WO2010151495A2 - Materials and methods for treating and preventing viral infections - Google Patents
Materials and methods for treating and preventing viral infections Download PDFInfo
- Publication number
- WO2010151495A2 WO2010151495A2 PCT/US2010/039195 US2010039195W WO2010151495A2 WO 2010151495 A2 WO2010151495 A2 WO 2010151495A2 US 2010039195 W US2010039195 W US 2010039195W WO 2010151495 A2 WO2010151495 A2 WO 2010151495A2
- Authority
- WO
- WIPO (PCT)
- Prior art keywords
- peptide
- peptidomimetic
- socs
- virus
- seq
- Prior art date
Links
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
- A61K38/16—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof
- A61K38/43—Enzymes; Proenzymes; Derivatives thereof
- A61K38/45—Transferases (2)
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/21—Esters, e.g. nitroglycerine, selenocyanates
- A61K31/215—Esters, e.g. nitroglycerine, selenocyanates of carboxylic acids
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/33—Heterocyclic compounds
- A61K31/395—Heterocyclic compounds having nitrogen as a ring hetero atom, e.g. guanethidine or rifamycins
- A61K31/495—Heterocyclic compounds having nitrogen as a ring hetero atom, e.g. guanethidine or rifamycins having six-membered rings with two or more nitrogen atoms as the only ring heteroatoms, e.g. piperazine or tetrazines
- A61K31/505—Pyrimidines; Hydrogenated pyrimidines, e.g. trimethoprim
- A61K31/519—Pyrimidines; Hydrogenated pyrimidines, e.g. trimethoprim ortho- or peri-condensed with heterocyclic rings
- A61K31/52—Purines, e.g. adenine
- A61K31/522—Purines, e.g. adenine having oxo groups directly attached to the heterocyclic ring, e.g. hypoxanthine, guanine, acyclovir
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/70—Carbohydrates; Sugars; Derivatives thereof
- A61K31/7042—Compounds having saccharide radicals and heterocyclic rings
- A61K31/7052—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides
- A61K31/7056—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides containing five-membered rings with nitrogen as a ring hetero atom
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/70—Carbohydrates; Sugars; Derivatives thereof
- A61K31/7042—Compounds having saccharide radicals and heterocyclic rings
- A61K31/7052—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides
- A61K31/706—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides containing six-membered rings with nitrogen as a ring hetero atom
- A61K31/7064—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides containing six-membered rings with nitrogen as a ring hetero atom containing condensed or non-condensed pyrimidines
- A61K31/7068—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides containing six-membered rings with nitrogen as a ring hetero atom containing condensed or non-condensed pyrimidines having oxo groups directly attached to the pyrimidine ring, e.g. cytidine, cytidylic acid
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K31/00—Medicinal preparations containing organic active ingredients
- A61K31/70—Carbohydrates; Sugars; Derivatives thereof
- A61K31/7042—Compounds having saccharide radicals and heterocyclic rings
- A61K31/7052—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides
- A61K31/706—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides containing six-membered rings with nitrogen as a ring hetero atom
- A61K31/7064—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides containing six-membered rings with nitrogen as a ring hetero atom containing condensed or non-condensed pyrimidines
- A61K31/7068—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides containing six-membered rings with nitrogen as a ring hetero atom containing condensed or non-condensed pyrimidines having oxo groups directly attached to the pyrimidine ring, e.g. cytidine, cytidylic acid
- A61K31/7072—Compounds having saccharide radicals and heterocyclic rings having nitrogen as a ring hetero atom, e.g. nucleosides, nucleotides containing six-membered rings with nitrogen as a ring hetero atom containing condensed or non-condensed pyrimidines having oxo groups directly attached to the pyrimidine ring, e.g. cytidine, cytidylic acid having two oxo groups directly attached to the pyrimidine ring, e.g. uridine, uridylic acid, thymidine, zidovudine
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
- A61K38/16—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof
- A61K38/17—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof from animals; from humans
- A61K38/19—Cytokines; Lymphokines; Interferons
- A61K38/21—Interferons [IFN]
- A61K38/212—IFN-alpha
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
- A61K38/16—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof
- A61K38/17—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof from animals; from humans
- A61K38/19—Cytokines; Lymphokines; Interferons
- A61K38/21—Interferons [IFN]
- A61K38/215—IFN-beta
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K38/00—Medicinal preparations containing peptides
- A61K38/16—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof
- A61K38/17—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof from animals; from humans
- A61K38/19—Cytokines; Lymphokines; Interferons
- A61K38/21—Interferons [IFN]
- A61K38/217—IFN-gamma
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K45/00—Medicinal preparations containing active ingredients not provided for in groups A61K31/00 - A61K41/00
- A61K45/06—Mixtures of active ingredients without chemical characterisation, e.g. antiphlogistics and cardiaca
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K9/00—Medicinal preparations characterised by special physical form
- A61K9/10—Dispersions; Emulsions
- A61K9/127—Liposomes
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P31/00—Antiinfectives, i.e. antibiotics, antiseptics, chemotherapeutics
- A61P31/12—Antivirals
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P31/00—Antiinfectives, i.e. antibiotics, antiseptics, chemotherapeutics
- A61P31/12—Antivirals
- A61P31/14—Antivirals for RNA viruses
- A61P31/16—Antivirals for RNA viruses for influenza or rhinoviruses
-
- C—CHEMISTRY; METALLURGY
- C12—BIOCHEMISTRY; BEER; SPIRITS; WINE; VINEGAR; MICROBIOLOGY; ENZYMOLOGY; MUTATION OR GENETIC ENGINEERING
- C12N—MICROORGANISMS OR ENZYMES; COMPOSITIONS THEREOF; PROPAGATING, PRESERVING, OR MAINTAINING MICROORGANISMS; MUTATION OR GENETIC ENGINEERING; CULTURE MEDIA
- C12N9/00—Enzymes; Proenzymes; Compositions thereof; Processes for preparing, activating, inhibiting, separating or purifying enzymes
- C12N9/10—Transferases (2.)
- C12N9/12—Transferases (2.) transferring phosphorus containing groups, e.g. kinases (2.7)
- C12N9/1205—Phosphotransferases with an alcohol group as acceptor (2.7.1), e.g. protein kinases
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K48/00—Medicinal preparations containing genetic material which is inserted into cells of the living body to treat genetic diseases; Gene therapy
Definitions
- Viruses are a heterogeneous group of intracellular infectious agents that depend in varying degrees on the host synthetic machinery for replication.
- the poxviruses are large, double-stranded DNA viruses that are assembled in the cytoplasm of infected cells involving complex replication mechanisms (Moss, 2007). Attachment, internalization, and disassembling of poxviruses precedes the initiation of three waves of mRNA synthesis. The early wave codes for virus growth factors and decoy cytokine receptors.
- Decoy receptors for both type I and type II interferons are produced during early protein synthesis in poxvirus infected cells, thus blunting perhaps the most important innate host defense system against viral infections (Moss and Shisler, 2001).
- a well- known example of this is the B8R protein of vaccinia virus, which is a homolog of the extracellular domain of the IFN ⁇ receptor (Moss, 2007).
- Encephalomyocarditis (EMC) virus is a small single-stranded RNA picornavirus of the plus strand orientation with wide host range (Racaniello, 2007).
- EMC virus infection is lethal, but is quite susceptible to IFN ⁇ or an IFN ⁇ mimetic treatment at early stages of infection (Mujtaba et ah, 2006).
- the IFN ⁇ mimetic is also effective against vaccinia virus infection even in the presence of B8R decoy receptor (Ahmed et ah, 2005; Ahmed et ah, 2007).
- the IFN ⁇ mimetic is a small peptide corresponding to the C- terminus of IFN ⁇ that functions intracellularly and thus does not interact with the extracellular domain of the IFN ⁇ receptor (Ahmed et ah, 2005).
- the IFN ⁇ mimetic is also effective against another large double-stranded DNA virus called herpes simplex 1 or HSV-I that replicates in the cell nucleus (Frey et ah, 2009). Close relatives include the herpes Zoster virus and cytomegalovirus (Roizman et ah, 2007).
- HSV-I herpes simplex 1
- Close relatives include the herpes Zoster virus and cytomegalovirus (Roizman et ah, 2007).
- the broad spectrum of antiviral activity of IFN ⁇ mimetics is unique in that we are unaware of any other small antiviral that exhibits strong activity against poxviruses, picornaviruses, and herpesviruses.
- the IFN system is regulated by an inducible endogenous tyrosine kinase inhibitor called suppressor of cytokine signaling 1 or SOCS-I (Yoshimura et ah, 2007; Mansell et ah, 2006; Yasukawa et ah, 1999; Kobayashi el ah, 2006; Croker et ah, 2008).
- SOCS-I is a member of a family of inducible proteins that negatively regulate IFN and other cytokine signaling via inhibition of JAK/STAT signaling (Yoshimura et ah, 2007).
- SOCS-I There are currently eight members of the SOCS family, SOCS-I to SOCS-7 and cytokine- inducible SH2 protein.
- SOCS-I has distinct regions or domains that define the mechanism by which it inhibits the function of JAK tyrosine kinases such as JAK2 that are involved in activation of STAT transcription factors (Yoshimura et ah, 2007).
- the N- terminus of SOCS-I contains a SH2 domain, and N-terminal to it is an extended SH2 sequence (ESS) adjacent to a kinase inhibitory region (KlR) (Yoshimura et ah, 2007).
- ESS extended SH2 sequence
- KlR kinase inhibitory region
- the C-te ⁇ ninus of SOCS-I contains a domain called the SOCS box, which is involved in proteasomal degradation of JAK2. It has been shown that the KIR sequence of SOCS-I binds to a peptide corresponding to the activation loop of JAK2, pJAK2(l 001-1013), and that the peptide pJAK2(1001-1013) blocked SOCS-I activity in cells (Waiboci et ah, 2007). Specifically, pJAK2(l 001-1013) enhances suboptimal IFN activity, blocks SOCS-I induced inhibition of STAT3 activation, enhances IFN ⁇ activation site promoter activity, and enhances antigen-specific proliferation.
- Influenza A virus is a segmented negative strand RNA virus that is responsible for over 30,000 deaths annually in the United States (Palese and Shaw, 2007). Pandemic influenza A virus infection can cause the deaths of millions world-wide. Type I IFNs are an important early innate immune response cytokine against influenza respiratory infections (Szretter et al, 2009). Influenza virus-encoded nonstructural protein NSl is multifunctional and is important in virus defense against IFNs by a mechanism(s) that is not fully understood but may involve induction of SOCS-I and SOCS-3, which in turn would negatively regulate IFN signaling (Pothlichet et al, 2008).
- Herpes Simplex Virus is a member of a broad class of double-stranded DNA viruses that undergo replication in the cell nucleus. Examples of other members are varicella-zoster virus (VZV) and cytomegalovirus (CMV) (Roizman el al, 2007). It is estimated that HSV-I infects 60 to 80 percent of the people throughout the world, and persists for life in the infected individuals (Diefenbach et al, 2008; Koelle and Corey, 2008; Cunningham et al, 2006). Primary infection commonly occurs through cells of the mucous membrane and is often asymptomatic.
- VZV varicella-zoster virus
- CMV cytomegalovirus
- HSV-I infection is characterized by a strong cytokine response in infected cells, particularly the induction of type I IFNs (Cunningham et al, 2006). Infection of keratinocytes, for example, results in induction of large amounts of IFN ⁇ and IFN ⁇ as well as interleukins 1, 6, and ⁇ -chemokines (Mikloska et al, 1998). IFNs, macrophages, natural killer (NK) cells, and gamma/delta T cells all play an important role in host innate immune response to HSV-I (Cunningham et al, 2006). Toll-like receptor (TLR) 2 is activated on the cell surface by HSV-I, while TLR-9 is activated intracellularly by viral DNA.
- TLR Toll-like receptor
- the latter stimulus is thought to play an important role in induction of IFN ⁇ by HSV-I (Cunningham et al, 2006).
- the adaptive immune response plays an important role in confining HSV-I and other herpesvirus infections to a latent state where CD 8 " T cells and IFN ⁇ play critical roles (Knickelbein et al, 2008; Sheridan et al, 2007; Decman et al, 2005). It is functionally connected to the innate immune system where NK cells can serve as a source of IFN ⁇ , which is also produced by CD4 and CD 8 + T cells.
- IFN ⁇ can exert direct antiviral activity as well as induce upregulation of MHC class I and class II molecules on macrophages, dendritic cells, and keratinocytes (Decman et al, 2005). Direct effects of IFN ⁇ as per a mouse model suggest that this IFN prevents reactivation of HSV by inhibition of function of the key intermediate protein ICPO (Mossman, 2005). Interaction of the antigen presenting cells with CD4 + T cells induces CD8 + T cells to control HSV-I levels in mucosal lesions (Arduino and Porter, 2008; Patel et al., 2007).
- HSV-I has developed several mechanisms to inhibit both the innate and adaptive immune responses to infection. HSV-I downregulation of class I MHC expression occurs through high affinity binding of viral immediate early gene product ICP47 to the transporter associated with antigen processing (TAP) (Burgos et al, 2006), which blocks IFN ⁇ induction of cytotoxic CD8 T cells (Goldsmith et al, 1998). IFN signaling is also inhibited by blockage of JAK/STAT transcription factor phosphorylation by an unknown mechanism (Chee and Roizman, 2004). ICPO is thought to enhance proteasome- dependent degradation of IFN stimulated genes (ISGs) (Halford et al, 2006; Edison et al, 2002). A recent study suggests that HSV-I can exert an anti -interferon effect by activation of a protein called suppressor of cytokine signaling 3 (SOCS-3) (Yokota et al, 2004).
- SOCS-3 suppressor of cytokine signaling 3
- SOCS consists of a family of inducible proteins that regulate the JAK/STAT transcription system that is critical in mediation of functions of cytokines such as the IFNs. These inducible proteins share domains of homology that characterize the SOCS family, which consists of eight identified members, SOCS-I to SOCS-7 and cytokine induced SH2 protein (CIS) (Yoshimura et al, 2007; Mansell et al, 2006; Croker et al, 2008). All of the SOCS proteins contain a SH2 domain and a C-terminal SOCS box domain that is involved in proteasomal degradation of SOCS-associated proteins.
- SOCS- 1 and SOCS-3 also contain a kinase inhibitory region (KIR) of 12 amino acids that, in conjunction with SH2, inhibits JAK tyrosine kinase activity (Yoshimura et al, 2007; Mansell et al., 2006; Croker et al, 2008).
- KIR kinase inhibitory region
- SOCS-I and SOCS-3 molecules can regulate cytokine function by proteasomal degradation and inhibition of the relevant JAK activity (Yoshimura et a!.. 2007; Croker el al., 2008).
- HIV infection probably due to HSV-associated lesions (WaId and Link, 2002). Because of this interplay between HSV and HIV, it is conceivable that anti-HSV treatment may reduce the incidence of infection with HIV.
- the subject invention concerns materials and methods for inhibiting activity and/or replication of a broad spectrum of viruses in humans and animals.
- a method for treating or preventing viral infection in a human or animal by administering an effective amount of a peptide that is an antagonist of SOCS-I and/or SOCS-3.
- the peptide corresponds to the activation loop of janus kinase JAK2.
- the peptide comprises the amino acid sequence: LPQDKEYYKVKEP (pJAK2 (1001 - 1013)) (SEQ ID NO:1), or a biologically active fragment or variant thereof that exhibits antiviral activity.
- viruses whose activity and/or replication can be inhibited using the present invention include, but are not limited to, vaccinia virus, EMC virus, influenza virus, and herpes simplex virus.
- the subject invention can also be used to prevent viral infection in an uninfected human or animal.
- the subject invention also concerns peptides, and compositions comprising the peptides, that are an antagonist of SOCS-I protein.
- the peptide corresponds to the activation loop of janus kinase JAK2.
- the peptide comprises the amino acid sequence: LPQDKEYYKVKEP (pJAK2 (1001- 1013)) (SEQ ID NO:1), or a biologically active fragment or variant thereof that exhibits antiviral activity.
- Compositions contemplated within the scope of the invention can comprise one or more peptides of the invention and optionally one or more other antiviral compounds.
- Figures 1A-1D Differential response to IFN ⁇ and IFN ⁇ mimetic peptide in fibroblasts (L929) and keratinocytes (HEL-30).
- L929 fibroblasts ( Figures IA and 1C) and HEL-30 keratinocytes ( Figures IB and ID) were grown overnight and treated with IFN- ⁇ ( Figures IA and IB), or IFN ⁇ mimetic ( Figures 1C and ID) at the indicated concentrations for 24 hours, after which HSV-I (syn 17 h ) was added at an moi of 0.1.
- Cells were incubated for 48 hours, rinsed with HBSS, fixed and stained with crystal violet.
- FIGS 2A-2D HSV-I infection causes induction of SOCS-I in keratinocytes (HEL-30 cells), but not in fibroblasts (L929 cells).
- Figure 2A HEL-30 and L929 cells were infected with HSV-I at an moi of 1 for 12 hours. Total RNA was extracted and used as a template for RT-PCR using primers specific for SOCS-I or GAPDH, the control. Data are presented as the ratio of SOCS-I to GAPDH.
- HEL-30 ( Figure 2B) and L929 Figure 2C). cells exhibit differences in SOCS-I protein expression as analyzed by Western blot analysis. Cells were infected with HSV-I at an moi of 2.
- HEL-30 Figure 3A
- L929 Figure 3B
- HEL-30 Figure 3A
- L929 Figure 3B
- HEL-30 Figure 3A
- L929 Figure 3B
- HEL-30 Figure 3A
- L929 Figure 3B
- HEL-30 Figure 3A
- L929 Figure 3B
- Cells were washed in PBS, harvested, lysed, and whole-cell extracts were isolated. Extracts were subjected to 10% SDS-PAGE. Proteins were blotted onto a PVDF membrane and probed with an antibody specific for pSTAT-la (Tyr 701). Filters were stripped and re-probed with antibody to total STATIa to ascertain equal loading of proteins.
- Figure 4. HSV-I infection increases transcription from the SOCS-I promoter.
- HEL-30 cells were cultured overnight in 12-well plates and transfected with a luciferase reporter construct containing the full-length SOCS-I promoter. Cells were incubated for 24 hours and then mock- infected or infected with HSV-I at an moi of 2 for 4 hours, after which they were treated with IFN- ⁇ at 2000 U/ml for 2 hours. Cell lysates were collected and luciferase activity was measured in a single-tube luminometer. Values given are expressed as luciferase units measured from the SOCS-I reporter divided by luciferase units measured from a co-transfected constitutive reporter and subsequently normalized to medium controls. Values are representative of triplicate wells of the two independent experiments.
- Figures SA and 5B A peptide antagonist of SOCS-I (Figure 5A) or siRNA for SOCS-I (Figure 5B) reduced HSV-I -induced CPE in HEL-30 cells.
- Figure 5A HEL-30 cells were cultured overnight in 96-well plates and treated with 100 U/ml IFN ⁇ alone or different concentrations of pJAK2(l 001 -1013) with or without 100 U/ml of IFN ⁇ . Following treatment for 24 hours, cells were mock-infected or infected with HSV-I at an moi of 0.1. Plates were incubated 48 hours, washed with PBS, fixed and stained with crystal violet. Absorbance units of each well were calculated using Multi-Gauge.
- HSV-I- induced cytopathic effect is reduced by treatment with SOCS-I siRNA.
- HEL-30 cells were transfected with control or SOCS-I siRNA, incubated for 48 hours, then treated with IFN- ⁇ for 6 hours, and subsequently infected with 100 pfu HSV-I (synl7 + ). At 72 hours post-infection, the cells were fixed and stained with crystal violet. Plates were scanned using a flatbed scanner. Densitometry measurements of each well were made using NIH Image J.
- FIGS 6A-6C Overexpression of SOCS-I inhibits the antiviral activity of IFN- ⁇ in HSV-I -infected L929 cells.
- Figure 6A Transfection with cDNA expressing SOCS- 1.
- L929 cells were transfected with SOCS-I expression plasmid for one day. Cell extracts were then electrophoresed and probed with an antibody to SOCS-I followed by stripping and probing with ⁇ -tubulin antibody as a control.
- Figure 6B L929 fibroblasts were grown overnight in 12 well-plates to -90% confluence. Cells were transfected with the indicated amounts of control plasmid or pFLAG-SOCS-1 plasmid.
- HSV-I HSV-I (syn 17+) at an moi of 0.1, and then incubated for 48 hours, washed with HBSS, fixed, and stained with crystal violet. Absorbance units of each well were calculated using Multi-Gauge software. ( Figure 6C). HSV-I -induced CPE is increased in L929 cells treated with a SOCS-I peptide mimetic.
- L929 fibroblasts were grown overnight and treated with ⁇ FN- ⁇ (100 U/ml) and Tkip (20 ⁇ M), or Tkip2A (20 ⁇ M) for 24 hours, after which HSV-I (syn 17+) was added at an moi of 0.1.
- Cells were incubated for 48 hours, washed with HBSS, fixed and stained with crystal violet as in (Figure 6A) above. Values are expressed as percent cell survival relative to mock-infected controls. Results are representative of duplicate wells of two independent experiments.
- Figures 7A-7C Reduction in SOCS-I gene activation by HSV-I ICPO mutant in HEL-30 keratinocytes.
- Figure 7A HEL-30 cells were cultured overnight in 24-well plates and treated with indicated amounts of IFN ⁇ . Following treatment for 24 hours, cells were mock-infected or infected with HSV-I at an moi of 0.1. Plates were incubated 48 hours, washed with PBS, fixed and stained with crystal violet. Absorbance units of each well were calculated using Multi-Gauge. Values are expressed as percent cell survival relative to mock-infected controls. Values are representative of duplicate wells of two independent experiments. ( Figure 7B).
- HEL-30 cells were cultured overnight in 24-well plates and treated with 100 U/ml IFN ⁇ alone and with different concentrations of Tkip. Following treatment for 24 hours, cells were mock-infected or infected with HSV-I ICPO mutant at an moi of 0.1. Plates were incubated 48 hours, washed with PBS, fixed and stained with crystal violet and absorbance measured as in (Figure 7A). There were statistically significant differences between IFN ⁇ , Tkip, IFN ⁇ + HSV-I and Tkip + HSV- 1 when compared to the untreated cells (P ⁇ 0.001) as determined by Mann-Whitney signed rank test. (Figure 7C).
- HEL-30 cells were cultured overnight in 12-well plates and transfected with a luciferase reporter construct containing the full-length SOCS-I promoter. Cells were incubated for 24 hours and then mock-infected or infected with HSV-I or HSV ICPO mutant at moi of 2 for 4 hours. Cell lysates were collected and luciferase activity was measured in a single-tube lurninometer. Values given are expressed as luciferase units measured from the SOCS-I reporter divided by luciferase units measured from a co-transfected constitutive reporter and subsequently normalized to medium controls. Values are representative of triplicate wells of the two independent experiments.
- FIG. 8 pJAK2(1001-1013) synergizes with IFN ⁇ to protect RAW264.7 murine macrophages against HSV-I.
- Murine macrophage cell line RAW264.7 was treated with IFN ⁇ , pJAK2(1001-1013). IFN ⁇ and different concentrations of pJAK2(1001-1013), or IFN ⁇ and different concentrations of an alanine substituted mutant pJAK2(1001-1013)2A, followed by infection with HSV-I at an moi of 0.1. Plates were incubated 48 hours, washed with PBS, fixed and stained with crystal violet. Absorbance units of each well were calculated using Multi-Gauge. Values are expressed as percent cell survival relative to mock-infected controls.
- vaccinia virus (2 x 10 6 pfu) was given intranasally. Survival of mice was followed over a period of 30 days. The significance of difference between different treatments was measured by log rank survival method, which gave P values of 0.002, 0.002. and 0.02 for the administration of 200, 50, and 10 ⁇ g of lipo- pJAK2(1001-1013) versus the control peptide, respectively.
- mice On day 0, mice were infected intranasally with 1 x 10 6 pfu of vaccinia virus. Survival of mice was followed over a period of 30 days.
- IFN ⁇ mimetic and pJAK2 peptides activate GAS promoter element synergistically.
- WISH cells were co-transfected with plasmids expressing a GAS promoter element linked to a firefly luciferase and another plasmid expressing Renilla luciferase an internal control, followed by addition of the peptides indicated. After overnight incubation, relative luciferase activity was measured, and is expressed as average ⁇ s.d.
- Figures 12A and 12B Time course of inhibition of vaccinia virus replication by pJAK2(1001-1013) by one-step growth curve.
- BSC-40 cells grown to confluency were left untreated, or treated with lipo- pJAK2(1001-1013), or its alanine substituted mutants at 50 ⁇ M for one hour. Cells were then infected with vaccinia virus at a moi of 5 for one hour. After one hour, the cells were washed and incubated in the presence of the same concentrations of peptides for the indicated times.
- Cell extracts ( Figure 12A) and supernatants (Figure 12B) obtained from these were titrated for the amount of intracellular and extracellular virus, respectively. Note the difference of the scale on y axis, indicating that there is less of extracellular virus than intracellular.
- FIGS 13A and 13B pJAK2(1001-1013) inhibits vaccinia virus replication in a dose-dependent manner as determined by a one-step growth curve.
- BSC-40 cells were grown to confluency and left untreated or treated with the indicated amounts of lipo- pJAK2(1001-1013) or the alanine substituted control peptide for one hour. Cells were next infected with vaccinia virus at a moi of 5. After one hour, the cells were washed and incubated in the presence of the same concentrations of peptides for one day. Supernatant and cell extracts obtained were titrated for the amount of intracellular (Figure 13A) and extracellular (Figure 13B) virus, respectively.
- FIGS 14A-14C pJAK2(1001-1013) treated cells had increased levels of endogenous IFNB.
- pJAK2(1001-1013) increases levels of endogenous TFN ⁇ .
- L929 cells were seeded onto 6-well plates at 1 x 10 6 cells/well, grown to confluency and treated with peptides at varying concentrations for 30 or 60 min at 37°C. The cells were washed and lysed and whole cell extracts were resolved on 12% SDS- PAGE, transferred onto a nitrocellulose membrane, and probed with anti-IFN ⁇ antibodies.
- pJAK2(1001-1013) has no effect on endogenous IFN ⁇ levels.
- L929 cells were seeded onto 6-well plates at 1 x 10 6 cells/well, grown to confluency and treated with peptides at varying concentrations for 30 or 60 min at 37 0 C. The cells were washed and lysed and whole cell extracts were resolved on 12% SDS-PAGE, transferred onto a nitrocellulose membrane, and probed with anti-IFN ⁇ antibodies.
- pJAK2(1001 -1013) decreased levels of endogenous SOCS-I.
- L929 cells were seeded onto 6-well plates at 1 x 10 6 cells/well, grown to confluency and treated with peptides at varying concentrations for 30 or 60 min at 37 0 C. The cells were washed and lysed and whole cell extracts were resolved on 12% SDS-PAGE, transferred onto a nitrocellulose membrane, and probed with anti-SOCSl-KIR antibodies.
- Figures ⁇ 5A-15F Adaptive immune response in mice that recovered from vaccinia virus infection with pJAK2(1001-1013) treatment.
- Figure 15A shows survival of mice against rechallenge with vaccinia virus.
- Figure 15B shows cell mediated immune response in mice that recovered from vaccinia virus infection with pJAK2(1001 -1013) treatment.
- [ 3 H] thymidine was added for 8 hours, and its incorporation was followed.
- Stimulation index refers to the incorporation in splenocytes cultured with test antigen divided by incorporation in splenocytes cultured with medium alone. The averages with s.d. are shown.
- Figures 16A-16C pJAK2(1001-1013) exerts an adjuvant effect at both cellular and humoral levels.
- Isolated splenocytes (5 x 10 6 per well) were seeded in quadruplicate in 96 well plate and incubated with 0.5 ⁇ g of BSA for three days with the addition of 1 ⁇ Ci per well of 3 H-thymidine for the last 6 hours. Cells were transferred to filter and counted in a scintillation counter. Data are representative of three individual experiments.
- FIG. 16C shows stimulation of macrophages.
- RAW 264.7 cells (5 x 10 6 per well) were seeded in triplicate in microtiter plates and incubated overnight. The indicated amounts of pJ AK2 or control peptide were added to the cells and incubated for 4 h. after which 2 ⁇ g pf LPS were added and the cells were incubated for 3 days. Nitric oxide was measured by Griess reagent and absorbance was read in a plate reader.
- FIGS 17A-17C pJAK2(1001-1013) possesses antiviral activity against EMCV.
- mouse L929 cells were plated and grown to confluence on a 96-well plate.
- Various concentrations of mouse IFN ⁇ , IFN ⁇ (95-125), IFN ⁇ (95-132), pJAK2 [pJAK2(1001-1013)] and JAK2m [pJAK2(1001-1013)2A] peptides were incubated with L929 cells for 2 h, after which 200 pfu/well of EMCV were added. After 1 h, virus was removed and media were added to all wells, followed by incubation for 24 h.
- FIG. 18 shows that SOCS antagonist and IFN mimetic possess antiviral activity against influenza virus.
- MDCK cells were treated with the above peptides at 2 ⁇ M for 18 hours. Cells were infected with influenza A/PR8 virus (103 TCID50/ml), and incubated for 1 hour at 35°C. The media was removed and replaced with infection media, and the cells were incubated for an additional 24 hours at 35°C. The cells were stained with crystal violet and absorbance was measured. Data from three replicates.
- Figure 19 shows HA inhibition of influenza A PR8 by IFN - ⁇ mimetic and SOCS- 1 antagonist.
- MDCK cells were treated with peptides for 2 hours, then challenged with influenza A/PR8 virus and incubated at 35 0 C for 36 hours. The supernatants were collected and a standard hemagglutination assay was performed in triplicate. The data are presented as hemagglutination units/ml ⁇ SEM and are representative of three independent experiments.
- Figure 20 shows pJAK2(1001-1013) can rescue mice from an intranasal infection with vaccinia virus.
- vaccinia virus (2 x 10 6 pfu) was given intranasally. Survival of mice was followed over a period of 30 days.
- Figures 21A and 21B show that lipo-pJAK2(1001-1013) is internalized by mouse peritoneal cells in vivo and by L929 fibroblast cells in culture. Lipo-pJAK2(l 001 -1013) was coupled to FlTC as per Materials and Methods.
- Figure 21 A shows peritoneal cell uptake. Mice were injected i.p. with 15 ⁇ g FITC-lipo- pJAK2(1001-1013) or an equivalent amount of FITC alone. Peritoneal cells were harvested after two hours and the cells were examined by confocal fluorescent and contrast microscopy for FITC labeling.
- Figure 21B shows L929 cells uptake.
- FIGS. 22A-22E show pJAK2(1001-1013) exerts an adjuvant effect at both cellular and humoral levels.
- mice received SOCS antagonist (200 ⁇ g), the control peptide (JAK2A) (200 ⁇ g), or a combination of SEA/SEB (SAg, 25 ⁇ g each).
- SOCS antagonist 200 ⁇ g
- JNK2A control peptide
- SAg 25 ⁇ g each
- BSA 50 ⁇ g
- SAg 25 ⁇ g each
- Sera were tested for IgG to LPS or BSA by ELISA.
- the secondary Ab used was anti-mouse IgG conjugated to HRP. After washing, substrate was added and color was allowed to develop before reading absorbance at 490 nm.
- FIG. 22D shows LPS stimulation.
- RAW264.7 cells (5 x 10 6 per well) were seeded in triplicate and incubated overnight. The indicated amounts of pJAK2(1001-1013) or control peptide, were added to the cells and incubated for 4 h, after which 2 ⁇ g/ml of LPS was added and the cells were incubated for 3 days. Nitric oxide was measured by Griess reagent and absorbance was read. *P ⁇ 0.001.
- Figure 22E shows Poly I:C stimulation.
- Murine macrophages (RAW264.7) were incubated with lipophilic pJAK2(1001-1013), or control peptide for 2 h, followed by stimulation with poly 1:C at 0.1 ⁇ g/ml for 72 h. Culture supematants were collected and nitrite concentration determined using Griess reagent. ** p ⁇ 0.0001.
- Figures 23A-23D show pJAK2(l 001-1013) binding to SOCSl-KIR and SOCS3- KIR as determined by an antibody ELISA and its reversal of SOCS-I and SOCS-3 mediated inhibition of GAS promoter activity.
- SOCSl-KIR Figure 23A
- SOCS3- KIR Figure 23B
- pJAK2 or control peptide IFN ⁇ (95-106) was immobilized at 3 ⁇ g per well in a 96 well plate. Following blocking, various concentrations of SOCSl-KIR or SOCS3-KIR were added and the plates were incubated for 1 hour.
- L929 cells were transfected with a GAS promoter linked to firefly iuciferase reporter gene and a control plasmid with constitutively expressed Renilla Iuciferase. Where indicated SOCS-I or SOCS-3 expressing plasmids were included in the transfection. A plasmid without a promoter attached to firefly Iuciferase was used as a control in the first bar indicated as empty vector. After 24 hr of transfection, cell extracts were assayed for relative Iuciferase activities. pJAK2 peptide was used at 30 ⁇ M. Figure 23D shows JAK2 associates with SOCS-3 in cells.
- IP immunoprecipitated
- FIG. 24 pJAK2(1001-1013)-treated cells had increased levels of phosphorylated STATIa.
- L929 cells were seeded onto six-well plates at 1 x 10 6 cells/well, grown overnight, and treated with pJAK2(1001-1013) (2, 10, 25 ⁇ M) or JAK2(1001-1013)2A (25 ⁇ M) for 1 h at 37 0 C. The cells were washed and lysed, and whole-cell extracts were resolved on 12% SDS-PAGE, transferred onto nitrocellulose membrane, and probed with antibodies to pSTATla or STATIa. Similar results were obtained in three different experiments. Relative intensities of the pSTATl a band are shown under the blot. As determined by the unpaired t test on non-normalized readings, the intensity in the pJAK2-treated band versus the untreated had ap value of 0.0002.
- Figure 25 shows synergy between SOCS-I antagonist and IFN- ⁇ mimetic in inhibition of EMC virus.
- pJAK2(1001-1013) at 2 ⁇ M and IFN- ⁇ (95-132) at 5 ⁇ M together were incubated with L929 cells, after which 200 PFU/well EMC virus was added. After 1 hour, virus was removed and media was added, followed by incubation for 24 hours. Cells were stained with crystal violet and plates were scanned. National Institutes of Health ImageJ software was used for analysis.
- Figure 26 shows synergy in protection of mice infected with EMC virus using suboptimal levels of pJAK2(10 ⁇ l-1013) (10 ⁇ g) and ⁇ FN- ⁇ (95-132) (2 ⁇ g).
- mice were injected daily i.p. beginning at day -2 with pJAK2(1001-1013) at 50, 100, and 200 ⁇ g and control peptide at 200 ⁇ g.
- 50 PFU/mouse was injected i.p.
- Survival data are presented as Kaplan-Meier plots. The significance of difference were/? ⁇ 0.005, ⁇ 0.005, and NS for 200, 100, and 50 ⁇ g of antagonist versus the control, respectively.
- SEQ ID NO:1 is an amino acid sequence of a pJAK2(1001 -1013) peptide of the present invention.
- SEQ ID NO:2 is an amino terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:3 is an amino terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:4 is an amino terminal deletion of the amino acid sequence shown in
- SEQ ID NO:5 is an amino terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:6 is an amino terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:7 is a carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:8 is a carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:9 is a carboxy terminal deletion of the amino acid sequence shown in
- SEQ ID NOtIO is a carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:11 is a carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO: 12 is an amino and carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO: 13 is an amino and carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO: 14 is an amino and carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO:15 is an amino and carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO:16 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO: 17 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO:l .
- SEQ ID NO: 18 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO: 19 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:20 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:21 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO: 22 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:23 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:24 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:25 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO:!.
- SEQ ID NO:26 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:27 is an amino te ⁇ ninal addition of the amino acid sequence shown in SEQ ID NO:!.
- SEQ ID NO:28 is an amino te ⁇ ninal addition of the amino acid sequence shown in SEQ ID NO:!.
- SEQ ID NO:29 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:30 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:31 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:!.
- SEQ ID NO:32 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:33 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:! .
- SEQ ID NO:34 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:35 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:36 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:37 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO.38 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NOt39 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NQ:40 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:41 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:42 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:43 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:44 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:!.
- SEQ ID NO:45 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:!.
- SEQ ID NO:46 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO:47 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO:48 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO:49 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:50 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO:51 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO:52 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO: 53 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO: 54 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO: 55 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:56 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO:57 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:58 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:59 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
- SEQ ID NO:60 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
- SEQ ID NO:61 is the amino acid sequence of a peptide designated herein as Tkip.
- SEQ ID NO:62 is the amino acid sequence of a peptide designated herein as Tkip.
- SEQ ID NO:63 is the amino acid sequence of a peptide designated herein as
- SEQ ID NO:64 is the amino acid sequence of a peptide designated herein as SOCS1-KIR2A.
- SEQ ID NO:65 is the amino acid sequence of a peptide designated herein as MuIFN ⁇ (95-106).
- SEQ ID NO:66 is the amino acid sequence of a peptide designated herein as MuIFN ⁇ (95-125).
- SEQ ID NO:67 is the amino acid sequence of a peptide designated herein as MuIFN ⁇ (95-132).
- SEQ ID NQ:68 is the amino acid sequence of a peptide designated herein as
- SEQ ID NO:69 is the amino acid sequence of a peptide designated herein as MAL Box 1.
- SEQ ID NO: 70 is the amino acid sequence of a peptide designated herein as MAL 159.
- SEQ ID NO:71 is the amino acid sequence of a peptide designated herein as JAK2(1001-1013)m.
- SEQ ID NO:72 is a nucleotide sequence of a forward primer for human SOCS-I promoter.
- SEQ ID NO:73 is a nucleotide sequence of a reverse primer for human SOCS-I promoter.
- SEQ ID NO:74 is a nucleotide sequence of a GAS promoter element of a human IRF-I gene.
- SEQ ID NO: 75 is the amino acid sequence of a peptide designated herein as huIFN ⁇ (95-134).
- SEQ ID NO: 76 is the amino acid sequence of a peptide designated herein as SOCS3-KIR. DETAILED DESCRIPTION OF THE INVENTION
- the subject invention concerns materials and methods for inhibiting activity and/or replication of a broad spectrum of viruses in humans and animals.
- a method for treating or preventing viral infection in a human or animal by administering an effective amount of peptide, or a polynucleotide encoding the peptide, or a peptidomimetic, that is an antagonist of SOCS- 1 and/or SOCS-3, or a composition comprising one or more of the peptide, peptidomimetic, or polynucleotide.
- the peptide corresponds to the activation loop of janus kinase JAK2.
- the peptide comprises the amino acid sequence: 10111 LPQDKEYYKVKEP 1013 (pJAK2 (1001-1013)) (SEQ ID NO:1), or a fragment or variant thereof that exhibits antiviral activity.
- the tyrosine at amino acid position 7 of SEQ ID NO:1 (which corresponds to the tyrosine at residue 1007 of JAK2) is phosphorylated.
- an effective amount of a polynucleotide encoding a peptide of the invention is administered to a person or animal in need of treatment.
- the polynucleotide is provided in an expression construct.
- the polynucleotide encodes a peptide comprising the amino acid sequence shown in SEQ ID NQ: 1, or a fragment or variant thereof that exhibits antiviral activity.
- viruses whose activity and/or replication can be inhibited using the present invention include, but are not limited to, herpes viruses, poxviruses, and picornaviruses, such as vaccinia virus. EMC virus, influenza virus, herpes zoster virus, cytomegalovirus, and herpes simplex virus (e.g., HSV-I).
- the influenza virus is an influenza A virus.
- the influenza A virus is serotype HlNl.
- the subject invention can also be used to prevent viral infection in an uninfected human or animal.
- the subject invention also concerns peptides that are an antagonist of SOCS-I and/or SOCS-3 protein, and compositions comprising the peptides.
- the peptide corresponds to the activation loop of janus kinase JAK2.
- the peptide comprises the amino acid sequence: 1001 LPQDKEYYKVKEP 1013 (pJAK2 (1001-1013)) (SEQ ID NO:1), or a fragment or variant thereof that exhibits antiviral activity.
- the tyrosine at amino acid position 7 of SEQ ID NO:1 i.e., the tyrosine that is underlined in the sequence LPQDKEYYKVKEP
- a peptide of the invention consists of the amino acid sequence shown in SEQ ID NO: 1, and optionally wherein the tyrosine at position 7 is phosphorylated.
- Peptides of the invention can be readily prepared using standard techniques known in the art, including chemical synthesis (Merrifield, 1963) and genetic engineering.
- the subject invention also concerns non-peptide compounds (peptidomimetics) that mimic the function of peptides of the present invention and that can be used in the methods of the present invention.
- peptidomimetics peptidomimetics
- Methods for preparing peptidomimetics based on structural features of the amino acid sequence of a peptide that pertain to functional or binding properties are known in the art (Kazmierski (1998)).
