en) | Stable non-aqueous pharmaceutical composition | |
| US9445992B2 (en) | Mucosal delivery compositions comprising a peptide complexed with a crown compound and/or a counter ion | |
| JP2010529956A5 (en) | ||
| WO2018065634A1 (en) | Pharmaceutical compositions for the nasal delivery of peptide or protein drugs | |
| Youn et al. | Improved peroral delivery of glucagon-like peptide-1 by site-specific biotin modification: design, preparation, and biological evaluation | |
| WO2022268208A1 (en) | Acylated insulin-containing pharmaceutical composition | |
| EP2714088B1 (en) | Mucosal delivery of drugs | |
| US20170128542A1 (en) | Non-aqueous glucagon formulations |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| WWE | Wipo information: entry into national phase |
Ref document number: 201080062361.9 Country of ref document: CN |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 2010323117 Country of ref document: AU |
|
| ENP | Entry into the national phase |
Ref document number: 2782056 Country of ref document: CA |
|
| NENP | Non-entry into the national phase |
Ref country code: DE |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 2012540439 Country of ref document: JP |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 220022 Country of ref document: IL |
|
| ENP | Entry into the national phase |
Ref document number: 2010323117 Country of ref document: AU Date of ref document: 20101125 Kind code of ref document: A |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 2010781909 Country of ref document: EP |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 5439/CHENP/2012 Country of ref document: IN |
|
| WWE | Wipo information: entry into national phase |
Ref document number: 13512001 Country of ref document: US |
|
| REG | Reference to national code |
Ref country code: BR Ref legal event code: B01A Ref document number: 112012012945 Country of ref document: BR |
|
| REG | Reference to national code |
Ref country code: BR Ref legal event code: B01E Ref document number: 112012012945 Country of ref document: BR Free format text: SOLICITA-SE APRESENTAR NOVO ARQUIVO ELETRONICO REFERENTE A LISTAGEM DE SEQUENCIAS BIOLOGICAS, UMA VEZ QUE O TITULO DO ARQUIVO ENCONTRA-SE DISTINTO DO TITULO DO PEDIDO. |
|
| ENP | Entry into the national phase |
Ref document number: 112012012945 Country of ref document: BR Kind code of ref document: A2 Effective date: 20120525 |