- the subject invention also concerns polynucleotides that encode the peptides of the invention and their use in the methods of the present invention.
- Methods and materials for synthesizing and preparing a polynucleotide encoding a peptide of the invention are well known in the art. Because of the degeneracy of the genetic code, a variety of different polynucleotide sequences can encode a peptide of the present invention. In addition, it is well within the skill of a person trained in the art to create alternative polynucleotide sequences encoding the same, or essentially the same, peptides of the subject invention.
- references to "essentially the same" sequence refers to sequences which encode amino acid substitutions, deletions, additions, and/or insertions which do not materially alter the functional activity of the peptide encoded by the polynucleotides of the present invention.
- Variant peptides having amino acid substitutions, deletions, additions, and/or insertions which do not materially alter the functional antiviral activity of the peptide can also be prepared using standard techniques known in the art, and such variant peptides are encompassed within the scope of the present invention.
- Polynucleotide sequences encoding a peptide of the invention can be selected based on preferred codon usage of the animal in which it is to be administered. For example, if the peptide is to be administered to a human, the polynucleotide sequence can be selected for preferred codon usage in human cells.
- the subject invention also concerns compositions comprising one or more peptides, peptidomimetics., or polynucleotides of the invention.
- a composition further comprises a suitable carrier, diluent, or buffer.
- compositions contemplated within the scope of the invention can comprise one or more peptides, peptidomimetics, or polynucleotides of the invention and, optionally, one or more other antiviral compounds.
- the pJAK2 peptide can be provided in a composition with one or more of IFN ⁇ , IFN ⁇ , IFN ⁇ , acyclovir (Zovirax), zidovudine (AZT), lamivudine (3TC), zanamivir (Relenza), oseltamivir (Tamiflu), valacyclovir (Valtrex), amantadine (Symmetrel), rimantadine (Flumadine), cidofovir (Vistide), foscamet (Foscavir), ganciclovir (Cytovene), ribavirin (Virazole), nelfmavir (Viracept), ritonavir (Norvir), rifampin (Rifadin), and
- the composition comprises a peptide of the invention in a pharmaceutically or physiologically acceptable carrier, buffer, or diluent.
- Compositions of the invention can also comprise peptides such as an IFN ⁇ mimetic. Examples of IFN ⁇ mimetic peptides are described in U.S. Patent Nos. 5,770,191 and 6,120,762.
- the IFN ⁇ mimetic peptide comprises the amino acid sequence shown in SEQ ID NO:67 or SEQ ID NO:75, or a fragment or variant thereof that exhibits antiviral activity.
- a composition of the invention can also comprise one or more peptides comprising the amino acid sequence shown in SEQ ID NO:61 (Tkip peptide), or a fragment or variant thereof that exhibits antiviral activity, and/or a peptide comprising the amino acid sequence shown in SEQ ID NO:63 (SOCSl-KIR), or a fragment or variant thereof that exhibits antiviral activity.
- a peptide, polynucleotide, peptidomimetic, composition or other agent of the invention is administered to the person or animal prior to infection by a virus. Also contemplated within the scope of the methods is that a peptide, polynucleotide, peptidomimetic, composition, or other agent of the invention is administered at the time of infection or after the person or animal has been infected.
- a person or animal to be treated is one that has previously been vaccinated against infection by a virus, such as a poxvirus. In another embodiment, the person or animal has not been previously vaccinated against the virus.
- peptides, polynucleotides, and peptidomimetics of the invention are modified so as to enhance uptake into a cell.
- a lipophilic group is attached to a peptide, polynucleotide, peptidomimetic. or other agent of the invention.
- a palmitoyl-lysine group is attached to the peptide, for example at the N-terminus of the peptide.
- Other methods for enhancing uptake of a peptide, polynucleotide, or peptidomimetic into a cell are known in the art and are contemplated within the scope of the invention.
- Peptides, polynucleotides, peptidomimetics, compositions, and other agents of the invention can also be delivered into cells by encapsulation of the peptide, polynucleotide, peptidomimetics, and other agents of the invention within a liposome.
- Methods for encapsulation of peptides, polynucleotides, peptidomimetics, and other agents of the invention within liposomes are well known in the art.
- the subject invention also concerns methods for inducing an antiviral state in a cell.
- a cell is contacted with an effective amount of a peptide, polynucleotide, peptidomimetic, or a composition of the invention.
- the peptide comprises the amino acid sequence of SEQ ID NO:1, or a fragment or variant thereof that exhibits antiviral activity.
- the tyrosine at amino acid position 7 of SEQ ID NO:1 (which corresponds to the tyrosine at position 1007 (i.e., the tyrosine that is underlined in the sequence LPQDKEYYKVKEP)) is phosphorylated.
- a peptide of the invention consists of the amino acid sequence shown in SEQ ID NO:1, wherein the tyrosine at position 7 is phosphorylated.
- the composition comprises a peptide of the invention and an antiviral drug and/or a IFN ⁇ mimetic.
- the cell can be a human or mammalian cell.
- the cell can be a keratinocyte, a fibroblast, a macrophage, or a lymphocyte.
- Peptides, polynucleotides, peptidomimetics, and/or other agents of the invention can be delivered to a cell either through direct contact of peptide, etc. with the cell or via a carrier means.
- Carrier means for delivering compositions to cells are known in the art and include encapsulating the composition in a liposome moiety, and attaching the peptide, polynucleotide, or peptidomimetic to a protein or nucleic acid that is targeted for delivery to the target cell.
- Published U.S. Patent Application Nos. 20030032594 and 20020120100 disclose amino acid sequences that can be coupled to another peptide, protein, or nucleic acid and that allows the peptide, protein, or nucleic acid to be translocated across biological membranes.
- Published U.S. Patent Application No. 20020035243 also describes compositions for transporting biological moieties, such as peptides and proteins across cell membranes for intracellular delivery.
- Peptides can also be delivered using a polynucleotide that encodes a subject peptide.
- the polynucleotide is delivered to the cell where it is taken up and the polynucleotide is transcribed into RNA and the RNA is translated into the encoded peptide.
- Antiviral activity can be induced in a cell against viruses such as vaccinia virus, EMC virus, influenza virus, herpes simplex virus (e.g., HSV-I). cytomegalovirus, herpes zoster virus, and other herpes viruses, poxvirus, coxsackie virus, lentivirus (e.g., HIV), and picornavirus.
- the subject invention also concerns methods for treating a disorder in a person or animal comprising administering an effective amount of a peptide, polynucleotide, peptidomimetic, composition, or other agent of the invention to the person or animal, wherein the disorder is associated with a SOCS protein, such as SOCS-I and/or SOCS-3 protein.
- the disorder is characterized by aberrant, constitutive, or elevated expression of a SOCS-I and/or SOCS-3 protein.
- the subject invention also concerns methods for modulating an immune response in a person or animal, wherein the method comprises administering an effective amount of a peptide, polynucleotide, peptidomimetic, composition, or other agent of the invention to the person or animal.
- the immune response involves expression and/or activity of a SOCS-I and/or SOCS-3 protein.
- the immune response can also involve expression and activation of a JAK and/or a STAT protein.
- SOCS-I induced inhibition of STAT3 activation is blocked using a peptide, polynucleotide, peptidomimetic, composition, or other agent of the invention.
- inhibition of JAK2 kinase activity by a SOCS protein e.g., SOCS-I or SOCS-3 is blocked or inhibited using the subject invention.
- the method enhances or increases the person's or animal's immune response against a tumor or cancer cell (or antigen thereon) or a virus (or an antigen thereof).
- the person or animal is infected with an immunodeficiency virus (e.g., human immunodeficiency virus (HIV)) and the method enhances or increases the person's or animal's immune response against the virus.
- immunodeficiency virus e.g., human immunodeficiency virus (HIV)
- Peptides useful in the methods of the subject invention include the specific peptides exemplified herein as well as equivalent peptides which may be. for example, somewhat longer or shorter than the peptides exemplified herein.
- peptides having from 1 to about 15 or more amino acids added to one or both ends of a peptide of the subject invention examples include peptides having amino acids added to one or both ends of the exemplified peptide (SEQ ID NO:1) and contemplated within the scope of the present invention are shown in SEQ ID NO: 16 to SEQ ID NO:60.
- SEQ ID NO: 16 to SEQ ID NO:60 examples of peptides having 1 to about 5 amino acids are removed from one or both ends of a peptide of the subject invention.
- peptide fragments of the exemplified peptides and contemplated within the scope of the present invention are shown in SEQ ID NO:2 to SEQ ID NO:15.
- amino acids could be added to one end of a peptide of the invention and amino acids removed from the other end of the peptide.
- the subject invention includes, but is not limited to, the exemplified longer and shorter peptides.
- Peptides included within the scope of the invention include peptides from about 5 to about 50 or more amino acids in length.
- peptides within the scope of the invention are peptides of 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, and 50 amino acids in length.
- peptides of the invention consist of about 10 to about 20 amino acids.
- peptides of the invention consist of about 10 to about 15 amino acids.
- AU longer and shorter peptides are within the scope of the subject invention as long as the longer or shorter peptide retains substantially the same antiviral activity as the peptides exemplified herein.
- the subject invention also concerns polypeptides that comprise a peptide sequence of the present invention, or a fragment or variant of that sequence, and that are able to inhibit viral activity.
- Peptides having substitution of amino acids other than those specifically exemplified in the subject peptides are also contemplated within the scope of the present invention.
- non-natural amino acids can be substituted for the amino acids of a peptide of the invention, so long as the peptide having substituted amino acids retains substantially the same activity as the peptide in which amino acids have not been substituted.
- non-natural amino acids include, but are not limited to, ornithine, citrulline, hydroxyproline, homoserine, phenylglycine, taurine, iodotyrosine, 2,4-diaminobutyric acid, a-amino isobutyric acid, 4-aminobutyric acid, 2-amino butyric acid, ⁇ -amino butyric acid, e-amino hexanoic acid, 6-amino hexanoic acid, 2-amino isobutyric acid, 3 -amino propionic acid, norleucine, norvaline, sarcosine, homocitralline, cysteic acid, t -butylglycine, t-butylalanine, phenylglycine, cyclohexylalanine, ⁇ -alanine, fluoro-amino acids, designer amino acids such as ⁇ -methyl amino acids, C-methyl
- Amino acids can be generally categorized in the following classes: non-polar, uncharged polar, basic, and acidic. Conservative substitutions whereby a peptide having an amino acid of one class is replaced with another amino acid of the same class fall within the scope of the subject invention so long as the peptide having the substitution still retains substantially the same biological activity as a peptide that does not have the substitution.
- Table 1 below provides a listing of examples of amino acids belonging to each class.
- the peptides of the present invention can be formulated into pharmaceutically- acceptable salt forms.
- Pharmaceutically-acceptable salt forms include the acid addition salts and include hydrochloric, hydrobromic, nitric, phosphoric, carbonic, sulphuric, and organic acids like acetic, propionic, benzoic, succinic, fumaric, mandelic, oxalic, citric, tartaric, maleic, and the like.
- Pharmaceutically-acceptable base addition salts include sodium, potassium, calcium, ammonium, and magnesium salts.
- Pharmaceutically- acceptable salts of the peptides of the invention can be prepared using conventional techniques.
- the subject invention also concerns polynucleotide expression constructs that comprise a polynucleotide of the present invention comprising a nucleotide sequence encoding a peptide of the present invention.
- the polynucleotide encodes a peptide comprising the amino acid sequence shown in SEQ ID NO:1, or a fragment or variant thereof that exhibits antiviral activity.
- operably linked refers to a juxtaposition of the components described wherein the components are in a relationship that permits them to function in their intended manner. In general, operably linked components are in contiguous relation.
- Expression constructs of the invention will also generally include regulatory elements that are functional in the intended host cell in which the expression construct is to be expressed.
- regulatory elements include promoters, transcription termination sequences, translation termination sequences, enhancers, and polyadenylation elements.
- An expression construct of the invention can comprise a promoter sequence operably linked to a polynucleotide sequence encoding a peptide of the invention. Promoters can be incorporated into a polynucleotide using standard techniques known in the art. Multiple copies of promoters or multiple promoters can be used in an expression construct of the invention. In a preferred embodiment, a promoter can be positioned about the same distance from the transcription start site as it is from the transcription start site in its natural genetic environment. Some variation in this distance is permitted without substantial decrease in promoter activity. A transcription start site is typically included in the expression construct. For expression in animal cells, an expression construct of the invention can comprise suitable promoters that can drive transcription of the polynucleotide sequence.
- promoters such as, for example, actin promoter, metallothionein promoter, NF-kappaB promoter, EGR promoter, SRE promoter, IL-2 promoter, NFAT promoter, osteocalcin promoter, SV40 early promoter and SV40 late promoter, Lck promoter, BMP 5 promoter, TRP-I promoter, murine mammary tumor virus long terminal repeat promoter, STAT promoter, or an immunoglobulin promoter can be used in the expression construct.
- the baculovirus polyhedrin promoter can be used with an expression construct of the invention for expression in insect cells.
- Promoters suitable for use with an expression construct of the invention in yeast cells include, but are not limited to, 3-phosphoglycerate kinase promoter, glyceraldehyde-3- phosphate dehydrogenase promoter, metallothionein promoter, alcohol dehydrogenase-2 promoter, and hexokinase promoter.
- an expression construct of the invention can comprise promoters such as, for example, alkaline phosphatase promoter, tryptophan (trp) promoter, lambda P L promoter, ⁇ -lactamase promoter, lactose promoter, phoA promoter, T3 promoter, T7 promoter, or tac promoter (de Boer et al, 1983).
- promoters such as, for example, the cauliflower mosaic virus (CaMV) 35S (including the enhanced CaMV 35S promoter (see, for example U.S. Patent No. 5,106,739)) or 19S promoter can be used.
- Plant promoters such as prolifera promoter, Ap3 promoter, heat shock promoters, T-DNA 1 '- or 2'-promoter of A. tumafaciens, polygalacturonase promoter, chalcone synthase A (CHS-A) promoter from petunia, tobacco PR- Ia promoter, ubiquitin promoter, actin promoter, alcA gene promoter, pin2 promoter (Xu et al., 1993), maize Wipl promoter, maize trpA gene promoter (U.S. Patent No. 5,625,136), maize CDPK gene promoter, and RUBISCO SSU promoter (U.S. Patent No. 5,034,322) can also be used.
- Seed-specific promoters such as the promoter from a ⁇ -phaseolin gene (of kidney bean) or a glycinin gene (of soybean), and others, can also be used.
- Constitutive promoters such as the CaMV, ubiquitin, actin, or NOS promoter
- tissue-specific promoters such as the E8 promoter from tomato
- developmentally-regulated promoters such as those promoters than can be induced by heat, light, hormones, or chemicals
- inducible promoters such as those promoters than can be induced by heat, light, hormones, or chemicals
- Expression constructs of the invention may optionally contain a transcription termination sequence, a translation termination sequence, signal peptide sequence, and/or enhancer elements.
- Transcription termination regions can typically be obtained from the 3' untranslated region of a eukaryotic or viral gene sequence. Transcription termination sequences can be positioned downstream of a coding sequence to provide for efficient termination.
- Signal peptides are a group of short amino terminal sequences that encode information responsible for the relocation of an operably linked peptide to a wide range of post-translational cellular destinations, ranging from a specific organelle compartment to sites of protein action and the extracellular environment.
- Chemical enhancers are cis-acting elements that increase gene transcription and can also be included in the expression construct. Chemical enhancer elements are known in the art, and include, but are not limited to, the CaMV 35S enhancer element, cytomegalovirus (CMV) early promoter enhancer element, and the SV40 enhancer element. DNA sequences which direct polyadenylation of the mRNA encoded by the structural gene can also be included in the expression construct.
- CMV cytomegalovirus
- Vectors refers to any genetic element, including for example, plasmids, cosmids, chromosomes, phage, virus, and the like, which is capable of replication when associated with proper control elements and which can transfer polynucleotide sequences between cells.
- Vectors contain a nucleotide sequence that permits the vector to replicate in a selected host cell.
- a number of vectors arc available for expression and/or cloning, and include, but are not limited to, pBR322, pUC series, Ml 3 series, and pBLUESCRIPT vectors (Stratagene, La Jolla, CA).
- Polynucleotides, vectors, and expression constructs of the subject invention can be introduced into a cell by methods known in the art. Such methods include transfection, microinjection, electroporation, lipofection, cell fusion, calcium phosphate precipitation, and by biolistic methods.
- a polynucleotide or expression construct of the invention can be introduced in vivo via a viral vector such as adeno-associated virus (AAV), herpes simplex virus (HSV), papillomavirus, adenovirus, and Epstein-Barr virus (EBV).
- AAV adeno-associated virus
- HSV herpes simplex virus
- papillomavirus adenovirus
- EBV Epstein-Barr virus
- Attenuated or defective forms of viral vectors that can be used with the subject invention are known in the art. Typically, defective virus is not capable of infection after the virus is introduced into a cell.
- Polynucleotides, vectors, and expression constructs of the invention can also be introduced in vivo via lipofection (DNA transfection via liposomes prepared from synthetic cationic lipids) (Feigner et al., 1987).
- Synthetic cationic lipids can be used to prepare liposomes to encapsulate a polynucleotide, vector, or expression construct of the invention.
- a polynucleotide, vector, or expression construct of the invention can also be introduced in vivo as naked DNA using methods known in the art, such as transfection, microinjection, electroporation, calcium phosphate precipitation, and by biolistic methods.
- Polynucleotides and peptides of the subject invention can also be defined in te ⁇ ns of more particular identity and/or similarity ranges with those exemplified herein.
- sequence identity will typically be greater than 60%, preferably greater than 75%, more preferably greater than 80%, even more preferably greater than 90%, and can be greater than 95%.
- the identity and/or similarity of a sequence can be 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81 , 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, or 99% as compared to a sequence exemplified herein.
- the subject invention also contemplates those polynucleotide molecules (encoding peptides of the invention) having sequences which are sufficiently homologous with the polynucleotide sequences encoding a peptide of the invention so as to permit hybridization with that sequence under standard stringent conditions and standard methods (Maniatis, T. et al, 1982).
- stringent conditions for hybridization refers to conditions wherein hybridization is typically carried out overnight at 20-25 C below the melting temperature (Tm) of the DNA hybrid in 6x SSPE, 5x Denhardt's solution, 0.1% SDS, 0.1 mg/ml denatured DNA.
- Tm melting temperature
- Tm 81.5 C+16.6 Log[Na+]-0.41(%G+C)-0.61(% formamide)-600/length of duplex in base pairs. Washes are typically carried out as follows:
- nucleic acid and “polynucleotide sequence'" refer to a deoxyribonucleotide or ribonucleotide polymer in either single- or double-stranded form, and unless otherwise limited, would encompass known analogs of natural nucleotides that can function in a similar manner as naturally-occurring nucleotides.
- the polynucleotide sequences include both the DNA strand sequence that is transcribed into RNA and the RNA sequence that is translated into protein.
- the polynucleotide sequences include both full-length sequences as well as shorter sequences derived from the full-length sequences.
- polynucleotide sequence includes the degenerate codons of the native sequence or sequences which may be introduced to provide codon preference in a specific host cell.
- the polynucleotide sequences falling within the scope of the subject invention further include sequences which specifically hybridize with the sequences coding for a peptide of the invention.
- the polynucleotide includes both the sense and antisense strands as either individual strands or in the duplex.
- the subject invention also concerns methods for preventing or treating a viral infection in a patient wherein the viral infection is associated with the expression of a SOCS protein, such as SOCS-I and/or SOCS-3.
- a SOCS protein such as SOCS-I and/or SOCS-3.
- an effective amount of a peptide, polynucleotide, peptidomimetic, and/or composition of the present invention is administered to a patient having a viral disorder and who is in need of treatment thereof.
- the peptide comprises the amino acid sequence: 1001 LPQDKEYYKVKEP 1013 (pJAK2 (1001-1013)) (SEQ ID NO:1), or a fragment or variant thereof that exhibits antiviral activity.
- the tyrosine at amino acid position 7 of SEQ ID NO: 1 i.e., the tyrosine that is underlined in the sequence LPQDKEYYKVKEP
- a peptide of the invention consists of the amino acid sequence shown in SEQ ID NO:1, and optionally wherein the tyrosine at position 7 is phosphorylated.
- the patient can be a human or other mammal, such as a dog, cat, or horse, or other animals having the disorder.
- peptides, polynucleotides, and peptidomimetics for administration to a patient are known in the art, examples of which are described herein.
- Peptides, polynucleotides, peptidomimetics, and/or compositions of the invention can be delivered to a cell either through direct contact of peptide, etc. with the cell or via a earner means.
- a peptide, etc. of the invention comprises an attached group that enhances cellular uptake of the peptide.
- the peptide, etc. is attached to an antibody that binds to a targeted cell.
- the peptide, etc. is encapsulated in a liposome.
- Peptides can also be delivered using a polynucleotide that encodes a subject peptide. Any polynucleotide having a nucleotide sequence that encodes a peptide of the invention is contemplated within the scope of the invention. In one embodiment, the polynucleotide is delivered to the cell where it is taken up and the polynucleotide is transcribed into RNA and the RNA is translated into the encoded peptide.
- viruses whose replication can be inhibited using the present invention include, but are not limited to, herpes viruses, poxviruses, and picomaviruses, such as vaccinia virus, EMC vims, influenza virus, herpes zoster virus, cytomegalovirus, and herpes simplex virus (e.g., HSV-I).
- herpes viruses poxviruses, and picomaviruses, such as vaccinia virus, EMC vims, influenza virus, herpes zoster virus, cytomegalovirus, and herpes simplex virus (e.g., HSV-I).
- the peptides, polynucleotides, peptidomimetics and compositions of this invention can be administered to a patient in need of treatment in combination with other antiviral substances.
- these other antiviral substances may be given at the same or different times as the peptides, polynucleotides, peptidomimetics, and compositions of this invention.
- the peptides, polynucleotides, peptidomimetics, and compositions of the present invention can be used in combination with one or more viral inhibitors such as interferons, and/or other drugs or antibodies, such as IFN ⁇ , IFN ⁇ , IFN ⁇ , acyclovir (Zovirax), zidovudine (AZT), lamivudine (3TC), zanamivir (Relenza), oseltamivir (Tamiflu), valacyclovir (Valtrex), amantadine (Symmetrel), rimantadine (Flumadine), cidofovir (Vistide), foscarnet (Foscavir), ganciclovir (Cytovene), ribavirin (Virazole), nelfmavir (Viracept), ritonavir (Norvir), rifampin (Rifadin), and famciclovir (Famvir), or drug or antibody that inhibit
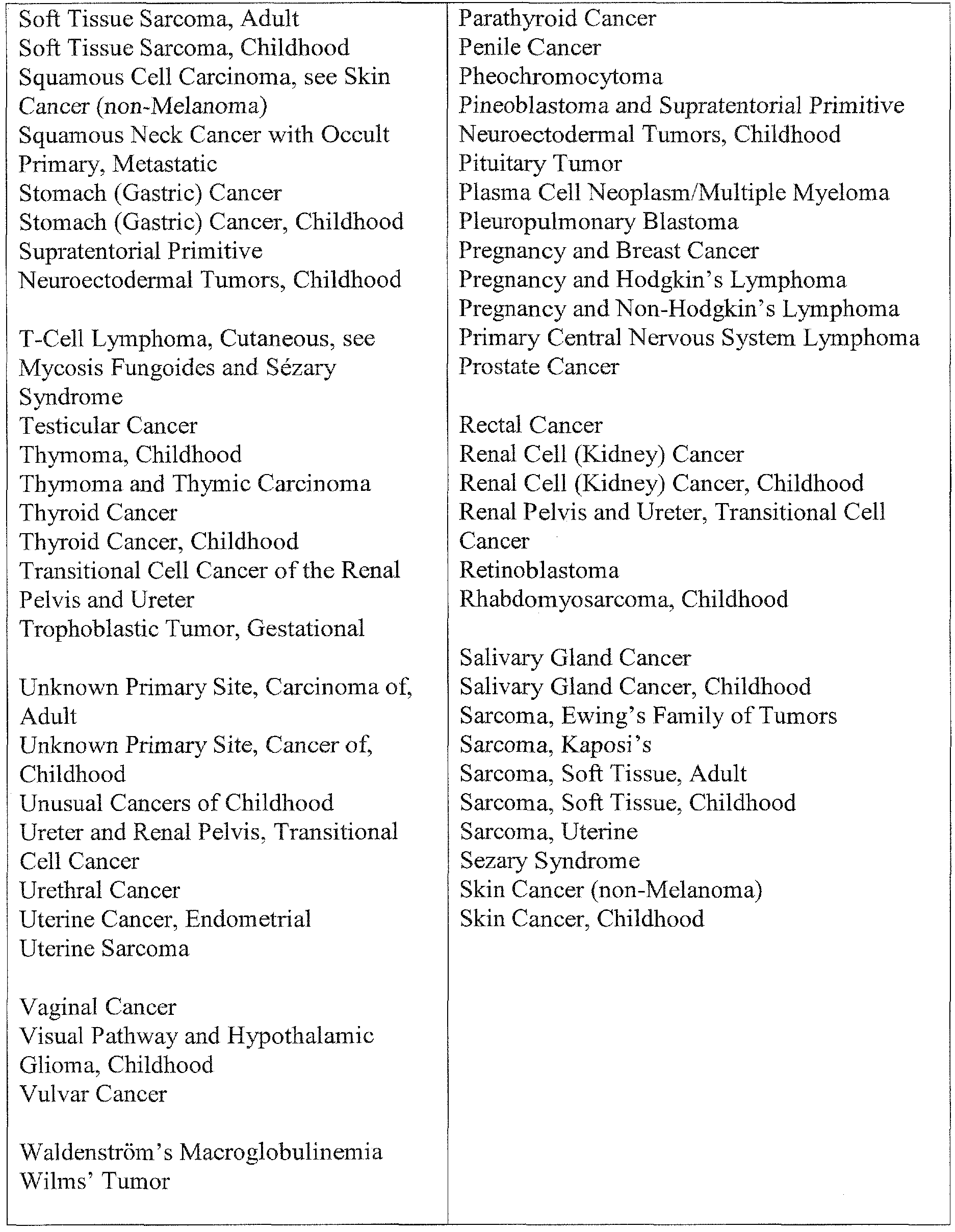
- the subject invention also concerns methods for treating oncological disorders in a patient, wherein the oncological disorder is associated with or characterized by expression of a SOCS protein, such as SOCS-I and/or SOCS-3.
- a SOCS protein such as SOCS-I and/or SOCS-3.
- an effective amount of a peptide, polynucleotide, peptidomimetic, or composition of the present invention that is an antagonist of a SOCS protein is administered to a patient having an oncological disorder and who is in need of treatment thereof.
- the peptide comprises the amino acid sequence: 1001 LPQDKEYYKVKEP 1013 (pJAK2 (1001 -1013)) (SEQ ID NO:1), or a fragment or variant thereof that exhibits anticancer activity.
- the tyrosine at amino acid position 7 of SEQ ID NO:1 i.e., the tyrosine that is underlined in the sequence LPQDKEYYKVKEP
- a peptide of the invention consists of the amino acid sequence shown in SEQ ID NO:1, and optionally wherein the tyrosine at position 1007 is phosphorylated.
- Methods of the invention can optionally include identifying a patient who is or may be in need of treatment of an oncological disorder.
- the patient can be a human or other mammal, such as a primate (monkey, chimpanzee, ape, etc.), dog, cat, cow, pig, or horse, or other animals having an oncological disorder.
- a primate monkey, chimpanzee, ape, etc.
- dog cat, cow, pig, or horse
- oncological disorder e.g., a human or other mammal
- Means for administering and formulating peptides, polynucleotides, peptidomimetics, or compositions of the invention for administration to a patient are known in the art, examples of which are described herein.
- Oncological disorders within the scope of the invention include, but are not limited to, cancer and/or tumors of the anus, bile duct, bladder, bone, bone marrow, bowel (including colon and rectum), breast, eye, gall bladder, kidney, mouth, larynx, esophagus, stomach, testis, cervix, head, neck, ovary, lung, mesothelioma, neuroendocrine, penis, skin, spinal cord, thyroid, vagina, vulva, uterus, liver, muscle, pancreas, prostate, blood cells (including lymphocytes and other immune system cells), and brain.
- cancer and/or tumors of the anus include, but are not limited to, cancer and/or tumors of the anus, bile duct, bladder, bone, bone marrow, bowel (including colon and rectum), breast, eye, gall bladder, kidney, mouth, larynx, esophagus, stomach, testis, cervix, head, neck, ova
- Specific cancers contemplated for treatment with the present invention include carcinomas, Karposi's sarcoma, melanoma, mesothelioma, soft tissue sarcoma, pancreatic cancer, lung cancer, leukemia (acute lymphoblastic, acute myeloid, chronic lymphocytic, chronic myeloid, and other), and lymphoma (Hodgkin's and non-Hodgkin's), and multiple myeloma.
- Carcinoid Tumor Childhood Lymphoma, Non-Hodgkin's During Carcinoid Tumor, Gastrointestinal Pregnancy Carcinoma of Unknown Primary Central Nervous System Lymphoma, Lymphoma, Primary Central Nervous System
- Endometrial Cancer Mycosis Fungoides Ependymoma, Childhood Myelodysplastic Syndromes Esophageal Cancer Myelodysplastic/Myeloproliferative Diseases Esophageal Cancer, Childhood Myelogenous Leukemia, Chronic Ewing's Family of Tumors Myeloid Leukemia, Adult Acute Extracranial Germ Cell Tumor, Myeloid Leukemia, Childhood Acute Childhood Myeloma, Multiple
- the peptides, polynucleotides, peptidomimetics, and compositions of this invention can be administered to a patient in need of treatment in combination with other antitumor or anticancer substances and/or with radiation and/or photodynamic therapy and/or with surgical treatment to remove a tumor.
- these other substances or treatments may be given at the same as or at different times from the peptides, polynucleotides, peptidomimetics, and compositions of this invention.
- the peptides, polynucleotides, peptidomimetics, and compositions of the present invention can be used in combination with mitotic inhibitors such as taxol or vinblastine, alkylating agents such as cyclophosamide or ifosfamide, antimetabolites such as 5 ⁇ fluorouracil or hydroxyurea, DNA intercalators such as adriamycin or bleomycin, topoisomerase inhibitors such as etoposide or camptothecin, antiangiogenic agents such as angiostatin, antiestrogens such as tamoxifen, and/or other anti-cancer drugs or antibodies, such as, for example, GLEEVEC (Novartis Pharmaceuticals Corporation) and HERCEPTIN (Genentech, Inc.), respectively.
- mitotic inhibitors such as taxol or vinblastine
- alkylating agents such as cyclophosamide or ifosfamide
- antimetabolites such as 5 ⁇ fluorouracil or hydroxyure
- Peptides, polynucleotides, peptidomimetics, and compositions of the invention can be used in combination with proteasome inhibitors, including, but not limited to, Bortezomib, Carfilzomib, and Salinosporamide A.
- proteasome inhibitors including, but not limited to, Bortezomib, Carfilzomib, and Salinosporamide A.
- Many tumors and cancers have viral genome present in the tumor or cancer cells.
- Epstein-Barr Virus is associated with a number of mammalian malignancies.
- the peptides, polynucleotides, peptidomimetics, and compositions of the subject invention can also be used alone or in combination with anticancer or antiviral agents, such as ganciclovir, azidothymidine (AZT), lamivudine (3TC), etc., to treat patients infected with a virus that can cause cellular transformation and/or to treat patients having a tumor or cancer that is associated with the presence of viral genome in the cells.
- anticancer or antiviral agents such as ganciclovir, azidothymidine (AZT), lamivudine (3TC), etc.
- the methods of the present invention can be used with humans and other animals.
- the other animals contemplated within the scope of the invention include domesticated, agricultural, or zoo- or circus-maintained animals.
- domesticated animals include, for example, dogs, cats, rabbits, ferrets, guinea pigs, hamsters, pigs, monkeys or other primates, and gerbils.
- Agricultural animals include, for example, horses, mules, donkeys, burros, cattle, cows, pigs, sheep, and alligators.
- Zoo- or circus-maintained animals include, for example, lions, tigers, bears, camels, giraffes, hippopotamuses, and rhinoceroses.
- one or more of the peptides of the subject invention can be provided in the form of a multiple peptide construct.
- a multiple peptide construct can be designed so that multiple peptides are linked to each other by intervening moieties wherein the intervening moieties are subsequently cleaved or removed following administration of the multiple peptide construct to a patient.
- Methods for constructing multiple peptide constructs are known in the art.
- peptides of the present invention can be provided in the form of a multiple antigenic peptide (MAP) construct.
- MAP constructs utilize a core matrix of lysine residues onto which multiple copies of an immunogen are synthesized.
- MAP constructs each containing different peptides, can be prepared and administered in accordance with methods of the present invention.
- a multiple peptide construct can be prepared by preparing the subject peptides having at least one metal chelating amino acid incorporated therein, preferably at the amino and/or carboxy terminal of the peptide as described, for example, in U.S. Patent No. 5,763,585. The peptides are then contacted with a solid support having attached thereto a metal ion specific for the metal chelating amino acid of the peptide.
- a multiple peptide construct of the invention can provide multiple copies of the exact same peptide, including variants or fragments of a subject peptide, or copies of different peptides of the subject invention.
- Therapeutic application of the subject peptides, polynucleotides, and peptidomimetics, and compositions containing them can be accomplished by any suitable therapeutic method and technique presently or prospectively known to those skilled in the art.
- the peptides, polynucleotides, and peptidomimetics can be administered by any suitable route known in the art including, for example, oral, nasal, rectal, parenteral, subcutaneous, or intravenous routes of administration.
- Administration of the peptides, polynucleotides, and peptidomimetics of the invention can be continuous or at distinct intervals as can be readily determined by a person skilled in the art.
- compositions useful in the subject invention can be formulated according to known methods for preparing pharmaceutically useful compositions. Formulations are described in detail in a number of sources which are well known and readily available to those skilled in the art. For example, Remington 's Pharmaceutical Science by E. W. Martin describes formulations which can be used in connection with the subject invention. In general, the compositions of the subject invention will be formulated such that an effective amount of the bioactive peptide, polynucleotide, or peptidomimetic is combined with a suitable carrier in order to facilitate effective administration of the composition. The compositions used in the present methods can also be in a variety of forms.
- compositions include, for example, solid, semi-solid, and liquid dosage forms, such as tablets, pills, powders, liquid solutions or suspension, suppositories, injectable and infusible solutions, and sprays.
- solid dosage forms such as tablets, pills, powders, liquid solutions or suspension, suppositories, injectable and infusible solutions, and sprays.
- the preferred form depends on the intended mode of administration and therapeutic application.
- the compositions also preferably include conventional pharmaceutically acceptable carriers and diluents which are known to those skilled in the art.
- Examples of carriers or diluents for use with the subject peptides, polynucleotides, and peptidomimetics include, but are not limited to, water, saline, oils including mineral oil, ethanol, dimethyl sulfoxide, gelatin, cyclodextrans, magnesium stearate, dextrose, cellulose, sugars, calcium carbonate, glycerol, alumina, starch, and equivalent carriers and diluents, or mixtures of any of these.
- Formulations of the peptide, polynucleotide, or peptidomimetic of the invention can also comprise suspension agents, protectants, lubricants, buffers, preservatives, and stabilizers.
- compositions of the invention will advantageously comprise between about 0.1% and 45%, and especially, 1 and 15% by weight of the total of one or more of the peptide, polynucleotide, or peptidomimetic based on the weight of the total composition including carrier or diluent.
- peptides, polynucleotides, peptidomimetics, and compositions of the subject invention can also be administered utilizing liposome technology, slow release capsules, implantable pumps, and biodegradable containers. These delivery methods can, advantageously, provide a uniform dosage over an extended period of time.
- the subject peptides, polynucleotides, and peptidomimetics can also be modified by the addition of chemical groups, such as PEG (polyethylene glycol).
- PEG polyethylene glycol
- PEGylated peptides typically generate less of an immunogenic response and exhibit extended half- lives in vivo in comparison to peptides that are not PEGylated when administered in vivo.
- Methods for PEGylating proteins and peptides known in the art see, for example, U.S. Patent No. 4,179,337).
- the subject peptides, polynucleotides, and peptidomimetics can also be modified to improve cell membrane permeability.
- cell membrane permeability can be improved by attaching a lipophilic moiety, such as a steroid, to the peptide, polynucleotide, or peptidomimetic.
- a lipophilic moiety such as a steroid
- Other groups known in the art can be linked to peptides, polynucleotides, and peptidomimetics of the present invention.
- the subject invention also concerns a packaged dosage formulation comprising in one or more containers at least one peptide, polynucleotide, peplidomimetic, and/or composition of the subject invention formulated in a pharmaceutically acceptable dosage.
- the package can contain discrete quantities of the dosage formulation, such as tablet. capsules, lozenge, and powders.
- the quantity of peptide, polynucleotide, and/or peptidomimetic in a dosage formulation and that can be administered to a patient can vary from about 1 mg to about 5000 mg, or about 1 mg to about 2000 mg, or more typically about 1 mg to about 500 mg, or about 5 mg to about 250 mg, or about 10 mg to about 100 mg.
- the subject invention also concerns kits comprising one or more peptides, polynucleotides, peptidomimetics, compositions, compounds, or molecules of the present invention in one or more containers.
- a kit contains a peptide, polynucleotide, peptidomimetic, and/or composition of the present invention.
- a kit comprises a peptide comprising the amino acid sequence shown in SEQ ID NO:1, or a fragment or variant of the peptide that exhibits antiviral activity.
- the tyrosine at position 7 of SEQ ID NO:1 (Le , the tyrosine that is underlined in the sequence LP QDKE Y YKVKEP) is phosphorylated.
- a kit comprises a peptide consisting of the amino acid sequence shown in SEQ ID NO:1, and optionally wherein the tyrosine at position 7 is phosphorylated.
- kits of the invention can also comprise one or more antiviral compounds, biological molecules, or drugs and/or one or more IFN ⁇ peptide mimetics.
- the biological molecule is one or more of IFN ⁇ , IFN ⁇ , or IFN ⁇ .
- a kit comprises one or more peptides of SEQ ID NO:67 and/or SEQ ID NO:75, or a fragment or variant thereof that exhibits antiviral activity.
- a kit can also comprise one or more peptides comprising the amino acid sequence shown in SEQ ID NO:61 (Tkip peptide), or a fragment or variant thereof that exhibits antiviral activity, and/or a peptide comprising the amino acid sequence shown in SEQ IDNO:63, or a fragment or variant thereof that exhibits antiviral activity.
- a kit comprises one or more of IFN ⁇ , IFN ⁇ , IFN ⁇ , acyclovir (Zovirax), zidovudine (AZT), lamivudine (3TC), zanamivir (Relenza), oseltamivir (Tamiflu), valacyclovir (Valtrex), amantadine (Symmetrel), rimantadine (Flumadine), cidofovir (Vistide), foscarnet (Foscavir), ganciclovir (Cytovene), ribavirin (Virazole), nelfinavir (Viracept), ritonavir (Norvir), rifampin (Rifadin), and famciclovir (Famvir).
- a kit comprises one or more of mitotic inhibitors such as taxol or vinblastine, alkylating agents such as cyclophosarnide or ifosfamide, antimetabolites such as 5 -fluoro uracil or hydroxyurea, DNA intercalators such as adriamycin or bleomycin, topoisomerase inhibitors such as etoposide or camptothecin, antiangiogenic agents such as angiostatin, antiestrogens such as tamoxifen, and/or other anti-cancer drugs or antibodies, such as, for example, GLEEVEC (Novartis Pharmaceuticals Corporation) and HERCEPTIN (Genentech, Inc.), respectively.
- mitotic inhibitors such as taxol or vinblastine
- alkylating agents such as cyclophosarnide or ifosfamide
- antimetabolites such as 5 -fluoro uracil or hydroxyurea
- DNA intercalators such as adriamycin or
- a kit of the invention includes instructions or packaging materials that describe how to administer a compound or composition of the kit.
- Containers of the kit can be of any suitable material, e.g., glass, plastic, metal, etc., and of any suitable size, shape, or configuration.
- a compound and/or agent of the invention is provided in the kit as a solid, such as a tablet, pill, or powder form.
- a compound and/or agent of the invention is provided in the kit as a liquid or solution.
- the kit comprises an ampoule or syringe containing a compound and/or agent of the invention in liquid or solution form.
- HEL-30 keratinocytes (Dr. D. Germolec, NIEHS, Durham, NC), L929 fibroblasts (CCL-I, ATCC, Manassas, VA), and Vero cells (CCL-
- HSV-I ICPO mutant designated as dll403 (Stow and Stow, 1986), was obtained from Dr. Rick Thompson (Univ Cincinnati, Cincinnati, OH), and was grown and titrated in U2OS cells (HTB-96, ATCC).
- U2OS cell were grown in McCoy's 5A medium with
- Mouse macrophage cell line RAW 264.7 was grown in RPMl with 10% FBS.
- Peptides The amino acid sequences for the peptide mimetics used in this study shown in Table 4. The peptides were synthesized on an Applied Biosystems 9050 automated peptide synthesizer using conventional fhiorenylmethyloxycarbonyl chemistry as previously described (Szente et ai, 1996). The addition of a lipophilic group (palmitoyllysine) to the N terminus of the synthetic peptide was performed as a last step, using semiautomated protocol (Thiam et ah, 1999). Peptides were characterized by mass spectrometry and were purified by HPLC. All peptides were dissolved in DMSO at a concentration of 10 mg/mL. Peptides were diluted in cell culture medium prior to addition to cells.
- L929 fibroblasts or HEL-30 keratinocytes were cultured and counted in a hemacytometer, added at densities of 2.0 x 10 4 to 3.0 x 10 4 to each well of a multiwell cell culture plate and incubated overnight. The following day, recombinant murine interferon gamma (IFN- ⁇ ) (Peprotech, Rocky Hill, NJ), IFN- ⁇ peptide mimetics, SOCS-I mimetic peptide, SOCS-I antagonist peptide, or IFN ⁇ mimetic peptide were added to the cultures at the indicated concentrations and incubated for 24 hours.
- IFN- ⁇ murine interferon gamma
- culture medium was aspirated, cells were rinsed with PBS and HSV-I added at an MOI of 0.1. Two days post-infection, medium was aspirated, cells were washed twice with Ix HBSS and fixed by addition of 10% formalin. Fixative was removed and cell layers were stained with crystal violet. Plates were rinsed with dH 2 O and dried overnight. Plates were scanned on an HP ScanJet 5300C or photographed using a Fuji LAS-300 CCD camera. Densitometry measurements of each well were computed using Multi-gauge software (FujiFilm USA, Burbank, CA) or NIH Im age- J. HSV-I infection of Monolayer Cultures.
- Cells were seeded into 35 mm culture dishes at a density of 1 x 10 4 cells/cm 2 and allowed to grow to -75% confluence. Culture medium was aspirated and monolayers washed with Ix PBS. HSV-I diluted in minimum essential medium (MEM) containing 2% calf serum (CS) was added to the culture medium at the indicated MOI and the cell cultures incubated for 2 hours at 37 0 C. Medium was removed and replaced with MEM containing 10% CS.
- MEM minimum essential medium
- CS 2% calf serum
- RNA isolation and Quantitation RNA was collected from cells at specified times after infection. Total RNA was isolated by using RNeasy mini kits (Qiagen Inc., Valencia, CA) according to the manufacturers' instructions. Samples were eluted 2x in a volume of 20 ⁇ L. RNA concentration was determined by measuring absorbance at 260 and 280 nm and purity calculated using ratios of absorbance at 260 and 280 nm (260/280). RNA integrity was checked by formaldehyde agarose gel electrophoresis. Briefly, each sample was added to one well of a 1.2% formaldehyde/agarose gel with ethidium bromide and electrophoresed at 5 V/cm. Bands were visualized with UV light and documented by capture with a CCD camera (Fujifilm USA, Burbank, CA).
- RT-PCR RT-PCR. Briefly, 2 ⁇ g of total RNA from each experimental sample was used in a reverse transcriptase (RT) reaction. Reaction conditions were: Ix RT buffer, 0.5 mM dNTP, 1 ⁇ M oligo-dT primer, 10 U/ ⁇ L RNase inhibitor, and 4 U/ ⁇ L RT enzyme in a total reaction volume of 20 ⁇ L. Each sample was incubated at 37° C for 1 hour. Each completed RT reaction mix was added to a PCR master mix. The resulting PCR cocktail was aliquoted (25 ⁇ L) into PCR tubes containing appropriate primers for the gene of interest.
- RT reverse transcriptase
- PCR was performed with 30 cycles of the following program: 30 sec at 95° C, 30 sec at 55° C, and 30 sec at 70° C. Following the completion of PCR, 10 ⁇ L of each sample was electrophoresed through a 2% agarose gel at 5 V/cm. Images were captured using a Fuji CCD camera. Data was normalized to expression of a housekeeping gene (GAPDH) and expressed as percent of control.
- GAPDH housekeeping gene
- HEL-30 keratinocytes or L929 fibroblasts were plated into cell culture plates and allowed to grow overnight. Cells were infected with HSV-I as described above. The virus was removed and fresh DMEM containing 10% BCS added. At the indicated time points, medium was removed and cells were rinsed 3x with PBS. Cells were then lysed with Complete Lysis Buffer M (Roche Diagnostics, Indianapolis, IN) by following manufacturer's suggestions. Equal amounts of lysate were combined with 6x Laemelli buffer and resolved by SDS-PAGE. Proteins were electro-blotted overnight onto PVDF. Membranes were blocked for one hour with 5% non-fat milk/TBS-Tween.
- Membranes were incubated with primary antibody to SOCS-I (Millipore, Temecula, CA), STAT-I, or p-STAT-1 (Santa Cruz Biotech, Santa Cruz, CA). Membranes were rinsed 3x with TBS-Tween and then incubated with secondary antibody. Proteins bands were resolved by chemiluminescence. Images were captured as before using a Fuji CCD camera.
- the PCR fragment was purified and digested with Nhe 1 and Hind III and ligated with pGL3 basic reporter plasmid (Promega, Madison, WI) expressing firefly luciferase, digested with similar enzymes.
- the sequence of the reporter plasmid thus generated, which contained nucleotides -1577 to -3 of the promoter was confirmed by DNA sequencing.
- Luciferase Assay HEL-30 cells were plated into 12-well cell culture dishes and allowed to grow overnight. Cells were co-transfected with the plasmids expressing SOCS-I promoter linked firefly luciferase and a constitutively expressed Renilla luciferase using GeneJammer (Stratagene, La Jolla, CA) transfection reagent for HEL-30 cells or Metafectene (Biontex Laboratories GmBh, Martinsreid, Germany) for L929 cells. Relative luciferase units were measured by using a dual luciferase assay kit form Promega (Madison, WI).
- HEL-30 cells or L929 cells were plated into 12-well cell culture dishes and allowed to grow overnight. Cells were transfected with a construct containing the full-length murine SOCS-I gene, pFL AG-SOCS-I (a kind gift of Dr. Douglas Hilton, Walter and Eliza Hall Institute, Victoria, Australia). Briefly, L929 cells at ⁇ 90% confluence were transfected with indicated amounts of pFLAG-SOCS-1 using Metafectene Pro (Biontex Laboratories GmbH, Martinsreid, Germany). Twenty-four hours later, cells were lysed and extracts used for Western blotting to confirm expression of the SOCS-I protein.
- pFL AG-SOCS-I a kind gift of Dr. Douglas Hilton, Walter and Eliza Hall Institute, Victoria, Australia.
- Example 1 ⁇ FN ⁇ induces an antiviral state against HSV-I in fibroblasts but not keratinocytes
- Keratinocytes are important for HSV-I replication in the epidermis, which plays a role in infection of nervous tissue (Roizman et al., 2007). We were therefore interested in determining the ability of IFN ⁇ to inhibit HSV-I replication in HEL-30 keratinocytes relative to L929 fibroblasts ( Figure 1). IFN ⁇ at concentrations of 12.5 to 50 U/ml protected fibroblasts infected with HSV-I at an moi of 0.1 ( Figure IA), while HEL-30 keratinocytes were susceptible to HSV-I -mediated lysis (CPE) in the presence of IFN ⁇ ( Figure IB).
- CPE HSV-I -mediated lysis
- HEL-30 keratinocytes were lysed in the presence of IFN ⁇ , while the fibroblasts were protected.
- a small peptide mimetic of mouse IFN ⁇ that consists of the C-terminus of IFN ⁇ with an attached palmitate for plasma membrane penetration (Table 4) (Szente et al., 1996) was used.
- the mimetic contains an essential alpha helix and polycationic nuclear localization sequence. It binds to the cytoplasmic domain of the lFN ⁇ receptor subunit, IFNGRl, and participates in activation of STATI a and transport of a complex of STATI a and IFNGRl to the GAS promoter element in genes specifically activated by IFN ⁇ (Ahmed and Johnson, 2006).
- IFN ⁇ mimetic showed similar but slightly less HSV-I inhibition patterns to IFN ⁇ in keratinocytes versus fibroblasts.
- Example 2 HSV-I infection induces SQCS-I expression in HEL-30 keratinocytes but not in L929 fibroblasts
- HSV-I infected HEL-30 fibroblasts showed increased levels by Western blots up to 6 hours post-infection as shown in Figure 2B.
- Figure 2C RT-PCR analysis of SOCS-I mRNA over time showed that similar levels were observed from 1 to 6 hours post-infection with HSV-I ( Figure 2D).
- Figure 2D the level of SOCS-I gene activation was similar at 1 and 2 moi and enhanced at 5 moi (data not shown).
- HSV-I differentially induced the activation of SOCS-I as per RT-PCR and Western blot analysis of HEL-30 and L929 cells, which is consistent with the ability of IFN ⁇ to inhibit HSV-I induced CPE in L929 fibroblasts but not in HEL-30 keratinocytes.
- Example 3 IFN ⁇ activation of STATIa is inhibited in HEL-30 keratinocvtes infected with HSV-I
- Example 5 A peptide antagonist of SOCS-I synergizes with IFN ⁇ to induce an antiviral state against HSV-I in HEL-30 keratinocvtes
- HEL-30 cells infected with HSV-I were minimally protected by 100 U/ml of lFN ⁇ alone.
- pJAK2(1001-1013) at 35 ⁇ M showed approximately 40 percent protection, while 17 and 8 ⁇ M were not protective.
- Combined treatment of infected cells with 100 U/ml of IFN ⁇ and 35 ⁇ M of pJAK2(1001-1013) resulted in 100 percent protection against HSV-I.
- This protection was concentration- dependent as 17 and 8 ⁇ M of pJAK2(1001-1013) and 100 U/ml IFN ⁇ resulted in approximately 70 and 25 percent protection, respectively.
- the IFN ⁇ mimetic also synergized with the SOCS-I antagonist (data not shown).
- HEL-30 cells were transfected with SOCS-I siRNA and determined the relative protection against HSV-I in the presence and absence of 400 U/ml of IFN ⁇ .
- siRNA alone provided similar protection to that observed in combination with IFN ⁇ .
- a control siRNA by comparison was relatively non-protective.
- the pJAK2(1001-1013) protection is supported by similar protection with SOCS-I siRNA transfected HEL-30 cells infected with HSV-I.
- Tkip tyrosine kinase inhibitor peptide
- L929 cells were treated with 100 U/ml of IFN ⁇ and 20 ⁇ M of either Tkip or Tkip2A peptide to determine the effect on HSV-I infection.
- Tkip but not Tki ⁇ 2A significantly inhibited the ability of IFN ⁇ to induce an antiviral state.
- the SOCS-I mimetic Tkip had a similar effect on IFN ⁇ treated L929 fibroblasts as did transfection with SOCS-I .
- Example 7 Reduction in SOCS-I gene activation by HSV-I ICPO mutant in HEL-30 keratinocytes
- ICPO is an IE virulence protein that increases expression of HSV-I genes in infected cells (Poon et al, 2006; Gu and Roizman, 2009; Cliffe and Knipe, 2008).
- One way that it functions is by blockage of histone deacetylation and/or increase in histone accetylation to facilitate HSV-I gene expression (Gu and Roizman, 2009; Cliffe and Knipe, 2008). It also causes degradation of host proteins that are involved in silencing HSV gene expression, such as the promyclocytic leukemia protein (Gu and Roizman, 2009).
- Example 8 SOCS-I antagonist svnergizes with IFN ⁇ in protection of macrophage cell line RAW264.7 against HSV-I
- SOCS-I acts at several sites in activation of Toll-like receptors (TLRs) in antigen presenting cells such as macrophages, perhaps to prevent an over-response of the innate immune system (Yoshimura et al, 2007; Mansell et al, 2006; Croker el al. 2008).
- TLRs Toll-like receptors
- the ability of SOCS-I antagonist to enhance the anti-HSV-1 effects of IFN ⁇ in the RAW264.7 macrophage cell line was determined. Infection of RAW264.7 cells with HSV-I at an moi of 0.1 resulted in 100% lysis in 48 hours in 96-well cultures as per Figure 8. IFN ⁇ at 100 U/nil resulted in 30% protection.
- SOCS-I antagonist p J AK2( 1001- 1013) at 25 ⁇ M did not protect against HSV-I.
- the combination of pJAK2(1001-1013) at 25 ⁇ M and IFN ⁇ at 100 U/ml resulted in 75% protection.
- pJAK2(l 001-1013) with alanine substitutions for tyrosines at positions 1007 and 1008 was much less effective at enhancement of IFN ⁇ activity.
- the SOCS-I antagonist enhanced IFN ⁇ effects against HSV-I in a macrophage cell line.
- JAK2(1001-1013) 1001 LPQDKEYYKVKEP (SEQ ID NO: 1)
- L929 cells (1.6 x 10 per well in 6-well plates) were treated with peptides for 24 h, followed by infection with HSV-I at moi 0.001 for 24 h. Cell lysates and supernatants were collected and viral yield was determined by standard plaque assay.
- BSC-40, MDCK, L929 and WISH cells were obtained from ATCC (Manassas, VA) and propagated on DMEM (BSC-40, L929, WISH) or EMEM (MDCK) with 10% fetal bovine serum. All cells were grown at 37°C in humidified atmosphere with 5% CO 2 .
- Vaccinia virus Western Reserve strain was a kind gift from Dr. Richard Condit (University of Florida). Vaccinia virus was grown, purified on sucrose gradient, and titrated on BSC-40 cells, as described (Earl and Moss, 1998). EMC virus was grown and titrated on L929 cells, as described (Mujtaba et ah, 2006). Influenza A/PR/8/34 virus was obtained from ATCC, and grown and titrated on MDCK cells, as described (Palese and Shaw, 2007).
- Peptides The sequence of peptides used is presented in Table 6. These peptides were synthesized on an Applied Biosystems 9050 automated peptide synthesizer using conventional fluorenylmethyloxycarbonyl chemistry as described previously (Szente el a!., 1994). The addition of a lipophilic group (palmitoyl-lysine) to the N-terminus of the synthetic peptide was performed as a last step, using semi-automated protocol. Peptides were characterized by mass spectrometry and were purified by HPLC.
- Western blot analysis Western blot analysis was carried out to determine whether Tkip and SOCSl-KIR inhibited the phosphorylation of STAT substrate by the various JAKs in cultured cells.
- Cells were incubated with various concentrations of lipophilic Tkip, Tkip2A, SOCSl-KIR, SOCS1-KIR2A or control peptide for 2 hours, after which interferon was added and the cells incubated for an additional 2 hours. The cells were washed in cold PBS and harvested in RlPA buffer containing protease and phosphatase inhibitor cocktails (Santa Cruz).
- Protein concentration was measured using a BCA kit (Pierce) and lysates were resolved on 12% SDS-PAGE, transferred onto nitrocellulose membranes, and probed with various anti-phosphotyrosine antibodies. The membranes were then stripped and reprobed with the indicated anti-protein antibodies. All antibodies used were from Santa Cruz Biotechnology. Scanning of the band intensity was carried out using Image J software from NIH. Mice. All animal protocols were approved by the Institutional Animal Use and
- mice Female C57BL/6 mice (6-8 weeks old) were purchased from Jackson Laboratories (Bar Harbor, ME). Peptides dissolved in PBS in a volume of 100 ⁇ l were administered intraperitoneally. For the oral administration of the peptides, indicated amounts of peptide in 0.5 ml PBS were given using a feeding needle. Intraperitoneal administration of vaccinia was done in a volume of 100 ⁇ l. For intranasal administration, vaccinia virus was taken in a volume of 10 ⁇ l, and 5 ⁇ l was delivered in each of the nostrils of a lightly anesthetized mouse. Following infection, mice were observed daily for signs of disease, such as lethargy, ruffled hair, weight loss, and eye secretions. Moribund mice were euthanized and counted as dead.
- signs of disease such as lethargy, ruffled hair, weight loss, and eye secretions.
- BSC-40 cells were seeded and grown overnight to confluency. Peptides at concentrations indicated were added to cells for one hour followed by infection with vaccinia virus at moi of 5 for one hour. This was followed by addition of growth medium containing the same amount of peptides as before and incubation for times indicated. Supematants were harvested, and the cells were scraped in 0.2 ml of cell lysis buffer consisting of 50 mM Tris.HCl, pH 7.5, 250 mM NaCl, 0.1% NP-40, 50 mM NaF and 5 mM EDTA, followed by three cycles of freeze thawing and sonication. The virus titer in the supernatant (extracellular) and cell extracts (intracellular) were measured by plaque assay on BSC-40 cells.
- CD4-deplction of splenocytes from na ⁇ ve or recovered mice was carried out by using the L3T4 antibody bound to Dynabeads (Invitrogen, Carlsbad, CA).
- ELISPOT assay was carried out by using a kit from Mabtech USA. Briefly, CD4-depleted cells (10 5 per well) were seeded in a microtiter plate, previously coated with an antibody to IFN ⁇ and incubated in the absence or presence of increasing amount of purified vaccinia virus for 24 hours at 37°C. After washing, diluted monoclonal antibody was added and incubated for 2 hours, followed by washing and addition of streptavidin-HRP.
- the plate was incubated for 2 hours at room temperature and washed three times with wash buffer.
- Peroxidase-conjugated goat anti-mouse IgA ( ⁇ chain specific), or IgG ( ⁇ chain specific) (both from Santa Cruz Biotechnology, Santa Cruz, CA) diluted in a volume of 0.1 ml, was added to each well, incubated for 1 hour, and washed five times with wash buffer.
- OPD in a volume of 0.1 ml was added and incubated for 15 min. The reaction was stopped by addition of 50 ⁇ l of 3 N HCl. The optical density at 490 nm was determined using a microtiter plate reader.
- Plaque reduction assay was carried out to test the ability of antibodies to inhibit viral infection of target cells, using the procedure described (Waiboci et al, 2007). BSC-40 cells were seeded to confiuency in a 6 well plate the day before the assay. Sera obtained from mice on days indicated were heated at 56 0 C for 30 min to inactivate the complement. Purified vaccinia virus (100 pfu) was incubated with a known dilution of serum at 37°C for 1 hour, followed by addition to BSC-40 cells. One hour later, the virus containing media was replaced with fresh medium containing 0.5% agarose and 0.01% neutral red. Three days later, the number of plaques was counted. The number of plaques in wells with vaccinia alone was taken as 100%. Percent reduction in other treatments carried out in triplicates was measured and is presented as average with standard deviation.
- the plasmid pGL3 promoter which expresses the firefly luciferase was obtained from Promega (Madison, WI).
- a constitutively expressed thymidine kinase promoter driven Renilla luciferase gene (pRL-TK) was used as an internal control in all of the reporter plasmid transfections.
- WISH cells were seeded in 12-well plates at 50% confiuency.
- Example 9 pJAK2f 1001-1013) protects mice against lethal vaccinia virus infection
- mice were injected LP. with 10, 50, and 200 ⁇ g of pJAK2(1001-1013) on days -2, -1, and 0 and challenged intranasally with 2 x 10 6 pfu of vaccinia virus (Figure 9). Complete protection was observed with 200 ⁇ g of SOCS-I antagonist, whereas 50 and 10 ⁇ g resulted in 80 and 20% protection from death, respectively. Recovered mice were completely free of any disease symptoms for the 40 days observed.
- Example 10 pJAK2(1001-1013) synergizes with an IFN mimetic in protecting mice against lethal vaccinia virus infection
- IFN ⁇ small peptide mimet ⁇ cs of TFN ⁇ , based not on the classical model of IFN ⁇ -initiatcd signaling by extracellular interaction, but rather on direct intracellular signaling by IFN ⁇ .
- IFN ⁇ its receptor subunit IFNGRl. and transcription factor STATl ⁇ are transported to the nucleus of cells as a complex where IFN ⁇ provides a classical polycationic nuclear localization sequence (NLS) for such transport (Ahmed and Johnson, 2006).
- the C-terminus of IFN ⁇ represented here by the mouse IFN ⁇ peptide, IFN ⁇ (95-132), was capable of forming a complex with IFNGRl and STATIa when introduced intracellularly and provided the NLS for nuclear transport (Ahmed et al, 2003).
- the IFN mimetic is a potent inhibitor of vaccinia virus infection in mice (Ahmed el ai, 2007).
- Example 11 Synergy between pJAK2(1001-1013) and IFN ⁇ mimetic in activation of GAS promoter element
- the transfected cells were incubated with pJAK2(l 001-1013), IFN ⁇ (95- 132), and the combination of the two for 24 hours, after which relative luciferase activity was measured.
- 10 ⁇ M of SOCS-I antagonist had minimal effect on reporter activation, while 5 ⁇ M IFN ⁇ mimetic was slightly more effective.
- 10 ⁇ M of antagonist plus 5 ⁇ M of IFN ⁇ mimetic together had a greater than four-fold effect on gene activation than did IFN ⁇ mimetic alone. This multiplicative effect is consistent with the synergy of protection against vaccinia virus of Figure 10.
- SOCS-I antagonist and IFN ⁇ mimetic show synergy at the level of IFN ⁇ gene activation.
- Example 12 pJAK2(l 001-1013) inhibits vaccinia virus replication as determined by a one-step growth curve
- pJAK2(1001-1013) inhibits vaccinia virus replication as opposed to just inhibiting spread.
- BSC-40 cells were treated with lipophilic pJAK2(1001-1013) at 50 ⁇ M for 1 hour, followed by infection with 5 moi of vaccinia virus to ensure simultaneous infection of all cells for a one-step growth curve.
- pJAK2(1001-1013) inhibited virus replication by approximately 92% as determined by intracellular virus yield ( Figure 12A) when compared to a variant, pJAK2(1001-1013)2A, with alanine substituted for tyrosine at positions 1007 and 1008 (Table 6).
- the alanine variant does not bind to KIR of SOCS-I (Unpublished observation). Inhibition was approximately 83% by extracellular virus yield ( Figure 12B).
- the SOCS-I antagonist pJAK2(1001-1013) inhibited vaccinia virus replication and not simply its release from cells.
- the fact that the alanine substituted variant of the antagonist did not inhibit virus replication suggests that the specificity of the antiviral effects of the antagonist is directed at SOCS-I in the cells.
- Example 13 pJAK2(1001-1013) treated cells had increased levels of endogenous IFN ⁇
- IFNB IF-induced IFNB
- pJAK2(1001-1013) affected the level of spontaneous IFNB, we treated L929 fibroblasts with the SOCS-I antagonist as well as the alanine substituted variant, pJAK2(l 001-1013)2A.
- IFN ⁇ signaling involves a complex of IFN ⁇ /IFNGRl/pSTATl ⁇ where the nuclear importins ⁇ and ⁇ bind to the complex via an NLS in IFN ⁇ (and the IFN ⁇ mimetic), which results in nuclear transport of the complex (Johnson et al., 2004).
- IFN ⁇ receptor chain IFNGRl functions as a transcription/cotranscription factor in conjunction with pSTATl ⁇ (Ahmed and Johnson, 2006).
- mice protected by the SOCS-I antagonist developed protective adaptive immunity to subsequent infection with a lethal dose of vaccinia virus.
- Mice protected by pJAK2(1001-1013) were rechallenged 10 weeks later with a second dose of 1 x 10 6 pfu of vaccinia virus administered intranasally without additional pJAK2(1001-1013) treatment. All five mice of the rechallenged group were protected against the lethality of the virus without showing symptoms of distress ( Figure 15A). Na ⁇ ve control mice all died by day 9.
- the pJAK2(1001-1013) in addition to providing protection against the first exposure to vaccinia virus, also allowed the mice to develop protective adaptive immunity to subsequent challenge with vaccinia virus.
- CD4-depleted splenocytes (10 5 /well) exposed to vaccinia virus showed increased secretion of IFN ⁇ by ELISPOT at 3 weeks after virus challenge (Figure 15C), suggesting the induction of vaccinia virus- specific cytotoxic CD8+ T cells. Control cells did not respond to virus.
- mice protected by pJAK2(1001-1013) mounted both a strong cellular and humoral immune response to vaccinia virus.
- Example 15 pj AK2 exerts an adjuvant effect on the immune system
- BSA bovine serum albumin
- pJAK2(l 001-1013) on days -2, -1, arid 0, and then assessed for enhancement of cellular and humoral immune responses.
- splenocytes of the mice were stimulated in cell culture with 0.5 ⁇ g of BSA.
- mice treated with p.TAK2(1001-1013) had an approximately eight-fold greater proliferative response to BSA.
- the humoral immune response as assessed by the serum IgG antibody response to BSA in the mice was also significantly enhanced in the pJAK2(1001-1013) treated mice at 3 and 4 weeks post-immunization ( Figure 16B).
- RAW264.7 cells treated with pJAK2(1001-1013) produced approximately a six-fold increase in nitric oxide (NO) upon lipopolysaccharide (LPS) stimulation compared with a control peptide ( Figure 16C).
- pJAK2(1001-1013) has an adjuvant effect in terms of the cellular and humoral immune responses as well as in macrophage activation.
- the antagonist in addition to direct inhibition of virus replication, the antagonist also has an adjuvant effect on the immune response.
- EMC virus is a rodent picomavirus, but can infect other species, including humans.
- EMC virus is a relatively simple, small plus stranded RNA virus (Racaniello,
- Example 17 pJAK2(1001-1013) induces an antiviral state against EMC virus in the presence of antibodies to IFN ⁇
- Example 18 pJAK2(l 001 -1013) protects mice against lethal EMC virus infection
- mice were treated i.p. with 50, 100, or 200 ⁇ g of pJAK2(1001-1013) or 200 ⁇ g of the alanine-substituted antagonist, pJAK2(100l -l Ol3)m with alanine substituted for tyrosine at residues 1007 and 1008, every day beginning at day -2.
- the mice were challenged with 50 pfu of EMC virus per mouse and monitored daily for survival.
- mice treated with the alanine-substituted antagonist all died by day 5 after EMC virus challenge.
- mice treated with 100 and 200 ⁇ g ⁇ JAK2(1001 -1013) showed 80% and 60% survival, respectively.
- Treatment with 50 ⁇ g of pJAK2(1001-1013) resulted in 20% of mice surviving EMC virus challenge.
- administration of pJAK2(1001-1013) at 100 and 200 ⁇ g daily resulted in significant protection of mice.
- JAK2(1001-1013)m 1001 LPQDKEAAKVKEP (SEQ ID NO:71)
- Example 19 SQCS antagonist and IFN mimetic possess antiviral activity against HlNl influenza virus
- MDCK cells were infected with influenza A PR8 virus and treated with SOCS antagonist pJAK2, IFN- ⁇ (95-132) mimetic peptide, alone or in combination, and the virus yield was estimated by hemagglutinin assay.
- SOCS antagonist peptide and IFN- ⁇ mimetic peptide provided synergistic protection against the influenza virus, as shown in Figure 19.
- BSC-40, L929, WISH, or RAW264.7 cells were obtained from ATCC (Manassas, VA) and propagated on DMEM with 10% fetal bovine serum (BSC-40, L929, WISH), or RPMI 1640 with 10% fetal bovine serum (RAW264.7). All cells were grown at 37 0 C in humidified atmosphere with 5% CO 2 .
- Vaccinia virus Western Reserve strain was a kind gift from Dr. Richard Condit (University of Florida). Vaccinia virus was grown, purified on sucrose gradient, and titrated on BSC-40 cells, as described (Ahmed et al. (2005)). EMC virus was grown and titrated on L929 cells, as described (Muitaba et al (2006)).
- Peptides The sequence of peptides used in this study is presented in Table 7. These peptides were synthesized on an Applied Biosystems 9050 automated peptide synthesizer using conventional fluorenylmethyloxycarbonyl chemistry as described previously (Szente et al. (1994)). The addition of a lipophilic group (palmitoyl-lysine) to the N-terminus of the synthetic peptide was performed as a last step, using semi- automated protocol. Peptides were characterized by mass spectrometry and were purified by HPLC. Mice. All animal protocols were approved by the Institutional Animal Care and
- mice Female C57BL/6 mice (6-8 weeks old) were purchased from Jackson Laboratories (Bar Harbor, ME). Peptides dissolved in PBS in a volume of 100 ⁇ l were administered intraperitoneally. For the oral administration of the peptides, indicated amounts of peptide in 0.5 ml PBS were given using a feeding needle. Intraperitoneal administration of EMCV was done in a volume of 100 ⁇ l. For intranasal administration, vaccinia virus was taken in a volume of 10 ⁇ l, and 5 ⁇ l was delivered in each of the nostrils of a lightly anesthetized mouse. Following infection, mice were observed daily for signs of disease, such as lethargy, ruffled hair, weight loss, and eye secretions. Moribund mice were euthanized and counted as dead.
- signs of disease such as lethargy, ruffled hair, weight loss, and eye secretions.
- FITC labeling and detection of cell penetration FITC was conjugated with lipo- pJAK2(1001-1013), according to the manufacturer's (Pierce, Rockford, IL) instruction. Mice were injected i.p. with 15 mg FITC-labeled lipo-pJAK2(1010-1013) or an equivalent amount of FITC alone. Two hours later, peritoneal cells were harvested and viewed in a fluorescent microscope. L929 cells were similarly treated with 5 niM FITC- labeled lipo-pJAK2(l 010-1013) or FITC alone for 2 h, followed by visualization in a fluorescent microscope. Reporter gene assays.
- the plasmid pGL3 promoter which expresses the firefly luciferase was obtained from Promega (Madison, WI).
- a constitutively expressed thymidine kinase promoter driven Renilla luciferase gene (pRL ⁇ TK) was used as an internal control in all of the reporter plasmid transfections.
- WISH or L929 cells were seeded in 12-well plates at 50% confluency.
- murine SOCS-I or SOCS-3 cDNA in CMV promoter driven constructs were included in the transfection. Measurement of intracellular and extracellular vaccinia virus formation. BSC-40 cells were seeded and grown overnight to confluency. Peptides at concentrations indicated were added to cells for one hour followed by infection with vaccinia virus at moi of 5 for one hour. This was followed by addition of growth medium containing the same amount of peptides as before and incubation for times indicated.
- Western blot analysis Western blot analysis was carried out to determine whether pJAK2(l 001-1013) had an effect on endogenous pSTATl , STATl , SOCS-I, IFNa, or IFNB levels.
- Cells were incubated with various concentrations of lipophilic pJAK2(1001- 1013) or JAK2(1001-1013)2A for 30 to 60 minutes. The cells were washed in cold PBS and harvested in RIPA buffer containing protease and phosphatase inhibitor cocktails (Santa Cruz Biotechnology, Santa Cruz, CA).
- Protein concentration was measured using a BCA kit (Pierce, Rockford, IL) and lysates were resolved on 12% SDS-PAGE, transferred onto nitrocellulose membranes, and probed with various antibodies. The membranes were then stripped and reprobed with the indicated anti-protein antibodies.
- IFN antibodies were from PBL (Piscataway, NJ)
- pSTATl and SOCS antibodies were custom made from GenScript (Pisactaway, NJ).
- STATl Abs were from Santa Cruz (Santa Cruz Biotechnology, Santa Cruz, CA). Scanning of the band intensity was carried out using Image J software from National Institutes of Health (Bethesda, MD).
- IFN- ⁇ ELISA L929 cells were treated with peptides for 30 or 60 min and then lysed with RIPA lysis buffer containing protease inhibitor cocktails (Sigma-Aldrich, St. Louis, MO). The cell lysates were analyzed with a murine IFN - ⁇ ELISA kit (PBL Biomedical Laboratories), following the manufacturer's instructions. Briefly, cell lysates were plated onto plate strips for 1 h at room temperature. The strips were washed three times with wash buffer and then incubated with the Ab solution for 1 h at room temperature. After washing the strips three times, they were incubated with the HRP solution for 1 h at room temperature.
- the strips were washed three times and incubated with TMB substrate solution for 15 min at room temperature. The reaction was stopped by addition of stop solution. The absorbance was measured at 450 nm with a standard plate reader (Bio-Tek Instruments, Winooski, VT).
- Spleens from naive or recovered mice at times indicated were homogenized to single cell suspension.
- Splenocytes (10 " cells per well) were incubated with medium alone, or medium containing UV-inactivated vaccinia virus at 37 0 C for 96 hours.
- the cultures were then pulsed with [ 3 H] -thymidine (1 ⁇ Ci/well; Amersham Biosciences, Piscataway, NJ) for 8 hours before harvesting onto filter paper discs using a cell harvester.
- Cell associated radioactivity was counted using a scintillation counter.
- Stimulation index refers to the incorporation in splenocytes cultured with test antigen divided by incorporation in splenocytes cultured with medium alone.
- vaccinia virus specific cellular response by IFN- ⁇ ELISPOT Measurement of vaccinia virus specific cellular response by IFN- ⁇ ELISPOT.
- CD4-depletion of splenocytes from na ⁇ ve or recovered mice was carried out by using the L3T4 antibody bound to Dynabeads (Invitrogen, Carlsbad, CA).
- diluted monoclonal antibody was added and incubated for 2 hours, followed by washing and addition of streptavidin-HRP. After 1 hour at room temperature, the wells were washed and TMB substrate was added, washed and the spots were counted.
- Microtiter plates were coated with 10 6 pfu of purified UV-inactivated vaccinia virus (900,000 ⁇ J/cm 2 for 5 min in a DNA cross-linker) in 100 ⁇ l of binding buffer (carbonate-bicarbonate, pH 9.6) overnight at 4 0 C. Plates were blocked for 2 hours at room temperature with PBS containing 5% fetal bovine serum. Mouse sera was serially diluted in PBS containing 0.1% Tween-20 (wash buffer). 0.1 ml of the diluted serum was added to each well. The plate was incubated for 2 hours at room temperature and washed three times with wash buffer.
- binding buffer carbonate-bicarbonate, pH 9.6
- Peroxidase-conjugated goat anti-mouse IgA ( ⁇ chain specific), or IgG ( ⁇ chain specific) both from Santa Cruz Biotechnology, Santa Cruz, CA
- diluted in a volume of 0.1 ml was added to each well, incubated for 1 hour, and washed five times with wash buffer.
- OPD in a volume of 0.1 ml was added and incubated for 15 min.
- the reaction was stopped by addition of 50 ⁇ l of 3 N HCl.
- the optical density at 490 nm was determined using a microtiter plate reader.
- Plaque reduction assay was carried out to test the ability of antibodies to inhibit viral infection of target cells.
- BSC-40 cells were seeded to confluency in a 6 well plate the day before the assay.
- Sera obtained from mice on days indicated were heated at 56 0 C for 30 min to inactivate the complement.
- Purified vaccinia virus (100 pfu) was incubated with a known dilution of serum at 37 0 C for 1 hour, followed by addition to BSC-40 cells.
- the virus containing media was replaced with fresh medium containing 0.5% agarose and 0.01% neutral red.
- Two days later, the number of plaques was counted.
- the number of plaques in wells with vaccinia alone was taken as 100%. Percent reduction in other treatments carried out in triplicates was measured and is presented as average with standard deviation.
- Binding assays were performed as previously described (Waiboci ei al. (2007)) withminor modifications. pJAK2(1001-1013) or JAK2(1001-1013)2A were bound to 96-well plates, in binding buffer (in 0.1 M carbonate-bicarbonate (pH 9.6)), at a final concentration of 3 ⁇ g/well.
- Macrophage stimulation Murine macrophage cells, RAW 264.7, were seeded on 96-well plates at a concentration of 5 X 10 6 cells/well in 200 ⁇ l volume and allowed to adhere. Lipo peptides, pJAK2( 1001-1013) or the control peptide JAK2(1001-1013)2A, at 25 ⁇ M were then added to the wells and the cells incubated for 4 h, after which 2 ⁇ g/ml of LPS or 0.1 ⁇ g/ml polyI:C were added and the cells were incubated for 3 days. Supernatants were transferred to fresh tubes and assayed for NO production using Griess reagent, according to the manufacturer's instructions (Alexis Biochemicals, Plymouth Meeting, PA).
- Antiviral assay for EMCV Antiviral assays for EMCV were performed by using a cytopathic effect reduction assay.
- Murine L929 cells (6 x 10 4 cell/well) were seeded in a 96-well plate and grown overnight to confluence for optimal growth.
- Various concentrations of IFN- ⁇ , IFN- ⁇ (95-132), IFN- ⁇ (95-125), pJAK2(1001-1013), and JAK2(1001-1013)2A were added and incubated for 2 h, after which 200 pfu/well of EMC virus was added to the plate and incubated. After 1 h, virus was removed, fresh media was added and incubated for 24 h. Cells were stained with 0.1% crystal violet.
- Unbound crystal violet was aspirated, and the plates were thoroughly rinsed with deionized water, blotted, and allowed to air dry. Plates were then scanned and analyzed using Image J 1.29 software (National Institutes of Health, Bethesda, MD) to assess cell survival. Percentages of cell survival were determined by comparing survival for the experimental treatment groups with that for the virus-only control group.
- Example 21 pJAK2(1001-1013) protects mice against lethal vaccinia virus infection
- mice were injected i.p. with 10, 50, and 200 ⁇ g of pJAK2(1001-1013) on days -2, -1 , and 0 and challenged intranasally with 2 x 10 pfu of vaccinia virus given intranasally ( Figure 20).
- Complete protection was observed with 200 ⁇ g of SOCS-I antagonist, whereas 50 and 10 ⁇ g resulted in 80 and 20% protection from death, respectively. Recovered mice were completely free of any disease symptoms for the 30 days observed.
- mice i.p. with 15 ⁇ g FITC-lipo-pJAK2(1001-1013) or treated L929 cells in culture with 5 ⁇ M FITC-lipo-pJAK2(1001-1013).
- An equivalent amount of FITC alone was used as a control.
- peritoneal cells or L929 cells were examined by confocal fluorescence microscopy for FITC uptake.
- FITC-lipo- pJAK2(1001-1013) but not FITC alone was internalized by peritoneal cells.
- FITC-lipo-pJAK2(1001-1013) was specifically taken up by L929 cells as shown in Figure 21B.
- the SOCS-I antagonist is internalized where it has access to the SOCS-I target.
- Example 22 pJAK2(1001 -1013) exerts an adjuvant effect on the immune system
- BSA bovine serum albumin
- mice treated with pJAK2(1001-1013) had an approximately eight-fold greater proliferative response to BSA.
- the humoral immune response as assessed by the serum IgG antibody response to BSA in the mice was also significantly enhanced in the pJAK2(1001-1013) treated mice at 3 and 4 weeks post- immunization ( Figure 22B).
- the SOCS antagonist can also enhance the antibody response to the T-cell independent antigen lipopolysaccharide (LPS). This is shown in Figure 22C, in which the antibody response of mice immunized with LPS was significantly enhanced by i.p. injection of pJAK2(1001-1013).
- staphylococcal entcrotoxin superantigens staphylococcal enterotoxin A (SEA) and staphylococcal enterotoxin B (SEB) enhanced T cell-dependent antibody production (Torres et al. (2002)), but SEA/SEB did not enhance the anti-LPS response.
- SEA/SEB did enhance the antibody response to bovine serum albumin (BSA), a T cell-dependent antigen.
- BSA bovine serum albumin
- TLR macrophage toll-like receptor
- TLR3 thus plays an important role in the antiviral responses to HSV-I, influenza virus, cytomegalovirus, and respiratory syncytial virus, all of which have a dsRNA stage in their replication (Vercammen et al (2008); Pothlichet et al. (2008)).
- SOCS-I negatively regulates TLR signaling at several stages including signaling by type I IFNs and by NF- KB transcription factor (Yoshimura et al. (2007); Mansell et al. (2006); Yasukawa et al. (1999); Kobayashi et al. (2006)).
- SOCS-I antagonist pJAK2(1001-1013) binds to SOCS-I via the SOCSl -KIR region (Yoshimura et al. (2007)).
- SOCS-3 also regulates immune functions and has been suggested to play the central role in inhibition of STAT3 activation in T helper 17 cells (Chen et al. (2006)). It is thus of interest with respect to possible regulation by the SOCS-I antagonist.
- both SOCSl- KIR and SOCS3-KIR bound similarly to the SOCS-I antagonist. Since pJAK2(1001- 1013) represents the activation loop of JAK2, this would suggest that the antagonist would inhibit the function of both SOCS-I and SOCS-3.
- mice were infected with EMC virus and treated with suboptimal doses of pJAK2(l 001 -1013) and IFN- ⁇ (95-132) in order to assess synergy.
- treatment with pJAK2(1001-1013) at 10 ⁇ g and IFN- ⁇ (95-132) at 2 ⁇ g resulted in 80% survival of infected mice, while pJAK2(1001-1013) treatment alone resulted in 40% survival, the same as that of PBS-treated mice.
- IFN- ⁇ (95-132) alone resulted in 60% survival of mice.
- Ahmed CM. K.N. Wills, HJ. Sugarman, D. E. Johnson, M. Ramachandra, T.L.
- IFN-gamma and its receptor subunit IFNGRl are recruited to the IFN-gamma-activated sequence element at the promoter site of IFN-gamma-activated genes: evidence of transactivational activity in IFNGRl. J. Immunol. 177:315-321
- ICP 47 Infected cell protein 47 enhances herpes simplex virus neurovirulence by blocking the CD8+ T cell response. J. Exp. Med. 187:341 -348
- TLR3 Interferon induction by double-stranded RNA including poly(I:C). Advanced Drug Deliv. Rev. 60: 805-812.
- Picornaviridae The viruses and their replication. In Fields Virology, 3rd ed. D. M. Knipe, and P.M. Howley, eds. Lippincott, Williams, and Wilkins, Philadelphia, PA. 795-838.
- herpes simplex virus type 1 alpha protein ICP27 can act as a trans-repressor or a trans-activator in combination with ICP4 and ICPO. J. Virol. 62:4510-4522
- the IFNARl subunit of the type I IFN receptor complex contains a functional nuclear localization sequence. FEBS Lett 578: 207-210.
- IFN- gamma-derived lipopeptides influence of lipid modification on the conformation and the ability to induce MHC class II expression on murine and human cells. J.
Abstract
The subject invention concerns materials and methods for inhibiting activity of a broad spectrum of viruses in humans and animals. In one embodiment of the invention, a method is provided for treating or preventing viral infection in an animal by administering an effective amount of peptide that is an antagonist of SOCS-I and/or SOCS-3. In a specific embodiment, the peptide corresponds to the activation loop of janus kinase JAK2. In an exemplified embodiment, the peptide has the amino acid sequence: LPQDKEYYKVKEP (pJAK2 (1001-1013)) (SEQ ID NO:1). Compositions contemplated within the scope of the invention include peptides of the invention and optionally one or more other antiviral compounds. Examples of viruses whose replication can be inhibited using the present invention include, but are not limited to, vaccinia virus, EMC virus, influenza virus, and herpes simplex virus. In addition to treating a human or animal having a viral infection, the subject invention can also be used to prevent viral infection in an uninfected human or animal.
Description
DESCRIPTION
MATERIALS AND METHODS FOR TREATING AND PREVENTING VIRAL INFECTIONS
CROSS-REFERENCE TO RELATED APPLICATIONS
The present application claims the benefit of U.S. Provisional Application Serial
No. 61/220,920, filed June 26, 2009 and U.S. Provisional Application Serial No. 61/354, 124, filed June 11 , 2010, each of which is hereby incorporated by reference herein in its entirety, including any figures, tables, nucleic acid sequences, amino acid sequences, and drawings.
GOVERNMENT SUPPORT The subject matter of this application has been supported by a research grant from the National Institutes of Health under grant numbers 5R01NS51245 and R01AI056152. Accordingly, the government has certain rights in this invention.
BACKGROUND OF THE INVENTION Viruses are a heterogeneous group of intracellular infectious agents that depend in varying degrees on the host synthetic machinery for replication. The poxviruses are large, double-stranded DNA viruses that are assembled in the cytoplasm of infected cells involving complex replication mechanisms (Moss, 2007). Attachment, internalization, and disassembling of poxviruses precedes the initiation of three waves of mRNA synthesis. The early wave codes for virus growth factors and decoy cytokine receptors. Decoy receptors for both type I and type II interferons (IFNs) are produced during early protein synthesis in poxvirus infected cells, thus blunting perhaps the most important innate host defense system against viral infections (Moss and Shisler, 2001). A well- known example of this is the B8R protein of vaccinia virus, which is a homolog of the extracellular domain of the IFNγ receptor (Moss, 2007).
Encephalomyocarditis (EMC) virus is a small single-stranded RNA picornavirus of the plus strand orientation with wide host range (Racaniello, 2007). In mice, EMC virus infection is lethal, but is quite susceptible to IFNγ or an IFNγ mimetic treatment at early stages of infection (Mujtaba et ah, 2006). The IFNγ mimetic is also effective against vaccinia virus infection even in the presence of B8R decoy receptor (Ahmed et ah, 2005; Ahmed et ah, 2007). The IFNγ mimetic is a small peptide corresponding to the C- terminus of IFNγ that functions intracellularly and thus does not interact with the extracellular domain of the IFNγ receptor (Ahmed et ah, 2005).
The IFNγ mimetic is also effective against another large double-stranded DNA virus called herpes simplex 1 or HSV-I that replicates in the cell nucleus (Frey et ah, 2009). Close relatives include the herpes Zoster virus and cytomegalovirus (Roizman et ah, 2007). The broad spectrum of antiviral activity of IFNγ mimetics is unique in that we are unaware of any other small antiviral that exhibits strong activity against poxviruses, picornaviruses, and herpesviruses. The IFN system is regulated by an inducible endogenous tyrosine kinase inhibitor called suppressor of cytokine signaling 1 or SOCS-I (Yoshimura et ah, 2007; Mansell et ah, 2006; Yasukawa et ah, 1999; Kobayashi el ah, 2006; Croker et ah, 2008). SOCS-I is a member of a family of inducible proteins that negatively regulate IFN and other cytokine signaling via inhibition of JAK/STAT signaling (Yoshimura et ah, 2007). There are currently eight members of the SOCS family, SOCS-I to SOCS-7 and cytokine- inducible SH2 protein. SOCS-I has distinct regions or domains that define the mechanism by which it inhibits the function of JAK tyrosine kinases such as JAK2 that are involved in activation of STAT transcription factors (Yoshimura et ah, 2007). The N- terminus of SOCS-I contains a SH2 domain, and N-terminal to it is an extended SH2 sequence (ESS) adjacent to a kinase inhibitory region (KlR) (Yoshimura et ah, 2007). These domains or regions of SOCS-I bind to the activation and catalytic regions of JAK2 and block its function. The C-teπninus of SOCS-I contains a domain called the SOCS box, which is involved in proteasomal degradation of JAK2. It has been shown that the KIR sequence of SOCS-I binds to a peptide corresponding to the activation loop of JAK2, pJAK2(l 001-1013), and that the peptide pJAK2(1001-1013) blocked SOCS-I activity in cells (Waiboci et ah, 2007). Specifically, pJAK2(l 001-1013) enhances suboptimal IFN activity, blocks SOCS-I induced inhibition of STAT3 activation,
enhances IFNγ activation site promoter activity, and enhances antigen-specific proliferation.
Influenza A virus is a segmented negative strand RNA virus that is responsible for over 30,000 deaths annually in the United States (Palese and Shaw, 2007). Pandemic influenza A virus infection can cause the deaths of millions world-wide. Type I IFNs are an important early innate immune response cytokine against influenza respiratory infections (Szretter et al, 2009). Influenza virus-encoded nonstructural protein NSl is multifunctional and is important in virus defense against IFNs by a mechanism(s) that is not fully understood but may involve induction of SOCS-I and SOCS-3, which in turn would negatively regulate IFN signaling (Pothlichet et al, 2008).
Herpes Simplex Virus (HSV) is a member of a broad class of double-stranded DNA viruses that undergo replication in the cell nucleus. Examples of other members are varicella-zoster virus (VZV) and cytomegalovirus (CMV) (Roizman el al, 2007). It is estimated that HSV-I infects 60 to 80 percent of the people throughout the world, and persists for life in the infected individuals (Diefenbach et al, 2008; Koelle and Corey, 2008; Cunningham et al, 2006). Primary infection commonly occurs through cells of the mucous membrane and is often asymptomatic. This is followed by uptake of virus by sensory nerve fibers and retrograde transport to the cell body of the neurons in the dorsal root or trigeminal ganglion. Here, acute infection is converted to latency and from which HSV-I periodically migrates down the nerve tissue to again infect mucosal cells for overt disease (Roizman el al, 2007; Diefenbach et al, 2008; Koelle and Corey, 2008; Cunningham et al, 2006).
HSV-I infection is characterized by a strong cytokine response in infected cells, particularly the induction of type I IFNs (Cunningham et al, 2006). Infection of keratinocytes, for example, results in induction of large amounts of IFNα and IFNβ as well as interleukins 1, 6, and β-chemokines (Mikloska et al, 1998). IFNs, macrophages, natural killer (NK) cells, and gamma/delta T cells all play an important role in host innate immune response to HSV-I (Cunningham et al, 2006). Toll-like receptor (TLR) 2 is activated on the cell surface by HSV-I, while TLR-9 is activated intracellularly by viral DNA. The latter stimulus is thought to play an important role in induction of IFNα by HSV-I (Cunningham et al, 2006).
The adaptive immune response plays an important role in confining HSV-I and other herpesvirus infections to a latent state where CD 8" T cells and IFNγ play critical roles (Knickelbein et al, 2008; Sheridan et al, 2007; Decman et al, 2005). It is functionally connected to the innate immune system where NK cells can serve as a source of IFNγ, which is also produced by CD4 and CD 8+ T cells. IFNγ can exert direct antiviral activity as well as induce upregulation of MHC class I and class II molecules on macrophages, dendritic cells, and keratinocytes (Decman et al, 2005). Direct effects of IFNγ as per a mouse model suggest that this IFN prevents reactivation of HSV by inhibition of function of the key intermediate protein ICPO (Mossman, 2005). Interaction of the antigen presenting cells with CD4+ T cells induces CD8+ T cells to control HSV-I levels in mucosal lesions (Arduino and Porter, 2008; Patel et al., 2007).
HSV-I has developed several mechanisms to inhibit both the innate and adaptive immune responses to infection. HSV-I downregulation of class I MHC expression occurs through high affinity binding of viral immediate early gene product ICP47 to the transporter associated with antigen processing (TAP) (Burgos et al, 2006), which blocks IFNγ induction of cytotoxic CD8 T cells (Goldsmith et al, 1998). IFN signaling is also inhibited by blockage of JAK/STAT transcription factor phosphorylation by an unknown mechanism (Chee and Roizman, 2004). ICPO is thought to enhance proteasome- dependent degradation of IFN stimulated genes (ISGs) (Halford et al, 2006; Edison et al, 2002). A recent study suggests that HSV-I can exert an anti -interferon effect by activation of a protein called suppressor of cytokine signaling 3 (SOCS-3) (Yokota et al, 2004).
SOCS consists of a family of inducible proteins that regulate the JAK/STAT transcription system that is critical in mediation of functions of cytokines such as the IFNs. These inducible proteins share domains of homology that characterize the SOCS family, which consists of eight identified members, SOCS-I to SOCS-7 and cytokine induced SH2 protein (CIS) (Yoshimura et al, 2007; Mansell et al, 2006; Croker et al, 2008). All of the SOCS proteins contain a SH2 domain and a C-terminal SOCS box domain that is involved in proteasomal degradation of SOCS-associated proteins. SOCS- 1 and SOCS-3 also contain a kinase inhibitory region (KIR) of 12 amino acids that, in conjunction with SH2, inhibits JAK tyrosine kinase activity (Yoshimura et al, 2007; Mansell et al., 2006; Croker et al, 2008). Thus, these SOCS-I and SOCS-3 molecules
can regulate cytokine function by proteasomal degradation and inhibition of the relevant JAK activity (Yoshimura et a!.. 2007; Croker el al., 2008).
Currently, there are no effective therapeutics available against HSV infection, except the nucleoside analog acyclovir (Dorsky and Crumpacker, 1987), which is known to have serious side effects. A search for a vaccine against HSV has remained elusive because of the successful adaptation to the host used by HSV (Koelle and Corey, 2008).
Along with direct effects, infection with HSV has been found to increase the incidence of
HIV infection, probably due to HSV-associated lesions (WaId and Link, 2002). Because of this interplay between HSV and HIV, it is conceivable that anti-HSV treatment may reduce the incidence of infection with HIV.
BRIEF SUMMARY OF THE INVENTION
The subject invention concerns materials and methods for inhibiting activity and/or replication of a broad spectrum of viruses in humans and animals. In one embodiment of the invention, a method is provided for treating or preventing viral infection in a human or animal by administering an effective amount of a peptide that is an antagonist of SOCS-I and/or SOCS-3. In a specific embodiment, the peptide corresponds to the activation loop of janus kinase JAK2. In an exemplified embodiment, the peptide comprises the amino acid sequence: LPQDKEYYKVKEP (pJAK2 (1001 - 1013)) (SEQ ID NO:1), or a biologically active fragment or variant thereof that exhibits antiviral activity. Examples of viruses whose activity and/or replication can be inhibited using the present invention include, but are not limited to, vaccinia virus, EMC virus, influenza virus, and herpes simplex virus. In addition to treating a human or animal having a viral infection, the subject invention can also be used to prevent viral infection in an uninfected human or animal.
The subject invention also concerns peptides, and compositions comprising the peptides, that are an antagonist of SOCS-I protein. In a specific embodiment, the peptide corresponds to the activation loop of janus kinase JAK2. In an exemplified embodiment, the peptide comprises the amino acid sequence: LPQDKEYYKVKEP (pJAK2 (1001- 1013)) (SEQ ID NO:1), or a biologically active fragment or variant thereof that exhibits antiviral activity. Compositions contemplated within the scope of the invention can
comprise one or more peptides of the invention and optionally one or more other antiviral compounds.
BRIEF DESCRIPTION OF THE DRAWINGS Figures 1A-1D. Differential response to IFNγ and IFNγ mimetic peptide in fibroblasts (L929) and keratinocytes (HEL-30). L929 fibroblasts (Figures IA and 1C) and HEL-30 keratinocytes (Figures IB and ID) were grown overnight and treated with IFN-γ (Figures IA and IB), or IFNγ mimetic (Figures 1C and ID) at the indicated concentrations for 24 hours, after which HSV-I (syn 17h) was added at an moi of 0.1. Cells were incubated for 48 hours, rinsed with HBSS, fixed and stained with crystal violet. Densitometry measurements of each well were computed using Multi-gauge software for quantitation of cell survival of the various treatment groups. Data are expressed as percentage of background corrected for medium control. Error bars indicate standard error of the means. The experiments were carried out in triplicate and data are representative of two independent experiments. There were statistically significant differences between IFNγ and or IFNγ peptide treated cells when compared to the untreated cells (P < 0.001) as determined by Mann-Whitney signed rank test.
Figures 2A-2D. HSV-I infection causes induction of SOCS-I in keratinocytes (HEL-30 cells), but not in fibroblasts (L929 cells). (Figure 2A). HEL-30 and L929 cells were infected with HSV-I at an moi of 1 for 12 hours. Total RNA was extracted and used as a template for RT-PCR using primers specific for SOCS-I or GAPDH, the control. Data are presented as the ratio of SOCS-I to GAPDH. HEL-30 (Figure 2B) and L929 (Figure 2C). cells exhibit differences in SOCS-I protein expression as analyzed by Western blot analysis. Cells were infected with HSV-I at an moi of 2. At the indicated time points, cells were harvested, washed, lysed, and whole-cell extracts were isolated. Lysates were subjected to 10% SDS-PAGE. Proteins were blotted onto a PVDF membrane and probed with an antibody specific for SOCS-I. Membranes were stripped and re-probed with β-tubulin to control for equal loading of samples. (Figure 2D) Time course of SOCS-I induction in HEL-30 cells. Cells were infected at an moi of 2 for the times indicated. RNA was extracted and used for RT-PCR as in (Figure 2A) above. Results are indicative of three independent experiments.
Figures 3A and 3B. Inhibition of STATIa phosphorylation upon HSV-I infection in HEL-30, but not in L929 cells. HEL-30 (Figure 3A) or L929 (Figure 3B) cells were mock treated or infected with HSV-I at an moi of 2 was used in 4 hour incubation. Some of the infected cells were also treated with 1000 U/ml IFN-γ for 10 minutes. Cells were washed in PBS, harvested, lysed, and whole-cell extracts were isolated. Extracts were subjected to 10% SDS-PAGE. Proteins were blotted onto a PVDF membrane and probed with an antibody specific for pSTAT-la (Tyr 701). Filters were stripped and re-probed with antibody to total STATIa to ascertain equal loading of proteins. Figure 4. HSV-I infection increases transcription from the SOCS-I promoter.
HEL-30 cells were cultured overnight in 12-well plates and transfected with a luciferase reporter construct containing the full-length SOCS-I promoter. Cells were incubated for 24 hours and then mock- infected or infected with HSV-I at an moi of 2 for 4 hours, after which they were treated with IFN-γ at 2000 U/ml for 2 hours. Cell lysates were collected and luciferase activity was measured in a single-tube luminometer. Values given are expressed as luciferase units measured from the SOCS-I reporter divided by luciferase units measured from a co-transfected constitutive reporter and subsequently normalized to medium controls. Values are representative of triplicate wells of the two independent experiments. The experiments were carried out in triplicate and data are representative of two independent experiments. There were statistically significant differences between IFNγ, HSV-I, and HSV-I + IFNγ treated cells when compared to the untreated cells (P < 0.001) as determined by Mann-Whitney signed rank test.
Figures SA and 5B. A peptide antagonist of SOCS-I (Figure 5A) or siRNA for SOCS-I (Figure 5B) reduced HSV-I -induced CPE in HEL-30 cells. (Figure 5A) HEL-30 cells were cultured overnight in 96-well plates and treated with 100 U/ml IFN γ alone or different concentrations of pJAK2(l 001 -1013) with or without 100 U/ml of IFNγ. Following treatment for 24 hours, cells were mock-infected or infected with HSV-I at an moi of 0.1. Plates were incubated 48 hours, washed with PBS, fixed and stained with crystal violet. Absorbance units of each well were calculated using Multi-Gauge. Values are expressed as percent cell survival relative to mock-infected controls. Values are representative of duplicate wells of two independent experiments. (Figure 5B) HSV-I- induced cytopathic effect is reduced by treatment with SOCS-I siRNA. HEL-30 cells
were transfected with control or SOCS-I siRNA, incubated for 48 hours, then treated with IFN-γ for 6 hours, and subsequently infected with 100 pfu HSV-I (synl7+). At 72 hours post-infection, the cells were fixed and stained with crystal violet. Plates were scanned using a flatbed scanner. Densitometry measurements of each well were made using NIH Image J.
Figures 6A-6C. Overexpression of SOCS-I inhibits the antiviral activity of IFN- γ in HSV-I -infected L929 cells. (Figure 6A). Transfection with cDNA expressing SOCS- 1. L929 cells were transfected with SOCS-I expression plasmid for one day. Cell extracts were then electrophoresed and probed with an antibody to SOCS-I followed by stripping and probing with β-tubulin antibody as a control. (Figure 6B). L929 fibroblasts were grown overnight in 12 well-plates to -90% confluence. Cells were transfected with the indicated amounts of control plasmid or pFLAG-SOCS-1 plasmid. Cells were incubated for 24 hours and treated with 100 U/ml IFNγ for 24 hours. Cells were washed once and infected with HSV-I (syn 17+) at an moi of 0.1, and then incubated for 48 hours, washed with HBSS, fixed, and stained with crystal violet. Absorbance units of each well were calculated using Multi-Gauge software. (Figure 6C). HSV-I -induced CPE is increased in L929 cells treated with a SOCS-I peptide mimetic. L929 fibroblasts were grown overnight and treated with ΪFN-γ (100 U/ml) and Tkip (20 μM), or Tkip2A (20 μM) for 24 hours, after which HSV-I (syn 17+) was added at an moi of 0.1. Cells were incubated for 48 hours, washed with HBSS, fixed and stained with crystal violet as in (Figure 6A) above. Values are expressed as percent cell survival relative to mock-infected controls. Results are representative of duplicate wells of two independent experiments.
Figures 7A-7C. Reduction in SOCS-I gene activation by HSV-I ICPO mutant in HEL-30 keratinocytes. (Figure 7A). HEL-30 cells were cultured overnight in 24-well plates and treated with indicated amounts of IFNγ. Following treatment for 24 hours, cells were mock-infected or infected with HSV-I at an moi of 0.1. Plates were incubated 48 hours, washed with PBS, fixed and stained with crystal violet. Absorbance units of each well were calculated using Multi-Gauge. Values are expressed as percent cell survival relative to mock-infected controls. Values are representative of duplicate wells of two independent experiments. (Figure 7B). HEL-30 cells were cultured overnight in 24-well plates and treated with 100 U/ml IFN γ alone and with different concentrations of Tkip. Following treatment for 24 hours, cells were mock-infected or infected with HSV-I
ICPO mutant at an moi of 0.1. Plates were incubated 48 hours, washed with PBS, fixed and stained with crystal violet and absorbance measured as in (Figure 7A). There were statistically significant differences between IFNγ, Tkip, IFNγ + HSV-I and Tkip + HSV- 1 when compared to the untreated cells (P < 0.001) as determined by Mann-Whitney signed rank test. (Figure 7C). HEL-30 cells were cultured overnight in 12-well plates and transfected with a luciferase reporter construct containing the full-length SOCS-I promoter. Cells were incubated for 24 hours and then mock-infected or infected with HSV-I or HSV ICPO mutant at moi of 2 for 4 hours. Cell lysates were collected and luciferase activity was measured in a single-tube lurninometer. Values given are expressed as luciferase units measured from the SOCS-I reporter divided by luciferase units measured from a co-transfected constitutive reporter and subsequently normalized to medium controls. Values are representative of triplicate wells of the two independent experiments.
Figure 8. pJAK2(1001-1013) synergizes with IFNγ to protect RAW264.7 murine macrophages against HSV-I. Murine macrophage cell line RAW264.7 was treated with IFNγ, pJAK2(1001-1013). IFNγ and different concentrations of pJAK2(1001-1013), or IFNγ and different concentrations of an alanine substituted mutant pJAK2(1001-1013)2A, followed by infection with HSV-I at an moi of 0.1. Plates were incubated 48 hours, washed with PBS, fixed and stained with crystal violet. Absorbance units of each well were calculated using Multi-Gauge. Values are expressed as percent cell survival relative to mock-infected controls. Values are representative of duplicate wells of two independent experiments. There were statistically significant differences between different concentrations of pJAK2 peptide and IFNγ when compared to untreated cells (P < 0.001) as determined by Mann-Whitney signed rank test. Figure 9. Phospho-JAK2 can rescue mice from an intranasal infection with vaccinia virus. Mice (C57BL/6, n=5) were pre-treated on days -2, -1 , and 0 with 200 ug (o), 50 ug (T), or 10 ug (o) of lipo-phospho-JAK2 peptide, or 200 μg (Δ) of a control peptide, lipo-IFNγ(95-125). On day 0, vaccinia virus (2 x 106 pfu) was given intranasally. Survival of mice was followed over a period of 30 days. The significance of difference between different treatments was measured by log rank survival method, which gave P values of 0.002, 0.002. and 0.02 for the administration of 200, 50, and 10 μg of lipo- pJAK2(1001-1013) versus the control peptide, respectively.
Figure 10. Phospho-JAK2 and IFNγ(95-132) act synergistically. Mice were pre- treated on days -2, -1, and 0 with 10 μg of pJAK2 (o). 2 μg of IFN mimetic (0), 5 μg of IFN mimetic (A), a control peptide (■), or treated in combination of 10 μg of pJAK2 and 2 μg of IFN mimetic (▼), or 10 μg of pJAK2 and 5 ug of IFN mimetic (o). On day 0, mice were infected intranasally with 1 x 106 pfu of vaccinia virus. Survival of mice was followed over a period of 30 days. The significance of difference between different treatments was measured by log rank survival method, which gave P values of 0.002, 0.04, 0.012, 0.017, and 0.017 for the administration of 10 μg pJAK2 and 5 μg IFN mimetic, 10 μg pJAK2 and 2 μg IFN mimetic, 5 μg of IFN mimetic, 2 μg IFN mimetic, and 10 μg pJAK2 versus the control peptide, respectively.
Figure 11. IFNγ mimetic and pJAK2 peptides activate GAS promoter element synergistically. WISH cells were co-transfected with plasmids expressing a GAS promoter element linked to a firefly luciferase and another plasmid expressing Renilla luciferase an internal control, followed by addition of the peptides indicated. After overnight incubation, relative luciferase activity was measured, and is expressed as average ± s.d.
Figures 12A and 12B. Time course of inhibition of vaccinia virus replication by pJAK2(1001-1013) by one-step growth curve. BSC-40 cells grown to confluency were left untreated, or treated with lipo- pJAK2(1001-1013), or its alanine substituted mutants at 50 μM for one hour. Cells were then infected with vaccinia virus at a moi of 5 for one hour. After one hour, the cells were washed and incubated in the presence of the same concentrations of peptides for the indicated times. Cell extracts (Figure 12A) and supernatants (Figure 12B) obtained from these were titrated for the amount of intracellular and extracellular virus, respectively. Note the difference of the scale on y axis, indicating that there is less of extracellular virus than intracellular.
Figures 13A and 13B. pJAK2(1001-1013) inhibits vaccinia virus replication in a dose-dependent manner as determined by a one-step growth curve. BSC-40 cells were grown to confluency and left untreated or treated with the indicated amounts of lipo- pJAK2(1001-1013) or the alanine substituted control peptide for one hour. Cells were next infected with vaccinia virus at a moi of 5. After one hour, the cells were washed and incubated in the presence of the same concentrations of peptides for one day. Supernatant
and cell extracts obtained were titrated for the amount of intracellular (Figure 13A) and extracellular (Figure 13B) virus, respectively.
Figures 14A-14C. pJAK2(1001-1013) treated cells had increased levels of endogenous IFNB. In Figure 14A, pJAK2(1001-1013) increases levels of endogenous TFNβ. L929 cells were seeded onto 6-well plates at 1 x 106 cells/well, grown to confluency and treated with peptides at varying concentrations for 30 or 60 min at 37°C. The cells were washed and lysed and whole cell extracts were resolved on 12% SDS- PAGE, transferred onto a nitrocellulose membrane, and probed with anti-IFNβ antibodies. In Figure 14B, pJAK2(1001-1013) has no effect on endogenous IFNα levels. L929 cells were seeded onto 6-well plates at 1 x 106 cells/well, grown to confluency and treated with peptides at varying concentrations for 30 or 60 min at 370C. The cells were washed and lysed and whole cell extracts were resolved on 12% SDS-PAGE, transferred onto a nitrocellulose membrane, and probed with anti-IFNα antibodies. In Figure 14C, pJAK2(1001 -1013) decreased levels of endogenous SOCS-I. L929 cells were seeded onto 6-well plates at 1 x 106 cells/well, grown to confluency and treated with peptides at varying concentrations for 30 or 60 min at 370C. The cells were washed and lysed and whole cell extracts were resolved on 12% SDS-PAGE, transferred onto a nitrocellulose membrane, and probed with anti-SOCSl-KIR antibodies.
Figures Ϊ5A-15F. Adaptive immune response in mice that recovered from vaccinia virus infection with pJAK2(1001-1013) treatment. Figure 15A shows survival of mice against rechallenge with vaccinia virus. Naive mice (J ) (n=5) or those that had recovered from vaccinia virus infection with pJAK2(1001-1013) treatment for 30 days (T), were infected intranasally with 2 x IQ6 pfu of vaccinia virus in 10 μl. Survival was followed for 4 weeks. The significance of difference as measured by log rank survival was p = 0.0002 for the rechallenged group vs the naϊve mice. Figure 15B shows cell mediated immune response in mice that recovered from vaccinia virus infection with pJAK2(1001 -1013) treatment. Splenocytes (105) from naϊve or recovered mice (n = 3), 2 or 3 wks after infection and pJAK2(1001-1013) treatment, were incubated with UV- inactivated purified vaccinia virus. Four days later, [3H] thymidine was added for 8 hours, and its incorporation was followed. Stimulation index refers to the incorporation in splenocytes cultured with test antigen divided by incorporation in splenocytes cultured with medium alone. The averages with s.d. are shown. In Figure 15C, vaccinia virus-
specific response in CD4 depleted splenocytes by ELISPOT analysis. Splenocytes from naϊve or recovered mice (n = 3), 3 weeks after infection with pJAK2(10Ql -1013) treatment were depleted of CD4 cells and 105 cells thus obtained were incubated in microtiter plates, previously coated with antibody to IFNγ in the presence of vaccinia virus (moi = 0.01). After 2 days of incubation, the number of spots (IFNγ secreting cells) per well were counted. The numbers represent the average with s.d. Figures 15D and 15E: Presence of vaccinia virus specific antibodies in mice that recovered from infection with pJAK2(l 001-1013) treatment. Sera collected from naϊve mice (n = 3) or those recovered from vaccinia virus infection with pJAKL2(1001-1013) treatment were collected in the weeks indicated. Sera were diluted as indicated and added to wells of microtiter plates coated with UV-inactivated vaccinia virus. After washing to remove nonspecific binding, secondary anti-mouse IgA (Figure 15D), or IgG (Figure 15E) antibody conjugated to HRP was added, followed by the addition of OPD substrate and absorption measurement. The values represent the average with s.d. Figure 15F: Neutralizing antibodies in recovered mice. Sera taken from naϊve mice (n = 3), or those recovered from vaccinia virus infection with pJAK2(1001-1013) treatment in the weeks indicated were diluted as shown, mixed with vaccinia virus (pfu = 100), incubated for 1 hour, followed by addition to BSC-40 cells. One hour later, regular growth medium was added to cells and incubated for two days. Reduction in the number of plaques is shown as percentage with s.d.
Figures 16A-16C. pJAK2(1001-1013) exerts an adjuvant effect at both cellular and humoral levels. Figure 16A shows splenocyte stimulation. Mice (C57BL/6, n=5) were pre-treated LP. on day -2, -1 and 0 with 200 μg each of pJAK2, control peptide, or PBS in a volume of 100 μl. On day 0, 50 μg of BSA (in 100 μl) was injected in mice in all groups, except the naϊve group. Four weeks later spleens were extracted. Isolated splenocytes (5 x 106 per well) were seeded in quadruplicate in 96 well plate and incubated with 0.5 μg of BSA for three days with the addition of 1 μCi per well of 3H-thymidine for the last 6 hours. Cells were transferred to filter and counted in a scintillation counter. Data are representative of three individual experiments. Figure 16B shows IgG production. Mice (C57BL/6, n=5) were pre-treated LP. on day -2, -1 and 0 with 200 μg or 66 μg each of pJAK2, control peptide, or PBS in a volume of 100 μl. On day 0, 50 μg of BSA (in 100 μl) was injected LP. into mice in all groups, except the naϊve group. After 2.
3 and 4 weeks mice were bled and sera isolated. 1 :1000 dilutions of sera were added to microtiter plates and IgG antibodies were measured in an ELISA assay. Figure 16C shows stimulation of macrophages. RAW 264.7 cells (5 x 106 per well) were seeded in triplicate in microtiter plates and incubated overnight. The indicated amounts of pJ AK2 or control peptide were added to the cells and incubated for 4 h. after which 2 μg pf LPS were added and the cells were incubated for 3 days. Nitric oxide was measured by Griess reagent and absorbance was read in a plate reader.
Figures 17A-17C. pJAK2(1001-1013) possesses antiviral activity against EMCV. In Figure 17A, mouse L929 cells were plated and grown to confluence on a 96-well plate. Various concentrations of mouse IFNγ, IFNγ(95-125), IFNγ(95-132), pJAK2 [pJAK2(1001-1013)] and JAK2m [pJAK2(1001-1013)2A] peptides were incubated with L929 cells for 2 h, after which 200 pfu/well of EMCV were added. After 1 h, virus was removed and media were added to all wells, followed by incubation for 24 h. Cells were stained with crystal violet solution, and plates were scanned and analyzed to assess cell survival. Image J software was used to analyze the image to obtain gray value to assess cell survival, presented here as percentages of the medium control value (100% cell survival). Data are representative of at least three experiments. Error bars indicate standard error of the means, hi Figure 17B, for extracellular antibody neutralization, cells were incubated with the peptides in the presence or absence of 500 U/ml of neutralizing antibody to IFNB for 2 h, after which 200 pfu/well of EMCV were added. After 1 h, virus was removed and media were added to all wells, followed by incubation for 24 h. Cells were stained with crystal violet solution, and plates were scanned and analyzed to assess cell survival as above. Data are representative of at least three experiments. Error bars indicate standard error of the means. In Figure 17C, pJAK2(1001-1013) protected C57B1/6 mice from lethal EMC virus infection. Mice were injected daily LP. beginning at day -2 with pJAK2(l 001-1013) at 50, 100, and 200 μg and alanine substituted antagonist JAK2(1001-1013)m at 200 μg. The mice were injected LP. with 50 pfu EMC virus per mouse on day 0. The mice (n = 5) were monitored daily for survival. Survival data arc presented as Kaplan-Meier plots. The significance of difference between antagonist treatment versus the alanine-substituted mutant was measured by log-rank survival method and gave values ofp < 0.005, < 0.005, and KS for doses of 200, 100, and 50 μg versus the mutant control, respectively.
Figure 18 shows that SOCS antagonist and IFN mimetic possess antiviral activity against influenza virus. MDCK cells were treated with the above peptides at 2 μM for 18 hours. Cells were infected with influenza A/PR8 virus (103 TCID50/ml), and incubated for 1 hour at 35°C. The media was removed and replaced with infection media, and the cells were incubated for an additional 24 hours at 35°C. The cells were stained with crystal violet and absorbance was measured. Data from three replicates.
Figure 19 shows HA inhibition of influenza A PR8 by IFN -γ mimetic and SOCS- 1 antagonist. MDCK cells were treated with peptides for 2 hours, then challenged with influenza A/PR8 virus and incubated at 350C for 36 hours. The supernatants were collected and a standard hemagglutination assay was performed in triplicate. The data are presented as hemagglutination units/ml ± SEM and are representative of three independent experiments.
Figure 20 shows pJAK2(1001-1013) can rescue mice from an intranasal infection with vaccinia virus. Mice (C57BL/6, n=5) were pre-treated on days -2, -1, and 0 with 200 μg (D), 50 μg (▼), or 10 μg (o) of lipo-p-JAK2(l 001-1013) peptide, or 200 μg (Δ) of a control peptide, lipo-JAK2(1001-1013)2A. On day 0, vaccinia virus (2 x 106 pfu) was given intranasally. Survival of mice was followed over a period of 30 days. The significance of difference between different treatments was measured by log rank survival method, which gave P values of 0.002, 0.002, and 0.02 for the administration of 200, 50, and 10 μg of lipo-pJAK2( 1001-1013) versus the control peptide, respectively.
Figures 21A and 21B show that lipo-pJAK2(1001-1013) is internalized by mouse peritoneal cells in vivo and by L929 fibroblast cells in culture. Lipo-pJAK2(l 001 -1013) was coupled to FlTC as per Materials and Methods. Figure 21 A shows peritoneal cell uptake. Mice were injected i.p. with 15 μg FITC-lipo- pJAK2(1001-1013) or an equivalent amount of FITC alone. Peritoneal cells were harvested after two hours and the cells were examined by confocal fluorescent and contrast microscopy for FITC labeling. Figure 21B shows L929 cells uptake. Cells were incubated with 5 μM of FlTC-lipo- pJAK2(1001-1013) or an equivalent amount of FITC alone for two hours, after which they were examined as above for uptake of FITC. Figures 22A-22E show pJAK2(1001-1013) exerts an adjuvant effect at both cellular and humoral levels. Figure 22A shows splenocyte stimulation. Mice (n=5) were pre-treated i.p. on day -2, -1 and 0 with pJAK2(1001-1013), control peptide JAK2(1001-
1013)2A, or PBS. On day 0, 50 μg of BSA was injected in mice in all groups, except the naϊve group. Four weeks later isolated splenocytes (5 x 10 per well) were seeded in quadruplicate and incubated with 0.5 μg of BSA for 3 days with the addition of 1 μCi per well of [3H] -thymidine for the last 6 hours and its incorporation was measured. Data are representative of three individual experiments. Figure 22B shows IgG production. Mice (n=5) were treated as in Figure 22A. Sera obtained in the weeks indicated were diluted (1 :1000) and added to microtiter plates. IgG antibodies were measured in an ELISA assay. Figure 22C shows SOCS antagonist enhances T cell-independent Ab production. Mice (C57BL6, n=3) were injected i.p. with T cell-independent Ag, LPS (50 μg each), or the T cell-dependent Ag, BSA (50 μg). Some of the mice received SOCS antagonist (200 μg), the control peptide (JAK2A) (200 μg), or a combination of SEA/SEB (SAg, 25 μg each). A set of mice were also injected with BSA (50 μg) and SAg. Two weeks later, mice Λvere bled. Sera were tested for IgG to LPS or BSA by ELISA. The secondary Ab used was anti-mouse IgG conjugated to HRP. After washing, substrate was added and color was allowed to develop before reading absorbance at 490 nm. Comparison of LPS versus LPS and SOCS antagonist by Student's t test resulted in p < 0.01 at 1/100 dilution. Figure 22D shows LPS stimulation. RAW264.7 cells (5 x 106 per well) were seeded in triplicate and incubated overnight. The indicated amounts of pJAK2(1001-1013) or control peptide, were added to the cells and incubated for 4 h, after which 2 μg/ml of LPS was added and the cells were incubated for 3 days. Nitric oxide was measured by Griess reagent and absorbance was read. *P<0.001. Figure 22E shows Poly I:C stimulation. Murine macrophages (RAW264.7) were incubated with lipophilic pJAK2(1001-1013), or control peptide for 2 h, followed by stimulation with poly 1:C at 0.1 μg/ml for 72 h. Culture supematants were collected and nitrite concentration determined using Griess reagent. ** p < 0.0001.
Figures 23A-23D show pJAK2(l 001-1013) binding to SOCSl-KIR and SOCS3- KIR as determined by an antibody ELISA and its reversal of SOCS-I and SOCS-3 mediated inhibition of GAS promoter activity. SOCSl-KIR (Figure 23A) and SOCS3- KIR (Figure 23B) bind to pJAK2(1001-1013). pJAK2 or control peptide IFNγ(95-106) was immobilized at 3 μg per well in a 96 well plate. Following blocking, various concentrations of SOCSl-KIR or SOCS3-KIR were added and the plates were incubated for 1 hour. Following washing, 1 :500 dilution of SOCSl-KIR or SOCS3-KIR antibody
was added for 1 hour incubation. Bound SOCS peptide was detected with a goat anti- rabbit IgG-HRP conjugate, followed by the addition of OPD substrate and 2N H2SO4. Absorbance was measured in a plate reader. The statistical significance of the binding was tested by a paired t-test and p values of < 0.001 and 0.0166 for the binding in A and B, respectively were observed. Figure 23C shows pJAK2(1001-1013) reverses SOCS-I and SOCS-3 inhibition of GAS promoter activity. L929 cells were transfected with a GAS promoter linked to firefly iuciferase reporter gene and a control plasmid with constitutively expressed Renilla Iuciferase. Where indicated SOCS-I or SOCS-3 expressing plasmids were included in the transfection. A plasmid without a promoter attached to firefly Iuciferase was used as a control in the first bar indicated as empty vector. After 24 hr of transfection, cell extracts were assayed for relative Iuciferase activities. pJAK2 peptide was used at 30 μM. Figure 23D shows JAK2 associates with SOCS-3 in cells. Whole cell extracts of L929 cells were immunoprecipitated (IP) with antibodies to JAK2. Western blot analysis of the immunoprecipitates showed association of SOCS-3. IP with nonspecific IgG was run as a control and showed no SOCS-3 association.
Figure 24. pJAK2(1001-1013)-treated cells had increased levels of phosphorylated STATIa. L929 cells were seeded onto six-well plates at 1 x 106 cells/well, grown overnight, and treated with pJAK2(1001-1013) (2, 10, 25 μM) or JAK2(1001-1013)2A (25 μM) for 1 h at 37 0C. The cells were washed and lysed, and whole-cell extracts were resolved on 12% SDS-PAGE, transferred onto nitrocellulose membrane, and probed with antibodies to pSTATla or STATIa. Similar results were obtained in three different experiments. Relative intensities of the pSTATl a band are shown under the blot. As determined by the unpaired t test on non-normalized readings, the intensity in the pJAK2-treated band versus the untreated had ap value of 0.0002.
Figure 25 shows synergy between SOCS-I antagonist and IFN-γ mimetic in inhibition of EMC virus. pJAK2(1001-1013) at 2 μM and IFN-γ(95-132) at 5 μM together were incubated with L929 cells, after which 200 PFU/well EMC virus was added. After 1 hour, virus was removed and media was added, followed by incubation for 24 hours. Cells were stained with crystal violet and plates were scanned. National Institutes of Health ImageJ software was used for analysis.
Figure 26 shows synergy in protection of mice infected with EMC virus using suboptimal levels of pJAK2(10ϋl-1013) (10 μg) and ΪFN-γ(95-132) (2 μg). Mice were injected daily i.p. beginning at day -2 with pJAK2(1001-1013) at 50, 100, and 200 μg and control peptide at 200 μg. On day 0, 50 PFU/mouse was injected i.p. Survival data are presented as Kaplan-Meier plots. The significance of difference were/? < 0.005, < 0.005, and NS for 200, 100, and 50 μg of antagonist versus the control, respectively.
BRIEF DESCRIPTION OF THE SEQUENCES
SEQ ID NO:1 is an amino acid sequence of a pJAK2(1001 -1013) peptide of the present invention.
SEQ ID NO:2 is an amino terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:3 is an amino terminal deletion of the amino acid sequence shown in SEQ ID NO: 1. SEQ ID NO:4 is an amino terminal deletion of the amino acid sequence shown in
SEQ ID NO: 1.
SEQ ID NO:5 is an amino terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:6 is an amino terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:7 is a carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:8 is a carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO: 1. SEQ ID NO:9 is a carboxy terminal deletion of the amino acid sequence shown in
SEQ ID NO: 1.
SEQ ID NOtIO is a carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:11 is a carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO: 12 is an amino and carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO:1.
SEQ ID NO: 13 is an amino and carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO:1.
SEQ ID NO: 14 is an amino and carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO:1. SEQ ID NO:15 is an amino and carboxy terminal deletion of the amino acid sequence shown in SEQ ID NO:1.
SEQ ID NO:16 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO: 17 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO:l .
SEQ ID NO: 18 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO: 19 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1. SEQ ID NO:20 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:21 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO: 22 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:23 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:24 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1. SEQ ID NO:25 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO:!.
SEQ ID NO:26 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:27 is an amino teπninal addition of the amino acid sequence shown in SEQ ID NO:!.
SEQ ID NO:28 is an amino teπninal addition of the amino acid sequence shown in SEQ ID NO:!.
SEQ ID NO:29 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:30 is an amino terminal addition of the amino acid sequence shown in SEQ ID NO: 1. SEQ ID NO:31 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:!.
SEQ ID NO:32 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:33 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:! .
SEQ ID NO:34 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:35 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1. SEQ ID NO:36 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:37 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO.38 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NOt39 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NQ:40 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1. SEQ ID NO:41 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:42 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:43 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:44 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:!.
SEQ ID NO:45 is a carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:!.
SEQ ID NO:46 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1. SEQ ID NO:47 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
SEQ ID NO:48 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
SEQ ID NO:49 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:50 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
SEQ ID NO:51 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1. SEQ ID NO:52 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
SEQ ID NO: 53 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
SEQ ID NO: 54 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO: 55 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:56 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1. SEQ ID NO:57 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:58 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:59 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO: 1.
SEQ ID NO:60 is an amino and carboxy terminal addition of the amino acid sequence shown in SEQ ID NO:1.
SEQ ID NO:61 is the amino acid sequence of a peptide designated herein as Tkip.
SEQ ID NO:62 is the amino acid sequence of a peptide designated herein as Tkip. SEQ ID NO:63 is the amino acid sequence of a peptide designated herein as
SOCSl-KIR.
SEQ ID NO:64 is the amino acid sequence of a peptide designated herein as SOCS1-KIR2A.
SEQ ID NO:65 is the amino acid sequence of a peptide designated herein as MuIFNγ(95-106).
SEQ ID NO:66 is the amino acid sequence of a peptide designated herein as MuIFNγ(95-125).
SEQ ID NO:67 is the amino acid sequence of a peptide designated herein as MuIFNγ(95-132). SEQ ID NQ:68 is the amino acid sequence of a peptide designated herein as
MuIFNGRl(253-287).
SEQ ID NO:69 is the amino acid sequence of a peptide designated herein as MAL Box 1.
SEQ ID NO: 70 is the amino acid sequence of a peptide designated herein as MAL 159.
SEQ ID NO:71 is the amino acid sequence of a peptide designated herein as JAK2(1001-1013)m.
SEQ ID NO:72 is a nucleotide sequence of a forward primer for human SOCS-I promoter. SEQ ID NO:73 is a nucleotide sequence of a reverse primer for human SOCS-I promoter.
SEQ ID NO:74 is a nucleotide sequence of a GAS promoter element of a human IRF-I gene.
SEQ ID NO: 75 is the amino acid sequence of a peptide designated herein as huIFNγ (95-134).
SEQ ID NO: 76 is the amino acid sequence of a peptide designated herein as SOCS3-KIR.
DETAILED DESCRIPTION OF THE INVENTION
The subject invention concerns materials and methods for inhibiting activity and/or replication of a broad spectrum of viruses in humans and animals. In one embodiment of the invention, a method is provided for treating or preventing viral infection in a human or animal by administering an effective amount of peptide, or a polynucleotide encoding the peptide, or a peptidomimetic, that is an antagonist of SOCS- 1 and/or SOCS-3, or a composition comprising one or more of the peptide, peptidomimetic, or polynucleotide. In a specific embodiment, the peptide corresponds to the activation loop of janus kinase JAK2. In an exemplified embodiment, the peptide comprises the amino acid sequence: 10111LPQDKEYYKVKEP1013 (pJAK2 (1001-1013)) (SEQ ID NO:1), or a fragment or variant thereof that exhibits antiviral activity. In a specific embodiment, the tyrosine at amino acid position 7 of SEQ ID NO:1 (which corresponds to the tyrosine at residue 1007 of JAK2) is phosphorylated. In another embodiment, an effective amount of a polynucleotide encoding a peptide of the invention is administered to a person or animal in need of treatment. In one embodiment, the polynucleotide is provided in an expression construct. In a specific embodiment, the polynucleotide encodes a peptide comprising the amino acid sequence shown in SEQ ID NQ: 1, or a fragment or variant thereof that exhibits antiviral activity. Examples of viruses whose activity and/or replication can be inhibited using the present invention include, but are not limited to, herpes viruses, poxviruses, and picornaviruses, such as vaccinia virus. EMC virus, influenza virus, herpes zoster virus, cytomegalovirus, and herpes simplex virus (e.g., HSV-I). In a specific embodiment, the influenza virus is an influenza A virus. In a more specific embodiment, the influenza A virus is serotype HlNl. In addition to treating a human or animal having a viral infection, the subject invention can also be used to prevent viral infection in an uninfected human or animal.
The subject invention also concerns peptides that are an antagonist of SOCS-I and/or SOCS-3 protein, and compositions comprising the peptides. In a specific embodiment, the peptide corresponds to the activation loop of janus kinase JAK2. In an exemplified embodiment, the peptide comprises the amino acid sequence: 1001LPQDKEYYKVKEP1013 (pJAK2 (1001-1013)) (SEQ ID NO:1), or a fragment or variant thereof that exhibits antiviral activity. In a specific embodiment, the tyrosine at
amino acid position 7 of SEQ ID NO:1 (i.e., the tyrosine that is underlined in the sequence LPQDKEYYKVKEP) is phosphorylated (this corresponds to the tyrosine at position 1007 of JAK2 protein sequence). In one embodiment, a peptide of the invention consists of the amino acid sequence shown in SEQ ID NO: 1, and optionally wherein the tyrosine at position 7 is phosphorylated. Peptides of the invention can be readily prepared using standard techniques known in the art, including chemical synthesis (Merrifield, 1963) and genetic engineering.
The subject invention also concerns non-peptide compounds (peptidomimetics) that mimic the function of peptides of the present invention and that can be used in the methods of the present invention. Methods for preparing peptidomimetics based on structural features of the amino acid sequence of a peptide that pertain to functional or binding properties are known in the art (Kazmierski (1998)).
The subject invention also concerns polynucleotides that encode the peptides of the invention and their use in the methods of the present invention. Methods and materials for synthesizing and preparing a polynucleotide encoding a peptide of the invention are well known in the art. Because of the degeneracy of the genetic code, a variety of different polynucleotide sequences can encode a peptide of the present invention. In addition, it is well within the skill of a person trained in the art to create alternative polynucleotide sequences encoding the same, or essentially the same, peptides of the subject invention. These variant or alternative polynucleotide sequences, and the peptides encoded thereby, are within the scope of the subject invention. As used herein, references to "essentially the same" sequence refers to sequences which encode amino acid substitutions, deletions, additions, and/or insertions which do not materially alter the functional activity of the peptide encoded by the polynucleotides of the present invention. Variant peptides having amino acid substitutions, deletions, additions, and/or insertions which do not materially alter the functional antiviral activity of the peptide can also be prepared using standard techniques known in the art, and such variant peptides are encompassed within the scope of the present invention. Polynucleotide sequences encoding a peptide of the invention can be selected based on preferred codon usage of the animal in which it is to be administered. For example, if the peptide is to be administered to a human, the polynucleotide sequence can be selected for preferred codon usage in human cells.
The subject invention also concerns compositions comprising one or more peptides, peptidomimetics., or polynucleotides of the invention. In one embodiment, a composition further comprises a suitable carrier, diluent, or buffer. Compositions contemplated within the scope of the invention can comprise one or more peptides, peptidomimetics, or polynucleotides of the invention and, optionally, one or more other antiviral compounds. For example, the pJAK2 peptide can be provided in a composition with one or more of IFNα, IFNβ, IFNγ, acyclovir (Zovirax), zidovudine (AZT), lamivudine (3TC), zanamivir (Relenza), oseltamivir (Tamiflu), valacyclovir (Valtrex), amantadine (Symmetrel), rimantadine (Flumadine), cidofovir (Vistide), foscamet (Foscavir), ganciclovir (Cytovene), ribavirin (Virazole), nelfmavir (Viracept), ritonavir (Norvir), rifampin (Rifadin), and famciclovir (Famvir). In one embodiment, the composition comprises a peptide of the invention in a pharmaceutically or physiologically acceptable carrier, buffer, or diluent. Compositions of the invention can also comprise peptides such as an IFNγ mimetic. Examples of IFNγ mimetic peptides are described in U.S. Patent Nos. 5,770,191 and 6,120,762. In one embodiment, the IFNγ mimetic peptide comprises the amino acid sequence shown in SEQ ID NO:67 or SEQ ID NO:75, or a fragment or variant thereof that exhibits antiviral activity. In one embodiment, a composition of the invention can also comprise one or more peptides comprising the amino acid sequence shown in SEQ ID NO:61 (Tkip peptide), or a fragment or variant thereof that exhibits antiviral activity, and/or a peptide comprising the amino acid sequence shown in SEQ ID NO:63 (SOCSl-KIR), or a fragment or variant thereof that exhibits antiviral activity.
The methods of the invention contemplate that a peptide, polynucleotide, peptidomimetic, composition or other agent of the invention is administered to the person or animal prior to infection by a virus. Also contemplated within the scope of the methods is that a peptide, polynucleotide, peptidomimetic, composition, or other agent of the invention is administered at the time of infection or after the person or animal has been infected. In one embodiment, a person or animal to be treated is one that has previously been vaccinated against infection by a virus, such as a poxvirus. In another embodiment, the person or animal has not been previously vaccinated against the virus.
In one embodiment, peptides, polynucleotides, and peptidomimetics of the invention are modified so as to enhance uptake into a cell. In one embodiment, a
lipophilic group is attached to a peptide, polynucleotide, peptidomimetic. or other agent of the invention. In an exemplified embodiment, a palmitoyl-lysine group is attached to the peptide, for example at the N-terminus of the peptide. Other methods for enhancing uptake of a peptide, polynucleotide, or peptidomimetic into a cell are known in the art and are contemplated within the scope of the invention.
Peptides, polynucleotides, peptidomimetics, compositions, and other agents of the invention can also be delivered into cells by encapsulation of the peptide, polynucleotide, peptidomimetics, and other agents of the invention within a liposome. Methods for encapsulation of peptides, polynucleotides, peptidomimetics, and other agents of the invention within liposomes are well known in the art.
The subject invention also concerns methods for inducing an antiviral state in a cell. In one embodiment, a cell is contacted with an effective amount of a peptide, polynucleotide, peptidomimetic, or a composition of the invention. In one embodiment, the peptide comprises the amino acid sequence of SEQ ID NO:1, or a fragment or variant thereof that exhibits antiviral activity. In a specific embodiment, the tyrosine at amino acid position 7 of SEQ ID NO:1 (which corresponds to the tyrosine at position 1007 (i.e., the tyrosine that is underlined in the sequence LPQDKEYYKVKEP)) is phosphorylated. In one embodiment, a peptide of the invention consists of the amino acid sequence shown in SEQ ID NO:1, wherein the tyrosine at position 7 is phosphorylated. In one embodiment, the composition comprises a peptide of the invention and an antiviral drug and/or a IFNγ mimetic. The cell can be a human or mammalian cell. In one embodiment, the cell can be a keratinocyte, a fibroblast, a macrophage, or a lymphocyte. Peptides, polynucleotides, peptidomimetics, and/or other agents of the invention can be delivered to a cell either through direct contact of peptide, etc. with the cell or via a carrier means. Carrier means for delivering compositions to cells are known in the art and include encapsulating the composition in a liposome moiety, and attaching the peptide, polynucleotide, or peptidomimetic to a protein or nucleic acid that is targeted for delivery to the target cell. Published U.S. Patent Application Nos. 20030032594 and 20020120100 disclose amino acid sequences that can be coupled to another peptide, protein, or nucleic acid and that allows the peptide, protein, or nucleic acid to be translocated across biological membranes. Published U.S. Patent Application No. 20020035243 also describes compositions for transporting biological moieties, such as
peptides and proteins across cell membranes for intracellular delivery. Peptides can also be delivered using a polynucleotide that encodes a subject peptide. In one embodiment, the polynucleotide is delivered to the cell where it is taken up and the polynucleotide is transcribed into RNA and the RNA is translated into the encoded peptide. Antiviral activity can be induced in a cell against viruses such as vaccinia virus, EMC virus, influenza virus, herpes simplex virus (e.g., HSV-I). cytomegalovirus, herpes zoster virus, and other herpes viruses, poxvirus, coxsackie virus, lentivirus (e.g., HIV), and picornavirus.
The subject invention also concerns methods for treating a disorder in a person or animal comprising administering an effective amount of a peptide, polynucleotide, peptidomimetic, composition, or other agent of the invention to the person or animal, wherein the disorder is associated with a SOCS protein, such as SOCS-I and/or SOCS-3 protein. In one embodiment, the disorder is characterized by aberrant, constitutive, or elevated expression of a SOCS-I and/or SOCS-3 protein. The subject invention also concerns methods for modulating an immune response in a person or animal, wherein the method comprises administering an effective amount of a peptide, polynucleotide, peptidomimetic, composition, or other agent of the invention to the person or animal. In one embodiment, the immune response involves expression and/or activity of a SOCS-I and/or SOCS-3 protein. The immune response can also involve expression and activation of a JAK and/or a STAT protein. In one embodiment, SOCS-I induced inhibition of STAT3 activation is blocked using a peptide, polynucleotide, peptidomimetic, composition, or other agent of the invention. In a further embodiment, inhibition of JAK2 kinase activity by a SOCS protein (e.g., SOCS-I or SOCS-3) is blocked or inhibited using the subject invention. In one embodiment, the method enhances or increases the person's or animal's immune response against a tumor or cancer cell (or antigen thereon) or a virus (or an antigen thereof). In a specific embodiment, the person or animal is infected with an immunodeficiency virus (e.g., human immunodeficiency virus (HIV)) and the method enhances or increases the person's or animal's immune response against the virus. Peptides useful in the methods of the subject invention include the specific peptides exemplified herein as well as equivalent peptides which may be. for example, somewhat longer or shorter than the peptides exemplified herein. For example, using the
teachings provided herein, a person skilled in the art could readily make peptides having from 1 to about 15 or more amino acids added to one or both ends of a peptide of the subject invention. Examples of peptides having amino acids added to one or both ends of the exemplified peptide (SEQ ID NO:1) and contemplated within the scope of the present invention are shown in SEQ ID NO: 16 to SEQ ID NO:60. Similarly, a person skilled in the art could readily prepare peptides in which 1 to about 5 amino acids are removed from one or both ends of a peptide of the subject invention. Examples of peptide fragments of the exemplified peptides and contemplated within the scope of the present invention are shown in SEQ ID NO:2 to SEQ ID NO:15. In addition, amino acids could be added to one end of a peptide of the invention and amino acids removed from the other end of the peptide. The subject invention includes, but is not limited to, the exemplified longer and shorter peptides.
Peptides included within the scope of the invention include peptides from about 5 to about 50 or more amino acids in length. Thus, within the scope of the invention are peptides of 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, and 50 amino acids in length. In one embodiment, peptides of the invention consist of about 10 to about 20 amino acids. In another embodiment, peptides of the invention consist of about 10 to about 15 amino acids. AU longer and shorter peptides are within the scope of the subject invention as long as the longer or shorter peptide retains substantially the same antiviral activity as the peptides exemplified herein. The subject invention also concerns polypeptides that comprise a peptide sequence of the present invention, or a fragment or variant of that sequence, and that are able to inhibit viral activity.
Peptides having substitution of amino acids other than those specifically exemplified in the subject peptides are also contemplated within the scope of the present invention. For example, non-natural amino acids can be substituted for the amino acids of a peptide of the invention, so long as the peptide having substituted amino acids retains substantially the same activity as the peptide in which amino acids have not been substituted. Examples of non-natural amino acids include, but are not limited to, ornithine, citrulline, hydroxyproline, homoserine, phenylglycine, taurine, iodotyrosine, 2,4-diaminobutyric acid, a-amino isobutyric acid, 4-aminobutyric acid, 2-amino butyric acid, γ-amino butyric acid, e-amino hexanoic acid, 6-amino hexanoic acid, 2-amino
isobutyric acid, 3 -amino propionic acid, norleucine, norvaline, sarcosine, homocitralline, cysteic acid, t -butylglycine, t-butylalanine, phenylglycine, cyclohexylalanine, β-alanine, fluoro-amino acids, designer amino acids such as β-methyl amino acids, C-methyl amino acids, N-methyl amino acids, and amino acid analogues in general. Non-natural amino acids also include amino acids having derivatized side groups. Furthermore, any of the amino acids in the protein can be of the D (dextrorotary) form or L (levorotary) form.
Amino acids can be generally categorized in the following classes: non-polar, uncharged polar, basic, and acidic. Conservative substitutions whereby a peptide having an amino acid of one class is replaced with another amino acid of the same class fall within the scope of the subject invention so long as the peptide having the substitution still retains substantially the same biological activity as a peptide that does not have the substitution. Table 1 below provides a listing of examples of amino acids belonging to each class.
Table 1.
Class of Amino Acid Examples of Amino Acids
Nonpolar Ala, VaI, Leu, He, Pro, Met, Phe, Trp Uncharged Polar GIy, Ser, Thr, Cys, Tyr, Asn, GIn
Acidic Asp, GIu Basic Lys, Arg, His
Single letter amino acid abbreviations are defined in Table 2.
The peptides of the present invention can be formulated into pharmaceutically- acceptable salt forms. Pharmaceutically-acceptable salt forms include the acid addition salts and include hydrochloric, hydrobromic, nitric, phosphoric, carbonic, sulphuric, and organic acids like acetic, propionic, benzoic, succinic, fumaric, mandelic, oxalic, citric, tartaric, maleic, and the like. Pharmaceutically-acceptable base addition salts include sodium, potassium, calcium, ammonium, and magnesium salts. Pharmaceutically- acceptable salts of the peptides of the invention can be prepared using conventional techniques.
The subject invention also concerns polynucleotide expression constructs that comprise a polynucleotide of the present invention comprising a nucleotide sequence encoding a peptide of the present invention. In one embodiment, the polynucleotide
encodes a peptide comprising the amino acid sequence shown in SEQ ID NO:1, or a fragment or variant thereof that exhibits antiviral activity.
As used herein, the term "expression construct" refers to a combination of nucleic acid sequences that provides for transcription of an operably linked nucleic acid sequence. As used herein, the term "operably linked" refers to a juxtaposition of the components described wherein the components are in a relationship that permits them to function in their intended manner. In general, operably linked components are in contiguous relation.
Expression constructs of the invention will also generally include regulatory elements that are functional in the intended host cell in which the expression construct is to be expressed. Thus, a person of ordinary skill in the art can select regulatory elements for use in. for example, bacterial host cells, yeast host cells, plant host cells, insect host cells, mammalian host cells, and human host cells. Regulatory elements include promoters, transcription termination sequences, translation termination sequences, enhancers, and polyadenylation elements.
An expression construct of the invention can comprise a promoter sequence operably linked to a polynucleotide sequence encoding a peptide of the invention. Promoters can be incorporated into a polynucleotide using standard techniques known in the art. Multiple copies of promoters or multiple promoters can be used in an expression construct of the invention. In a preferred embodiment, a promoter can be positioned about the same distance from the transcription start site as it is from the transcription start site in its natural genetic environment. Some variation in this distance is permitted without substantial decrease in promoter activity. A transcription start site is typically included in the expression construct. For expression in animal cells, an expression construct of the invention can comprise suitable promoters that can drive transcription of the polynucleotide sequence. If the cells are mammalian cells, then promoters such as, for example, actin promoter, metallothionein promoter, NF-kappaB promoter, EGR promoter, SRE promoter, IL-2 promoter, NFAT promoter, osteocalcin promoter, SV40 early promoter and SV40 late promoter, Lck promoter, BMP 5 promoter, TRP-I promoter, murine mammary tumor virus long terminal repeat promoter, STAT promoter, or an immunoglobulin promoter can be used in the expression construct. The baculovirus polyhedrin promoter can be
used with an expression construct of the invention for expression in insect cells. Promoters suitable for use with an expression construct of the invention in yeast cells include, but are not limited to, 3-phosphoglycerate kinase promoter, glyceraldehyde-3- phosphate dehydrogenase promoter, metallothionein promoter, alcohol dehydrogenase-2 promoter, and hexokinase promoter.
For expression in prokaryotic systems, an expression construct of the invention can comprise promoters such as, for example, alkaline phosphatase promoter, tryptophan (trp) promoter, lambda PL promoter, β-lactamase promoter, lactose promoter, phoA promoter, T3 promoter, T7 promoter, or tac promoter (de Boer et al, 1983). If the expression construct is to be provided in a plant cell, plant viral promoters, such as, for example, the cauliflower mosaic virus (CaMV) 35S (including the enhanced CaMV 35S promoter (see, for example U.S. Patent No. 5,106,739)) or 19S promoter can be used. Plant promoters such as prolifera promoter, Ap3 promoter, heat shock promoters, T-DNA 1 '- or 2'-promoter of A. tumafaciens, polygalacturonase promoter, chalcone synthase A (CHS-A) promoter from petunia, tobacco PR- Ia promoter, ubiquitin promoter, actin promoter, alcA gene promoter, pin2 promoter (Xu et al., 1993), maize Wipl promoter, maize trpA gene promoter (U.S. Patent No. 5,625,136), maize CDPK gene promoter, and RUBISCO SSU promoter (U.S. Patent No. 5,034,322) can also be used. Seed-specific promoters such as the promoter from a β-phaseolin gene (of kidney bean) or a glycinin gene (of soybean), and others, can also be used. Constitutive promoters (such as the CaMV, ubiquitin, actin, or NOS promoter), tissue-specific promoters (such as the E8 promoter from tomato), developmentally-regulated promoters, and inducible promoters (such as those promoters than can be induced by heat, light, hormones, or chemicals) are contemplated for use with the polynucleotides of the invention.
Expression constructs of the invention may optionally contain a transcription termination sequence, a translation termination sequence, signal peptide sequence, and/or enhancer elements. Transcription termination regions can typically be obtained from the 3' untranslated region of a eukaryotic or viral gene sequence. Transcription termination sequences can be positioned downstream of a coding sequence to provide for efficient termination. Signal peptides are a group of short amino terminal sequences that encode information responsible for the relocation of an operably linked peptide to a wide range of
post-translational cellular destinations, ranging from a specific organelle compartment to sites of protein action and the extracellular environment. Targeting a peptide to an intended cellular and/or extracellular destination through the use of operably linked signal peptide sequence is contemplated for use with the peptides of the invention. Chemical enhancers are cis-acting elements that increase gene transcription and can also be included in the expression construct. Chemical enhancer elements are known in the art, and include, but are not limited to, the CaMV 35S enhancer element, cytomegalovirus (CMV) early promoter enhancer element, and the SV40 enhancer element. DNA sequences which direct polyadenylation of the mRNA encoded by the structural gene can also be included in the expression construct.
Unique restriction enzyme sites can be included at the 5' and 3' ends of the expression construct to allow for insertion into a polynucleotide vector. As used herein, the term "vector" refers to any genetic element, including for example, plasmids, cosmids, chromosomes, phage, virus, and the like, which is capable of replication when associated with proper control elements and which can transfer polynucleotide sequences between cells. Vectors contain a nucleotide sequence that permits the vector to replicate in a selected host cell. A number of vectors arc available for expression and/or cloning, and include, but are not limited to, pBR322, pUC series, Ml 3 series, and pBLUESCRIPT vectors (Stratagene, La Jolla, CA). Polynucleotides, vectors, and expression constructs of the subject invention can be introduced into a cell by methods known in the art. Such methods include transfection, microinjection, electroporation, lipofection, cell fusion, calcium phosphate precipitation, and by biolistic methods. In one embodiment, a polynucleotide or expression construct of the invention can be introduced in vivo via a viral vector such as adeno-associated virus (AAV), herpes simplex virus (HSV), papillomavirus, adenovirus, and Epstein-Barr virus (EBV). Attenuated or defective forms of viral vectors that can be used with the subject invention are known in the art. Typically, defective virus is not capable of infection after the virus is introduced into a cell. Polynucleotides, vectors, and expression constructs of the invention can also be introduced in vivo via lipofection (DNA transfection via liposomes prepared from synthetic cationic lipids) (Feigner et al., 1987). Synthetic cationic lipids (LIPOFECTIN, Invitrogen Corp., La Jolla, CA) can be used to prepare liposomes to encapsulate a polynucleotide, vector, or expression construct of the
invention. A polynucleotide, vector, or expression construct of the invention can also be introduced in vivo as naked DNA using methods known in the art, such as transfection, microinjection, electroporation, calcium phosphate precipitation, and by biolistic methods. Polynucleotides and peptides of the subject invention can also be defined in teπns of more particular identity and/or similarity ranges with those exemplified herein. The sequence identity will typically be greater than 60%, preferably greater than 75%, more preferably greater than 80%, even more preferably greater than 90%, and can be greater than 95%. The identity and/or similarity of a sequence can be 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81 , 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, or 99% as compared to a sequence exemplified herein. Unless otherwise specified, as used herein percent sequence identity and/or similarity of two sequences can be determined using the algorithm of Karlin and Altschul (1990), modified as in Karlin and Altschul (1993). Such an algorithm is incorporated into the NBLAST and XBLAST programs of Altschul et al. (1990). BLAST searches can be performed with the NBLAST program, score = 100, wordlength = 12, to obtain sequences with the desired percent sequence identity. To obtain gapped alignments for comparison purposes, Gapped BLAST can be used as described in Altschul et al (1997). When utilizing BLAST and Gapped BLAST programs, the default parameters of the respective programs (NBLAST and XBLAST) can be used. See NCBI/NIH website.
The subject invention also contemplates those polynucleotide molecules (encoding peptides of the invention) having sequences which are sufficiently homologous with the polynucleotide sequences encoding a peptide of the invention so as to permit hybridization with that sequence under standard stringent conditions and standard methods (Maniatis, T. et al, 1982). As used herein, "stringent" conditions for hybridization refers to conditions wherein hybridization is typically carried out overnight at 20-25 C below the melting temperature (Tm) of the DNA hybrid in 6x SSPE, 5x Denhardt's solution, 0.1% SDS, 0.1 mg/ml denatured DNA. The melting temperature is described by the following formula (Beltz, G.A. et al, 1983):
Tm=81.5 C+16.6 Log[Na+]-0.41(%G+C)-0.61(% formamide)-600/length of duplex in base pairs.
Washes are typically carried out as follows:
(1) Twice at room temperature for 15 minutes in Ix SSPE, 0.1% SDS (low stringency wash).
(2) Once at Tm-20 C for 15 minutes in 0.2x SSPE, 0.1% SDS (moderate stringency wash).
As used herein, the terms "nucleic acid" and "polynucleotide sequence'" refer to a deoxyribonucleotide or ribonucleotide polymer in either single- or double-stranded form, and unless otherwise limited, would encompass known analogs of natural nucleotides that can function in a similar manner as naturally-occurring nucleotides. The polynucleotide sequences include both the DNA strand sequence that is transcribed into RNA and the RNA sequence that is translated into protein. The polynucleotide sequences include both full-length sequences as well as shorter sequences derived from the full-length sequences. It is understood that a particular polynucleotide sequence includes the degenerate codons of the native sequence or sequences which may be introduced to provide codon preference in a specific host cell. The polynucleotide sequences falling within the scope of the subject invention further include sequences which specifically hybridize with the sequences coding for a peptide of the invention. The polynucleotide includes both the sense and antisense strands as either individual strands or in the duplex.
The subject invention also concerns methods for preventing or treating a viral infection in a patient wherein the viral infection is associated with the expression of a SOCS protein, such as SOCS-I and/or SOCS-3. In one embodiment, an effective amount of a peptide, polynucleotide, peptidomimetic, and/or composition of the present invention is administered to a patient having a viral disorder and who is in need of treatment thereof. In an exemplified embodiment, the peptide comprises the amino acid sequence: 1001LPQDKEYYKVKEP1013 (pJAK2 (1001-1013)) (SEQ ID NO:1), or a fragment or variant thereof that exhibits antiviral activity. In a specific embodiment, the tyrosine at amino acid position 7 of SEQ ID NO: 1 (i.e., the tyrosine that is underlined in the sequence LPQDKEYYKVKEP) is phosphorylated (this corresponds to the tyrosine at position 1007 of JAK2 protein sequence). In one embodiment, a peptide of the invention consists of the amino acid sequence shown in SEQ ID NO:1, and optionally wherein the tyrosine at position 7 is phosphorylated. The patient can be a human or other mammal, such as a dog, cat, or horse, or other animals having the disorder. Means for
administering and formulating peptides, polynucleotides, and peptidomimetics for administration to a patient are known in the art, examples of which are described herein. Peptides, polynucleotides, peptidomimetics, and/or compositions of the invention can be delivered to a cell either through direct contact of peptide, etc. with the cell or via a earner means. In one embodiment, a peptide, etc. of the invention comprises an attached group that enhances cellular uptake of the peptide. In one embodiment, the peptide, etc. is attached to an antibody that binds to a targeted cell. In another embodiment, the peptide, etc. is encapsulated in a liposome. Peptides can also be delivered using a polynucleotide that encodes a subject peptide. Any polynucleotide having a nucleotide sequence that encodes a peptide of the invention is contemplated within the scope of the invention. In one embodiment, the polynucleotide is delivered to the cell where it is taken up and the polynucleotide is transcribed into RNA and the RNA is translated into the encoded peptide. Examples of viruses whose replication can be inhibited using the present invention include, but are not limited to, herpes viruses, poxviruses, and picomaviruses, such as vaccinia virus, EMC vims, influenza virus, herpes zoster virus, cytomegalovirus, and herpes simplex virus (e.g., HSV-I).
For the treatment of viral infections, the peptides, polynucleotides, peptidomimetics and compositions of this invention can be administered to a patient in need of treatment in combination with other antiviral substances. These other antiviral substances may be given at the same or different times as the peptides, polynucleotides, peptidomimetics, and compositions of this invention. For example, the peptides, polynucleotides, peptidomimetics, and compositions of the present invention can be used in combination with one or more viral inhibitors such as interferons, and/or other drugs or antibodies, such as IFNα, IFNβ, IFNγ, acyclovir (Zovirax), zidovudine (AZT), lamivudine (3TC), zanamivir (Relenza), oseltamivir (Tamiflu), valacyclovir (Valtrex), amantadine (Symmetrel), rimantadine (Flumadine), cidofovir (Vistide), foscarnet (Foscavir), ganciclovir (Cytovene), ribavirin (Virazole), nelfmavir (Viracept), ritonavir (Norvir), rifampin (Rifadin), and famciclovir (Famvir), or drug or antibody that inhibit function of a SOCS protein, such as SOCS-I and/or SOCS-3. The subject invention also concerns methods for treating oncological disorders in a patient, wherein the oncological disorder is associated with or characterized by expression of a SOCS protein, such as SOCS-I and/or SOCS-3. In one embodiment, an
effective amount of a peptide, polynucleotide, peptidomimetic, or composition of the present invention that is an antagonist of a SOCS protein is administered to a patient having an oncological disorder and who is in need of treatment thereof. In an exemplified embodiment, the peptide comprises the amino acid sequence: 1001LPQDKEYYKVKEP1013 (pJAK2 (1001 -1013)) (SEQ ID NO:1), or a fragment or variant thereof that exhibits anticancer activity. In a specific embodiment, the tyrosine at amino acid position 7 of SEQ ID NO:1 (i.e., the tyrosine that is underlined in the sequence LPQDKEYYKVKEP) is phosphorylated (this corresponds to the tyrosine at position 1007 of JAK2 protein sequence). In one embodiment, a peptide of the invention consists of the amino acid sequence shown in SEQ ID NO:1, and optionally wherein the tyrosine at position 1007 is phosphorylated. Methods of the invention can optionally include identifying a patient who is or may be in need of treatment of an oncological disorder. The patient can be a human or other mammal, such as a primate (monkey, chimpanzee, ape, etc.), dog, cat, cow, pig, or horse, or other animals having an oncological disorder. Means for administering and formulating peptides, polynucleotides, peptidomimetics, or compositions of the invention for administration to a patient are known in the art, examples of which are described herein. Oncological disorders within the scope of the invention include, but are not limited to, cancer and/or tumors of the anus, bile duct, bladder, bone, bone marrow, bowel (including colon and rectum), breast, eye, gall bladder, kidney, mouth, larynx, esophagus, stomach, testis, cervix, head, neck, ovary, lung, mesothelioma, neuroendocrine, penis, skin, spinal cord, thyroid, vagina, vulva, uterus, liver, muscle, pancreas, prostate, blood cells (including lymphocytes and other immune system cells), and brain. Specific cancers contemplated for treatment with the present invention include carcinomas, Karposi's sarcoma, melanoma, mesothelioma, soft tissue sarcoma, pancreatic cancer, lung cancer, leukemia (acute lymphoblastic, acute myeloid, chronic lymphocytic, chronic myeloid, and other), and lymphoma (Hodgkin's and non-Hodgkin's), and multiple myeloma.
Examples of cancers that can be treated according to the present invention are listed in Table 3.
Table 3. Examples of Cancer Types
Acute Lymphoblastic Leukemia, Adult Hairy Cell Leukemia
Acute Lymphoblastic Leukemia, Head and Neck Cancer
Childhood Hepatocellular (Liver) Cancer, Adult
Acute Myeloid Leukemia, Adult (Primary)
Acute Myeloid Leukemia, Childhood Hepatocellular (Liver) Cancer, Childhood
Adrenocortical Carcinoma (Primary)
Adrenocortical Carcinoma, Childhood Hodgkin's Lymphoma, Adult
AIDS-Related Cancers Hodgkin's Lymphoma, Childhood
AIDS-Related Lymphoma Hodgkin's Lymphoma During Pregnancy
Anal Cancer Hypopharyngeal Cancer
Astrocytoma, Childhood Cerebellar Hypothalamic and Visual Pathway Glioma,
Astrocytoma, Childhood Cerebral Childhood
Basal Cell Carcinoma Intraocular Melanoma
Bile Duct Cancer, Extrahepatic Islet Cell Carcinoma (Endocrine Pancreas)
Bladder Cancer
Bladder Cancer, Childhood Kaposi's Sarcoma
Bone Cancer, Osteo sarcoma/Malignant Kidney (Renal Cell) Cancer
Fibrous Histiocytoma Kidney Cancer, Childhood
Brain Stem Glioma, Childhood
Brain Tumor, Adult Laryngeal Cancer
Brain Tumor, Brain Stem Glioma, Laryngeal Cancer, Childhood
Childhood Leukemia, Acute Lymphoblastic, Adult
Brain Tumor, Cerebellar Astrocytoma, Leukemia, Acute Lymphoblastic, Childhood
Childhood Leukemia, Acute Myeloid, Adult
Brain Tumor, Cerebral Leukemia, Acute Myeloid, Childhood
Astrocytoma/Malignant Glioma. Leukemia, Chronic Lymphocytic
Childhood Leukemia, Chronic Myelogenous
Brain Tumor, Ependymoma, Childhood Leukemia, Hairy Cell
Brain Tumor, Medulloblastoma, Lip and Oral Cavity Cancer
Childhood Liver Cancer, Adult (Primary)
Brain Tumor, Supratentorial Primitive Liver Cancer, Childhood (Primary)
Neuroectodermal Tumors, Childhood Lung Cancer, Non-Small Cell
Brain Tumor, Visual Pathway and Lung Cancer, Small Cell
Hypothalamic Glioma, Childhood Lymphoma, AIDS-Related
Brain Tumor, Childhood Lymphoma, Burkitt's
Breast Cancer Lymphoma, Cutaneous T-CeIl, see Mycosis
Breast Cancer, Childhood Fungoides and Sezary Syndrome
Breast Cancer, Male Lymphoma, Hodgkin's, Adult
Bronchial Adenomas/Carcinoids, Lymphoma, Hodgkin's, Childhood
Childhood Lymphoma, Hodgkin's During Pregnancy
Burkitt's Lymphoma Lymphoma, Non-Hodgkin's, Adult
Lymphoma, Non-Hodgkin's, Childhood
Carcinoid Tumor, Childhood Lymphoma, Non-Hodgkin's During Carcinoid Tumor, Gastrointestinal Pregnancy Carcinoma of Unknown Primary
Central Nervous System Lymphoma, Lymphoma, Primary Central Nervous System
Primary
Cerebellar Astrocytoma, Childhood Macroglobulinemia, Waldenstrom's
Cerebral Astrocytoma/Malignant Malignant Fibrous Histiocytoma of
Glioma, Childhood Bone/Osteosarcoma
Cervical Cancer Medulloblastoma, Childhood
Childhood Cancers Melanoma
Chronic Lymphocytic Leukemia Melanoma, Intraocular (Eye)
Chronic Myelogenous Leukemia Merkel Cell Carcinoma
Chronic Myeloproliferative Disorders Mesothelioma, Adult Malignant
Colon Cancer Mesothelioma, Childhood
Colorectal Cancer, Childhood Metastatic Squamous Neck Cancer with
Cutaneous T-CeIl Lymphoma, see Occult Primary
Mycosis Fungoides and Sezary Multiple Endocrine Neoplasia Syndrome,
Syndrome Childhood
Multiple Myeloma/Plasma Cell Neoplasm
Endometrial Cancer Mycosis Fungoides Ependymoma, Childhood Myelodysplastic Syndromes Esophageal Cancer Myelodysplastic/Myeloproliferative Diseases Esophageal Cancer, Childhood Myelogenous Leukemia, Chronic Ewing's Family of Tumors Myeloid Leukemia, Adult Acute Extracranial Germ Cell Tumor, Myeloid Leukemia, Childhood Acute Childhood Myeloma, Multiple
Extragonadal Germ Cell Tumor Myeloproliferative Disorders, Chronic Extrahepatic Bile Duct Cancer Eye Cancer, Intraocular Melanoma Nasal Cavity and Paranasal Sinus Cancer Eye Cancer, Retinoblastoma Nasopharyngeal Cancer Nasopharyngeal Cancer, Childhood
Gallbladder Cancer Neuroblastoma
Gastric (Stomach) Cancer Non-Hodgkin's Lymphoma, Adult
Gastric (Stomach) Cancer, Childhood Non-Hodgkin's Lymphoma, Childhood
Gastrointestinal Carcinoid Tumor Non-FIodgkin's Lymphoma During Pregnancy
Germ Cell Tumor, Extracranial, Non-Small Cell Lung Cancer
Childhood
Germ Cell Tumor, Extragonadal Oral Cancer, Childhood
Germ Cell Tumor, Ovarian Oral Cavity Cancer, Lip and
Gestational Trophoblastic Tumor Oropharyngeal Cancer
Glioma, Adult Osteosarcoma/Malignant Fibrous
Glioma, Childhood Brain Stem Histiocytoma of Bone
Glioma, Childhood Cerebral Ovarian Cancer, Childhood
Astrocytoma Ovarian Epithelial Cancer
Glioma, Childhood Visual Pathway and Ovarian Germ Cell Tumor
Hypothalamic Ovarian Low Malignant Potential Tumor
Skin Cancer (Melanoma) Pancreatic Cancer Skin Carcinoma, Merkel Cell Pancreatic Cancer, Childhood Small Cell Lung Cancer Pancreatic Cancer, Islet Cell Small Intestine Cancer Paranasal Sinus and Nasal Cavity Cancer
For the treatment of oncological disorders, the peptides, polynucleotides, peptidomimetics, and compositions of this invention can be administered to a patient in need of treatment in combination with other antitumor or anticancer substances and/or
with radiation and/or photodynamic therapy and/or with surgical treatment to remove a tumor. These other substances or treatments may be given at the same as or at different times from the peptides, polynucleotides, peptidomimetics, and compositions of this invention. For example, the peptides, polynucleotides, peptidomimetics, and compositions of the present invention can be used in combination with mitotic inhibitors such as taxol or vinblastine, alkylating agents such as cyclophosamide or ifosfamide, antimetabolites such as 5~fluorouracil or hydroxyurea, DNA intercalators such as adriamycin or bleomycin, topoisomerase inhibitors such as etoposide or camptothecin, antiangiogenic agents such as angiostatin, antiestrogens such as tamoxifen, and/or other anti-cancer drugs or antibodies, such as, for example, GLEEVEC (Novartis Pharmaceuticals Corporation) and HERCEPTIN (Genentech, Inc.), respectively. Peptides, polynucleotides, peptidomimetics, and compositions of the invention can be used in combination with proteasome inhibitors, including, but not limited to, Bortezomib, Carfilzomib, and Salinosporamide A. Many tumors and cancers have viral genome present in the tumor or cancer cells.
For example, Epstein-Barr Virus (EBV) is associated with a number of mammalian malignancies. The peptides, polynucleotides, peptidomimetics, and compositions of the subject invention can also be used alone or in combination with anticancer or antiviral agents, such as ganciclovir, azidothymidine (AZT), lamivudine (3TC), etc., to treat patients infected with a virus that can cause cellular transformation and/or to treat patients having a tumor or cancer that is associated with the presence of viral genome in the cells.
The methods of the present invention can be used with humans and other animals.
The other animals contemplated within the scope of the invention include domesticated, agricultural, or zoo- or circus-maintained animals. Domesticated animals include, for example, dogs, cats, rabbits, ferrets, guinea pigs, hamsters, pigs, monkeys or other primates, and gerbils. Agricultural animals include, for example, horses, mules, donkeys, burros, cattle, cows, pigs, sheep, and alligators. Zoo- or circus-maintained animals include, for example, lions, tigers, bears, camels, giraffes, hippopotamuses, and rhinoceroses. In one embodiment, one or more of the peptides of the subject invention can be provided in the form of a multiple peptide construct. Such a construct can be designed so that multiple peptides are linked to each other by intervening moieties wherein the
intervening moieties are subsequently cleaved or removed following administration of the multiple peptide construct to a patient. Methods for constructing multiple peptide constructs are known in the art. For example, peptides of the present invention can be provided in the form of a multiple antigenic peptide (MAP) construct. The preparation of MAP constructs has been described in Tarn (1988). MAP constructs utilize a core matrix of lysine residues onto which multiple copies of an immunogen are synthesized. Multiple MAP constructs, each containing different peptides, can be prepared and administered in accordance with methods of the present invention. In another embodiment, a multiple peptide construct can be prepared by preparing the subject peptides having at least one metal chelating amino acid incorporated therein, preferably at the amino and/or carboxy terminal of the peptide as described, for example, in U.S. Patent No. 5,763,585. The peptides are then contacted with a solid support having attached thereto a metal ion specific for the metal chelating amino acid of the peptide. A multiple peptide construct of the invention can provide multiple copies of the exact same peptide, including variants or fragments of a subject peptide, or copies of different peptides of the subject invention.
Therapeutic application of the subject peptides, polynucleotides, and peptidomimetics, and compositions containing them, can be accomplished by any suitable therapeutic method and technique presently or prospectively known to those skilled in the art. The peptides, polynucleotides, and peptidomimetics can be administered by any suitable route known in the art including, for example, oral, nasal, rectal, parenteral, subcutaneous, or intravenous routes of administration. Administration of the peptides, polynucleotides, and peptidomimetics of the invention can be continuous or at distinct intervals as can be readily determined by a person skilled in the art.
Compounds and compositions useful in the subject invention can be formulated according to known methods for preparing pharmaceutically useful compositions. Formulations are described in detail in a number of sources which are well known and readily available to those skilled in the art. For example, Remington 's Pharmaceutical Science by E. W. Martin describes formulations which can be used in connection with the subject invention. In general, the compositions of the subject invention will be formulated such that an effective amount of the bioactive peptide, polynucleotide, or peptidomimetic is combined with a suitable carrier in order to facilitate effective administration of the composition. The compositions used in the present methods can
also be in a variety of forms. These include, for example, solid, semi-solid, and liquid dosage forms, such as tablets, pills, powders, liquid solutions or suspension, suppositories, injectable and infusible solutions, and sprays. The preferred form depends on the intended mode of administration and therapeutic application. The compositions also preferably include conventional pharmaceutically acceptable carriers and diluents which are known to those skilled in the art. Examples of carriers or diluents for use with the subject peptides, polynucleotides, and peptidomimetics include, but are not limited to, water, saline, oils including mineral oil, ethanol, dimethyl sulfoxide, gelatin, cyclodextrans, magnesium stearate, dextrose, cellulose, sugars, calcium carbonate, glycerol, alumina, starch, and equivalent carriers and diluents, or mixtures of any of these. Formulations of the peptide, polynucleotide, or peptidomimetic of the invention can also comprise suspension agents, protectants, lubricants, buffers, preservatives, and stabilizers. To provide for the administration of such dosages for the desired therapeutic treatment, pharmaceutical compositions of the invention will advantageously comprise between about 0.1% and 45%, and especially, 1 and 15% by weight of the total of one or more of the peptide, polynucleotide, or peptidomimetic based on the weight of the total composition including carrier or diluent.
The peptides, polynucleotides, peptidomimetics, and compositions of the subject invention can also be administered utilizing liposome technology, slow release capsules, implantable pumps, and biodegradable containers. These delivery methods can, advantageously, provide a uniform dosage over an extended period of time.
The subject peptides, polynucleotides, and peptidomimetics can also be modified by the addition of chemical groups, such as PEG (polyethylene glycol). PEGylated peptides typically generate less of an immunogenic response and exhibit extended half- lives in vivo in comparison to peptides that are not PEGylated when administered in vivo. Methods for PEGylating proteins and peptides known in the art (see, for example, U.S. Patent No. 4,179,337). The subject peptides, polynucleotides, and peptidomimetics can also be modified to improve cell membrane permeability. In one embodiment, cell membrane permeability can be improved by attaching a lipophilic moiety, such as a steroid, to the peptide, polynucleotide, or peptidomimetic. Other groups known in the art can be linked to peptides, polynucleotides, and peptidomimetics of the present invention.
The subject invention also concerns a packaged dosage formulation comprising in one or more containers at least one peptide, polynucleotide, peplidomimetic, and/or composition of the subject invention formulated in a pharmaceutically acceptable dosage. The package can contain discrete quantities of the dosage formulation, such as tablet. capsules, lozenge, and powders. The quantity of peptide, polynucleotide, and/or peptidomimetic in a dosage formulation and that can be administered to a patient can vary from about 1 mg to about 5000 mg, or about 1 mg to about 2000 mg, or more typically about 1 mg to about 500 mg, or about 5 mg to about 250 mg, or about 10 mg to about 100 mg. The subject invention also concerns kits comprising one or more peptides, polynucleotides, peptidomimetics, compositions, compounds, or molecules of the present invention in one or more containers. In one embodiment, a kit contains a peptide, polynucleotide, peptidomimetic, and/or composition of the present invention. In a specific embodiment, a kit comprises a peptide comprising the amino acid sequence shown in SEQ ID NO:1, or a fragment or variant of the peptide that exhibits antiviral activity. In a specific embodiment, the tyrosine at position 7 of SEQ ID NO:1 (Le , the tyrosine that is underlined in the sequence LP QDKE Y YKVKEP) is phosphorylated. In a more specific embodiment, a kit comprises a peptide consisting of the amino acid sequence shown in SEQ ID NO:1, and optionally wherein the tyrosine at position 7 is phosphorylated. A kit of the invention can also comprise one or more antiviral compounds, biological molecules, or drugs and/or one or more IFNγ peptide mimetics. In one embodiment, the biological molecule is one or more of IFNα, IFNβ, or IFNγ. In one embodiment, a kit comprises one or more peptides of SEQ ID NO:67 and/or SEQ ID NO:75, or a fragment or variant thereof that exhibits antiviral activity. In one embodiment, a kit can also comprise one or more peptides comprising the amino acid sequence shown in SEQ ID NO:61 (Tkip peptide), or a fragment or variant thereof that exhibits antiviral activity, and/or a peptide comprising the amino acid sequence shown in SEQ IDNO:63, or a fragment or variant thereof that exhibits antiviral activity. In one embodiment, a kit comprises one or more of IFNα, IFNβ, IFNγ, acyclovir (Zovirax), zidovudine (AZT), lamivudine (3TC), zanamivir (Relenza), oseltamivir (Tamiflu), valacyclovir (Valtrex), amantadine (Symmetrel), rimantadine (Flumadine), cidofovir (Vistide), foscarnet (Foscavir), ganciclovir (Cytovene), ribavirin (Virazole), nelfinavir
(Viracept), ritonavir (Norvir), rifampin (Rifadin), and famciclovir (Famvir). In another embodiment, a kit comprises one or more of mitotic inhibitors such as taxol or vinblastine, alkylating agents such as cyclophosarnide or ifosfamide, antimetabolites such as 5 -fluoro uracil or hydroxyurea, DNA intercalators such as adriamycin or bleomycin, topoisomerase inhibitors such as etoposide or camptothecin, antiangiogenic agents such as angiostatin, antiestrogens such as tamoxifen, and/or other anti-cancer drugs or antibodies, such as, for example, GLEEVEC (Novartis Pharmaceuticals Corporation) and HERCEPTIN (Genentech, Inc.), respectively.
In one embodiment, a kit of the invention includes instructions or packaging materials that describe how to administer a compound or composition of the kit. Containers of the kit can be of any suitable material, e.g., glass, plastic, metal, etc., and of any suitable size, shape, or configuration. In one embodiment, a compound and/or agent of the invention is provided in the kit as a solid, such as a tablet, pill, or powder form. In another embodiment, a compound and/or agent of the invention is provided in the kit as a liquid or solution. In one embodiment, the kit comprises an ampoule or syringe containing a compound and/or agent of the invention in liquid or solution form.
MATERIALS AND METHODS FOR EXAMPLES 1-8
Cell Culture and Virus. HEL-30 keratinocytes (Dr. D. Germolec, NIEHS, Durham, NC), L929 fibroblasts (CCL-I, ATCC, Manassas, VA), and Vero cells (CCL-
81, ATCC) were cultured in DMEM supplemented with 10% BCS. Cells were plated into 75 cm2 tissue culture flasks and incubated at 37° C, 95% air/5% CO2 in a humidified incubator. HSV-I (syn 17+) (provided initially by Dr. Nancy Sawtell, Children's
Hospital Medical Center, Cincinnati, OH) was routinely passaged and titrated in Vero cells. HSV-I ICPO mutant, designated as dll403 (Stow and Stow, 1986), was obtained from Dr. Rick Thompson (Univ Cincinnati, Cincinnati, OH), and was grown and titrated in U2OS cells (HTB-96, ATCC). U2OS cell were grown in McCoy's 5A medium with
10% FBS. Mouse macrophage cell line RAW 264.7 was grown in RPMl with 10% FBS.
Peptides. The amino acid sequences for the peptide mimetics used in this study shown in Table 4. The peptides were synthesized on an Applied Biosystems 9050 automated peptide synthesizer using conventional fhiorenylmethyloxycarbonyl chemistry as previously described (Szente et ai, 1996). The addition of a lipophilic group
(palmitoyllysine) to the N terminus of the synthetic peptide was performed as a last step, using semiautomated protocol (Thiam et ah, 1999). Peptides were characterized by mass spectrometry and were purified by HPLC. All peptides were dissolved in DMSO at a concentration of 10 mg/mL. Peptides were diluted in cell culture medium prior to addition to cells.
Cytopathic Effect Inhibition Assay. L929 fibroblasts or HEL-30 keratinocytes were cultured and counted in a hemacytometer, added at densities of 2.0 x 104 to 3.0 x 104 to each well of a multiwell cell culture plate and incubated overnight. The following day, recombinant murine interferon gamma (IFN-γ) (Peprotech, Rocky Hill, NJ), IFN-γ peptide mimetics, SOCS-I mimetic peptide, SOCS-I antagonist peptide, or IFNγ mimetic peptide were added to the cultures at the indicated concentrations and incubated for 24 hours. At 100% confluence, culture medium was aspirated, cells were rinsed with PBS and HSV-I added at an MOI of 0.1. Two days post-infection, medium was aspirated, cells were washed twice with Ix HBSS and fixed by addition of 10% formalin. Fixative was removed and cell layers were stained with crystal violet. Plates were rinsed with dH2O and dried overnight. Plates were scanned on an HP ScanJet 5300C or photographed using a Fuji LAS-300 CCD camera. Densitometry measurements of each well were computed using Multi-gauge software (FujiFilm USA, Burbank, CA) or NIH Im age- J. HSV-I infection of Monolayer Cultures. Cells were seeded into 35 mm culture dishes at a density of 1 x 104 cells/cm2 and allowed to grow to -75% confluence. Culture medium was aspirated and monolayers washed with Ix PBS. HSV-I diluted in minimum essential medium (MEM) containing 2% calf serum (CS) was added to the culture medium at the indicated MOI and the cell cultures incubated for 2 hours at 370C. Medium was removed and replaced with MEM containing 10% CS.
RNA isolation and Quantitation. RNA was collected from cells at specified times after infection. Total RNA was isolated by using RNeasy mini kits (Qiagen Inc., Valencia, CA) according to the manufacturers' instructions. Samples were eluted 2x in a volume of 20 μL. RNA concentration was determined by measuring absorbance at 260 and 280 nm and purity calculated using ratios of absorbance at 260 and 280 nm (260/280). RNA integrity was checked by formaldehyde agarose gel electrophoresis. Briefly, each sample was added to one well of a 1.2% formaldehyde/agarose gel with
ethidium bromide and electrophoresed at 5 V/cm. Bands were visualized with UV light and documented by capture with a CCD camera (Fujifilm USA, Burbank, CA).
RT-PCR. Briefly, 2 μg of total RNA from each experimental sample was used in a reverse transcriptase (RT) reaction. Reaction conditions were: Ix RT buffer, 0.5 mM dNTP, 1 μM oligo-dT primer, 10 U/μL RNase inhibitor, and 4 U/μL RT enzyme in a total reaction volume of 20 μL. Each sample was incubated at 37° C for 1 hour. Each completed RT reaction mix was added to a PCR master mix. The resulting PCR cocktail was aliquoted (25 μL) into PCR tubes containing appropriate primers for the gene of interest. PCR was performed with 30 cycles of the following program: 30 sec at 95° C, 30 sec at 55° C, and 30 sec at 70° C. Following the completion of PCR, 10 μL of each sample was electrophoresed through a 2% agarose gel at 5 V/cm. Images were captured using a Fuji CCD camera. Data was normalized to expression of a housekeeping gene (GAPDH) and expressed as percent of control.
Western Blotting. HEL-30 keratinocytes or L929 fibroblasts were plated into cell culture plates and allowed to grow overnight. Cells were infected with HSV-I as described above. The virus was removed and fresh DMEM containing 10% BCS added. At the indicated time points, medium was removed and cells were rinsed 3x with PBS. Cells were then lysed with Complete Lysis Buffer M (Roche Diagnostics, Indianapolis, IN) by following manufacturer's suggestions. Equal amounts of lysate were combined with 6x Laemelli buffer and resolved by SDS-PAGE. Proteins were electro-blotted overnight onto PVDF. Membranes were blocked for one hour with 5% non-fat milk/TBS-Tween. Membranes were incubated with primary antibody to SOCS-I (Millipore, Temecula, CA), STAT-I, or p-STAT-1 (Santa Cruz Biotech, Santa Cruz, CA). Membranes were rinsed 3x with TBS-Tween and then incubated with secondary antibody. Proteins bands were resolved by chemiluminescence. Images were captured as before using a Fuji CCD camera.
Cloning of SOCS-I reporter constructs. A DNA fragment containing the human SOCS-I promoter was amplified using genomic DNA purified from WISH cells. The forward and reverse primers used for amplification were 5'- TTTGCTAGCTCTTCCGCAGCCGGGTAGTG-S' (SEQ ID NO:72) and 5"- TCCAAGCTTT ACAGAAGGGGCCAGCCGGA-3' (SEQ ID NO:73), respectively. The following conditions were used for PCR. 94° C, 30 sec: 62° C, 30 sec; 68° C. 90 sec; for
30 cycles. The PCR fragment was purified and digested with Nhe 1 and Hind III and ligated with pGL3 basic reporter plasmid (Promega, Madison, WI) expressing firefly luciferase, digested with similar enzymes. The sequence of the reporter plasmid thus generated, which contained nucleotides -1577 to -3 of the promoter was confirmed by DNA sequencing.
Luciferase Assay. HEL-30 cells were plated into 12-well cell culture dishes and allowed to grow overnight. Cells were co-transfected with the plasmids expressing SOCS-I promoter linked firefly luciferase and a constitutively expressed Renilla luciferase using GeneJammer (Stratagene, La Jolla, CA) transfection reagent for HEL-30 cells or Metafectene (Biontex Laboratories GmBh, Martinsreid, Germany) for L929 cells. Relative luciferase units were measured by using a dual luciferase assay kit form Promega (Madison, WI). Twenty-four hours after transfection, cells were either treated with 2000 LVmL murine IFN-γ or infected with HSV-I at an MOI of 2.0 for 4 hours prior to treatment with IFN-γ. After treatment, cells were lysed with Passive Lysis Buffer. Lysates were then assayed for luciferase activity using Dual Luciferase Assay Kit (Promega, Madison, WI). Luciferase levels were normalized to levels of the constitutive reporter.
SOCS-I Transfection. HEL-30 cells or L929 cells were plated into 12-well cell culture dishes and allowed to grow overnight. Cells were transfected with a construct containing the full-length murine SOCS-I gene, pFL AG-SOCS-I (a kind gift of Dr. Douglas Hilton, Walter and Eliza Hall Institute, Victoria, Australia). Briefly, L929 cells at ~90% confluence were transfected with indicated amounts of pFLAG-SOCS-1 using Metafectene Pro (Biontex Laboratories GmbH, Martinsreid, Germany). Twenty-four hours later, cells were lysed and extracts used for Western blotting to confirm expression of the SOCS-I protein.
Statistics. GraphPad Prism 5 software from GraphPad software, Inc. (La Jolla, CA) was used to determine the statistical significance of different treatments.
All patents, patent applications, provisional applications, and publications referred to or cited herein are incorporated by reference in their entirety, including all figures and tables, to the extent they are not inconsistent with the explicit teachings of this specification.
Following are examples that illustrate procedures for practicing the invention. These examples should not be construed as limiting. All percentages are by weight and all solvent mixture proportions are by volume unless otherwise noted.
Example 1 — ΪFNγ induces an antiviral state against HSV-I in fibroblasts but not keratinocytes
Keratinocytes are important for HSV-I replication in the epidermis, which plays a role in infection of nervous tissue (Roizman et al., 2007). We were therefore interested in determining the ability of IFNγ to inhibit HSV-I replication in HEL-30 keratinocytes relative to L929 fibroblasts (Figure 1). IFNγ at concentrations of 12.5 to 50 U/ml protected fibroblasts infected with HSV-I at an moi of 0.1 (Figure IA), while HEL-30 keratinocytes were susceptible to HSV-I -mediated lysis (CPE) in the presence of IFNγ (Figure IB). Specifically, HEL-30 keratinocytes were lysed in the presence of IFNγ, while the fibroblasts were protected. These observations suggest a possible basis for the successful pathogenesis of HSV-I in keratinocytes even in the presence of IFNγ and also provide an approach to possible prevention of HSV-I pathogenesis.
A small peptide mimetic of mouse IFNγ that consists of the C-terminus of IFNγ with an attached palmitate for plasma membrane penetration (Table 4) (Szente et al., 1996) was used. The mimetic contains an essential alpha helix and polycationic nuclear localization sequence. It binds to the cytoplasmic domain of the lFNγ receptor subunit, IFNGRl, and participates in activation of STATI a and transport of a complex of STATI a and IFNGRl to the GAS promoter element in genes specifically activated by IFNγ (Ahmed and Johnson, 2006). The mimetic peptide, IFNγ (95-132) (SEQ ID NO:67), inhibited HSV-I -induced CPE at 15 to 30 μM in L929 fibroblasts in a manner similar to IFNγ (Figure 1C), while having little or no antiviral effect in HEL-30 keratinocytes (Figure ID). Thus, the IFNγ mimetic showed similar but slightly less HSV-I inhibition patterns to IFNγ in keratinocytes versus fibroblasts.
Example 2 — HSV-I infection induces SQCS-I expression in HEL-30 keratinocytes but not in L929 fibroblasts
IFN activity is negatively regulated by SOCS-I, so we infected HEL-30 keratinocytes and L929 fibroblasts with HSV-I to investigate possible differential
induction of SOCS-I. RT-PCR analysis of SOCS-I mRNA expression in HSV-I (moi of 1) infected fibroblasts and keratinocytcs showed an increase of 4-fold for keratin ocytes while having a negligible effect on fibroblasts (Figure 2A). Expression of SOCS-I mRNA was normalized to the levels of GAPDH mRNA expression and presented as fold induction over uninfected cells. Levels of GAPDH or another housekeeping gene β- tubulin did not change during these treatments. At the protein level, HSV-I infected HEL-30 fibroblasts showed increased levels by Western blots up to 6 hours post-infection as shown in Figure 2B. By comparison, there was minimal to no effect on induction of SOCS-I protein in L929 fibroblasts (Figure 2C). RT-PCR analysis of SOCS-I mRNA over time showed that similar levels were observed from 1 to 6 hours post-infection with HSV-I (Figure 2D). Further, the level of SOCS-I gene activation was similar at 1 and 2 moi and enhanced at 5 moi (data not shown). Thus, HSV-I differentially induced the activation of SOCS-I as per RT-PCR and Western blot analysis of HEL-30 and L929 cells, which is consistent with the ability of IFNγ to inhibit HSV-I induced CPE in L929 fibroblasts but not in HEL-30 keratinocytes.
Example 3 — IFNγ activation of STATIa is inhibited in HEL-30 keratinocvtes infected with HSV-I
Activation of STATlα transcription factor by the IFNγ/IFNγ receptor complex is critical for induction of the antiviral state (Ahmed and Johnson, 2006). Accordingly, we determined the effect of HSV-I infection of HEL-30 keratinocytes and L929 fibroblasts on IFNγ activation of STATlα in these cells. As shown in Figure 3 A, treatment of HEL- 30 keratinocytes with IFNγ activated STATlα as indicated by tyrosine phosphorylation. Treatment of cells that were infected with HSV-I reduced phosphorylation to the basal level. By contrast, the activation of STATIa in the presence of HSV-I infection of L929 cells was not inhibited (Figure 3B). Activation of STATIa is dependent on the tyrosine kinase JAK2 and we have shown that SOCS-I via the kinase inhibitory region (KIR) inhibits JAK2 function by binding to its activation loop (Flowers et al., 2004). Thus, induction of SOCS-I in HEL-30 keratinocytes is consistent with inhibition of STATIa activation by IFNγ and the resultant failure of IFNγ to induce an antiviral state in HEL-30 cells.
Example 4 — HSV-I infection of HEL-30 keratinocytes increases transcription from the SOCS-I promoter
The dramatic increase in SOCS-I mRNA and protein in HSV-I infected HEL-30 keratinocytes, would suggest an effect on the SOCS-I promoter. Accordingly, we fused the SOCS-I promoter (nucleotides -1577 to -3) to the luciferase reporter gene and transfected this reporter plasmid into HEL-30 cells. As shown in Figure 4, treatment of the cells with 2000 U/ml of IFNγ caused a two-fold increase in relative luciferase activity. Remarkably, infection of the cells with HSV-I increased luciferase activity approximately three-fold that was not reduced in the presence of IFNγ. These results are consistent with the induction of endogenous SOCS-I message and protein in HEL-30 keratinocytes infected with HSV-I in the absence and presence of IFNγ and is explanatory of the refractiveness to the induction of an antiviral state to HSV-I in these cells.
Example 5 — A peptide antagonist of SOCS-I synergizes with IFNγ to induce an antiviral state against HSV-I in HEL-30 keratinocvtes
We have developed an antagonist of SOCS-I that is a peptide corresponding to the activation loop of JAK2 (Waiboci et al, 2007). The peptide, pJAK2(1001-1013) (SEQ ID NO:1), was synthesized with a phosphotyrosine at position 1007, corresponding to the activation state of JAK2 (Lucet et al, 2006). pJAK2(1001-1013) binds to the KIR region of SOCS-I , enhances IFNγ activity, reverses SOCS-I inhibition of STAT activation, and enhances GAS promoter activity of IFNγ (Waiboci et al., 2007). A palmitate group was attached to pJAK2(1001-1013) for cell penetration and it was examined to see if it could synergize with IFNγ in induction of an antiviral state in HEL- 30 cells infected with HSV-I.
As shown in Figure 5A, HEL-30 cells infected with HSV-I were minimally protected by 100 U/ml of lFNγ alone. pJAK2(1001-1013) at 35 μM showed approximately 40 percent protection, while 17 and 8 μM were not protective. Combined treatment of infected cells with 100 U/ml of IFNγ and 35 μM of pJAK2(1001-1013) resulted in 100 percent protection against HSV-I. This protection was concentration- dependent as 17 and 8 μM of pJAK2(1001-1013) and 100 U/ml IFNγ resulted in approximately 70 and 25 percent protection, respectively. The IFNγ mimetic also
synergized with the SOCS-I antagonist (data not shown). These results provide further evidence that the refractiveness to induction of an antiviral state in HEL-30 cells to HSV- 1 is due to induction of SOCS-I. Additionally, the results suggest an approach to counter the induction of SOCS-I by viruses as a mechanism to avoid IFN induction of an antiviral state in cells.
As a correlate to the peptide antagonist experiment, HEL-30 cells were transfected with SOCS-I siRNA and determined the relative protection against HSV-I in the presence and absence of 400 U/ml of IFNγ. As shown in Figure 5B, siRNA alone provided similar protection to that observed in combination with IFNγ. A control siRNA, by comparison was relatively non-protective. Thus, the pJAK2(1001-1013) protection is supported by similar protection with SOCS-I siRNA transfected HEL-30 cells infected with HSV-I.
Consistent with inhibition of HSV-I replication in L929 fibroblasts by IFNγ mimetic peptide IFNγ(95-132) as determined by CPE, yield reductions in L929 cells demonstrate that the IFNγ mimetic at 50 μM and 25 μM inhibited plaque formation by 77- fold and by 14-fold, respectively (Table 5). The SOCS-I antagonist pJAK2(1001- 1013) had a negligible effect on HSV-I replication in L929 cells at 25 μM (also at 50 μM, data not shown). This is consistent with the lack of induction of SOCS-I in these cells by HSV-I . The yield reduction assay indicates that the protections observed were due to inhibition of virus replication rather than to some nonreplicative toxic effect of HSV-I on the cells.
Example 6 — Overexpression of SOCS-I in L929 fibroblasts results in inhibition of IFNγ induction of an antiviral state to HSV-I HSV-I infection of L929 fibroblasts does not cause significant induction of
SOCS-I and does not inhibit induction of an antiviral state by IFNγ. Accordingly, L929 cells were transfected with SOCS-I expression plasmid (Figure 6A) to determine if this would cause a blockage of IFNγ induction of an antiviral state against HSV-I . As shown in Figure 6B, IFNγ induced an antiviral state in cells lransfected with two μg of control plasmid, while one and two μg of SOCS-I expression plasmid transfected cells showed a dose-dependent reduction in the ability of IFNγ to induce an antiviral state.
A small peptide mimetic of SOCS-I, WLVFFVIFYFFR (SEQ ID N0:61), called tyrosine kinase inhibitor peptide or Tkip (Table 4) (Flowers et al, 2004). Tkip specifically binds to the activation loop of JAK2 as per the SOCS-I antagonist peptide pJAK2(l 001 -1013). Substitution of alanine for phenylalanine at positions 8 and 11 in Tkip, the peptide is designated Tkip2A (SEQ ID NO:62), abrogates binding to pJAK2(l 001-1013) as well as inhibition of activation of STATl α by IFNγ (data not shown). As a corollary to SOCS-I transfection, L929 cells were treated with 100 U/ml of IFNγ and 20 μM of either Tkip or Tkip2A peptide to determine the effect on HSV-I infection. As shown in Figure 6C, Tkip but not Tkiρ2A significantly inhibited the ability of IFNγ to induce an antiviral state. Thus, the SOCS-I mimetic Tkip had a similar effect on IFNγ treated L929 fibroblasts as did transfection with SOCS-I . These results mimicked those obtained with HEL-30 fibroblasts and support the data showing that induction of SOCS-I in the latter by HSV-I infection renders these cells refractory to the antiviral effects of IFNγ.
Example 7 — Reduction in SOCS-I gene activation by HSV-I ICPO mutant in HEL-30 keratinocytes
ICPO is an IE virulence protein that increases expression of HSV-I genes in infected cells (Poon et al, 2006; Gu and Roizman, 2009; Cliffe and Knipe, 2008). One way that it functions is by blockage of histone deacetylation and/or increase in histone accetylation to facilitate HSV-I gene expression (Gu and Roizman, 2009; Cliffe and Knipe, 2008). It also causes degradation of host proteins that are involved in silencing HSV gene expression, such as the promyclocytic leukemia protein (Gu and Roizman, 2009). To deteπnine if ICPO might play a role in HSV-I refractiveness to IFNγ in HEL- 30 keratinocytes, we infected the cells with HSV-I synl7+ that had mutated and thus had a non-functional ICPO (Stow and Stow, 1986). ICPO mutated HSV-I (ICPOmut, dll403) was similarly lytic for HEL-30 cells as wild type virus, but unlike the wild type virus was inhibited by IFNγ (Figure 7A). Refractiveness to IFNγ was restored when the cells were treated with the SOCS-I mimetic Tkip at the time of IFNγ treatment where 100 U/ml of IFNγ activity was significantly blocked by as little as 2.5 μM of SOCS-I mimetic (Figure 7B). To assess as to how all this might be related to ICPO, SOCS-I, and IFNγ in HEL-30 cells, the cells were transfected with a luciferase reporter containing the SOCS-I
promoter (nucleotides -1577 to -3), infected the transfected cells with wild type HSV-I and HSV-I ICPOmut and compared them for reporter gene activation. As shown in Figure 7C, wild type HSV-I was more than 2-fold more effective than ICPOmut in activation of the reporter gene at comparable levels of infectivity. It has been reported that ICPO does not bind to DNA (Sekulovich et al. , 1988), but it obviously has an activation effect on the SOCS-I gene in HEL-30 keratinocytes. Observations suggest that ICPO has a direct or indirect effect on SOCS-I gene activation in keratinocytes either as per mechanisms indicated above with respect to its known function or in some cases it might function as a transcription/cotranscription factor.
Example 8 — SOCS-I antagonist svnergizes with IFNγ in protection of macrophage cell line RAW264.7 against HSV-I
SOCS-I acts at several sites in activation of Toll-like receptors (TLRs) in antigen presenting cells such as macrophages, perhaps to prevent an over-response of the innate immune system (Yoshimura et al, 2007; Mansell et al, 2006; Croker el al. 2008). The ability of SOCS-I antagonist to enhance the anti-HSV-1 effects of IFNγ in the RAW264.7 macrophage cell line was determined. Infection of RAW264.7 cells with HSV-I at an moi of 0.1 resulted in 100% lysis in 48 hours in 96-well cultures as per Figure 8. IFNγ at 100 U/nil resulted in 30% protection. SOCS-I antagonist p J AK2( 1001- 1013) at 25 μM did not protect against HSV-I. However, the combination of pJAK2(1001-1013) at 25 μM and IFNγ at 100 U/ml resulted in 75% protection. pJAK2(l 001-1013) with alanine substitutions for tyrosines at positions 1007 and 1008 was much less effective at enhancement of IFNγ activity. Thus, the SOCS-I antagonist enhanced IFNγ effects against HSV-I in a macrophage cell line. Such enhancement reflects the linkage between SOCS-I and the negative regulation of TLR signaling (Yoshimura el al, 2007; Mansell et al, 2006; Croker et al, 2008).
Table 4. List of peptides used in this study.
Peptides Sequences
Tkip WLVFF VIFYFFR (SEQ ID NO:61)
Tkip2A WLVFFVIAYFAR (SEQ ID NO:62)
SOCSl-KIR 53DTHFRTFRSHSDYRRI (SEQ ID NO:63)
SOCS1-KIR2A 53DTHFATFASHSDYRRI (SEQ ID NO:64)
JAK2(1001-1013) 1001 LPQDKEYYKVKEP (SEQ ID NO: 1)
MuϊFNγ(95-106) 95AKFEVNNPQVQR (SEQ ID NO:65)
MuIFNγ(95-125) 95AKFEVNNPQVQRQAFNELIRWHQLLPESSL (SEQ ID NO:66)
95
MulFNγ(95-132) AKFEVNNPQVQRQAFNELIRVVHQLLPESSLRKRKRSR (SEQ ID NO:67)
All the peptides were synthesized with an attached lipophilic group, palmitic acid, for cell penetration. MuIFNγ(95-106), MuIFNγ(95-125), and MuIFNGRl (253-287) were used as control peptides. These peptides do not show significant biological activity in the assays for which they have been used as control peptides.
Table 5. Yield reduction of HSV-I in L929 fibroblasts treated with IFNγ mimetic and SOCS-I antagonist.
L929 cells (1.6 x 10 per well in 6-well plates) were treated with peptides for 24 h, followed by infection with HSV-I at moi 0.001 for 24 h. Cell lysates and supernatants were collected and viral yield was determined by standard plaque assay.
MATERIALS AND METHODS FOR EXAMPLES 9-18
Cells and Virus. BSC-40, MDCK, L929 and WISH cells were obtained from ATCC (Manassas, VA) and propagated on DMEM (BSC-40, L929, WISH) or EMEM (MDCK) with 10% fetal bovine serum. All cells were grown at 37°C in humidified
atmosphere with 5% CO2. Vaccinia virus Western Reserve strain was a kind gift from Dr. Richard Condit (University of Florida). Vaccinia virus was grown, purified on sucrose gradient, and titrated on BSC-40 cells, as described (Earl and Moss, 1998). EMC virus was grown and titrated on L929 cells, as described (Mujtaba et ah, 2006). Influenza A/PR/8/34 virus was obtained from ATCC, and grown and titrated on MDCK cells, as described (Palese and Shaw, 2007).
Peptides. The sequence of peptides used is presented in Table 6. These peptides were synthesized on an Applied Biosystems 9050 automated peptide synthesizer using conventional fluorenylmethyloxycarbonyl chemistry as described previously (Szente el a!., 1994). The addition of a lipophilic group (palmitoyl-lysine) to the N-terminus of the synthetic peptide was performed as a last step, using semi-automated protocol. Peptides were characterized by mass spectrometry and were purified by HPLC.
Western blot analysis. Western blot analysis was carried out to determine whether Tkip and SOCSl-KIR inhibited the phosphorylation of STAT substrate by the various JAKs in cultured cells. Cells were incubated with various concentrations of lipophilic Tkip, Tkip2A, SOCSl-KIR, SOCS1-KIR2A or control peptide for 2 hours, after which interferon was added and the cells incubated for an additional 2 hours. The cells were washed in cold PBS and harvested in RlPA buffer containing protease and phosphatase inhibitor cocktails (Santa Cruz). Protein concentration was measured using a BCA kit (Pierce) and lysates were resolved on 12% SDS-PAGE, transferred onto nitrocellulose membranes, and probed with various anti-phosphotyrosine antibodies. The membranes were then stripped and reprobed with the indicated anti-protein antibodies. All antibodies used were from Santa Cruz Biotechnology. Scanning of the band intensity was carried out using Image J software from NIH. Mice. All animal protocols were approved by the Institutional Animal Use and
Care Committee (IACUC) at the University of Florida. Female C57BL/6 mice (6-8 weeks old) were purchased from Jackson Laboratories (Bar Harbor, ME). Peptides dissolved in PBS in a volume of 100 μl were administered intraperitoneally. For the oral administration of the peptides, indicated amounts of peptide in 0.5 ml PBS were given using a feeding needle. Intraperitoneal administration of vaccinia was done in a volume of 100 μl. For intranasal administration, vaccinia virus was taken in a volume of 10 μl, and 5 μl was delivered in each of the nostrils of a lightly anesthetized mouse. Following
infection, mice were observed daily for signs of disease, such as lethargy, ruffled hair, weight loss, and eye secretions. Moribund mice were euthanized and counted as dead.
Measurement of intracellular and extracellular vaccinia virus formation. BSC-40 cells were seeded and grown overnight to confluency. Peptides at concentrations indicated were added to cells for one hour followed by infection with vaccinia virus at moi of 5 for one hour. This was followed by addition of growth medium containing the same amount of peptides as before and incubation for times indicated. Supematants were harvested, and the cells were scraped in 0.2 ml of cell lysis buffer consisting of 50 mM Tris.HCl, pH 7.5, 250 mM NaCl, 0.1% NP-40, 50 mM NaF and 5 mM EDTA, followed by three cycles of freeze thawing and sonication. The virus titer in the supernatant (extracellular) and cell extracts (intracellular) were measured by plaque assay on BSC-40 cells.
Measurement of vaccinia virus specific cellular response by proliferation assay. Spleens from naϊve or recovered mice at times indicated were homogenized to single cell suspension. Splenocytes (105 cells per well) were incubated with medium alone, or medium containing UV-inactivated vaccinia virus at 37°C for 96 hours. The cultures were then pulsed with H-thymidine (1 μCi/well; Amersham Biosciences) for 8 hours before harvesting onto filter paper discs using a cell harvester. Cell associated radioactivity was counted using a scintillation counter. Measurement of vaccinia virus specific cellular response by IFNγ ELISPOT.
CD4-deplction of splenocytes from naϊve or recovered mice was carried out by using the L3T4 antibody bound to Dynabeads (Invitrogen, Carlsbad, CA). ELISPOT assay was carried out by using a kit from Mabtech USA. Briefly, CD4-depleted cells (105 per well) were seeded in a microtiter plate, previously coated with an antibody to IFNγ and incubated in the absence or presence of increasing amount of purified vaccinia virus for 24 hours at 37°C. After washing, diluted monoclonal antibody was added and incubated for 2 hours, followed by washing and addition of streptavidin-HRP. After 1 hour at room temperature, the wells were washed and TMB substrate was added and absorbance was measured in a plate reader. Measurement of anti-vaccinia antibody response by ELISA. Microtiter plates were coated with 10 pfu of purified UV-inactivated vaccinia virus (900,000 μJ/cm" for 5 min in a DNA cross-linker) in 100 μl of binding buffer (carbonate-bicarbonate, pH 9.6)
overnight at 4°C. Plates were blocked for 2 hours at room temperature with PBS containing 5% fetal bovine serum. Mouse sera was serially diluted in PBS containing 0.1% Tween-20 (wash buffer). 0.1 ml of the diluted serum was added to each well. The plate was incubated for 2 hours at room temperature and washed three times with wash buffer. Peroxidase-conjugated goat anti-mouse IgA (α chain specific), or IgG (γ chain specific) (both from Santa Cruz Biotechnology, Santa Cruz, CA), diluted in a volume of 0.1 ml, was added to each well, incubated for 1 hour, and washed five times with wash buffer. OPD in a volume of 0.1 ml was added and incubated for 15 min. The reaction was stopped by addition of 50 μl of 3 N HCl. The optical density at 490 nm was determined using a microtiter plate reader.
Measurement of vaccinia virus neutralizing antibodies. Plaque reduction assay was carried out to test the ability of antibodies to inhibit viral infection of target cells, using the procedure described (Waiboci et al, 2007). BSC-40 cells were seeded to confiuency in a 6 well plate the day before the assay. Sera obtained from mice on days indicated were heated at 560C for 30 min to inactivate the complement. Purified vaccinia virus (100 pfu) was incubated with a known dilution of serum at 37°C for 1 hour, followed by addition to BSC-40 cells. One hour later, the virus containing media was replaced with fresh medium containing 0.5% agarose and 0.01% neutral red. Three days later, the number of plaques was counted. The number of plaques in wells with vaccinia alone was taken as 100%. Percent reduction in other treatments carried out in triplicates was measured and is presented as average with standard deviation.
Reporter gene assays. The plasmid pGL3 promoter, which expresses the firefly luciferase was obtained from Promega (Madison, WI). A sequence containing three copies of the GAS promoter element from human IRF-I gene, 5'- AGCCTGATTTCCCCGAAATGACGCG-3' (SEQ ID NO:74), was inserted in the multiple cloning site of pGL3. A constitutively expressed thymidine kinase promoter driven Renilla luciferase gene (pRL-TK) was used as an internal control in all of the reporter plasmid transfections. WISH cells were seeded in 12-well plates at 50% confiuency. The next day, 200 ng of GAS promoter-driven firefly luciferase and 10 ng of pRL-TK were cotransfected using lipofectamine reagent (Invitrogen, Carlsbad, CA). The indicated amounts of pJAK2(1001-1013) and/or IFNγ(95-132) peptide were added. One day later, the cell lysates were used to assay for firefly and Renilla luciferase, using a dual
luciferase assay kit from Promega, according to the manufacturer's instructions. Luciferase activity in relative luciferase units was standardised by dividing firefly by Renilla luciferase activity in each sample.
Statistical analysis. AU experimental data on mice studies were measured for statistical significance by Kaplan-Meier survival curve and log-rank test with the GraphPad Prism software from GraphPad Software, Inc., San Diego, CA.
Example 9 — pJAK2f 1001-1013) protects mice against lethal vaccinia virus infection
Key to SOCS-I inhibition of JAK2 kinase activity is the binding to the catalytic loop comprising the residues 1001-1013 of JAK2, with phosphorylated tyrosine at 1007 (Table 6) (Yasukawa et ah, 1999). We synthesized a peptide corresponding to the catalytic loop of JAK2 with a phosphotyrosine at 1007, pJAK2(l 001-1013), with a lipophilic group, palmitate, attached for cell penetration (Waiboci et ah, 2007). We reasoned that pJAK2(1001-1013) would enhance innate and possibly adaptive immunity by preventing SOCS-I from inhibiting IFN activity. We therefore examined pJAK2(1001-1013) for its ability to protect mice challenged with a lethal dose of the Western Reserve strain of vaccinia virus. C57BL/6 mice were injected LP. with 10, 50, and 200 μg of pJAK2(1001-1013) on days -2, -1, and 0 and challenged intranasally with 2 x 106 pfu of vaccinia virus (Figure 9). Complete protection was observed with 200 μg of SOCS-I antagonist, whereas 50 and 10 μg resulted in 80 and 20% protection from death, respectively. Recovered mice were completely free of any disease symptoms for the 40 days observed. A control peptide that consisted of alanine substitutions for tyrosines at residues 1007 and 1008 was not protective where all of the mice died by day 9. Thus, pJAK2(1001-1013) was able to completely protect mice against a lethal dose of vaccinia virus.
Example 10 — pJAK2(1001-1013) synergizes with an IFN mimetic in protecting mice against lethal vaccinia virus infection
We have developed small peptide mimetϊcs of TFNγ, based not on the classical model of IFNγ-initiatcd signaling by extracellular interaction, but rather on direct intracellular signaling by IFNγ. IFNγ, its receptor subunit IFNGRl. and transcription factor STATl α are transported to the nucleus of cells as a complex where IFNγ provides
a classical polycationic nuclear localization sequence (NLS) for such transport (Ahmed and Johnson, 2006). The C-terminus of IFNγ, represented here by the mouse IFNγ peptide, IFNγ(95-132), was capable of forming a complex with IFNGRl and STATIa when introduced intracellularly and provided the NLS for nuclear transport (Ahmed et al, 2003). The IFN mimetic is a potent inhibitor of vaccinia virus infection in mice (Ahmed el ai, 2007).
In order to determine if the SOCS-I antagonist can synergize with the IFN mimetic to protect mice against vaccinia virus, C57BL/6 mice were treated on days -2, -1, and 0 with suboptimal amounts of the two peptides either alone or in combination. Both peptides contain a lipophilic group (palmitate) for cell penetration. Combined treatment LP. with 10 μg of pJAK2(1001-1013) and 5 μg of IFNγ(95-132) resulted in complete protection of the mice against
1 x 106 pfu of intranasally administered vaccinia virus (Figure 10). Ten μg of antagonist plus 2 μg of mimetic resulted in 60% survival. Five μg and 2 μg of IFN mimetic alone resulted in 40 and 20% protection, respectively. Ten μg of SOCS-I antagonist alone resulted in 20% protection. Thus, we have shown here that SOCS-I antagonist and IFN mimetic can synergize to protect mice against vaccinia virus infection. The synergy or protection described here is similar to that originally observed by us with regards to type I and type II IFNs in induction of antiviral activity (Fleischmann et al. , 1979).
Example 11 — :Synergy between pJAK2(1001-1013) and IFNγ mimetic in activation of GAS promoter element
We have shown in Figure 10 that pJAK2(1001-1013) and the IFNγ mimetic IFNγ(95-132) synergized in protecting mice against vaccinia virus infection. In order to examine this synergy at the level of gene activation, we fused the IFNγ activated sequence (GAS) promoter with firefly luciferase and used this construct to transfect WISH cells. Co-transfection with a Renilla luciferase expression plasmid was carried out to normalize the expression of firefly luciferase and activation is expressed as relative luciferase units. The transfected cells were incubated with pJAK2(l 001-1013), IFNγ(95- 132), and the combination of the two for 24 hours, after which relative luciferase activity was measured. As shown in Figure 11, 10 μM of SOCS-I antagonist had minimal effect
on reporter activation, while 5 μM IFNγ mimetic was slightly more effective. Notably, 10 μM of antagonist plus 5 μM of IFNγ mimetic together had a greater than four-fold effect on gene activation than did IFNγ mimetic alone. This multiplicative effect is consistent with the synergy of protection against vaccinia virus of Figure 10. Thus, SOCS-I antagonist and IFNγ mimetic show synergy at the level of IFNγ gene activation.
Example 12 — pJAK2(l 001-1013) inhibits vaccinia virus replication as determined by a one-step growth curve
In order to determine if pJAK2(1001-1013) inhibits vaccinia virus replication as opposed to just inhibiting spread, we carried out a one-step growth curve experiment. BSC-40 cells were treated with lipophilic pJAK2(1001-1013) at 50 μM for 1 hour, followed by infection with 5 moi of vaccinia virus to ensure simultaneous infection of all cells for a one-step growth curve. pJAK2(1001-1013) inhibited virus replication by approximately 92% as determined by intracellular virus yield (Figure 12A) when compared to a variant, pJAK2(1001-1013)2A, with alanine substituted for tyrosine at positions 1007 and 1008 (Table 6). The alanine variant does not bind to KIR of SOCS-I (Unpublished observation). Inhibition was approximately 83% by extracellular virus yield (Figure 12B). Thus, the SOCS-I antagonist pJAK2(1001-1013) inhibited vaccinia virus replication and not simply its release from cells. The fact that the alanine substituted variant of the antagonist did not inhibit virus replication suggests that the specificity of the antiviral effects of the antagonist is directed at SOCS-I in the cells.
There was a dose-response effect in the inhibition of vaccinia virus replication by pJAK2(1001-1013), where 1 to 25 μM of antagonist resulted in a dose-response reduction in yield of both intracellular (Figure 13A) and extracellular (Figure 13B) virus with approximately 87% inhibition of yield at 25 μM. Thus, SOCS-I antagonist pJAK2(1001- 1013) specifically inhibited vaccinia virus replication.
Example 13 — pJAK2(1001-1013) treated cells had increased levels of endogenous IFNβ
For efficient induction of an antiviral state, cells contain low levels of spontaneously or constitutively produced IFNB (Takaoka et ah, 2000). A subtle increase in this low level of IFNB plays an important role in a positive feedback loop to increase type I IFN production and induction of a potent antiviral state in cells (Takaoka et ah,
2000). To determine if pJAK2(1001-1013) affected the level of spontaneous IFNB, we treated L929 fibroblasts with the SOCS-I antagonist as well as the alanine substituted variant, pJAK2(l 001-1013)2A. As seen in Figure 14A, cells treated with 12 or 24 μM of pJAK2(1001-1013) for 30 or 60 minutes showed a significant increase in IFNB as determined by Western blot, while the alanine-substituted variant had little or no effect on IFNB levels. By comparison, IFNa levels were not altered in the same cells (Figure 14B). Western blots for SOCS-I in the cells showed significant declines for pJAK2(1001-1013) treated cells, while the variant, pJAK2(1001-1013)2A, had no significant effect on the SOCS-I protein levels (Figure 14C). Thus, the increase in IFNB in the cells corresponded to a decrease in SOCS-I, and would suggest that the SOCS-I antagonist played a role in SOCS-I degradation, probably via proteasomal degradation mediated through the SOCS box of SOCS-I (Yoshimura et al, 2007).
As indicated above, we showed that IFNγ signaling involves a complex of IFNγ/IFNGRl/pSTATlα where the nuclear importins α and β bind to the complex via an NLS in IFNγ (and the IFNγ mimetic), which results in nuclear transport of the complex (Johnson et al., 2004). We further showed that the IFNγ receptor chain IFNGRl functions as a transcription/cotranscription factor in conjunction with pSTATlα (Ahmed and Johnson, 2006). These findings address the issue of specificity of gene activation and signaling by a plethora of cytokines, growth factors, and hormones that use the same STAT transcription factors but differ dramatically in the induced functions even under conditions where the same type of cells are involved (Johnson et ah, 2004). We have shown in the case of type I IFN signaling that importin β but not importin α directly binds the type I IFN receptor chain IFNARl (data not shown). Further, we have previously shown that IFNARl contains a functional NLS (Subramaniam and Johnson, 2004). Figure 14D shows the results of immunoprecipitations of IFNARl in whole cell extracts of Daudi cells under conditions of treatment with IFN α2. These results are consistent with the low level of function that is ascribed to endogenous IFNβ in untreated cells and the enhanced activity that occurs after exogenous IFN treatment (Takaoka et al, 2000).
Example 14 — Potent adaptive immunity develops in mice that are protected against lethal vaccinia virus infection by pJAK2(l QOl -1013) treatment
It has recently been shown that suppression of SOCS-I in dendritic cells by small interfering RNA (siRNA) enhances the immune response (Shen et ah, 2004). The question arises therefore, as to whether mice protected by the SOCS-I antagonist developed protective adaptive immunity to subsequent infection with a lethal dose of vaccinia virus. Mice protected by pJAK2(1001-1013) were rechallenged 10 weeks later with a second dose of 1 x 106 pfu of vaccinia virus administered intranasally without additional pJAK2(1001-1013) treatment. All five mice of the rechallenged group were protected against the lethality of the virus without showing symptoms of distress (Figure 15A). Naϊve control mice all died by day 9. Thus, the pJAK2(1001-1013), in addition to providing protection against the first exposure to vaccinia virus, also allowed the mice to develop protective adaptive immunity to subsequent challenge with vaccinia virus.
Various immunological parameters were examined in the combined vaccinia virus and pJAK2(1001-1013) treated mice. Splenocytes obtained 2 and 3 weeks after virus challenge from protected mice as well as from naϊve mice were incubated with purified UV-inactivated vaccinia virus in a proliferation assay. The protected mice had a stimulation index of 8 at 3 weeks post-challenge with the virus (Figure 15B). Splenocytes from the naive mice did not respond to vaccinia virus. The proliferation results suggest the induction of virus-specific CD4" T cells. Splenocytes were also tested for the production of the cytokine IFNγ by ELISPOT assay. Similar to the proliferative response, CD4-depleted splenocytes (105/well) exposed to vaccinia virus showed increased secretion of IFNγ by ELISPOT at 3 weeks after virus challenge (Figure 15C), suggesting the induction of vaccinia virus- specific cytotoxic CD8+ T cells. Control cells did not respond to virus.
Sera from protected mice were examined for antibodies over 4 weeks. As shown in Figure 15D, IgA antibodies peaked at 2 to 4 weeks, but were significant out to 4 weeks postinfection, while the IgG antibody response peaked over 2 to 4 weeks after challenge (Figure 15E). The IgA antibodies are particularly relevant to the intranasal route of virus challenge. The antibody response also resulted in the production of neutralizing antibodies that peaked at 2 to 4 weeks and probably involved both IgA and IgG antibodies to vaccinia virus as shown in Figure 15F. Thus, mice protected by
pJAK2(1001-1013) mounted both a strong cellular and humoral immune response to vaccinia virus.
Example 15 — pj AK2 exerts an adjuvant effect on the immune system In addition to its inhibitory effects on virus replication in cells and related to the potent anti-vaccinia response, we were interested in determining possible adjuvant effects of SOCS-I antagonist on the immune response. Accordingly, C57BL/6 mice were immunized LP. with 50 μg of bovine serum albumin (BSA), treated LP. with 200 μg of pJAK2(l 001-1013) on days -2, -1, arid 0, and then assessed for enhancement of cellular and humoral immune responses. Four weeks after immunization, splenocytes of the mice were stimulated in cell culture with 0.5 μg of BSA. As shown in Figure 16A, untreated mice or mice given PBS mounted a weak proliferation response. By comparison, mice treated with p.TAK2(1001-1013) had an approximately eight-fold greater proliferative response to BSA. The humoral immune response as assessed by the serum IgG antibody response to BSA in the mice was also significantly enhanced in the pJAK2(1001-1013) treated mice at 3 and 4 weeks post-immunization (Figure 16B). At the level of macrophage function, RAW264.7 cells treated with pJAK2(1001-1013) produced approximately a six-fold increase in nitric oxide (NO) upon lipopolysaccharide (LPS) stimulation compared with a control peptide (Figure 16C). These results demonstrate that pJAK2(1001-1013) has an adjuvant effect in terms of the cellular and humoral immune responses as well as in macrophage activation. Thus, in addition to direct inhibition of virus replication, the antagonist also has an adjuvant effect on the immune response.
Example 16 — SOCS-I antagonist possesses antiviral activity against a picornavirus Encephalomyocarditis (EMC) virus is a rodent picomavirus, but can infect other species, including humans. In contrast to the complex, large double stranded vaccinia virus, EMC virus is a relatively simple, small plus stranded RNA virus (Racaniello,
2007). It thus provides considerable contrast for assessing the antiviral effects of pJAK2(1001-1013). We treated L929 fibroblasts with the SOCS-I antagonist prior to infection with EMC virus, similar to the cell culture treatments above with vaccinia virus.
As shown in Figure 17 A, pJAK2(1001-1013) along with IFNγ and the IFNγ mimetic
IFNγ(95-132) significantly inhibited EMC virus growth in cells treated with 200 pfu per
well of virus. Specifically, the antagonist and IFNγ reduced CPE by approximately 50% at 24 μM and 100 units per ml, respectively, while the IFNγ mimetic at 24 μM was completely protective. Of note, alanine substituted SOCS-I antagonist was only about 7% protective at 24 μM. This is consistent with the inability of the alanine substituted antagonist to increase endogenous IFNB protein in L929 cells. Thus, the SOCS-I antagonist pJAK2(l 001-1013) inhibits EMC virus replication, similar to inhibition of vaccinia virus replication.
Example 17 — pJAK2(1001-1013) induces an antiviral state against EMC virus in the presence of antibodies to IFNβ
The increase in IFNB in cells treated with the SOCS-I antagonist raises the possibility that this IFN exerts its effects intracellularly and thus does not need to be secreted for subsequent interaction with the extracellular domain of the type I IFN receptor. To address this, we treated L929 cells with 24 μM pJAK2(l 001-1013) in the presence or absence of neutralizing antibodies to IFNB subsequent to infection with 200 pfu of EMC virus. Complete protection by antagonist was reduced to approximately 60 % in the presence of a saturating level of anti-IFNB antibody (Figure 17B). Alanine- substituted antagonist was not protective. The data suggest that some of the increased intracellular IFNB exerted its effects intracellularly. The ability of type I and type II IFNs to exert their effects intracellulariy has recently been well established (Ahmed et ai, 2001, 2003).
Example 18 — pJAK2(l 001 -1013) protects mice against lethal EMC virus infection
Based on the antiviral effects of pJAK2(1001-1013) in tissue culture, we tested the therapeutic effects of the antagonist in a mouse model of lethal EMC virus infection. C57BL/6 mice were treated i.p. with 50, 100, or 200 μg of pJAK2(1001-1013) or 200 μg of the alanine-substituted antagonist, pJAK2(100l -l Ol3)m with alanine substituted for tyrosine at residues 1007 and 1008, every day beginning at day -2. On day 0 the mice were challenged with 50 pfu of EMC virus per mouse and monitored daily for survival. As shown in Figure 17C, mice treated with the alanine-substituted antagonist all died by day 5 after EMC virus challenge. In contrast, mice treated with 100 and 200 μg ρJAK2(1001 -1013) showed 80% and 60% survival, respectively. Treatment with 50 μg of
pJAK2(1001-1013) resulted in 20% of mice surviving EMC virus challenge. Thus, administration of pJAK2(1001-1013) at 100 and 200 μg daily resulted in significant protection of mice.
Table 6. List of peptides.
Peptide Sequence pJAK2(1001-1013) UKTT LPQDKEYYKVKEP (SEQ ID NO: 1)
JAK2(1001-1013)m 1001 LPQDKEAAKVKEP (SEQ ID NO:71)
(alanine substituted control)
MuIFNγ(95-106) 95AKFEVNNPQVQR (SEQ ID NO:65)
MuIFNγ(95-125) 915AKFEVNNPQVQRQAFNELIRVVHQLLPESSL (SEQ ID NO:66)
MuIFNγ(95-132) 95AKFEVNNPQVQRQAFNELIRVVHQLLPESSLRKRKRSR (SEQ ID NO:67)
MuIFNGRl (253- 253TKKNSFKRKSIMLPKSLLSVVKSATLETKPESKYS (SEQ 287) ID NO:68)
All the peptides were synthesized with an attached lipophilic group, palmitic acid, for cell penetration. MuIFNγ(95-106), MuIFNγ(95-125), and MuIFNGRl (253-287) were used as control peptides. These peptides do not show significant biological activity in the assays for which they have been used as control peptides.
Example 19 — SQCS antagonist and IFN mimetic possess antiviral activity against HlNl influenza virus
We have tested our SOCS antagonist and IFN mimetic against the PR8 strain of influenza virus, which is of the HlNl type, the same as the swine flu virus. As shown in Figure 18, the antagonist ρJAK2(1001-1013) (pJAK2) (SEQ ID NO:1), inhibited virus replication in MDCK cells, while the mutant alanine substituted JAK2(1001-1013)2A (JAK2m) (SEQ ID NO:71) had little effect. The IFNγ mimetic, IFNγ(95-132), also inhibited influenza virus replication. These results evidence the broad antiviral activity of SOCS antagonist and IFNγ mimetic.
Example 20 — Synergistic protection against influenza A virus by SOCS antagonist and IFN-γ mimetic
MDCK cells were infected with influenza A PR8 virus and treated with SOCS antagonist pJAK2, IFN-γ (95-132) mimetic peptide, alone or in combination, and the virus yield was estimated by hemagglutinin assay. A combination of SOCS antagonist peptide and IFN-γ mimetic peptide provided synergistic protection against the influenza virus, as shown in Figure 19.
MATERIALS AND METHODS FOR EXAMPLES 21-26 Cell culture and virus. BSC-40, L929, WISH, or RAW264.7 cells were obtained from ATCC (Manassas, VA) and propagated on DMEM with 10% fetal bovine serum (BSC-40, L929, WISH), or RPMI 1640 with 10% fetal bovine serum (RAW264.7). All cells were grown at 370C in humidified atmosphere with 5% CO2. Vaccinia virus Western Reserve strain was a kind gift from Dr. Richard Condit (University of Florida). Vaccinia virus was grown, purified on sucrose gradient, and titrated on BSC-40 cells, as described (Ahmed et al. (2005)). EMC virus was grown and titrated on L929 cells, as described (Muitaba et al (2006)).
Peptides. The sequence of peptides used in this study is presented in Table 7. These peptides were synthesized on an Applied Biosystems 9050 automated peptide synthesizer using conventional fluorenylmethyloxycarbonyl chemistry as described previously (Szente et al. (1994)). The addition of a lipophilic group (palmitoyl-lysine) to the N-terminus of the synthetic peptide was performed as a last step, using semi- automated protocol. Peptides were characterized by mass spectrometry and were purified by HPLC. Mice. All animal protocols were approved by the Institutional Animal Care and
Use Committee (IACUC) at the University of Florida. Female C57BL/6 mice (6-8 weeks old) were purchased from Jackson Laboratories (Bar Harbor, ME). Peptides dissolved in PBS in a volume of 100 μl were administered intraperitoneally. For the oral administration of the peptides, indicated amounts of peptide in 0.5 ml PBS were given using a feeding needle. Intraperitoneal administration of EMCV was done in a volume of 100 μl. For intranasal administration, vaccinia virus was taken in a volume of 10 μl, and 5 μl was delivered in each of the nostrils of a lightly anesthetized mouse. Following
infection, mice were observed daily for signs of disease, such as lethargy, ruffled hair, weight loss, and eye secretions. Moribund mice were euthanized and counted as dead.
FITC labeling and detection of cell penetration. FITC was conjugated with lipo- pJAK2(1001-1013), according to the manufacturer's (Pierce, Rockford, IL) instruction. Mice were injected i.p. with 15 mg FITC-labeled lipo-pJAK2(1010-1013) or an equivalent amount of FITC alone. Two hours later, peritoneal cells were harvested and viewed in a fluorescent microscope. L929 cells were similarly treated with 5 niM FITC- labeled lipo-pJAK2(l 010-1013) or FITC alone for 2 h, followed by visualization in a fluorescent microscope. Reporter gene assays. The plasmid pGL3 promoter, which expresses the firefly luciferase was obtained from Promega (Madison, WI). A sequence containing three copies of the GAS promoter element from human IRF-I gene, 5'- AGCCTGATTTCCCCGAAATGACGCG-3' (SEQ ID NO:74), was inserted in the multiple cloning site of pGL3. A constitutively expressed thymidine kinase promoter driven Renilla luciferase gene (pRL~TK) was used as an internal control in all of the reporter plasmid transfections. WISH or L929 cells were seeded in 12-well plates at 50% confluency. The next day, 500 ng of GAS promoter-driven firefly luciferase and 50 ng of pRL-TK were cotransfected using lipofectamine reagent (Invitrogen, Carlsbad, CA). The indicated amounts of pJAK2(1001-1013) and/or IFNγ(95-132) peptide were added. One day later, the cell lysates were used to assay for firefly and Renilla luciferase, using a dual luciferase assay kit from Promega, according to the manufacturer's instructions. Luciferase activity in relative luciferase units was standardized by dividing firefly by Renilla luciferase activity in each sample. Where indicated, murine SOCS-I or SOCS-3 cDNA in CMV promoter driven constructs were included in the transfection. Measurement of intracellular and extracellular vaccinia virus formation. BSC-40 cells were seeded and grown overnight to confluency. Peptides at concentrations indicated were added to cells for one hour followed by infection with vaccinia virus at moi of 5 for one hour. This was followed by addition of growth medium containing the same amount of peptides as before and incubation for times indicated. Supernatants were harvested, and the cells were scraped in 0.2 ml of cell lysis buffer consisting of 50 niM Tris HCl (pH 7.5), 250 mM NaCl, 0.1% Nonidet P-40, 50 mM NaF, and 5 niM EDTA. followed by three cycles of freeze thawing and sonication. The virus titer in the
supernatant (extracellular) and cell extracts (intracellular) were measured by plaque assay on BSC-40 cells.
Western blot analysis. Western blot analysis was carried out to determine whether pJAK2(l 001-1013) had an effect on endogenous pSTATl , STATl , SOCS-I, IFNa, or IFNB levels. Cells were incubated with various concentrations of lipophilic pJAK2(1001- 1013) or JAK2(1001-1013)2A for 30 to 60 minutes. The cells were washed in cold PBS and harvested in RIPA buffer containing protease and phosphatase inhibitor cocktails (Santa Cruz Biotechnology, Santa Cruz, CA). Protein concentration was measured using a BCA kit (Pierce, Rockford, IL) and lysates were resolved on 12% SDS-PAGE, transferred onto nitrocellulose membranes, and probed with various antibodies. The membranes were then stripped and reprobed with the indicated anti-protein antibodies. IFN antibodies were from PBL (Piscataway, NJ), pSTATl and SOCS antibodies were custom made from GenScript (Pisactaway, NJ). STATl Abs were from Santa Cruz (Santa Cruz Biotechnology, Santa Cruz, CA). Scanning of the band intensity was carried out using Image J software from National Institutes of Health (Bethesda, MD).
IFN- β ELISA. L929 cells were treated with peptides for 30 or 60 min and then lysed with RIPA lysis buffer containing protease inhibitor cocktails (Sigma-Aldrich, St. Louis, MO). The cell lysates were analyzed with a murine IFN -β ELISA kit (PBL Biomedical Laboratories), following the manufacturer's instructions. Briefly, cell lysates were plated onto plate strips for 1 h at room temperature. The strips were washed three times with wash buffer and then incubated with the Ab solution for 1 h at room temperature. After washing the strips three times, they were incubated with the HRP solution for 1 h at room temperature. The strips were washed three times and incubated with TMB substrate solution for 15 min at room temperature. The reaction was stopped by addition of stop solution. The absorbance was measured at 450 nm with a standard plate reader (Bio-Tek Instruments, Winooski, VT).
Measurement of vaccinia virus specific cellular response by proliferation assay. Spleens from naive or recovered mice at times indicated were homogenized to single cell suspension. Splenocytes (10" cells per well) were incubated with medium alone, or medium containing UV-inactivated vaccinia virus at 370C for 96 hours. The cultures were then pulsed with [3H] -thymidine (1 μCi/well; Amersham Biosciences, Piscataway, NJ) for 8 hours before harvesting onto filter paper discs using a cell harvester. Cell associated
radioactivity was counted using a scintillation counter. Stimulation index refers to the incorporation in splenocytes cultured with test antigen divided by incorporation in splenocytes cultured with medium alone.
Measurement of vaccinia virus specific cellular response by IFN-γ ELISPOT. CD4-depletion of splenocytes from naϊve or recovered mice was carried out by using the L3T4 antibody bound to Dynabeads (Invitrogen, Carlsbad, CA). ELISPOT assay was carried out by using a kit from Mabtech USA. Briefly, CD4-depleted cells (10" per well) were seeded in a microtiter plate, previously coated with an antibody to IFNγ and incubated in the absence or presence of purified vaccinia virus (moi = 0.01) for 24 hours at 37°C. After washing, diluted monoclonal antibody was added and incubated for 2 hours, followed by washing and addition of streptavidin-HRP. After 1 hour at room temperature, the wells were washed and TMB substrate was added, washed and the spots were counted.
Measurement of anti-vaccinia antibody response by ELlSA. Microtiter plates were coated with 106 pfu of purified UV-inactivated vaccinia virus (900,000 μJ/cm2 for 5 min in a DNA cross-linker) in 100 μl of binding buffer (carbonate-bicarbonate, pH 9.6) overnight at 40C. Plates were blocked for 2 hours at room temperature with PBS containing 5% fetal bovine serum. Mouse sera was serially diluted in PBS containing 0.1% Tween-20 (wash buffer). 0.1 ml of the diluted serum was added to each well. The plate was incubated for 2 hours at room temperature and washed three times with wash buffer. Peroxidase-conjugated goat anti-mouse IgA (α chain specific), or IgG (γ chain specific) (both from Santa Cruz Biotechnology, Santa Cruz, CA), diluted in a volume of 0.1 ml, was added to each well, incubated for 1 hour, and washed five times with wash buffer. OPD in a volume of 0.1 ml was added and incubated for 15 min. The reaction was stopped by addition of 50 μl of 3 N HCl. The optical density at 490 nm was determined using a microtiter plate reader.
Measurement of vaccinia virus specific neutralizing antibodies. Plaque reduction assay was carried out to test the ability of antibodies to inhibit viral infection of target cells. BSC-40 cells were seeded to confluency in a 6 well plate the day before the assay. Sera obtained from mice on days indicated were heated at 560C for 30 min to inactivate the complement. Purified vaccinia virus (100 pfu) was incubated with a known dilution of serum at 370C for 1 hour, followed by addition to BSC-40 cells. One hour later, the virus
containing media was replaced with fresh medium containing 0.5% agarose and 0.01% neutral red. Two days later, the number of plaques was counted. The number of plaques in wells with vaccinia alone was taken as 100%. Percent reduction in other treatments carried out in triplicates was measured and is presented as average with standard deviation.
Binding assays. Binding assays were performed as previously described (Waiboci ei al. (2007)) withminor modifications. pJAK2(1001-1013) or JAK2(1001-1013)2A were bound to 96-well plates, in binding buffer (in 0.1 M carbonate-bicarbonate (pH 9.6)), at a final concentration of 3 μg/well. Weils were then washed in wash buffer (PBS containing 0.9% NaCl and 0.05% Tween 20), blocked with 2% gelatin and 0.05% Tween 20 in PBS for 1 h at room temperature, washed three times with wash buffer, and incubated with various concentrations of SOCSl-KIR or SOCS3-KIR for 1 h at room temperature in blocking buffer. Following incubation, wells were washed five times to remove unbound peptide. Bound peptides were detected by incubation with 1 :500 dilution of antibodies to SOCSl-KIR or SOCS3-KIR. After washing, detection was carried out with a goat anti- rabbit IgG-HRP conjugate, followed by the addition of OPD substrate and 2N H2SO4. Absorbance was measured using a 450-microplate reader (Bio-Rad) at 490 nm.
Macrophage stimulation. Murine macrophage cells, RAW 264.7, were seeded on 96-well plates at a concentration of 5 X 106 cells/well in 200 μl volume and allowed to adhere. Lipo peptides, pJAK2( 1001-1013) or the control peptide JAK2(1001-1013)2A, at 25 μM were then added to the wells and the cells incubated for 4 h, after which 2 μg/ml of LPS or 0.1 μg/ml polyI:C were added and the cells were incubated for 3 days. Supernatants were transferred to fresh tubes and assayed for NO production using Griess reagent, according to the manufacturer's instructions (Alexis Biochemicals, Plymouth Meeting, PA).
Antiviral assay for EMCV. Antiviral assays for EMCV were performed by using a cytopathic effect reduction assay. Murine L929 cells (6 x 104 cell/well) were seeded in a 96-well plate and grown overnight to confluence for optimal growth. Various concentrations of IFN-γ, IFN-γ(95-132), IFN-γ(95-125), pJAK2(1001-1013), and JAK2(1001-1013)2A were added and incubated for 2 h, after which 200 pfu/well of EMC virus was added to the plate and incubated. After 1 h, virus was removed, fresh media was added and incubated for 24 h. Cells were stained with 0.1% crystal violet.
Unbound crystal violet was aspirated, and the plates were thoroughly rinsed with deionized water, blotted, and allowed to air dry. Plates were then scanned and analyzed using Image J 1.29 software (National Institutes of Health, Bethesda, MD) to assess cell survival. Percentages of cell survival were determined by comparing survival for the experimental treatment groups with that for the virus-only control group.
Statistical analysis. All experimental data were measured for statistical significance by Student t test for peptide binding assays, by Kaplan-Meier survival curve and log-rank test for the mice studies, and by nonparametric (Wilcoxon-Mann- Whitney) tests for relative intensities in Western blots, using the GraphPad Prism software from GraphPad Software (San Diego, CA).
Example 21 — pJAK2(1001-1013) protects mice against lethal vaccinia virus infection
Key to SOCS-I inhibition of JAK2 kinase activity is the binding to the activation loop comprising the residues 1001-1013 of JAK2, with phosphorylated tyrosine at 1007 (Table 7) (Waiboci et al. (2007)). We synthesized a peptide corresponding to the activation loop of JAK2 with a phosphotyrosine at 1007, pJAK2(1001-1013), with a lipophilic group, palmitate, attached for cell penetration (Waiboci et al. (2007)). We reasoned that pJAK2(1001-1013) would enhance innate and possibly adaptive immunity by preventing SOCS-I from inhibiting IFN activity. We therefore examined p.TAK2(1001-1013) for its ability to protect mice challenged with a lethal dose of the Western Reserve strain of vaccinia virus. C57BL/6 mice were injected i.p. with 10, 50, and 200 μg of pJAK2(1001-1013) on days -2, -1 , and 0 and challenged intranasally with 2 x 10 pfu of vaccinia virus given intranasally (Figure 20). Complete protection was observed with 200 μg of SOCS-I antagonist, whereas 50 and 10 μg resulted in 80 and 20% protection from death, respectively. Recovered mice were completely free of any disease symptoms for the 30 days observed. A control peptide that consisted of alanine substitutions for tyrosines at residues 1007 and 1008, JAK2(1001-1013)2A, was not protective where all of the mice died by day 9. Thus, pJAK2(1001-1013) was able to completely protect mice against a lethal dose of vaccinia virus.
Table 7. List of peptides used in this study. Peptide Sequence
~pJAK2(1001-1013) ^'LPQDKEYYKVKEP (SEQ ID NO:1) JAK2(1001 - 1001LPQDKEAAKVKEP (SEQ ID NO:71)
1013)2 A alanine substituted control
MuIFNγ(95-106) 95AKFEVNNPQVQR (SEQ ID NO:65) MuIFNγ(95-125) 95AKFEVNNPQVQRQAFNELIRVVHQLLPESSL (SEQ ID
NO:66) MuIFNγ(95-l 32) 95AKFEVNNPQVQRQAFNELIRVVHQLLPESSLRKRKRSR
(SEQ ID NO:67)
SOCSl -KIR 53DTHFRTFRSHSDYRRI (SEQ ID NO:63)
SOCS3-KIR 20LRLKTFSSKSEYQLVV (SEQ ID NO:76)
All the peptides were synthesized with an attached lipophilic group, palmitic acid, for cell penetration. JAK2(1001-1013)2A, MuIFNγ(95-125), and MuIFNγ(95-106) were used as control peptides. These peptides do not show significant biological activity in the assays for which they have been used as control peptides.
In order to verify that palmitated (lipo)-pJAK2(1001-1013) was internalized by cells, we injected mice i.p. with 15 μg FITC-lipo-pJAK2(1001-1013) or treated L929 cells in culture with 5 μM FITC-lipo-pJAK2(1001-1013). An equivalent amount of FITC alone was used as a control. After 2 h, peritoneal cells or L929 cells were examined by confocal fluorescence microscopy for FITC uptake. As shown in Figure 2 IA, FITC-lipo- pJAK2(1001-1013), but not FITC alone was internalized by peritoneal cells. Similarly, FITC-lipo-pJAK2(1001-1013) was specifically taken up by L929 cells as shown in Figure 21B. Thus, the SOCS-I antagonist is internalized where it has access to the SOCS-I target.
Example 22 — pJAK2(1001 -1013) exerts an adjuvant effect on the immune system
In addition to its inhibitory effects on virus replication in cells and related to the potent anti-vaccinia response, we were interested in determining possible adjuvant effects of SOCS-I antagonist on the immune response. Accordingly, C57BL/6 mice were
immunized i.p. with 50 μg of bovine serum albumin (BSA), treated i.p. with 200 μg of pJAK2(1001-1013) on days -2, -1, and 0, and then assessed for enhancement of cellular and humoral immune responses. BSA is a relatively weak antigen in mice. Four weeks after immunization, splenocytcs from the mice were stimulated in cell culture with 0.5 μg of BSA. As shown in Figure 22A, untreated mice or mice given PBS mounted a weak proliferation response. By comparison, mice treated with pJAK2(1001-1013) had an approximately eight-fold greater proliferative response to BSA. The humoral immune response as assessed by the serum IgG antibody response to BSA in the mice was also significantly enhanced in the pJAK2(1001-1013) treated mice at 3 and 4 weeks post- immunization (Figure 22B). The SOCS antagonist can also enhance the antibody response to the T-cell independent antigen lipopolysaccharide (LPS). This is shown in Figure 22C, in which the antibody response of mice immunized with LPS was significantly enhanced by i.p. injection of pJAK2(1001-1013). We previously showed that staphylococcal entcrotoxin superantigens staphylococcal enterotoxin A (SEA) and staphylococcal enterotoxin B (SEB) enhanced T cell-dependent antibody production (Torres et al. (2002)), but SEA/SEB did not enhance the anti-LPS response. SEA/SEB did enhance the antibody response to bovine serum albumin (BSA), a T cell-dependent antigen. Thus, the SOCS antagonist has a direct effect on B cell function independent of T helper cells. At the level of macrophage toll-like receptor (TLR) function, RAW264.7 cells treated with pJAK2(1001-1013) produced approximately a five-fold increase in nitric oxide (NO) production upon lipopolysaccharide (LPS) stimulation (via TLR4) compared with a control peptide (Figure 22D). We also examined the effect of pJAK2(1001-1013) on TLR3 activation. Poly I:C is a synthetic double-stranded RNA (dsRNA) that activates macrophages and dendritic cells via TLR3 (Matsumoto and Seya (2008)). TLR3 thus plays an important role in the antiviral responses to HSV-I, influenza virus, cytomegalovirus, and respiratory syncytial virus, all of which have a dsRNA stage in their replication (Vercammen et al (2008); Pothlichet et al. (2008)). SOCS-I negatively regulates TLR signaling at several stages including signaling by type I IFNs and by NF- KB transcription factor (Yoshimura et al. (2007); Mansell et al. (2006); Yasukawa et al. (1999); Kobayashi et al. (2006)). Given the importance of TLR3 in the innate immune response against viruses, we treated the macrophage cell line RAW264.7 with poly I:C
and determined the enhancing effect of the SOCS-I antagonist pJAK2(1001-1013) on nitric oxide (NO) production. As shown in Figure 22E, poly I:C at 0.1 μg/ml had a negligible effect on NO production, which was increased over 20-fold by 25 μM pJAK2(l 001-1013). Alanine substituted JAK2(1001-1013)2A had a negligible effect on NO production. Thus, the SOCS-I antagonist enhanced the poly I:C activation of TLR3. The SOCS-I effect would suggest that SOCS-I induction has a regulatory effect on TLR3 activation and that the SOCS antagonist blocks this effect. These results demonstrate that pJAK2(1001-1013) has an adjuvant effect in terms of the cellular and humoral immune responses as well as in macrophage activation. Thus, in addition to direct inhibition of virus replication, the antagonist also has an adjuvant effect on the immune response.
Example 23— SOCS-I antagonist inhibits both SOCS-I and SOCS-3 function
As indicated the SOCS-I antagonist pJAK2(1001-1013) binds to SOCS-I via the SOCSl -KIR region (Yoshimura et al. (2007)). SOCS-3 also regulates immune functions and has been suggested to play the central role in inhibition of STAT3 activation in T helper 17 cells (Chen et al. (2006)). It is thus of interest with respect to possible regulation by the SOCS-I antagonist. As shown in Figures 23A and 23B, both SOCSl- KIR and SOCS3-KIR bound similarly to the SOCS-I antagonist. Since pJAK2(1001- 1013) represents the activation loop of JAK2, this would suggest that the antagonist would inhibit the function of both SOCS-I and SOCS-3. Accordingly, we co-transfected the mouse fibroblast L929 cell line with the IFN-γ GAS promoter coupled to the luciferase reporter gene and with SOCS-I or SOCS-3 cDNA expression plasmids. Reporter gene activity was inhibited in cells transfected with either SOCS cDNA, which was reversed by treatment of cells with the SOCS-I antagonist pJAK2(1001-1013) (Figure 23C). These results show that pJAK2(1001-1013) inhibits both SOCS-I and SOCS-3 function. Consistent with the binding results, JAK2 associated with SOCS-3 in L929 cells (Figure 23D). This, along with the reporter gene results in L929 cells suggests that pJAK2(1001-1013) interaction with SOCS3-KIR occurred at the level of SOCS-3 protein.
Example 24
To determine if the SOCS-I antagonist had any effect on STATIa activation, we treated cells with pJAK2(1001-1013) or JAK2(1001-1013)2A and probed for phosphorylated STATIa (Figure 24). Treatment with the SOCS antagonist at 25 μM increased pSTATla levels by >2-fold over untreated cells. Thus, pJAK2(1001-1013) enhances activation of STATIa.
Example 25
Synergy between pJAK2(1001-1013) and IFN-γ(95-132) was observed at treatments with suboptimal concentrations where 2 μM of SOCS-I antagonist and 5 μM of IFN-y mimetic combined completely protected L929 cells against EMC virus, whereas separately, the peptides at these concentrations showed 20% or less protection (Figure
25).
Example 26
Mice were infected with EMC virus and treated with suboptimal doses of pJAK2(l 001 -1013) and IFN-γ(95-132) in order to assess synergy. As shown in Figure 26, treatment with pJAK2(1001-1013) at 10 μg and IFN-γ(95-132) at 2 μg resulted in 80% survival of infected mice, while pJAK2(1001-1013) treatment alone resulted in 40% survival, the same as that of PBS-treated mice. IFN-γ(95-132) alone resulted in 60% survival of mice.
It should be understood that the examples and embodiments described herein are for illustrative purposes only and that various modifications or changes in light thereof will be suggested to persons skilled in the art and are to be included within the spirit and purview of this application and the scope of the appended embodiments. In addition, any elements or limitations of any invention or embodiment thereof disclosed herein can be combined with any and/or all other elements or limitations (individually or in any combination) or any other invention or embodiment thereof disclosed herein, and all such combinations are contemplated with the scope of the invention without limitation thereto.
REFERENCES
U.S. Patent No. 4,179,337
U.S. Patent No. 5,034,322 U.S. Patent No. 5,106,739 U.S. Patent No. 5,625,136 U.S. Patent No. 5,763,585 U.S. Patent No. 5,770,191 U.S. Patent No. 6,120,762
U.S. Published Patent Application No. 20020035243 U.S. Published Patent Application No. 20020120100
U.S. Published Patent Application No. 20030032594
Ahmed CM., K.N. Wills, HJ. Sugarman, D. E. Johnson, M. Ramachandra, T.L.
Nagabhushan, and J. A. Howe (2001). Selective expression of nonsecreted interferon by adenoviral vector confers antiproliferative and antiviral properties and causes reduction of tumor growth in nude mice. J. Interferon Cytokine Res 21 :
399-408.
Ahmed, CM. and H. M. Johnson (2006) IFN-gamma and its receptor subunit IFNGRl are recruited to the IFN-gamma-activated sequence element at the promoter site of IFN-gamma-activated genes: evidence of transactivational activity in IFNGRl. J. Immunol. 177:315-321
Ahmed, CM., J.P. Martin, and H. M. Johnson (2007) IFN mimetic as a therapeutic for lethal vaccinia virus infection: Possible effects on innate and adaptive immune responses. J. Immunol. 178:4576-4583.
Ahmed, CM., M.A. Burkhart, M. G. Mujtaba, and H.M. Johnson (2005) Peptide mimetics of interferon gamma possess antiviral properties against vaccinia and other viruses in the presence of poxvirus B8R protein. J. Virol 79:5632-5639.
Ahmed, CM., M.A. Burkhart, M.G. Mujtaba, P. S. Subramaniam, and H.M. Johnson (2003) The role of IFN gamma nuclear localization sequence in intracellular function. J Cell Sci. 116:3089-3098. Altschul, S. F. et al. (1990) "Basic Local Alignment Search Tool" J. MoI. Biol. 215:403- 410.
Altschul, S. F. el al (1997) "Gapped BLAST and PSI-BLAST: A New Generation of Protein Database Search Programs" Nucl. Acids Res. 25:3389-3402.
Arduino, P. G. and S.R. Porter (2008) Herpes Simplex Virus type I infection: Overview on relevant clinic-pathological features. J. Oral Pathol. Med. 37:107-121
Beltz, G.A., Jacobs, K. A., Eickbush, T. H., Cherbas, P. T., Kafatos, F. C. (1983) "Isolation of multigene families and determination of homologies by filter hybridization methods" Methods of Enzymoiogy, R. Wu, L. Grossman and K. Moldave [cds.] Academic Press, New York 100:266-285. Burgos, J.S., E. Serrano-Saiz, I. Sastre, and F. Valdivieso (2006) ICP47 mediates viral neuroinvasiveness by induction of TAP protein following intravenous inoculation of herpes simplex virus 1 in mice. J. Neurovirol. 12:420-427
Chee, A.V. and B. Roizman (2004) Herpes simplex virus 1 gene products occlude the interferon signaling pathway at multiple sites. J. Virol. 78:4185-4196 Chen, Z., A. Laurence, Y. Kanno, M. Pacher-Zavisin, B. Zhu, C. Tato. A. Yoshimura, L. Henninghausen, and J. J. O'Shea, JJ. 2006. Selective regulatory function of SOCS3 in the formation of IL-17-secreting cells. Proc. Natl Acad USA 103: 8137- 8142.
Cliffe, A.R. and D. M. Knipe (2008) Herpes Simplex Virus ICPO promotes both histone removal and acetylation on viral DNA during lytic infection. J Virol. 82:12030-
12038
Croker, B.A., H. Kiu, and S.E. Nicholson (2008) SOCS regulation of JAK/STAT signaling pathway. Sem. Cell Dew Biol. 19:414-422
Cunningham, A. L., RJ. Diefenbach. M. Miranda- S aksena, L. Bosnjak, M. Kim. C. Jones, and M.W. Douglas (2006) The cycle of human herpes simplex virus infection: virus transport and immune control. J. Infect. Dis. 194:S11-S18 de Boer, H. A., Comstock, L. J., Vasser, M. (1983) "The tac promoter: a functional hybrid derived from the trp and lac promoters" Proc. Natl. Acad. ScL USA 80(l):21-25. Decman, V., P.R. Kinchington, S.A. Harvey, and R.L. Hendricks (2005) Gamma interferon can block herpes simplex virus type 1 reactivation from latency, even in the presence of late gene expression. J. Virol. 79:10339-10347
Diefenbach, RJ., M. Miranda-Saksena, M.W. Douglas, and A. L. Cunningham (2008) Transport and egress of herpes simplex virus in neurons. Rev. Med. Virol. 18:35- 51
Dorsky D.I. and CS. Crumpacker (1987) Drugs five years later: acyclovir. Ann. Intern. Med. 107:859-874
Earl P. L., and B. Moss (1998). Characterization of recombinant vaccinia viruses and their products. In Current Protocols in Molecular Biology vol 2 Ausubel et al. Eds. Wiley Interscience, New York. 16.18.11-16.18.11.
Edison, K.M., W.E. Hobbs, BJ. Manning, P. Carlson, N.A. and DeLuca (2002) Expression of herpes simplex virus ICPO inhibits the induction of interferon- stimulated genes by viral infection. J. Virol. 76:2180-2191
Feigner, P.L., T.R. Gadek, M. Holm, R. Roman, H. W. Chan, M. Wenz, J.P. Northrop, G. M. Ringold, M. Danielsen (1987) "Lipofection: a highly efficient, Iipid- mediated DNA-transfection procedure" Proc Natl Acad Sci U.S.A. 84(21 ):7413- 7417.
Fleischmann, W. R., J.A. Georgiades, L.C. Osborne, and H.M. Johnson (1979) Potentiation of interferon activity by mixed preparation of fibroblast and immune interferon. Infection and Immunity. 26:248-253.
Flowers, L.O., H.M. Johnson, M.G. Mujtaba, M.R. Ellis, S.M. Haider, and P. S. Subramaniam (2004) Characterization of a peptide inhibitor of Janus kinase 2 that mimics suppressor of cytokine signaling 1 function. J. Immunol. 172:7510-7518
Frey, K.G., CM. Ahmed, R. Dabelic, E.N. Noon-Song, S.M. Haider, and H.M. Johnson (2009) HIV-I induced SOCS-I expression in keratinocytes: Use of a SOCS-I antagonist to block a novel mechanism of viral immune evasion. J. Immunol, (in press).
Goldsmith, K., W. Chen, D.C. Johnson, R.L. and Hendricks (1998) Infected cell protein (ICP) 47 enhances herpes simplex virus neurovirulence by blocking the CD8+ T cell response. J. Exp. Med. 187:341 -348
Gu, H. and B. Roizman (2009) The two functions of Herpes Simplex Virus 1 ICPO, inhibition of silencing by the CoREST/REST/HDAC complex and degradation of
PML, are executed in tandem. J. Virol. 83:181 -187
Halford, W.P., C. Weisend, J. Grace, M. Soboleski, DJ. Cair, J.W. Balliet, Y. Imai, T.P. Margolis, and B.M. Gebhardt (2006) ICPO antagonizes STATl -dependent repression of herpes simplex virus: Implications for the regulation of viral latency. Virology J. 3:44-49
Johnson H.M., P. S. Subramaniam, S. Olsnes, and D.A. Jans (2004). Trafficking and signaling pathways of nuclear localizing protein ligands and their receptors. BioEssays. 26: 993-1004.
Karlin S., Altschul, S. F. (1990) "Methods for Assessing the Statistical Significance of Molecular Sequence Features by Using General Scoring Schemes" Proc. Natl.
Acad. ScL USA 87:2264-2268.
Karlin S., Altschul, S. F. (1993) "Applications and Statistics for Multiple High-Scoring Segments in Molecular Sequences" Proc. Natl. Acad. ScL USA 90:5873-5877.
Kazmierski. W. M. (Ed.) (1998) Peptidomimetics Protocols (Methods in Molecular Medicine), Humana Press.
Knickelbein, J.E., K.M. Khanna, M.B. Yee, CJ. Baty, P.R. Kinchington, and R.L. Hendricks (2008) Noncytotoxic lytic granule-mediated CD8+ T cell inhibition of HSV-I reactivation from neuronal latency. Science 322:268-271
Kobayashi, T., G. Takaesu, and A. Yoshimura (2006) Mal-function of TLRs by SOCS. Nat. Immunol. 7: 123-124.
Koelle, D.M. and L. Corey (2008) Herpes Simplex: Insights on pathogenesis and possible vaccines. Ann. Rev. Med. 59:381-395
Lucet, LS., E. Fantino, M. Styles, R. Bamert, O. Patel, S. E. Broughton et al. (2006) The structural basis of Janus kinase 2 inhibition by a potent and specific pan-Janus kinase inhibitor. Blood 107:176-183
Maniatis, T., Fritsch, E. F., Sambrook, J. (1982) Molecular Cloning: A Laboratory Manual, Cold Spring Harbor Laboratory, Cold Spring Harbor, NY.
Mansell, A., R. Smith, SX. Doyle, P. Gray, J.E. Fenner, PJ. Crack et al. (2006) Suppressor of cytokine signaling 1 negatively regulates Toll-like receptor signaling by mediating MaI degradation. Nat. Immunol 7:148-155
Matsumoto, M., and T. Seya T. 2008. TLR3: Interferon induction by double-stranded RNA including poly(I:C). Advanced Drug Deliv. Rev. 60: 805-812.
Merrifield, R.B. (1963) "Solid Phase Peptide Synthesis. 1. The Synthesis of a Tetrapeptide" J. Amer. Chem. Soc. 85:2149-2154.
Mikloska, Z., V.A. Danis, S. Adams, A.R. Lloyd, D. L. Adrian, and A.L. Cunningham (1998) In vivo production of cytokines and beta (C-C) chemokines in human recurrent herpes simplex lesions-do herpes simplex virus-infected keratinocytes contribute to their production? J Infect Dis 177:827-838
Moss, B. (2007) Poxviridae. In Fields Virology, 3rd ed. D. M. Knipe, and P.M. Howley, eds. Lippincott, Williams, and Wilkins, Philadelphia, PA. 2905-2945.
Moss, B. and J. L. Shisler (2001) Immunology 101 at poxvirus U: immune evasion genes. Semin. Immunol. 13:59-66.
Mossman, K. (2005) Analysis of anti-interferon properties of the herpes simplex virus type 1 ICPO protein. Methods MoI Med 116:195-205
Mujtaba, M.G., CB. Patel, R.A. Patel, L.O. Flowers, M.A. Burkhart, L.W. WaibocL J.
Martin, M.I. Haider, CM. Ahmed, and H.M. Johnson (2006) The gamma interferon mimetic peptide IFN-gamma (95-132) prevents encephalomyocarditis virus infection both in tissue culture and in mice. Clin Vaccine Immunol 13:944-
952.
Palese, P. and M.L. Shaw (2007) Orthomyxoviridae: The viruses and their replication. In Fields Virology, 3rd ed. D. M. Knipe, and P.M. Howley, eds. Lippincott, Williams, and Wilkins, Philadelphia, PA. 1647-1689.
Patel, A.R., P. Romanelli, B. Roberts, and R.S. Kirsner (2007) Treatment of herpes simplex virus infection: rationale for occlusion. Adv. Skin Wound Care 20:408- 412
Poon, A.P., H. Gu, and B. Roizman (2006) ICPO and Us3 protein kinase of herpes simplex virus 1 independently block histone deacetylation to enable gene expression. Proc. Natl. Acad. ScL USA 103:9993-9998
Pothlichet, J., M. Chignard, and M. Si-Tahar (2008) Cutting edge: innate immune response triggered by influenza A virus is negatively regulated by SOCSl and SOCS3 through a RIG-I /IFNARl -dependent pathway. J. Immunol. 180:2034- 2038.
Racaniello, V.R. (2007) Picornaviridae: The viruses and their replication. In Fields Virology, 3rd ed. D. M. Knipe, and P.M. Howley, eds. Lippincott, Williams, and Wilkins, Philadelphia, PA. 795-838.
Roizman, B.D., Knipe, M., and Whitley, RJ. (2007) "Herpes Simplex Viruses" In Fields VViirroollooggyy,, 33rr eedd.. DD.. MM.. KKnniippee,, aanndd PP..M. Howley, eds. Lippincott, Williams, and Wilkins, Philadelphia, PA. 2501-2602
Sekulovich, R.E., K. Leary, and R.M. Sandri-Goldin (1988) The herpes simplex virus type 1 alpha protein ICP27 can act as a trans-repressor or a trans-activator in combination with ICP4 and ICPO. J. Virol. 62:4510-4522
Shen L., K. Evel-Kabler, R. Strube, and S.Y. Chen (2004). Silencing SOCS-I enhances antigen presentation by dendritic cells and antigen-specific anti-tumor immunity.
Nat Biotechnology 22: 1546- 1553.
Sheridan, B.S., J. E. Knickelbein, and R.L. Hendricks (2007) CD8+ T cells and latent herpes simplex virus type 1 : keeping the peace in sensory ganglia. Expert Opin Biol Ther 7:1323-1331 Stow, N.D. and E.C. Stow (1986) Isolation and characterization of a Herpes Simplex Virus type 1 mutant containing a deletion within the gene encoding the immediate early polypeptide Vmwl l O. J. Gen. Virol. 67:2571-2585
Subramaniam P.S., and H.M. Johnson (2004). The IFNARl subunit of the type I IFN receptor complex contains a functional nuclear localization sequence. FEBS Lett 578: 207-210.
Szente, B. E., LJ. Weiner, MJ. Jablonsky, N. R. Krishna, B.A. Torres, and H.M. Johnson (1996) Structural requirements for agonist activity of a murine interferon-gamma peptide. J. Interferon Cytokine Res. 16:813-817
Szente, B. E., J. M. Soos, and H.M. Johnson (1994) The C-terminus of IFN gamma is sufficient for intracellular function. Biochem. Biophys. Res. Commun. 203:1645-
1654.
Szretter K.J., S. Gangappa, J.A. Besler, H. Zeng, H. Chen, Y. Matsuoka S. Sambhara, D.E. Swayne, T.M. Tumpey, and J.M. Katz (2009). Early control of H5N1 influenza virus replication by the type I interferon response in mice. J. Virol. 83: 5825-5834.
Takaoka A., Y. Mitani, H. Suemori, M. Sato, T. Yokochi, S. Noguchi, N. Tanaka, and T. Taniguchi (2000) Cross talk between interferon-γ and -a/β signaling components in caveolar membrane domains. Science 288:2357-2360.
Tam, J. P. (1988) "Synthetic Peptide Vaccine Design: Synthesis and Properties of a High-Density Multiple Antigenic Peptide System" Biochemistry 85:5409-5413.
Thiam, K., E. Loing, C. Verwaerde, C. Auriault, and H. Gras-Masse et al. (1999) IFN- gamma-derived lipopeptides: influence of lipid modification on the conformation and the ability to induce MHC class II expression on murine and human cells. J.
Med. Chem. 42:3732-3736 Torres, B. A., G. Q. Perrin, M. G. Mujtaba, P. S. Subramaniam, A. K. Anderson, and H. M. Johnson. 2002. Supcrantigen enhancement of specific immunity: antibody production and signaling pathways. J. Immunol. 169:2907-2914.
Vercammen, E., J. Staal, and R. Beyaert. 2008. Sensing of viral infection and activation of innate immunity by toll-like receptor 3. CHn. Microb. Rev. 21 : 13-25. Waiboci, L.W., CM. Ahmed, M.G. Mujtaba, L.O. Flowers, J.P. Martin et al. (2007) Both the suppressor of cytokine signaling 1 (SOCS-I) kinase inhibitory region and
SOCS-I mimetic bind to JAK2 autophosphorylation site: implications for the development of a SOCS-I antagonist. J. Immunol. 178:5058-5068
WaId, A. and K. Link (2002) Risk of human immunodeficiency virus infection in herpes simplex virus type 2-seropositive persons: a meta-analysis. J. Infect. Dis. 185:45- 52
Xu, D., McElroy, D., Thornburg, R. W., Wu, R. el al. (1993) "Systemic induction of a potato pin2 promoter by wounding, methyl jasmonate, and abscisic acid in transgenic rice plants" Plant Molecular Biology 22:573-588.
Yasukawa, H., H. Misawa, H. Sakamoto, M. Masuhara, A. Sasaki, T. Wakioka et al. (1999) The JAK-binding protein JAB inhibits Janus tyrosine kinase activity through binding in the activation loop. EMBO J. 18 : 1309- 1320
Yokota, S., N. Yokosawa. T. Okabayashi, T. Suzutani, S. Miura, K. Jimbow, and N. Fujii (2004) Induction of suppressor of cytokine signaling-3 by Herpes Simplex Virus type 1 contributes to inhibition of interferon signaling pathway. J. Virol. 78:6282- 6286
Yoshimura, A., T. Naka, and M. Kubo (2007) SOCS proteins, cytokine signalling and immune regulation. Nat. Rev. Immunol. 7:454-465
Claims
1 : A method for treating or preventing infection by a virus in a human or animal, said method comprising administering to the person or animal an effective amount of i) a peptide or pcptidomimetic that is an antagonist of a SOCS-I and/or SOCS-3 protein, or ii) a polynucleotide that encodes a peptide that is an antagonist of a SOCS-I and/or SOCS-3 protein.
2: The method according to claim 1, wherein the peptide or peptidomimetic corresponds to the activation loop of a JAK2 protein.
3: The method according to claim 1, wherein the peptide comprises the amino acid sequence of SEQ ID NO:1, or a fragment thereof that exhibits antiviral activity.
4: The method according to claim 3, wherein one or both tyrosine amino acids of SEQ ID NO:1 is phosphorylated.
5: The method according to claim 4, wherein the tyrosine at amino acid position 7 of SEQ ID NO:1 is phosphorylated.
6: The method according to claim 1, wherein the virus is a herpes virus, poxvirus, or picomavirus.
7: The method according to claim 1, wherein the virus is a vaccinia virus, encephalomyocarditis (EMC) virus, influenza virus, herpes simplex virus (HSV), cytomegalovirus (CMV), herpes zoster virus, and other herpes viruses, poxvirus, coxsackie virus, lenti virus, or picomavirus.
8: The method according to claim 7, wherein the influenza virus is an influenza A virus.
9: The method according to claim 8, wherein the influenza A virus is serotype HlNl .
10: The method according to claim 1, wherein the peptide or peptidomimetic or polynucleotide is administered to the person or animal prior to infection by the virus.
] 1 : The method according to claim 1 , wherein the peptide or peptidomimetic or polynucleotide is administered in conjunction with one or more antiviral compounds.
12: The method according to claim 11, wherein the antiviral compound is IFNa, IFNβ, IFNγ, acyclovir (Zovirax), zidovudine (AZT), lamivudine (3TC), zanamivir (Relenza), oseltamivir (Tamiflu), valacyclovir (Valtrex), amantadine (Symmetrel), rimantadine (Flumadine), cidofovir (Vistide), foscarnet (Foscavir), ganciclovir (Cytovene), ribavirin (Virazole), nelfinavir (Viracept), ritonavir (Norvir), rifampin (Rifadin), or famciclovir (Famvir).
13: The method according to claim 1, wherein the peptide or peptidomimetic or polynucleotide is administered in conjunction with an interferon -gamma (IFN-γ) peptide mimetic.
14: The method according to claim 13, wherein the IFN -γ peptide mimetic comprises the amino acid sequence shown in SEQ ID NO:67 or SEQ ID NO:75, or a fragment thereof that exhibits antiviral activity.
15: The method according to claim 1, wherein the peptide or peptidomimetic or polynucleotide are provided in a carrier means for delivering the peptide or peptidomimetic or polynucleotide to a cell and, optionally, facilitating transport of the peptide or peptidomimetic or polynucleotide into the cell.
16: The method according to claim 15, wherein the carrier means comprises liposome encapsulating the peptide or peptidomimetic or polynucleotide.
17: The method according to claim 15, wherein the carrier means comprises a protein or nucleic acid that is attached to the peptide or peptidomimetic or polynucleotide and that
J:'
targets delivery to the cell and/or that provides for translocation of the peptide or peptidomimetic or polynucleotide across a biological membrane of the cell.
18: A method for inducing an antiviral state in a cell, comprising contacting the cell with an effective amount of i) a peptide or peptidomimetic that is an antagonist of a SOCS-I and/or SOCS-3 protein, or ii) a polynucleotide that encodes a peptide that is an antagonist of a SOCS-I and/or SOCS-3 protein.
19: The method according to claim 18, wherein the peptide or peptidomimetic corresponds to the activation loop of a J AK2 protein.
20: The method according to claim 18, wherein the peptide comprises the amino acid sequence of SEQ ID NO:1, or a fragment thereof that exhibits antiviral activity.
21 : The method according to claim 20, wherein one or both tyrosine amino acids of SEQ ID NO:1 is phosphorylated.
22: The method according to claim 21, wherein the tyrosine at amino acid position 7 of SEQ ID TNO: 1 is phosphorylated.
23: The method according to claim 18, wherein the virus is a herpes virus, poxvirus, or picornavirus.
24: The method according to claim 18, wherein the virus is a vaccinia virus, encephalomyocarditis (EMC) virus, influenza virus, herpes simplex virus (HSV), cytomegalovirus (CMV), herpes zoster virus, and other herpes viruses, poxvirus, coxsackie virus, lentivirus, or picornavirus.
25: The method according to claim 24, wherein the influenza virus is an influenza A virus.
26: The method according to claim 25, wherein the influenza A virus is serotype
HlNl.
27: The method according to claim 18, wherein the peptide or peptidomimetic or polynucleotide is contacted with the cell prior to infection by the virus.
28: The method according to claim 18, wherein the peptide or peptidomimetic or polynucleotide is contacted with the cell in conjunction with one or more antiviral compounds.
29: The method according to claim 28, wherein the antiviral compound is IFNa, IFNβ, IFNγ, acyclovir (Zovirax), zidovudine (AZT), lamivudine (3TC), zanamivir (Relenza), oseltamivir (Tamiflu), valacyclovir (Valtrex), amantadine (Symmetrel), rimantadine (Flumadine), cidofovir (Vistide), foscarnet (Foscavir), ganciclovir (Cytovene), ribavirin (Virazole), nelfinavir (Viracept), ritonavir (Norvir), rifampin (Rifadin), or famciclovir (Famvir).
30: The method according to claim 18, wherein the peptide or peptidomimetic or polynucleotide is administered in conjunction with an interferon-gamma (IFN-γ) peptide mimetic.
31 : The method according to claim 30, wherein the IFN-γ peptide mimetic comprises the amino acid sequence shown in SEQ ID IMO:67 or SEQ ID NO:75, or a fragment thereof that exhibits antiviral activity.
32: The method according to claim 18, wherein the peptide or peptidomimetic or polynucleotide are provided in a carrier means for delivering the peptide or peptidomimetic or polynucleotide to a cell and, optionally, facilitating transport of the peptide or peptidomimetic or polynucleotide into the cell.
33: The method according to claim 32, wherein the carrier means comprises liposome encapsulating the peptide or peptidomimetic or polynucleotide.
34: The method according to claim 32, wherein the carrier means comprises a protein or nucleic acid that is attached to the peptide or peptidomirnetic or polynucleotide and that targets delivery to the cell and/or that provides for translocation of the peptide or peptidomirnetic or polynucleotide across a biological membrane of the cell.
35: A method for treating an oncological disorder in a person or animal, comprising administering to the person or animal an effective amount of i) a peptide or peptidomimetic that is an antagonist of a SOCS-I and/or SOCS-3 protein, or ii) a polynucleotide that encodes a peptide that is an antagonist of a SOCS-I and/or SOCS-3 protein.
36: The method according to claim 35, wherein the peptide or peptidomimetic corresponds to the activation loop of a J AK2 protein.
37: The method according to claim 35, wherein the peptide comprises the amino acid sequence of SEQ ID NO:1 , or a fragment thereof that exhibits antiviral activity.
38: The method according to claim 37, wherein one or both tyrosine amino acids of SEQ ID NO:1 is phosphorylated.
39: The method according to claim 38, wherein the tyrosine at amino acid position 7 of SEQ ID NO:1 is phosphorylated.
40: The method according to claim 35, wherein the peptide or peptidomimetic or polynucleotide is administered in conjunction with one or more anticancer or antitumor compound for treating an oncological disorder.
41 : The method according to claim 40, wherein the anticancer or antitumor compound is taxol, vinblastine, cyclophosamide, ifosfamide, 5-fluorouracil, hydroxyurea, adriamycin, bleomycin, etoposide, camptothecin, angiostatin, tamoxifen, GLEEVEC, HERCEPTIN, Bortezomib, Carfilzomib, or Salinosporamide A.
42: The method according to claim 35, wherein the oncological disorder is cancer and/or tumors of the anus, bile duct, bladder, bone, bone marrow, bowel (including colon and rectum), breast, eye, gall bladder, kidney, mouth, larynx, esophagus, stomach, testis, cervix, head, neck, ovary, lung, mesothelioma, neuroendocrine, penis, skin, spinal cord, thyroid, vagina, vulva, uterus, liver, muscle, pancreas, prostate, blood cells (including lymphocytes and other immune system cells), and brain; carcinomas, Karposi's sarcoma, melanoma, mesothelioma, soft tissue sarcoma, pancreatic cancer, lung cancer, leukemia (acute lymphoblastic, acute myeloid, chronic lymphocytic, chronic myeloid, and other), lymphoma (Hodgkin's and non-Hodgkin's), and multiple myeloma.
43: The method according to claim 35, wherein the peptide or peptidomimetic or polynucleotide are provided in a carrier means for delivering the peptide or peptidomimetic or polynucleotide to a cell and, optionally, facilitating transport of the peptide or peptidomimetic or polynucleotide into the cell.
44: The method according to claim 43, wherein the carrier means comprises liposome encapsulating the peptide or peptidomimetic or polynucleotide.
45: The method according to claim 43, wherein the carrier means comprises a protein or nucleic acid that is attached to the peptide or peptidomimetic or polynucleotide and that targets delivery to the cell and/or tbat provides for translocation of the peptide or peptidomimetic or polynucleotide across a biological membrane of the cell.
46: A peptide or peptidomimetic that is an antagonist of a SOCS-I and/or SOCS-3 protein and that exhibits antiviral activity.
47: The peptide or peptidomimetic according to claim 46, wherein the peptide or peptidomimetic corresponds to the activation loop of a JAK2 protein.
48: The peptide or peptidomimetic according to claim 46, wherein the peptide comprises the amino acid sequence of SEQ ID NO: 1, or a fragment thereof that exhibits antiviral activity.
J:\
49: The peptide or peptidomimetic according to claim 48, wherein one or both tyrosine amino acids of SEQ ID NO:1 is phosphorylated.
50: The peptide or peptidomimetic according to claim 49, wherein the tyrosine at amino acid position 7 of SEQ ID NO:1 is phosphorylated.
51: The peptide or peptidomimetic according to claim 46, wherein the peptide or peptidomimetic comprises a protein or nucleic acid that is attached to the peptide or peptidomimetic and that targets delivery to the cell and/or that provides for translocation of the peptide or peptidomimetic across a biological membrane of the cell.
52: The peptide or peptidomimetic according to claim 46, wherein a lipophilic group is attached thereto.
53: The peptide or peptidomimetic according to claim 52, wherein the lipophilic group is a palmitoyl-lysine group.
54: A composition comprising i) a peptide or peptidomimetic according to any of claims 46-53, or ii) a polynucleotide that encodes a peptide according to any of claims 46-53; and a suitable carrier, diluent, or buffer.
55: The composition according to claim 54, wherein the composition further comprises i) one or more antiviral compounds, or ii) one or more anticancer or antitumor compounds.
56: The composition according to claim 55, wherein the one or more antiviral compound is IFNα, IFNβ, IFNγ, acyclovir (Zovirax), zidovudine (AZT), lamivudine (3TC), zanamivir (Relenza), oseltamivir (Tamiflu), valacyclovir (Valtrex), amantadine (Symmetrel), rimantadine (Flumadine), cidofovir (Vistide), foscarnet (Foscavir), ganciclovir (Cytovene), ribavirin (Virazole), nelflnavir (Viracept), ritonavir (Norvir), rifampin (Rifadin), or famciclovir (Famvir).
57: The composition according to claim 55, wherein the one or more antiviral compounds is an interferon-gamma (IFN-γ) peptide mimetic.
58: The composition according to claim 57, wherein the IFN-γ peptide mimetic comprises the amino acid sequence shown in SEQ ID NO:67 or SEQ ID NO:75, or a fragment thereof that exhibits antiviral activity.
59: The composition according to claim 54, wherein the one or more anticancer or antitumor compound is taxol, vinblastine, cyclophosamide, ifosfamide, 5-fluorouracil, hydroxyurea, adriamycin, bleomycin, etoposide, camptothecin, angiostatin, tamoxifen, GLEEVEC, HERCEPTIN, Bortezomib, Carfilzomib, or Salinosporamide A.
60: A kit comprising in one or more containers: i) a peptide or peptidomimetic according to any of claims 46-53; ii) a polynucleotide encoding a peptide according to any of claims 46-53; and/or iii) a composition according to any of claims 55-59.
61: A method for modulating an immune response associated with expression or activity of a SOCS-I and/or SOCS-3 protein in a person or animal, said method comprising administering to the person or animal an effective amount of one or more of: i) a peptide or peptidomimetic according to any of claims 46-53; ii) a polynucleotide encoding a peptide according to any of claims 46-53; and/or iii) a composition according to any of claims 55-59.
62: The method according to claim 1, wherein a lipophilic group is attached to the peptide or peptidomimetic.
63: The method according to claim 18, wherein a lipophilic group is attached to the peptide or peptidomimetic.
64: The method according to claim 35, wherein a lipophilic group is attached to the peptide or peptidomimetic.
65: The method according to claim 62, wherein the lipophilic group is a palmitoyl- lysine group.
66: The method according to claim 63, wherein the lipophilic group is a palmitoyl- lysine group.
67: The method according to claim 64, wherein the lipophilic group is a palmitoyl- lysine group.
J:1
Applications Claiming Priority (4)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US22092009P | 2009-06-26 | 2009-06-26 | |
| US61/220,920 | 2009-06-26 | ||
| US35412410P | 2010-06-11 | 2010-06-11 | |
| US61/354,124 | 2010-06-11 |
Publications (2)
| Publication Number | Publication Date |
|---|---|
| WO2010151495A2 true WO2010151495A2 (en) | 2010-12-29 |
| WO2010151495A3 WO2010151495A3 (en) | 2011-04-28 |
Family
ID=43387105
Family Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| PCT/US2010/039195 WO2010151495A2 (en) | 2009-06-26 | 2010-06-18 | Materials and methods for treating and preventing viral infections |
Country Status (1)
| Country | Link |
|---|---|
| WO (1) | WO2010151495A2 (en) |
Cited By (10)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| WO2012013979A1 (en) * | 2010-07-28 | 2012-02-02 | The University Court Of The University Of Edinburgh | Anti-viral agent |
| CN102964432A (en) * | 2012-11-22 | 2013-03-13 | 中国科学院微生物研究所 | Method for restraining phosphorylation of M1 protein of influenza virus A and applications of method |
| CN103007350A (en) * | 2012-12-14 | 2013-04-03 | 中国人民解放军第三军医大学第二附属医院 | Modified rat accellular spinal cord bracket material and preparation method thereof |
| JP2013516170A (en) * | 2009-12-31 | 2013-05-13 | バイオリオン テクノロジーズ ビー.ブイ. | Interferon analog |
| CN103266086A (en) * | 2013-06-15 | 2013-08-28 | 中国人民解放军第一七四医院 | Method for preparing dendritic cells for effectively submitting gastric cancer antigens |
| US20140134237A1 (en) * | 2011-06-21 | 2014-05-15 | University Of Florida Research Foundation, Inc. | Type i interferon mimetics as therapeutics for cancer, viral infections, and multiple sclerosis |
| WO2015181427A1 (en) | 2014-05-28 | 2015-12-03 | Fundació Hospital Universitari Vall D'hebron - Institut De Recerca | Socs1-derived peptide for use in chronic complications relating to diabetes |
| EP3096775A4 (en) * | 2014-01-24 | 2017-10-11 | University of Florida Research Foundation, Inc. | Socs mimetics for the treatment of diseases |
| CN110183515A (en) * | 2019-04-28 | 2019-08-30 | 浙江中医药大学 | It is a kind of for PTP1B detection polypeptide and include the fluorescence probe of the polypeptide |
| CN114502570A (en) * | 2019-07-16 | 2022-05-13 | 吉恩森有限公司 | Peptide therapeutics for autoimmune and inflammatory diseases |
Citations (2)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US20020142466A1 (en) * | 1999-04-20 | 2002-10-03 | Flier Jeffrey S. | Methods and compositions for modulating ciliary neurotrophic factor activity |
| US6683052B1 (en) * | 1998-02-06 | 2004-01-27 | Institut National De La Sante Et De La Recherche Medicale Inserm | Lipopeptides containing an interferon-γ fragment, and uses thereof in pharmaceutical compositions |
-
2010
- 2010-06-18 WO PCT/US2010/039195 patent/WO2010151495A2/en active Application Filing
Patent Citations (2)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US6683052B1 (en) * | 1998-02-06 | 2004-01-27 | Institut National De La Sante Et De La Recherche Medicale Inserm | Lipopeptides containing an interferon-γ fragment, and uses thereof in pharmaceutical compositions |
| US20020142466A1 (en) * | 1999-04-20 | 2002-10-03 | Flier Jeffrey S. | Methods and compositions for modulating ciliary neurotrophic factor activity |
Non-Patent Citations (4)
| Title |
|---|
| AHMED, C. M. ET AL.: 'Enhancement of antiviral immunity by small molecule antagonist of suppressor of cytokine signaling.' J. IMMUNOL. vol. 185, no. 2, 11 June 2010, pages 1103 - 1113 * |
| FREY, K. G. ET AL.: 'HSV-1-induced SOCS-1 expression in keratinocytes: use of a SOCS-1 antagonist to block a novel mechanism of viral immune evasion.' J. IMMUNOL. vol. 183, no. 2, 19 June 2009, pages 1253 - 1262 * |
| MULLINS, D. W. ET AL.: 'Taxol, a microtubule-stabilizing antineoplastic agent, differentially regulates normal and tumor-bearing host macrophage nitric oxide production.' IMMUNOPHARMACOLOGY. vol. 37, no. 1, August 1997, pages 63 - 73 * |
| WAIBOCI, L. W. ET AL.: 'Both the suppressor of cytokine signaling 1 (SOCS-1) kinase inhibitory region and SOCS-1 mimetic bind to JAK2 autophosphorylation site: implications for the development of a SOCS-1 antagonist.' J. IMMUNOL. vol. 178, no. 8, 15 April 2007, pages 5058 - 5068 * |
Cited By (19)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| JP2013516170A (en) * | 2009-12-31 | 2013-05-13 | バイオリオン テクノロジーズ ビー.ブイ. | Interferon analog |
| WO2012013979A1 (en) * | 2010-07-28 | 2012-02-02 | The University Court Of The University Of Edinburgh | Anti-viral agent |
| US20130205416A1 (en) * | 2010-07-28 | 2013-08-08 | Anthony Nash | Anti-viral agent |
| US9951111B2 (en) * | 2011-06-21 | 2018-04-24 | University Of Florida Research Foundation, Incorporated | Type I interferon mimetics as therapeutics for cancer, viral infections, and multiple sclerosis |
| US20140134237A1 (en) * | 2011-06-21 | 2014-05-15 | University Of Florida Research Foundation, Inc. | Type i interferon mimetics as therapeutics for cancer, viral infections, and multiple sclerosis |
| CN102964432A (en) * | 2012-11-22 | 2013-03-13 | 中国科学院微生物研究所 | Method for restraining phosphorylation of M1 protein of influenza virus A and applications of method |
| CN102964432B (en) * | 2012-11-22 | 2014-02-05 | 中国科学院微生物研究所 | Method for restraining phosphorylation of M1 protein of influenza virus A and applications of method |
| CN103007350A (en) * | 2012-12-14 | 2013-04-03 | 中国人民解放军第三军医大学第二附属医院 | Modified rat accellular spinal cord bracket material and preparation method thereof |
| CN103266086B (en) * | 2013-06-15 | 2014-11-19 | 中国人民解放军第一七四医院 | Method for preparing dendritic cells for effectively submitting gastric cancer antigens |
| CN103266086A (en) * | 2013-06-15 | 2013-08-28 | 中国人民解放军第一七四医院 | Method for preparing dendritic cells for effectively submitting gastric cancer antigens |
| EP3096775A4 (en) * | 2014-01-24 | 2017-10-11 | University of Florida Research Foundation, Inc. | Socs mimetics for the treatment of diseases |
| US11603387B2 (en) | 2014-01-24 | 2023-03-14 | University Of Florida Research Foundation, Inc. | SOCS mimetics for the treatment of diseases |
| WO2015181427A1 (en) | 2014-05-28 | 2015-12-03 | Fundació Hospital Universitari Vall D'hebron - Institut De Recerca | Socs1-derived peptide for use in chronic complications relating to diabetes |
| US10532082B2 (en) | 2014-05-28 | 2020-01-14 | Fundació Hospital Universitari Vall D'hebron-Institut De Recerca | SOCS1-derived peptide for use in chronic complications of diabetes |
| CN110183515A (en) * | 2019-04-28 | 2019-08-30 | 浙江中医药大学 | It is a kind of for PTP1B detection polypeptide and include the fluorescence probe of the polypeptide |
| CN110183515B (en) * | 2019-04-28 | 2020-09-29 | 浙江中医药大学 | Polypeptide for PTP1B detection and fluorescent probe containing polypeptide |
| CN114502570A (en) * | 2019-07-16 | 2022-05-13 | 吉恩森有限公司 | Peptide therapeutics for autoimmune and inflammatory diseases |
| JP2022540498A (en) * | 2019-07-16 | 2022-09-15 | ジェンセン・カンパニー・リミテッド | Peptide therapeutics for autoimmune and inflammatory diseases |
| EP4001295A4 (en) * | 2019-07-16 | 2023-05-31 | Genesen Co., Ltd. | Peptide therapeutics for autoimmune diseases and inflammatory diseases |
Also Published As
| Publication number | Publication date |
|---|---|
| WO2010151495A3 (en) | 2011-04-28 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| WO2010151495A2 (en) | Materials and methods for treating and preventing viral infections | |
| Vilas Boas et al. | Antiviral peptides as promising therapeutic drugs | |
| Madavaraju et al. | Herpes simplex virus cell entry mechanisms: an update | |
| Galdiero et al. | Peptide inhibitors against herpes simplex virus infections | |
| Frey et al. | HSV-1-induced SOCS-1 expression in keratinocytes: use of a SOCS-1 antagonist to block a novel mechanism of viral immune evasion | |
| US9951111B2 (en) | Type I interferon mimetics as therapeutics for cancer, viral infections, and multiple sclerosis | |
| Rey-Jurado et al. | Contribution of autophagy to antiviral immunity | |
| US11130790B2 (en) | Cell penetrating peptides that inhibit IRF5 nuclear localization | |
| Siebert et al. | Tuftsin-properties and analogs | |
| US20130205416A1 (en) | Anti-viral agent | |
| ES2924521T3 (en) | HSV vectors for the administration of NT3, and treatment of CIPN | |
| US11304989B2 (en) | Peptides for use in the treatment of viral infections | |
| CA3173064A1 (en) | Soluble ace2 and fusion protein, and applications thereof | |
| Zhang et al. | Advances in developing ACE2 derivatives against SARS-CoV-2 | |
| Lalani et al. | Antiviral peptides against Enterovirus A71 causing hand, foot and mouth disease | |
| WO2019206285A1 (en) | Nucleic acid molecules and dual-functional peptides having antiviral activity and delivery activity, compositions and methods thereof | |
| ES2526060T3 (en) | Peptide and treatment for HIV-1 infection | |
| JP6910043B2 (en) | Hemagglutinin-binding peptide and preventive / therapeutic agents for influenza virus infections containing it | |
| RU2609857C1 (en) | Application of composition consisting of cationic ltp peptide and molecules of rna against respiratory viruses | |
| CN114853911A (en) | Trefoil factor 2/interferon alpha 2 fusion protein and application thereof in preventing and treating virus infectious diseases | |
| WO2017149098A1 (en) | Fusion respiratory syncytial virus inhibitors and use thereof | |
| WO2021046562A1 (en) | Antiviral peptoid compositions | |
| US20160289288A1 (en) | Type i interferon mimetics as therapeutics for cancer, viral infections, and other diseases | |
| US20240108713A1 (en) | Novel replication deficient influenza a virus inducing high levels of type i interferon | |
| US20200093888A1 (en) | Labyrinthopeptins as anti-viral agents |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| 121 | Ep: the epo has been informed by wipo that ep was designated in this application |
Ref document number: 10792548 Country of ref document: EP Kind code of ref document: A2 |
|
| 122 | Ep: pct application non-entry in european phase |
Ref document number: 10792548 Country of ref document: EP Kind code of ref document: A2 |
|
| NENP | Non-entry into the national phase in: |
Ref country code: DE |